Abstract
Background:
Few brief, self-report measures exist that can reliably predict adverse suicidality outcomes in patients with BD. This study utilized the Concise Health Risk Tracking Self-Report (CHRT) to assess suicidality in patients with BD and examined its psychometric performance, clinical correlates, and prospective value in predicting adverse events related to suicidality.
Methods:
The CHRT was administered at baseline and follow-up to 482 adult patients in Bipolar CHOICE, a 6-month randomized comparative effectiveness trial. The Columbia Suicide Severity Rating Scale (CSSRS) was used at baseline to assess lifetime history of suicide attempts and related behaviors. Clinician-rated measures of mood (Bipolar Inventory of Symptoms Scale) and bipolar symptoms (Clinical Global Impressions-Bipolar Version) were conducted at baseline and follow-up.
Results:
The CHRT showed excellent internal consistency and construct validity and was highly correlated with clinician ratings of depression, anxiety, and overall functioning at baseline and throughout the study. Baseline CHRT scores significantly predicted risk of subsequent suicidality-related Serious Adverse Events (sSAEs), after controlling for mood and comorbidity. Specifically, the hazard of a sSAE increased by 76% for every 10-point increase in baseline CHRT score. Past history of suicide attempts and related behaviors, as assessed by the CSSRS, did not predict subsequent sSAEs.
Limitations:
The CSSRS was used to assess static risk factors in terms of past suicidal behaviors and may have been a more powerful predictor over longer-term follow-up.
Conclusions:
The CHRT offers a quick and robust self-report tool for assessing suicidal risk and has important implications for future research and clinical practice.
Keywords: Bipolar disorder, Suicide, Psychometrics, Self-report, Risk
1. Introduction
Bipolar disorder (BD) is associated with standardized mortality ratios between 1.6 and 2.1 (Osby et al., 2001), mostly due to high rates of suicide and cardiovascular disease (Roshanaei-Moghaddam and Katon, 2009). Patients with BD have about an eight-fold higher risk of suicide and a two-fold increased risk of death from chronic medical illnesses as compared to those in the general population (Cerimele et al., 2013). Major depressive episodes associated with BD are the most lethal phase of the disorder, associated with the majority of lifetime suicide attempts, which occur in 25% to 56% of patients, and deaths by suicide, which occur in 10% to 19% (Nierenberg et al., 2001). Thus, close monitoring of suicidality in BD is undoubtedly essential; however, this is limited by the lack of brief, reliable, self-report ratings of suicidal ideation and behavior.
Although there are clinician-rated measures that track suicidality in BD (e.g. the Columbia Suicide Severity Rating Scale (CSSRS); (Posner et al., 2011)), these measures require intensive training and have significant limitations since patients may not feel comfortable speaking directly to clinicians about suicidal thoughts. Given the sensitive nature of suicidal ideation and behavior, it is important to get the patients’ honest report of their current state. Self-report measures involve less in-person confrontation, and hence could provide more insight into suicidality and allow patients to disclose with more candor. Even the CSSRS, which is often viewed as the gold standard for assessing suicidality, has recently been formulated into an electronic, self-report version to reduce clinician burden and encourage patient self-disclosure (Mundt et al., 2013).
While self-report scales may offer significant advantages in assessing suicidal ideation, the value of positively predicting suicidal acts must also be considered. In a study of 191 patients with BD, suicidal ideation was assessed at baseline using the self-report Beck Depression Inventory – item 9 (BDI; Beck and Steer, 1990), and two clinician-rated measures: the Scale for Suicidal Ideation (SSI; Beck et al., 1979) and the Hamilton Depression Scale – item 3 (HAM-D; Hamilton, 1960). The predictive value of these different measures was investigated during a six-month follow-up, with a baseline SSI score ≥ 8 having the best combination of sensitivity and specificity and a positive predictive value of 32% for an attempted suicide during follow-up (Valtonen et al., 2009).
The Concise Health Risk Tracking Scale (CHRT) is a novel self-report measure initially developed to assess suicidality in patients with unipolar major depressive disorder (Trivedi et al., 2011). The measure includes questions about hopelessness, self-worth, pessimism about the future, perception of social support, and active suicidal plans. The items are scored on 5 point Likert scales, ranging from “Strongly Disagree” to “Strongly Agree.” Previous studies with unipolar major depressive disorder samples have demonstrated that the CHRT has excellent psychometric properties, with an internal consistency (Chronbach alpha) of 0.78 and a consistent factor structure with 3 independent factors (current suicidal thoughts and plans, perceived lack of social support, and hopelessness) (Trivedi et al., 2011). These three factors are consistent with the findings of Beck and colleagues, linking suicidal ideation/plans, perceived lack of social support, and hopelessness with eventual suicide (Beck et al., 1974, 1976, 1990; Brown et al., 2000). In developing the CHRT, Trivedi et al. (2011) found that suicidal thoughts and plans were more likely to be endorsed by patient self-report than by clinician assessment (they compared 2 versions of the CHRT: one clinician rated and one self-report by the patient), and clinicians compared to patients were less likely to use the more extreme rating (“strongly agree”). These results suggested the possibility that patients may be more willing to endorse suicidal ideation on self-report assessments or that some physicians may inadequately record suicidal ideation.
One previous study used the CHRT to evaluate suicidality in BD and found excellent initial support for its psychometric properties (Ostacher et al., 2015). This paper further explores the CHRT’s psychometric properties and clinical correlates in Bipolar CHOICE and it is the first paper to examine the prospective value of the CHRT in predicting adverse events related to suicidality in patients with BD.
2. Methods
2.1. Procedure
The Bipolar CHOICE (Clinical and Health Outcomes Initiative in Comparative Effectiveness) study (Nierenberg et al., 2014) was a six-month nationwide multi-site, randomized comparative effectiveness trial comparing lithium, a classic mood stabilizer, to quetiapine, a second generation antipsychotic approved by the Food and Drug Administration to treat BD. Study physicians were able to prescribe additional medications as needed (regardless of treatment assignment) as long as it was consistent with an established BD treatment guideline (Suppes et al., 2005) and personalized to the needs of the patient given their current symptoms and functioning (Asao et al., 2006). The rationale, design, and methods of the Bipolar CHOICE study are reported elsewhere (Nierenberg et al., 2014).
2.2. Participants
The Institutional Review Boards of the eleven study sites approved the study protocol. The Bipolar CHOICE study enrolled 482 individuals between the ages of 18 and 68 years, with 58.7% females. In terms of race, 72.2% were White, 19.9% were Black, 3.3% were Asian, and 4.6% were other. In terms of ethnicity, 11% were Hispanic or Latino. Limited inclusion and exclusion criteria were designed to maximize generalizability (Nierenberg et al., 2014), but participants were required to have a DSM-IV TR BPI or BPII diagnosis and to be at least mildly symptomatic (CGI-BP ≥ 3) at intake. All participants supplied written informed consent after receiving a full description of the study.
2.3. Assessments
DSM-IV TR diagnoses were determined by trained raters using the Extended Mini-International Neuropsychiatric Interview (MINI), an electronic version of a validated structured diagnostic interview (Sheehan et al., 1998). The MINI suicide module also assessed suicidal risk at baseline, classifying risk levels as none, low, moderate, and high. The Clinical Global Impressions-Bipolar Version (CGI-BP) assessed BP illness severity and comprised three separate severity scores, ranging from 1 to 7 (normal to very severely ill), for mania, depression, and overall bipolar illness (Spearing et al., 1997). Symptom severity was also measured with the clinician-administered Bipolar Inventory of Symptoms Scale (BISS) (Bowden et al., 2007; Gonzalez et al., 2008) from which a total score and depression, mania, anxiety, irritability, and psychosis domain scores were derived. Clinical interviews obtained demographic information, psychiatric/medical history, and current medications. Serious adverse events (SAEs) were systematically recorded during the study. The Clinical Events Committee, chaired by the Director of Training and Assessments (AuthorNR-H), classified each SAE as related or unrelated to suicidal behavior, while blind to randomization status. Suicidal ideation was assessed at baseline and at each follow-up visit using the Concise Health Risk Tracking Scale (CHRT) (Trivedi et al., 2011). A 14-item self-report version of the CHRT was used, which includes 2 items related to impulsivity. Fig. 1 displays the scale items, with the 7 items that comprise the short version listed in bold. The Columbia Suicide Severity Rating Scale (CSSRS) (Posner et al., 2011) was used by trained raters at baseline to assess a lifetime history of suicide attempts and related behaviors.
Fig. 1.
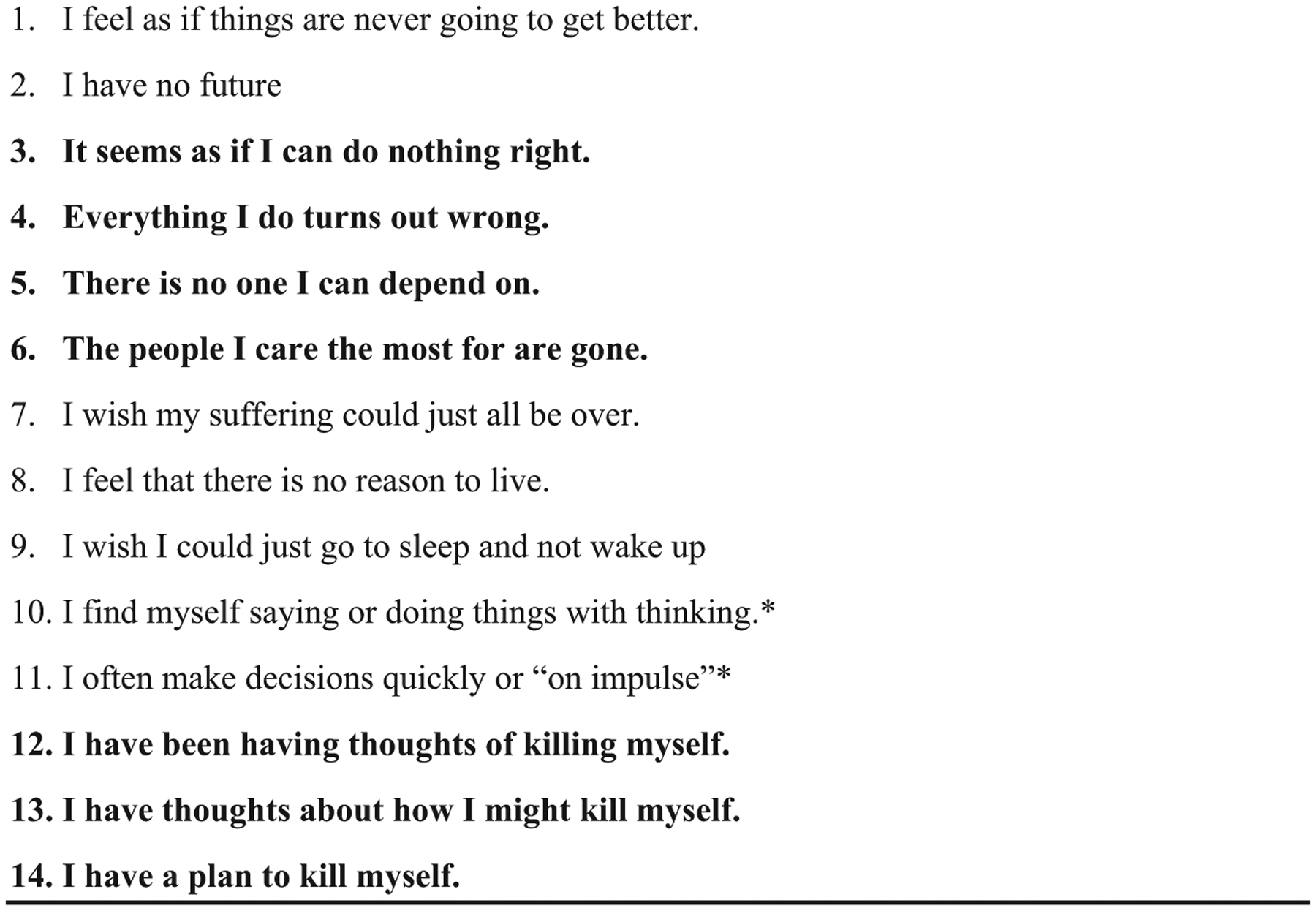
Concise Health Risk Tracking (CHRT) items. ©Trivedi 2011.
Note: Items listed in bold comprise the 7-item version of the CHRT. Factors include hopelessness (items 3 and 4), perceived lack of social support (items 5 and 6), and current suicidal thoughts and plans (items 12, 13, and 14).
*Items 10 & 11 reflecting impulsivity have been omitted from some previous published versions of the CHRT
2.4. Statistical analyses
Descriptive data were reported as frequencies or mean and standard deviation, as appropriate. Cronbach’s coefficient alpha was calculated to assess internal consistency reliability between the scale items for both versions of the CHRT (14-item and 7-item). A confirmatory factor analysis was performed on the 7-item version, assuming each of the items loaded onto one of the three independent factors (current suicidal thoughts and plans, perceived lack of social support, and hopelessness), which have been previously reported in unipolar major depressive disorder samples (Trivedi et al., 2011). Model fit was assessed using the Goodness of Fit index (GFI), adjusted GFI (AGFI), and the RMSEA estimate.
To assess correlates of suicidality at baseline, we reported Pearson correlation coefficients and odds ratios, as appropriate. Potential clinical correlates of suicide included BISS depression, mania, and anxiety domain scores, CGI-BP depression, mania, and overall scores, bipolar disorder subtype, and the presence or absence of a current major depressive episode, and current anxiety disorders. We examined the relationship between each CHRT item as well as the 7-item and 14-item scores with each clinical correlate. We also considered the relationship between both CHRT scales and other measures of suicidality, such as the individual lifetime behavioral items of the CSSRS, the MINI suicide risk score, and the BISS suicide item.
For our longitudinal analyses, we used two different approaches to determine whether the CHRT and other baseline suicide metrics predicted suicide-related SAEs (sSAEs) over the study period. First, we compared the different suicidality metrics between groups (sSAE versus no sSAE) using a Fisher’s exact test or a two-sample t-test, as appropriate. Then, we used multivariate Cox proportional hazards models to assess whether suicidality predicted time to first sSAE. This second approach took into account differential follow-up and adjusted for BISS depression domain score, presence of any anxiety disorder, post-traumatic stress disorder, and substance abuse at baseline. We investigated the extent to which overall changes in clinical variables (e.g. BISS, CGI-BP) correlated with changes in suicidality (CHRT 14-item) over the 6-month study period using mixed effects regression models to estimate the covariance (and correlation) between the patient-specific slopes of each outcome. Two-tailed p-values less than 0.05 were considered statistically significant. Statistical analyses were performed using SAS 9.4 (Cary, NC, USA).
3. Results
3.1. Part 1: Psychometric properties of the CHRT at baseline
3.1.1. Internal consistency
Both the 14-item and 7-item versions had strong reliability with Cronbach’s coefficient alphas of 0.88 and 0.79, respectively. Conventionally, a scale is thought to have acceptable internal consistency reliability with alpha greater than 0.70 (since Cronbach’s alpha is a lower bound of reliability). Thus, all items in both versions have little within-item variability, and thus have strong inter-correlation at baseline.
3.1.2. Construct validity
Our confirmatory factor analysis resulted in a GFI of 0.99, AGFI of 0.96 (conventional cutoff for both of > 0.90 for “satisfactory” fit), and RMSEA of 0.05 (conventional cutoff is < 0.06). These diagnostics supported that the 7-item scale fit the given 3 factor construct (current suicidal thoughts and plans, perceived lack of social support, and hopelessness; Fig. 1) which have been previously reported in unipolar samples (Trivedi et al., 2011).
3.2. Part 2: Clinical correlates at baseline
Of the 482 patients enrolled, 283 (59%) were female, 329 (68%) met criteria for BPI, 303 (63%) had a current major depressive episode, 277 (57%) met criteria for a current anxiety disorder (Panic Disorder, Agoraphobia, Social Phobia, and Generalized Anxiety Disorder), and 58 (12%) met criteria for current PTSD. The average CGI-BP score was 4.5 (SD=0.9) at intake. Based on the MINI Suicide module, 77 (16%) patients were considered to be at high risk of suicide, 63 (13%) were at moderate risk, 284 (59%) were at low risk, and 58 (12%) were at no risk. As assessed by the CSSRS at baseline, 173 (36%) had a history of past suicide attempts, 59 (12%) had a history of aborted attempts, 30 (6%) had a history of interrupted attempts, 71 (15%) had a history of preparatory acts or behaviors, 89 (19%) had a history of hospitalization instituted or recommended to prevent suicide, and 82 (17%) had a history of non-suicidal self-injurious behavior.
Table 1 summarizes the clinical correlates of 14-item and 7-item CHRT at baseline. Higher (worse) scores on the CHRT were significantly related to higher MINI suicide risk, BISS suicidality, depression and anxiety domain scores, and CGI-BP overall, and depression scores. Neither the 7-item nor the 14-item CHRT total score correlated significantly with the BISS mania domain score or the CGI-BP mania score; however, several individual CHRT items did significantly correlate with mania measures. The two CHRT items assessing impulsivity “I find myself saying or doing things without thinking” and “I often make decisions quickly or on impulse” were significantly correlated with the BISS mania domain score (Pearson’s r=0.21 and 0.28; p < 0.001) and CGI-BP mania (r=0.18 and 0.25; p < 0.001). Also, the CHRT item “There is no one I can depend on” correlated significantly with the BISS mania domain score (r=0.10; p=0.03) and correlated marginally with the CGI-BP mania score (r=0.08; p=0.07).
Table 1.
Clinical correlates of 14-item and 7-item CHRT at baseline.
| Variable | CHRT14-item | CHRT 7-item | ||
|---|---|---|---|---|
| Pearson’s r | P-value | Pearson’s r | P-value | |
| CGI-BP | ||||
| Overall severity | 0.39 | <0.001 | 0.36 | <0.001 |
| Depression | 0.51 | <0.001 | 0.45 | <0.001 |
| Mania | 0.05 | 0.27 | 0.05 | 0.25 |
| BISS | ||||
| Depression | 0.58 | <0.001 | 0.51 | <0.001 |
| Mania | 0.07 | 0.15 | 0.06 | 0.18 |
| Suicidality item | 0.56 | <0.001 | 0.54 | <0.001 |
| MINI suicide risk | 0.49 | <0.001 | 0.51 | <0.001 |
| OR [95% CI]* | OR [95% CI]* | |||
| CSSRS | ||||
| Actual attempt | 1.05 [1.03, 1.07] | <0.001 | 1.10 [1.06, 1.15] | <0.001 |
| Interrupted attempt | 1.05 [1.01, 1.09] | 0.02 | 1.11 [1.04, 1.20] | 0.003 |
| Aborted attempt | 1.02 [0.99, 1.05] | 0.224 | 1.05 [0.99, 1.10] | 0.10 |
| Preparatory acts/behaviors | 1.06 [1.03, 1.09] | <0.001 | 1.12 [1.06, 1.17] | <0.001 |
| Hospitalized to prevent suicide | 1.03 [1.00, 1.05] | 0.04 | 1.04 [1.00, 1.09] | 0.07 |
| Non-suicidal self-injurious behavior | 1.02 [1.00, 1.05] | 0.06 | 1.05 [1.01, 1.10] | 0.03 |
| Current major depressive episode | 1.07 [1.05, 1.10] | <0.001 | 1.13 [1.08, 1.18] | <0.001 |
| Bipolar I | 1.01 [0.99, 1.03] | 0.29 | 1.02 [0.98, 1.06] | 0.36 |
| Current anxiety disorder | 1.05 [1.03, 1.07] | <0.001 | 1.08 [1.04, 1.12] | <0.001 |
| Current PTSD | 1.06 [1.03, 1.09] | <0.001 | 1.09 [1.03, 1.15] | 0.002 |
Abbreviations: BISS: Bipolar Inventory of Symptoms Scale, CGI-BP: Clinical Global Impressions-Bipolar Version, CHRT: Concise Health Risk Tracking, CI: confidence interval, CSSRS: Columbia Suicide Severity Rating Scale, MADRS: Montgomery-Asberg Depression Rating Scale, OR: odds ratio, PTSD: Posttraumatic Stress Disorder, YMRS: Young Mania Rating.
Based on logistic regression.
The 7-item and 14-item CHRT total scores also correlated significantly with having a current major depressive episode, anxiety disorder (Panic Disorder, Agoraphobia, Social Phobia, and Generalized Anxiety Disorder as assessed by the MINI), and PTSD.
Considering relationships between the CHRT and CSSRS, we found that the 7-item and 14-item CHRT total scores correlated significantly with lifetime histories of suicide attempts, interrupted attempts, and preparatory acts/behaviors. Only the 7-item CHRT total score was correlated significantly with a history of non-suicidal self-injurious behavior. Only the 14-item CHRT total score correlated significantly with a history of hospitalization to prevent suicide.
3.3. Part 3: Longitudinal analyses
3.3.1. Prediction of suicide related SAEs
A total of 26 patients (5% of cohort) experienced SAEs that were classified as related to suicidality (sSAEs) during the course of the study. Patients who did compared to those who did not experience at least one sSAE during the study had a significantly higher mean+SD baseline 14-item CHRT total score (29.9+11.7 versus 23.7+9.6, p=0.003). This effect remained significant when accounting for differential follow-up and adjusting for other baseline covariates (i.e. using our multivariate Cox PH model), such that a 10-point increase in baseline 14-item CHRT total score increased the hazard of a sSAE by 76% (hazard ratio [95% CI]=1.76 [1.01,3.05], p=0.04).
The relationship between lifetime suicidal behaviors (assessed by the CSSRS at baseline) and subsequent suicidal SAEs during the study was also examined. Patients with histories of suicide attempts, interrupted attempts, aborted attempts and non-suicidal self-injurious behavior (assessed by baseline CSSRS) were not more likely to have a sSAE during the study compared to those without (all p’s > 0.05, data not shown). Although patients with compared to without histories of preparatory acts were more likely to have a sSAE during the study, this finding lost significance after accounting for differential follow-up and adjusting for other baseline covariates (p=0.32, data not shown).
A significant relationship was found between baseline MINI suicidal risk score and subsequent sSAEs during the study (p=0.001) and remained marginally significant after adjusting for BISS depression domain score, presence of any anxiety disorder, post-traumatic stress disorder, or substance abuse at baseline using our multivariate Cox PH model (p=0.10). Specifically, adjusting for other baseline covariates, (BISS depression domain score, presence of any anxiety disorder, post-traumatic stress disorder, or substance abuse at baseline) the MINI high risk group had 2.8 times the hazard of having a sSAE compared to the aggregate group of none, low, and moderate risk (95% CI=[1.00, 7.72], p=0.049).
3.3.2. Longitudinal correlations
Table 2 summarizes association between changes in clinical variables and the 14-item CHRT total score during the 6-month study. We found changes in suicidality were significantly and positively correlated with changes in BISS total, depression, and anxiety domain scores, as well as CGI-BP overall and depression scores. Of these significant associations, trends in depressive symptom severity correlated most strongly with trends in suicidality over the study. Neither 7-item nor 14-item CHRT total score correlated significantly with the BISS mania domain score or CGI-BP mania score.
Table 2.
Association between changes in clinical variables and 14-item CHRT over 6-months.
| Variable | Covariance of slopes [95% CI] | Correlation coefficient | P-value |
|---|---|---|---|
| CGI-BP | |||
| Overall severity | 0.35 [0.21, 0.49] | 0.54 | <0.0001 |
| Depression | 0.44 [0.28, 0.60] | 0.58 | <0.0001 |
| Mania | 0.10 [−0.03, 0.23] | 0.13 | 0.14 |
| BISS | |||
| Total | 6.87 [4.56, 9.19] | 0.63 | <0.0001 |
| Depression | 3.15 [2.19, 4.12] | 0.73 | <0.0001 |
| Mania | 0.02 [−0.59, 0.62] | 0.00 | 0.95 |
| Anxiety | 2.59 [1.66, 3.52] | 0.56 | <0.0001 |
| Irritability | 2.41 [1.43, 3.40] | 0.53 | <0.0001 |
| Psychosis | 0.47 [0.06, 0.88] | 0.20 | 0.02 |
Abbreviations: BISS: Bipolar Inventory of Symptoms Scale, CGI-BP: Clinical Global Impressions-Bipolar Version, CHRT: Concise Health Risk Tracking.
Note: Numbers in table are based on mixed effects regression models, which estimated the covariance (and correlation) between patient-specific slopes of each outcome.
4. Discussion
As one of the first studies to utilize the CHRT in a bipolar sample, these findings confirm strong internal consistency for both the 7-item and 14-item versions. Furthermore, a confirmatory factor analysis of the 7-item version confirmed its construct validity, yielding the 3 factors of current suicidal thoughts and plans, perceived lack of social support, and hopelessness which had been previously reported in unipolar major depressive disorder samples.
Baseline self-reported, 7-item and 14-item CHRT total scores correlated significantly with clinician-rated measures of current and lifetime suicidality, including the MINI suicide risk score, BISS suicidality item, and CSSRS past suicide attempt, past interrupted attempts, and past preparatory acts/behaviors. The 7-item CHRT total score correlated significantly with CSSRS past history of non-suicidal self-injurious behavior, while the 14-item CHRT total score correlated significantly with a history of hospitalization to prevent suicide. These findings suggest that the CHRT is a powerful self-report instrument that has the potential to capture suicidal ideation and behavior as consistently as more widely established clinician-rated measures.
At baseline and during the study, CHRT total scores correlated significantly with measures of depression and anxiety, as assessed by the BISS and CGI-BP. Although CHRT total scores did not correlate with measures of mania at baseline or during the study, 2 CHRT item scores assessing impulsivity (which were deleted from the CHRT in previous studies with unipolar major depressive disorder samples) correlated significantly with the CGI-BP mania and BISS mania domain score at baseline, suggesting that these items may be relevant when assessing suicidality among bipolar samples.
Most importantly, baseline self-report CHRT total score served as a robust predictor of subsequent sSAEs during the study, even after controlling for BISS depression domain score, presence of any anxiety disorder, PTSD, or substance abuse at baseline. This finding has profound implications for both research and clinical practice in patients with BP. While the risk of suicide in BP is significantly higher compared to the general population, accurate prediction of suicidal behavior remains elusive. The CHRT has the advantage of being a quick, straightforward, self-report measure that can easily be administered, requiring minimal clinician training and time. Although the MINI suicide risk score at baseline also served as a powerful predictor of subsequent sSAEs in patients classified as “high risk,” the MINI requires clinician training and administration, and significant time commitment.
Multiple previous studies have shown that a history of suicide attempts predicts future attempts in patients with BP (Greist et al., 2014; Umamaheswari et al., 2014; Oquendo et al., 2004; Galfalvy et al., 2006; Antypa et al., 2013). Surprisingly, a past history of actual suicide attempts with an intent to die, as assessed by the CSSRS, did not predict subsequent sSAEs during the study. Likewise, patients with past histories of interrupted attempts, aborted attempts and non-suicidal self-injurious behavior were no more likely than patients without such histories to experience a sSAE during the study. While patients with compared to without a history of preparatory acts were more likely to have a sSAE during the study, this finding lost statistical significance after adjusting for BISS depression domain score, presence of any anxiety disorder, post-traumatic stress disorder, or substance abuse at baseline. A history of preparatory acts, therefore, appeared to be a proxy for severity. Similarly, this finding lost statistical significance when using survival methods to account for differential follow-up times. These findings may indicate that when assessing for suicidality, intent to behave (suicide) may be a stronger predictor of future behavior than a prior history of behavior (history of suicide/suicidal behaviors). This may have a significant impact on clinical practice during suicide risk assessment.
Several limitations exist in the current study. Previous studies using the CSSRS as a predictive tool for future attempts utilized both the lifetime history of suicidal behaviors in combination with CSSRS assessment of current ideation. The CHOICE study only used the clinician-based lifetime modules of the CSSRS to assess a past history of suicidal behaviors. Perhaps a combined assessment of previous behaviors and current ideation could have yielded a higher predictive value, as both static (e.g, history of lifetime attempts) and dynamic, and potentially modifiable, (e.g., hopelessness) risk factors have been shown to play important roles in predicting suicide. In the current study, the CSSRS was only used to assess static risk factors in terms of past suicidal behaviors. Furthermore, the study was only 6 months long and a past history of suicidal behaviors may have been a more powerful predictor over the course of longer-term follow-up.
Cultural sensitivity in the assessment of suicidality may also be a limitation in our study, as suicide presentation and risk may vary tremendously across ethnic and sexual minority groups (Chu et al., 2010, 2013). The recently published Cultural Assessment of Risk for Suicide measure (CARS; Chu et al., 2013) may have an advantage over the CHRT in assessing suicidal risk in ethnic and sexual minority groups, as it was specifically developed to assess unique risk factors in these groups, such as perceived discrimination. In our current sample of participants, 19.9% were Black, 3.3% were Asian, 4.6% were other, and 11% identified as Hispanic or Latino. Future research should directly examine the psychometric properties and predictive value of the CHRT with ethnic and sexual minority samples.
Both the 14-item and 7-item CHRT versions demonstrated strong reliability, with Cronbach’s coefficient alphas of 0.88 and 0.79, respectively. For research purposes, a scale is thought to have acceptable internal consistency reliability with alpha greater than 0.70, when used to distinguish differences between groups. However, for clinical purposes, a higher alpha is of 0.90 is recommended, when the value of an individual’s scale is considered (Bland and Altman, 1997). Given its higher internal consistency, the 14-item version is likely preferable to the 7-item version for clinical use. Alternatively, the 12-item CHRT version (which eliminates the 2 items assessing impulsivity) was found to have an even stronger internal consistency of 0.90 in a previous study by Ostacher et al. (2015). The CHRT has potentially important clinical and research applications and it is vital to acknowledge these issues when selecting a version for use.
The accurate assessment of suicidal risk is vitally important for primary care settings, as well as in psychiatric practice (McDowell et al., 2011). Patients dying from suicide saw their primary care physicians twice as often as their mental health clinicians and an estimated 45% of patients dying from suicide saw their primary care physicians in the past month (Luoma et al., 2002). However, there is scant data to support the predictive validity of the Joint Commission’s recommended Suicide Assessment Five-step Evaluation and Triage (SAFE-T; Jacobs, 2011), which includes: identification of risk factors, protective factors, suicidal inquiry (suicidal thoughts, plans, behavior and intent), determination of risk level/intervention, and documentation. While this method provides a useful framework, a validated self-report instrument with predictive value, such as the CHRT, would be a valuable addition to this procedure, with no incremental clinician burden.
A growing trend for depression screening in primary care is the Patient Health Questionnaire-9 (PHQ-9; Wittkampf et al., 2007, 2009), which contains 9 questions assessing major depressive criteria from DSM-IV. While a recent study found that Item 9 of the PHQ-9 (thoughts of being better off dead or hurting self) identified outpatients at increased risk of suicide attempt or death, further screening of those at high risk is recommended (Simon et al., 2013). The CHRT offers a brief, yet robust method that could potentially be used to monitor those at risk.
In clinical trials research, the CHRT offers the potential of predicting at baseline which patients will have a sSAE during the course of follow-up. In the current study, baseline CHRT scores significantly predicted risk of subsequent suicidality-related Serious Adverse Events (sSAEs), after controlling for mood and comorbidity, with the hazard of sSAE increasing by 76% for every 10-point increase in baseline CHRT score. This predictive value was particularly powerful considering the 6 month time frame for follow up. The role of intense affective states, particularly desperation, have also shown great promise in predicting even shorter-term, acute risk for suicidal behavior and could be examined in conjunction with the CHRT in future studies (Hendin et al., 2010).
In conclusion, our findings suggest that the CHRT offers a quick, straightforward, and robust self-report tool for assessing suicidal risk that is highly correlated with clinician-rated measures of mood and suicidality. Future research studies and clinical practice could benefit by incorporating the self-report CHRT, and continuing to examine its relevance as a predictor of future suicidal behavior in patients with not only unipolar major depressive disorder, but also BD.
References
- Antypa N, Antonioli M, Serretti A, 2013. Clinical, psychological and environmental predictors of prospective suicide events in patients with Bipolar Disorder. J. Psychiatry Res 47, 1800–1808. [DOI] [PubMed] [Google Scholar]
- Asao K, Kao WH, Baptiste-Roberts K, Bandeen-Roche K, Erlinger TP, Brancati FL, 2006. Short stature and the risk of adiposity, insulin resistance, and type 2 diabetes in middle age: the Third National Health and Nutrition Examination Survey (NHANES III), 1988–1994. Diabetes Care 29, 1632–1637. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA, 1990. Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. Am. J. Psychiatry 147, 190–195. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A, 1979. Assessment of suicidal intention: the scale for suicidal ideation. J. Consult. Clin. Psychol 47, 343–352. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, 1990. Manual for Beck Depression Inventory. Psychological Corporation, San Antonio, TX. [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L, 1976. Classification of suicidal behaviors. II. Dimensions of suicidal intent. Arch. Gen. Psychiatry 33, 835–837. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L, 1974. The measurement of pessimism: the hopelessness scale. J. Consult. Clin. Psychol 42, 861–865. [DOI] [PubMed] [Google Scholar]
- Bland JM, Altman DG, 1997. Chronbach’s alpha. BMJ 314, 572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowden CL, Singh V, Thompson P, Gonzalez JM, Katz MM, Dahl M, Prihoda TJ, Chang X, 2007. Development of the bipolar inventory of symptoms scale. Acta Psychiatr. Scand 116, 189–194. [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR, 2000. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J. Consult. Clin. Psychol 68, 371–377. [PubMed] [Google Scholar]
- Cerimele JM, Chwastiak LA, Chan YF, Harrison DA, Unutzer J, 2013. The presentation, recognition and management of bipolar depression in primary care. J. Gen. Intern. Med 28, 1648–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu JP, Floyd R, Diep H, Pardo S, Goldblum P, Bongar B, 2013. A tool for the culturally competent assessment of suicide: the Cultural Assessment of Risk for Suicide (CARS) measure. Psychol. Assess 25, 424–434. [DOI] [PubMed] [Google Scholar]
- Chu JP, Goldblum P, Floyd R, Bongar B, 2010. The cultural theory and model of suicide. Appl. Prev. Psychol 14, 25–40. [Google Scholar]
- Galfalvy H, Oquendo MA, Carballo JJ, Sher L, Grunebaum MF, Burke A, Mann JJ, 2006. Clinical predictors of suicidal acts after major depression in bipolar disorder: a prospective study. Bipolar Disord. 8, 586–595. [DOI] [PubMed] [Google Scholar]
- Gonzalez JM, Bowden CL, Katz MM, Thompson P, Singh V, Prihoda TJ, Dahl M, 2008. Development of the Bipolar Inventory of Symptoms Scale: concurrent validity, discriminant validity and retest reliability. Int. J. Methods Psychiatr. Res 17, 198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greist JH, Mundt JC, Gwaltney CJ, Jefferson JW, Posner K, 2014. Predictive value of baseline electronic Columbia-Suicide Severity Rating Scale (eC-SSRS) assessments for identifying risk of prospective reports of suicidal behavior during research participation. Innov. Clin. Neurosci 11, 23–31. [PMC free article] [PubMed] [Google Scholar]
- Hamilton M, 1960. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendin H, Al Jurdi RK, Houck PR, Hughes S, Turner JB, 2010. Role of intense affects in predicting short-term risk for suicidal behavior: a prospective study. J. Nerv. Ment. Dis 198, 220–225. [DOI] [PubMed] [Google Scholar]
- Jacobs DG, 2011. Suicide assessment five-step evaluation and triage. In: Best Practices Registry (BPR) for Suicide Prevention. SPRC (Suicide Prevention Resource Center) Web site. ⟨http://www.sprc.org/library/safe_t_pcktcrd_edc.pdf⟩ (accessed 22.03.11.). [Google Scholar]
- Luoma JB, Martin CE, Pearson JL, 2002. Contact with mental health and primary care providers before suicide: a review of the evidence. Am. J. Psychiatry 159, 909–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell AK, Lineberry TW, Bostwick JM, 2011. Practical suicide-risk management for the busy primary care physician. Mayo Clin. Proc 86, 792–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundt JC, Greist JH, Jefferson JW, Federico M, Mann JJ, Posner K, 2013. Prediction of suicidal behavior in clinical research by lifetime suicidal ideation and behavior ascertained by the electronic Columbia-Suicide Severity Rating Scale. J. Clin. Psychiatry 74, 887–892. [DOI] [PubMed] [Google Scholar]
- Nierenberg AA, Gray SM, Grandin LD, 2001. Mood disorders and suicide. J. Clin. Psychiatry 62 (Suppl. 25), S27–S30. [PubMed] [Google Scholar]
- Nierenberg AA, Sylvia LG, Leon AC, Reilly-Harrington NA, Shesler LW, McElroy SL, Friedman ES, Thase ME, Shelton RC, Bowden CL, Tohen M, Singh V, Deckersbach T, Ketter TA, Kocsis JH, McInnis MG, Schoenfeld D, Bobo WV, Calabrese JR, Bipolar CHOICE Study Group, 2014. Clinical Health Outcomes Initiative in Comparative Effectiveness for Bipolar Disorder (Bipolar CHOICE): a pragmatic trial of complex treatment for a complex disorder. Clin. Trials 11, 114–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Galfalvy H, Russo S, Ellis SP, Grunebaum MF, Burke A, Mann JJ, 2004. Prospective study of clinical predictors to suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am. J. Psychiatry 161, 1433–1441. [DOI] [PubMed] [Google Scholar]
- Osby U, Brandt L, Correia N, Ekbom A, Sparen P, 2001. Excess mortality in bipolar and unipolar disorder in Sweden. Arch. Gen. Psychiatry 58, 844–850. [DOI] [PubMed] [Google Scholar]
- Ostacher MJ, Nierenberg AA, Rabideau D, Reilly-Harrington NA, Sylvia LG, Gold AK, Shesler LW, Ketter TA, Bowden CL, Calabrese JR, Friedman ES, Iosifescu DV, Thase ME, Leon AC, Trivedi MH, 2015. A clinical measure of suicidal ideation, suicidal behavior, and associated symptoms in bipolar disorder: psychometric properties of the Concise Health Risk Tracking Self-Report (CHRT-SR). J. Psychiatr. Res 71, 126–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, Mann JJ, 2011. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am. J. Psychiatry 168, 1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roshanaei-Moghaddam B, Katon W, 2009. Premature mortality from general medical illnesses among persons with bipolar disorder: a review. Psychiatr. Serv 60, 147–156. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC, 1998. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 59 (Suppl. 20), S22–S33 (quiz 34–57). [PubMed] [Google Scholar]
- Simon GE, Rutter CM, Peterson D, Oliver M, Whiteside U, Operskalski B, Ludman H, 2013. Does response on the PHQ-9 depression questionnaire predict subsequent suicide attempt or suicide death. Psychiatr. Serv 64, 1195–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W, 1997. Modification of the Clinical Global Impressions (CGI) Scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res. 73, 159–171. [DOI] [PubMed] [Google Scholar]
- Suppes T, Dennehy EB, Hirschfeld RM, Altshuler LL, Bowden CL, Calabrese JR, Crismon ML, Ketter TA, Sachs GS, Swann AC, Texas Consensus Conference Panel onMedication Treatment of Bipolar Disorder, 2005. The Texas implementation of medication algorithms:update to the algorithms for treatment of bipolar I disorder. J. Clin. Psychiatry 66, 870–886. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Wisniewski SR, Morris DW, Fava M, Gollan JK, Warden D, Nierenberg AA, Gaynes BN, Husain MM, Luther JF, Zisook S, Rush AJ, 2011. Concise Health Risk Tracking scale: a brief self-report and clinician rating of suicidal risk. J. Clin. Psychiatry 72, 757–764. [DOI] [PubMed] [Google Scholar]
- Umamaheswari V, Avasthi A, Grover S, 2014. Risk factors for suicidal ideations in patients with bipolar disorder. Bipolar Disord. 16, 642–651. [DOI] [PubMed] [Google Scholar]
- Valtonen HM, Suominen K, Sokero P, Mantere O, Avrilommi P, Leppamaki S, Isometsa ET, 2009. How suicidal bipolar patients are depends on how suicidal ideation is defined. J. Affect. Disord 118, 48–54. [DOI] [PubMed] [Google Scholar]
- Wittkampf K, Naeije L, Schene AH, Huyser J, van Weert HC, 2007. Diagnostic accuracy of the mood module of the Patient Health Questionnaire: a systematic review. Gen. Hosp. Psychiatry 29, 388–395. [DOI] [PubMed] [Google Scholar]
- Wittkampf K, van Ravesteijn H, Baas K, van de Hoogen H, Schene A, Bindels P, Lucassen P, van de Lisdonk E, van Weert H, 2009. The accuracy of Patient Health Questionnaire-9 in detecting depression and measuring depression severity in high-risk groups in primary care. Gen. Hosp. Psychiatry 31, 451–459. [DOI] [PubMed] [Google Scholar]


