Abstract
Objectives:
Noise induced hearing loss (NIHL) remains one of the most prevalent occupational diseases. Occupational hearing conservation programs (HCPs) can reduce the risk of NIHL, but there remains no consensus on assessing HCP effectiveness. We conducted a multi-site, mixed-method assessment of HCP programs.
Methods:
At thirteen manufacturing plants, we performed assessments, including interviews with program staff and worker focus groups and surveys. We analyzed the association between these assessments and age-corrected NIHL rates.
Results:
Only a few items from the HCP staff interviews correlated with NIHL rates. For the employee survey, management commitment to NIHL prevention and being counseled about NIHL were strongly associated with NIHL rates.
Conclusion:
Management commitment and counseling of workers about NIHL may be key factors in program effectiveness. A combination of qualitative and quantitative methods appears to be useful for assessing HCPs.
Keywords: hearing conservation, occupational hearing loss, program evaluation
BACKGROUND
Occupational noise induced hearing loss (NIHL) was first described as a condition by Ramazzini in his classic 18th century treatise De Morbis Artificum Diatriba (Diseases of workers) [1]. Over the course of history it has been noted in many industries and occupational groups including boilermakers [2], civil war veterans [3], weavers [4] and farmers [5]. During the late 20th century, hearing conservation programs (HCPs) were introduced in many workplace settings, often under regulations such as the 1983 OSHA Hearing Conservation Amendment [6], which mandated HCPs in worksites where exposures met or exceeded OSHA’s Action Level of 85 dBA on an 8-hour Time Weighted Average (TWA). Under the OSHA regulation, an HCP includes five key elements: assessment and control of noise exposure; training of workers in the importance of protecting their hearing; provision of hearing protection devices at no cost to the worker; performance of annual audiometric surveillance of noise exposed workers; and record keeping.
Despite the existence of such programs, NIHL remains one of the most prevalent occupational conditions in the US [7] and other industrialized countries, and constitutes an even greater burden of adult hearing loss in developing countries [8]. A possible explanation for the continued excess loss of hearing among noise-exposed workers is that many workplaces, especially in less formal but noisy occupational settings such as construction, entertainment, and farming, may not have formal HCPs. Another explanation is that even when a worksite has an HCP, that program may not be sufficiently effective in preventing hearing loss.
In 2006, the National Academy of Sciences recommended devoting greater research attention to the challenge of determining the effectiveness of HCPs [9]. Despite the fact that analysis of a number of individual programs has shown benefits from hearing conservation efforts [10, 11] a number of recent systematic reviews have noted the paucity of rigorous evidence regarding the impact of preventive programs on hearing loss risk [12, 13]. At the same time, anecdotal reports of successful hearing conservation efforts in particular settings continue to appear in the literature [10]. Given the considerable expense and effort now devoted to hearing conservation in many industries, it is important to continue to develop improved methods to assess the effectiveness of such programs [14]. At present, there remains no consensus regarding the assessment of program effectiveness or the components or activities of a program that are most responsible for improving effectiveness. While several decades ago a proposed draft national standard for hearing conservation effectiveness, based on methods for audiometric database analysis (ADBA) and focused in large part on the year-to-year variability of sequential audiograms, was considered by the American National Standards Institute (ANSI), it was never formally adopted, due in part to concerns about both feasibility and reliability [15]. Even if it had been adopted, the proposed method would have addressed only one lagging indicator of HCP effectiveness (i.e., trends in audiometric testing results). To the best of our knowledge, no comprehensive methodology for assessing HCP effectiveness is currently under formal consideration as a standard.
In the absence of agreed-upon methods of assessing program quality and effectiveness, managers of HCPs may rely on program audit checklists such as that developed by the National Institute for Occupational Safety and Health (NIOSH) [16]. They can also compare their program elements with the requirements of regulations such as those of the Occupational Safety and Health Administration (OSHA) to determine whether the program is in regulatory compliance. Additional ways to assess programs include tracking the annual occurrence of hearing loss indicators such as standard threshold shifts (a change from baseline of at least 10dB in the average of hearing thresholds at 2,3, and 4000 Hz) [13] or assessing changes in noise levels over time [17, 18]. Use of lagging rather than leading indicators of hearing loss to measure program effectiveness, however, is far from ideal, since by the time a standard threshold shift has occurred, affected workers already exhibit significant degrees of hearing loss [19]. Similarly, assessment of noise exposures alone does not consider health impacts of exposure. For this reason, other approaches have been proposed, such as looking at the rate of audiometric “early flags” for hearing loss (earlier changes in an audiogram prior to development of an STS) [20] or using worker focus groups (facilitated group sessions with employees to qualitatively explore attitudes regarding hearing conservation) to assess program component quality [21].
To explore the relative value of different components of an HCP in preventing hearing loss, we conducted site visits at a number of industrial facilities, gathered information about their HCPs from management and workers, and compared the assessment of program components with the actual rates of hearing loss occurring in each facility.
METHODS
Site selection and recruitment
The study took place at multiple, geographically dispersed plant locations of a large metal manufacturing company in the United States. The company, at the time of the study, had approximately 40 plant locations in the US. Plant selection criteria included having workers enrolled in an HCP and availability of noise measurement and audiometric data for at least five years prior to the site visit. The study team contacted all company facilities meeting these criteria (N-15) and requested permission to perform site visit assessments. Fourteen plants agreed to site visits. Three of the facilities were engaged in primary metal production, while the others were engaged in some form of metal fabrication. We used one site as a pilot site to pilot test the assessment tools. Management at each site was informed that the information about the site and their HCP would be kept confidential, not be released to the company or other facilities in an identifiable manner, and that no individual-identifying information would be collected. Following site visits, the study team provided site management with a consultation report based on the site assessment and analysis of location specific audiometric and noise exposure data. The study team also requested feedback to correct any items noted in the report as an additional quality control step. Complete site visit data was available for 13 of the 14 plants. One plant participated only in the management survey and noise-sampling aspects of the site visit (without worker survey or focus groups); therefore, we excluded this plant from further analysis.
Site visits
The study team performed site visits of 2 – 3 days’ duration between 2012 and 2015. Assessments included plant walkthroughs, administration of a standardized in person interview to HCP managers and medical providers, a short written survey of workers (self-administered during meetings and work breaks), personal dosimetry measurements of noise levels, and worker focus groups. All study procedures were pilot-tested at a single company site, which is not included in the analysis presented here. The study protocols were reviewed and approved by the Yale University School of Medicine Human Investigation Committee (Protocol # 0509000588) to assure protection of the rights of research subjects.
The management survey was adapted from the NIOSH Hearing Conservation Program checklist on the NIOSH website [16], and consisted of over 100 items encompassing program components including general program administration, worker training, noise assessment and control, hearing protection devices, audiometric testing, and record keeping. Also included were questions about the costs of program administration; these data will be described in detail elsewhere (manuscript in preparation). This survey was constructed with input from experts in HCPs, and pretested with plant managers and health and safety professionals in the study company prior to being finalized. The survey is included as an appendix (see supplementary materials). Responses to surveys were entered into the Research Electronic Data Capture (REDCaP) platform [22] for further analysis.
The anonymous employee survey consisted of eight questions that employees could answer in approximately one minute. These questions covered worker perception of risk and management commitment to preventing hearing loss. As an incentive to complete the survey, workers received a raffle ticket for gift cards. The study team distributed surveys directly to the workers during meetings, meal breaks, and other worker gatherings, and collected them immediately after completion. The goal during each site visit was to have at as many of the workers in the HCP as possible complete the survey, although actual worker completion percentages varied between facilities. The worker survey is included as an appendix (see supplementary materials).
Focus groups, led by members of the research team, were conducted in groups of 4–12 volunteers, and lasted between 15 and 40 minutes. Participants received a cash incentive ($20 USD). Company management was not permitted to be present during the focus groups. During a typical site visit 8–10 focus groups were conducted, and in each facility, the number of groups conducted was more than sufficient to reach theme saturation [23]. Audio recordings of each group were transcribed and the transcripts reviewed to identify salient themes. These data were entered into ATLAS-ti (version 7.5.6) for further analysis. With input from the plant health and safety manager during each site visit, full-shift personal noise dosimetry (DoseBadge®, Cirrus Research, North Yorkshire, UK) was performed on a representative sample of workers during plant visits, with a focus on high noise areas and areas that were in the opinion of the local health and safety management a noise control priority. Sampling measurements took place across day, night, and swing shifts. The number of dosimetry measurements varied between plants based on the size of the noise-exposed workforce. All dosimeters were configured to the OSHA hearing conservation requirements [6], and were calibrated pre- and post-measurement. Results were compared to the OSHA action level of 85 dBA TWA. We calculated the average noise levels for each facility as the average of results from the onsite dosimetry performed during study site assessment visits.
Calculation of Hearing loss rates for study locations
Under a longstanding research agreement between the company and the study team, company data sets including audiometric surveillance data were available for analysis. Details of the research agreement have been described previously [19]. For each facility, we calculated the average annual rate of high frequency hearing loss, defined as the annual rate of change in the binaural average of hearing thresholds for individuals at the noise-sensitive frequencies of 3, 4, and 6 kHz, for all individuals in the location who had at least three audiograms over a five year or greater time period over the previous 10 years. We corrected these values for age using ANSI standard S3.44 [24]. For each facility, we also calculated the annual rate of standard threshold shifts (age-adjusted 10dB change from baseline in the average of hearing thresholds at 2, 3, and 4 kHz) for the previous ten years, using age correction tables from the OSHA Hearing Conservation Standard [6]. We then calculated annual average test-test variability for the previous ten years as well; this metric was based on previously published audiometric database analysis (ABDA) methods [25]. The test-test variability statistic involved comparing sequential audiometric tests for individuals at each facility and determining the annual percentage of audiometric tests in that facility showing either sequential improvement or worsening of hearing thresholds of 15 dB or more in any of the frequencies from 1–6000 Hz.
Statistical Analysis for predictors of hearing loss
Since the data for this study are naturally nested, with multiple workers associated with each facility, multilevel regression models were used to assess the independent association between hearing loss and both the worker and facility characteristics. (Table 4). This strategy separates within-facility variation from between-facility variation and models the assumption that underlying differences in the quality of the hearing conservation program lead to systematic differences among facility hearing loss rates. We performed this modeling using the Generalized Linear Mixed Model (GLIMMIX) procedure in SAS statistical software V.9.4 (SAS Institute, Cary NC). The model used as the outcome each individual’s annual rate of change in the binaural average of hearing thresholds for 3, 4, and 6 kHz over the previous 10-year period (see above). We included in the model, as individual-level fixed effects, worker age, race/ethnicity, sex, baseline hearing threshold level and presence of tinnitus. Categorical responses to the management survey items as well as grouped response rates (by facility) to each of the employee survey items - dichotomized at the 50th percentile for participating plants - were examined as plant-level fixed effects in models adjusted for the individual level fixed effects. Separate preliminary models, adjusted only for the fixed effects of age, race/ethnicity and gender, examined contribution of other individual level and plant level variables, Items were retained for inclusion in the fully adjusted model if statistical significance of 0.1 or less was reached in the preliminary models. Average noise exposure levels, STS rates, and audiogram test-test variability were also examined as plant-level fixed effects in preliminary models adjusted for age, gender, and race/ethnicity. We retained variables for inclusion in the fully adjusted model if their statistical significance reached 0.1 or less. To account for unmeasured between-site variation, we included “plant” as a random effect in the fully adjusted model.
Table 4.
Predictors of high frequency hearing loss
| Variable | Preliminary Models each Adjusted for Age, Gender, Race* | Fully Adjusted Multilevel Model (only significant variables included)** | ||
|---|---|---|---|---|
| estimate | P-value | estimate | p-value | |
| Employee Variables | ||||
| Age | 0.016 | <.0001 | 0.018 | <.0001 |
| Male (vs female) | 0.174 | <.0001 | 0.183 | <.0001 |
| Race/Ethnicity | ||||
| Black (vs white) | −0.196 | <.0001 | −0.202 | <.0001 |
| Hispanic (vs white) | −0.087 | 0.0133 | −0.089 | 0.009 |
| Tinnitus | 0.197 | <.0001 | 0.216 | <.0001 |
| Tinnitus unknown | −0.083 | 0.0008 | −0.083 | 0.001 |
| Baseline hearing (mean 3,4,6KHz) | −0.002 | 0.0058 | −0.003 | <.0001 |
| Location level Variables | ||||
| Employee survey responses | ||||
| When you had your most recent hearing test, did anyone talk to you about your hearing? (% yes >=85%) | −0.142 | 0.0361 | −0.191 | <.0001 |
| Workplace level of commitment to hearing loss prevention (high or exceptional >=70% ) | −0.124 | 0.0944 | −0.119 | 0.001 |
| Manager survey responses | ||||
| Annual audiograms conducted before work shift (vs during/after work shift) | −0.363 | 0.0027 | −0.300 | 0.003 |
| Hearing protection devices required when noise levels exceed 85dBA (vs >90 or other criteria) | −0.174 | 0.0110 | ||
| Noise monitoring conducted using both personal and area measurements (compared to personal measurements only) | −0.181 | 0.0747 | −0.158 | 0.025 |
| Work-relatedness of hearing loss determined by Professional supervisor (Physician or Audiologist) vs other professional | −0.145 | 0.0903 | ||
| Have any workers complained that HPDs interfere with their ability to do their jobs at your facility (yes vs no) | 0.153 | 0.0244 | 0.094 | 0.006 |
Separate models each adjusted for age, gender, and race/ethnicity
Items were retained for inclusion in the full multilevel model if statistical significance of 0.1 or less was reached in the preliminary analysis adjusting for age, gender, and race/ethnicity.
RESULTS
Plant and Worker Characteristics
Table 1 shows the demographics of the workers enrolled in hearing conservation programs at the study facilities and overall plant characteristics. The participating facilities had an average of about 600 workers, but ranged substantially in size, from 165 to 1,425 workers. The number of personal noise dosimetry measurements per site ranged from 28 to 44 (total N=513), and the average noise exposure across the 13 participating plants was 83.1 dBA (standard deviation across sites 3.1 dBA, range 78.5 – 87.5). At the plant level, between 18 and 75% of dosimetry measurements exceeded the OSHA Action Level of 85 dBA TWA. Overall, 168 (32.7%) of the 513 individual dosimetry measurements exceeded 85 dBA. The test-test variability statistic for a plant location (i.e. how many periodic audiograms showed significant improvements or worsening of 15dB or more at one or more frequencies between sequential tests) ranged between 31.3 and 44.5% (mean=37.0). This represented the average over the previous 10-year period. The mean annual age corrected raw STS rate (regardless of work relatedness determination) was 3.5± 2.0%. Hearing conservation program cost averaged nearly $300 per worker.
Table 1.
Plant and Worker Characteristics
| Characteristic | Mean/n | SD/% |
|---|---|---|
| Plant characteristics (n=13) | ||
| No. of workers - mean, SD | 617.5 | 445.4 |
| Noise levels - mean, SD (dBA) | 83.1 | 3.0 |
| Test-test variability statistic- mean, SD (%) | 37.0 | 3.6 |
| Annual overall STS rate – mean, SD | 3.5 | 2.0 |
| Annual cost of HCP ($USD/worker) - mean, SD | $294 | $62 |
| Employee characteristic (n=8,028) | ||
| Age - mean, SD | 42.8 | 9.6 |
| Gender - n,% | ||
| Male | 6589 | 82.1 |
| Female | 1439 | 17.9 |
| Race/Ethnicity - n,% | ||
| White | 6080 | 75.7 |
| Black | 916 | 11.4 |
| Hispanic | 813 | 10.1 |
| Other | 219 | 2.7 |
| Hearing at baseline (binaural average of hearing thresholds at 3,4,6KHz) - mean, SD | 21.7 | 16.4 |
| Annualized hearing loss rate in average 3,4,6KHz (dB/yr) – mean, SD | 0.61 | 0.78 |
The average age of workers in the HCP at the participating sites was approximately 43 years at time of entry into our study cohort (age at their first audiometric test included in our study). Workers in our study cohort were predominantly white, and had a hearing threshold of approximately 22 dB HL at the binaural average of 3, 4, and 6 kHz for the first audiometric test included in the study. Slightly more than 18% of workers reported tinnitus at some point during the follow up period (data not shown).
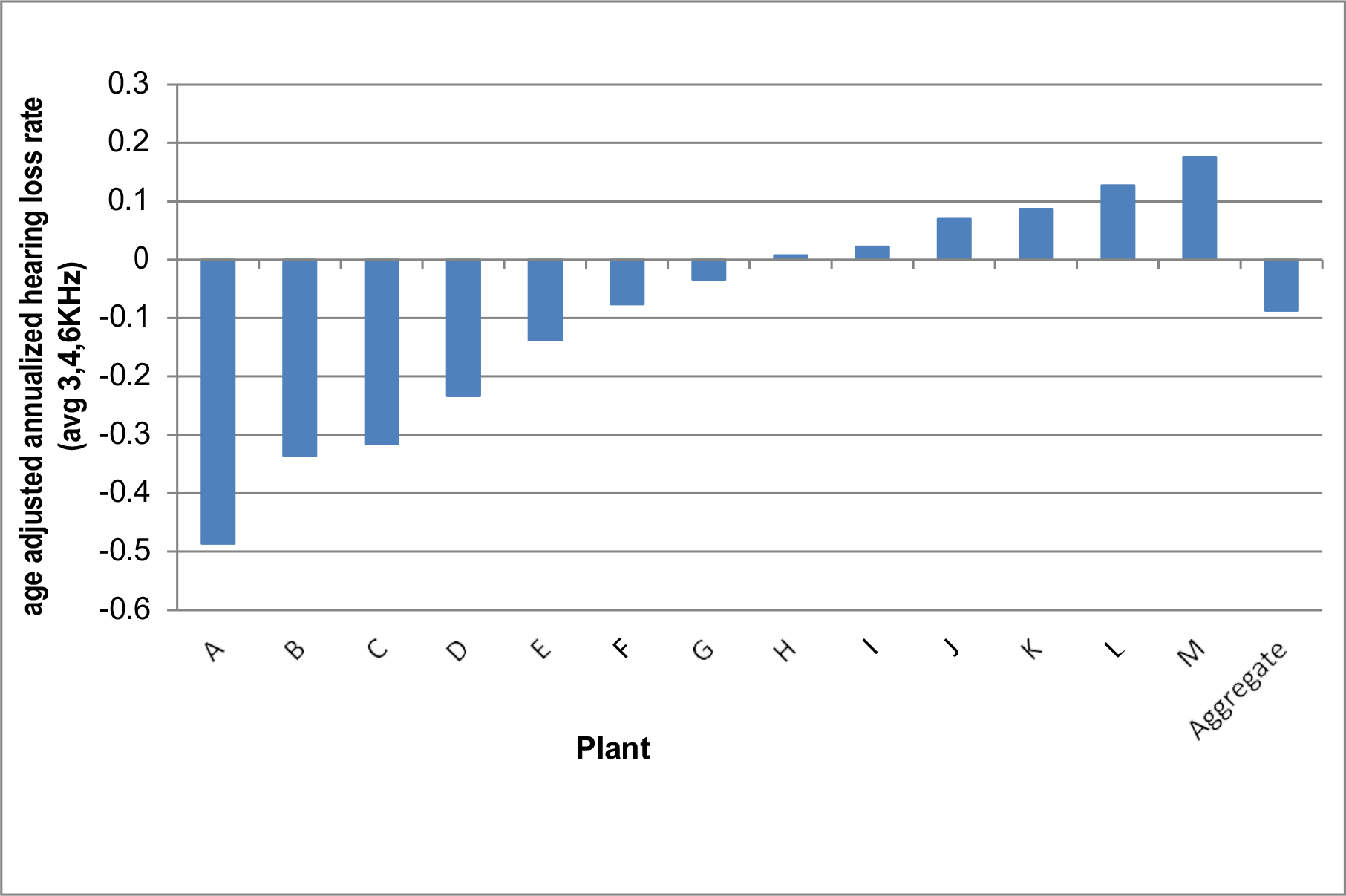
Figure 1 shows average rates of hearing loss, in dB per year for the average of hearing thresholds at 3, 4, and 6 kHz, for workers enrolled in HCPs in each of these facilities. Negative numbers for the corrected rate implies that in general, individuals at the plant were losing less hearing than predicted by age by the ANSI 3.44 formula.
Figure 1. Age Adjusted Annualized Hearing Loss Rates by Plant - Average 3,4,6KHz (2005–2014).
Management and employee surveys
Table 2 shows the distribution of responses to manager survey items retained for inclusion in the fully adjusted model. These included questions about timing of hearing testing, type of noise sampling performed, whether a professional supervisor (physician or audiologist) determined work relatedness, requiring hearing protection for full-shift exposures >85 dBA, and whether workers were complaining about work interference by hearing protectors. Notably, for many questions on the manager survey, including some of the items shown in Table 2, the plant managers answered in the same way, demonstrating little response variability between plants. Table 3 shows the results of responses to the employee survey, averaged across all facilities, as well as the range of response rates across plants. Overall, more than 80 percent of workers reported that during the annual hearing test process, they received counseling about their hearing. This percentage ranged between 56% and 92% for different locations. Similarly, while 68% of workers overall rated management commitment to hearing loss prevention as “High or exceptional”, the rates varied from a low of 45% to a high of 87% percent. More than 50% of employees expressed high or extreme concern about hearing loss, while over 40% also expressed concern about the potential for accidents related to noise or the use of hearing protection. Less than 50% of workers reported “never” removing their hearing protectors to communicate during a work shift.
Table 2.
Responses to selected items in Manager Survey
| Survey Item | Yes | No | ||
|---|---|---|---|---|
| n | % | n | % | |
| Annual audiograms conducted before workshift (vs during/after) | 1 | 7.7 | 12 | 92.3 |
| Hearing protection devices required when noise levels exceed 85 dBA (vs >90 or other criteria) | 7 | 53.8 | 6 | 46.2 |
| Noise monitoring conducted using personal measurements only (versus both personal and area measurements) | 2 | 15.4 | 11 | 84.6 |
| Work-relatedness of hearing loss determined by Professional supervisor (Physician or Audiologist) vs other professional | 9 | 69.2 | 4 | 30.8 |
| Have any workers complained that HPDs interfere with their ability to do their jobs at your facility | 8 | 61.5 | 5 | 61.5 |
Table 3.
Employee Survey: percentage of employees in each facility with certain responses_
| Question | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| When you had your most recent hearing test, did anyone talk to you about your hearing? (% answering “yes”) | 82.5 | 9.3 | 56.0 | 92.0 |
| When you had your most recent hearing test, did anyone talk to you about how to best use your hearing protective device? (% answering “yes”) | 74.9 | 10.3 | 55.0 | 92.0 |
| What percentage of time does your supervisor wear his/her hearing protective device while on the floor? (% answering “76–100%”) | 82.9 | 17.1 | 39.0 | 96.0 |
| In areas where hearing protection is required, how often do other workers wear their hearing protective devices? (% answering “always”) | 68.8 | 15.7 | 43.0 | 87.0 |
| How would you rate the level of management commitment to preventing hearing loss at your workplace? (% answering “high or exceptional”) | 68.7 | 10.3 | 45.0 | 87.0 |
| How much of a personal concern do you have about losing your hearing because of on the job noise exposure? (% answering “high or extreme”) | 54.8 | 8.4 | 41.0 | 75.0 |
| How much of a personal concern do you have about injuries or accidents occurring because of noise, hearing loss or wearing hearing protective devices? (% answering “high or extreme”) | 43.7 | 5.2 | 35.0 | 53.0 |
| On average, how many times during each work day do you have to remove your hearing protective device in order to communicate? (% answering “never”) | 45.7 | 11.2 | 29.0 | 64.0 |
Focus groups
Across the 13 plants participating in all study components, we conducted 126 focus groups, with a range of 6 to 14 groups per site for a total of 767 participants. Major themes included the perceived level of management commitment to hearing conservation; the extent to which a variety of HPDs were available and accessible; and whether or not workers were encouraged to take hearing protectors home for use when exposed to non-occupational sources of noise. In the majority of plants visited. Focus group participants described a high level of management commitment to the HCP and high levels of personal commitment to protecting hearing on the job. In contrast, in less than half of the study sites did focus group participants report a strong personal investment in protecting hearing off the job.
Predictors of hearing loss
Table 4 shows the variables achieving statistical significance of p=.10 or less in preliminary analyses (adjusted for age, race/ethnicity and gender) that were retained in the fully adjusted models as well as the results of the fully adjusted models of individual and plant level predictors s for high frequency hearing loss among employees at the study facilities.
Significant individual-level factors predictive of hearing loss in the fully adjusted model included age, sex, race, ethnicity, tinnitus, and baseline hearing (with worse baseline hearing associated with lower risk of further hearing loss). Plants for which at least 85% of employees surveyed reported receiving counseling during their annual hearing test experienced less hearing loss, and plants for which at least 70% of workers reported the highest levels of workplace commitment to preventing hearing loss showed lower rates of hearing loss among workers. Each of these variables retained significance in the fully-adjusted model. Manager survey items remaining in the fully-adjusted, final multilevel model included: the timing of annual audiograms; whether noise sampling included personal sampling vs. personal and area sampling; and whether or not workers complained about HPDs interfering with work. Plants that conducted annual audiometric testing during or after work shifts compared to before work shifts showed higher rates of hearing loss. Plants for which noise-monitoring efforts included both personal and area sampling showed lower rates of hearing loss. Finally, plants in which managers had received worker complaints that HPDs interfered with their ability to perform their jobs had higher rates of hearing loss. Neither measures of test-test audiogram variability mean plant noise levels, nor hearing conservation program size (number of persons in HCP), or annual per capita expenditures on the hearing conservation program were significant plant level predictors of hearing loss after adjusting for age, gender, and race/ethnicity.
DISCUSSION
The results of this field study, which gathered a large amount of data about HCP components at 13 separate plants within a single company, reveal the challenges of assessing hearing conservation program effectiveness. The manager interview that we administered in the different locations, which was based on publicly available checklists for assessing hearing conservation programs, showed limited variation in some responses between study locations. While certain factors such as timing of hearing testing, frequency of training, and the existence of certain policies showed weak or borderline associations with plant hearing loss rates in partially adjusted models, none of the manager survey elements retained significance in a multivariate, multilevel model that included information from the worker survey. This suggests that the use of HCP manager surveys to assess hearing conservation program effectiveness, a common method currently, may provide less insight into the actual effectiveness of the program than other data sources such as surveys of employees. Specifically, we found that asking workers about whether they were counseled during their hearing test, and the perceived management commitment to hearing loss prevention, provided useful information about the effectiveness of the program. Other location characteristics, including dollars spent per worker on the hearing conservation program, noise levels, and audiometric test-test variability, were not associated with hearing loss risk.
The study had a number of strengths, including the number of facilities assessed and the in-depth nature and mixed methods approach to data collection at each location. Study limitations include the retrospective nature of the outcome data, and the fact that all study locations were part of a single company with a company-wide hearing conservation policy. Inclusion of more diverse companies in our sample may have produced greater variation in program components or manager survey assessments.
Our finding of limited variability in responses between plants to many of the questions in the manager interview could have a number of explanations. One possible explanation is that all the plants visited were part of a single company with a set of corporate procedures regarding hearing conservation, although we recognize that each facility’s hearing conservation program was locally administered, and there was variation in the scope and emphasis among programs. This is reflected in the significant differences (SD>20%) in the amount of spending on hearing conservation among the different plants. Moreover, although the plants followed corporate procedures regarding hearing conservation, there was significant variation in how these procedures were implemented as evidenced by differences across plants in the level of management commitment to hearing loss prevention as perceived by workers. Another possibility is that there could have been a tendency for managers to recognize the “correct” answer to a question and be more likely to agree with the desired response. A third possibility is that managers were simply not that familiar with specific components and activities of their HCPs. Finally, a fourth possibility is that variations in the intensity, frequency, or quality of hearing conservation activities varied by plant, but that our manager survey did not capture these variations. Since the program manager may not be the person actually carrying out certain HCP activities such as training, he or she may be unaware how effective such activities are in a particular plant. The frequency of training, for example, may not reflect the quality of the training activities.
Despite this limited variability, some items in the manager survey were associated with hearing loss rates. Testing workers before rather than during work shifts was associated with lower rates of audiometric loss. This could be an artifact of testing, since testing during a work shift can help detect temporary hearing threshold shifts. The plants that sampled more comprehensively for noise (both area and personal measurements) experienced less hearing loss than those sampling only workers, suggesting that attention to noise exposure and control could be playing a role. Plants where managers reported employees were complaining about interference by hearing protective devices had on average higher rates of hearing loss, suggesting that hearing protection might be less effective in such locations.
The employee survey finding that plants where high percentages of workers reported someone talked to them about their hearing during annual audiometric testing demonstrated lower hearing loss rates suggests that such counseling could have a beneficial impact on worker protective behavior. Behavior changes to prevent hearing loss could include more effective use of hearing protection, and avoiding noise exposures both at work and away from work. While our study did not assess such linkages, other studies have reported a beneficial effect of worker counseling about hearing protection use [26].
Another plant-level factor showing a significant association with hearing conservation effectiveness in the multivariate model – perceived management commitment to hearing conservation – suggests that the safety climate and culture in a facility can impact the effectiveness of hearing loss prevention programs. This is consistent with a growing body of evidence regarding the importance of safety culture in implementing prevention activities in the workplace [27].
Our finding that increased management commitment to hearing loss prevention predicts] [28–32] decreased hearing loss is consistent with the substantial literature showing that management commitment to safety positively affects safety outcomes [1, 2, 3, 4]. Further, in a study of wood manufacturing employees, it was found that management commitment to safety was positively related to non-safety related employee outcomes [5]. These were job satisfaction, organizational commitment, and withdrawal, which includes behaviors such as absenteeism, and daydreaming. Employees attitude in response to their perceptions of how much management values them, and management commitment to safety and hearing loss prevention is an aspect of that valuing, has been termed perceived organizational response [6].
The results of our onsite noise measurements showed that even in a company with a long-standing commitment to hearing conservation, noise overexposures are common; for example, one-third of measurements exceeded the OSHA Action Level for noise overall, but at several plants between half and two-thirds of measurements exceeded this level. At the same time, manager survey reports regarding the intensity of noise control efforts did not correlate with hearing loss rates in a facility. In addition, measured noise levels at a location were not predictive of hearing loss. Previous studies have reported a lack of a linear relationship between ambient noise levels and hearing loss risk [33], and may relate to individual differences in hearing protection use. While the importance of noise control seems inherently obvious [34], further documentation of the effectiveness of noise control efforts is needed.
Hearing protective devices were in routine use in the facilities we visited, and the uniformity of company policies made it difficult to assess the impact of such policies. At the same time, many employees reported removing hearing protectors during a work shift to communicate, suggesting opportunities for greater effectiveness of such devices. Previous studies have found that reported compliance with hearing protective devices [35] and policies enforcing hearing protector use [36] was predictive of hearing loss. The locations in our study did not routinely track such compliance, and policies for hearing protection use were similar across the facilities, preventing effective comparisons of this factor. The worker survey question regarding how often they removed hearing protectors during a work shift did not show a significant correlation with hearing loss rates.
The overall message from these results is the importance of worker input into program evaluation, as well as the importance of worker counseling and management commitment to occupational health and prevention. A combination of qualitative and quantitative assessments, such as we performed, is likely to contribute to the assessment of program quality and effectiveness.
Supplementary Material
Clinical Significance:
Despite widespread implementation of hearing conservation programs in noisy workplaces, there remains no agreed-upon method to evaluate the effectiveness of such programs. We report on an in-depth evaluation of hearing conservation programs that provides novel guidance for program effectiveness assessment, including worker surveys to assess
Funding source:
NIOSH 5 R01 OH 010132-04 REV
The study was supported by a grant from the National Institute for Occupational Safety and Health (NIOSH) (5 RO1 OH010132).
Footnotes
COI: None declared
Contributor Information
Peter Rabinowitz, Department of Environmental and Occupational Health Sciences, University of Washington, 1959 NE Pacific Street, Box 357234, Seattle, WA 98195-7234, USA.
Linda F Cantley, Yale Occupational and Environmental Medicine Program, Yale University School of Medicine, New Haven, CT, USA.
Deron Galusha, Yale Occupational and Environmental Medicine Program, Yale University School of Medicine, New Haven, CT, USA.
Sally Trufan, Department of Environmental and Occupational Health Sciences, University of Washington, Seattle, WA, USA.
Arthur Swersey, Yale School of Management, Yale University, New Haven, CT, USA
Christine Dixon-Ernst, Otogienex, LLC, Pittsburgh, PA, USA.
Vickie Ramirez, Department of Environmental and Occupational Health Sciences, University of Washington, Seattle, WA, USA.
Richard Neitzel, Department of Environmental Health Sciences, University of Michigan, Ann Arbor, MI, USA.
REFERENCES
- 1.Ramazzini B, De Morbis Artificum Diatriba [Diseases of Workers]. American Journal of Public Health, 1713. 91(9): p. 1380–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atherley G and Noble W, Occupational deafness: the continuing challenge of early German and Scottish research. American Journal of Industrial Medicine, 1985. 8: p. 101–117. [DOI] [PubMed] [Google Scholar]
- 3.Sewell RK, et al. , Hearing loss in Union Army veterans from 1862 to 1920. Laryngoscope, 2004. 114(12): p. 2147–2153. [DOI] [PubMed] [Google Scholar]
- 4.Taylor W, et al. , Study of Noise and Hearting in Jute Weaving. Journal of the Acoustical Society of America, 1965. 38: p. 268–273. [DOI] [PubMed] [Google Scholar]
- 5.Thelin JW, et al. , High-frequency hearing loss in male farmers of Missouri. Public Health Reports, 1983. 98: p. 268–273. [PMC free article] [PubMed] [Google Scholar]
- 6.Occupational Safety & Health Administration (OSHA), CFR Occupational Noise Exposure: Hearing Conservation Amendment (Final Rule), in 1910.95. 1983. [Google Scholar]
- 7.Masterson EA, et al. , Hearing Impairment Among Noise-Exposed Workers - United States, 2003–2012, in MMWR Morbidity and Mortality Weekly Report. 2016. p. 389–94. [DOI] [PubMed] [Google Scholar]
- 8.Nelson DI, et al. , The global burden of occupational noise-induced hearing loss. Am J Ind Med, 2005. 48(6): p. 446–58. [DOI] [PubMed] [Google Scholar]
- 9.Institute of Medicine: Hearing Loss Research at NIOSH. Reviews of Research Programs of the National Institute for Occupational Safety and Health. 2006. [cited 2016 9/6/16]; Available from: https://www.nap.edu/read/11721/chapter/1
- 10.Donoghue AM, et al. , Hearing conservation in the primary aluminium industry. Occup Med (Lond)., 2016. 66(3 ): p. 208–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hager WL, Hoyle ER, and Hermann ER, Efficacy of enforcement in an industrial hearing conservation program. Am Ind Hyg Assoc J 1982. 43: p. 455–465 [DOI] [PubMed] [Google Scholar]
- 12.Verbeek JH, et al. , Interventions to prevent occupational noise-induced hearing loss: a Cochrane systematic review. Int J Audiol., 2014. 53(Suppl 2): p. S84–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daniell WE, et al. , Noise exposure and hearing loss prevention programmes after 20 years of regulations in the United States. Occup Environ Med, 2006. 63(5): p. 343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morata TC and Meinke D, Uncovering effective strategies for hearing loss prevention Acoust Aust, 2016. 44(1): p. 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adera T, et al. , Should the audiometric database analysis method (draft ANSI S12.13–1991) for evaluating the effectiveness of hearing conservation programs be accepted as a US national standard?. J Am Acad Audiol. 1995. 6(4 ): p. 302–10. [PubMed] [Google Scholar]
- 16.NIOSH. Noise and Hearing Loss Prevention 8/4/16]; Available from: http://www.cdc.gov/niosh/topics/noise/hearingchecklist.html.
- 17.Daniell WE, Stover BD, and Takaro TK, Comparison of criteria for significant threshold shift in workplace hearing conservation programs. Journal of Occupational and Environmental Medicine, 2003. 45(3): p. 295–304. [DOI] [PubMed] [Google Scholar]
- 18.Neitzel RL, et al. , Methods for evaluating temporal trends in noise exposure. Int J Audiol, 2014. 53 Suppl 2: p. S76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McTague MF, et al. , Impact of daily noise exposure monitoring on occupational noise exposures in manufacturing workers. Int J Audiol, 2013. 52 Suppl 1: p. S3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rabinowitz PM, et al. , Audiometric “early flags” for occupational hearing loss. J Occup Environ Med, 2007. 49(12): p. 1310–6. [DOI] [PubMed] [Google Scholar]
- 21.Prince MM, et al. , The Contribution of Focus Groups in the Evaluation of Hearing Conservation Program (HCP) Effectiveness. Journal of Safety Research, 2004. 35: p. 91–106. [DOI] [PubMed] [Google Scholar]
- 22.Vanderbilt University, REDCap: Research Electronic Data Capture. 2004.
- 23.Fusch PI and Ness LR, Are We There Yet? Data Saturation in Qualitative Research. The Qualitative Report, 2015. 20(9): p. 1408–1416. [Google Scholar]
- 24.ANSI, American National Standard S3.44–1996 (R 2006): Determination of Occupational Noise Exposure and Estimation of Noise-Induced Hearing Impairment. Acoustical Society of America. 1996, New York, NY. [Google Scholar]
- 25.Royster JD and Royster LH, Using audiometric data base analysis J Occup Med Toxicol, 1986. 28 (10): p. 1055–68. [DOI] [PubMed] [Google Scholar]
- 26.Smith PS, Monaco BA, and Lusk SL, Attitudes toward use of hearing protection devices and effects of an intervention on fit-testing results. Workplace Health Saf, 2014. 62(12): p. 491–9. [DOI] [PubMed] [Google Scholar]
- 27.Cook JM, et al. , Evaluation of safety climate and employee injury rates in healthcare. Occup Environ Med, 2016. 73(9): p. 595–9. [DOI] [PubMed] [Google Scholar]
- 28.O’Toole MO, The relationship between employees’ perceptions of safety and organizational culture. Journal of Safety Research, 2002. 33: p. 231–243. [DOI] [PubMed] [Google Scholar]
- 29.Thompson RC, Hilton TF, and Witt LA, Where the Safety Rubber Meets the Shop Floor: A Confirmatory Model of Management Influence on Workplace Safety. Journal of Safety Research, 1998. 29(1): p. 15–24. [Google Scholar]
- 30.Michael JH, et al. , Management commitment to safety as organizational support: relationships with non-safety outcomes in wood manufacturing employees. J Safety Res, 2005. 36(2): p. 171–9. [DOI] [PubMed] [Google Scholar]
- 31.Rhoades L and Eisenberger R, Perceived organizational support: A review of the literature. Journal of Applied Psychology, 2002. 87(4): p. 698–714. [DOI] [PubMed] [Google Scholar]
- 32.Zohar D and Luria G, The use of supervisory practices as leverage to improve safety behavior: A cross-level intervention model. Journal of Safety Research, 2003. 34(5): p. 567–577. [DOI] [PubMed] [Google Scholar]
- 33.Rabinowitz PM, et al. , Do ambient noise exposure levels predict hearing loss in a modern industrial cohort? Occup Environ Med, 2007. 64(1): p. 53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kovalchik PG, et al. , Application of Prevention through Design for hearing loss in the mining industry. J Safety Res, 2008. 39(2): p. 251–4. [DOI] [PubMed] [Google Scholar]
- 35.Brink LL, et al. , Changes over time in audiometric thresholds in a group of automobile stamping and assembly workers with a hearing conservation program. AIHA J (Fairfax, Va), 2002. 63(4): p. 482–7. [DOI] [PubMed] [Google Scholar]
- 36.Heyer N, et al. , Use of historical data and a novel metric in the evaluation of the effectiveness of hearing conservation program components. Occup Environ Med,. 68(7): p. 510–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


