Abstract
Firearms are the leading cause of death for high-school age teens. To inform prevention efforts, we characterize the prevalence of healthcare provider (HCP) counseling of caregivers of teens around firearm safety, safety conversation elements, and caregiver receptivity towards counseling. A cross-sectional web survey (6/24/2020–7/22/2020) was conducted among caregivers (n = 2924) of teens (age:14–18). Weights were applied to generate nationally representative estimates. Bivariate analyses and multivariate regressions were examined. Among respondents, 56.0% were women, 75.1% were non-Hispanic White, and mean (SD) age was 47.4. Firearm safety was the least discussed topic among caregivers reporting their teen received HCP preventative counseling (14.9%). For caregivers receiving counseling, the most common issues discussed were household firearms screening (75.7%); storing firearms locked (66.8%); and storing firearms unloaded (53.0%). Only 24.6% of caregivers indicated firearm safety was an important issue for teen HCPs to discuss and only 21.9% trusted teen HCPs to counsel about firearm safety. Female caregivers (aOR = 1.86;95%CI = 1.25–2.78), those trusting their teen’s HCP to counsel on firearm safety (aOR = 9.63;95%CI = 6.37–14.56), and those who received teen HCP firearm safety counseling (aOR = 5.14;95%CI = 3.02–8.72) were more likely to favor firearm safety counseling. Caregivers of teens with prior firearm safety training (aOR = 0.50;95%CI = 0.31–0.80) were less likely to agree that firearm safety was an important preventative health topic. In conclusion, few caregivers receive preventive counseling on firearm safety from their teen’s HCP, with trust a key barrier to effective intervention delivery. Future research, in addition to understanding barriers and establishing effective strategies to increase safety practices, should focus on increasing provider counseling competency.
Keywords: Firearm, Injury prevention, Safe storage, Counseling, Preventative health, Caregiver, Teen
1. Introduction
Firearms are the leading cause of death for high-school aged teens (age 14–18) in the U.S., with 59% resulting from homicide, 37% from suicide, and 3% from unintentional injuries (Cunningham et al., 2018; Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2022). Fatal firearm injuries among teens have increased nearly 44% since 2013, with increases for both homicide and suicide (Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2022). During the past decade, non-fatal firearm injuries among were responsible for ~100,000 emergency department (ED) visits among teens (Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2022). Such injuries are associated with long-term consequences, including increased risk for substance use disorders (Walton et al., 2017), mental health issues (e.g., PTSD) (Garbarino et al., 2002), physical disabilities (DiScala and Sege, 2004), and repeat fatal/non-fatal firearm injuries (Cunningham et al., 2015a; Rowhani-Rahbar et al., 2015). Disparities exist, with firearm homicides/assaults disproportionally affecting Black teens within urban settings and firearm suicides and unintentional injuries disproportionately affecting White and American Indian/Alaskan native teens within suburban/rural settings (Cunningham et al., 2018; Centers for Disease Control and Prevention, National Center for Health Statistics, 2020). Economic costs are substantial, with acute medical treatment for pediatric firearm injuries estimated at nearly $110 million annually before including long-term costs (e.g., lost wages/productivity) (Taylor et al., 2021; Peek-Asa et al., 2017). Given elevated mortality and economic costs, national medical organizations have highlighted the urgent need for research identifying public health solutions that reduce adolescent firearm injury risk (Cunningham et al., 2019; Damari et al., 2018; McLean et al., 2019).
Firearm access remains the most significant risk factor for teen firearm injuries, regardless of underlying intent (Grossman et al., 1999; Johnson et al., 2010; Schnitzer et al., 2019; Miller et al., 2007). In 80% of completed teen firearm suicides and 90% of fatal unintentional firearm injuries, the firearm was obtained from the decedent’s home or the home of a relative (Grossman et al., 1999; Monuteaux et al., 2019). Ecologic studies also demonstrate an association between household firearm ownership rates and teen firearm homicide (Miller et al., 2007). An estimated 34% of U.S. households with children own/maintain firearms, with 21% storing firearms unlocked and loaded, though storing firearms locked and unloaded is considered the safest firearm storage practice (Azrael et al., 2018). Compared to households with younger children, households with teens are more likely to store firearms unlocked and loaded, increasing access and injury risk (Johnson et al., 2006). Given that healthcare provider (HCP) behavioral counseling of caregivers has been shown to increase household locked storage practices in prior studies (Rowhani-Rahbar et al., 2016) and that 92% of adolescents had a well-child visit in 2019 (National Center for Health Statistics, 2019), increasing HCP firearm safety counseling has the potential to reduce teen firearm access and associated injury outcomes.
While data suggests caregivers are receptive to firearm safety counseling (Garbutt et al., 2016; Haught et al., 1995; Forbis et al., 2007), less than 50% of HCPs report conducting routine screening or counseling during patient encounters (Damari et al., 2018). Such research has focused on physician self-report of counseling (Damari et al., 2018; Farcy et al., 2021; Pallin et al., 2019; Juang et al., 2019), with less research examining caregiver attitudes, experiences, and responses to HCP counseling (Garbutt et al., 2016; Haught et al., 1995; Forbis et al., 2007; Fuzzell et al., 2018). Therefore, using data from a nationally representative sample, we: 1) estimate the prevalence of HCP firearm safety screening and/or counseling of U.S. caregivers of high-school age teens in relation to other preventative health topics; 2) assess the key elements of these conversations, as well as any adjustments made to firearm safety practices in response to counseling; and, 3) examine caregiver receptivity towards HCP firearm safety counseling using unadjusted and adjusted logistic regressions. We hypothesized that: 1) firearm safety is the least discussed preventative health topic during teen HCP visits; 2) teen HCP firearm safety counseling is largely focused on storage practices; and 3) caregiver trust in teen HCP and caregiver firearm ownership are key drivers of whether caregivers are receptive towards teen HCP firearm safety counseling. Understanding the teen caregiver’s perspective towards HCP firearm counseling will inform opportunities to enhance current counseling practices and clinician training.
2. Methods
Data are from a cross-sectional, web-based survey of 2924 U.S. primary caregivers of teenage children (age 14–18); conducted (6/24/2020–7/22/2020) by Gallup for the Firearm Safety Among Children and Teens (FACTS) Consortium (Sokol et al., 2021a; Sokol et al., 2021b). Participants were recruited from the Gallup Panel, a probability-based panel of non-institutionalized civilians constructed to be broadly representative of the U.S. population. Gallup regularly recruits panel participants using random-digit dialing (landlines/cell phones) and address-based sampling while intentionally oversampling young adults (age:18–34), individuals from lower educational backgrounds, and members of racial/ethnic minority groups. Eligible panel participants included biological parents and/or primary caregivers (e.g., grandparents) of high-school aged teens who the teen resided with at least some of the time. Eligible caregivers were randomly sampled from the panel and sent email invitations to participate. Following informed consent, panelists self-administered the web-based survey (~15 min-per-participant). Respondents received $5 for survey completion. The University of Michigan IRB reviewed/approved all study procedures. Participants were provided links to online substance use, mental health, and violence resources. For this study, the analytic sample was restricted to the caregiver sample.
3. Measures
3.1. Preventative firearm safety counseling
Past five-year caregiver receipt of preventative counseling about firearm safety (yes/no) by the teen’s HCP, including firearm access screening and/or safety counseling (e.g., locked storage), was measured using an adapted item based on the Counseling on Access to Lethal Means (CALM) model.32 Parallel items regarding screening/counseling for other teen health issues (e.g., bicycle helmets, seat belts, mood) were selected based on American Academy of Pediatrics (AAP) best-practice recommendations (Hagan et al., 2017).
Caregivers indicating receipt of firearm safety counseling were subsequently asked about conversation elements, including screening for household firearm ownership, firearm accessibility (i.e., locked vs. unlocked), storage practices (i.e., loaded vs. unloaded), ammunition accessibility, off-property access, and/or discussions centered around reducing teen access during high-risk periods (e.g., when teen is a risk to themselves/others) (Runyan et al., 2016; Zalsman et al., 2016). Response options were not mutually exclusive, reflecting the possibility for discussions with multiple components.
These caregivers were also asked about changes made in response to counseling, including discussing firearm safety with their teen, moving firearms to an inaccessible location (in the home), purchasing/using locking devices, and/or temporary/permanent removal of firearms from the home. A write-in other option recorded additional safety changes, with responses recoded as appropriate to the response options above.
3.2. Firearm safety counseling receptivity
The dependent variable, caregiver receptivity to firearm safety counseling by their teen’s HCP, was measured using an adapted item from Southwestern Ohio ambulatory research network (SOAR-Net) firearm safety survey (Haught et al., 1995; Forbis et al., 2007). Respondents indicated level of agreement on a 5-point Likert scale (strongly agree-strongly disagree) with the statement “It is important for healthcare providers to discuss gun safety with teens.” For analysis, response options were dichotomized indicating whether caregivers were receptive towards firearm safety, with neutral categorized as not receptive to counseling, consistent with prior research (agree/strongly agree = agree; strongly disagree/disagree/neutral = disagree) (Jeong and WC., 2016; Sieving et al., 2021).
3.3. Provider trust
Caregiver trust in their teen’s HCP to counsel about their teen’s health and firearm safety was assessed with two adapted items from the Wake Forest Physician Trust Scale (Hall et al., 2002). Firearm owning caregivers were also asked how respectful their teens’ HCP was about family firearm ownership. Responses for all three items were measured using a 5-point Likert scale (strongly agree-strongly disagree) and dichotomized for analysis (Jeong and WC., 2016; Sieving et al., 2021).
3.4. Household firearm ownership
Two items assessed whether the primary caregiver or other household members owned firearm(s) using items from the 2015 National Firearm Survey (Cleveland et al., 2017). Items were collapsed to indicate any household firearm ownership (yes/no). Caregiver household firearm ownership (e.g., self and/or spouse/partner/grandparent) was assessed using an item from the 2019 National Firearm Survey (Conner et al., 2021).
3.5. Teen firearm safety training
Caregivers indicated whether their teen ever received (yes/no) any caregiver or professional (e.g., hunter safety course) firearm safety training (i.e., handling, shooting, or storing firearms) using an item created for this survey.
3.6. Community violence exposure
A 9-item version of the “Things I have seen/heard Survey” assessed past 12-months community violence exposure (Richters and Martinez, 1990). An adapted response scale using dichotomized responses (yes/no) was used and a summary score (range 0–9) was created (α = 0.7) (Carter et al., 2016; Carter et al., 2017).
3.7. Risky teen behavior
Eleven items assessed caregiver knowledge about their teen’s involvement in risk behaviors (yes/no) in the prior 12-months. Items were based on AAP best-practice recommendations for screening/counseling on risky teen behavior (e.g., unsafe driving, smoking/vaping, fighting) (Hagan et al., 2017). For analysis, a summary score (range 0–11) was created with higher scores indicating more involvement in risky behaviors (α = 0.7) (Carter et al., 2020).
3.8. Socio-demographics
Gallup survey items measured socio-demographic characteristics (age, biological sex, race/ethnicity, region, educational attainment, marital status, region, military service). Race/ethnicity and educational attainment were collapsed to indicate whether the respondent was non-Hispanic White (vs. other) or had any post-secondary education (yes/no). Respondents were also asked about young children (< age 10, in addition to their teen) living in the household and receipt of public assistance (yes/no) using items from the 2016 American Community Survey (United States Census Bureau, 2020).
3.8.1. Analysis
Following data collection, Gallup provided final survey weights that combined pre-sample weights for constructing national estimates with study-specific post-stratification weights adjusting for differential survey non-response. To construct the final survey weights, the panel sample frame is first weighted to be representative of the general U.S. adult (18+) population based on age, gender, education, race, ethnicity, census region, and age/gender of children using targets from the U.S. Census Bureau’s Current Population Survey 2017 data (United States Census Bureau, 2022). Next, the weighted panel is subset to the intended sample of caregivers with high-school age children (age 14–18), with the resultant weighted distributions used to determine final target population characteristics. Finally, initial weights are adjusted using these targets to address participant non-response and/or case completion. Among invited panelists, 4% (n = 400) initiated but did not complete the full survey (non-completers).
It is important to note that given the sampling design/recruitment strategy, it is not possible to calculate a true participant survey response rate for the sample. Specifically, Gallup maintains basic demographic information on panel participants (including whether they have a child), but does not have information on whether a child was in the eligible age range for this study population (i.e., age 14–18). Thus, sampling proceeded, as noted above, by sending the survey invitation to all panelists known to have at least one child (n = 9352). Survey invitations highlighted the opportunity to participate in a survey intended for caregivers of high-school age children. Thus, panelists with a child outside of this age range may have chosen not to respond to the invitation knowing they were not eligible (rather than being eligible and refusing to complete the planned survey). Within this context of this limitation, Gallup calculated a conservative response rate of 31% from sampled panelists with at least one child.
The analytic sample was restricted to the 95% of caregivers indicating their teen received regular medical care (unweighted N = 2924; restricted sample weighted N = 2753). In total, 7.1% of the unweighted sample was missing data for one or more covariates, with no individual covariate missing more than 3.7% of responses. Given this, missingness was considered negligible and the analytic sample was restricted to those with complete data available (final weighted N = 2535). We also conducted comparisons across key socio-demographic factors between missing vs. non-missing data and found no differences that would suggest systematic bias within the sample due to missingness. Descriptive statistics were analyzed using weighted percentages and corresponding 95% confidence intervals. Key descriptive data (e.g., firearm safety topics discussed by a HCP) were also examined by whether the respondent endorsed household firearm ownership Unadjusted logistic regressions describe bivariate associations with the dependent variable of interest, HCP counseling receptivity. A multivariable logistic regression model was created to estimate the adjusted covariate effects on receptivity towards firearm safety counseling. Model independent variables were chosen based on theory and bivariate significance. Specifically, we focused on the question of trust as a critical aspect of caregiver receptivity given prior literature on vaccine hesitancy and counseling (Benin et al., 2006; Connors et al., 2017). In addition, while not significant bi-variately, we included caregiver perceptions of teen risky behavior (e.g., binge drinking) and community violence exposure given the importance of considering the roles of these co-occurring risk behaviors (e.g., Jessor Problem Behavior Theory) and environmental factors to adolescent firearm outcomes (Carter et al., 2017; Jessor, 1987; Goldstick et al., 2017; Carter et al., 2015; Schmidt et al., 2019). Analyses were conducted using SAS software, Version 9.4.
4. Results
Among our sample of U.S. caregivers of high-school age teens, mean caregiver age was 47.4 years, 56.0% were female, 78.7% married, 15.2% on public assistance, and 14.2% had prior military experience. Further, 75.1% were non-Hispanic White, with additional race and ethnicity breakdowns as follows: 83.4 White, 7.7% Native Hawaiian or Pacific Islander, 5.4% Asian, 2.5% American Indian of Alaskan Native, and 1.0% Black or African American with 92.3% of the sample identifying as non-Hispanic and 7.7% identifying as of Hispanic ethnicity. Among respondents, 54.9% reported household firearm ownership (94.8% owned by the parent and or spouse/partner) and 57.2% indicated their teen received firearm safety training.
4.1. Preventative health counseling
Past five-year caregiver self-report of preventative health counseling from teen HCP is shown in Fig. 1. Among preventative health topics, firearm safety was the least discussed, with 14.9% of caregivers noting a firearm safety discussion during a teen healthcare visit. Among the subset of caregivers receiving counseling (Table 1), the most discussed topics included the presence (yes/no) of firearms, firearm accessibility, and ammunition accessibility. Less discussed topics included off-property access (i.e., asking about firearms in other homes) and reducing teen access during high-risk periods (i.e., risk to themselves/others). Notably, there were no differences in any of the discussed firearm safety topics between firearm owners (weighted N = 147.1) and non-firearm owners (weighted N = 229.7).
Fig. 1.
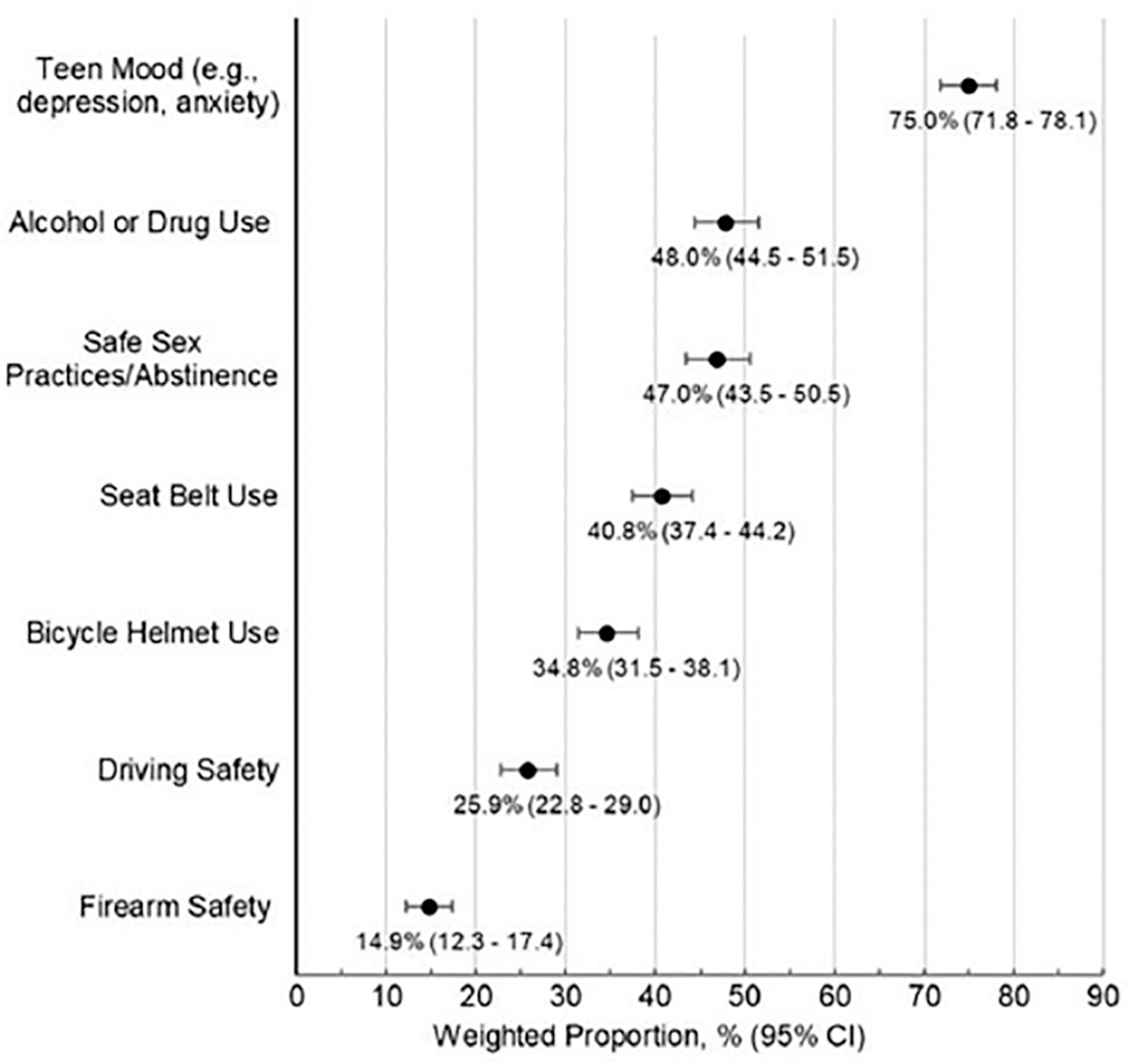
Caregiver self-report of receiving preventative health counseling for key teen preventive health issues within the past five-years from their teen’s HCP. Note: Weighted N=2535; Unweighted N=2522.
Table 1.
Caregiver self-report of subject matter discussed with their teen’s HCP for the subset of caregivers who reported receiving any firearm safety counseling during a routine clinical encounter in the prior five-years.
| Caregiver HCP counseling on firearm safety issues | Caregiver %; (95% CI) |
|---|---|
|
| |
| Screening for firearm(s) in the home | 75.7 (67.2, 84.2) |
| Firearm accessibility (i.e., storing firearms locked) | 66.8 (58.0, 75.5) |
| Storage method (i.e., storing firearms unloaded) | 53.0 (43.7, 62.3) |
| Ammunition accessibility (i.e., storing ammunition separately from firearms) | 51.9 (42.6, 61.2) |
| Off-property access (i.e., access to firearms in homes teens may visit) Reducing firearm access during high-risk periods |
44.2 (34.8, 53.5) |
| Teen is at risk of harming others / having behavioral problems | 36.7 (27.6, 45.9) |
| Teen is at risk of harming themselves / experiencing depression | 34.9 (25.9, 43.9) |
Notes: Subject matter topics are not mutually exclusive; Caregivers may have indicated discussion of more than one topic area; Weighted N = 377; Unweighted N = 367
Among caregivers discussing firearm safety with their teen’s HCP, only 9.8% (95%CI = 3.5–16.2) indicated they made safety changes following the discussion. The most common change was to discuss firearm safety with their teen (50.9%; 95%CI = 14.7–87.1), followed by moving the firearm(s) to an inaccessible home area (33.5%; 95%CI = 0.0–68.8). Only 5.9% (95%CI = 0.0–13.7) reported they purchased or started using a locking device (e.g., safe, cable lock) and 4.1% (95%CI = 0.0–10.5) reported temporary/permanent firearm(s) removal. Notably, while 6.4% (n = 24) of caregivers received a locking device from the teen’s HCP, none used the device.
4.2. Caregiver receptivity towards HCP firearm safety counseling
Among caregivers of high-school age teens, 24.6% indicated they were receptive to their teen’s HCP discussing firearm safety (Table 2). Caregivers noting greater receptivity to counseling discussions were more likely female, from advanced educational backgrounds, and less likely to have a military background. Receptivity to firearm safety counseling also differed by firearm-related factors, with caregivers from firearm owning households and households with teens who received prior firearm safety training less receptive to counseling.
Table 2.
Total sample characteristics and unadjusted bivariate comparisons of caregiver factors associated with being receptive or not receptive towards firearm safety counseling as an important preventative health topic.
| αImportance of firearm safety Counseling for teens | |||||
|---|---|---|---|---|---|
|
|
|
||||
| Agree |
Disagree |
Total % (95% CI) | OR (95% CI) | ||
| 24.6% (CI = 21.7–27.5) % (95% CI) | 75.4% (CI = 72.5–78.3) % (95% CI) | ||||
|
| |||||
| SOCIO-DEMOGRAPHICS | |||||
| Age (mean age) | 47.4 (46.0, 48.9) | 47.4 (46.5, 48.3) | 47.4 (46.1, 50.2) | 1.00 (0.98, 1.02) | |
| Sex (% female) | 70.2 (64.1, 76.3) | 51.4 (47.3, 55.5) | 56.0 (52.5, 59.5) | 2.23 (1.60, 3.11) | |
| Race / ethnicity (% non-Hispanic white) | 72.8 (66.3, 79.3) | 75.8 (72.1, 79.5) | 75.1 (71.9, 78.3) | 0.85 (0.58, 1.25) | |
| Region | |||||
| Northeast | 18.1 (13.6, 22.7) | 15.2 (12.2, 18.3) | 16.0 (13.4, 18.5) | Ref | |
| Midwest | 18.7 (13.8, 23.6) | 23.4 (19.9, 27.0) | 22.3 (19.4, 25.2) | 0.67 (0.41, 1.08) | |
| South | 36.7 (30.0, 43.5) | 37.5 (33.5, 41.4) | 37.3 (33.9, 40.7) | 0.82 (0.53, 1.29) | |
| West | 26.4 (20.8, 32.0) | 23.8 (20.4, 27.3) | 24.5 (21.5, 27.4) | 0.93 (0.59, 1.47) | |
| Education level (% > high school) | 78.5 (70.9, 86.1) | 68.4 (63.7, 73) | 70.9 (66.9, 74.9) | 1.69 (1.03, 2.78) | |
| Marital status (% married) | 78.3 (72.0, 84.5) | 78.8 (75.2, 82.4) | 78.7 (75.6, 81.8) | 0.97 (0.63, 1.48) | |
| Military service (% served) | 7.2 (3.5, 10.9) | 16.5 (13.4, 19.6) | 14.2 (11.7, 16.8) | 0.39 (0.22, 0.72) | |
| Public assistance (% receive) | 13.3 (8.8, 17.8) | 15.8 (12.6, 19) | 15.2 (12.5, 17.9) | 0.82 (0.52, 1.30) | |
| βhild < 10 y/o in household (% yes) | 24.4 (18.3, 30.6) | 27.5 (23.7, 31.3) | 26.7 (23.5, 30) | 0.86 (0.58, 1.26) | |
| FIREARM OWNERSHIP/SAFETY | |||||
| γHousehold firearm ownership (% owners) | 43.3 (36.5, 50.0) | 58.8 (54.7, 62.8) | 54.9 (51.5, 58.4) | 0.54 (0.39, 0.74) | |
| Teen firearm safety training (% trained) | 43.0 (36.4, 49.7) | 61.8 (57.8, 65.8) | 57.2 (53.7, 60.6) | 0.47 (0.34, 0.64) | |
| HEALTHCARE PROVIDER RELATIONSHIP | |||||
| Provider trust (% yes) | 94.2 (91.5, 96.9) | 83.6 (80.4, 86.8) | 86.2 (83.7, 88.8) | 3.17 (1.83, 5.50) | |
| Provider trust for firearm safety counseling (% yes) | 59.2 (52.7, 65.7) | 9.7 (7.3, 12.1) | 21.9 (19.1, 24.7) | 13.54 (9.24, 19.84) | |
| Received firearm safety counseling (% yes) | 38.2 (31.6, 44.8) | 7.2 (5.0, 9.4) | 14.9 (12.3, 17.4) | 7.92 (5.14, 12.19) | |
| VIOLENCE EXPOSURE | |||||
| Friend/family shot/ killed by firearms (% yes) | 13.2 (7.9, 18.5) | 10.7 (8.1, 13.3) | 11.3 (9.0, 13.7) | 1.26 (0.74, 2.16) | |
| δCommunity violence exposure (mean summary score; (SD)) | 0.7 (0.6, 0.9) | 0.9 (0.8, 1.0) | 0.9 (0.8, 1.0) | 0.88 (0.77, 1.02) | |
| PERCEIVED TEEN BEHAVIORS | |||||
| εRisky teen behaviors (mean summary score; (SD)) | 0.7 (0.5, 0.9) | 0.8 (07, 10) | 0.8 (0.7, 0.9) | 0.95 (0.82, 1.09) | |
Weighted N = 2535, Unweighted N=2522
Response categories dichotomized: Agree/strongly agree = agree; strongly disagree/disagree/neutral = disagree.
Children < 10yo living in household, in addition to teen.
Defined as household firearm ownership (parent/family member/teen).
Community violence— summary score (range 0–9) assessing past 12-months exposure (yes/no) to violence in their community.
Risky teen behavior— summary score (range 0–11) assessing past 12-months caregiver reports of teen engagement in any of 11 risky behaviors (e.g., unsafe driving; smoking/vaping; physical fights; risky sexual behaviors).
Caregivers indicating they trusted their teen’s HCP to counsel them about their teen’s health and those receiving HCP firearm safety counseling were three and eight times more likely, respectively, to indicate they were also receptive to firearm safety discussions. These findings were more pronounced when focused specifically on trust in the HCP to counsel around firearm safety, with caregivers trusting their teen’s HCP to counsel on firearm safety thirteen times more likely to also be receptive to counseling (Table 2). Notably, trust in HCPs to provide firearm safety counseling were lower among firearm than non-firearm owning households (18.5%-vs.-25.9%; OR = 0.65 [95% CI = 0.47–0.91]) and higher among those who received firearm safety counseling (57.5%; OR = 7.30 [95% CI = 4.756–11.185]). Within firearm-owning households, caregivers were noted to be three times more likely to indicate receptiveness to counseling when the HCP was also felt to be respectful of their decision to own firearms (73.3%-vs.-45.6%; OR = 3.28 [95% CI = 1.46–7.37]).
In the multivariate analysis (Table 3), female caregivers, those trusting their teen’s HCP to counsel on firearm safety, and those receiving HCP firearm safety counseling were more likely to indicate receptivity towards HCP firearm safety counseling. Conversely, caregivers indicating their teen received firearm safety training previously were less likely to be receptive to counseling.
Table 3.
Multiple logistic regression model examining caregiver factors associated with receptivity towards firearm safety counseling as an important preventative health topic for teens.
| Caregiver characteristics | AOR [95% CI] |
|---|---|
|
| |
| Age | 1.01 (0.98, 1.03) |
| Sex (female) | 1.86 (1.25, 2.78) |
| Race/ethnicity (white, non-Hispanic vs. other) | 1.09 (0.68, 1.73) |
| Public assistance | 0.75 (0.37, 1.52) |
| Educational level | 1.40 (0.75, 2.58) |
| Military service | 0.77 (0.42, 1.42) |
| Household firearm ownership | 0.85 (0.53, 1.36) |
| Provider trust for firearm safety counseling | 9.63 (6.37, 14.56) |
| Received firearm safety counseling | 5.14 (3.02, 8.72) |
| Teen firearm safety training | 0.50 (0.31, 0.80) |
| aCommunity violence exposure | 0.89 (0.73, 1.09) |
| bRisky teen behavior | 1.06 (0.92, 1.23) |
Weighted N = 2535, Unweighted N = 2522.
Community violence— summary score (range 0–9) assessing past 12-months exposure (yes/no) to violence in their community.
Risky teen behavior— summary score (range 0–11) assessing past 12-months caregiver reports of teen engagement in any of 11 risky behaviors (e. g., unsafe driving; smoking/vaping; physical fights; risky sexual behaviors).
5. Discussion
Despite being the leading cause of death for high-school age teens (Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2022), we found that among U.S. caregivers of teens, firearm safety remained the least discussed preventative health issue during routine teen healthcare visits, with less than 15% of caregivers indicating they received counseling by their teen’s HCP in the prior five-years. As 94.8% of household firearms are owned by parents and or their spouse/partner in this population, the extent to which caregivers receive firearm safety counseling from their teen’s HCP is an important component of firearm injury prevention Further, while rates of counseling reported by caregivers in our sample are similar to those observed in other studies of caregivers (Garbutt et al., 2016; Haught et al., 1995), they are lower than those reported by HCPs (Damari et al., 2018; Butkus and Weissman, 2014; Finch et al., 2008; Olson et al., 2007), likely reflecting that HCPs may overestimate the frequency of delivering counseling or that counseling discussions they are having are not resonating effectively with caregivers (Ha and Longnecker, 2010). Regardless, findings highlight that few HCPs currently screen or counsel about firearm safety. This is particularly concerning considering the elevated risk for firearm injury that currently exists for U.S. teens (Garbutt et al., 2016; Haught et al., 1995; Forbis et al., 2007; Fuzzell et al., 2018). Low HCP screening/counseling rates may reflect a lack of HCP confidence in their role or ability to counsel on firearm safety (Olson et al., 2007; Ha and Longnecker, 2010; Walters et al., 2012; Roszko et al., 2016; Price et al., 2013), uncertainty that their counseling is efficacious (Price et al., 2013), clinical time constraints (Olson et al., 2007; Roszko et al., 2016; Barkin et al., 1999), political concerns (Walters et al., 2012), and/or concern about the effect of counseling on the provider-caregiver relationship (Garbutt et al., 2016; Olson et al., 2007; Walters et al., 2012). Our finding that over half of caregivers of teens report having firearm(s) in their home is higher than previous studies (Azrael et al., 2018), potentially reflecting increases in firearm ownership since the onset of COVID (Miller et al., 2022), that families with teens have higher household firearm ownership (Schuster et al., 2000), and/or our examination of household firearm ownership rather than individual respondent ownership (Azrael et al., 2000; Coyne-Beasley et al., 2005). Regardless, elevated rates of ownership combined with prior data that 21% of firearm owning households with children keep at least one firearm unlocked and unloaded (Azrael et al., 2018), and that firearm access is the most significant risk factor for teen firearm injuries, suggest a need to increase caregiver screening and safety counseling during routine teen health visits. This is particularly salient given that researchers reported lower rates of pediatric injury and death within households practicing locked storage (Grossman et al., 2005). Behavioral counseling can be efficacious at increasing locked storage, especially when employing a non-judgmental, structured motivational interviewing approach paired with providing safety devices (Rowhani-Rahbar et al., 2016; Carter et al., 2016; Grossman et al., 2005; Barkin et al., 2008; Carbone et al., 2005; Grossman et al., 2012) Considering 92% of adolescents attended a well-child check-up in 2019 (National Center for Health Statistics, 2019), future research should focus on understanding and addressing barriers to HCP firearm screening/counseling.
Among caregivers receiving counseling, our data indicate most conversations were limited to screening for household firearm ownership and/or discussing storage practices, regardless of household firearm ownership. While such conversation elements are critical, a broader focus on firearm safety is also warranted. Given that parents, relatives, friends, or parents of a friend are the source for firearms used in 69% of unintentional firearm injuries/deaths (Grossman et al., 1999), 82% of fatal suicides (Grossman et al., 1999; Johnson et al., 2010), and 74% of school shootings (National Threat Assessment Center, 2019), such conversations would benefit from including a focus on both on- and off-property firearm access, particularly regarding households their teen frequently visits (e.g., grandparents). Further, data on best-practice counseling methods (Carter et al., 2016; Resnicow and McMaster, 2012; Prochaska and Velicer, 1997) emphasizes that providing a menu of harm reduction measures allows patients increased autonomy over their actions and is more effective at evoking behavior change. Thus, in addition to identifying optimal storage practices (e.g., unloaded and locked using locking device and/or firearm safe), expanding discussions to include a range of safety approaches such as making firearms less lethal (e.g., removing firing pin from weapons not currently in use; replacing current firearm with smart firearms) and/or decreasing unsupervised teen access (e.g., storing firearms in an offsite location during high-risk time periods; technology-enhanced firearm safes) may enhance counseling efficacy (Carter et al., 2022). Given that more in-depth counseling approaches are routinely employed for other teen health issues (e.g., safer sex; alcohol/drug use) (Walton et al., 2017; Chin et al., 2012; Cunningham et al., 2015b), our findings may reflect a lack of technical knowledge about firearms and available safety options, especially given that no families used provided safety devices and few instituted safety changes in response to counseling provided in the current context. Taken together, such data highlights that in addition to addressing barriers to routine counseling as a component of their practice, there is a need to provide clinicians training on counseling approaches and technical aspects of firearm safety that will enhance their counseling competency (Marino et al., 2018; Betz and Wintemute, 2015).
While improving counseling competency is essential, it is also important to note that only a quarter of caregivers indicated they were receptive to safety counseling by their teen’s HCP. Rates of receptivity in our nationally representative sample were lower than those observed in several other studies (Garbutt et al., 2016; Haught et al., 1995; Forbis et al., 2007), likely reflecting variability in the populations sampled. Prior studies have been mostly conducted among convenience samples of caregivers/parents from pediatric offices as compared to a broad nationally representative sample. Alternatively, this finding may reflect our focus on caregiver receptivity towards the HCP providing firearm counseling to their teen as opposed to direct counseling of caregivers. Future studies should delineate whether caregiver receptivity towards counseling is dependent on their inclusion within the counseling discussion Further, we found the most salient factor associated with increased receptivity was caregiver trust, indicating that counseling may need to unfold over multiple encounters that address caregiver readiness-to-change and willingness to engage in safety discussions. Regardless, it is vital that such conversations emphasize a patient-centered approach, with non-judgmental, non-confrontational, apolitical discussions about safety/harm reduction (Betz et al., 2018) that respect caregiver values about firearm ownership and safety. Fundamental to increasing trust is to normalize firearm safety conversations in ways that are analogous to discussions about other risk behaviors (e.g., teen drinking and driving). This includes universal firearm safety screening/counseling for all families, not only those owning firearms, as caregivers who received counseling in this sample were more likely to be receptive to counseling and indicated more trust in HCPs to counseling on firearm safety. Further, our findings parallel research on the importance of trust for counseling of caregivers exhibiting vaccine hesitancy, with data demonstrating that building sufficient trust is linked to employing approaches that respect underlying caregiver values, address caregiver concerns, and demonstrate the HCP’s knowledge and competence on complex health issues (Benin et al., 2006; Connors et al., 2017). Given prior data indicating that time constraints may limit physicians from having effective conversations (Olson et al., 2007; Roszko et al., 2016; Barkin et al., 1999), it is important to consider how trusted non-physician team members (e.g., social workers, nurses) may be utilized to provide counseling. Alternatively, as technology-assisted brief interventions are efficacious for reducing other risk behaviors (e. g., underage drinking, prescription drug/marijuana use) (Roszko et al., 2016; Cunningham et al., 2015b; Waller et al., 2019), there may be a role for developing technology focused firearm counseling modules. Regardless, our data highlight the importance of considering ways to enhance trust in the provider-patient relationship when considering best-practices for firearm safety counseling.
We also found that receptivity towards counseling was lower among caregivers that provided their teen with firearm safety training, either themselves or through established programs (e.g., hunter-safety training). This is consistent with data demonstrating that firearm owners believe safety training is their personal responsibility (Jager-Hyman et al., 2019; Aitken et al., 2020) and that law enforcement, hunting/outdoor sporting groups, and active-duty military personnel are more effective safety messengers than physicians (Crifasi et al., 2018). Given such programs and individualized training varies widely (Rowhani-Rahbar et al., 2018; Berrigan et al., 2019; Hemenway et al., 2019) with prior data emphasizing that many skills-based programs lack efficacy for reducing firearm handling/access (Rowhani-Rahbar et al., 2018; Berrigan et al., 2019), it is important that HCPs understand the elements of a teen’s prior firearm training and continue to counsel caregivers about limiting unsupervised teen firearm access, especially during high-risk time periods. Yet, given low receptivity to HCP-focused counseling efforts overall, such data also suggests there may be a role for HCPs to work with local trusted community partners to provide critical elements of safety counseling, and/or promote the validity of safety messages provided as part of their practice (Betz and Wintemute, 2015; Aitken et al., 2020; Crifasi et al., 2018). Future research exploring HCP safety counseling that integrates external partnerships with more trusted messengers, such as law enforcement, and enhanced by incorporating caregiver input/feedback on messaging, may be an avenue for addressing the lack of trust for HCP-delivered counseling and ensuring the safety information delivered is more acceptable to caregivers.
Consistent with data demonstrating that women are more likely to seek preventative healthcare for themselves (Thompson et al., 2016; Hughes and Wingard, 2008), as well as for their children (Blumberg et al., 2004; Thakkar et al., 2019), female caregivers were twice as receptive to safety counseling as male caregivers. Despite this, female caregivers personally owning firearms are also more likely than their male counterparts to store at least one firearm loaded and unlocked, citing the need to protect their family (Azrael et al., 2018; Wolfson et al., 2020). Further, among married heterosexual partners, over 80% of men and women report that firearm storage is the husband’s responsibility (Coyne-Beasley et al., 2005). Taken together, such data indicates that important gender differences exist and HCP counseling may need to integrate tailored approaches reflecting caregiver roles regarding firearm ownership, motives, counseling beliefs, and safety practices. Future studies may also examine whether fathers/mothers counsel their children differently based on gender.
Study limitations should be considered. First, while self-report measures raise the potential for social desirability and/or recall bias, prior research indicates that this approach retains high reliability/validity when privacy/confidentiality are assured, as was done in this case (Grossman et al., 2000; Webster et al., 1992; Betz et al., 2020; Buchan et al., 2002; Brener et al., 2003; Turner et al., 1998; Wright and Supple, 1998). Further, online survey delivery generates more accurate results and reduces social desirability bias compared to traditional telephone surveys (Kreuter et al., 2008; Chang, 2009); and online selection bias was decreased as participants without email access were mailed surveys to their selected address. Second, while the potential exists for missing data to bias results, we observed that fewer than 1% of the sample did not answer questions regarding firearm ownership and/or attitudes towards HCP counseling, increasing the likelihood that population estimates are valid/accurate. Third, because the sample is representative by U.S. region we are not able to examine such factors of rurality or urbanicity on our outcome variable. Future studies will need to be developed to specifically examine differences in receptivity by rurality/urbanicity. Finally, the cross-sectional nature of our survey study limits the ability for causal attributions.
6. Conclusions
While firearms are currently the leading cause of death for U.S. high-school age teens, less than 15% of caregivers indicate they received firearm safety counseling from their teen’s HCP during the prior five years. Further, only a quarter of caregivers indicate they are receptive to such counseling measures, driven largely by a lack of trust in their teen’s HCP to counsel on firearm safety. Future research is needed to understand the best methods for increasing HCP competency to provide effective firearm safety counseling within their current practice, including partnerships with trusted community partners. Also establishing counseling methods that enhance provider-patient trust and lead to increased uptake of firearm safety practices may help decrease the substantial rates of firearm death and injury currently occurring among adolescent populations.
Acknowledgements
The authors wish to acknowledge project staff, including Lynn Massey LMSW and Carrie Musolf for their assistance in data and manuscript preparation.
Funding sources/disclosures
This research study was funded by NIH/NICHD 5R24HD08714903; and Dr. Seewald’s time was funded by NIH/NICHD T32HD108054, NIH/NICHD 5R24HD08714903 and CDC 5R49CE003085-02. Findings and conclusions are those of the authors and do not necessarily represent the official position of the funding agencies. No honoraria, grants or other form of payment were received for producing this manuscript.
Abbreviations:
- HCP
Healthcare provider
Appendix A. Survey Item for Dependent Variable of Interest (Firearm Safety Counseling Receptivity)
Please share the extent to which you agree with the following statement:
“It is important for health care providers to discuss gun safety with teens.”
Select only one.
[]Strongly agree []Agree []Neither agree nor disagree []Disagree [] Strongly disagree.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Prior presentations
Society for Academic Emergency Medicine (SAEM) 2020.
Previous submissions
Our manuscript has been submitted solely to Preventative Medicine and is not published, in press, or submitted elsewhere.
Credit author statement
Author contributions: LS, MZ, RC, and PC were responsible for study concept/design; LS, MM, MZ, RC, LR, and PC were responsible for data acquisition; LS, MM, MZ, MW, RC, LR, MH, and PC provided analysis and data interpretation; All authors assisted in drafting the manuscript/providing critical revisions of the manuscript.
Data availability
Data will be made available on request.
References
- Aitken ME, Minster SD, Mullins SH, Hirsch HM, Unni P, Monroe K, et al. , 2020. Parents’ perspectives on safe storage of firearms. J. Community Health 45 (3), 469–477. [DOI] [PubMed] [Google Scholar]
- Azrael D, Miller M, Hemenway D, 2000. Are household firearms stored safely? It depends on whom you ask. Pediatrics 106 (3), E31. [DOI] [PubMed] [Google Scholar]
- Azrael D, Cohen J, Salhi C, Miller M, 2018. Firearm storage in gun-owning households with children: results of a 2015 National Survey. J. Urban Health 95 (3), 295–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkin S, Ryan G, Gelberg L, 1999. What pediatricians can do to further youth violence prevention—a qualitative study. Inj Prev. 5 (1), 53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkin SL, Finch SA, Ip EH, Scheindlin B, Craig JA, Steffes J, et al. , 2008. Is office-based counseling about media use, timeouts, and firearm storage effective? Results from a cluster-randomized, controlled trial. Pediatrics. 122 (1), e15–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES, 2006. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 117 (5), 1532–1541. [DOI] [PubMed] [Google Scholar]
- Berrigan J, Azrael D, Hemenway D, Miller M, 2019. Firearms training and storage practices among US gun owners: a nationally representative study. Inj Prev 25 (Suppl. 1) (i31–i8). [DOI] [PubMed] [Google Scholar]
- Betz ME, Wintemute GJ, 2015. Physician Counseling on firearm safety: a new kind of cultural competence. JAMA. 314 (5), 449–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz ME, McCourt AD, Vernick JS, Ranney ML, Maust DT, Wintemute GJ, 2018. Firearms and dementia: clinical considerations. Ann. Intern. Med. 169, 47–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz ME, Azrael D, Johnson RL, Knoepke CE, Ranney ML, Wintemute GJ, et al. , 2020. Views on firearm safety among caregivers of people with Alzheimer disease and related dementias. JAMA Netw. Open 3 (7), e207756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumberg SJ, Halfon N, Olson LM, 2004. The National Survey of early childhood health. Pediatrics. 113 (6 Suppl), 1899–1906. [PubMed] [Google Scholar]
- Brener ND, Billy JO, Grady WR, 2003. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J. Adolesc. Health 33 (6), 436–457. [DOI] [PubMed] [Google Scholar]
- Buchan BJ, Tims FM, Diamond GS, 2002. Cannabis use: consistency and validity of self-report, on-site urine testing and laboratory testing. Addiction. 97 (Suppl. 1), 98–108. [DOI] [PubMed] [Google Scholar]
- Butkus R, Weissman A, 2014. Internists’ attitudes toward prevention of firearm injury. Ann. Intern. Med. 160 (12), 821–827. [DOI] [PubMed] [Google Scholar]
- Carbone PS, Clemens CJ, Ball TM, 2005. Effectiveness of gun-safety counseling and a gun lock giveaway in a Hispanic community. Archives of pediatrics & adolescent medicine. 159 (11), 1049–1054. [DOI] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Roehler DR, Goldstick J, Zimmerman MA, Blow FC, et al. , 2015. Firearm violence among high-risk emergency department youth after an assault injury. Pediatrics. 135 (5), 805–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Zimmerman MA, Chermack ST, Roche JS, Cunningham RM, 2016. Efficacy of a universal brief intervention for violence among urban emergency department youth. Acad. Emerg. Med. 23 (9), 1061–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Goldstick J, Epstein-Ngo QM, Zimmerman MA, Mercado MC, et al. , 2017. Violent firearm-related conflicts among high-risk youth: an event-level and daily calendar analysis. Prev. Med. 102, 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter P, Losman E, Roche J, Malani P, Kullgren J, Solway E, Kirch M, Singer D, Walton M, Zeoli A, Cunningham R, 2022. Firearm ownership, attitudes, and safe storage practices among a nationally representative sample of older U.S. adults age 50 to 80. Prev. Med. 156, 106955. [DOI] [PubMed] [Google Scholar]
- Carter PM, Mouch CA, Goldstick JE, Walton MA, Zimmerman MA, Resnicow K, et al. , 2020. Rates and correlates of risky firearm behaviors among adolescents and young adults treated in an urban emergency department. Prev. Med. 130, 105891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Health Statistics, 2020. Underlying Cause of Death 1999–2019 on CDC WONDER Online Database. Accessed September 23, 2022. http://wonder.cdc.gov/ucd-icd10.html.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2022. Web-based Injury Statistics Query and Reporting System (WISQARS). US Centers for Disease Control and Prevention Data 2006–2019. Accessed September 23, 2022. www.cdc.gov/ncipc/wisqars. [Google Scholar]
- Chang LKJ, 2009. National surveys via RDD telephone interviewing versus the internet: comparing sample representativeness and response quality. Public Opinion Quarterly. 73 (4), 641–678. [Google Scholar]
- Chin HB, Sipe TA, Elder R, Mercer SL, Chattopadhyay SK, Jacob V, et al. , 2012. The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: two systematic reviews for the guide to community preventive services. Am. J. Prev. Med. 42 (3), 272–294. [DOI] [PubMed] [Google Scholar]
- Cleveland EC, Azrael D, Simonetti JA, Miller M, 2017. Firearm ownership among American veterans: findings from the 2015 National Firearm Survey. Inj Epidemiol. 4 (1), 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner A, Azrael D, Miller M, 2021. Firearm safety discussions between clinicians and U.S. adults living in households with firearms: results from a 2019 National Survey. Ann. Intern. Med. 174 (5), 725–728. [DOI] [PubMed] [Google Scholar]
- Connors JT, Slotwinski KL, Hodges EA, 2017. Provider-parent communication when discussing vaccines: a systematic review. J. Pediatr. Nurs. 33, 10–15. [DOI] [PubMed] [Google Scholar]
- Coyne-Beasley T, Baccaglini L, Johnson RM, Webster B, Wiebe DJ, 2005. Do partners with children know about firearms in their home? Evidence of a gender gap and implications for practitioners. Pediatrics. 115 (6), e662–e667. [DOI] [PubMed] [Google Scholar]
- Crifasi CK, Doucette ML, McGinty EE, Webster DW, Barry CL, 2018. Storage practices of US gun owners in 2016. Am. J. Public Health 108 (4), 532–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Carter PM, Ranney M, Zimmerman MA, Blow FC, Booth BM, et al. , 2015a. Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study. JAMA Pediatr. 169 (1), 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Chermack ST, Ehrlich PF, Carter PM, Booth BM, Blow FC, et al. , 2015b. Alcohol interventions among underage drinkers in the ED: a randomized controlled trial. Pediatrics. 136 (4), e783–e793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Walton MA, Carter PM, 2018. The major causes of death in children and adolescents in the United States. N. Engl. J. Med. 379 (25), 2468–2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Carter PM, Ranney ML, Walton M, Zeoli AM, Alpern ER, et al. , 2019. Prevention of firearm injuries among children and adolescents: consensus-driven research agenda from the firearm safety among children and teens (FACTS) consortium. JAMA Pediatr. 173 (8), 780–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damari ND, Ahluwalia KS, Viera AJ, Goldstein AO, 2018. Continuing medical education and firearm violence Counseling. AMA J. Ethics 20 (1), 56–68. [DOI] [PubMed] [Google Scholar]
- DiScala C, Sege R, 2004. Outcomes in children and young adults who are hospitalized for firearms-related injuries. Pediatrics. 113 (5), 1306–1312. [DOI] [PubMed] [Google Scholar]
- Farcy DA, Doria N, Moreno-Walton L, Gordon H, Sanchez J, Cubeddu LX, et al. , 2021. Emergency physician survey on firearm injury prevention: where can we improve? West. J. Emerg. Med. 22 (2), 257–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch SA, Weiley V, Ip EH, Barkin S, 2008. Impact of pediatricians’ perceived self- efficacy and confidence on violence prevention counseling: a national study. Matern. Child Health J. 12 (1), 75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbis SG, McAllister TR, Monk SM, Schlorman CA, Stolfi A, Pascoe JM, 2007. Children and firearms in the home: a southwestern Ohio ambulatory research network (SOAR-net) study. J. Am. Board Fam. Med. 20 (4), 385–391. [DOI] [PubMed] [Google Scholar]
- Fuzzell LN, LaJoie AS, Smith KT, Philpott SE, Jones KM, Politi MC, 2018. Parents’ adherence to pediatric health and safety guidelines: importance of patient-provider relationships. Patient Educ. Couns. 101 (9), 1570–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbarino J, Bradshaw CP, Vorrasi JA, 2002. Mitigating the effects of gun violence on children and youth. Futur. Child. 12 (2), 72–85. [PubMed] [Google Scholar]
- Garbutt JM, Bobenhouse N, Dodd S, Sterkel R, Strunk RC, 2016. What are parents willing to discuss with their Pediatrician about firearm safety? A Parental Survey. J Pediatr. 179, 166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick JE, Carter PM, Walton MA, Dahlberg LL, Sumner SA, Zimmerman MA, et al. , 2017. Development of the SaFETy score: a clinical screening tool for predicting future firearm violence risk. Ann. Intern. Med. 166 (10), 707–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman DC, Reay DT, Baker SA, 1999. Self-inflicted and unintentional firearm injuries among children and adolescents: the source of the firearm. Arch Pediatr Adolesc Med. 153 (8), 875–878. [DOI] [PubMed] [Google Scholar]
- Grossman DC, Cummings P, Koepsell TD, Marshall J, D’Ambrosio L, Thompson RS, et al. , 2000. Firearm safety counseling in primary care pediatrics: a randomized, controlled trial. Pediatrics. 106 (1 Pt 1), 22–26. [DOI] [PubMed] [Google Scholar]
- Grossman DC, Mueller BA, Riedy C, Dowd MD, Villaveces A, Prodzinski J, et al. , 2005. Gun storage practices and risk of youth suicide and unintentional firearm injuries. JAMA. 293 (6), 707–714. [DOI] [PubMed] [Google Scholar]
- Grossman DC, Stafford HA, Koepsell TD, Hill R, Retzer KD, Jones W, 2012. Improving firearm storage in Alaska native villages: a randomized trial of household gun cabinets. Am. J. Public Health 102 (S2) (S291–S7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha JF, Longnecker N, 2010. Doctor-patient communication: a review. Ochsner J. 10 (1), 38–43. [PMC free article] [PubMed] [Google Scholar]
- Hagan JF, Shaw JS, Duncan PM (Eds.), 2017. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, 4th ed. Elk Grove Village, IL, American Academy of Pediatrics. [Google Scholar]
- Hall MA, Camacho F, Dugan E, Balkrishnan R, 2002. Trust in the medical profession: conceptual and measurement issues. Health Serv. Res. 37 (5), 1419–1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haught K, Grossman D, Connell F, 1995. Parents’ attitudes toward firearm injury prevention counseling in urban pediatric clinics. Pediatrics. 96 (4 Pt 1), 649–653. [PubMed] [Google Scholar]
- Hemenway D, Rausher S, Violano P, Raybould TA, Barber CW, 2019. Firearms training: what is actually taught? Inj Prev. 25 (2), 123–128. [DOI] [PubMed] [Google Scholar]
- Hughes SC, Wingard DL, 2008. Parental beliefs and children’s receipt of preventive care: another piece of the puzzle? Health Serv. Res 43 (1 Pt 1), 287–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jager-Hyman S, Benjamin Wolk C, Ahmedani BK, Zeber JE, Fein JA, Brown GK, et al. , 2019. Perspectives from firearm stakeholders on firearm safety promotion in pediatric primary care as a suicide prevention strategy: a qualitative study. J. Behav. Med. 42 (4), 691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong HL, WC., 2016. The level of collapse we are allowed: comparison of different response scales in safety attitudes questionnaire. Biom biostat. Int. J 4 (4), 128–134. [Google Scholar]
- Jessor R, 1987. Problem-behavior theory, psychosocial development, and adolescent problem drinking. Br. J. Addict. 82 (4), 331–342. [DOI] [PubMed] [Google Scholar]
- Johnson RM, Miller M, Vriniotis M, Azrael D, Hemenway D, 2006. Are household firearms stored less safely in homes with adolescents?: analysis of a national random sample of parents. Arch Pediatr Adolesc Med. 160 (8), 788–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RM, Barber C, Azrael D, Clark DE, Hemenway D, 2010. Who are the owners of firearms used in adolescent suicides? Suicide Life Threat Behav. 40 (6), 609–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juang DD, McDonald DL, Johnson-Young EA, Burrell TD, Silver DL, Wang Y, et al. , 2019. Assessment of Pediatric Residents’ attitudes toward anticipatory Counseling on gun safety. Children (Basel). 6 (11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter F, Pressor S, Tourangeau R, 2008. Social desirability bias in CATI, IVR and web surveys: the effects of mode and question sensitivity. Public Opinion Quarterly. 72 (5), 847–865. [Google Scholar]
- Marino E, Wolsko C, Keys S, Wilcox H, 2018. Addressing the cultural challenges of firearm restriction in suicide prevention: a test of public health messaging to protect those at risk. Arch Suicide Res. 22 (3), 394–404. [DOI] [PubMed] [Google Scholar]
- McLean RM, Harris P, Cullen J, Maier RV, Yasuda KE, Schwartz BJ, et al. , 2019. Firearm-related injury and death in the United States: a call to action from the Nation’s leading physician and public health professional organizations. Ann. Intern. Med. 171 (8), 573–577. [DOI] [PubMed] [Google Scholar]
- Miller M, Hemenway D, Azrael D, 2007. State-level homicide victimization rates in the US in relation to survey measures of household firearm ownership, 2001–2003. Soc. Sci. Med. 64 (3), 656–664. [DOI] [PubMed] [Google Scholar]
- Miller M, Zhang W, Azrael D, 2022. Firearm purchasing during the COVID-19 pandemic: results from the 2021 National Firearms Survey. Ann. Intern. Med. 175 (2), 219–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monuteaux MC, Azrael D, Miller M, 2019. Association of Increased Safe Household Firearm Storage with Firearm Suicide and Unintentional Death among US youths. JAMA Pediatr. 173 (7), 657–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics, 2019. Percentage of having a well child check-up in the past 12 months for children under age 18 years, United States. National Health Interview Survey. Accessed September 23, 2022. https://wwwn.cdc.gov/NHISDataQueryTool/SHS_2019_CHILD3/index.html. [Google Scholar]
- Olson LM, Christoffel KK, O’Connor KG, 2007. Pediatricians’ involvement in gun injury prevention. Inj Prev. 13 (2), 99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallin R, Spitzer SA, Ranney ML, Betz ME, Wintemute GJ, 2019. Preventing firearm-related death and injury. Ann. Intern. Med. 170 (11), ITC81–ITC96. [DOI] [PubMed] [Google Scholar]
- Peek-Asa C, Butcher B, Cavanaugh JE, 2017. Cost of hospitalization for firearm injuries by firearm type, intent, and payer in the United States. Inj Epidemiol. 4 (1), 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price JH, Thompson A, Khubchandani J, Wiblishauser M, Dowling J, Teeple K, 2013. Perceived roles of emergency department physicians regarding anticipatory guidance on firearm safety. J Emerg Med. 44 (5), 1007–1016. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, 1997. The transtheoretical model of health behavior change. Am. J. Health Promot. 12 (1), 38–48. [DOI] [PubMed] [Google Scholar]
- Resnicow K, McMaster F, 2012. Motivational interviewing: moving from why to how with autonomy support. Int. J. Behav. Nutr. Phys. Act. 9, 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richters JE, Martinez P, 1990. Things I Have Seen and Heard: A Structured Interview for Assessing Young children’s Violence Exposure. National Institute of Mental Health, Rockville, MD. [Google Scholar]
- Roszko PJ, Ameli J, Carter PM, Cunningham RM, Ranney ML, 2016. Clinician attitudes, screening practices, and interventions to reduce firearm-related injury. Epidemiol. Rev. 38 (1), 87–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowhani-Rahbar A, Zatzick D, Wang J, Mills BM, Simonetti JA, Fan MD, et al. , 2015. Firearm-related hospitalization and risk for subsequent violent injury, death, or crime perpetration: a cohort study. Ann. Intern. Med. 162 (7), 492–500. [DOI] [PubMed] [Google Scholar]
- Rowhani-Rahbar A, Simonetti JA, Rivara FP, 2016. Effectiveness of interventions to promote safe firearm storage. Epidemiol. Rev. 38 (1), 111–124. [DOI] [PubMed] [Google Scholar]
- Rowhani-Rahbar A, Lyons VH, Simonetti JA, Azrael D, Miller M, 2018. Formal firearm training among adults in the USA: results of a national survey. Inj Prev. 24 (2), 161–165. [DOI] [PubMed] [Google Scholar]
- Runyan CW, Becker A, Brandspigel S, Barber C, Trudeau A, Novins D, 2016. Lethal means Counseling for parents of youth seeking emergency Care for Suicidality. West. J. Emerg. Med. 17 (1), 8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt CJ, Rupp L, Pizarro JM, Lee DB, Branas CC, Zimmerman MA, 2019. Risk and protective factors related to youth firearm violence: a scoping review and directions for future research. J. Behav. Med. 42 (4), 706–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnitzer PG, Dykstra HK, Trigylidas TE, Lichenstein R, 2019. Firearm suicide among youth in the United States, 2004–2015. J. Behav. Med. 42 (4), 584–590. [DOI] [PubMed] [Google Scholar]
- Schuster MA, Franke TM, Bastian AM, Sor S, Halfon N, 2000. Firearm storage patterns in US homes with children. Am. J. Public Health 90 (4), 588–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Threat Assessment Center, 2019. Protecting America’s Schools: A U.S. Secret Service Analysis of Targeted School Violence. U.S. Secret Service, Department of Homeland Security, pp. 1–68. [Google Scholar]
- Sieving RE, McRee AL, Mehus C, Gewirtz O’Brien JR, Wang S, Brar P, et al. , 2021. Sexual and reproductive health discussions during preventive visits. Pediatrics. 148 (2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol RL, Marineau L, Zimmerman MA, Rupp LA, Cunningham RM, Carter PM, 2021a. Why some parents made firearms more accessible during the beginning of the COVID-19 pandemic: results from a national study. J. Behav. Med. 44 (6), 867–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol RL, Zimmerman MA, Rupp L, Heinze JE, Cunningham RM, Carter PM, 2021b. Firearm purchasing during the beginning of the COVID-19 pandemic in households with teens: a national study. J. Behav. Med. 44 (6), 874–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JS, Madhavan S, Han RW, Chandler JM, Tenakoon L, Chao S, 2021. Financial burden of pediatric firearm-related injury admissions in the United States. PLoS One 16 (6), e0252821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakkar MY, Hao L, Marcell AV, 2019. Adolescents’ and Young Adults’ routine care use: the role of their Mothers’ Care use Behaviors. J. Adolesc. Health 64 (1), 107–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson AE, Anisimowicz Y, Miedema B, Hogg W, Wodchis WP, Aubrey-Bassler K, 2016. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam. Pract. 17, 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL, 1998. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 280 (5365), 867–873. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau, 2020. American Community Survey: 2016 Data Release, 31. Accessed September 23, 2022. www.census.gov/programs-surveys/acs/news/data-releases/2016.html.
- United States Census Bureau, 2022. Current Population Survey, 2017 data release. Accessed September 23.
- Waller R, Bonar EE, Fernandez AC, Walton MA, Chermack ST, Cunningham RM, et al. , 2019. Exploring the components of an efficacious computer brief intervention for reducing marijuana use among adults in the emergency department. J. Subst. Abus. Treat. 99, 67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters H, Kulkarni M, Forman J, Roeder K, Travis J, Valenstein M, 2012. Feasibility and acceptability of interventions to delay gun access in VA mental health settings. Gen. Hosp. Psychiatry 34 (6), 692–698. [DOI] [PubMed] [Google Scholar]
- Walton MA, Ngo QM, Chermack ST, Blow FC, Ehrlich PF, Bonar EE, et al. , 2017. Understanding mechanisms of change for brief alcohol interventions among youth: examination of within-session interactions. J Stud Alcohol Drugs. 78 (5), 725–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster DW, Wilson ME, Duggan AK, Pakula LC, 1992. Parents’ beliefs about preventing gun injuries to children. Pediatrics. 89 (5 Pt 1), 908–914. [PubMed] [Google Scholar]
- Wolfson JA, Azrael D, Miller M, 2020. Gun ownership among US women. Inj Prev. 26 (1), 49–54. [DOI] [PubMed] [Google Scholar]
- Wright DLAW, Supple AJ, 1998. A comparison of computer-assisted and paper-and-pencil self-administered questionnaires in a survey on smoking, alcohol, and drug use. Public Opinion Quarterly. 62 (3), 331–353. [Google Scholar]
- Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, Carli V, Höschl C, Barzilay R, Balazs J, Purebl G, Kahn JP, Sáiz PA, Lipsicas CB, Bobes J, Cozman D, Hegerl U, Zohar J, 2016. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry 3 (7), 646–659. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.


