Abstract
Owing to the paucity of information on the clinical outcomes in female patients with acute myocardial infarction (AMI) in relation to the comorbid disease burden, we explored the differences in their clinical outcomes and identified predictive indicators. A total of 3,419 female AMI patients were stratified into two groups: Group A (those with zero or one comorbid diseases) (n=1,983) and Group B (those with two to five comorbid diseases) (n=1,436). Five comorbid conditions were considered: hypertension, diabetes mellitus, dyslipidemia, prior coronary artery disease, and prior cerebrovascular accidents. The primary outcome was major adverse cardiac and cerebrovascular events (MACCEs). The incidence of MACCEs was higher in Group B than in Group A in both the unadjusted and propensity score-matched data. Among the comorbid conditions, hypertension, diabetes mellitus, and prior coronary artery disease were found to be independently associated with an increased incidence of MACCEs. Higher comorbid disease burden was positively associated with adverse outcomes in the female population with AMI. Since both hypertension and diabetes mellitus are modifiable and independent predictors of adverse outcomes after AMI, it may be necessary to focus on the optimal management of blood pressure and glucose levels to improve cardiovascular outcomes.
Keywords: Female, Multimorbidity, Myocardial infarction, Treatment outcome
INTRODUCTION
Cardiovascular disorders (CVDs) have been one of the primary causes of death in women for approximately a century. The total number of global female deaths attributable to CVDs gradually increased from 6.0 million in 1990 to 8.4 million in 2017.1 Women account for more than half of the nearly 1 million CVD-related deaths in the United States each year.2 Although both men and women share many risk factors for CVD, women tend to be at an increased risk.3 In women, the onset of CVD is typically 5-10 years later than that in men,4,5 and there is a remarkable increase of CVD risk during ages coinciding with menopause.6 That is, women aged 40 years and older experience hormonal and physical changes as well as body fat accumulation, which increases their susceptibility to CVD.7
Acute myocardial infarction (AMI), a subtype of CVD, is one of the leading causes of mortality. It is a significant public health concern and is closely related to several common comorbidities, such as hypertension, diabetes, and dyslipidemia.8 Female patients with AMI tend to be older and have a higher number of comorbidities than their male counterparts.9 With respect to treatment outcomes following percutaneous coronary intervention (PCI), women are susceptible to unfavorable outcomes, with higher incidences of adverse cardiovascular events and death than men.10 Despite mounting evidence that sex-dependent trends impact the clinical characteristics and treatment outcomes of AMI,3,11 the clinical outcomes of female patients with AMI in relation to comorbid disease burdens remain uncertain.
To address these uncertainties, we investigated the relationship between the quantity of significant comorbid conditions and clinical outcomes following AMI in female patients.
MATERIALS AND METHODS
1. Study design and data source
The Korean Acute Myocardial Infarction Registry (KAMIR) was established in 2005 by the Korean Society of Cardiology to determine the risk factors, clinical features, procedural findings, and medical treatments of the Korean AMI population and to improve their clinical outcomes.12 The KAMIR-National Institute of Health (KAMIR-NIH) database was established as part of a systematic and organized effort to develop a national registry funded by the National Institutes of Health aimed toward creating a better understanding of AMI in Korea. The KAMIR-NIH database includes real-world trends in treatment practices and post-treatment outcomes in Korean patients diagnosed with AMI.12 Clinical data of participants were acquired from this Korean population-based observational registry between November 2011 and December 2015.
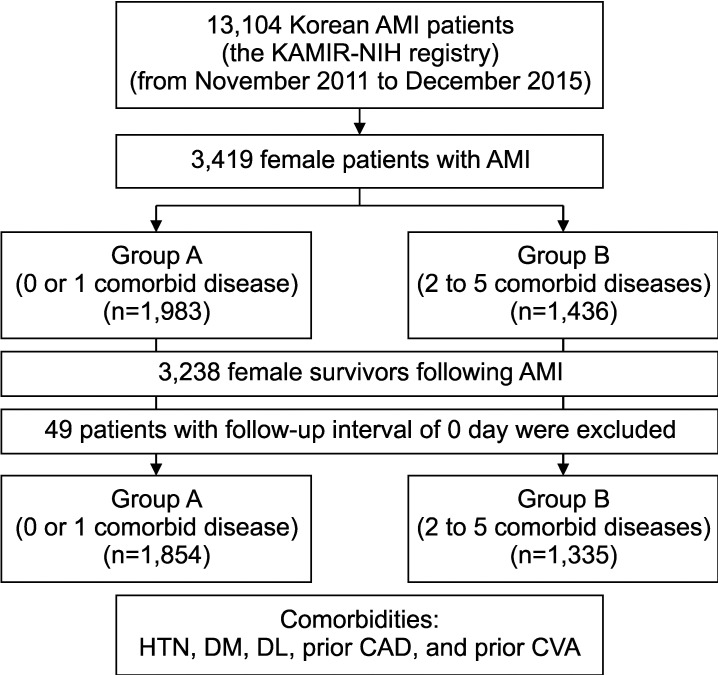
Among the 13,104 AMI patients in the KAMIR-NIH registry, we extracted the data of 3,419 female patients. All participants were stratified into two groups according to their comorbid disease burden: Group A (those with zero or one comorbid disease) (n=1,983) and Group B (those with two to five comorbid diseases) (n=1,436). We considered five comorbid conditions of interest: hypertension, diabetes mellitus, dyslipidemia, preexisting coronary artery disease (CAD), and prior cerebrovascular accident (CVA) (Fig. 1).
FIG. 1. Study population flow chart. Female patients with AMI were categorized into two groups according to their comorbid disease burden: Group A (those with zero or one comorbid disease) (n=1,983) and Group B (those with two to five comorbid diseases) (n=1,436). Five comorbid conditions were considered: HTN, DM, DL, prior CAD, and prior CVA. AMI: acute myocardial infarction, CAD: coronary artery disease, CVA: cerebrovascular accident, DL: dyslipidemia, DM: diabetes mellitus, HTN: hypertension, KAMIR-NIH: Korea Acute Myocardial Infarction-National Institutes of Health.
The study protocol was designed according to the ethical principles of the Declaration of Helsinki and was certified by the Institutional Review Board of Chonnam National University Hospital (Institutional Review Board No. CNUH-2022-112). The need for informed consent was waived considering the retrospective design of this study.
2. Definitions
Depending on contemporary guidelines and standards, AMI is diagnosed based on the presence of elevated cardiac biomarker levels and specific clinical manifestations, including: (i) AMI-related clinical symptoms, (ii) fresh T-wave inversion or ST-segment deviation on a 12-lead electrocardiogram, (iii) novel pathological Q-waves on a 12-lead electrocardiogram, and (iv) definite evidence of viable myocardium loss or detection of abnormal regional wall motion on imaging. ST-segment elevation myocardial infarction (STEMI) constitutes of an AMI with recently discovered ST segment elevation in >2 continuous leads on a 12-lead electrocardiogram.13 The presence of comorbid variables of interest was determined by either explicit documentation in medical records or existing medical treatments for the comorbid conditions. A family history of CAD was defined as the presence of a previous or current medical history of CAD or heart failure among any immediate family member of the patient. Intravascular imaging guidance during PCI comprised periprocedural use of intravascular ultrasound or optical coherence tomography. Left main coronary artery (LMCA) disease refers to the existence of a LMCA lesion with ≥50% angiographic narrowing. Multivessel CAD refers to significant angiographic narrowing in two or more coronary arteries, defined as either ≥70% narrowing in two or more coronary arteries or ≥70% narrowing in one coronary artery with ≥50% narrowing of the LMCA. The thrombolysis in myocardial infarction (TIMI) flow grading system was utilized to stratify the degree of antegrade coronary flow. To quantify heart function, the left ventricular ejection fraction (LVEF) was estimated using transthoracic echocardiography. An infarct-related artery (IRA) refers to a coronary artery, where plaque disruption and subsequent thrombus formation results in an AMI. Lesion characteristics were categorized as A/B1 or B2/C in accordance with the coronary lesion morphology criteria of the American College of Cardiology/American Heart Association (ACC/AHA).
3. Study outcomes
We investigated time-dependent incidences of adverse outcomes following AMI. We primarily established the incidence of major adverse cardiac and cerebrovascular events (MACCEs). MACCE was defined as the composite outcome of all-cause mortality, non-fatal myocardial infarction (NFMI), revascularization, CVA, rehospitalization, and stent thrombosis. Additionally, we established MACCE components. NFMI was defined as the recurrence of clinical symptoms and/or signs of angina, with increased levels of cardiac biomarker levels. Any revascularization was defined as repeated PCI for any segment of the epicardial coronary vessel or coronary artery bypass surgery. Rehospitalization was defined as the first hospital admission for angina or heart failure. Stent thrombosis was defined as being either definite or probable in accordance with the Academic Research Consortium.14
4. Statistical analysis
All data were analyzed using STATA (version 15.0, StataCorp, College Station, TX, USA) and Statistical Package for the Social Sciences (version 25.0, IBM Corp., Armonk, NY, USA). For the baseline characteristics, continuous variables, which were reported as means and standard deviations, were examined using Student’s t-test or Mann-Whitney test. Discrete variables, reported as frequencies and percentages, were examined using Pearson’s chi-square test, Fisher’s exact test, or the Mantel–Haenszel linear-by-linear association. p<0.05 was set as a reasonable cutoff value for statistical significance.
The primary goal of this analysis was to identify associations between comorbid disease burdens and an increased risk of MACCEs following AMI. This was examined using the Cox proportional-hazards regression. We selected 26 baseline covariates, which included the following: age, treatment delay (symptom-to-door time [S2DT] and door-to-balloon time [D2BT]), utilization of emergency medical service (EMS), Killip functional class, body mass index, smoking status, family history of CAD, serum creatinine level, medications at discharge (aspirin, P2Y12 inhibitors, beta-blockers, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, and statins), vascular access during PCI, use of glycoprotein IIb/IIIa inhibitors, use of image guidance during PCI, IRA, ACC/AHA lesion characteristics, TIMI flow grade, presence or absence of success during PCI, use of thrombolysis, LMCA disease, multivessel CAD, LVEF, and final diagnosis. The present study used propensity score matching (PSM) to reduce selection bias due to the heterogeneity of baseline characteristics between the two groups and determine the influence of comorbid disease burdens on clinical outcomes following AMI. The propensity score was constructed using the aforementioned 26 covariates. To illustrate the cumulative estimated incidence of MACCE in both groups, Kaplan-Meier survival curves were constructed.
We further investigated independent predictors for MACCE using a Cox proportional-hazards regression analysis. In this statistical analysis, we selected 30 baseline covariates, which included the following: age, total ischemic time (TIT), utilization of EMS, Killip functional class, body mass index, smoking status, family history of CAD, serum creatinine level, medications at discharge (aspirin, P2Y12 inhibitors, beta-blockers, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, and statins), vascular access during PCI, use of glycoprotein IIb/IIIa inhibitors, use of image guidance during PCI, IRA, ACC/AHA lesion characteristics, TIMI flow grade, presence or absence of success during PCI, use of thrombolysis, LMCA disease, multivessel CAD, LVEF, and final diagnosis. The receiver-operating characteristic (ROC) curve analyses and area under curve (AUC) were used to estimate the discriminatory power of this Cox proportional-hazards regression analysis.
RESULTS
1. Baseline characteristics
Among a total of 3,419 female patients with confirmed AMI, we included a total of 3,238 survivors into the statistical analyses. Among them, patients with one comorbid disease (n=1,203) were ranked first, followed by those with two comorbid diseases (n=915), those with no comorbid disease (n=679), those with three comorbid diseases (n=350), those with four comorbid diseases (n=82), and those with five comorbid diseases (n=9) (Fig. 2). The baseline characteristics of the participants are summarized in Tables 1 and 2. Group A patients were younger and more likely to smoke than those in Group B. Despite similar S2DT between both groups, patients in Group B exhibited an in-hospital delay with prolongation of D2BT, resulting in prolongation of TIT. Patients in Group B had higher rates of Killip classes III–IV. Group B patients also tended to be more obese, had worse renal and cardiac functions with higher serum creatinine levels, and a lower LVEF relative to Group A patients. Notably, STEMI occurred more frequently in patients with Group A.
FIG. 2. The number of comorbid disease burden in female patients with confirmed AMI. AMI: acute myocardial infarction.
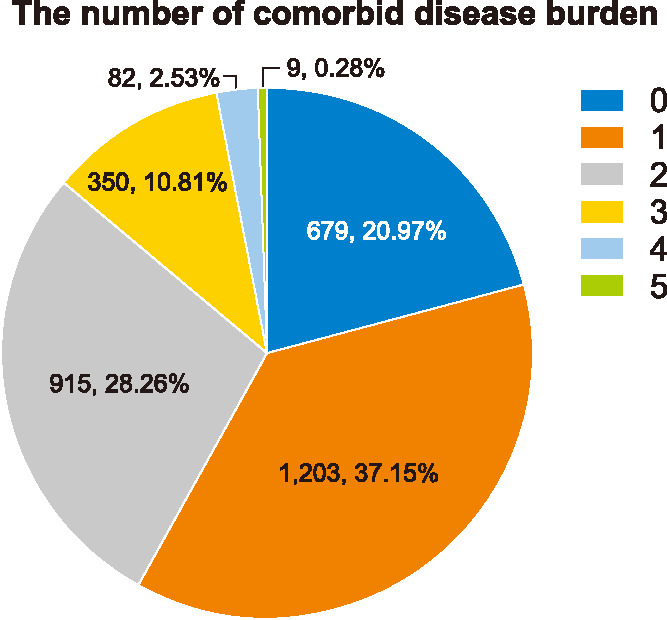
TABLE 1. Baseline characteristics of the survived participants.
Values are presented as number (percentage) for categorical values and means ± standard deviation for continuous variables.
BMI: body mass index, CAD: coronary artery disease, CVA: cerebrovascular accident, D2BT: door-to-balloon time, EMS: emergency medical service, LVEF: left ventricular ejection fraction, S2DT: symptom-to-door time, STEMI: ST-segment elevation myocardial infarction, TIT: total ischemic time.
TABLE 2. Procedural profiles and medications at discharge.
Values are presented as number (percentage) for categorical values.
ACC/AHA: the American College of Cardiology/the American Heart Association, ACE: angiotensin-converting enzyme, ARB: angiotensin receptor blocker, CAD: coronary artery disease, GPIIb/IIIa: glycoprotein IIb/IIIa, LAD: left anterior descending coronary artery, LCX: left circumflex coronary artery, LMCA: left main coronary artery, PCI: percutaneous coronary intervention, RCA: right coronary artery, TIMI: Thrombolysis In Myocardial Infarction.
Groups A and B patients underwent PCI at a similar rate with comparable success. Relative to those in Group A, patients in Group B had higher rates of femoral-access PCI and multivessel CAD as well as lower rates of TIMI flow grade of 0 (no flow) to 1 (penetration without perfusion). Some discharge medications including aspirin, P2Y12 inhibitors, and statins were more frequently prescribed in Group A than in Group B.
The differences in baseline characteristics between the two groups were adequately balanced after adjusting for covariates using PSM.
2. Clinical outcomes
Among a total of 3,238 surviving patients, patients with a post-discharge follow-up interval of 0 days were excluded. A total of 3,190 consecutive patients were included in the survival analysis. The median follow-up period was 2.99 years. We summarized the adverse outcomes following AMI during the 3-year follow-up (Tables 3 and 4, Fig. 3). The treatment estimates contained MACCEs and their individual components, including all-cause mortality, cardiac death, non-cardiac death, NFMI, any revascularization, CVA, rehospitalization, and stent thrombosis.
TABLE 3. Three-year clinical outcomes in propensity score matched patients.
Values are presented as percentage (number) for categorical values.
CI: confidence interval, CVA: cerebrovascular accident, HR: hazard ratio, MACCE: major adverse cardiac and cerebrovascular events, NFMI: non-fatal myocardial infarction, PSM: propensity score matching.
TABLE 4. Crude incidences of three-year clinical outcomes in 3,190 participants.
CI: confidence interval, CVA: cerebrovascular accident, HR: hazard ratio, MACCE: major adverse cardiac and cerebrovascular events, NFMI: non-fatal myocardial infarction.
FIG. 3. Event rates of MACCE for all the patients after a 3-year follow-up (before and after PSM-adjusted analysis). Kaplan–Meier curves are shown for cumulative event rates stratified according to comorbidity burden. MACCE: major adverse cardiac and cerebrovascular accident, PSM: propensity score matching.
In the unadjusted data (Table 3), the incidence of all adverse clinical outcomes was higher in Group B than in Group A, except for CVA and stent thrombosis. The incidence of most outcome variables, except for stent thrombosis, tended to increase according to the number of comorbid disease burden (Table 4). In PSM-adjusted data (Table 3), the incidence of adverse clinical outcomes including MACCE, all-cause mortality, cardiac death, any revascularization, and rehospitalization remained higher in Group B.
3. Independent predictors for MACCE
We conducted a Cox proportional hazards regression analysis using 30 covariates (by adding the five items of comorbid diseases to the 25 covariates) to verify independent predictors of MACCEs. The results, as summarized in Table 5, showed that hypertension, diabetes mellitus, and prior CAD, were independently associated with an increased incidence of MACCE. Other associated variables included age ≥75 years, Killip classes III–IV, family history of CAD, creatinine ≥1.5 mg/dL, LVEF <40%, femoral-access PCI, RCA as an IRA, multivessel CAD, and beta-blockers as a discharge medication. A time-dependent ROC curve analysis was conducted, and the AUC was 0.725, indicating an acceptable discriminatory ability (Supplementary Fig. 1).
TABLE 5. Independent predictors for MACCE (Cox proportional-hazards regression analysis for MACCE).
ACC/AHA: the American College of Cardiology/the American Heart Association, ACE: angiotensin-converting enzyme, ARB: angiotensin receptor blocker, BMI: body mass index, CAD: coronary artery disease, CI: confidence interval, CVA: cerebrovascular accident, HR: hazard ratio, LAD: left anterior descending coronary artery, LCX: left circumflex coronary artery, LMCA: left main coronary artery, LVEF: left ventricular ejection fraction, OR: odds ratio, PCI: percutaneous coronary intervention, RCA: right coronary artery, STEMI: ST-segment elevation myocardial infarction, TIMI: Thrombolysis In Myocardial Infarction, TIT: total ischemic time.
DISCUSSION
In the literature review, there is mounting evidence about gender difference in outcomes following PCI in patients with AMI. They have demonstrated that female patients tend to have poorer outcomes than their male counterparts.3,15,16,17 According to a clinical study based on the KAMIR-NIH cohort, female patients had greater burdens of comorbidities and worse 30-days and 1-year outcomes after PCI than male patients.3 Given the relatively high comorbidities of women, and mounting evidence of the association of cardiovascular comorbidities with outcomes in patients after AMI,18 it could be inferred that clinical prognosis may be stratified in accordance to comorbidities among female patients with AMI.
In this study, we analyzed the comorbid disease burdens of 3,238 surviving female patients with AMI using data extracted from the KAMIR-NIH observational cohort. Clinical outcomes, including MACCE, were better in patients with a lower comorbid disease burden. The number of comorbid diseases was 2.41±0.64 and 0.64±0.48 for patients in Group B and Group A, respectively.
Patients in Group B were older, less likely to smoke, and more likely to present with atypical angina. Given that elderly individuals are more likely to experience atypical angina or no chest pain,19 this finding appears to be reasonable. Although statistically insignificant, patients in Group B tended to utilize more EMS due to their advanced age, higher comorbid disease burdens, and greater clinical severity. Relative to Group A, Group B had an in-hospital delay between admission and PCI along with prolonged D2BTs. This finding was attributable to the lower incidence of STEMI which is more time sensitive.
Patients in Group B had a greater incidence of multivessel CAD and lower rates of TIMI flow grades of 0-1; this was expected, given that multivessel CAD is associated with increased age, diabetes mellitus, and higher creatinine level,20 which characterized patients in Group B. The higher prevalence of TIMI flow grades 0-1 in Group A was sufficiently accounted for by higher rates of STEMI, which is generally caused by a complete occlusion of the IRA. In contrast, non-STEMI is caused by a transient or incomplete occlusion.21
Hypertension was the most prevalent type of comorbid disease in both groups (47.4% of patients in Group A vs. >90% in Group B), followed by diabetes mellitus. Our female-centered study showed a high hypertension prevalence in line with reports that about 25% of Korean women over the age of 20 years have hypertension.22 Hypertension induces shear stress on arterial vasculature and vascular inflammation, which contributes to the development of atherosclerosis and arterial stiffness.23 Diabetes mellitus may enhance arterial stiffness via multiple processes within the vascular bed, including changes in intra-arterial components, increased oxidative stress, and low-grade inflammation.24 Moreover, many clinical studies have emphasized that these comorbid diseases are often associated with adverse events following AMI.25
Patients in Group B experienced worse adverse clinical outcomes than those in Group A; this was consistent even after the PSM adjustment. It may have been influenced by Group B’s patient characteristics known to influence outcomes following AMI, such as advanced age, a higher degree of Killip functional class, elevated creatinine levels, and lower LVEF.26,27,28 Additionally, D2BT influences mortality rates in AMI patients,29 accounting for the poor outcomes in Group B with a prolonged D2BT. Comorbid disease variables were also related with poor clinical outcomes after AMI.25
In the Cox proportional-hazards logistic regression analysis (Table 4), we verified that hypertension, diabetes mellitus, and prior CAD were positively associated with MACCE incidence. Both hypertension and diabetes mellitus are major risk factors for CVD that are associated with worse cardiovascular outcomes such as MACCE in patients with coexisting CAD.30 Meanwhile, as patients with preexisting CAD tend to be older with a higher incidence of coexisting comorbid diseases,31 it seems reasonable that CAD may be an independent predictor of MACCE. This is consistent with the results of historical clinical studies.32 Unlike preexisting CAD, both hypertension and diabetes mellitus are modifiable predictors and also, they were more frequently seen in female patients with AMI than in male counterparts.3 Therefore, they can be managed sufficiently by controlling the blood pressure and glucose levels.
We also investigated the in-hospital outcomes between the two groups, as described in Supplementary Table 1. Patients in Group B experienced higher rates of new-onset heart failure and acute kidney injury and received more cardiopulmonary resuscitation than their counterparts in Group A. Higher Killip class, reduced creatinine clearance, reduced LVEF, hypertension, and diabetes, are associated with an increased risk of in-hospital outcomes,33,34 consistent with our study’s findings. Despite these differences, the incidence of in-hospital deaths was similar in both groups, implying that both patient groups received a similar level of appropriate treatment.
In addition, we further analyzed patient mortality during index hospitalization between the two groups, as summarized in Supplementary Table 2. Among the deceased patients in Group A, there was a higher proportion of patients that were ≥75 years of age with LMCA disease; however, there were fewer patients with multivessel CAD than in Group B. This trend was not surprising, given that comorbid conditions, including hypertension and diabetes mellitus, may enhance the risk of more extensive coronary artery plaques.35 Nonetheless, as both advanced age and LMCA CAD are correlated with worse in-hospital outcomes,36 the incidence of in-hospital death was comparable in both groups despite inter-group inequality of comorbid disease burden attributable to the relatively lower comorbid disease burden in Group A.
Although our results highlight the association between comorbid disease burden and outcomes in female patients with AMI, several limitations need to be discussed. Primarily, it is impossible to explain the causal relationship between comorbid disease burden and clinical outcomes because the KAMIR-NIH registry is an observational nonrandomized cohort. Second, despite our endeavors to eliminate selection bias using PSM, selection bias may have persisted due to the exclusion of data with missing values and other unmeasured confounders. Prospective randomized control studies are required to further validate this theory. Third, since the KAMIR-NIH registry was established from November 2011 to December 2015, the database used in the present study does not contain any information on several novel drugs for CVDs expected to improve the cardiovascular outcomes of these patients such as sacubitril/valsartan, sodium-glucose cotransporter-2 inhibitors, and proprotein convertase subtilisin/kexin type 9 inhibitors. Finally, the hypothesis that effective management of hypertension and diabetes mellitus can reduce adverse outcomes after AMI should also be evaluated.
In conclusion, a high comorbid disease burden was associated with poor clinical outcomes in the female AMI population. Since hypertension and diabetes mellitus are independent and modifiable predictors of adverse outcomes after AMI, it may be necessary to focus on their optimal management to improve cardiovascular outcomes. Prospective randomized studies are imperative to further examine and validate this hypothesis.
ACKNOWLEDGEMENTS
This work was supported by grants from the Korean Health Technology R&D Project, Ministry of Health & Welfare [grant number HI13C1527], and Research of Korea Centers for Disease Control and Prevention [grant number 2016-ER6304-01], Republic of Korea. We politely state that this research article is a continuation of work presented in the Master’s thesis of Jeong Shim Kim.
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
SUPPLEMENTARY MATERIALS
The ROC curve at 3 years in the Cox proportional hazards regression analysis for MACCE. AUC: area under curve, MACCE: major adverse cardiac and cerebrovascular accident, ROC: receiver-operating characteristic.
In-hospital outcomes clinical outcomes during index hospitalization
Baseline characteristics of 181 female patients who were deceased during the index hospitalization
References
- 1.Jagannathan R, Patel SA, Ali MK, Narayan KMV. Global updates on cardiovascular disease mortality trends and attribution of traditional risk factors. Curr Diab Rep. 2019;19:44. doi: 10.1007/s11892-019-1161-2. [DOI] [PubMed] [Google Scholar]
- 2.Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, et al. American Heart Association. Effectiveness-based guidelines for the prevention of cardiovascular disease in women--2011 update: a guideline from the American Heart Association. J Am Coll Cardiol. 2011;57:1404–1423. doi: 10.1016/j.jacc.2011.02.005. Erratum in: J Am Coll Cardiol 2012;59:1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee M, Kim DW, Park MW, Lee K, Chang K, Chung WS, et al. Gender differences in clinical outcomes of acute myocardial infarction undergoing percutaneous coronary intervention: insights from the KAMIR-NIH Registry. J Geriatr Cardiol. 2020;17:680–693. doi: 10.11909/j.issn.1671-5411.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gili M, Sala J, López J, Carrión A, Béjar L, Moreno J, et al. [Impact of comorbidities on in-hospital mortality from acute myocardial infarction, 2003-2009] Rev Esp Cardiol. 2011;64:1130–1137. doi: 10.1016/j.recesp.2011.07.010. Spanish. [DOI] [PubMed] [Google Scholar]
- 5.Bairey Merz CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, Olson M, et al. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: Part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol. 2006;47(3 Suppl):S21–S29. doi: 10.1016/j.jacc.2004.12.084. [DOI] [PubMed] [Google Scholar]
- 6.El Khoudary SR, Aggarwal B, Beckie TM, Hodis HN, Johnson AE, Langer RD, et al. American Heart Association Prevention Science Committee of the Council on Epidemiology and Prevention; Council on Cardiovascular and Stroke Nursing. Menopause transition and cardiovascular disease risk: implications for timing of early prevention: a scientific statement from the American Heart Association. Circulation. 2020;142:e506–e532. doi: 10.1161/CIR.0000000000000912. [DOI] [PubMed] [Google Scholar]
- 7.Garcia M, Mulvagh SL, Merz CN, Buring JE, Manson JE. Cardiovascular disease in women: clinical perspectives. Circ Res. 2016;118:1273–1293. doi: 10.1161/CIRCRESAHA.116.307547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–477. doi: 10.1093/eurheartj/ehz425. Erratum in: Eur Heart J 2020;41:4242. [DOI] [PubMed] [Google Scholar]
- 9.Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N Engl J Med. 1999;341:217–225. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 10.Clayton TC, Pocock SJ, Henderson RA, Poole-Wilson PA, Shaw TR, Knight R, et al. Do men benefit more than women from an interventional strategy in patients with unstable angina or non-ST-elevation myocardial infarction? The impact of gender in the RITA 3 trial. Eur Heart J. 2004;25:1641–1650. doi: 10.1016/j.ehj.2004.07.032. [DOI] [PubMed] [Google Scholar]
- 11.Batchelor WB, Anstrom KJ, Muhlbaier LH, Grosswald R, Weintraub WS, O’Neill WW, et al. Contemporary outcome trends in the elderly undergoing percutaneous coronary interventions: results in 7,472 octogenarians. National Cardiovascular Network Collaboration. J Am Coll Cardiol. 2000;36:723–730. doi: 10.1016/s0735-1097(00)00777-4. [DOI] [PubMed] [Google Scholar]
- 12.Kim JH, Chae SC, Oh DJ, Kim HS, Kim YJ, Ahn Y, et al. Korea Acute Myocardial Infarction-National Institutes of Health Registry Investigators. Multicenter cohort study of acute myocardial infarction in Korea-interim analysis of the Korea Acute Myocardial Infarction Registry-National Institutes of Health registry. Circ J. 2016;80:1427–1436. doi: 10.1253/circj.CJ-16-0061. [DOI] [PubMed] [Google Scholar]
- 13.Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC) Eur Heart J. 2016;37:267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 14.Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Academic Research Consortium. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115:2344–2351. doi: 10.1161/CIRCULATIONAHA.106.685313. [DOI] [PubMed] [Google Scholar]
- 15.Kelsey SF, James M, Holubkov AL, Holubkov R, Cowley MJ, Detre KM. Results of percutaneous transluminal coronary angioplasty in women. 1985-1986 National Heart, Lung, and Blood Institute’s Coronary Angioplasty Registry. Circulation. 1993;87:720–727. doi: 10.1161/01.cir.87.3.720. [DOI] [PubMed] [Google Scholar]
- 16.Malenka DJ, O’Connor GT, Quinton H, Wennberg D, Robb JF, Shubrooks S, et al. Northern New England Cardiovascular Disease Study Group. Differences in outcomes between women and men associated with percutaneous transluminal coronary angioplasty. A regional prospective study of 13,061 procedures. Circulation. 1996;94(9 Suppl):II99–II104. [PubMed] [Google Scholar]
- 17.Milcent C, Dormont B, Durand-Zaleski I, Steg PG. Gender differences in hospital mortality and use of percutaneous coronary intervention in acute myocardial infarction: microsimulation analysis of the 1999 nationwide French hospitals database. Circulation. 2007;115:833–839. doi: 10.1161/CIRCULATIONAHA.106.664979. [DOI] [PubMed] [Google Scholar]
- 18.Baechli C, Koch D, Bernet S, Gut L, Wagner U, Mueller B, et al. Association of comorbidities with clinical outcomes in patients after acute myocardial infarction. Int J Cardiol Heart Vasc. 2020;29:100558. doi: 10.1016/j.ijcha.2020.100558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brieger D, Eagle KA, Goodman SG, Steg PG, Budaj A, White K, et al. GRACE Investigators. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004;126:461–469. doi: 10.1378/chest.126.2.461. [DOI] [PubMed] [Google Scholar]
- 20.José de Carvalho Cantarelli M, Castello HJ, Gonçalves R, Gioppato S, Batista de Freitas Guimarães J, Pracchia Ribeiro EK, et al. [Independent predictors of multivessel coronary artery disease: results from Angiocardio Registry] Rev Bras Cardiol Invasiva. 2015;23:266–270. Portuguese. [Google Scholar]
- 21.Karwowski J, Poloński L, Gierlotka M, Ciszewski A, Hawranek M, Bęćkowski M, et al. Total coronary occlusion of infarct-related arteries in patients with non-ST-elevation myocardial infarction undergoing percutaneous coronary revascularisation. Kardiol Pol. 2017;75:108–116. doi: 10.5603/KP.a2016.0130. [DOI] [PubMed] [Google Scholar]
- 22.Kim HC, Cho SMJ, Lee H, Lee HH, Baek J, Heo JE Korean Society of Hypertension (KSH) – Hypertension Epidemiology Research Working Group. Korea hypertension fact sheet 2020: analysis of nationwide population-based data. Clin Hypertens. 2021;27:8. doi: 10.1186/s40885-021-00166-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu D, Kassab GS. Role of shear stress and stretch in vascular mechanobiology. J R Soc Interface. 2011;8:1379–1385. doi: 10.1098/rsif.2011.0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Oliveira Alvim R, Santos PCJL, Musso MM, de Sá Cunha R, Krieger JE, Mill JG, et al. Impact of diabetes mellitus on arterial stiffness in a representative sample of an urban Brazilian population. Diabetol Metab Syndr. 2013;5:45. doi: 10.1186/1758-5996-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee MG, Jeong MH, Lee KH, Park KH, Sim DS, Yoon HJ, et al. Prognostic impact of diabetes mellitus and hypertension for mid-term outcome of patients with acute myocardial infarction who underwent percutaneous coronary intervention. J Cardiol. 2012;60:257–263. doi: 10.1016/j.jjcc.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 26.Widimsky P, Motovská Z, Bílková D, Aschermann M, Groch L, Zelízko M. The impact of age and Killip class on outcomes of primary percutaneous coronary intervention. Insight from the PRAGUE-1 and -2 trials and registry. EuroIntervention. 2007;2:481–486. [PubMed] [Google Scholar]
- 27.Kümler T, Gislason GH, Kober L, Gustafsson F, Schou M, Torp-Pedersen C. Renal function at the time of a myocardial infarction maintains prognostic value for more than 10 years. BMC Cardiovasc Disord. 2011;11:37. doi: 10.1186/1471-2261-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sutton NR, Li S, Thomas L, Wang TY, de Lemos JA, Enriquez JR, et al. The association of left ventricular ejection fraction with clinical outcomes after myocardial infarction: findings from the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry-Get With the Guidelines (GWTG) Medicare-linked database. Am Heart J. 2016;178:65–73. doi: 10.1016/j.ahj.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Brodie BR, Gersh BJ, Stuckey T, Witzenbichler B, Guagliumi G, Peruga JZ, et al. When is door-to-balloon time critical? Analysis from the HORIZONS-AMI (Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction) and CADILLAC (Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications) trials. J Am Coll Cardiol. 2010;56:407–413. doi: 10.1016/j.jacc.2010.04.020. Erratum in: J Am Coll Cardiol 2010;56:1168. [DOI] [PubMed] [Google Scholar]
- 30.Wright AK, Kontopantelis E, Emsley R, Buchan I, Mamas MA, Sattar N, et al. Cardiovascular risk and risk factor management in type 2 diabetes mellitus. Circulation. 2019;139:2742–2753. doi: 10.1161/CIRCULATIONAHA.118.039100. [DOI] [PubMed] [Google Scholar]
- 31.Motivala AA, Tamhane U, Ramanath VS, Saab F, Montgomery DG, Fang J, et al. A prior myocardial infarction: how does it affect management and outcomes in recurrent acute coronary syndromes? Clin Cardiol. 2008;31:590–596. doi: 10.1002/clc.20356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kang SH, Ahn JM, Lee CH, Lee PH, Kang SJ, Lee SW, et al. Differential event rates and independent predictors of long-term major cardiovascular events and death in 5795 patients with unprotected left main coronary artery disease treated with stents, bypass surgery, or medication: insights from a large international multicenter registry. Circ Cardiovasc Interv. 2017;10:e004988. doi: 10.1161/CIRCINTERVENTIONS.116.004988. [DOI] [PubMed] [Google Scholar]
- 33.Shah RV, Holmes D, Anderson M, Wang TY, Kontos MC, Wiviott SD, et al. Risk of heart failure complication during hospitalization for acute myocardial infarction in a contemporary population: insights from the National Cardiovascular Data ACTION Registry. Circ Heart Fail. 2012;5:693–702. doi: 10.1161/CIRCHEARTFAILURE.112.968180. [DOI] [PubMed] [Google Scholar]
- 34.Sun YB, Liu BC, Zou Y, Pan JR, Tao Y, Yang M. Risk factors of acute kidney injury after acute myocardial infarction. Ren Fail. 2016;38:1353–1358. doi: 10.3109/0886022X.2016.1148558. [DOI] [PubMed] [Google Scholar]
- 35.Jiang Y, Li Y, Shi K, Wang J, Qian WL, Yan WF, et al. The additive effect of essential hypertension on coronary artery plaques in type 2 diabetes mellitus patients: a coronary computed tomography angiography study. Cardiovasc Diabetol. 2022;21:1. doi: 10.1186/s12933-021-01438-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nishihira K, Kojima S, Takegami M, Honda S, Nakao YM, Takahashi J, et al. JAMIR Investigators. Clinical characteristics and in-hospital mortality according to left main and non-left main culprit lesions-report from the Japan Acute Myocardial Infarction Registry (JAMIR) Circ Rep. 2019;1:601–609. doi: 10.1253/circrep.CR-19-0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The ROC curve at 3 years in the Cox proportional hazards regression analysis for MACCE. AUC: area under curve, MACCE: major adverse cardiac and cerebrovascular accident, ROC: receiver-operating characteristic.
In-hospital outcomes clinical outcomes during index hospitalization
Baseline characteristics of 181 female patients who were deceased during the index hospitalization