The COVID-19 pandemic has led to increases in anxiety and depression worldwide.1 While mental health challenges and pandemic-related stress may trigger alcohol drinking to cope,2 there is substantial heterogeneity in changes of drinking patterns from before to during the pandemic.3 Individuals with a history of Alcohol Use Disorder (AUD) may be vulnerable to COVID-related complications and alcohol relapse.4,5 We examined longitudinal changes in alcohol-related and quality of life (QoL) outcomes among individuals with AUD (separated by treatment history) and contrasted these time changes to those observed among healthy controls.
Method
From June 3, 2020, to March 5, 2021, we reached out to 1,203 prior participants of the National Institute on Alcohol Abuse and Alcoholism (NIAAA) Natural History Protocol. After excluding participants that (1) did not respond (n = 548), (2) declined/withdrew (n = 233), (3) completed the survey after March 11, 2021 (n = 23), and (4) had missing data on primary study variables (n = 21), 378 participants were enrolled in the NIAAA COVID-19 Pandemic Impact of Alcohol (C19-PIA) Study. Data were collected by phone and/or through an online survey. The study sample was 46.6% female, 52.7% White, 32.0% Black, and 15.3% Other Race. Most participants (91.0%) resided in Maryland (57.4%), Washington, DC (19.8%), or Virginia (13.8%). AUD diagnosis was determined to be positive in 163 participants (43.1%), using Structured Clinical Interview for DSM-IV or DSM-5, in the Natural History Protocol.6 Of these individuals, 109 underwent inpatient treatment at NIAAA. Based on history of AUD treatment status, we created three groups: “healthy control” (56.9%; n = 215, of which 36 were nondrinkers); “non-treatment AUD” (14.3%; n = 54); and “treatment AUD” (28.8%; n = 109). Of the 378 participants, 320 (84.7%) were asked to report alcohol craving and 293 (77.5%) also provided data on QoL. The study was approved by the National Institutes of Health Intramural Institutional Review Board.
Data mapping onto 3 timepoints were extracted from the Natural History Protocol (T1) and the C19-PIA Study (T2: retrospectively reported pre-pandemic timepoint; T3: timepoint during the pandemic). Time lapsed from T1 to C19-PIA Study (“cohort”) ranged from 28.8% <1 year, 37.6% 1-2 years, and 33.6% 3-5 years. Participant enrollment was stratified into 3 phases: from June 3, 2020, to July 31, 2020 (27.8%); from August 1, 2020, to November 22, 2020 (37.0%); and from November 23, 2020, to March 5, 2021 (35.2%). Study outcomes included Alcohol Use Disorders Identification Test (AUDIT) for problematic drinking,7 Penn Alcohol Craving Scale for alcohol craving,8 and World Health Organization QoL-BREF for 4 QoL domains.9 Multilevel modeling was used to account for the nesting structure of observations across time within participants. The multilevel models tested interactions of time and AUD treatment status on study outcomes while adjusting for age, sex, race, cohort, and enrollment phase.
Results
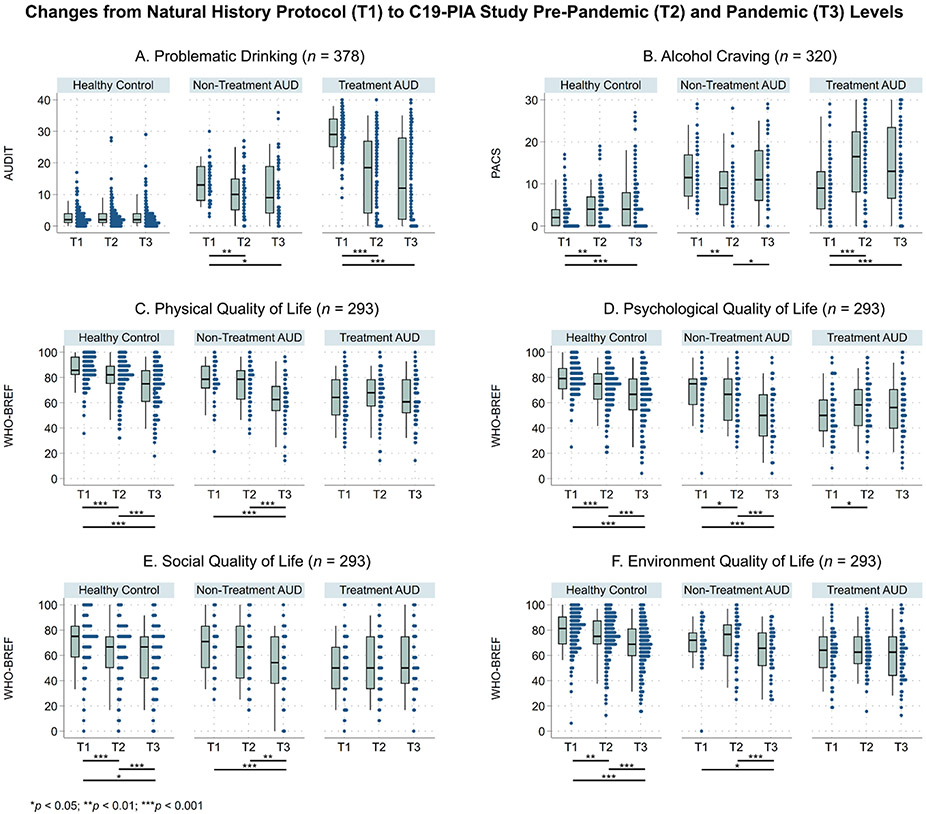
Longitudinal changes in outcomes varied by AUD-treatment status (Figure 1). Pairwise effects of time on outcomes are presented in Supplemental Table 1. Problematic drinking in the healthy control group remained low across time. Individuals with AUD regardless of treatment history scored lower on problematic drinking at T2 and T3 relative to T1. Despite these declines, AUDIT scores remained the highest in the treatment AUD group at T3 (Mean = 15.0, SD = 13.2). Increases in alcohol craving from T1 to T3 were observed in the healthy control and treatment AUD groups. Alcohol craving in the non-treatment AUD group decreased from T1 to T2 and increased from T2 to T3. All 4 QoL domains in the healthy control group decreased across time. Similar declines were observed for most QoL domains in the non-treatment AUD group. QoL scores in the treatment AUD group were the lowest at T1 and remained generally low across time.
Figure.
Changes in problematic drinking, alcohol craving, and quality of life domains by AUD-treatment groups
The box plots show the 5th, 25th, 50th, 75th, and 95th percentiles of study outcomes, and the distributions of data points are plotted to the right of the box plots. More heterogeneous responses were observed at T2 and T3 than at T1. Missing data in PACS (n = 58) reflected a skip logic for individuals who abstained from alcohol at T3. Missing data in quality of Life (QoL) were found in 85 participants. Missingness in QoL did not differ by age, sex, race, cohort, or enrollment phase, and were handled using complete case analyses.
Abbreviations: AUD = alcohol use disorder, AUDIT = Alcohol Use Disorders Identification Test, PACS = Penn Alcohol Craving Scale, WHOQOL-BREF = World Health Organization QoL-BREF. T1, Natural History Protocol; T2, C19-PIA Study Retrospective Report of Pre-Pandemic Levels; T3, C19-PIA Study During Pandemic.
Discussion
Relative to pre-pandemic levels, problematic drinking remained low among healthy controls and declined among individuals with a history of AUD during the pandemic. Reductions in AUDIT scores in the treatment AUD group may reflect potential beneficial effects of the NIAAA inpatient treatment program and/or more limited social opportunities for drinking during the pandemic.10,11 However, despite within-group reductions, the average pandemic AUDIT score in this group was still above the clinical threshold (≥8), indicating the need for continued intervention.
Increases in alcohol craving in the healthy control and treatment-seeking AUD groups revealed an understudied dimension of drinking warranting surveillance. Fewer recreational and social activities along with higher COVID-related stress (e.g., unemployment, losing a loved one, financial stress) may have contributed to QoL reductions among healthy controls.12,13 Lack of change in QoL among individuals with AUD may reflect a floor effect given the initially low QoL levels.
Study limitations include a convenience regional sample limiting generalizability, attrition from Natural History Protocol, varied time lapsed from T1 to the C19-PIA Study, T2 retrospective report, partial data on QoL, and lack of AUD diagnostic and treatment data at T3. More research is needed to understand challenges individuals with AUD encountered during the pandemic (e.g., social isolation, disruption to treatment) to inform approaches (e.g., telemedicine) to support recovery from AUD.
Supplementary Material
Acknowledgements:
The authors would like to thank Betsy Davis, Cheryl Jones, Samantha Fede, Alyssa Brooks, Tonette Vinson, Yvonne Horneffer, LaToya Sewell, the ClinDB IT team (Thuy Van, Etienne Lamoreaux, Denise Gates-Nee, Nancy Agarwal, Patty Bates, Jonathan Folkers), and the intrepid postbaccalaurate Intramural Research Training Award fellows (Hannah Kim, Noa Leiter, Emma McCabe, Carlos Melendez, Kurren Parida, Rhianna Vergeer, Ugne Ziausyte) for supporting the execution of the C19-PIA Study.
Funding Support:
This study was supported by NIAAA Division of Intramural Clinical and Biological Research (Z1A AA000130, Z1A AA000466) and an NIAID Intramural Targeted Anti-COVID (ITAC) Award.
Footnotes
Role of the Sponsor: The content of this study is solely the responsibility of the authors. The sponsors funded the C19-PIA Study and had no role in the design, analysis, or interpretation of study findings.
Conflicts of Interest: The authors do not have any conflicts of interest to disclose.
Previous Presentation: An earlier version of this study was presented virtually at the 2021 American Psychiatric Association (APA) Annual Meeting.
Trial Registration: ClinicalTrials.gov identifier: NCT04391816
References
- 1.COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koob GF, Powell P, White A. Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19. American Journal of Psychiatry. 2020;177(11):1031–1037. [DOI] [PubMed] [Google Scholar]
- 3.Acuff SF, Strickland JC, Tucker JA, Murphy JG. Changes in alcohol use during COVID-19 and associations with contextual and individual difference variables: A systematic review and meta-analysis. Psychol Addict Behav. 2022;36(1):1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim JU, Majid A, Judge R, et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. The Lancet Gastroenterology & Hepatology. 2020;5(10):886–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bailey KL, Samuelson DR, Wyatt TA. Alcohol use disorder: A Pre-existing Condition for COVID-19? Alcohol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.First MB. Structured clinical interview for the DSM (SCID). The encyclopedia of clinical psychology. 2014:1–6. [Google Scholar]
- 7.Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT: The alcohol use disorders identification test: Guidelines for use in primary health care. In: AUDIT: The alcohol use disorders identification test: Guidelines for use in primary health care. World Health Organization; 1992. [Google Scholar]
- 8.Flannery B, Volpicelli J, Pettinati H. Psychometric properties of the Penn alcohol craving scale. Alcoholism: Clinical and Experimental Research. 1999;23(8):1289–1295. [PubMed] [Google Scholar]
- 9.Group WHOQOL. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological medicine. 1998;28(3):551–558. [DOI] [PubMed] [Google Scholar]
- 10.Bramness JG, Bye EK, Moan IS, Rossow I. Alcohol use during the COVID-19 pandemic: self-reported changes and motives for change. European Addiction Research. 2021:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jackson KM, Merrill JE, Stevens AK, Hayes KL, White HR. Changes in Alcohol Use and Drinking Context due to the COVID-19 Pandemic: A Multimethod Study of College Student Drinkers. Alcoholism: clinical and experimental research. 2021;45(4):752–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park KH, Kim AR, Yang MA, Lim SJ, Park JH. Impact of the COVID-19 pandemic on the lifestyle, mental health, and quality of life of adults in South Korea. PLoS One. 2021;16(2):e0247970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luk JW, Stangl BL, Schwandt ML, et al. A person-centered approach to capture health disparities and multidimensional impact of COVID-related stressors. Am Psychol. Published online August 25, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.