Abstract
Heart failure (HF) with depression is a common comorbidity associated with worse clinical status and quality of life. Although there have been numerous high-quality studies and relevant reviews on HF comorbid with depression, few bibliometric analyses of this field have been reported. In order to understand the development process, research hotspots and future directions, this review analyzes the papers on HF comorbid with depression from January 2002 to December 2021 through CiteSpace and VOSviewer. Visual cooperative networks between countries, authors and institutions were conducted to understand the basic development status of HF comorbid with depression. Furthermore, we performed co-occurrence analysis, burst detection, and timeline analysis for keywords to understand this field's research directions and hotspots. Finally, a detailed review and analysis of the classical literature in this field were conducted based on co-citation analysis. This bibliometric analysis provides an overview of studies on HF comorbid with depression and emphasizes the research on comorbidity mechanisms and more effective interventions as a priority for future research.
Keywords: Heart failure, Depression, Bibliometric analysis, Research trends
Abbreviations: HF, heart failure; AHF, acute heart failure; CHF, chronic heart failure; CVDs, cardiovascular diseases; MDD, major depression disorder; BDI, beck depression inventory; PHQ-9, patient health questionnaire-9; SSRIs, selective serotonin reuptake inhibitors; CBT, cognitive-behavioral therapy; WoSCC, web of science core collection; US, United States; CAD, coronary artery disease; SCAD, stable coronary artery disease
Highlights
-
•
There were few high-quality bibliometric analyses on heart failure comorbid with depression.
-
•
Through CiteSpace and VOSviewer, basic development status is analyzed to guide future studies in the field.
-
•
Based on the results of the bibliometric analysis, we discuss the current challenges and future directions in this field.
1. Introduction
Heart failure (HF) is the terminal stage of all cardiovascular diseases (CVDs), which has become an increasingly urgent public health problem worldwide due to its high morbidity and poor prognosis. A study showed that mortality and readmission rates were respectively 17.4% and 43.9% for patients with acute heart failure (AHF) and 7.2% and 31.9% for patients with chronic heart failure (CHF) [1]. Comorbidities of HF are common and associated with worse cardiac function and prognosis [2]. Depression is a chronic mood disorder characterized by anhedonia and aversion to activity. Recent studies showed that 41.9% of HF patients suffered from depression [3], and the estimated prevalence of depression will increase dramatically in the future [4]. Moreover, the comorbidity of HF with depression can contribute to reduced treatment adherence, increased hospitalization and mortality [5,6]. For example, multiple meta-analyses suggested that the risk of mortality was 57% higher for HF patients comorbid with depression (HR 1.57, 95% CI 1.30–1.89, P < 0.001) [5]. Furthermore, depression seems to increase the risk of HF in patients without CVDs. The Nord-Trøndelag Health Study found that the severity of depression symptoms was significantly associated with the prevalence of HF in a population of 62 567 healthy subjects [7].
Since the Hippocratic period, the association between emotions and cardiac has begun to attract attention [8]. In 1998, Koenig [9] first reported that patients with CHF are significantly more likely to suffer from major depression disorder (MDD) than patients without CHF. Currently, depression has been confirmed as an independent predictor of all-cause mortality in HF patients [10,11]. Although the physiopathology of depression in HF is not fully clear, there are some common mechanisms and risk factors, such as inflammation, neuroendocrine function, insulin resistance, gut dysbiosis, and social factors. Considering the high prevalence and poor prognosis of depression in HF patients, the European Society of Cardiology (ESC) and the American College of Cardiology/American Heart Association (ACC/AHA) heart failure guidelines recommended timely detection and treatment for depression in HF patients [2,12]. Currently, the diagnosis of depression in HF patients is mainly based on traditional depression scales, including the Beck Depression Inventory (BDI), the Cardiac Depression Scale, Hamilton Depression Scale, and Patient Health Questionnaire-9 (PHQ-9) [2,[13], [14], [15]]. The treatments for depression in HF patients mainly consist of pharmacological and non-pharmacological treatments. In terms of pharmacological treatment, selective serotonin reuptake inhibitors (SSRIs) are the main drugs used to improve depression symptoms with a more favourable safety profile [16]. Tricyclic antidepressants should be avoided in the treatment due to the adverse effects, including hypotension, worsening HF and arrhythmias [2]. Notably, studies showed that drugs for HF (such as Sacubitril-Valsartan) were associated with a reduction in depression symptoms after improvement in cardiovascular status, suggesting that treatment for HF is fundamental to HF patients comorbid with depression [17,18]. The main non-pharmacological treatments for depression in HF patients are cognitive-behavioral therapy (CBT) and exercise therapy. CBT is a composite psychological strategy that aims to modify the patient's negative cognitive and behavioral processes. The NCIE guidelines recommend CBT for depression patients as a treatment option [19]. After 6 months of CBT, HF patients had a lower depression score on BDI compared to usual care (12.8 [10.6] vs 17.3 [10.7]; P = 0.008) [20]. Exercise therapy effectively improves depressive symptoms [21], but it is questionable whether the exercise can be maintained over time in HF patients. Only a few studies showed improvements in exercise capacity and quality of life [22], despite these treatments have shown beneficial effects in reducing depression symptoms. Therefore, more effective treatments are needed to improve exercise capacity and quality of life, and further reduce hospitalization and mortality rates in HF patients comorbid with depression.
Bibliometrics is an interdisciplinary that utilizes mathematical and statistical methods to quantitatively analyze papers. The evolution and trends of a field can be obtained through bibliometric analysis. Bibliometric is an objective and reasonable tool to analyze the influence and value of research achievements. Visualization software not only uses data mining techniques to extract valuable information, but also displays the obtained information in different dimensions. Based on the obtained data, the Knowledge-Map can be constructed to further evaluate academic productivity, summarize academic hotspots, and predict the trends. Over the past 20 years, a large number of papers have been published in the field of HF comorbid with depression, making it difficult to extract their information manually. Therefore, bibliometric software is necessary to summarize research outcomes in the field systematically. CiteSpace and VOSviewer are the most commonly used bibliometric tools among various software [[23], [24], [25]]. Using VOSviewer, the visual cooperative graphs between the various elements based on elements such as countries, institutions, and authors can be displayed in three dimensions (including Network Visualization, Overlay Visualization and Density Visualization). The above features of VOSviewer match our requirements for building cooperative networks. CiteSpace is a software based on set theory for data analysis and visualization, with a special focus on the time dimension. CiteSpace analyzes time slices through timeline analysis to further explore the development trend in the field. Furthermore, burst keywords and classical literature can be identified through burst detection and co-citation analysis, which further provides a comprehensive analysis of the development of the field.
Although there are bibliometric analyses on depression [26,27], few bibliometric studies have been reported in the field of HF comorbid with depression. In addition, this study provided a review of the classical literature to understand the development and challenges of the field, which is different from other bibliometric analyses. This review collected a total of 4846 papers on HF comorbid with depression from January 2002 to December 2021 for bibliometric analysis. The remainder of this review will be organized as follows: in the second section, we will introduce the material sources and analysis methods; in the third section, we will show detailed information, including annual publications, countries, authors, institutions and keywords; in the fourth section, we summarize results of this paper and discuss the development status and trends of the field.
2. Material sources and analysis methods
2.1. Data retrieval and collection
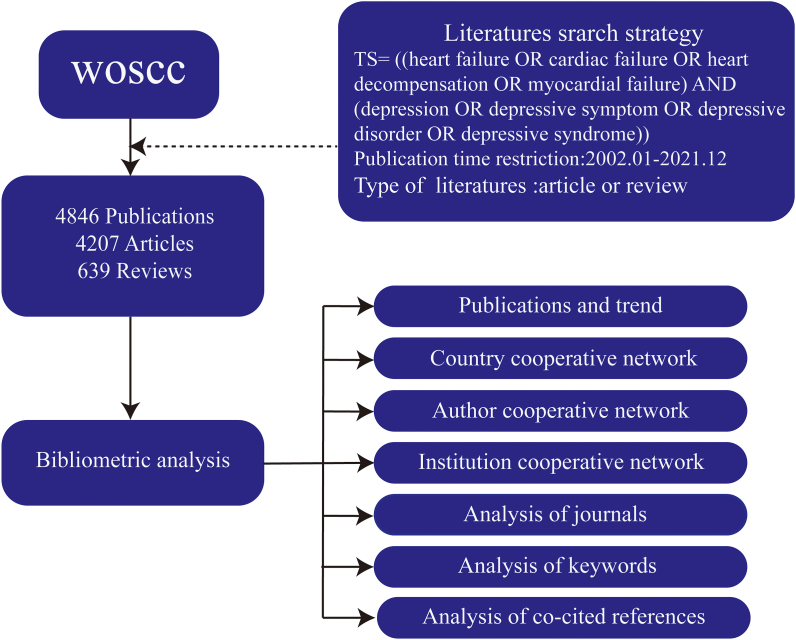
The Web of Science Core Collection (WoSCC) was selected as the data source in this study. WoSCC, as the largest comprehensive academic resource database, contains the most influential core academic journals in various fields including biomedicine, natural science and engineering technology. Valuable scientific information and a comprehensive understanding of this field can be acquired conveniently using the powerful search function of WoSCC. The search strategy for this study was “TS= ((heart failure OR cardiac failure OR heart decompensation OR myocardial failure) AND (depression OR depressive symptom OR depressive disorder OR depressive syndrome))”, and the "citation index" was set as SCI-EXPANDED and SSCI. The publication time ranges from January 2002 to December 2021, and the type of papers is constrained to “article OR review” without language restrictions. A total of 4846 papers were collected, and the records were exported in “plain text” and “tab delimited file” format (Fig. 1). The papers were exported within 1 day (2022.12.30) to avoid data bias.
Fig. 1.
Flow diagram of literature identification.
2.2. Data analysis and visualization methods
CiteSpace 6.1. R2 and VOSviewer 1.6.17 were selected as the main bibliometric analysis tools to comprehensively analyze and summarize papers on HF comorbid with depression over the past 20 years. Based on the contributions of countries, authors, and institutions, the cooperative co-occurrence graphs were drawn to analyze the connections between the elements. To understand the evolution of hotspots and predict the trends, we conducted a cluster analysis and burst detection of keywords. Finally, we identified the classical literature in the field through the co-citation analysis of literature. In addition, the WoSCC and Microsoft Excel 365 (Microsoft Corporation, Redmond, WA, USA) were used for data processing. Journal Impact Factor was searched from Journal Citation Reports of 2021.
3. Results
3.1. Analysis of publications and trends
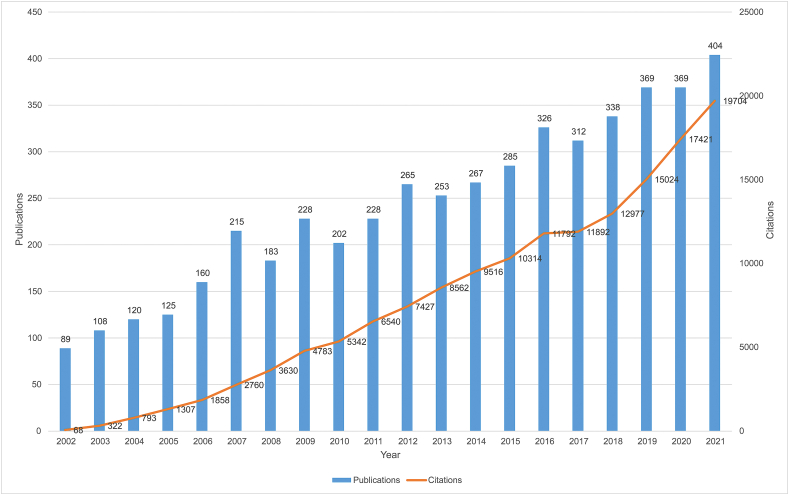
The trends and speed of the field can be determined based on the number of publications and citations per year. From January 2002 to December 2021, WoSCC collected 4846 papers on HF comorbid with depression, with 170 173 citations, an average of 35.12 citations per article, and an H-index of 163. Among the 4846 papers, 4207 articles, 639 reviews, and 32 highly cited papers were included. In terms of paper languages, English was the most frequently used language, accounting for 96.8% (4692/4846). As shown in Fig. 2, the number of publications and citations has been increased rapidly in the last 20 years. Starting in 2009, the annual publications have consistently reached more than 200 for 13 years, up to 404 papers in 2021, indicating that this field has become more popular and attracted increasing attention.
Fig. 2.
Trends in the growth of publications and the number of cited articles worldwide from 2002 to 2021.
3.2. Cooperative network
3.2.1. Country cooperative network
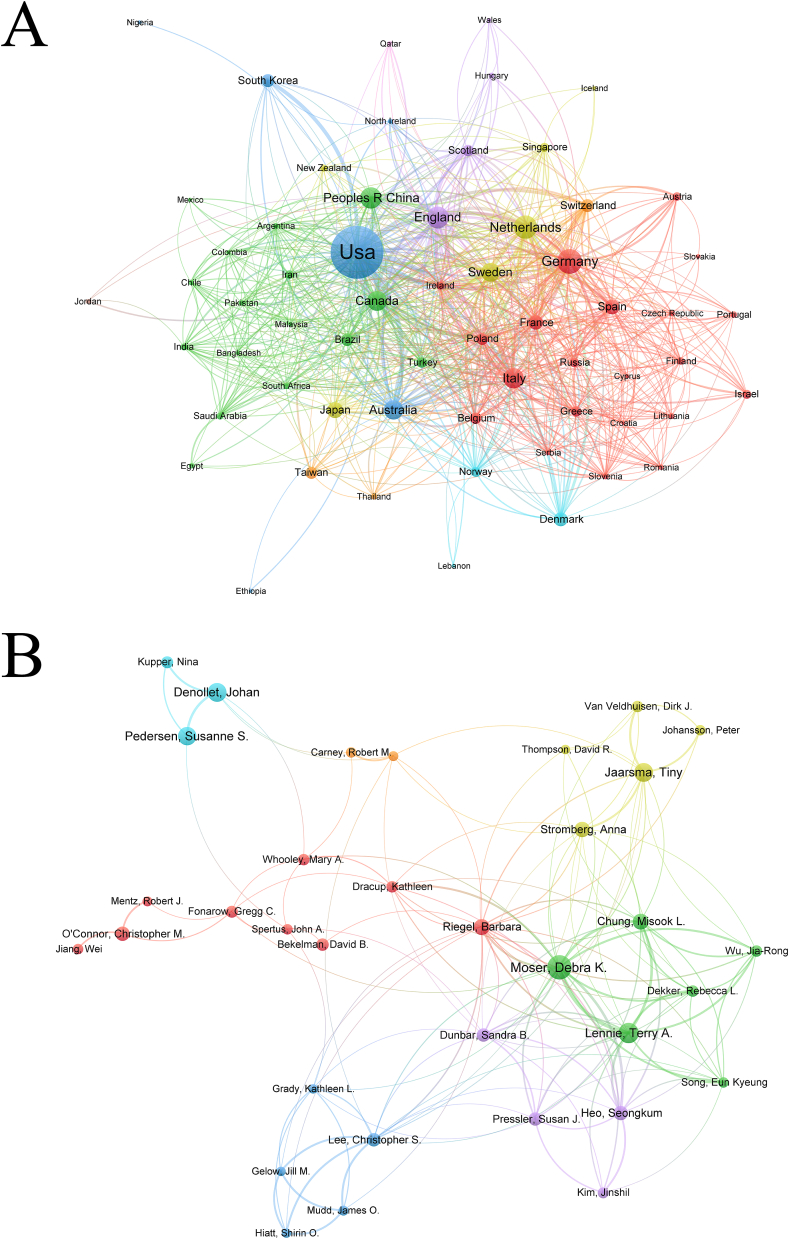
We can identify the influential countries in the field and draw a country cooperative network by analyzing the number of publications per country. A total of 100 countries/regions were involved in HF comorbid with depression from January 2002 to December 2021. The United States (US) was the most productive and influential country which contributed 2191 relevant papers (45.2%), with 43.08 citations per article, and an H-index of 140. There was a wide gap between the US and other countries in terms of publications and the top effect was significant. The top 10 countries in terms of publications contributed the majority of papers (4706/4846) (Table S1). It is noteworthy that the Netherlands contributed 354 papers, mainly attributed to three professors, Denollet Johan, Jaarsma Tiny, and Pedersen Susanne.
Cooperation between countries is vital for the development of this field. The country cooperative co-occurrence diagram, according to VOSviewer, showed that the US, England, Netherlands, Germany, and Sweden made significant contributions to this field (Fig. 3A). The size of the nodes represents the number of publications; the connecting lines between the nodes indicate cooperation between countries; the number and thickness of the connecting lines represent the closeness of the cooperation between countries. The US had a total link strength of 953 with other countries, which indicated that the US was at the center of the field and had a strong influence on the relationship in the network. The countries with the strongest links to the US are Canada and Australia.
Fig. 3.
Cooperative networks of cooperative relationship in HF with depression according to VOSviewer. (A) Cooperative network of countries with more than 4 publications (B) Co-occurrence diagram of authors with more than 14 publications.
3.2.2. Author cooperative network
A total of 23 061 authors published papers on HF comorbid with depression from January 2002 to December 2021. According to the Price Law, the criteria for core authors can be expressed by this formula: , where is the number of papers published by the most productive author and is the minimum number of papers among core authors. Authors who published more than 7 papers in this field are core authors. There were 200 authors who met this criterion, accounting for 0.86% of the total (200/23 061). These core authors published 1221 papers, accounting for 25.2% of the total publications (1221/4846) with 39.74 citations per article.
By analyzing the top 10 productive authors (Table S2), we found that 6 are American scholars, which further emphasized the significant contribution of American scholars to the field. Professor Moser Debra from the University of Kentucky, who published 103 papers, was the most influential author with a citation frequency of 38.13 and an H-index of 34. Main research of Moser Debra focused on self-care and improving the quality of life of HF patients comorbid with depression. Fig. 3B showed the cooperative co-occurrence diagram for authors with more than 14 publications (without unconnected authors), and the network was centered on Professor Moser Debra. Lennie Terry and Chung Misook were the most closely associated authors with Professor Moser Debra. Additionally, Professors Denollet Johan, O'Connor Christopher, and Riegel Barbara had high H-index and average frequency of citations, indicating that they are also leaders in this field.
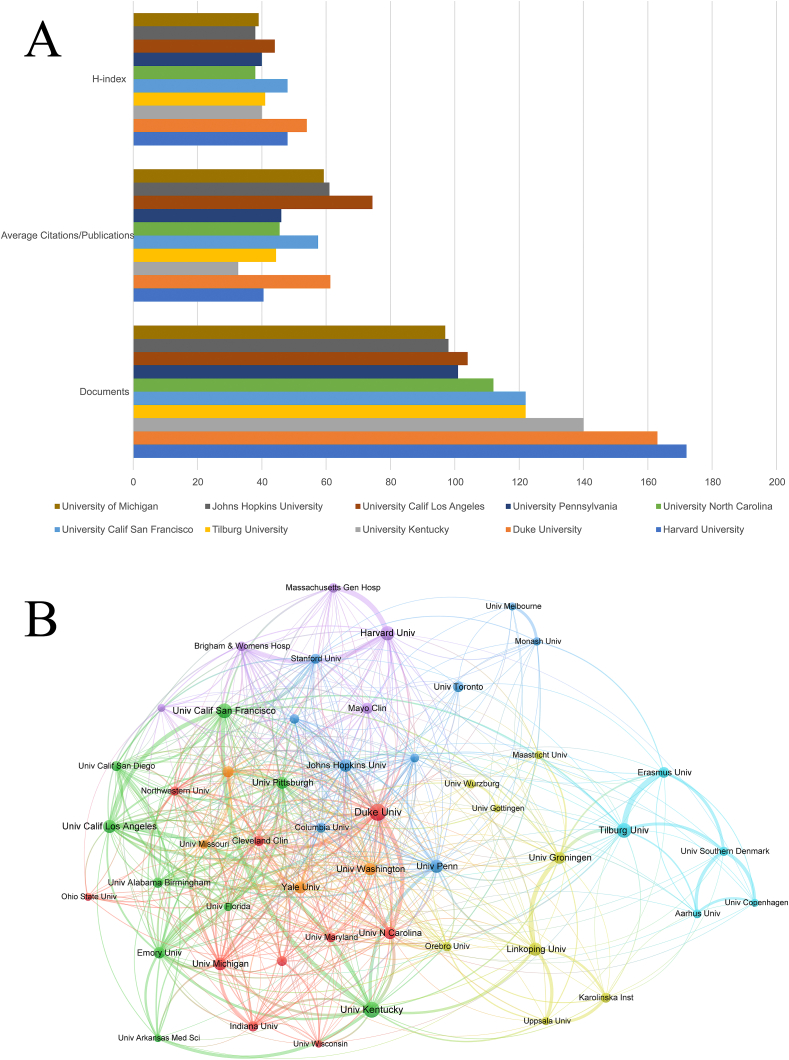
3.2.3. Institution cooperative network
From January 2002 to December 2021, a total of 5264 institutions contributed to papers on HF comorbid with depression. Duke University contributed to 163 papers and had the highest H-index of 54, fully demonstrating that it was the most influential institution in the field. The top 10 contributors were listed in Fig. 4A, with 9 institutions from US and 1 from the Netherlands. In medicine, the US has long been recognized as a leader. Moreover, it is noteworthy that Linköping University made a significant contribution to Sweden with 96 articles, representing 42.1% of the total publications in Sweden. The cooperative relationship between the top 50 productive institutions was shown in Fig. 4B. The institution most closely linked to Duke University is the University of Southern California. And both Duke University and University of Southern California published high-quality articles, suggesting that collaboration between institutions is helpful in significantly advancing the field. Additionally, most fund institutions of articles focused on the national level, which showed that the field has attracted significant attention.
Fig. 4.
(A) The total number of publications, average citation per item, and H index of the top 10 institutions. (B) Cooperative network of top 50 institutions according to VOSviewer.
3.3. Analysis of journals
The top 10 journals in terms of publications are listed in Table S3. Among these, Journal of Cardiovascular Nursing (IF = 2.468, Q3) was the most published journal in this field, with 124 articles and 22.65 citations per article. European Journal of Heart Failure (IF = 17.349, Q1) was the most frequently cited journal, with 64.41 citations per article and the highest impact factor. European Journal of Heart Failure is dedicated to spreading knowledge in the field of HF and is one of the most influential journals in the field. Journal of Cardiac Failure (IF = 6.592, Q2) and America Heart Journal (IF = 5.099, Q2) had a relatively high impact factor and average frequency of citations compared to other journals. These journals not only had high impact factors, but also published numerous articles on HF with depression, making them attractive for researchers in this field.
3.4. Analysis of keywords
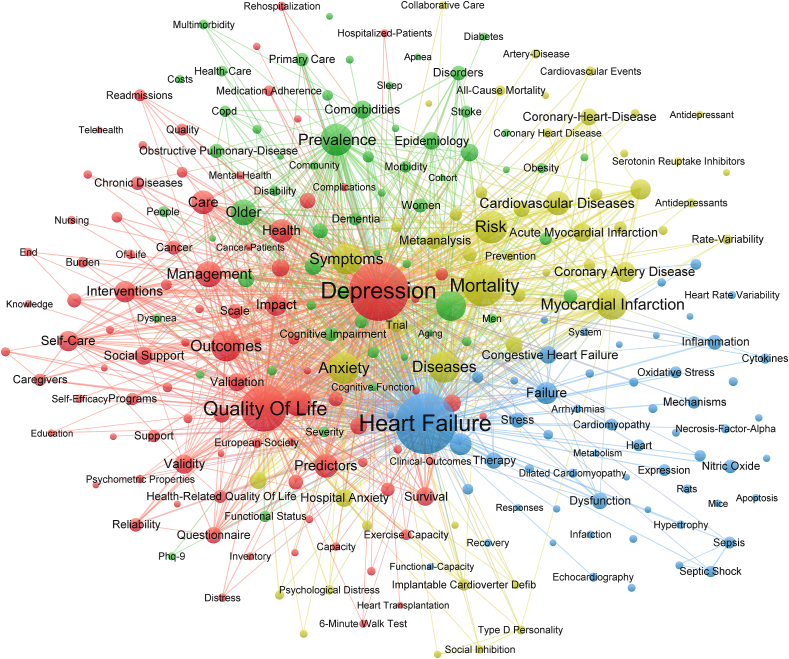
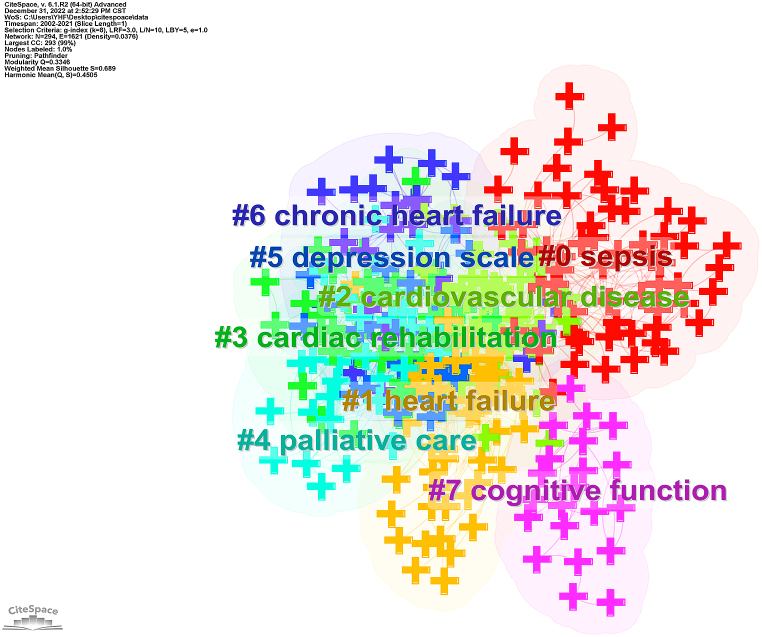
Since the keywords condense the essence of an article, we can capture the main directions and hotspots in the field of HF comorbid with depression based on keyword co-occurrence analysis. There are 13 574 keywords in 4846 articles on HF comorbid with depression. VOSviewer was used to draw a keywords co-occurrence diagram in this field, and the keywords with a frequency of more than 27 were selected for visualization (Fig. 5). The top 5 keywords include depression, heart failure, quality of life, mortality and risk. In order to identify further research themes in the field over the past 20 years, we performed a cluster analysis of keywords. Keywords were divided into 8 clusters (Fig. 6), mainly including sepsis, heart failure, cardiovascular disease, cardiac rehabilitation, palliative care. Burst keywords are those keywords that frequently emerge in a short period. As shown in Table S4, burst keywords in this field prior to 2016 focused on specific diseases, such as congestive heart failure, acute myocardial infarction, and dilated cardiomyopathy. Whereas the burst keywords after 2017 focused on screening and treatments, such as self care, systematic review and PHQ-9. The timeline diagram provided by CiteSpace is presented to understand the development progress of HF comorbid with depression research in the time dimension. As shown in Figure S1, most of the important keywords, such as quality of life and prevalence, focused on the period before 2010. In comparison, there were no important keywords in recent years, which was contrary to the increasing number of publications and citations in this field.
Fig. 5.
Diagram of the co-occurrence analysis among the keywords which occurred at least 27 times according to VOSviewer.
Fig. 6.
Cluster diagram of keywords according to CiteSpace.
3.5. Analysis of co-cited references
The co-citation refers to 2 or more articles cited by 1 or more articles simultaneously. As the co-citation relationships of literature change over time, the development and evolution dynamics in this field can be explored by analyzing co-cited literature. Through co-citation analysis and burst detection, the classical literature in this field can be identified. After reading its content, this classical literature can be divided into 2 main groups.
3.5.1. Association between HF and depression
There is a close association between HF and depression in terms of risk factors, epidemiology, clinical outcome. In 2004, Gottlieb et al. [28] published an article in the Journal of the American College of Cardiology entitled “The influence of age, gender, and race on the prevalence of depression in heart failure patients”. This study found that HF patients comorbid with depression were younger than those without depression, and women (64%) seemed to have a higher risk of depression than men (44%). Regarding race, white male patients (54%) were more likely to be depressed than black male patients (34%). In 2006, Rutledge et al. [29] published the first meta-analysis in the field of HF patients comorbid with depression. This paper systematically illustrated three issues: Firstly, the prevalence of significant depression was 21.5% in HF patients and varied by the use of questionnaires (33.6%) versus diagnostic interviews (19.3); Secondly, HF patients comorbid with depression were associated with higher rates of mortality and secondary events (HR 2.1, 95% CI 1.7–2.6), as well as higher rates of hospitalization and emergency room visits; Thirdly, the results of interventions for depression in HF patients are promising, but more studies with larger sample sizes, and replicable interventions are needed. Jiang and Rumsfeld et al. [30,31] found that HF patients comorbid with depression experienced worse health status both in the short and long term, and depression symptoms could be a predictor of poor prognosis in HF patients. Unfortunately, most studies in this field focused on the epidemiology and poor prognosis of HF patients comorbid with depression, and the mechanisms between HF and depression are not fully unclear. In summary, depression is a common comorbidity of HF and is associated with worse clinical status and prognosis, and more studies on the mechanisms are needed in future.
3.5.2. Intervention of HF comorbid with depression
Considering the high morbidity and mortality of HF comorbid with depression, it is necessary to provide timely and effective intervention for patients. In 2010, O'Connor et al. [16] published the results of the SADHART-CHF trial in the Journal of The American College of Cardiology. The SADHART-CHF trial was a 12-week randomized, placebo-controlled trial of sertraline in HF patients comorbid with depression. Unfortunately, although sertraline is safe in HF patients, sertraline treatment did not significantly improve patients' depression symptoms or cardiovascular function compared with placebo. Angermann's team [31] found that escitalopram treatment neither significantly reduced all-cause mortality and hospitalization nor significantly improved depression symptoms compared with placebo. In 2015, Freedland et al. [20] valuated the treatment effects of CBT for depression in HF patients. CBT was effective in improving patients' depression symptoms, which is effective in reducing anxiety and fatigue and improving social function. However, there were no significant differences between CBT and usual care on the Self-Care Maintenance or Confidence subscale scores or on physical functioning measures. The ESC and AHA have provided numerous guidelines for the treatment of HF patients comorbid with depression. The “2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure” was the most influential [2], with a total of 187 co-citations and a burst intensity of 74.50. The guidelines mentioned that routine screening with validated questionnaires is necessary. Besides, cognitive behavioral therapy and structured educational programs beyond the standard of care for patients can reduce depression severity, anxiety and fatigue symptoms, and improve social functioning and quality of life related to depression and HF. In conclusion, there was no effective intervention for depression in HF patients, and further research is urgently needed to develop effective treatments.
4. Discussion
This study conducted a bibliometric analysis in the field of HF comorbid with depression from 2002 to 2021 and visualized the results through CiteSpcae and VOSviewer to demonstrate the evolution and hotspots of the field quantitatively and intuitively. Specifically, the number of publications has been increased rapidly and this field has improved significantly over the past 20 years. A quantitative analysis of detailed information, including countries, authors, and institutions, was performed. Professor Moser Debra from the US is the most influential author in the field, with the most publications and the highest H-index. In terms of institutions, those from the US came out in front in both the number and quality of papers. Therefore, the US had an important position in this field. Based on the cluster analysis and burst detection of keywords, this paper predicts that future research hotspots in this field may focus on screening and treatment of depression in HF patients. Finally, the classical literature in the field was identified by co-citation analysis and burst detection. Prior to 2010, studies in this field mainly focused on the association between HF and depression. However, studies in this field mainly focused on interventions for depression after 2010. Currently, there is a comprehensive understanding of influence factors, epidemiology, and adverse clinical outcomes of HF comorbid with depression.
Although this field has achieved significant development in the past 20 years, there are some challenges in future development process. Firstly, there are few breakthrough studies on the mechanisms between HF and depression. Inflammatory dysregulation, such as interferon-γ, tumor necrosis factor-α, interleukin-6, perforin, and granzyme B, may be potential mechanisms between HF and depression [32]. A study showed that inflammatory markers are associated with all-cause mortality in HF patients [33]. However, the credibility of these studies is controversial due to small sample sizes and more clinical studies are required to confirm this evidence. Gut dysbiosis is also a possible shared mechanism between depression and HF. Dysbiosis of gut microflora and its metabolites occurs in both HF and depression patients. Similarly, gut dysbiosis contributes to inflammation and immune response through intestinal barrier damage and bacterial translocation, which further aggravates HF and depression [[34], [35], [36]]. But the specific mechanism of gut dysbiosis involved in HF comorbid with depression is not well understood. Secondly, screening for depression in HF with traditional questionnaires is complex and challenging due to the overlap of HF symptoms and risk factors for depression, so the objective indicators for assessing depressive symptoms in hospitalized patients with HF are necessary. A study showed that the risk of depression in hospitalized HF patients can be identified by a predictive model consisting of six predictor variables, including history of CVD hospitalization, obesity, renal insufficiency, NT-proBNP (lnNT-proBNP), N (%), and RDW [37]. Thirdly, the current treatment of depression in HF patients is not fully effective. Interestingly, N-methyl-d-aspartate receptor (NMDAR) antagonists and Omega-3 polyunsaturated fatty acids (PUFAs) gradually showed antidepressant effects in HF patients. NMDAR are glutamatergic, ligand-gated, ion channel receptors, and NMDAR antagonists improve depression symptoms by reducing glutamatergic hyperactivity, increasing neurotrophic factor, and modulating synaptic plasticity [38]. The US Food and Drug Administration has approved S-enantiomer of ketamine, a safe and fast-acting NMDAR antagonists, for patients with treatment-resistant depression [39]. However, its safety and efficacy in HF patients require further evaluation. Lack of omega-3 PUFAs is associated with mood disorders and poor survival in HF patients comorbid with depression [40]. The Omega-3 Supplementation for Co-Morbid Depression and Heart Failure Treatment trial, which included 108 CHF patients comorbid with MDD, showed that supplementation with omega-3 fatty acids significantly improved cognitive depression symptoms and social function. Finally, most studies focus on the treatment of depression, while relatively few studies are concerned with preventing new-onset depression. In a meta-analysis of 19 studies, prevention interventions (such as CBT and interpersonal psychotherapy) of depression reduced the incidence of depression by 22% compared to control groups [41]. Preventive interventions in stepped care for high-risk groups of depression may be expected [42]. However, there seem to be few studies on the effects of preventive strategies for depression symptoms in HF patients.
It is also notable that other CVDs, such as coronary artery disease (CAD), are closely associated with depression. In a cross-sectional study including 144 patients with stable coronary artery disease (SCAD), the prevalence of moderate/severe depression symptoms in patients with SCAD was 18.8% [43]. And low-density lipoprotein, high-density lipoprotein, and creatinine levels are risk factors for depression symptoms. Besides, Wu et al., 2019 [44] found CAD patients comorbid with depression have a higher readmission rate, frequency of chest pain, and risk of major cardiovascular events. These results emphasize the necessity of screening for depression symptoms in CAD patients. If available in the future, we will also perform a bibliometric analysis of coronary heart disease comorbid with depression.
5. Limitation
The limitations of this study are as follows: firstly, although WoSCC is the most widely used search database, it is inevitable to omit some articles; secondly, since the database is constantly updated, there is a certain lag in the data obtained, such as the number of articles, citations and H-index; thirdly, the quality of the articles collected in this study is uneven, which may also affect the reliability of this study.
6. Conclusion
In this study, 4846 papers published from January 2002 to December 2021 were collected to illustrate the research progress, hotspots and trends in the field of HF comorbid with depression. This field has gained significant development in the last 20 years and there is a comprehensive understanding of the influence factors, epidemiology, and adverse clinical outcomes. In addition, more research is required on comorbidity mechanisms and effective interventions.
Author contributions
Drs Hengfeng Ying, Ling Yang designed the study. Dr. Hengfeng Ying wrote the manuscript. Drs Hengfeng Ying and Xinying Zhang performed the data analysis. All the authors critically revised the manuscript and approved the submission.
Declaration of competing interest
No conflicts of interest to declare.
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (to L.Y., 82070405).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.heliyon.2023.e13054.
Contributor Information
Ling Yang, Email: linda_yl@sina.com.
Jiahao Duan, Email: djh120575@sina.com.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Maggioni A.P., et al. EURObservational research programme: regional differences and 1-year follow-up results of the heart failure pilot survey (ESC-HF pilot) Eur. J. Heart Fail. 2013;15(7):808–817. doi: 10.1093/eurjhf/hft050. [DOI] [PubMed] [Google Scholar]
- 2.McDonagh T.A., et al. Corrigendum to: 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2021;42(48):4901. doi: 10.1093/eurheartj/ehab670. [DOI] [PubMed] [Google Scholar]
- 3.Moradi M., et al. Global prevalence of depression among heart failure patients: a systematic review and meta-analysis. Curr. Probl. Cardiol. 2022;47(6) doi: 10.1016/j.cpcardiol.2021.100848. [DOI] [PubMed] [Google Scholar]
- 4.Trautmann S., Rehm J., Wittchen H.U. The economic costs of mental disorders: do our societies react appropriately to the burden of mental disorders? EMBO Rep. 2016;17(9):1245–1249. doi: 10.15252/embr.201642951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Celano C.M., et al. Depression and anxiety in heart failure: a review. Harv. Rev. Psychiatr. 2018;26(4):175–184. doi: 10.1097/HRP.0000000000000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vongmany J., et al. Anxiety in chronic heart failure and the risk of increased hospitalisations and mortality: a systematic review. Eur. J. Cardiovasc. Nurs. 2016;15(7):478–485. doi: 10.1177/1474515116635923. [DOI] [PubMed] [Google Scholar]
- 7.Gustad L.T., et al. Symptoms of anxiety and depression and risk of heart failure: the HUNT Study. Eur. J. Heart Fail. 2014;16(8):861–870. doi: 10.1002/ejhf.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alberti F.B. Heartfelt emotions. Lancet. 2009;374(9689):519–520. doi: 10.1016/s0140-6736(09)61476-8. [DOI] [PubMed] [Google Scholar]
- 9.Koenig H.G. Depression in hospitalized older patients with congestive heart failure. Gen. Hosp. Psychiatr. 1998;20(1):29–43. doi: 10.1016/s0163-8343(98)80001-7. [DOI] [PubMed] [Google Scholar]
- 10.Sokoreli I., et al. Depression and anxiety as predictors of mortality among heart failure patients: systematic review and meta-analysis. Heart Fail. Rev. 2016;21(1):49–63. doi: 10.1007/s10741-015-9517-4. [DOI] [PubMed] [Google Scholar]
- 11.Carney R.M., Freedland K.E. Depression and coronary heart disease. Nat. Rev. Cardiol. 2017;14(3):145–155. doi: 10.1038/nrcardio.2016.181. [DOI] [PubMed] [Google Scholar]
- 12.Heidenreich P.A., et al. AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American heart association joint committee on clinical practice guidelines. Circulation. 2022;145(18):e895–e1032. doi: 10.1161/CIR.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 13.Lahlou-Laforet K., et al. Validity of Beck Depression Inventory for the assessment of depressive mood in chronic heart failure patients. J. Affect. Disord. 2015;184:256–260. doi: 10.1016/j.jad.2015.05.056. [DOI] [PubMed] [Google Scholar]
- 14.Lee E.J., Hall L.A., Moser D.K. Psychometric properties of the patient health questionnaire-9 in patients with heart failure and gastrointestinal symptoms. J. Nurs. Meas. 2014;22(2):E29–E40. doi: 10.1891/1061-3749.22.2.E29. [DOI] [PubMed] [Google Scholar]
- 15.Ski C.F., et al. Cardiac Depression Scale: mokken scaling in heart failure patients. Health Qual. Life Outcome. 2012;10:141. doi: 10.1186/1477-7525-10-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Connor C.M., et al. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline against Depression and Heart Disease in Chronic Heart Failure) trial. J. Am. Coll. Cardiol. 2010;56(9):692–699. doi: 10.1016/j.jacc.2010.03.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cacciatore F., et al. Effect of Sacubitril-Valsartan in reducing depression in patients with advanced heart failure. J. Affect. Disord. 2020;272:132–137. doi: 10.1016/j.jad.2020.03.158. [DOI] [PubMed] [Google Scholar]
- 18.Dereli S., et al. Impact of sacubitril/valsartan treatment on depression and anxiety in heart failure with reduced ejection fraction. Acta Cardiol. 2020;75(8):774–782. doi: 10.1080/00015385.2020.1730577. [DOI] [PubMed] [Google Scholar]
- 19.Depression in Adults: Recognition and Management. 2018. (London) [PubMed] [Google Scholar]
- 20.Freedland K.E., et al. Cognitive behavior therapy for depression and self-care in heart failure patients: a randomized clinical trial. JAMA Intern. Med. 2015;175(11):1773–1782. doi: 10.1001/jamainternmed.2015.5220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blumenthal J.A., et al. Effects of exercise training on depressive symptoms in patients with chronic heart failure: the HF-ACTION randomized trial. JAMA. 2012;308(5):465–474. doi: 10.1001/jama.2012.8720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.von Haehling S., et al. Improving exercise capacity and quality of life using non-invasive heart failure treatments: evidence from clinical trials. Eur. J. Heart Fail. 2021;23(1):92–113. doi: 10.1002/ejhf.1838. [DOI] [PubMed] [Google Scholar]
- 23.van Eck N.J., Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–538. doi: 10.1007/s11192-009-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen C.M. CiteSpace II: detecting and visualizing emerging trends and transient patterns in scientific literature. J. Am. Soc. Inf. Sci. Technol. 2006;57(3):359–377. [Google Scholar]
- 25.Pan X.L., et al. Examining the usage, citation, and diffusion patterns of bibliometric mapping software: a comparative study of three tools. J. Informet. 2018;12(2):481–493. [Google Scholar]
- 26.He T., et al. A bibliometric analysis of research on (R)-ketamine from 2002 to 2021. Neuropharmacology. 2022;218 doi: 10.1016/j.neuropharm.2022.109207. [DOI] [PubMed] [Google Scholar]
- 27.He T., et al. A bibliometric analysis of research on the role of BDNF in depression and treatment. Biomolecules. 2022;12(10) doi: 10.3390/biom12101464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gottlieb S.S., et al. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J. Am. Coll. Cardiol. 2004;43(9):1542–1549. doi: 10.1016/j.jacc.2003.10.064. [DOI] [PubMed] [Google Scholar]
- 29.Rutledge T., et al. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J. Am. Coll. Cardiol. 2006;48(8):1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 30.Rumsfeld J.S., et al. Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J. Am. Coll. Cardiol. 2003;42(10):1811–1817. doi: 10.1016/j.jacc.2003.07.013. [DOI] [PubMed] [Google Scholar]
- 31.Jiang W., et al. Relationship between depressive symptoms and long-term mortality in patients with heart failure. Am. Heart J. 2007;154(1):102–108. doi: 10.1016/j.ahj.2007.03.043. [DOI] [PubMed] [Google Scholar]
- 32.Xiong G.L., et al. Inflammation markers and major depressive disorder in patients with chronic heart failure: results from the sertraline against depression and heart disease in chronic heart failure study. Psychosom. Med. 2015;77(7):808–815. doi: 10.1097/PSY.0000000000000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mommersteeg P.M.C., et al. Depression and markers of inflammation as predictors of all-cause mortality in heart failure. Brain Behav. Immun. 2016;57:144–150. doi: 10.1016/j.bbi.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 34.Chen X., et al. Current understanding of gut microbiota alterations and related therapeutic intervention strategies in heart failure. Chin. Med. J. 2019;132(15):1843–1855. doi: 10.1097/CM9.0000000000000330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu R.T., Walsh R.F.L., Sheehan A.E. Prebiotics and probiotics for depression and anxiety: a systematic review and meta-analysis of controlled clinical trials. Neurosci. Biobehav. Rev. 2019;102:13–23. doi: 10.1016/j.neubiorev.2019.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liang S., et al. Recognizing depression from the Microbiota(-)Gut(-)Brain Axis. Int. J. Mol. Sci. 2018;19(6) doi: 10.3390/ijms19061592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duan J., et al. Role of depressive symptoms in the prognosis of heart failure and its potential clinical predictors. ESC Heart Fail. 2022;9(4):2676–2685. doi: 10.1002/ehf2.13993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zanos P., Gould T.D. Mechanisms of ketamine action as an antidepressant. Mol. Psychiatr. 2018;23(4):801–811. doi: 10.1038/mp.2017.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim J., et al. Esketamine for treatment-resistant depression - first FDA-approved antidepressant in a new class. N. Engl. J. Med. 2019;381(1):1–4. doi: 10.1056/NEJMp1903305. [DOI] [PubMed] [Google Scholar]
- 40.Jiang W., et al. Long-chain omega-3 fatty acid supplements in depressed heart failure patients: results of the OCEAN trial. JACC Heart Fail. 2018;6(10):833–843. doi: 10.1016/j.jchf.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 41.Cuijpers P., et al. Preventing the onset of depressive disorders: a meta-analytic review of psychological interventions. Am. J. Psychiatr. 2008;165(10):1272–1280. doi: 10.1176/appi.ajp.2008.07091422. [DOI] [PubMed] [Google Scholar]
- 42.Beekman A.T., et al. Preventing depression in high-risk groups. Curr. Opin. Psychiatr. 2010;23(1):8–11. doi: 10.1097/YCO.0b013e328333e17f. [DOI] [PubMed] [Google Scholar]
- 43.Wu Y., et al. Prevalence and predisposing factors of depressive symptoms in patients with stable coronary artery disease: a cross-sectional single-center study. Aging (Albany NY) 2019;11(12):3958–3968. doi: 10.18632/aging.102026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wu Y., et al. New insights into the comorbidity of coronary heart disease and depression. Curr. Probl. Cardiol. 2021;46(3) doi: 10.1016/j.cpcardiol.2019.03.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.