This case report concerns the rare case of an adolescent with a distal semimembranosus tendinopathy leading to operative management. Her history and examination were in keeping with the diagnosis; however, her medical imaging had some additional features not described for this particular condition and more consistent with a chronic traction injury and partial rupture with incomplete avulsion of the tendon at its insertion. The aim of operative management was to restore anatomy and function, including power in a young, high-level athlete, as well as to alleviate pain. This article may help as a guide for clinicians in the future diagnosis and treatment of this uncommon condition.
Semimembranosus tendinopathy is defined according to the International Consensus (ICON) 2019 statement as persistent tendon pain and loss of function related to mechanical loading. 22 In cases of greater than 6 weeks duration, as in this case study, this is referred to as chronic, thus leading to potential pathologic changes of interstitial microscopic failures, central necrosis, or partial rupture. 9 There are few articles in the literature regarding semimembranosus tendinopathy. A literature search was performed on PubMed for both paediatric and adolescent types. Searching for semimembranosus tendinopathy alone revealed 5 articles based on adult case series. 7,11,12,19,20 Therefore, there was relatively little information in the literature to guide us in our approach to managing this adolescent case.
Anatomy
The semimembranosus muscle appears to play an integral role in stabilization of the rotating knee. 4,10,15 External rotational movement of the knee joint with rapid acceleration and deceleration cutting maneuvers requiring activation of the medial hamstrings are noted in female European handball players. 5 The anatomic characteristics of the semimembranosus are detailed in Table 1 and Figure 1.
Table 1.
Anatomy of the Semimembranosus 17
| Origin | Ischial tuberosity |
|---|---|
| Insertion |
|
| Innervation | Sciatic nerve, tibial division L5, S1. |
| Function | Acts to flex the knee and to internally rotate the knee joint. It also acts to extend the hip. |
Figure 1.
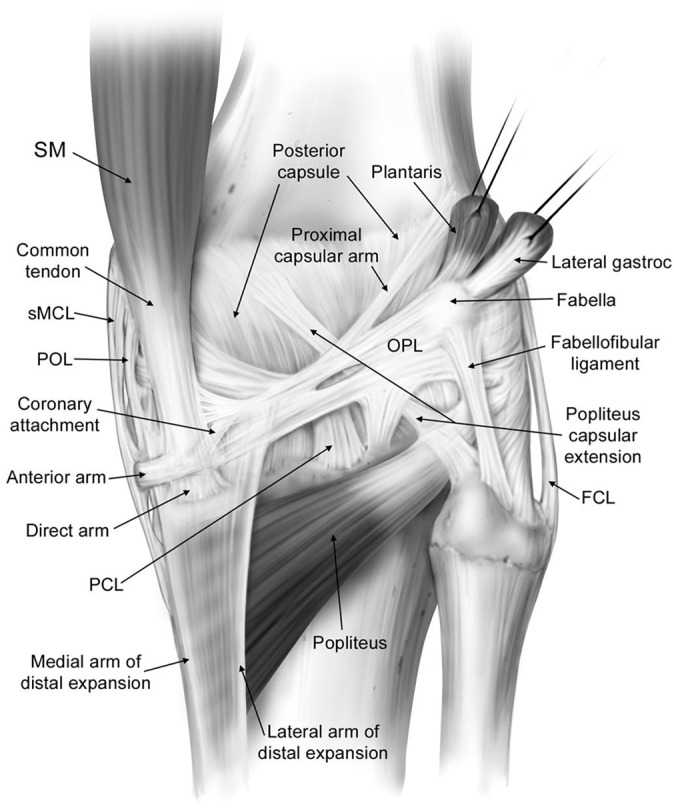
Anatomy of the posterior aspect of a right knee with the medial and lateral gastrocnemius complexes and neurovascular structures removed. FCL, fibular (lateral) collateral ligament; Lateral gastric, lateral gastrocnemius; OPL, oblique popliteal ligament; PCL, posterior cruciate ligament; POL, posterior oblique ligament; SM, semimembranosus muscle; sMCL, superficial medial collateral ligament. Image from LaPrade et al 17 . Reproduced with permission from Wolters Kluwer.
There are a number of causes of medial knee pain in an adolescent athlete. These differential diagnoses include intra- and extra-articular pathologies and should also include more sinister pathologies. These are listed in Table 2. These differential diagnoses can be excluded by history, physical examination, and imaging. Of note is the potential for concomitant pathology. Some authors consider that concomitant pathology may be causal to the semimembranosus tendinitis because of a change in knee mechanics or function. 20 One must also consider tumor and infection as a differential diagnosis in all patients, but especially so in the young with pain about the knee.
Table 2.
Differential Diagnosis of Posteromedial Knee Pain a
| Differential Diagnosis | Comments |
|---|---|
| Semimembranosus muscle tear | History of acute injury. Imaging: radiograph for avulsion, MRI for soft tissue |
| Medial collateral ligament injury | History and examination. Valgus stress pain and laxity |
| Medial meniscal tear | History, clinical examination, MRI. May be concomitant with SMT |
| Femoral/tibial osteonecrosis | Joint pain. Imaging: Abnormal radiographs, CT, MRI |
| Pes anserine bursitis | Located more anteriorly and distally than SMT, medial to tibial tuberosity |
| Bony stress reaction/fracture | Examination: localized pain. MRI |
| Baker (popliteal) cyst | Examination: posterior mass. Imaging: MRI scan |
| Semimembranosus bursitis | Clinical examination and MRI scan |
| Osteoarthritis (medial) | Joint line pain. Imaging: changes on radiographs, CT, MRI |
| Snapping knee syndrome | Palpable snap between semitendinosus and gracilis |
| Tumor/infection | History, red flags, imaging, blood laboratory results |
a CT, computed tomography; MRI, magnetic resonance imaging; SMT, semimembranosus tendinopathy.
Methods
Ethics committee approval was received for this case report, and written consent was attained from both the patient and parent.
History
The female patient presented first at age 15 years with insidious onset of posteromedial left knee pain and swelling. This gradually worsened over a period of 9 months. The patient was a high-level active European handball player with a past medical history of iron- and vitamin D deficiency for which she takes supplements. She noted pain primarily in the posteromedial aspect of her knee after training or competing in European handball, in which she performed explosive type activities including running and jumping, stopping abruptly, and rapid direction changing. She had onset of pain after completing her activity, and the pain would last for days. This pain was severe, sharp, and localized to the posteromedial aspect of the knee. She had associated swelling in the same region. After onset, her pain was exacerbated by activities such as running, jumping, and climbing stairs. She was awoken at night with the pain and was uncomfortable sitting in a chair at rest during the days after training or competing. She rested from training and competition for 10 weeks, with little pain during this time. There was a rapid return of pain upon resuming handball. A second pause in activity and adjusted training did not result in any improvement in symptoms. Her pain was not relieved by simple analgesia or nonsteroidal anti-inflammatory medication.
Examination
On examination, she had normal alignment of the lower limb and a normal gait. Swelling and tenderness were noted of the posteromedial aspect of the knee in the location of the tibial attachment of the semimembranosus. There was no defect along the tendon. There was no joint effusion. She had full range of motion. Isometric testing of the hamstrings reproduced her pain. Her meniscal, ligament, and patellofemoral examinations were unremarkable. Her Knee injury and Osteoarthritis Outcome Score (KOOS) results were as follows: pain 61, symptoms 93, activities of daily living 44, sport 10, and quality of life 25.
Investigations
A magnetic resonance imaging (MRI) scan was conducted first. This demonstrated fluid signal intensity changes at the tendon-bone interface in keeping with cystic change within the defect at the insertion of the direct arm of the semimembranosus tendon. There was marked increased signal in the subcortical proximal tibia adjacent to the defect indicative of a stress response (Figure 2). This is not a common finding in semimembranosus tendinopathy on MRI scans reported in the literature. 16,21,26 Peritendinous edema was also noted. There were no other changes in the surrounding soft tissue. These findings were in keeping with an active chronic traction injury.
Figure 2.
Magnetic resonance images of the patient’s knee. (A) Axial image showing increased signal in the tibia and signal at the tendon-bone interface (arrow). (B) Sagittal image shows increased signal surrounding the semimembranosus tendon (arrow). (C) Coronal image demonstrating increased signal surrounding the semimembranosus tendon and bony edema.
Computed tomography (CT) demonstrated a depression in the proximal posteromedial tibia in the location of the semimembranosus insertion of the direct head. There was sclerosis and also cystic changes at this site (Figure 3).
Figure 3.
(A) Axial, (B) sagittal, and (C) coronal CT images of left knee demonstrating a defect with a saucer-like depression (arrows) and cortical thickening at the attachment site of the semimembranosus.
Of note, there were no aggressive features and no mass lesions in the medical imaging to suggest a neoplastic process.
Surgical Management
Upon failure of nonoperative therapy for over 9 months, the decision was made to proceed to operative management. This was done as open exploration of the semimembranosus tendon and proximal posteromedial tibia. Consent for the procedure was obtained from both the adolescent patient and her parent.
The patient was given a general anesthetic and femoral nerve block, placed supine on the operating table, a lateral side support was placed at the thigh and a bolster was used for flexion positioning to 90°. A tourniquet was applied to the thigh, but not inflated. An examination under anesthesia was then performed; the knee ligaments were stable and there was full range of motion.
A posteromedial approach was made to the knee. A longitudinal incision was made over the posteromedial aspect of the knee, extending from the joint line distally approximately 4 cm in length. The adductor tubercle and the posteromedial proximal tibia were used as landmarks. The subcutaneous fat was incised. Care was taken with the main structures at risk - the infrapatellar branch of the saphenous nerve, the saphenous nerve, and saphenous vein. The sartorius fascia was incised. The semimembranosus tendon and bursa were identified.
On inspection, the semimembranosus tendon bursa was noted to be thickened and the tendon itself was thickened and sat slackened without tension with the knee both in extension and in flexion. It was still attached to its insertion site on the tibia via thickened degenerative fibrotic tissue (Figure 4, A and B). The attachment was elevated with sharp dissection. It appeared macroscopically to be a chronic traction type injury to the insertion with associated granulation tissue. The distal tendon substance was degenerative and fibrotic. Healthy tendon was debrided of degenerative tissue. The insertion site was debrided of soft tissue, curetted to freshen up the bone for healing and checked for bone cortical integrity. There was noted concavity in the bone, but no cyst. Solid cortical bone was found here and deemed suitable for use of a 2-anchor technique for reattachment of the tendon. Two Juggerknot 3.5-mm anchors (Zimmer Biomet) were placed approximately 1 cm apart proximally and distally at the semimembranosus tendon insertion site, each anchor having 2 braided nonabsorbable sutures with needle attached. Locking stitches were placed in the tendon and then the tendon was cinched down to the anchor site (Figure 4C). Tension was checked in both flexion and full extension before final locking knots being tied. The knee was checked through range of motion again and the repair noted to be stable. The operative site was cleansed with normal saline and a layered closure performed using absorbable braided sutures. After dressings were applied, a range of motion brace was applied to the knee, locked to limit extension to 30° with flexion to 90°.
Figure 4.
Photographs demonstrating the medial aspect of the knee. (A) A depression in the tibia at the insertion site of the semimembranosus (arrow). (B) The semimembranosus tendon with thickened degenerative tissue distally (arrow). (C) The repaired tendon.
Postoperative Assessment and Rehabilitation
The initial 3 weeks postsurgery were spent in the range of motion brace full time, with extension limited to 30° and flexion to 90°. Crutches and partial weightbearing were instructed for 6 weeks postoperatively. All active flexion of the knee was avoided during the first 6 weeks and hip flexion should be associated with passive flexion of the knee. Passive range of motion started day 1 postoperatively. Extension range of motion was gradually increased from week 3 to full extension under orthopaedic and physiotherapy guidance. Stationary cycling on a high seat without resistance was also commenced. Active range of motion was commenced at this time. Loaded activity of the hamstrings began at week 6 postoperatively starting with isometric training. Heavy strength training was avoided for the first 3 months. A return to full active sport was planned no earlier than 6 months postoperatively with the avoidance of explosive type activity in the interim.
At 6 weeks postoperatively, the patient had little pain in her knee, and had full extension and flexion to 110°. There was good quadriceps control and hamstring activation. She had little swelling, and all wounds were well healed. At 4 months postoperatively, the patient had no pain in her knee for all daily activities. She could run on a flat surface pain free. She was undertaking strength training pain free. There was no pain at rest including night-time. She required no analgesia. She had full range of motion and equal strength to her contralateral knee, including hamstrings, on testing with physiotherapy. The KOOS at this point was 100 for pain, symptoms, and activities of daily living; sports was 90, and quality of life 75.
At 6-month follow-up, she had returned to full sporting activity, including European handball tournaments, and was pain free. Isokinetic testing was performed, and her strength was equal bilaterally. This was tested before return to sport. Her ongoing management included a sport-specific continuing regime of hamstring strengthening, stretching, and warm up exercises to reduce the risk of recurrence.
Discussion
A search of PubMed was conducted for articles related to the surgical treatment of semimembranosus tendinitis. Inclusion criteria included articles related specifically to semimembranosus tendonitis, tendinopathy, or similar pathology, for example tenosynovitis. Exclusion criteria were acute traumatic injuries. A total of 5 articles regarding surgical management of semimembranosus tendonitis or related diagnoses were found. 7,11,12,19,20
This case is unique in its presentation to the literature in that it is the first reported adolescent case of semimembranosus chronic traction injury at its distal insertion requiring operative management. It differs from the cases of semimembranosus tenosynovitis reported by Melton et al 19 in that this appears to be more likely either a chronic traction injury resulting in a stress response at the tendon bone interface with associated edema in the tibia noted on MRI scan, or this could represent a rupture that has healed with poor quality tissue. There were the operative findings of thickening and slackening of the tendon rather than just inflammation of the tenosynovium. 11,19 The tendon itself macroscopically had chronic degenerative fibrotic changes in keeping with chronic tendinopathic changes. 9,18 Histologic samples were not taken, as they were unfortunately discarded in error. This is a weakness of this study. We thus use the term tendinopathy in our description as opposed to tendinosis or tendinitis. 9,18 Changes in the tendon may be similar to those seen in other tendinopathy, for example, tennis elbow with a concentration of fibroblasts, vascular hyperplasia, and disorganized collagen. 1 This may have been caused in this adolescent athlete by repetitive overloading during explosive activation of the semimembranosus muscle during her participation in high level European handball. Another cause may be an occult injury that has healed poorly, because of repeated subsequent overloading with her sporting activities. Given the infrequent presentation of this problem, an occult precipitating injury could explain the initiation of her pathology.
The MRI findings of bone marrow edema within the proximal tibia and cystic changes at the semimembranosus insertion are not mentioned in the literature as associated with semimembranosus tendinopathy. 16,21,26 Thus, confirmation of the diagnosis became an indication for surgery. Some of these MRI findings have been mentioned in the literature associated with complete avulsion injuries of the semimembranosus tendon. 3,14,23,25 Other imaging reports in the literature regarding semimembranosus tendon ruptures do not mention bony changes on MRI scan. 2,8,13,25 There have been a small number of reports in the literature of semimembranosus distal tendon rupture and avulsion injuries. These occur in sports such as rugby, football (soccer), and American football. 3,6,8,23,25 Our case report appears to represent a chronic traction injury with tendinopathy and a likely associated with an incomplete avulsion injury of the semimembranosus at its insertion on the tibia.
The aim of the specific surgical technique used in this procedure was to restore normal anatomy and thus function and power, which is required in the young athlete in addition to the goal of pain relief. Elevation of the tendon with excision of chronic degenerative tissue was required in this case similar to that described by Ray et al. 20 Reinsertion of the tendon to its corrected length in an anatomically correct position was deemed the most appropriate intervention at the time of operation. This is in contrast to that described by Ray et al 20 where the tendon was rerouted to reduce mechanical irritation. Also, in contrast to other previously described surgical treatments, this case required treatment restoring length tension relationship of the muscle and tendon rather than incision and, or excision of the tendon sheath and bursa. 11,19 Release of the tendon as described by Hendel et al 10,12 in cases of post total knee replacement was not indicated here, because this would reduce hamstring power and function in a high-level athlete.
Arthroscopy was not performed in this case as there was clear diagnostic features specific to the tendon and no intraarticular pathology clinically or on advanced imaging with CT and MRI. This case would thus be deemed, as per the Ray et al 20 classification, a primary semimembranosus tendinitis. At our institute, we believe that arthroscopy should be undertaken if indicated by history, clinical features, and imaging and not for all cases of semimembranosus tendinopathy; however, it may be used diagnostically if there is concomitant intra-articular pathology. 7,19 The diagnosis of this extra-articular condition is made by concise use of history, examination, and advanced imaging and thus arthroscopy may not be required.
We believe imaging in this case did not need to include bone scan for diagnostic purposes in agreeance with Melton et al. 19 Clear findings on history and physical examination excluding intra-articular pathology and use of high-quality CT and MRI allow for accurate location of the pathology.
In summary, the diagnosis of semimembranosus tendinopathy is uncommon, and the occurrence in the athlete population is unknown. 7 As previously noted in the literature regarding this problem, nonoperative management should be attempted primarily, and only on failure of this should operative intervention be undertaken. 7,11,12,19,20 Nonoperative interventions may include avoidance of aggravating activity, activity modification, sports rehabilitation training, physiotherapy, and anti-inflammatory medications. Corticosteroid injection may be used in some cases of distal hamstring irritation with moderate success. 24 However, we recommend cautious use in the young sporting population with concern for risk of tendon rupture. There are no previously documented cases of operative management of semimembranosus tendinopathy in the pediatric and adolescent population.
Conclusion
This case report involved a relatively uncommonly diagnosed, and even more rarely surgically treated, problem in the adolescent sports population and may be used as a reference point for future cases.
Footnotes
Final revision submitted September 27, 2022; accepted October 11, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: D.M.'s fellowship was supported indirectly by Smith & Nephew. M.J.S. has received research support and consulting fees from Smith & Nephew. L.E. has received research support from Zimmer, fellowship support from Smith & Nephew, consulting fees from Smith & Nephew, and royalties from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Norwegian Regional Committee for Medicine and Health Research Ethics (ref No. 341626).
References
- 1. Ahmad Z, Siddiqui N, Malik SS, Abdus-Samee M, Tytherleigh-Strong G, Rushton N. Lateral epicondylitis: a review of pathology and management. Bone Joint J. 2013;95-B(9):1158–1164. [DOI] [PubMed] [Google Scholar]
- 2. Aldebeyan S, Boily M, Martineau PA. Complete tear of the distal hamstring tendons in a professional football player: a case report and review of the literature. Skeletal Radiol. 2016;45(3):427-430. [DOI] [PubMed] [Google Scholar]
- 3. Alioto RJ, Browne JE, Barnthouse CD, Scott AR. Complete rupture of the distal semimembranosus complex in a professional athlete. Clin Orthop 1997;336:162–165. [DOI] [PubMed] [Google Scholar]
- 4. Bejui J, Walch G, Gonon GP, Carret JP, Neidhardt JH, Fischer LP. Anatomical and functional study on the musculus semimembranosus. Anat Clin. 1984;6(3):215–223. [DOI] [PubMed] [Google Scholar]
- 5. Bencke J, Curtis D, Krogshede C, Jensen LK, Bandholm T, Zebis MK. Biomechanical evaluation of the side-cutting manoeuvre associated with ACL injury in young female handball players. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1876–1881. [DOI] [PubMed] [Google Scholar]
- 6. Blakeney WG, Thaunat M, Ouanezar H, de Campos GC, de Padua VBC, Sonnery-Cottet B. Distal semimembranosus tendon avulsions: acute surgical repair in a professional rugby player. Orthop J Sports Med. 2017;5(10):2325967117731102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bylund WE, de Weber K. Semimembranosus tendinopathy: one cause of chronic posteromedial knee pain. Sports Health. 2010;2(5):380–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chan KK, Resnick D, Goodwin D, Seeger LL. Posteromedial tibial plateau injury including avulsion fracture of the semimembranous tendon insertion site: ancillary sign of anterior cruciate ligament tear at MR imaging. Radiology. 1999;211(3):754–758. [DOI] [PubMed] [Google Scholar]
- 9. Clancy WG. Tendinitis and plantar fasciitis in runners. Orthopedics. 1983;6(2):217–323. [DOI] [PubMed] [Google Scholar]
- 10. Flaxman TE, Alkjær T, Simonsen EB, Krogsgaard MR, Benoit DL. Predicting the functional roles of knee joint muscles from internal joint moments. Med Sci Sports Exerc. 2017;49(3):527–537. [DOI] [PubMed] [Google Scholar]
- 11. Halperin N, Oren Y, Hendel D, Nathan N. Semimembranosus tenosynovitis: operative results. Arch Orthop Trauma Surg. 1987;106(5):281–4. [DOI] [PubMed] [Google Scholar]
- 12. Hendel D, Weisbort M, Garti A. Semimembranosus tendonitis after total knee arthroplasty: good outcome after surgery in 6 patients. Acta Orthop Scand. 2003;74(4):429–430. [DOI] [PubMed] [Google Scholar]
- 13. John R, Chouhan DK, Dhillon MS. Neglected, semimembranosus osteochondral avulsion fracture of the posteromedial tibial plateau. Trauma Case Rep. 2018. 26;15:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Khoshnoodi P, Tehranzadeh AD, Dunn JM, Tehranzadeh J. Semimembranosus tendon avulsion fracture of the posteromedial tibial plateau associated with posterior cruciate ligament tear and capsular rupture. Skeletal Radiol. 2014;43(2):239–242. [DOI] [PubMed] [Google Scholar]
- 15. Kittl C, Becker DK, Raschke MJ, et al. Dynamic restraints of the medial side of the knee: the semimembranosus corner revisited. Am J Sports Med. 2019;47(4):863–869. [DOI] [PubMed] [Google Scholar]
- 16. Koulouris G, Connell D. Hamstring muscle complex: an imaging review. Radiographics. 2005;25(3):571-586. doi: 10.1148/rg.253045711. Erratum in: Radiographics . 2005;25(5):1436. [DOI] [PubMed] [Google Scholar]
- 17. LaPrade RF, Morgan PM, Wentorf FA, Johansen S, Engebretsen L. The anatomy of the posterior aspect of the knee. An anatomic study. J Bone Joint Surg Am. 2007;89(4):758–764. [DOI] [PubMed] [Google Scholar]
- 18. Maffulli N, Khan KM, Puddu G. Overuse tendon conditions: time to change a confusing terminology. Arthroscopy. 1998;14(8):840–843. [DOI] [PubMed] [Google Scholar]
- 19. Melton JK, Memarzadeh A, Dunbar WH, Cross MJ. Semimembranosus tenosynovitis: diagnosis and management of a commonly missed cause of posteromedial knee pain. Knee. 2017;24(2):305–309. [DOI] [PubMed] [Google Scholar]
- 20. Ray JM, Clancy WG, Jr, Lemon RA. Semimembranosus tendinitis: an overlooked cause of medial knee pain. Am J Sports Med. 1988;16(4):347–351. [DOI] [PubMed] [Google Scholar]
- 21. Rothstein CP, Laorr A, Helms CA, Tirman PF. Semimembranosus-tibial collateral ligament bursitis: MR imaging findings. Am J Roentgenol. 1996;166(4):875–877. [DOI] [PubMed] [Google Scholar]
- 22. Scott A, Squier K, Alfredson H, et al. ICON 2019: International Scientific Tendinopathy Symposium Consensus: clinical terminology. Br J Sports Med 2020;54(5):260–262. [DOI] [PubMed] [Google Scholar]
- 23. Varela JR, Rodríguez Soler R, Gonzalez J, Pombo S. Complete rupture of the distal semimembranosus tendon with secondary hamstring muscles atrophy: MR findings in two cases. Skeletal Radiol 2000;29(6):362–364. [DOI] [PubMed] [Google Scholar]
- 24. Weiser HI. Semimembranosus insertion syndrome: a treatable and frequent cause of persistent knee pain. Arch Phys Med Rehabil. 1979. Jul;60(7):317–319. [PubMed] [Google Scholar]
- 25. Yao L, Lee JK. Avulsions of the posteromedial tibial plateau by the semimembranosus tendon: diagnosis with MR imaging. Radiology 1989;172(2):513–551. [DOI] [PubMed] [Google Scholar]
- 26. Yoon MA, Choi JY, Lim HK, et al. High prevalence of abnormal MR findings of the distal semimembranosus tendon: contributing factors based on demographic, radiographic, and MR features. Am J Roentgenol. 2014;202(5):1087–1093. [DOI] [PubMed] [Google Scholar]





