Abstract
Background:
New-onset postpartum preeclampsia has a higher risk of maternal morbidity and mortality when compared to preeclampsia with antepartum onset, underscoring the need for earlier identification of elevated blood pressure among this population. Given the decrease in healthcare engagement that is typical of the postpartum period, new-onset postpartum hypertension often goes unrecognized. Currently, there are no recommendations for universal postpartum blood pressure surveillance in women without hypertensive disorders of pregnancy. With the shift to telemedicine related to the COVID 19 pandemic, our institution’s approach was to distribute blood pressure cuffs to women receiving any portion of their prenatal care virtually, thus also providing access to an opportunity for blood pressure measurement during the postpartum period for all women.
Objective:
To explore the feasibility of a patient-driven universal postpartum home blood pressure monitoring program in women without a diagnosis of a hypertensive disorder of pregnancy.
Study Design:
A prospective observational study of all postpartum women who were discharged from our institution from July 2020 through June 2021 not previously identified to have hypertension. A clinical algorithm was developed and followed. All women received discharge educational materials and were called at a 1-week interval by a nurse to review blood pressure and preeclampsia symptoms. Maternal demographics and delivery outcomes were recorded.
Results:
Of the 10,092 deliveries during the study period, 5,959 (59%) were successfully contacted. 352 were excluded as they did not deliver at the primary hospital, 1,052 (18%) had a prior hypertensive disorder of pregnancy diagnosis, 1,522 (26%) did not have a blood pressure cuff, and 1,841 (31%) planned to take their blood pressure at a later time. Precautions and blood pressure parameters were given to this last group. Of the remaining 1,192, 222 (19%) had an initial elevated blood pressure. Of these, 98 had a second elevated blood pressure on recheck, 17 were referred to the emergency room for evaluation with 8 being diagnosed with severe preeclampsia, and the remainder were recommended to follow with their obstetric provider and enrolled in our institution’s remote blood pressure management program. Of 1,192 women, 8.2% of women potentially had a new diagnosis of a hypertensive disorder of pregnancy with 0.7% having severe hypertension. Compared to women without elevated blood pressures, those with elevated blood pressures were more likely to be of non-Hispanic black race and were also more likely to have a higher early pregnancy body mass index.
Conclusions:
Our study indicates a patient-driven postpartum blood pressure monitoring program is feasible and may be incorporated using existing resources. Additionally, our findings suggest the incidence of new-onset postpartum hypertensive disorders of pregnancy may be higher than previously assessed in retrospective cohorts. Thus, there may be a role for closer surveillance of all women with patient-driven home blood pressure monitoring, particularly those with risk factors or in the setting of limited resources.
Keywords: Obstetrics, pregnancy, postpartum, hypertension, preeclampsia, blood pressure, quality improvement, remote care, telehealth, telemedicine
Introduction:
Hypertensive disorders of pregnancy, including preeclampsia, are a leading cause of maternal morbidity and mortality.[1] [2] Although hypertensive disorders of pregnancy are typically associated with the antenatal and intrapartum periods, there is an important population of women who develop de novo preeclampsia postpartum. [3] [4] [5] This is typically recognized as the new development of preeclampsia 48 hours to 6 weeks following delivery.[3] [4] [5] New-onset postpartum preeclampsia has a higher risk of maternal morbidity and mortality when compared to preeclampsia with antepartum onset and is associated with serious outcomes including seizure, stroke, and death[6] [7] [8] This underscores the need for earlier identification of elevated blood pressure (blood pressure) among this population. The incidence of de novo postpartum preeclampsia is not well defined and limited to small case series, however the best available estimates range from 0.3–27.5%.[9] Risk factors are similar to those for antenatal hypertensive disorders and include demographic factors such as obesity, increasing maternal age, gestational diabetes, non-Hispanic black race, and cesarean delivery.[6] [10] [11] [12] [13]
As awareness of hypertensive disorders of pregnancy has risen, there has been an increasing effort to monitor women with pre-pregnancy hypertension or antenatal hypertensive disorders of pregnancy after hospital discharge, including using telehealth platforms modeled on the success in non-obstetric populations. [14] [15] [16] [17] However, there remains a subset of women at risk for the development of de novo postpartum hypertension but do not receive the same degree of surveillance. Currently, there are no recommendations for postpartum blood pressure surveillance in women without hypertensive disorders of pregnancy. Women are instead often discharged to routine care and may then develop new onset postpartum preeclampsia that goes unrecognized until progressing to severe disease requiring Emergency Department evaluation and often readmission. [7] Postpartum day 7 is the median time of readmission at our institution for a new diagnosis of postpartum preeclampsia, as noted during a 52 month time period of 121 women. [11]
Our institution is a tertiary care center with greater than 10,000 deliveries annually. In light of the COVID-19 pandemic, a significant portion of prenatal care has shifted to telehealth. Women within our health system that receive any portion of their prenatal care virtually are provided with a blood pressure cuff, a resource they are given indefinitely. Women who received the entirety of their prenatal care in person were not provided with blood pressure cuffs. Given this unique development, we identified an opportunity to utilize these tools to target postpartum hypertension. Benefits may include early identification of women with de novo postpartum preeclampsia to allow for intervention as an outpatient prior to progression to severe disease. However, if women are identified that do require Emergency Department evaluation it is possible that identification at an earlier stage may allow for timely intervention and truncation of progression to severe disease that necessitates hospital readmission or aversion of severe maternal morbidity. The objective of this study is to explore the feasibility and outcomes of a patient-driven universal postpartum home blood pressure monitoring program in women without a diagnosis of pre-pregnancy hypertension or a hypertensive disorder of pregnancy.
Materials and Methods:
This is a prospective observational study that is part of an ongoing quality improvement initiative of all postpartum discharges from July 2020 through June 2021 at our institution. All women received postpartum discharge instructions by a clinical nurse that included written material pertaining to postpartum preeclampsia. A nurse or patient educator then called all patients in the first week postpartum for a wellness check following a script reviewing several relevant postpartum issues, such as mood and lactation. This includes an algorithm to triage blood pressures and symptoms that may be related to preeclampsia. These symptoms include headaches, shortness of breath, chest pain, difficulty breathing while laying flat, vision changes, worsening extremity swelling, or right upper quadrant or epigastric pain. Diagnoses of hypertensive disorders were made by the clinical care team using the American College of Obstetricians and Gynecologists’ criteria. [1] Maternal demographics and delivery characteristics were recorded from the medical record (Table 1).
Table 1:
Maternal Demographics and Outcomes
| Normotensive N (%) 1,043 (87.5%) |
New elevated blood pressure* N (%) 149 (12.5%) |
p-value | |
|---|---|---|---|
| Maternal Age (years) | 30.8 (7.4) | 30.4 (5.4) | 0.60 |
| Race | 0.004 | ||
| Non-Hispanic White | 741 (71.0%) | 100 (67.1%) | |
| Non-Hispanic Black | 144 (13.8%) | 36 (24.2%) | |
| Asian or Pacific Islander | 94 (9.0%) | 8 (5.4%) | |
| Other | 64 (6.1%) | 5 (3.4%) | |
| Early pregnancy BMI (kg/m2) median (interquartile range) | 25.2 (22.4–30.1) | 29.2 (25.0–34.5) | <0.001 |
| BMI Category (kg/m2) | <0.001 | ||
| Normal and Underweight (<25.0) | 432 (48.4%) | 30 (24.8%) | |
| Overweight (25.0–29.9) | 231 (25.9%) | 36 (29.8%) | |
| Obese (≥30.0) | 229 (25.7%) | 55 (45.5%) | |
| Nulliparous | 594 (57.0%) | 81 (54.4%) | 0.55 |
| Gestational diabetes | 85 (8.1%) | 10 (6.7%) | 0.54 |
| Gestational age at delivery (week), mean (SD) | 39.0 (3.0) | 39.1 (1.8) | 0.85 |
| Birth weight (g), mean (SD) | 3276.1 (546.7) | 3342.6 (559.8) | 0.17 |
| Cesarean delivery | 289 (28.8%) | 41 (27.5%) | 0.75 |
| Multiple gestation | 17 (1.7%) | 1 (0.7%) | 0.35 |
2 elevated values, or provided 1 elevated value and second value not obtained
Women were asked if they had access to a blood pressure cuff, and if so were asked to record a value. Women were excluded if they did not have a cuff or if they had a pre-pregnancy diagnosis of hypertension or a hypertensive disorder of pregnancy, as those women were previously enrolled in our institution’s electronic remote monitoring blood pressure program. This program involves daily submission of blood pressures electronically via text message to a clinical provider for monitoring and management of hypertension postpartum.[16]
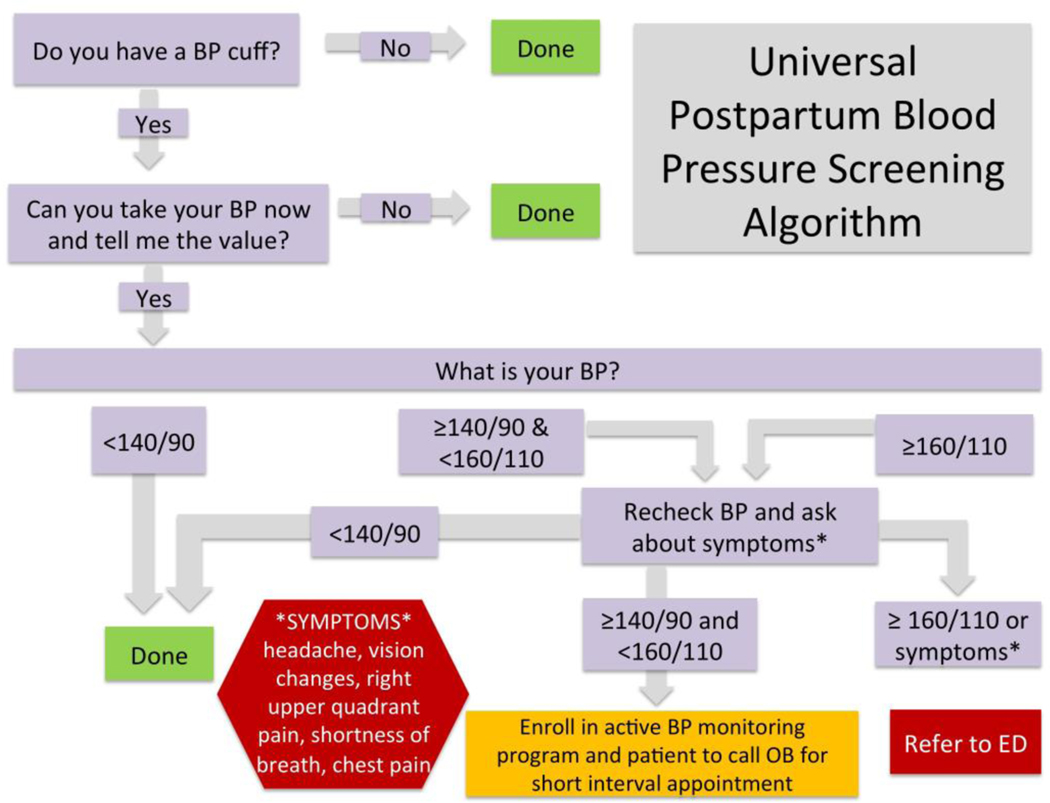
If the woman was normotensive, the blood pressure was recorded and no further action was taken. If the woman had an elevated blood pressure, an algorithm was followed (Figure 1). If the initial blood pressure was greater than or equal to 140/90 mmHg, they were asked to recheck their blood pressure at a 15-minute interval. If the repeat blood pressure was greater than or equal to 140/90 mmHg and less than 160/110 mmHg and the patient was asymptomatic, she was instructed to call her primary obstetrician to schedule a short interval visit and enrolled into our remote monitoring blood pressure program. If symptoms were present or repeat blood pressure was greater than or equal to 160/110 mmHg, the patient was instructed to present to the Emergency Department. If the repeat blood pressure was less than 140/90 mmHg the patient was instructed regarding symptom monitoring and rechecking her blood pressure with parameters to call if her blood pressure was 140/90 mmHg or higher.
Figure 1:
Universal Postpartum blood pressure Screening Algorithm
We sought to assess feasibility of such a program, which we quantified by the proportion of women for whom blood pressure was ascertained, resource utilization, and identification and triage to appropriate follow up. Additional outcomes of interest included the incidence of new-onset postpartum preeclampsia, postpartum systolic and diastolic blood pressure values, enrollment into our remote monitoring blood pressure program, and Emergency Department evaluation and hospital readmission for postpartum hypertension. Finally, we evaluated the presence of risk factors for new-onset postpartum hypertension (maternal age ≥ 35, pre-pregnancy BMI ≥ 30 kg/m2, gestational diabetes, non-Hispanic black race, and cesarean delivery).[6] [10] [11][12] [13] This study received exemption approval from the Institutional Review Board.
Statistical analyses were performed using Stata IC 16 software (College Station, TX, StataCorp LLC). Maternal characteristics and delivery outcomes were compared between women with a normal blood pressure and women with newly elevated blood pressure postpartum (defined as greater than or equal to 140/90 mmHg). Continuous variables were compared using Student’s t -tests and Wilcoxon-Mann-Whitney tests and categorical variables were analyzed using chi-square or Fisher exact.
Results:
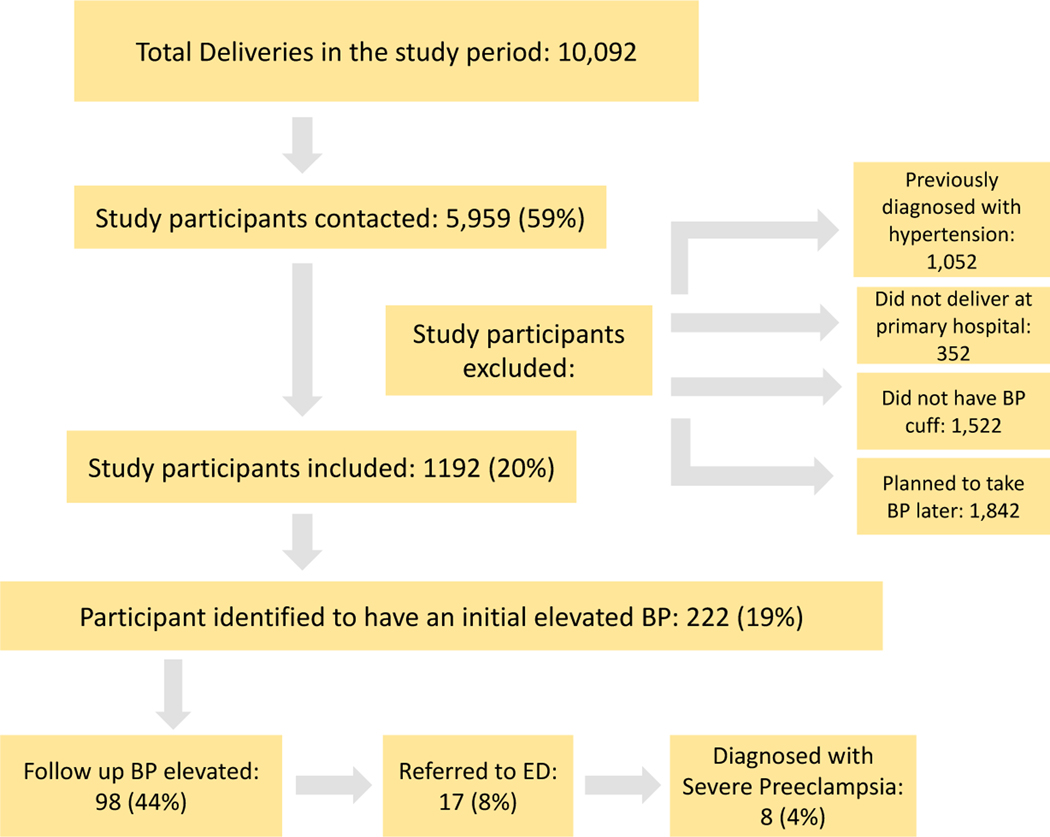
Of the 10,092 deliveries during the study period, 5,959 (59%) were successfully contacted (Figure 2). 1,052 (18%) were excluded as they had a diagnosis of pre-pregnancy hypertension or a hypertensive disorder of pregnancy. 352 (6%) were excluded as they did not deliver at our institution and 1,522 (26%) were excluded as they did not have a blood pressure cuff. 1842 (31%) planned to take their blood pressure at a later time citing either they were occupied or were not in proximity to or had a dysfunctional blood pressure cuff. Precautions and blood pressure parameters were given to this group.
Figure 2: Flow Chart of Study Participant Screening.
Of the remaining 1,192 women, 222 (19%) had an initial elevated blood pressure with 98 having an elevated blood pressure on recheck. 51 women did not provide a follow up blood pressure. 17 women were referred to the Emergency Department for evaluation in the setting of a persistently severe range blood pressure or because of mild blood pressure elevations and the presence of symptoms. 8 (0.7%) of these women were diagnosed with severe preeclampsia all requiring hospital readmission. The remaining women were referred for short interval follow up with their obstetric provider and enrolled in our institution’s remote monitoring blood pressure program. Overall, of 510 women, 98 (8.2%) had a new diagnosis of a postpartum hypertensive disorder, though this number may be potentially higher (149) if the 51 women who did not provide a repeat blood pressure were found to be persistently hypertensive.
Participation with answering the screening phone call varied, ranging from 49% (September) to 64% (July). Additionally, the proportion of women with access to a blood pressure cuff increased each month. For example, in the first 6 months of the study, 60% of women contacted that were eligible for inclusion had a cuff with this proportion increasing in the second 6 months to 73%.
For women who provided their blood pressure, the median length of phone call was 14 minutes (interquartile range 10–18) compared to 8 minutes (interquartile range 6–12) for women that did not provide a blood pressure. The mean systolic blood pressure for women with normotensive values was 121 mmHg (SD 11.1) and diastolic was 78 mmHg (SD 8.4). For those with elevated values, the mean systolic blood pressure was 141 mmHg (SD 13.4) and diastolic was 93 mmHg (SD 7.7).
To identify risk factors for new-onset blood pressure elevations postpartum, we compared demographic and delivery characteristics between groups. Compared with normotensive patients, those with newly elevated blood pressure were more likely to be of non-Hispanic Black race and more likely to have a higher early pregnancy BMI (Table 1). Increasing BMI category was associated with a statistically significant increasing risk of elevated blood pressure. There was no difference between groups in terms of maternal age, gestational age at delivery, mode of delivery, parity, gestational diabetes, and multiple gestations. In total, 109 (73.2%) of women with newly elevated blood pressure had at least one risk factor for postpartum preeclampsia, compared to 624 (59.8%) of women who were normotensive (p=0.002). Of note, 40 (27%) women with newly elevated blood pressure had no risk factors for postpartum preeclampsia.
Additionally, we sought to explore whether differences existed between those that participated in the program and provided their blood pressure at the time of the call compared to those who did not as they either did not participate in the phone call, did not have a blood pressure cuff, or declined to provide their blood pressure at the time of the phone call (Table 2). Compared with those patients who provided their blood pressure, those who did not were more likely to have differences in race category (p=0.004), being more likely to be of Non-Hispanic White or Non-Hispanic Black race and less likely to be of Asian or Pacific Islander, or other race category. Additionally, those who did not participate in the phone call were more likely to deliver at a slightly earlier gestational age (38.9 vs 39.1, p=0.004). The remaining maternal characteristics and delivery outcomes were similar between groups.
Table 2.
Maternal Demographics and Outcomes by Program Participation.
| Blood pressure obtained (n=1,192) |
Eligible but did not participate (n= 7,618) |
p-value | |
|---|---|---|---|
| Maternal Age (years) | 31.1 (8.7) | 30.6 (10.7) | 0.19 |
| Race | 0.004 | ||
| Non-Hispanic White | 841 (70.6%) | 5577 (73.5%) | |
| Non-Hispanic Black | 180 (15.1%) | 1337 (17.6%) | |
| Asian or Pacific Islander | 102 (8.6%) | 468 (6.2%) | |
| Other | 71 (6.0%) | 210 (2.8%) | |
| Early pregnancy BMI (kg/m2) median (interquartile range) | 25.4 [22.5–30.3] | 25.9 [22.7–30.9] | 0.13 |
| BMI Category (kg/m2) | 0.10 | ||
| Normal and Underweight (<25.0) | 462 (45.6%) | 2406 (43.2%) | |
| Overweight (25.0–29.9) | 267 (26.4%) | 1596 (28.7%) | |
| Obese (≥30.0) | 284 (28.0%) | 1563 (28.1%) | |
| Gestational diabetes | 95 (8.0%) | 587 (7.7%) | 0.71 |
| Gestational age at delivery (week), mean (SD) | 39.1 (2.6) | 38.9 (2.4) | 0.004 |
| Birth weight (g), mean (SD) | 3285 (550) | 3252 (599) | 0.09 |
| Cesarean delivery | 330 (27.7%) | 2336 (30.7%) | 0.49 |
| Multiple gestation | 18 (1.5%) | 142 (1.9%) | 0.45 |
Discussion/Comment:
Principal Findings
This ongoing study details the implementation and outcomes of a universal patient-driven postpartum blood pressure monitoring program and endeavors to demonstrate feasibility. We contacted nearly 6000 women and diagnosed and provided care to an important and greater than expected proportion with new-onset postpartum hypertension as well as identified risk factors for its development. This highlights the potential role for universal surveillance of all women with patient-driven home blood pressure monitoring, particularly those with risk factors. An unanticipated finding was the challenge in engaging women during the fourth trimester of pregnancy, this emphasizes the vulnerability of this time and need to optimize postpartum care.
Results
Our findings suggest the incidence of new-onset postpartum hypertensive disorder of pregnancy may be higher than previously assessed in retrospective cohorts, which primarily report incidence based on the number of women readmitted with likely the most severe forms of postpartum preeclampsia.[5] [18] In our study, 8.2% of women had persistently elevated blood pressures and 0.7% met criteria for postpartum preeclampsia with severe features. In regards to maternal characteristics and outcomes, we saw similar risk factors for the development of de novo postpartum hypertension consistent with prior studies, although those again largely have been focused on hospital readmission. A study by Redman et al demonstrated maternal age of 35 years or older, pre-pregnancy BMI of 30 kg/m2 or greater, cesarean delivery, and non-Hispanic black race to be associated with new-onset postpartum preeclampsia requiring readmission.[11] A separate study found maternal age of ≥40 years, antenatal prescription of low-dose aspirin, non-Hispanic black race and BMI of ≥30 kg/m2.[19] Given the increasing evidence regarding risk factors for de novo postpartum hypertension, it may be reasonable to monitor women with these risk factors more closely postpartum. This may be particularly important if resources are limited and universal postpartum blood pressure monitoring is not feasible. However, it should be noted that in populations with similar demographics, a risk-based screening model would miss 27% of women with new-onset postpartum hypertension.
Clinical Implications
Given the greater than expected incidence of de novo postpartum hypertension, there may be a role for closer surveillance of all women, not just those with a prior diagnosis of pre-pregnancy hypertension or a hypertensive disorder of pregnancy. Although 8 out of the 17 women who presented for urgent Emergency Department evaluation ultimately were admitted for inpatient management, it is plausible that these women were identified earlier in the disease process as they had not recognized their need for medical attention. This very likely is applicable to the women who were identified to have persistently elevated blood pressure but were determined to not require Emergency Department evaluation and were enrolled in our remote monitoring blood pressure program and referred for short interval follow up with their primary obstetric provider. Potentially, a subset of these women would have required Emergency Department evaluation should their disease had progressed and would not otherwise have been able to be managed as an outpatient. These results suggest that universal monitoring may identify and prevent significant maternal morbidity. An additional potential long-term benefit of the program may include increasing women’s awareness of cardiovascular disease and becoming champions of their own health through the familiarization of taking their own blood pressure and self-monitoring for signs and symptoms of high blood pressure.
A component of the initiative’s success likely relates to utilization of preexisting medical equipment and the increasing familiarity and accessibility of a virtual health platform. As telehealth is increasingly utilized this leads to growing acceptability of this method of healthcare delivery as a component of pregnancy care. A study of our institution’s remote postpartum blood pressure monitoring program using a text message based platform demonstrated promising results regarding engagement, feasibility, and patient satisfaction.[16] Given the use of preexisting resources in the form of blood pressure cuffs and familiar technological platforms, a remote postpartum blood pressure program in normotensive women may be an implementable, innovative, and feasible intervention.
Research Implications
An unforeseen challenge in our project was the number of women eligible to participate in the study who declined to provide a blood pressure. Future considerations to overcome this barrier may include expanding patient education to achieve buy in from patients. Considerations may also be made in lieu of a phone call, alternative ways of engaging women. This may include strategies such as measuring blood pressure in the pediatrician’s office or a text based program. Our institution has previously demonstrated success in our remote monitoring blood pressure text based program for women with hypertension.[16] We had assumed a phone-based system would have analogous success, however our findings demonstrated this to not be true. Potential reasons include the modality of communication. We found that women who did not participate were overall fairly similar demographically to those that did participate, however further investigation into any common characteristics of those who declined participation may shed future light on how to best engage this population.
Strengths/Limitations
This project had several strengths, including capturing a large cohort with a significant incidence of postpartum hypertensive disorders while further describing the frequency of the disorder. This allows for the description of both the spectrum of hypertensive disorders of pregnancy as well as risk factors.
This study was not without limitations. These included that all patients were treated at a single tertiary-care hospital and therefore our methods and results may not be readily generalizable to other populations. For example, all clinical settings may not have the resources to provide blood pressure cuffs to their patients or provide follow up calls in the postpartum period. Data was collected from women at one data point and therefore there may be subsets of patients that developed preeclampsia prior to or after this that were omitted. Furthermore, we were not powered to identify women with transient or mild hypertension that were not detected at the time of the phone call. Given the small sample size of the hypertensive group, there is an increased risk for error when comparing demographic and outcomes between groups. Additionally, it is difficult to quantify resource utilization and needs for such a program given this was an adjunct to an existing program, including costs and time associated with blood pressure collection and required follow up and care coordination. Thus, further study is needed to explore the feasibility of a standalone program. The program did not delineate whether women had access to a blood pressure cuff as part of their telemedicine prenatal care or for an alternative reason. Although, the program is described as patient-driven, given that the patient’s provided and recorded their own blood pressures, it did require the resources of a phone call to gather this information and provide instructions regarding management. Finally, our institution may be unique in the available resources dedicated to this issue and thus our program may not be generalizable to all health care settings.
Conclusions:
Delayed-onset postpartum preeclampsia is associated with significant morbidity and current healthcare models demonstrate opportunities for improvement. There is increasing awareness regarding the importance of the fourth trimester of pregnancy and a solution may be emerging in leveraging telehealth and patient driven monitoring to address this healthcare challenge. Our study indicates a patient-driven postpartum blood pressure monitoring program is feasible and may be incorporated using existing resources allowing for the earlier recognition and treatment of postpartum preeclampsia. An unanticipated finding was the challenge in engaging patients during this time period, highlighting the vulnerability of this period. We additionally found that specific risk factors were associated with elevated blood pressure, thus targeted monitoring may be an alternative to universal blood pressure monitoring if resources are limited.
AJOG at a Glance.
A. New onset postpartum preeclampsia is an important contributor to maternal morbidity and mortality. Given the decrease in health care engagement typical of the postpartum period, new onset postpartum hypertension often goes unrecognized. The objective of this study is to explore the feasibility and outcomes of a patient-driven universal postpartum home blood pressure monitoring program.
B. Our study indicates universal patient-driven postpartum blood pressure monitoring is feasible with new onset postpartum hypertension affecting a significant proportion of women. Risk factors for postpartum elevated blood pressure include non-Hispanic black race and higher BMI.
C. A universal patient-driven postpartum blood pressure monitoring program can be incorporated using existing resources and allow for the recognition and treatment of postpartum hypertension. Additionally, identification of risk factors for postpartum hypertension may be of value when allocating resources.
Condensation:
A universal patient-driven postpartum blood pressure monitoring program is feasible and may be incorporated using existing resources allowing for recognition and treatment of postpartum hypertension.
Financial Support:
The project described was supported by the Magee-Womens Hospital Medical Staff through Grant Award FY2021 and by the National Institute of Health through Grant Number UL1 TR001857 to Dr. Hacker This work was additionally supported by NIH/ORWH Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) NIH K12HD043441 scholar funds to Dr. Hauspurg. The funding sources had no role in study design, collection, analysis and interpretation of data, writing of the report, or decision to submit the article for publication.
Presented as a poster (#563) at the 41st Annual Meeting of the Society for Maternal-Fetal, virtual meeting, Jan 25th- 30th, 2021.
Footnotes
Disclosures: The authors report no conflict of interest
References:
- 1.Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. American College of Obstetricians and Gynecologists," Obstet Gynecol, vol. 133, pp. e1–25, 2019 [Google Scholar]
- 2.Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010. Aug 21;376(9741):631–44. doi: 10.1016/S0140-6736(10)60279–6. [DOI] [PubMed] [Google Scholar]
- 3.Filetti LC, Imudia AN, Al-Safi Z, Hobson DT, Awonuga AO, Bahado-Singh RO. New onset delayed postpartum preeclampsia: different disorders? J Matern Fetal Neonatal Med. 2012. Jul;25(7):957–60. doi: 10.3109/14767058.2011.601365. [DOI] [PubMed] [Google Scholar]
- 4.Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011. Nov;118(5):1102–1107. doi: 10.1097/AOG.0b013e318231934c. [DOI] [PubMed] [Google Scholar]
- 5.Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004. May;190(5):1464–6. doi: 10.1016/j.ajog.2004.02.037. [DOI] [PubMed] [Google Scholar]
- 6.Wen T, Wright JD, Goffman D, et al. Hypertensive Postpartum Admissions Among Women Without a History of Hypertension or Preeclampsia. Obstet Gynecol. 2019. Apr;133(4):712–719. doi: 10.1097/AOG.0000000000003099. [DOI] [PubMed] [Google Scholar]
- 7.Too G, Wen T, Boehme AK, et al. Timing and Risk Factors of Postpartum Stroke. Obstet Gynecol. 2018. Jan;131(1):70–78. doi: 10.1097/AOG.0000000000002372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yancey LM, Withers E, Bakes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011 Apr;40(4):380–4. doi: 10.1016/j.jemermed.2008.02.056. [DOI] [PubMed] [Google Scholar]
- 9.Sibai BM. Etiology and management of postpartum hypertension-preeclampsia. Am J Obstet Gynecol. 2012. Jun;206(6):470–5. doi: 10.1016/j.ajog.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Larsen WI, Strong JE, Farley JH. Risk factors for late postpartum preeclampsia. J Reprod Med. 2012. Jan-Feb;57(1–2):35–8. [PubMed] [Google Scholar]
- 11.Redman EK, Hauspurg A, Hubel CA, Roberts JM, Jeyabalan A. Clinical Course, Associated Factors, and Blood Pressure Profile of Delayed-Onset Postpartum Preeclampsia. Obstet Gynecol. 2019. Nov;134(5):995–1001. doi: 10.1097/AOG.0000000000003508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bigelow CA, Pereira GA, Warmsley A, et al. Risk factors for new-onset late postpartum preeclampsia in women without a history of preeclampsia. Am J Obstet Gynecol. 2014. Apr;210(4):338.e1–338.e8. doi: 10.1016/j.ajog.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Takaoka S, Ishii K, Taguchi T, et al. Clinical features and antenatal risk factors for postpartum-onset hypertensive disorders. Hypertens Pregnancy. 2016;35(1):22–31. doi: 10.3109/10641955.2015.1100308. [DOI] [PubMed] [Google Scholar]
- 14.Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens. 2012. Mar;30(3):449–56. doi: 10.1097/HJH.0b013e32834e4aed. [DOI] [PubMed] [Google Scholar]
- 15.Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D; American Heart Association; American Society of Hypertension; Preventive Cardiovascular Nurses Association. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008 Jul;52(1):1–9. doi: 10.1161/HYPERTENSIONAHA.107.189011. [DOI] [PubMed] [Google Scholar]
- 16.Hoppe KK, Williams M, Thomas N, et al. Telehealth with remote blood pressure monitoring for postpartum hypertension: A prospective single-cohort feasibility study. Pregnancy Hypertens. 2019. Jan;15:171–176. doi: 10.1016/j.preghy.2018.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hauspurg A, Lemon LS, Quinn BA, et al. A Postpartum Remote Hypertension Monitoring Protocol Implemented at the Hospital Level. Obstet Gynecol. 2019. Oct;134(4):685–691. doi: 10.1097/AOG.0000000000003479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atterbury JL, Groome LJ, Hoff C. Blood pressure changes in normotensive women readmitted in the postpartum period with severe preeclampsia/eclampsia. J Matern Fetal Med. 1996. Jul-Aug;5(4):201–5. doi: . [DOI] [PubMed] [Google Scholar]
- 19.Smithson SD, Greene NH, Esakoff TF. Risk factors for re-presentation for postpartum hypertension in patients without a history of hypertension or preeclampsia. Am J Obstet Gynecol MFM. 2021. Mar;3(2):100297. doi: 10.1016/j.ajogmf.2020.100297. [DOI] [PubMed] [Google Scholar]
- 20.Podymow T, August P. Postpartum course of gestational hypertension and preeclampsia. Hypertens Pregnancy. 2010;29(3):294–300. doi: 10.3109/10641950902777747. [DOI] [PubMed] [Google Scholar]