Abstract
Introduction: Spinal anesthesia is commonly used for various surgical procedures. Prediction of spinal anesthesia block height is always a challenging task for anesthetists. Higher than desired levels of spinal anesthesia blocks are associated with serious side effects, while inadequate block height does not provide satisfactory surgical anesthesia. In this study, we observed the relationship between the ratio of trunk length (TL) and square of the abdominal circumference (AC2) and spinal anesthesia sensory block height in geriatric patients undergoing transurethral resection of the prostate (TURP).
Material & Methods: This is a cross-sectional study conducted at the Aga Khan University Hospital Karachi, Pakistan, on geriatric patients undergoing TURP under spinal anesthesia. Forty-three elderly patients (American Society of Anaesthesiology level I-III) between 60 and 80 years were recruited for the study. In hospital wards, trunk length (TL) and abdominal circumference were recorded before the procedure. In the operating rooms, spinal anesthesia was performed at L3-L4 intervertebral space with 0.5% hyperbaric bupivacaine 10mg (2mls). Block height was measured by the placement of ice pads at different dermatomes. Spearman rank correlation coefficient was used to analyze the physical parameters (TL/AC2) and spinal anesthesia block height.
Results: The ratio of trunk length and square of the abdominal circumference (TL/AC2) correlates with spinal anesthesia block height in geriatric patients, where the spearman rank correlation coefficient was r =-0.284 with p = 0.015.
Conclusion: The ratio of the long axis (TL) and transection area of the abdomen (AC2), which coincides with (TL/AC2), correlated with spinal anesthesia sensory block height. Hence, elderly patients with a low TL/AC2 ratio will have higher block height after spinal anesthesia.
Keywords: transurethral resection of prostate, block height, abdominal circumference, trunk length, turp, spinal anaesthesia
Introduction
Spinal anesthesia is commonly used for various surgical procedures in obstetrics, orthopedics, gynecology, and urology. It is well known that spinal anesthesia is associated with procedure-related complications, including post-dural puncture headache (PDPH) (0.16%-1.3%) [1], transient neurological symptoms (10.2%-24%) [2], spinal epidural hematoma (1:2,700-1:190,000) [3], and excessive block height (0.2%) [4].
Excessive block height is associated with a higher incidence of adverse effects of spinal anesthesia, such as nausea, vomiting, bradycardia, and hypotension [5]. However, the inadequate spread of local anesthetics does not provide satisfactory surgical conditions [6]. Therefore, it is important to be able to predict and control the intrathecal spread of local anesthetics and spinal anesthesia block height (SABH).
Factors that affect SABH have been investigated in multiple studies, and contributing factors include clinical technique used, characteristics of drug solution injected, and patients’ general features, i.e., age, height, weight, and sex [7,8]. In the geriatric population, there is a small but significant increase in SABH, rate of onset of motor block, and cardiovascular instability regardless of the drug solution used [9-13]. These changes are linked to age-related changes in spinal anatomy, nerve physiology, and cardiovascular reflexes [7]. Increased intra-abdominal pressure, changes in anteroposterior spinal curves, and lumber lordosis are also associated with increased SABH [14-17]. However, measuring these parameters is difficult in daily practice.
Hartwell et al. found that vertebral column length had a much better correlation than body height to predict the spread of subarachnoid hyperbaric bupivacaine in term parturient [18]. Lee and co-researchers found in 30 terms Taiwanese parturient that Trunk Length (TL)/Abdominal Circumference2 (AC2) values, which simulated the ratio of the long axis and transection area of the abdomen, correlate with maximal SABH, and parturient with low TL/AC2 values tended to have high SABH with standardized spinal anesthesia [8].
The study mentioned above showed clinically significant results in term parturient. The parameter TL/AC2 was statistically correlated with high SABH (Spearman correlation coefficient, -0.45 with p < 0.02) [8]. However, no such relationship was investigated in geriatric patients shown to have variation in SABH compared to younger adults [9-13]. Geriatric patients often have multiple co-morbidities, and side effects or complications of spinal anesthesia are bound to be more troublesome for these patients [19]. Therefore, to avoid complications or side effects, it is important to be able to predict and control SABH more precisely and accurately in geriatric patients. This study has improved our understanding of the relationship of the SABH with TL/AC2 in the geriatric patient population.
Materials and methods
This cross-sectional study was conducted in the operating rooms of Aga Khan University Hospital in Karachi, Pakistan, from 20th December 2016 to 19th June 2017. The sample size was calculated based on previous research in which the correlation coefficient between the ratio of TL/AC2 and SABH was -0.45 (p-value 0.02) [8]. For a spearman correlation coefficient of at least 0.45, which is the minimum value to have clinical interest, and the probability of type I error ≤ 0.05, the sample size must be at least 29 for 80% power and 40 for 90% power. To increase power, we included 45 patients in this study. A non-probability consecutive sampling technique was applied. All adult male (American Society of Anaesthesiology level I-III) patients, aged 60 to 80, undergoing Trans-Uretheral Resection of Prostate (TURP) electively under spinal anesthesia, were included in the study. On the other hand, exclusion criteria included obesity (BMI > 30 kg/m2) [20,21], cachexia (BMI < 20kg/m2) [22], patient refusal, known spinal abnormalities (kyphosis, scoliosis, lordosis), history of spinal surgeries, large abdominal mass (in the past or present), tumor or ascites, and height less than 150 cm and more than 170 cm.
Data collection procedure
After approval from the ethical review committee of Aga Khan University, written informed consent was obtained from all the participants. Before coming to the operating room, measurements (TL/AC2) of all the patients fulfilling the inclusion criteria were taken in the ward. Abdominal circumference was measured (in cm) in the supine position with a measuring tape at the level of the umbilicus at end-expiration, and trunk length (in cm) in the left lateral decubitus position from C7 spinous process to sacral hiatus. After starting intravenous fluids (0.9% normal saline) and establishing routine peri-operative monitoring (i.e., non-invasive blood pressure, pulse oximeter, three lead ECG), spinal anesthesia was administered with an aseptic technique using a 25-gauge pencil-point spinal needle wherein 0.5% hyperbaric bupivacaine (10 mg) was injected at L3-L4 spinal level after confirmation of free flow of cerebrospinal fluid (CSF) in sitting position. Patients were put in a supine position immediately after the successful spinal injection. Sensory block height was measured by the application of an ice pad over different dermatomes every five minutes after the successful spinal injection for 20 minutes. Surgery was allowed to start after the achievement of the T-10 level block.
Data analysis procedure
All statistical analyses were performed using IBM Corp. Released 2010. IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp. Mean and standard deviation (SD) were computed for age, height, weight, trunk length, abdominal circumference, and the ratio of TL/(AC)2. Frequency and percentage were calculated for ASA level. Spearman correlation (non-normal data) between the ratio of TL/(AC)2 and maximum block height (spinal level) was computed, and p≤0.05 was considered significant. Stratification analysis was performed to observe the confounding effect of AC and BMI on the correlation between TL/(AC)2 and maximum block height (spinal level).
Operational definitions
Trunk Length in cm: In left lateral decubitus position from C-7 spinous process to sacral hiatus with measuring tape [8]. C-7 spinous process: The largest and most inferior spinous process in the neck. It can be identified with the palpation/flexion/extension method [23]. Sacral hiatus: The opening into the vertebral canal in the midline of the dorsal surface of the sacrum. It can be identified by palpation of sacral cornua at the lower end of the sacrum. Abdominal Circumference in cm: In supine position at the level of umbilicus with measuring tape. Sensory block: Unable to appreciate cold sensations when ice cube placed over the anesthetized area. Block Height: Unable to appreciate cold sensations at the level of Umbilicus = T-10, Xiphoid process = T-6, Nipple = T-4. L3-L4. Level identification: The line joining the superior aspect of the iliac crests posteriorly (the intercristal line) is L4-L5, and the interspace is just above L4-L5. Geriatric age: Chronological age of 60 years and above [24].
Results
A total of 45 geriatric patients, scheduled to undergo TURP under spinal anesthesia, and fulfilling inclusion criteria, were enrolled for the study. Two of them refused, perioperatively, repeated measurements of sensory block height with ice pad placement and hence were excluded from the study. The rest of the 43 patients were included in the study. Out of 43 patients, 24 were between 60 and 70 years, and 19 were between 70 and 80 years (Figure 1).
Figure 1. Age Distribution of the Patients.
However, the age of the patients was 69 +/-6.47 (Mean +/- SD) years, as shown in Table 1. Other demographic variables are also shown in Table 1. Regarding ASA status, 2.33% were ASA-I, 67.44% were ASA-II, and 30.23% were ASA-III, as shown in Figure 2.
Table 1. Demographic Characteristics of Patients n= 43.
| Variables | Mean | SD | 95% Confidence Interval for Mean | Min | Max | |
| LowerBound | UpperBound | |||||
| Age (Years) | 69 | 6.47 | 67.01 | 70.99 | 60 | 80 |
| Weight (kg) | 71.08 | 10.73 | 67.78 | 74.38 | 50 | 90 |
| Height (cm) | 164.84 | 5.48 | 163.15 | 166.52 | 150 | 170 |
| BMI (kg/m2) | 26.21 | 3.09 | 25.25 | 27.16 | 20.02 | 31.14 |
Figure 2. ASA Distribution of the Patients.
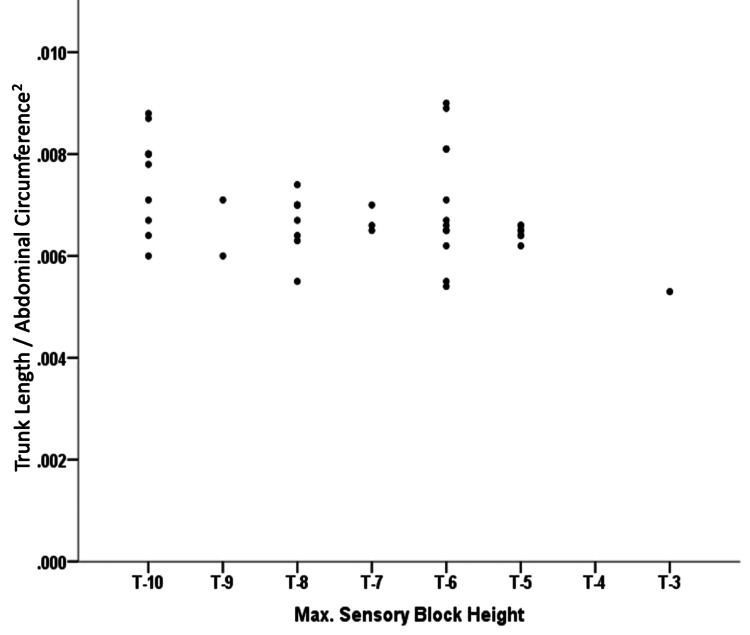
The co-morbidities of patients are shown in Figure 3. The mean TL of the patients was 63.02 +/- 5.71 (Mean +/- SD), and the TL/AC2 ranges from 0.005-0.009, as shown in Table 2. The lowest SABH observed was at the T-10 level, while the highest was at the T-3 level, which is evident from Figure 4.
Table 2. Measurements TL, AC and TL/(AC)2.
| Variables | Mean ± SD | 95% Confidence Interval for Mean | Min-Max | |
| LowerBound | UpperBound | |||
| Trunk length cm | 63.02±5.71 | 61.26 | 64.77 | 50-70 |
| Abdominal circumference cm | 95.29±8.68 | 92.62 | 97.96 | 77-112 |
| Trunk length (TL) / Abdominal circumference (AC)2 | 0.0067±0.00126 | 0.0063 | 0.0071 | 0.005-0.0092 |
Figure 3. Co-morbidities of Patients.
Figure 4. Relationship of Trunk Length/Abdominal Circumference2 (TL/AC2) to SABH.
The spearman rank correlation coefficient between maximal sensory block height and TL/AC2 was -0.284. Therefore, the ratio of trunk length and square of abdominal circumference TL/AC2 was significantly related to spinal anesthesia block height in geriatric patients undergoing TURP (p=0.015), as shown in Table 3.
Table 3. Spearman Rank Correlation Coefficient Between Trunk Length/Abdominal Circumference2 (TL/AC2) and SABH.
| Statistics | Trunk Length /Abdominal Circumference2 (TL/AC2) to SABH |
| n | 43 |
| Correlation Coefficient | -0.284 |
| P-Value | 0.015 |
Abdominal circumference was found to be significantly related to block height (p=0.036) (Table 4). BMI also showed a significant relationship with spinal anesthesia block height (p=0.02) (Table 5).
Table 4. Spearman Rank Correlation Coefficient Between Abdominal Circumference (AC) and SABH.
| Statistics | Abdominal Circumference and SABH |
| n | 43 |
| Correlation Coefficient | -0.321 |
| P-Value | 0.036 |
Table 5. Spearman Rank Correlation Coefficient Between BMI and SABH.
| Statistics | BMI and SABH |
| n | 43 |
| Correlation Coefficient | -0.346 |
| P-Value | 0.023 |
Discussion
The study was conducted to observe the relationship between the ratio of trunk length and square of the abdominal circumference with SABH in geriatric patients undergoing TURP. The results revealed a statistically significant relationship between the ratio TL/AC2 and SABH, i.e., r = -0.284 and p = 0.015 (r = Spearman's rank correlation coefficient). This means that geriatric patients with shorter trunk lengths and larger abdominal circumferences would tend to have higher SABH when performed with a standardized clinical technique and intrathecal local anesthetic solution.
Lee et al. conducted a similar study on term parturients undergoing lower-section cesarean section and found comparable results. They concluded that there is a significant relationship between TL/AC2 and spinal anesthesia block height; the spearman rank correlation coefficient (r) was -0.45 with p-value=0.02 [8]. Our study has revealed a comparable and statistically significant relationship with (r) = -0.284 and p-value= 0.015. Our sample size was 43, compared to 29 in the study by Lee et al. [8].
Multiple studies have been conducted to investigate the association between SABH and different patient characteristics [7,25,26]. Zhou et al. studied the relationship between vertebral column length and SABH in patients undergoing lower limb orthopedic surgery and found a strong link between the parameters (r = -0.243 and p = 0.009) [26]. In 2017, Chang et al. reported an even stronger correlation (r = -0.711, p < 0.0001) between TL and SABH in a study on the term parturient [27]. Hartwell et al. also studied this phenomenon in terms of parturient and found a positive relationship (r = 0.38 and p = 0.006) [18].
In this study, we did not find a statistically significant relationship between TL and SABH (r = -0.028). This lack of correlation can be explained by the geriatric nature of our study population. We included patients above the age of 60, while Zhou et al. excluded patients over the age of 55. This viewpoint was also highlighted by Pargger et al.; they found no correlation between trunk length and peak sensory level in elderly age group patients [28]. Therefore, age-related degenerative changes may have possibly played a role.
Zhou et al. [26] also studied the relationship between abdominal girth and SABH and found a strong relationship between both variables (r = 0.821 and p < 0.0001). Chang et al. studied this relationship in the term parturient and found a similar correlation (r = 0.372, p<0.0001) [27]. In our study, the relationship was statistically significant (r = 0.321 and p = 0.036) but with a weaker statistical difference compared to those found by Zhou et al. and Chang et al.
The mechanism by which abdominal circumference influences spinal anesthesia block height might be related to the changes in intra-abdominal pressure in sitting and supine positions. Intra-abdominal pressure rises as the patient lies down following the induction of spinal anesthesia [29]. This rise in intra-abdominal pressure will be proportional to the abdominal circumference and could result in the transfer of local anesthetics to the higher spinal levels [30]. Another possible mechanism could be the shifting of soft tissues to intervertebral foramina, causing a decrease in CSF volume [30,31]. Engorgement of the epidural veins, as seen in the parturient, can cause dura to encroach on the subarachnoid membrane, which could be another possible mechanism [32,33]. However, Seyhan et al. [34] studied the correlation of intra-abdominal pressure with SABH and concluded that there is no relationship between intra-abdominal pressure and block height.
As the results were conflicting when TL or AC was studied as an individual parameter, Lee and co-researchers [8] conceptualized the three-dimensional nature of the body and its influences on the spinal canal. They proposed that it is the three-dimensional aspect of the body that leads to discrepancies in correlations with SABH when studied using one dimension alone, i.e., long axis (TL) or short axis (AC).
Thus, Lee et al. [8] combined both the parameters, TL and AC, to discover a link between the ratio of both the parameters and spinal anesthesia block height. The premise was that by taking both characteristics into account, the correlation would improve.
This hypothesis can be rationalized by looking at the three-dimensional nature of the body. If we draw the transection area of the abdomen as an ellipse or circle, the diameter of this circle will have the same trend as the abdominal circumference (AC). On the other hand, AC2 will represent the maximal transection area of the abdomen. Therefore, TL/AC2 is the ratio between the long axis and transection area of the abdomen. When considered individually, TL and AC have the opposite effect on the SABH. Their ratio has the potential to improve the correlation with SABH.
Lee et al. [8] identified a positive relationship between TL/AC2 and sensory block height in the parturient, while our study identified a similar relationship in the geriatric population. In our study, all the parameters, including spinal level (L3-L4), drug dose (0.5% hyperbaric bupivacaine 10 mg), and technique, were standardized for all the patients.
Limitations
It should be noted that our study has some limitations. The study was conducted on a geriatric population aged between 60 and 80 undergoing TURP with 0.5% hyperbaric bupivacaine spinal anesthesia. Therefore, the results could not be generalized to patients of all ages undergoing various surgeries under spinal anesthesia. As the study population was undergoing TURP in a lithotomy position, it could have influenced the block height [35]. The spinal level was identified through the intercristal line (i.e., Tuffier’s line) using the palpatory method. This method is not 100% accurate, and discrepancies could occur, as reported by Christopher and colleagues [36]. Similarly, the C-7 spinous process can be identified correctly in only 77.1% of the population by the palpatory method [23]. Successful identification of sacral hiatus through the palpatory method is reported in up to 75% literature [37-39]. These two factors can influence trunk length measurement.
Conclusions
Adequate spinal anesthesia block height is necessary to avoid side effects or complications of spinal anesthesia and provide adequate surgical conditions. It is difficult to predict the spread of local anesthetics in subarachnoid space, and various methods are used to predict the block height. This observational study shows a significant correlation between spinal anesthesia block height and the ratio of trunk length and abdominal circumference, which coincides with the ratio of the long axis and transection area of the abdomen in geriatric patients. Therefore, a geriatric patient with a short trunk length and a large abdominal circumference might have a high spinal anesthesia sensory block height.
However, it would be unrealistic to consider a single factor as the sole determinant of spinal anesthesia block height, keeping in view the complexity of mechanisms of intrathecal drug spread. Clinicians should consider all the relevant factors while administering spinal anesthesia and not rely on a single factor.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Ethics Review Committee issued approval 4329-Ane-ERC-16. October 26. 2016 Dr. Aliya Ahmed Department of Anesthesiology The Aga Khan University Karachi Dear Dr. Aliya Ahmed, 4329-Ane-ERC-16. Resident - Dr Muhammad Yahya, Supervisor - Dr. Aliya Ahmed: Relationsnip or abdominal circumierence and trunk lengen with spinal anaesthesia level in geriatrics parents undergoing transurethral resection Thank you for your response to ERC recommendations received on October 25, 2016, regarding the above-mentioned study. Your response adequately answered the recommendations made by the committee. The study was given approval for a period of one year with effect from October 26, 2016. For further extension a request must be submitted along with the annual report. Any changes in the protocol or extension in the period of study should be notified to the committee lor prior approval. All informed consents should be retained for tuture reference. A progress report should be submitted to ERC office after six months. Thank you. Yours sincerely, Dr. Shaista Khan, FRCS (Edin.) Chairperson Ethics Review Committee Stadium Road. P. O. Box 3500. Karachi 74800. Pakistan
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Post-dural puncture headache. Ghaleb A, Khorasani A, Mangar D. Int J Gen Med. 2012;5:45–51. doi: 10.2147/IJGM.S17834. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 2.The incidence of transient neurologic symptoms (TNS) after spinal anaesthesia in patients undergoing surgery in the supine position. Hyperbaric lidocaine 5% versus hyperbaric bupivacaine 0.5% Keld DB, Hein L, Dalgaard M, Krogh L, Rodt SA. Acta Anaesthesiol Scand. 2000;44:285–290. doi: 10.1034/j.1399-6576.2000.440311.x. [DOI] [PubMed] [Google Scholar]
- 3.Epidural hematoma after neuraxial blockade: a retrospective report from China. Li SL, Wang DX, Ma D. Anesth Analg. 2010;111:1322–1324. doi: 10.1213/ANE.0b013e3181f1b9ea. [DOI] [PubMed] [Google Scholar]
- 4.Spinal anesthesia for intrapartum Cesarean delivery following epidural labor analgesia: a retrospective cohort study. Visser WA, Dijkstra A, Albayrak M, Gielen MJ, Boersma E, Vonsée HJ. Can J Anaesth. 2009;56:577–583. doi: 10.1007/s12630-009-9113-y. [DOI] [PubMed] [Google Scholar]
- 5.Incidence and risk factors for side effects of spinal anesthesia. Carpenter RL, Caplan RA, Brown DL, Stephenson C, Wu R. Anesthesiology. 1992;76:906–916. doi: 10.1097/00000542-199206000-00006. [DOI] [PubMed] [Google Scholar]
- 6.A prospective audit of regional anaesthesia failure in 5080 Caesarean sections. Kinsella SM. Anaesthesia. 2008;63:822–832. doi: 10.1111/j.1365-2044.2008.05499.x. [DOI] [PubMed] [Google Scholar]
- 7.Intrathecal drug spread. Hocking G, Wildsmith JA. Br J Anaesth. 2004;93:568–578. doi: 10.1093/bja/aeh204. [DOI] [PubMed] [Google Scholar]
- 8.Relationship of abdominal circumference and trunk length with spinal anesthesia level in the term parturient. Lee YH, Wang YC, Wang ML, Lin PL, Huang CH, Huang HH. J Anesth. 2014;28:202–205. doi: 10.1007/s00540-013-1715-4. [DOI] [PubMed] [Google Scholar]
- 9.Spinal analgesia using bupivacaine 0.5% plain. Variation in the extent of the block with patient age. Cameron AE, Arnold RW, Ghorisa MW, Jamieson V. Anaesthesia. 1981;36:318–322. doi: 10.1111/j.1365-2044.1981.tb10211.x. [DOI] [PubMed] [Google Scholar]
- 10.Influence of age on spinal anaesthesia with isobaric 0.5% bupivacaine. Pitkänen M, Haapaniemi L, Tuominen M, Rosenberg PH. Br J Anaesth. 1984;56:279–284. doi: 10.1093/bja/56.3.279. [DOI] [PubMed] [Google Scholar]
- 11.Spinal analgesia with hyperbaric bupivacaine: influence of age. Racle JP, Benkhadra A, Poy JY, Gleizal B. Br J Anaesth. 1988;60:508–514. doi: 10.1093/bja/60.5.508. [DOI] [PubMed] [Google Scholar]
- 12.Spinal anaesthesia with hyperbaric bupivacaine. Effects of age on neural blockade and pharmacokinetics. Veering BT, Burm AG, Spierdijk J. Br J Anaesth. 1988;60:187–194. doi: 10.1093/bja/60.2.187. [DOI] [PubMed] [Google Scholar]
- 13.Spinal anaesthesia withglucose-free bupivacaine: effects of age on neural blockade and pharmacokinetics. Veering BT, Burm AGL, van Kleef JW, Hennis PJ, Spierdijk J. https://journals.lww.com/anesthesia-analgesia/Abstract/1987/10000/Spinal_Anesthesia_with_Glucose_Free_Bupivacaine_.7.aspx. Anaesth Analg.1987. 66:965–970. [PubMed] [Google Scholar]
- 14.Does cough increase the spread of subarachnoid anaesthesia? Dubelman AM, Forbes AR. https://journals.lww.com/anesthesia-analgesia/Abstract/1979/07000/Does_Cough_Increase_the_Spread_of_Subarachnoid.9.aspx. Anaesth Analg. 1979;58:306–308. doi: 10.1213/00000539-197907000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Spread of spinal anaesthesia for caesarean section in singleton and twin pregnancies. Jawan B, Lee JH, Chong ZK, Chang CS. Br J Anaesth. 1993;70:639–641. doi: 10.1093/bja/70.6.639. [DOI] [PubMed] [Google Scholar]
- 16.The lumbar spine and subarachnoid block. Smith TC. Anesthesiology. 1968;29:60–64. doi: 10.1097/00000542-196801000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Trendelenburg position with hip flexion as a rescue strategy to increase spinal anaesthetic level after spinal block. Kim JT, Shim JK, Kim SH, Jung CW, Bahk JH. Br J Anaesth. 2007;98:396–400. doi: 10.1093/bja/ael370. [DOI] [PubMed] [Google Scholar]
- 18.Vertebral column length and spread of hyperbaric subarachnoid bupivacaine in the term parturient. Hartwell BL, Aglio LS, Hauch MA, Datta S. https://pubmed.ncbi.nlm.nih.gov/2007099/ Reg Anesth. 1991;16:17–19. [PubMed] [Google Scholar]
- 19.Cardiovascular effects of low-dose spinal anaesthesia as a function of age: An observational study using echocardiography. Lairez O, Ferré F, Portet N, et al. Anaesth Crit Care Pain Med. 2015;34:271–276. doi: 10.1016/j.accpm.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 20.Obesity is independently associated with spinal anesthesia outcomes: a prospective observational study. Kim HJ, Kim WH, Lim HW, et al. PLoS One. 2015;10:0. doi: 10.1371/journal.pone.0124264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Who EC. Lancet. 2004;363:157. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 22.Cachexia: A new definition. Evans WJ, Morley JE, Argilés J, et al. Clin Nutr. 2008;27:793–799. doi: 10.1016/j.clnu.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 23.Identification of the correct cervical level by palpation of spinous processes. Shin S, Yoon DM, Yoon KB. Anesth Analg. 2011;112:1232–1235. doi: 10.1213/ANE.0b013e3182110f9f. [DOI] [PubMed] [Google Scholar]
- 24.United Nations High Commissioner for Refugees: Emergency handbook, older persons. [ Dec; 2022 ]. 2022. https://emergency.unhcr.org/entry/43935/older-persons https://emergency.unhcr.org/entry/43935/older-persons
- 25.Distribution of local anaesthetic solutions within the subarachnoid space. Greene NM. https://journals.lww.com/anesthesia-analgesia/Citation/1985/07000/Distribution_of_Local_Anesthetic_Solutions_within.12.aspx. Analg. 1985;64:715–730. [PubMed] [Google Scholar]
- 26.Abdominal girth, vertebral column length, and spread of spinal anesthesia in 30 minutes after plain bupivacaine 5 mg/mL. Zhou QH, Xiao WP, Shen YY. Anesth Analg. 2014;119:203–206. doi: 10.1213/ANE.0000000000000199. [DOI] [PubMed] [Google Scholar]
- 27.Abdominal girth, vertebral column length and spread of intrathecal hyperbaric bupivacaine in the term parturient. Wei CN, Zhang YF, Xia F, Wang LZ, Zhou QH. Int J Obstet Anesth. 2017;31:63–67. doi: 10.1016/j.ijoa.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 28.Combined effect of patient variables on sensory level after spinal 0.5% plain bupivacaine. Pargger H, Hampl KF, Aeschbach A, Paganoni R, Schneider MC. Acta Anaesthesiol Scand. 1998;42:430–434. doi: 10.1111/j.1399-6576.1998.tb05137.x. [DOI] [PubMed] [Google Scholar]
- 29.Effect of posture on extradural pressure. Shah JL. Br J Anaesth. 1984;56:1373–1377. doi: 10.1093/bja/56.12.1373. [DOI] [PubMed] [Google Scholar]
- 30.Magnetic resonance imaging of cerebrospinal fluid volume and the influence of body habitus and abdominal pressure. Hogan QH, Prost R, Kulier A, Taylor ML, Liu S, Mark L. Anesthesiology. 1996;84:1341–1349. doi: 10.1097/00000542-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Influence of lumbosacral cerebrospinal fluid density, velocity, and volume on extent and duration of plain bupivacaine spinal anesthesia. Higuchi H, Hirata J, Adachi Y, Kazama T. Anesthesiology. 2004;100:106–114. doi: 10.1097/00000542-200401000-00019. [DOI] [PubMed] [Google Scholar]
- 32.The fiberscopic findings of the epidural space in pregnant women. Igarashi T, Hirabayashi Y, Shimizu R, Saitoh K, Fukuda H, Suzuki H. Anesthesiology. 2000;92:1631–1636. doi: 10.1097/00000542-200006000-00021. [DOI] [PubMed] [Google Scholar]
- 33.Effects of the pregnant uterus on the extradural venous plexus in the supine and lateral positions, as determined by magnetic resonance imaging. Hirabayashi Y, Shimizu R, Fukuda H, Saitoh K, Igarashi T. Br J Anaesth. 1997;78:317–319. doi: 10.1093/bja/78.3.317. [DOI] [PubMed] [Google Scholar]
- 34.The effect of intra-abdominal pressure on sensory block level of single-shot spinal anesthesia for cesarean section: an observational study. Ozkan Seyhan T, Orhan-Sungur M, Basaran B, Savran Karadeniz M, Demircan F, Xu Z, Sessler DI. Int J Obstet Anesth. 2015;24:35–40. doi: 10.1016/j.ijoa.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 35.The effect of patient positioning onthe spread of sensory blockade in hyperbaric and isobaric spinal anaesthesia usingbupivacaine. Tecklenburg-Weier E, Quest F, Nolte H, Meyer J. https://europepmc.org/article/med/2236713. Reg Anaesth. 1990;13:163–167. [PubMed] [Google Scholar]
- 36.Ultrasound assessment of the vertebral level of the palpated intercristal (Tuffier's) line. Pysyk CL, Persaud D, Bryson GL, Lui A. Can J Anaesth. 2010;57:46–49. doi: 10.1007/s12630-009-9208-5. [DOI] [PubMed] [Google Scholar]
- 37.Renfrew DL, Moore TE, Kathol MH, El-Khoury G, Lemke JH, Walker CW. http://www.ajnr.org/content/12/5/1003. Correct placement of epidural steroid injections: fluoroscopic guidance and contrastadministration. Am J Neuroradiol. 1991;12:1003–1007. [PMC free article] [PubMed] [Google Scholar]
- 38.Stitz MY, Sommer HM. https://journals.lww.com/spinejournal/Abstract/1999/07010/Accuracy_of_Blind_Versus_Fluoroscopically_Guided.16.aspx. Accuracy of blind versus fluoroscopically guided caudalepidural injection. Spine. 1999;24:1371. doi: 10.1097/00007632-199907010-00016. [DOI] [PubMed] [Google Scholar]
- 39.Caudal epidurals: the accuracy of blind needle placement and the value of a confirmatory epidurogram. Barham G, Hilton A. Eur Spine J. 2010;19:1479–1483. doi: 10.1007/s00586-010-1469-8. [DOI] [PMC free article] [PubMed] [Google Scholar]