Abstract
Platelet derived growth factor (PDGF) signaling has been extensively studied in the context of vascular disease, but the genetics of this pathway remain to be established. Genome wide association studies (GWAS) for coronary artery disease (CAD) have identified a risk locus at 11q22.3, and we have verified with fine mapping approaches that the regulatory variant rs2019090 and PDGFD represent the functional variant and putative functional gene. Further, FOXC1/C2 transcription factor (TF) binding at rs2019090 was found to promote PDGFD transcription through the CAD promoting allele. Employing a constitutive Pdgfd knockout allele along with SMC lineage tracing in a male atherosclerosis mouse model we mapped single cell transcriptomic, cell state, and lesion anatomical changes associated with gene loss. These studies revealed that Pdgfd promotes expansion, migration, and transition of SMC lineage cells to the chondromyocyte phenotype and vascular calcification. This is in contrast to protective CAD genes TCF21, ZEB2, and SMAD3 which we have shown to promote the fibroblast-like cell transition or perturb the pattern or extent of transition to the chondromyocyte phenotype. Further, Pdgfd expressing fibroblasts and pericytes exhibited greater expression of chemokines and leukocyte adhesion molecules, consistent with observed increased macrophage recruitment to the plaque. Despite these changes there was no effect of Pdgfd deletion on SMC contribution to the fibrous cap or overall lesion burden. These findings suggest that PDGFD mediates CAD risk through promoting SMC expansion and migration, in conjunction with deleterious phenotypic changes, and through promoting an inflammatory response that is primarily focused in the adventitia where it contributes to leukocyte trafficking to the diseased vessel wall.
Introduction
Coronary artery disease (CAD) is predicted to continue as the worldwide leading cause of human mortality for at least the next two decades 1, 2. While as much as half of the disease risk is conferred by classical risk factors that have been ameliorated by the development of targeted therapies, but the remainder of the risk is still unaddressed. Genome wide association studies (GWAS) have identified hundreds of genomic loci that contribute to the genetic risk for CAD, with further studies indicating that genes in these loci regulate the primary cellular processes that underlie the remaining disease risk through their effect on vascular wall cellular and molecular mechanisms, as well as disease related processes in liver and adipose tissues 3, 4, 5, 6. These data suggest that investigation of the molecular pathways that are embedded in CAD gene regulatory networks will provide new and effective approaches to treating this devastating disease. Indeed, there are currently no drugs that effectively target the primary disease process in the vessel wall.
Recent GWAS meta-analyses have identified approximately 250 loci that confer CAD risk 7, 8. While only a handful of these loci have been studied thus far, it is increasingly clear that smooth muscle cells (SMC), endothelial cells and macrophages confer a significant portion of the genetic disease risk 9, through phenotypic transitions that are mediated by dramatic cell state changes 10, 11, 12, 13, 14. For SMC, these phenotypic changes have been linked to disease risk through single cell RNA sequencing (scRNAseq) and cellular lesion anatomy studies showing that expression of protective CAD associated gene Tcf21 promotes transition primarily to the fibroblast-like fibromyocyte (FMC) phenotype, and that protective Tgfb signaling molecules Zeb2 and Smad3 fundamentally alter or inhibit transition to the chondrocyte-like chondromyocyte (CMC) phenotype 12, 15, 16. While atherosclerosis has been characterized as a primarily inflammatory disease 17, there has been a dearth of such molecules linked to the disease process by human GWAS studies.
Although not guided by human genetic data, platelet-derived growth factors (PDGFs) have been implicated in the fundamental biology of vascular wall development as well as the pathophysiology of atherosclerosis 18, 19. PDGFs were originally identified in platelets and serum as potent mitogens for smooth muscle cells and fibroblasts in vitro 20, 21. The PDGF family consists of four ligands, A-D, forming dimeric proteins that signal through two tyrosine kinase receptors, PDGFRA and PDGFRB. The ligands and receptors can form homodimers or heterodimers depending on cell type, receptor expression, and ligand availability 22, 23, 24, 25. Interestingly, the most recently characterized ligand PDGFD can bind PDGFRB homodimers, PDGFRA-PDGFRB heterodimers as well as heterodimers involving NRP1 and PDGFRB 25. Signaling through PDGFRB has been shown to initiate endothelial, pericyte, and smooth muscle cell proliferation and migration both in vitro and in vivo 23, 24. The PDGFB and PDGFRB system is critical for the migration and proliferation of pericytes and the development of a functional vasculature 26, 27. Deletion of Pdgfrb in the disease setting has been shown to abrogate the SMC cell state changes that represent the response of this cell type to disease stimuli 28.
The locus encoding PDGFD has been identified in GWAS studies to be associated with CAD risk 8, 29. However, biological investigation of a role for PDGFD in atherosclerosis has yet to be defined. Here, through fine mapping approaches we present data suggesting that PDGFD is the disease gene for CAD at this locus and further provide evidence to support the mechanism of association to be due to FOXC1/C2 differential binding at the rs2019090 associated variant. By generating a Pdgfd−/− mouse model on an atherosclerosis genetic background with SMC lineage tracing combined, single cell transcriptomics and lesion anatomy studies, we show that this factor modulates SMC expansion, phenotypic transition, and migration into the plaque with additional effects on monocyte recruitment and vascular inflammation. Together, we provide evidence that supports PDGFD as the disease gene at this CAD risk locus and reveal insights into its role in mediating vascular smooth muscle specific phenotypic changes and plaque biology.
Results
Fine mapping and epigenome editing at the 11q22.3 CAD GWAS locus implicates rs2019090 as the functional associated variant and PDGFD as a disease gene
Our group previously identified 87 candidate genetic variants that are associated with CAD, using human coronary artery smooth muscle cell (HCASMC) ATAC-seq and ChIP-seq data with CARDIoGRAMplusC4D CAD GWAS variants 30. After filtering for variants with a combination of known and predicted regulatory elements in the intergenic regions and evidence of transcription factor binding in vivo, we prioritized 64 variants in HCASMC. Six CAD SNPs in high linkage disequilibrium were noted to be associated to CAD risk by GWAS at 11q23.2. One of these SNPs, rs2019090, was localized 150 kilobases (kb) downstream of PDGFD in an intron of the long non-coding RNA (lncRNA) AP002989.1, in HCASMC peaks for ATACseq identified open chromatin and enhancer related H3K27ac histone modification, in juxtaposition to ChIPseq peaks for CAD transcription factors (TFs) TCF21 and SMAD3 (Figs. 1A – 1C). GWAS data curated in the NHGRI-EBI GWAS Catalog (V1.0.2) also indicated association with carotid intimal-medial thickness (IMT), with the A allele identified as promoting disease risk for both CAD and IMT 31, 32, 33, 34. Rs2019090 was shown to serve as an expression quantitative trait locus (eQTL) variant in analysis of GTEx data (p=1.6e-8), with the risk ‘A’ allele being associated with greater expression of PDGFD 5, 32, 35, 36, as well as increased expression of AP002989.1 in an early GTEx analysis of aortic tissue (p=3.72e-5) 37. In addition, this variant was identified with GTEx data as a splicing QTL (sQTL) for AP002989.1 (p=4.1e-8). Further, mapping of recent CAD GWAS association findings to vascular eQTL data using the locuscompare.com tool (locuscompare.com) suggests that rs2019090 provides the greatest contribution to CAD risk and PDGFD expression (Figs. 1D, Suppl. Fig. 1A). This was validated with the enloc genome-wide co-localization analysis algorithm 38 employing CAD GWAS meta-analysis summary level data and GTEx vascular tissue eQTL data (Suppl. Fig. 1B). PDGFD was identified as significant with a regional level colocalization probability (RCP) of 0.2 as the recommended cutoff to select significant colocalization between the GWAS and eQTL data 39.
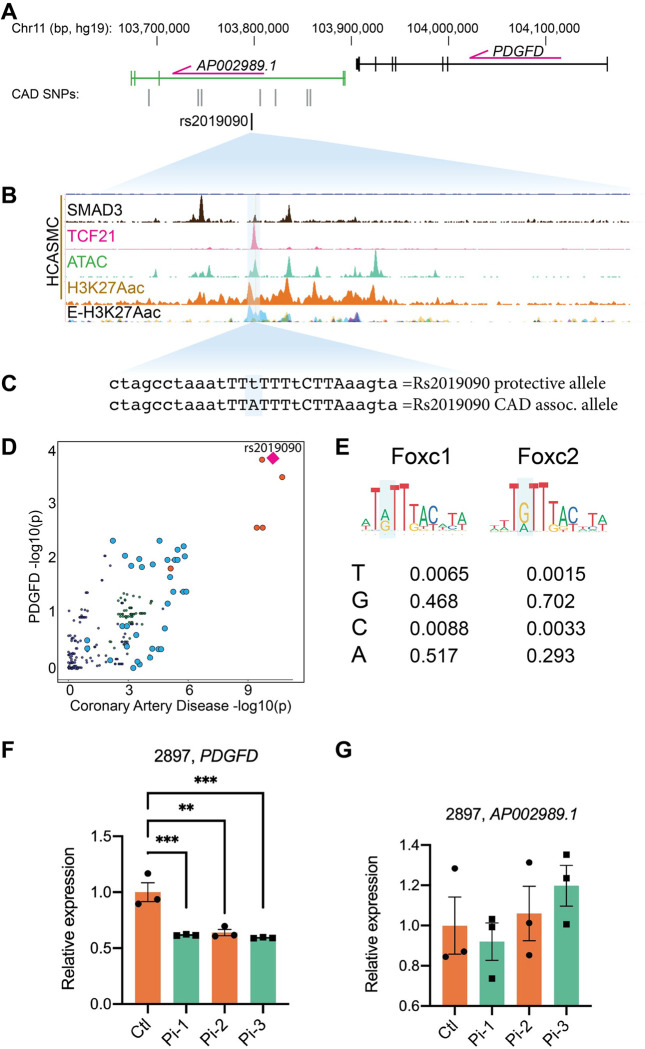
Figure 1. Functional mapping of candidate 11q22.3 locus proposes regulatory mechanisms of PDGFD expression and disease association.
(A) UCSC browser screenshot at 11q22.3 locus showing position of PDGFD gene and lncRNA AP002989.1 relative to the candidate SNP rs2019090, and (B) overlap of rs2019090 with ChIP-seq tracks for CAD risk transcription factors SMAD3 and TCF21. Also shown are ATAC-seq open chromatin and active enhancer histone modification H3K27ac ChIP-seq tracks in human coronary artery smooth muscle cells (HCASMC), as well as ENCODE layered H3K27ac for HUVEC (blue) and NHLF (purple) cells. Genomic coordinates refer to hg19 assembly. (C) Genomic sequence at rs2019090 for protective and disease alleles, with FOXC1/C2 motifs indicated. (D) Co-localization of coronary artery disease (CAD) GWAS signal and PDGFD eQTL data (GTEx v8, aorta). (E) Position weight matrices for FOXC1 and FOXC2, as per JASPAR database. (F, G) CRISPRi epigenetic silencing by transduction of dCad9KRAB and single guide RNAs targeted around rs2019090 in a HCASMC line with AA genotype. Expression of PDGFD and lncRNA AP002989.1 were evaluated by quantitative RT-PCR.
Further, we have examined the DNA sequence at rs2019090 and found that this SNP is localized in a putative FOXC1/C2 binding site. Searches of relevant TF position weight matrices (PWMs) in the JASPAR database 40 with the motif comparison MEME Suite tool Tomtom 41 have found a significant match (p=3e-3) for the two highly homologous TFs FOXC1 and FOXC2 (Figs 1C, 1E). Interestingly, the rs2019090 polymorphism is multi-allelic. A is the reference allele but T is the alternate allele in European cohorts with C and G serving as additional alternatives. As evident from the FOXC1/C2 PWMs, both A and G are common at the SNP site, and T is the least common base, suggesting that replacement of A with T by the rs2019090 variant would decrease FOXC1/C2 binding and expression of the target PDGFD gene (Fig. 1E). Both FOXC1 and FOXC2 reside in loci found to be associated with CAD 7, 8, although definitive experiments have not been conducted to prove that they are the disease associated genes in their respective loci.
To experimentally investigate whether PDGFD is the disease related gene at 11q22.3, we employed epigenetic targeting at the rs2019090 variant. CRISPRi was conducted by transducing an HCASMC line with the AA genotype, line 2897, with lentiviruses encoding dCad9KRAB along with one of three single guide RNAs (Suppl. Fig. 1C). Gene expression was evaluated by quantitative real-time PCR, for both PDGFD and the lncRNA AP002989.1 (Fig. 1F, G). These experiments indicated that PDGFD expression was highly significantly suppressed by all three guides, but interestingly the lncRNA expression was not affected. It is a consideration that CRISPRi with this approach suppresses over a distance of 1–2 kilobases, but there are no other protein coding genes withing 100,000 base pairs of the targeted region. These findings support the identification of PDGFD as the disease associated gene and indicate that lncRNA AP002989.1 is not a direct target of the disease association mechanism.
FOXC1 regulates PDGFD expression via functional CAD associated SNP rs2019090 to establish a complex gene regulatory network
We evaluated allele-specific transcription of the rs2019090 enhancer region by FOXC1 and FOXC2, with dual luciferase assays in the A7r5 rat vascular smooth muscle cell line. Three copies of the 150 bp region of the AP002989.1 intron flanking the candidate SNP rs2019090, containing either the A or the T allele, were cloned into a luciferase reporter construct and co-transfected with FOXC1 or FOXC2 expression constructs. These and other in vitro assays were performed at least three times with each having at least three biological replicates. Luciferase activity showed that over-expression of FOXC1 and FOXC2 significantly activated the A allele but suppressed the T allele reporter, indicating a direct and allele-specific regulation by FOXC1 and FOXC2 (Figs. 2A, 2B). While both of these TFs reside in CAD associated loci, and thus may be directly linked to CAD risk 8, we have decided to focus subsequent studies on FOXC1. The transcriptionally active A allele is more highly represented in its binding sites, FOXC1 mutations have been linked to PDGF signaling in the context of cerebral small vessel disease 42, and this gene has also been linked to vascular risk factors including hypertension, systolic blood pressure, and waist hip ratio (GWAS catalog). FOXC2 has been related primarily to non-vascular phenotypes, including cortical thickness and white matter hyperintensity volume (GWAS catalog).
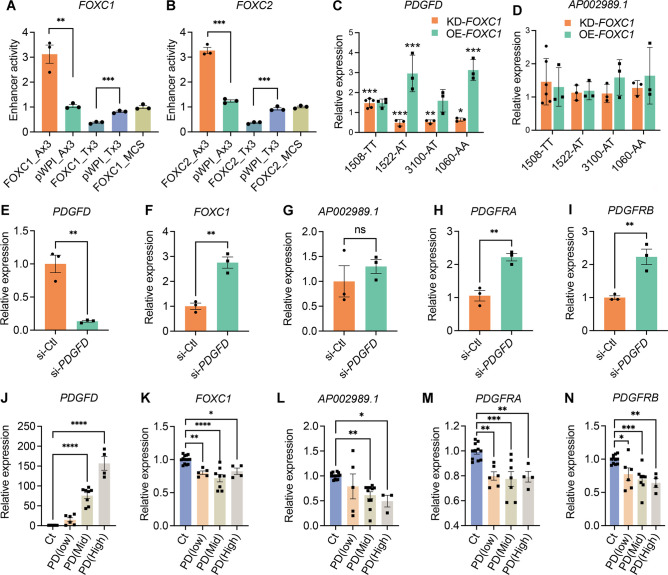
Figure 2. FOXC1 regulates PDGFD expression via causal SNP rs2019090 to establish a complex gene regulatory network.
Results of enhancer trap assay for (A) FOXC1 and (B) FOXC2 co-transfected with luciferase reporters with three copies of the 150 basepair region containing the A allele (rs-2019090-A) or T allele (rs-2019090-T) cloned into the minimal promoter-driven luciferase reporter vector pLUC-MCS. A7r5 rat vascular smooth muscle cells were used for these assays. Values represent mean ± s.e.m. of triplicates for a representative experiment, expressed as fold change relative to pWPI-empty plasmid with p-values obtained with an unpaired t-test. Abbreviations: FOXC1_Ax3, FOXC1 or 2 over-expression with A allele reporter; Pwpi_Ax3, empty expression plasmid with A allele reporter; FOXC1_Tx3, FOXC1 or 2 over-expression with T allele reporter; Pwpi_Tx3, empty expression plasmid with A allele reporter. (C) Results of quantitative polymerase chain reaction (qPCR) analysis for PDGFD or (D) AP002989.1 expression with knockdown (KD) or over-expression (OE) of FOXC1 in HCASMC carrying different genotypes for rs2019090. Each dot represents a biological replicate. Data were normalized relative to controls and expressed as mean ± s.e.m with p-values using an unpaired t-test. (E) qPCR analysis for expression levels of PDGFD, (F) FOXC1, (G) AP002989.1, (H) PDGFRA, and (I) PDGFRB with PDGFD knockdown (KD) in HCASMC. Each dot represents a biological replicate. Data were expressed as mean ± s.e.m with p-values using an unpaired t-test. (J) qPCR analysis for expression levels of PDGFD, (K) FOXC1, (L) AP002989.1, (M) PDGFRA, and (N) PDGFRB with PDGFD overexpression (OE) in HCASMC. Data grouped based on expression levels of PDGFD and expressed as mean ± s.e.m of biological replications with p-values. Each dot represents a biological replicate. Analysis was performed using one-way ANOVA with Dunnett’s multiple comparisons post-hoc test. Data represented as relative expression as control ratio (treatment of scramble siRNA (si-Ctl, KD control) or empty-pWPI (Ct, OE control). * p<0.05, ** p<0.01, *** p<0.001, **** p<0.0001.
To determine FOXC1 allele-specific cis-effects on endogenous PDGFD expression, we performed short interfering RNA (siRNA)-mediated knockdown (KD) or lentivirus-mediated overexpression (OE) of FOXC1 in four different human coronary artery smooth muscle cell (HCASMC) lines known to have AA, AT, or TT genotypes at rs2019090 (Fig. 2C) 43. We found that PDGFD expression is decreased with FOXC1-KD and increased with FOXC1-OE in both A/A homozygous and A/T heterozygous but not in T/T homozygous HCASMC, indicating that endogenous FOXC1 positively regulates PDGFD expression through the A allele of SNP rs2019090. Overall, these results were consistent with the enhancer trap assays and suggested that FOXC1 promotes PDGFD expression through the disease-associated A allele. With the knockdown studies we did not find evidence that FOXC1 suppresses PDGFD expression through the T allele at SNP rs2019090 in T/T homozygous HCASMC. Given that rs2019090 is located within the structural AP002989.1 lncRNA, and eQTL studies have associated splicing of this lncRNA with genotype at rs2019090, we performed similar studies examining the effects of FOXC1 perturbation on expression of this gene. In contrast to the results for PDGFD expression, neither increased or decreased FOXC1 expression altered mRNA levels for AP002989.1 (Fig. 2D).
We further investigated the regulatory relationship among members of the FOXC1-PDGFD pathway. We found that FOXC1 expression is significantly increased with PDGFD-KD (Figs. 2E, 2F, Suppl. Fig. 2) suggesting a negative regulatory interaction between these factors and supporting their pathway relationship. PDGFD-KD in HCASMC did not show a significant change in expression of AP002989.1 (Fig. 2G). Receptors are commonly counter-regulated by ligand levels and we investigated the expression of the two receptors known to bind PDGFD. Both the PDGFRA and PDGFRB receptor genes showed upregulation with knockdown of PDGFD (Figs. 2H, 2I), further linking these factors in a functional PDGFD signaling pathway in SMC. To complement these loss of function studies in HCASMC, we performed gain of function studies by lentivirus transduction to over-express PDGFD in these cells. We grouped batches of HCASMC expressing varying levels of PDGFD after transduction with lentivirus, dividing them into tertiles for low, moderate and high expression levels, and used quantitative RT-PCR to study the transcriptional response of related factors to increased PDGFD. We identified and employed viral titers that provided low-, medium-, and high-level expression of PDGFD (Fig. 2J). In keeping with interactions identified with PDGFD-KD, expression levels of FOXC1, PDGFRA and PDGFRB genes showed the opposite response to PDGFD by decreasing their expression (Figs. 2K, 2M, N). Surprisingly, AP002989.1 expression level was significantly reduced in response to moderate and high PDGFD expression (Fig. 2L), suggesting a counter-regulatory interaction between these two genes.
Pdgfd promotes SMC phenotypic transitions as well as monocyte-macrophage recruitment
To investigate the cellular and molecular mechanisms by which PDGFD regulates atherosclerosis development and CAD risk we developed a mouse atherosclerosis model that provided constitutive knockout of Pdgfd, as well as SMC-specific lineage marking in the ApoE−/−, C57BL/6 background. A constitutive Pdgfd knockout (KO) mouse allele that was previously generated by replacing exon1 in the Pdgfd gene with a LacZ expression cassette 44 was combined with a Cre-activatable tandem dimer Tomato (tdT) fluorescent marker gene in the ROSA26 locus 45, 46, and the highly SMC-specific Myh11-Cre recombinase transgenic allele12, 47, 48, in the atherogenic ApoE knockout (PdgfdlacZ/lacZ, Myh11CreERT2, ROSAfloxtdT/+, ApoE−/−, designated KO). Lineage tracing allows for highly efficient and permanent labeling of smooth muscle cells, and their progeny, with tdT during subsequent cell state changes 12, 15, 16. Both Pdgfd KO and control (Pdgfd+/+, Myh11CreERT2, ROSAtdT/+, ApoE−/−, designated as Ctl) mice were administrated tamoxifen at the age of 8 weeks, followed by high-fat diet (HFD) feeding for 16 weeks to induce atherosclerosis (Fig. 3A). We did not observe significant differences in total body weight with HFD feeding compared to wild-type control mice as reported previously 44. Atherosclerotic lesions in the aortic roots were dissected, tissue digested, and isolated cells subjected to FACS to separate aortic tdT positive and negative cells from both KO (three groups, two mice each group) and Ctl mice (two groups, two mice each group), employing methods that we have previously described 12. Cells were captured with the 10X Genomics Chromium microfluidics device and libraries generated and sequenced as described (Fig. 3A) 12.
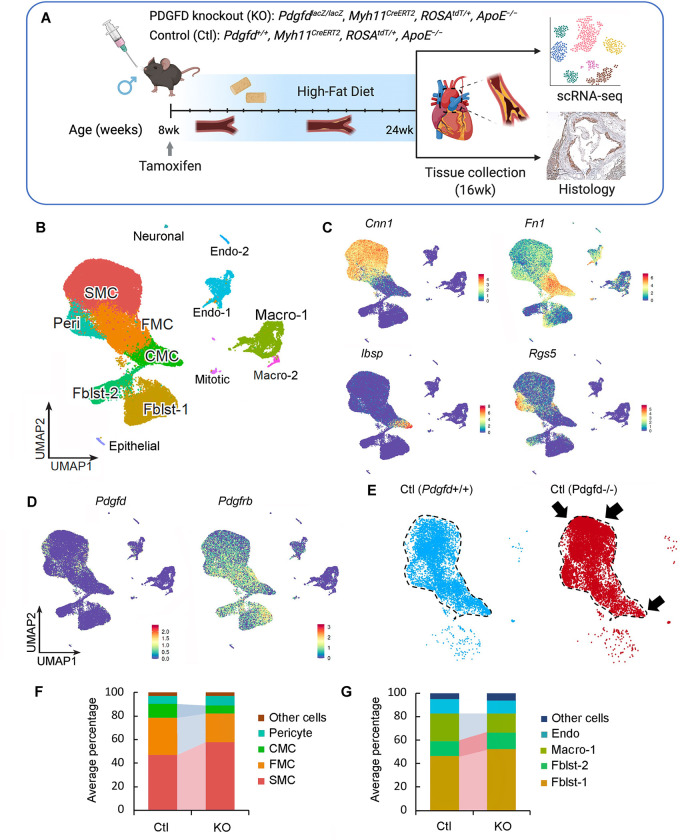
Figure 3. Single-cell transcriptomic profiling of mouse atherosclerotic aortic root in Pdgfd KO mice.
(A) Schematic of experimental design showing that dissected aortic tissues were harvested for single cell RNA sequencing (scRNAseq) and histology analyses from SMC-specific lineage tracing control (Ctl) and lineage tracing Pdgfd knockout (KO) mice. Eight-week-old mice, 2 Ctl and 3 KO captures (two mice per capture), were treated with tamoxifen twice at 3-day intervals and subsequently fed high fat diet for 16 weeks and then sacrificed. Tissues were digested to single cells, tdTomato positive (tdT+) fluorescence and negative (tdT−) cells collected and captured on the10x Chromium controller, libraries generated and sequenced. (B) Uniform manifold approximation and projection (UMAP) of scRNAseq results identified 13 different clusters at 2.6 clustering resolution, with respective biological cluster identities as defined by cluster marker genes. (C) UMAP displaying expression of indicated markers reflecting unique cluster identity: Cnn1, SMC; Fn1, FMC; Ibsp, CMC; Rgs5, pericytes. (D) UMAP visualizing dimension reduction plots of Pdgfd and Pdgfrb expression. (E) UMAP images comparing feature expression of tdTomato positive cells from Ctl and KO mice. The dotted line is generated based on the Ctl image. (F) Bar plot presenting the average percentage of lineage traced cells and (G) non-lineage traced cells in Ctl and KO groups.
After quality control assessment, scRNAseq data were visualized using uniform manifold approximation and projection (UMAP) dimensionality reduction plots (Fig. 3B). Unsupervised clustering analysis at the optimal 2.6 resolution parameter identified a total of 13 clusters and cell-specific markers used to identify cluster lineages (Figs. 3B, Suppl. Figs. 3A – 3C, Suppl. Table 1). Lineage traced cells were identified by tdT expression and noted to contribute to four separate clusters as we have described previously: SMC, fibroblast-like fibromyocytes (FMC), endochondral bone like chondromyocytes (CMC), as well as pericytes 15, 16. Quiescent and transition SMC clusters were readily separated from other clusters with low resolution parameters. At this resolution, endothelial cells, and fibroblasts each contributed to two separate clusters, Endo-1 vs Endo-2 and Fblst-1 vs Fblst-2 respectively, as previously described 15, 16. Feature plots (Figs. 3C, 3D) and violin plots (Suppl. Fig. 3D) were employed to visualize the cluster-specific expression of Pdgfd and Pdgfb, as well as Pdgfra and Pdgfrb. In lineage traced cells in control tissue, Pdgfd was expressed in SMC and FMC, but showed lower expression levels in CMC. In non-SMC lineage cells, there was robust expression in pericytes, Endo-1 and epithelial cells, and modest expression in fibroblasts. Interestingly, Pdgfrb was expressed in all SMC lineage cells, including the CMC, as well as Fblst-1, Fblst-2 and pericyte cluster cells. Knockout of Pdgfd produced an apparent increase in SMC and decrease in transition CMC (Fig. 3E), and also a modest decrease in Pdgfrb expression in all cells expressing significant levels of Pdgfd (Suppl. Fig. 3E). We also analyzed the average expression of Pdgfra as well as other PDGF ligands Pdgfa and Pdgfb but found no significant change in their expression level in vascular cells (Suppl. Fig. 3E).
To examine changes in relative cluster cell numbers, we measured the average percentage of cells in different clusters separately for lineage traced and non-lineage traced cells (Figs. 3F, 3G). In traced cells, loss of Pdgfd increased the relative proportion of differentiated SMC but decreased FMC and CMC cluster numbers. Importantly, in non-lineage cells, loss of Pdgfd resulted in a decrease in macrophage number. While this analysis indicated a relative increase in fibroblasts among non-tdT lineage traced cells, the absolute number was the same for both genotypes (0.47% versus 0.51%). Also, it is important to note that the relative representation of adventitial cells in scRNAseq experiments is highly variable due to differences in extent of adventitial tissue included in the aortic tissue isolation. Together, these data indicate that loss of Pdgfd inhibits SMC phenotypic transition and monocyte-macrophage recruitment during atherosclerosis development.
Pdgfd activates a broad gene expression program to establish SMC transition phenotypes and promote inflammatory pathway activation
Using the FindMarker algorithm of Seurat, we analyzed the scRNAseq data to identify genes that are differentially regulated with Pdgfd loss in comparison to control. Using a cutoff value set to 0.05 for the false discovery rate (FDR) q-value, a total of 165 transcripts were identified (Fig. 4A). While 58 transcripts were upregulated, 107 transcripts were downregulated, across all cellular phenotypes (Suppl. Table 2). Interestingly, more than half of upregulated genes belonged to quiescent SMC (38/58, 65.5%), whereas most of the down-regulated genes belonged to SMC-derived FMC (35/107, 32.7%) and CMC (11/107, 10.3%) as well as macrophage clusters (39/107, 36.4%). Two CMC markers, Col2a1 and Ibsp, were the most overall highly decreased transcripts (Suppl. Table S2). We found an increase in SMC differentiation markers, such as Acta2 and Tagln, but a decrease in FMC and CMC markers, such as Vcam1 and Col2a1, respectively. These data suggest that Pdgfd enhances SMC de-differentiation and phenotypic transition as well as monocyte-macrophage recruitment in the disease setting. Using the Molecular Signatures Database (MSigDB) molecular pathway enrichment tool, we predicted the Biological Pathways enriched with those up and down-regulated transcripts (Suppl. Fig. 4A). This pathway analysis identified highly significant immune related terms and cell-matrix interaction and vascular development terms as the top pathways associated with down- and up-regulated genes, respectively. We further examined the potential functional implication of differentially expressed genes between KO and Ctl tissues for disease pathogenesis. Differentially regulated genes were enriched and highly interconnected in disease categories related to fibrosis and aortic aneurysm formation (Fig. 4B), suggesting that these pathways overlap those involved in Pdgfd-mediated atherosclerosis.
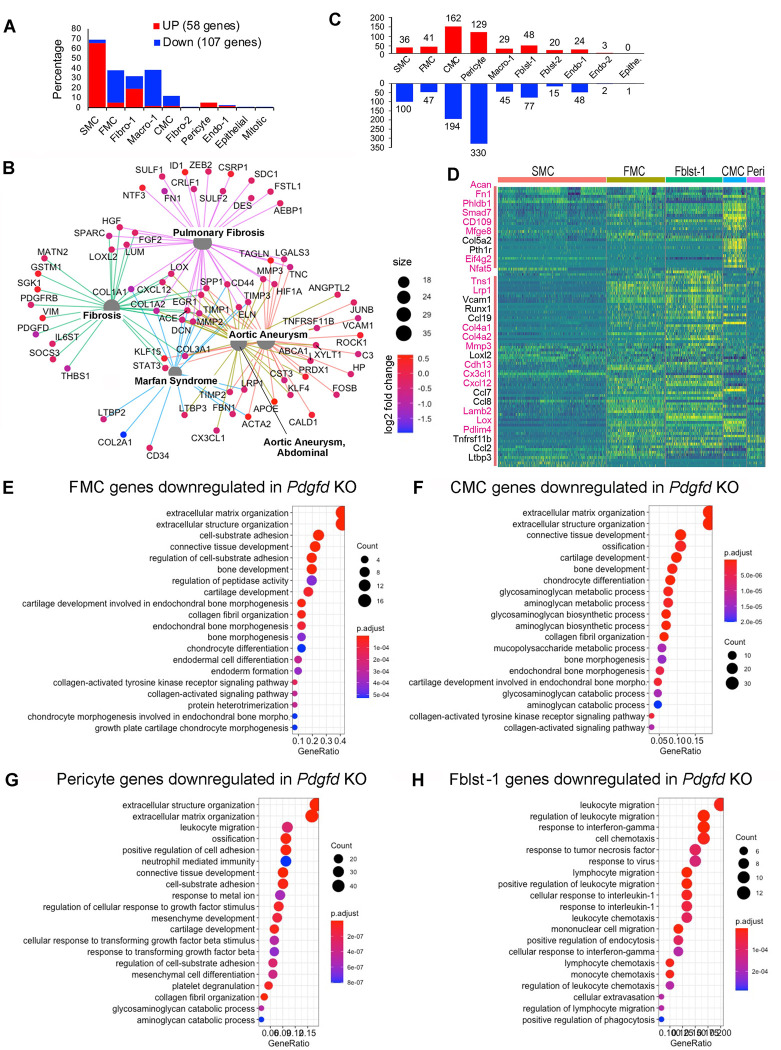
Figure 4. Loss of Pdgfd mitigates the smooth muscle cell chondrogenic transition and inflammatory pathway activation.
(A) Bar plot showing the number of upregulated genes (58, red bars) and down-regulated genes (107, blue bars) derived from all KO compared to all Ctl disease tissues. (B) Gene-disease network analysis of the differentially expressed genes (DEGs) among lineage traced cells in KO compared with Ctl as determined by enrichplot. (C) Bar plot displaying numbers of DEGs in individual clusters, for KO compared with Ctl. (D) Heatmap showing expression patterns of down-regulated DEGs across different cluster groups, based on fold-change of gene expression. Yellow color indicates differential expression, genes in red text reside in window of lead SNP ± 500 kilobases. (E-H) Graphs depicting gene set enrichment analysis underlying biological process of DEGs for (E) FMC, (F) CMC, (G) pericytes, and (H) Fibroblasts-1 as determined by clusterProfiler.
To examine how Pdgfd specifically affects gene expression in clusters of cells with similar phenotype, we dissected the number of differentially regulated genes in individual clusters comparing between KO and Ctl tissues (Figs. 4C, 4D, Suppl. Table 2). Enrichment of these genes in biological processes (BP) as annotated with gene ontology terms were identified separately for clusters of interest. SMC down-regulated genes identified terms related to extracellular matrix assembly and organization and TGFB pathway signaling (Suppl. Fig. 4B). FMC down-regulated genes were enriched for extracellular matrix terms, but importantly also genes related to early chondrogenic processes, as indicated by identification of terms “bone development“ and “cartilage development” (Fig. 4E). Genes downregulated in these pathways included Col1a1, Col2a1, Col5a1, Thbs1, Ccnd1, and Fbn1.
Down-regulated genes for the CMC transition phenotype were 4-fold greater in number than those identified for the FMC phenotype (Fig. 4C), and the differentially regulated genes assigned to pathways included Acan, Col2a1, Col10a1, Sox6, Pth1r, and Scrg1. The majority of GO BP terms enriched for CMC regulated genes in the Pdgfd KO vascular tissue reflected a prominent role for this growth factor in transition of SMC to a chondrogenic phenotype, including “ossification” and “chondrocyte differentiation” (Fig. 4F). Terms for this chondrogenic transition phenotype showed greater gene ratios and lower p-values compared to FMC gene pathways. Also, the heatmap of differentially regulated genes per cluster showed a significant difference between FMC and CMC gene expression (Fig. 4D). Interestingly, down-regulated genes for the CMC phenotype included a greater number of putative CAD GWAS genes compared to other clusters, including Acan, Fn1, Mfge8, Phldb1, Smad7, Cd109, Eif4g2, and Nfat5 3, 7, 8. There were an equally large number of downregulated genes in the Pdgfd knockout compared to wildtype CMC clusters, but these genes were not enriched in pathways that were informative regarding Pdgfd function or disease mechanisms. Pathways identified included “multicellular organism process” and “developmental process” among other general terms.
Pericytes showed the greatest number of down-regulated genes with Pdgfd deletion, and there was considerable overlap with SMC differentially expressed genes and pathways (Fig. 4G, Suppl. Table 2). Surprisingly, pericytes showed down-regulation of numerous genes also down-regulated in FMC, including Loxl2, Casp4, Col1a1, and Thbs1, as well as several CMC genes, including Timp3, Lox, Fgf2, Fgfr1, Col5a1, and Col5a2 (Fig. 4D). These differentially regulated genes contributed to enrichment of GO BP terms “extracellular matrix organization”, “positive regulation of cell adhesion”, and “ossification.” There was also down-regulation of leukocyte recruitment and adhesion molecules such as Cxcl1, Cxcl5, Cxcl12, Ccl19 and Alcam, providing enrichment for terms ”leukocyte migration” and “neutrophil mediated immunity.” Further, pericytes with deletion of Pdgfd showed a decrease in Tgfb2 expression, as well as genes related to Tgfb signaling, identifying terms “cellular response to Tgfb” and “response to Tgfb”. These data suggest that Pdgfd activates gene expression patterns in pericytes related to Tgfb signaling and those identified with SMC transition phenotypes.
Analysis of gene expression changes in the Fblst-1 cluster indicated that Pdgfd promotes a highly specific phenotypic program in these cells related to inflammatory cell recruitment (Figs. 4H, Suppl. Table 2). Pdgfd deletion was associated with down-regulation of a broad range of inflammatory mediators that interact with monocytes, neutrophils, T and B cells, including chemokines Ccl2, Ccl7, Ccl8, Ccl19, Cxcl12, Cxcl14, Cxcl16, proinflammatory cytokine Il6, and acute phase reactants C1s1, C3, and C4b. Interestingly, fibroblasts upregulated genes in Pdgfd KO cells related to SMC phenotype, including Acta2, Tagln, and Myl9, suggesting that Pdgfd may inhibit the transition of fibroblasts to the myofibroblast lineage, in favor of a more inflammatory phenotypic profile. To validate some of these results, we studied the expression of chemokines CCL2 and CCL7, as well as the PDGFRB gene, in the human lung fibroblast cell line, IMR-90, after treatment with PDGFD (Suppl. Figs. 5A–5C). These studies confirmed that the PDGFD signaling is functional in fibroblasts, as shown by down-regulation of PDGFRB receptor expression, and that these potent chemokines can be upregulated in human fibroblast cells in the context of PDGFD stimulation.
Although EC exhibited a limited number of genes differentially regulated with Pdgfd KO, they did downregulate expression of leukocyte adhesion molecules Icam1 and Selp, inflammatory mediator Il6st, and the monocyte chemotactic factor gene Ccl8. Cells in the macrophage cluster showed down-regulation of a limited number of genes, including inflammatory mediators Ccl8, Ccl12, and Ccr2. This is consistent with the finding that they express low levels of Pdgf receptors (Suppl. Fig. 3D).
Pdgfd promotes SMC phenotypic transition, expansion, and migration along with monocyte recruitment, but does not affect overall plaque burden
We next used histology methods to investigate the role of Pdgfd in atherosclerotic lesion features in the proximal aorta of the atherosclerosis mouse model. First, we employed X-gal staining to visualize the expression of the lacZ reporter gene integrated into the Pdgfd KO mouse genome 44. We observed Xgal stained areas corresponding to SMC that comprise the medial layer of the aorta (Fig 5A). Also, in the proximal aorta we observed patchy X-gal staining, and thus Pdgfd expression, in endothelial cells that lined the lumen of aortic regions with plaque. Interestingly, we also observed staining of endothelial cells lining the proximal coronary arteries, where SMC expression was not detected (Fig. 5A).
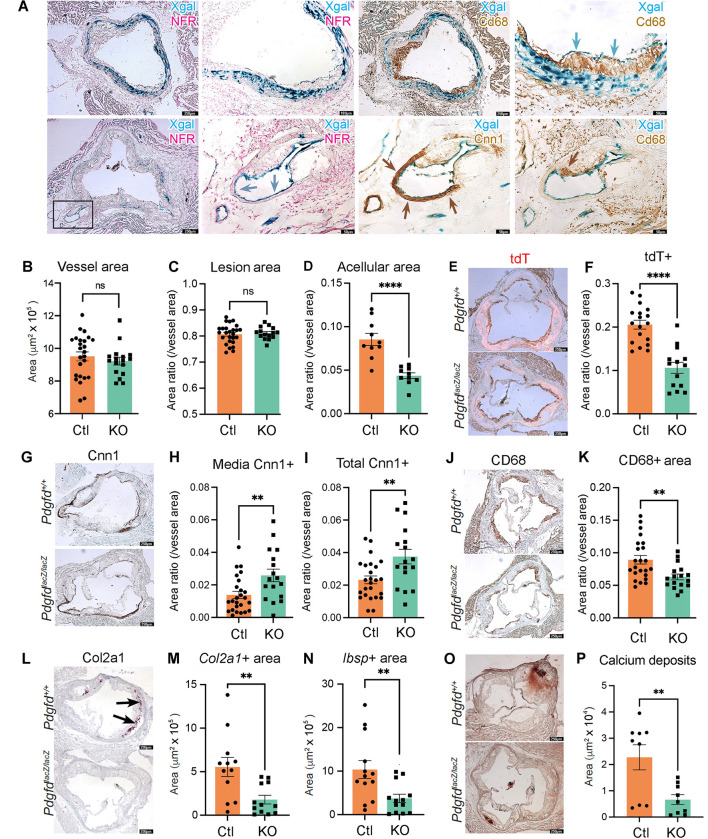
Figure 5. In situ studies of mouse atherosclerosis reveal that Pdgfd KO lessens SMC cell state transitions and inflammation but without impact on plaque burden.
(A) X-gal staining visualizing β-galactosidase activity (lacZ, blue precipitate) to determine the cellular location of Pdgfd expression in mouse model atherosclerosis. Aortic root sections were also stained with a generic nuclear marker nuclear fast red (NFR), immunohistochemistry for the Cd68 macrophage marker or Cnn1 marker for SMC identification. (B) Quantification of total vessel area. (C) Quantification of lesion, and (D) acellular areas in Ctl and KO groups expressed as a ratio of the total vessel area per section. (E) Representative images identifying expression of the tdTomato gene to visualize the SMC lineage traced cells in aortic sections. (F) Quantification of tdTomato positive (tdT+) area relative to total vessel area. (G) Representative sections stained for Cnn1, a marker of the differentiated SMC. (H) Quantification of Cnn1 positive (Cnn1+) area at the media, and (I) compared to total cross-sectional area expressed as a ratio of the total vessel area per section. (J) Representative images of Cd68-stained aortic root area to quantify monocyte recruitment. (K) Quantification of Cd68 positive (Cd68+) area relative to the vessel area. (L) Representative images of Col2a1 RNAscope of the aortic root in Ctl and KO mice. (M) Quantitative RNAscope of Col2a1 and (N) Ibsp expression. (O) Representative images stained for calcium deposits with alizarin Red S. (P) Quantification of calcium deposits. Each dot represents quantification from identical level sections from individual animals. Data expressed as mean ± s.e.m with p-values using an unpaired t-test. ** p<0.01, *** p<0.001.
We also used histology to investigate the effect of Pdgfd deletion on atherosclerotic lesion anatomy in the aortic root by comparing KO and Ctl tissues after 16-week of HFD. The overall vessel area was not different between KO and Ctl vessels (Fig. 5B), and lesion area was not significantly different when compared to whole vessel (Fig. 5C) or medial area (Suppl. Fig. 6A). However, there was a significant decrease in acellular area (Fig. 5D). While the cellular mechanism underlying the origin of these regions is not clear, we have correlated lesion acellular area to SMC transition to the CMC phenotype, where these cells are localized in the plaque 16. Importantly, we identified a highly significant decrease in total tdT lineage traced SMC in the vessel (Figs. 5E, 5F), and also in the plaque area (Suppl. Fig. 6B), suggesting that Pdgfd is responsible for promoting expansion of the SMC lineage cells and their migration into the plaque. To quantify changes in SMC content in the different vessel compartments in the Pdgfd KO compared to Ctl mice, we performed Cnn1 staining and immunoreactive area measurements. We found a modest mean increase in Cnn1 staining in the fibrous cap but this difference was not statistically significant (Suppl. Fig. 6C), but there was significantly increased staining in the medial layer, as well as the overall area of KO vessels (Figs. 5G – 5I). These results are consistent with findings in the scRNAseq data showing an increase in vessel number of differentiated contractile SMC. Plaque macrophage content as assessed with CD68 staining was decreased in the whole vessel (Figs. 5J, 5K) and specifically in the lesion area (Suppl. Fig. 6D) in the knockout mice, consistent with decreased monocyte recruitment. Also, expression of CMC markers Col2a1 and Ibsp were significantly decreased in KO lesions compared to Ctl littermates (Figs. 5L – 5N), and this decrease correlated to decreased aortic calcification as assessed with alizarin red S staining and quantification (Fig. 5O, 5P).
Taken together, these results support the scRNAseq findings and suggest two prominent mechanisms by which Pdgfd expression may promote disease risk. Pdgfd was found to promote de-differentiation of SMC, their migration into the plaque, and transition to the CMC phenotype, which we have correlated to disease risk 15, 16. Further, Pdgfd expression promotes monocyte-macrophage number in vascular lesions, presumably through recruitment, thus contributing to an inflammatory milieu. Surprisingly, these changes were not associated with a measurable effect on plaque burden.
Blocking Pdgfd function in the mouse atherosclerosis model validates the molecular and cellular mechanisms of disease risk
To verify the effects of PDGFD toward disease pathophysiology as identified with the constitutive Pdgfd mouse knockout model, we treated the lineage tracing atherosclerosis ApoE−/− mouse model with a murine derived inhibitory monoclonal antibody directed against Pdgfd (25E17, PD-ab) or with a control IgG (Ctl-ab) (Fig. 6A). Its blocking activity was validated with in vitro studies with human aortic smooth muscle cells, which showed decreased proliferation and migration in response to PDGFDD in the presence of antibody (Suppl. Fig. 7A, 7B). Our previous scRNAseq data indicated that Pdgfd RNA expression is low at baseline, and then increases with plaque progression and becomes prominent after 3 weeks of HFD feeding 12. Therefore, we started administration of PD-ab in 11-week-old animals that had received 3 weeks of HFD and continued treatment until sacrificing animals after either 8 weeks exposure to the diet (5 weeks antibody) or 16 weeks diet (13 weeks antibody), and conducted scRNAseq at these timepoints, using identical methods to those described for the Pdgfd KO. Differential gene expression was identified using a cutoff value set to 0.05 for false discovery rate (FDR) q-value, and this analysis was conducted across all clusters because of the small number of differentially expressed genes in the SMC lineage clusters with Pdgfd blockade versus control antibody treatment (Suppl. Table 3).
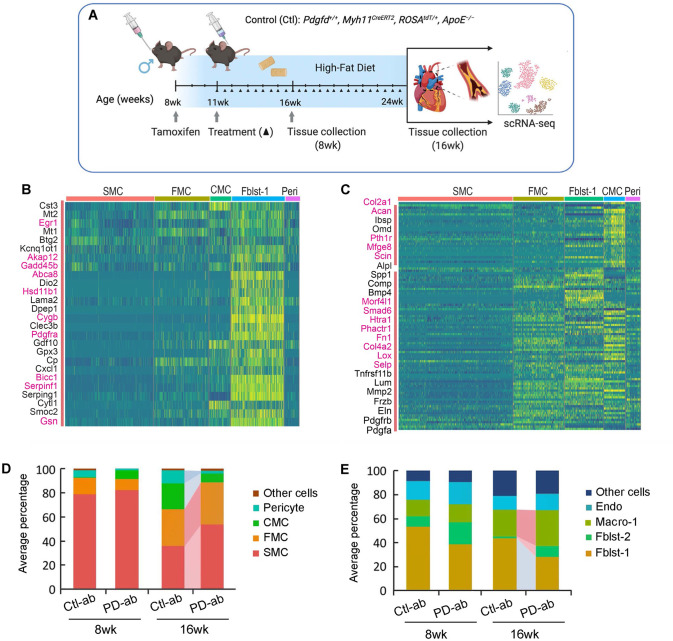
Figure 6. Single cell RNA-seq studies of antibody mediated Pdgfd knockdown in the mouse atherosclerosis model.
(A) Schematic of experimental design showing that SMC-specific lineage tracing widltype mice were treated with tamoxifen at 8 weeks age and tissues harvested after 8 and 16 weeks of high fat diet. Blocking Pdgfd antibody or isotype control antibody administration was initiated at 11 weeks and continued until animals were sacrificed after either 8 weeks exposure to the diet (5 weeks antibody) or 16 weeks diet (13 weeks antibody), and scRNAseq conducted at these timepoints. (B) Heatmap showing gene expression changes after 5 weeks of antibody treatment. The Fblst-1 cluster shows early downregulation of Pdgfd regulated genes, and FMC and CMC cluster cells beginning to show evidence of upregulation of these genes as the SMC lineage cells are undergoing phenotypic transition in the developing lesion. Yellow color indicates differential downregulation, genes in red text reside in window of lead SNP ± 500 kilobases. (C) Heatmap showing decreases in Pdgfd regulated genes across different cell clusters in targeted animals compared to controls. (D) Bar plot presenting the average percentage of lineage traced cells and (E) non-lineage traced cells in Ctl and KO groups.
A striking finding at the 8-week timepoint was the downregulation of genes in fibroblasts after 5 weeks of antibody treatment (Fig. 6B). These Fblst-1 genes which are upregulated by Pdgfd in the early disease setting included those related to extracellular matrix and migration (Lama2, Smoc2), proliferation and apoptosis (Btg2, Akap12, Gadd45b), endochondral bone formation and calcification (Gdf10, Serpinf1, Clec3b), chemotaxis (Cxcl1, Cytl1), and Pdgf signaling pathway (Pdgfra). Although not well represented in the heatmap, pericytes showed down-regulation of a number of immediate early genes including Fos, Fosb, Junb, Ier2, Ier3, and Egr1, suggesting an early effect on the response phenotype of these cells to Pdgfd stimulation. Upregulation of these genes would be expected if the differential expression was due to cellular stress conditions.
By 16 weeks of diet, there were extensive gene expression differences due to antibody blockade of Pdgfd protein function (Fig. 6C, Suppl. Table 3). The overall patterns of gene expression were similar to those identified with Pdgfd KO (Fig. 4D). Specific significant gene expression changes with Pdgfd Ab were most highly correlated with the knockout data for the CMC lineage phenotype, with 52 of the 89 Pdgfd Ab differentially down-regulated genes showing significant decreased expression with Ab treatment. Pathways identified with antibody blockade of Pdgfd were also highly similar to those identified with the KO studies. FMC pathways were again identified as those supporting extracellular matrix and endochondral bone formation, and also showing enrichment for Tgfb regulated genes (Suppl. Fig. 7C). CMC pathways were almost totally restricted to endochondral bone formation and ossification (Suppl. Fig. 7D). Pericyte genetic pathways identified with Pdgfd inhibition included those related to extracellular matrix organization and BMP signaling, with numerous different bone development pathways (Suppl. Fig. 7E). Inflammatory genes down-regulated in the Fblst-1 cells were enriched in vascular disease peptidase pathways 49, 50, and there was also enrichment for genes related to BMP signaling and bone development (Suppl. Fig. 7F).
Compared to Ctl-ab, PD-ab treatment induced suppression of SMC phenotypic transition as evidenced by a decreased relative number of CMC and increased number of SMC, and these effects were prominent after16-weeks of HFD (Fig. 6D). The modest increase in FMC could be due to reduced transition to the CMC phenotype. Also, after 16 weeks of HFD, the PD-ab significantly reduced the number of pericytes in lineage traced cells and Fblst-1 cells in the non-lineage analysis (Figs. 6D, 6E). Surprisingly, the relative number of macrophages was found to be increased, but this was due in large part to the decrease in fibroblast and pericyte number in this type of analysis.
Discussion
Signaling through the PDGF pathway is critical for the recruitment and expansion of mural vascular cell types during embryogenesis 26. Renewed expression of PDGF ligands in the setting of disease has been linked to similar SMC cell state changes, but disease pathophysiology has not been ascribed to these functions. Although most recently discovered and least studied, PDGFD is the only PDGF pathway gene identified thus far in a CAD GWAS locus. The highly vascular cell specific expression of this PDGF ligand and the fact that it binds the Pdgfrb receptor links it to the fundamental pathophysiology of atherosclerosis and specifically the contribution of the PDGF pathway to vascular wall cellular and molecular processes that promote CAD risk. In studies reported here we have linked CAD GWAS association at 11q22.3 to PDGFD expression and have proposed a transcriptional mechanism for this association involving another putative CAD GWAS gene FOXC1 that also has known regulatory roles in arterial development 51. We have shown that expression of Pdgfd in experimental animal models mimics much of the same features that mark the behavior of mural cell progenitors in embryonic development. In addition, in the disease setting Pdgfd produced by SMC and mural lineage cells promotes expression of chemokines to promote the recruitment of inflammatory cells to the plaque.
Experiments reported here employing scRNAseq transcriptomic analysis showed that constitutive deletion of Pdgfd led to increased expression of SMC lineage genes and down-regulation of CMC gene expression profiles, as well as decreased numbers of cells that fit the FMC and CMC marker gene profiles 16. Histology lesion analysis revealed that Pdgfd loss was associated with decreased total lineage traced cells in the vessel, decreased tdT positive cells in the lesion, and increased medial SMC number. Taken together, these data suggest that Pdgfd promotes SMC phenotypic modulation, proliferation, and migration into the plaque where SMC transition into modulated phenotypes. Previous data from the Owens lab has shown that Pdgfrb SMC-specific deletion resulted in loss of the majority of SMC in the lesion 28. While Pdgfd KO reveals a significant decrease in SMC migration into the plaque the phenotypic transition is obviously not as extensive, suggesting that Pdgfd contributes a substantial portion but not all of the migratory effect of Pdgf signaling, which is likely mediated through the Pdgfrb receptor. Despite these striking changes in vascular SMC phenotype, neither our studies of Pdgfd or the recent study of Pdgfrb showed a substantial effect on plaque burden in knockout mice for these two genes. Taken together these data suggest that SMC in general, and the PDGFD/PDGFRB signaling pathway, do not mediate CAD risk through altering extent of disease but rather through regulation of disease features that regulate vascular stability.
The embryonic paradigm suggests that PDGF ligands produced by endothelial cells promote the contribution of smooth muscle progenitor cells to expansion, migration, and contribution to vascular development, and the effects of this pathway in the disease setting seem analogous. In mouse, Pdgfd is expressed at modest levels by Endo-1 cluster cells, at least in those cells associated with disease plaque, and Pdgfrb expressed by a majority of all SMC phenotype cells (Figs. 5A, Suppl. Fig. 3D). This is consistent with the scRNAseq and lesion histology data indicating that loss or blockade of Pdgfd function is associated with decreased numbers of SMC transition cells, and that Pdgfd deletion is associated with a decreased number of SMC lineage cells in the plaque and decreased overall SMC lineage number. Our data indicate that any endothelial chemotactic effect on SMC lineage cells is not entirely due to Pdgfd, as the loss of Pdgfrb results in a much greater decrease in SMC contribution to plaque than seen with knockout of Pdgfd in these studies. Interestingly, Pdgfd is also expressed by SMC and FMC, which may contribute to expansion of the SMC lineage cells by an autocrine pathway, at least in the early stages of disease.
Despite the extensive evidence that inflammation is a key component of atherosclerosis, there has not been a large GWAS signal in loci harboring pro-inflammatory cytokines or chemokines, IL6R and CXCL12 loci being notable exceptions. In studies reported here we documented a greater number of lesion macrophages in Pdgfd expressing compared to knockout animals, and this correlated with a more prominent expression of inflammatory genes in adventitial cells in the wildtype lesions. Expression differences for both adventitial fibroblasts and pericytes identified down-regulated genes in the Pdgfd KO mice that were highly enriched for cytokine and chemokine chemotaxis mediators, with highly significant p-values and high relative numbers of represented genes per pathway. Compared to Pdgfd KO cells, wildtype pericytes were found to express genes related to leukocyte migration but also genes associated with FMC-like pathways such as extracellular matrix organization, and CMC-like pathways, including those related to ossification, suggesting that in the context of vascular disease processes and Pdgfd stimulation pericytes adopt a phenotypic modulation not unlike medial disease associated SMC. The inflammatory response to Pdgf signaling in mural cells has been reported previously, most notably in an elegant series of studies by Olson et al. with constitutive activation of the Pdgfrb receptor in transgenic mouse models 52. Whether these gene expression changes in fibroblasts and pericytes reflect activation by Pdgfd emanating from the plaque cells or adventitial cells could not be addressed with this constitutive Pdgfd knockout model. The precise mechanisms by which chemokines expressed by adventitial cells might contribute to increased leukocyte trafficking to the plaque are not well understood, but a role for activated pericytes has been reported in the recruitment of immune cells to the vascular wall to promote inflammation and mitigate tumor growth 52, 53. Interestingly we saw only minimal changes in macrophage gene expression with Pdgfd KO, similar to findings in the Smad3 KO where we did not see a significant number of DE genes with loss of Smad3 expression 16. Thus, the effect of this cell lineage on plaque anatomy may be primarily one of regulation of monocyte-macrophage number and not phenotype. We propose that PDGFD is an important contributor to the inflammatory cell milieu in the plaque, and that this mechanism accounts at least in part for its contribution to CAD risk.
SMC contribute the greatest portion of genetic attributable risk among all cells that participate in the vascular disease process, including endothelial, macrophage, T-cells, etc. 9. For genome wide significant genes that we have studied thus far, TCF21, ZEB2, AHR, and SMAD3, all inhibit disease risk. PDGFD is the first gene that we have studied that would promote disease risk, so comparison with other CAD disease genes expressed in SMC is important. The marked difference between the SMC transition program of these other CAD genes and PDGFD is that they promote transition primarily to the FMC phenotype or inhibit or fundamentally alter the CMC transition, while PDGFD promotes the SMC transition to cells that exhibit a CMC phenotype. An important corollary is that Pdgfd also promotes vascular calcification, e.g., while CAD risk inhibiting Smad3 gene mitigates against vascular calcification. This is expected to contribute to detrimental features of plaque stability. Similar to TCF21 and the other protective CAD genes, PDGFD also increases transition to the FMC phenotype, but any beneficial effects of this function may be offset by an increase in the risk related CMC phenotype. Further work is required to better understand the trajectories that usher cells into and through the FMC phenotype.
Finally, it is important to mention the limitations of these studies. While all human genetic data and a variety of fine mapping approaches point to rs2019090 and PDGFD as the disease CAD effectors at 11q22.3, there is considerable variation regarding which alleles at this locus promote disease risk and PDGFD expression. For instance, in early CAD GWAS studies the T allele was identified as promoting disease risk and PDGFD expression 29, while subsequent studies have primarily established that A is the CAD risk allele, and both GTEx and STARNET data reported as showing the A allele as also promoting PDGFD expression 31. Despite GTEx eQTL findings reported here, our original analysis of STARNET data had identified the T allele as promoting PDGFD expression 30. However, the accumulated human genetic data along with in vitro transcriptional studies reported here convincingly show that FOXC1/C2 binding at the A allele of rs2019090 promotes both disease risk and PDGFD expression. In addition, we point out the limitations of our constitutive Pdgfd knockout model, which may not fully or accurately reflect the in vivo role of this gene in disease, due to compensation during embryogenesis or in the disease environment. However, antibody blocking studies provide compelling evidence that genetic and cellular disease related functions of this factor are accurately represented.
Methods
Colocalization analyses
Genomic location figures were generated in the UCSC Genome Browser. Visualization of CAD GWAS association and PDGFD expression quantitative trait loci was performed with locuscompare.com, as created by the Stephen Montgomery lab, Stanford. We conducted formal colocalization analysis using the fastEnloc method, with the meta-analysis results between CARDIoGRAMplusC4D and UK Biobank from van der Harst 6 and aortic artery eQTL from GTEx v8 35. For GWAS data, we generated posterior inclusion probability (PIP) using torus. For eQTL, we used the precomputed PIP provided by fastEnloc. The GWAS and eQTL PIPs were used as input to fastEnloc for colocalization analysis. We selected a regional level colocalization probability (RCP) of 0.2 as the cutoff to select significant colocalization between the GWAS and eQTL.
CRISPRi epigenome editing at rs2019090
Both dCas9-KRAB and single guide RNA sequences were cloned together into a lentiviral vector, virus packaged, and transduced into rs2019090 genotype AA homozygous HCASMC. After 6 hours of virus infection, cells were refreshed with a complete medium and incubated for 3 days. RNA was then extracted, converted to cDNA, and analyzed using qPCR for expression of PDGFD and lncRNA AP002989.1.
Culture of human coronary artery smooth muscle cell (HCASMC)
Primary HCASMCs were purchased from Cell Applications, Inc (San Diego, CA) and were cultured in complete smooth muscle basal media (Lonza, #CC-3182) according to the manufacturer’s instructions. All experiments were performed with HCASMC between passages 5–8. Rat aortic smooth muscle cells (A7r5) and human embryonic kidney 293 cells (HEK293) were purchased from ATCC and cultured in Dulbecco’s Modified Eagle Medium (DMEM) high glucose (Fisher Scientific, #MT10013CV) with 10% FBS at 37 °C and 5% CO2. A7r5 at passage 6–18 were used for experiments. IMR90 fetal lung fibroblasts at passage 7 were cultured in FGM-2 lung fibroblast basal media (Lonza, #CC-3131) according to the manufacturer’s instructions.
Knockdown and over-expression
For the siRNA transfection, cells were grown to 30% confluence, then treated with siRNA or scramble control to a final concentration of 20nM with RNAiMax (Invitrogen, Carlsbad, CA). The siRNAs for PDGFD were purchased from Origene (SR312885), and an equimolar combination of SR312885B and SR312885C employed. siRNA for AP002989.1 was purchased from Dharmacon (SO-2964013G), and an equimolar combination of NGUTJ-000031 and NGUTJ-000033 were used for knockdown. Two different types of siRNAs for FOXC1 and FOXC2 were purchased from Thermo Fisher Scientific: Silencer (ASSAY ID #41733 for FOXC1, # s194416 for FOXC2), and Stealth (ASSAY ID #HSS142037 for FOXC1 and #HSS142054 for FOXC2) reagents. Cells were treated with an equimolar combination of Silencer and Stealth and collected 72 hours after transfection. For the overexpression study, viruses were produced with 8.5 × 105 HEK293T cells plated in each well of a 6-well plate. The following day, plasmid encoding lentivirus was co-transfected with pMD2.G and pCMV-dR8.91 into the cells using Lipofectamine 3000 (Thermo Fisher, L3000015) according to the manufacturer’s instructions. ViralBoost Reagent (AllStem Cell Advancements, VB100) was added (1:500) with fresh media after 5 hours. Supernatant containing viral particles was collected 72 hours after transfection and filtered. HCASMC were transduced with 2nd generation lentivirus with cDNAs cloned into pWPI (Addgene, 12254) using NEBuilder HiFi cloning (New England Biolabs). Cells were treated at 60% confluence with lentivirus for 5 to 24 hours. The virus was removed and replaced with fresh media 48 hours prior to collection for downstream applications. For PDGFD treatment study, IMR90 fibroblasts at 70–80 % confluent were serum starved overnight and treated with 50ng/ml of recombinant human PDGF-DD (R&D system, 1159-SB-025) for 24h.
For evaluation of the effect of knockdown and over-expression of FOXC1/2 on expression of endogenous genes, we normalized experimental results to the empty vector control results for each genotype group. This was necessary due to variation in the specific features of the individual genotype lines, such as transfection efficiency and transduction efficiency for these primary cultured human cells. All control values became one, and relative target expression thus determined. The t-test was performed between control and target within each genetic background for the reasons noted. These results, showing only the normalized target data and p-values, were presented in the final graph for presentation purposes.
RNA isolation and qRT-PCR
RNA was isolated using RNeasy plus micro kit (Qiagen, #74034) and total cDNA was prepared using High-capacity RNA-to-cDNA kit (Life Technologies, #4388950). Gene expression was assessed using TaqMan qPCR probes (Thermo Fisher) for PDGFD (Hs00228671_m1), AP002989.1 (hs04980451_m1), FOXC1 (Hs00559473_s1), FOXC2 (Hs00270951_s1), PDGFRA (Hs00998018_m1), PDGFRB (Hs01019589_m1), CCL2 (Hs00234140_m1), and CCL7 (Hs00171147_m1) according to the manufacturer’s instructions on a ViiA7 Real-Time PCR system (Applied Biosystems, Foster City, CA). Relative expression was normalized to GAPDH (Thermo Fisher Sci., #4310884E) levels.
Dual luciferase assays
FOXC1 or FOXC2 cDNAs were cloned into pWPI and transfect into A7R5 cells along with reporter constructs containing 3 copies of a 150 bp fragment encoding PDGFD locus sequence for the A allele (rs-2019090-A) or T allele (rs-2019090-T) at rs2019090. A7r5 cells were seeded into 24 well plate (1.5×104 cells/well) in DMEM containing 10% FBS and incubated at 37 °C and 5% CO2 overnight. Cells were transfected with luciferase reporter plasmids (pLuc-MCS (empty), pLuc-Ax3, or pLuc-Tx3), cDNAs (pWPI (empty), pWPI-FOXC1 or pWPI-FOXC2), and Renilla luciferase plasmid using Lipofectamine 3000 (Invitrogen, #L3000015). Six hours after transfection, the media was changed to fresh complete media. Relative luciferase activity (firefly/Renilla luciferase ratio) was measured by SpectraMax L luminometer (Molecular Devices) 24 hours after transfection. All experiments were conducted in triplicate and repeated at least 4 times.
Mouse strains
For the unbiased fate mapping of SMCs with Pdgfd loss during disease progression, the PdgfdlacZ/lacZ mouse strain obtained from Dr. Eriksson 44 was crossed with an SMC-specific lineage tracing ApoE−/− tandem dimer Tomato (tdT) fluorescent marker mouse model 12. BAC transgenic mice that express a tamoxifen-inducible Cre recombinase driven by the SMC-specific Myh11 promoter (TgMyh11-CreERT2, JAX# 019079) were bred with a floxed tandem dimer tomato (tdT) fluorescent reporter line (B6.Cg-Gt(ROSA)26Sortm14(CAGtdTomato)Hze/J, JAX# 007914) to allow SMC-specific lineage tracing. Mice were bred onto the C56BL/6, ApoE−/− background. Final genotypes of SMC lineage-tracing control (Ctl) mice were: Pdgfd+/+, Myh11CreERT2, ROSAtdT/+, ApoE−/−. Final genotypes of SMC lineage-tracing, Pdgfd KO mice were: PdgfdlacZ/lacZ, Myh11CreERT2, ROSAtdT/+, ApoE−/−. As the Cre-expressing BAC was integrated into the Y chromosome, all lineage tracing mice in the study were male. The animal study protocol was approved by the Administrative Panel on Laboratory Animal Care (APLAC) at Stanford University.
Induction of lineage marker by Cre recombinase
All mice received two doses of tamoxifen, at 0.2 mg/g−1 bodyweight, at a three day of interval by oral gavage at 8 weeks of age to activate Myh11-Cre, before the HFD (Dyets, #101511, 21% anhydrous milk fat, 19% casein and 0.15% cholesterol) was initiated.
Mouse aortic root/ascending aorta cell dissociation
After 16 weeks of HFD for Pdgfd KO model experiments, or 8 weeks and 16weeks HFD for PDGFD antibody experiments, animals were sacrificed and perfused with phosphate buffered saline (PBS). The aortic root and ascending aorta were excised, up to the level of the brachiocephalic artery, and washed three times in PBS. Collected tissues were placed into an enzymatic dissociation cocktail (2 U ml−1 liberase, Sigma–Aldrich #5401127001; 2 U ml−1 elastase, (Worthington, #LS002279) in Hank’s Balanced Salt Solution (HBSS)) and minced. After incubation at 37 °C for 1 h, the cell suspension was strained, pelleted by centrifugation at 500 × g for 5 min, and resuspended in fresh HBSS. For each scRNA capture, two mice were pooled as a group. Three and two separate pairs of isolation were performed for Ctl and Pdgfd-KO mice, respectively. Two separate pairs of isolations were performed for mice treated with control antibodies (Ctl-ab) or Pdgfd antibodies (PD-ab).
FACS of mouse aortic root/ascending aorta cells
Cells were sorted by fluorescence-activated cell sorting (FACS), on a BD Aria II instrument, based on tdTomato expression. tdT+ cells (considered to be of SMC lineage) and tdT− cells were captured on separate but parallel runs of the same scRNAseq workflow, with gating strategy and threshold identical to those published in previous work 12, and datasets were later combined for all subsequent analyses.
Single cell capture and library preparation
All single cell capture and library preparation was performed at the Stanford Functional Genomics Facility (SFGF). Cells were loaded into a 10X Genomics microfluidics chip and encapsulated with barcoded oligo-dT-containing gel beads using the 10X Genomics Chromium controller according to the manufacturer’s instructions. Single-cell libraries were then constructed according to the manufacturer’s instructions. Libraries from individual samples were multiplexed into one lane prior to sequencing on an Illumina platform with targeted depth of 50,000 reads per cell.
Preparation of mouse aortic root sections
Immediately after sacrifice, mice were perfused with 0.4% PFA. The mouse aortic root and proximal ascending aorta, along with the base of the heart, was excised and immersed in 4% PFA at 4 °C for 12 hours. After passing through a sucrose gradient, tissue was frozen in OCT to make blocks. Blocks were cut into 7μm-thick sections for further analysis.
Immunohistochemistry and calcification assay
Slides were prepared and processed according to standard IHC protocol. Sections were incubated overnight at 4 °C with an anti-Cnn1 rabbit monoclonal primary antibody (1:400 dilution; TA327614; Origene), or a CD68 rabbit polyclonal antibody (1:300 dilution; ab125212; Abcam), after development with Dab, samples were mounted with EcoMount medium (Biocare Medical #EM897L). The processed sections were visualized using a Leica DM5500 microscope and images were obtained using Leica Application Suite X software. Areas of interest were quantified using ImageJ (NIH) software and compared using a two-sided t-test. Lesion size was defined by the area encompassing the intimal edge of the lesion to the border of Cnn1 positive intimal-medial junction. All area quantification was performed in a genotype blinded fashion with ImageJ using length information embedded in exported files. Cells near the caps were defined as cells within 30um of the lumen, as previously defined 13. All biological replicates for each staining were performed simultaneously on position-matched aortic root sections to limit intra-experimental variance.
In situ assessment of lesion calcification in plaque sections was performed with 1% alizain red s solution as per established protocol 54 and quantitation performed as described for immunohistochemistry studies.
RNAscope assay
Slides were processed according to the manufacturer’s instructions, and all reagents were obtained from ACD Bio (Newark, CA). Sections were incubated with commercially available probes against mouse Col2a1 (#407221), Ibsp (#415501), or a negative control probe (#310043) for 2 hrs at 40 °C. Colorimetric assays were performed per the manufacturer’s instructions.
Analysis of scRNAseq data
Fastq files from each experimental group and mouse genotype were aligned to the reference genome (mm10) individually using CellRanger Software (10x Genomics). Individual datasets were aggregated using the CellRanger aggr command without subsampling normalization. The aggregated dataset was then analyzed using the R package Seurat v4.1.1 55. The dataset was trimmed of cells expressing fewer than 500 genes, and genes expressed in fewer than 50 cells. The number of genes, number of unique molecular identifiers and the percentage of mitochondrial genes were examined to identify outliers. As an unusually high number of genes can result from a ‘doublet’ event, in which two different cell types are captured together with the same barcoded bead, cells with >6000 genes were discarded. Cells containing >7.5% mitochondrial genes were presumed to be of poor quality and were also discarded. The gene expression values then underwent library-size normalization and normalized using established Single-Cell-Transform function in Seurat. Principal component analysis was used for dimensionality reduction, followed by clustering in principal component analysis space using a graph-based clustering approach via the Louvain algorithm. UMAPs were used for two-dimensional visualization of the resulting clusters. Analysis, visualization and quantification of gene expression and generation of gene module scores were performed using Seurat’s built-in functions such as “FeaturePlot”, “VlnPlot”, “DimPlot”, “DotPlot”, “DoHeatmap”, “FindMarkers”, and “AverageExpression”. Heatmaps were generated with normalized data, based on top 40 differentially down-regulated genes in individual clusters, except for the 8-week antibody treatment heatmap which was based on all differentially down-regulated genes across all cells in that dataset. Putative CAD associated genes were identified as those residing in a window of lead SNP ± 500 kilobases, drawing association data from the recent Million Veterans Program data analyses 8. DAVID / GSEA analyses were performed using a web-based platform at David.ncifcrf.gov and gsea-msigdb.org.
Pdgfd blocking antibody generation and in vitro effects on human SMC
Mouse IgG1 anti-PDGFD monoclonal antibodies were generated by immunizing Pdgfd knockout mice with mature recombinant human PDGFD. Hybridoma clones were screened for binding antibodies to both human and mouse PDGFD. High affinity binders were screened for blocking PDGFD-mediated tyrosine 751 phosphorylation of the PDGFR beta expressed by mouse cardiac fibroblast, human osteosarcoma, and human aorta vascular smooth muscle cells. High potency blockers were screened for high selectivity over PDGFB and PDGFC binding. An isotype matched mouse IgG1 antibody that does not bind a mammalian protein served as a control antibody. Antibodies were formulated in 10 mM sodium acetate, 9% sucrose, pH 5.2, and administered at 10 mg/kg subcutaneously twice per week.
Pdgfd antibody blockade of SMC proliferation –
Human aortic smooth muscle cells (HASMC) were plated at 5000 cells per well in 96-well plates and left to attach and spread for 30 hours. Cells were then washed with serum free media 2 times and incubated in serum free media for 6 hours. PDGF-DD (R&D systems, #1159-SB) was solubilized in 4mM HCl (Vehicle). PDGF-DD (17.85nM) was preincubated for 20 mins with or without anti-PDGF-DD antibody 25E17 (35.7nM) in serum free medium. Cells were treated with PDGF-DD with or without antibody in serum free media. Vehicle was added in control wells. Live cell proliferation was measured with the Incucyte Live-Cell Analysis system (Essen Bioscience). All data is expressed as the mean ± standard error of the mean (SEM). Statistical analysis performed using a repeated measures one-way ANOVA with Tukey correction.
Pdgfd antibody blockade of SMC migration –
Human aortic smooth muscle cells (HASMC) were plated at 8000 cells per well in upper chamber of 96-well transmigration plates from Incucyte (cat # 4648) and left to attach and spread for 30 hours. Cells were then washed with serum free media 2 times and incubated in serum free media for 12 hours. PDGF-DD (R&D systems, #1159-SB) was solubilized in 4mM HCl (Vehicle). PDGF-DD (17.85nM) was preincubated for 20 mins with or without anti-PDGF-DD antibody 25E17 (35.7nM) in serum free medium. PDGF-DD with or without antibody was added to the lower chamber of transmigration plates. Vehicle was added in control wells. Live cell migration was measured with the Incucyte Live-Cell Analysis system (Essen Bioscience). All data is expressed as the mean ± standard error of the mean (SEM). Statistical analysis performed using a repeated measures one-way ANOVA with Tukey correction.
Statistical analysis
All statistical analyses were conducted using GraphPad Prism software version 9. Difference between two groups were determined using an unpaired two-tailed Student’s t-test. Differences between multiple groups were evaluated by one-way analysis of variance (ANOVA) followed by Dunnett’s post-hoc test after the sample distribution was tested for normality. P values <0.05 were considered statistically significant. All error bars represent standard error of the mean. Number of stars for the P-values in the graphs: *** P <0.001; ** P <0.01; * P <0.05.
Supplementary Material
Acknowledgements
The authors express their deepest gratitude to Dr. Eriksson at the Karolinska for providing the constitutive Pdgfd knockout mouse. In addition, we thank Haiyue Meng and Yujiao Luo for their help in making the colocalization plot, and Dr’s Jae Lee, Aaron Winters, Chadwick King, and Chris Paszty for identification of the Pdgfd blocking antibody.
Sources of funding
This work was supported by National Institutes of Health grants K08HL153798 (PC), F32HL160067 (CW), L30HL159413 (CW), R01HL134817 (TQ), R01HL139478 (TQ), R01HL156846 (TQ), R01HL151535 (TQ), R01HL145708 (TQ), UM1 HG011972 (TQ), as well as a Human Cell Atlas grant from the Chan Zuckerberg Foundation. This work was also supported by a grant from the American Heart Association 20CDA35310303 (PC) and Amgen, Inc. (TQ).
Footnotes
Disclosures: CSW is a consultant for Tensixteen Bio and Renovacor, TQ is a consultant for Saliogen, and a member of the Cardiometabolic Scientific Advisory Board of Amgen. This work was supported in part by Amgen, Inc.
Supplemental Table 1. Top 30 mouse cell cluster markers distinguishing each cluster (reference cluster) from the remaining clusters.
Supplemental Table 2. Differentially regulated genes per cluster in Pdgfd knockout compared to widltype animals.
Supplemental Table 3. Differentially regulated genes per cluster in Pdgfd antibody treated compared to widltype animals.
Data availability
Data generated through these studies have been uploaded to the Gene Expression Omnibus (GSE214423) and will become publicly available coincident with publication of this manuscript.
References
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 3, e442 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roth GA, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation 132, 1667–1678 (2015). [DOI] [PubMed] [Google Scholar]
- 3.Erdmann J, Kessler T, Munoz Venegas L, Schunkert H. A decade of genome-wide association studies for coronary artery disease: the challenges ahead. Cardiovasc Res 114, 1241–1257 (2018). [DOI] [PubMed] [Google Scholar]
- 4.Klarin D, et al. Genetic analysis in UK Biobank links insulin resistance and transendothelial migration pathways to coronary artery disease. Nat Genet 49, 1392–1397 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelson CP, et al. Association analyses based on false discovery rate implicate new loci for coronary artery disease. Nat Genet 49, 1385–1391 (2017). [DOI] [PubMed] [Google Scholar]
- 6.van der Harst P, Verweij N. The Identification of 64 Novel Genetic Loci Provides an Expanded View on the Genetic Architecture of Coronary Artery Disease. Circ Res 122, 433–443 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aragam KG, et al. Discovery and systematic characterization of risk variants and genes for coronary artery disease in over a million participants. medRxiv, 2021.2005.2024.21257377 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tcheandjieu C, et al. A large-scale multi-ethnic genome-wide association study of coronary artery disease. Nat Medicine 28, 1679–1692 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turner AW, et al. Single-nucleus chromatin accessibility profiling highlights regulatory mechanisms of coronary artery disease risk. Nat Genet 54, 804–816 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu Y, Kovacic JC. Endothelial to Mesenchymal Transition in Health and Disease. Annu Rev Physiol, (2022). [DOI] [PubMed] [Google Scholar]
- 11.Alencar GF, et al. The Stem Cell Pluripotency Genes Klf4 and Oct4 Regulate Complex SMC Phenotypic Changes Critical in Late-Stage Atherosclerotic Lesion Pathogenesis. Circulation 142, 2045–2059 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wirka R, et al. Single cell analysis of smooth muscle cell phenotypic modulation in vivo reveals a critical role for coronary disease gene TCF21 in mice and humans. Nat Med 25, 1280–1289 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim JB, et al. The Environment-Sensing Aryl-Hydrocarbon Receptor Inhibits the Chondrogenic Fate of Modulated Smooth Muscle Cells in Atherosclerotic Lesions. Circulation 142, 575–590 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pan H, et al. Single-Cell Genomics Reveals a Novel Cell State During Smooth Muscle Cell Phenotypic Switching and Potential Therapeutic Targets for Atherosclerosis in Mouse and Human. Circulation, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng P, et al. ZEB2 Shapes the Epigenetic Landscape of Atherosclerosis. Circulation, (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheng P, et al. Smad3 regulates smooth muscle cell fate and mediates adverse remodelling and calcification of the atherosclerotic plaque. Nature Cardiovascular Research in press, (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. The New England journal of medicine 352, 1685–1695 (2005). [DOI] [PubMed] [Google Scholar]
- 18.Andrae J, Gallini R, Betsholtz C. Role of platelet-derived growth factors in physiology and medicine. Genes Dev 22, 1276–1312 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hu W, Huang Y. Targeting the platelet-derived growth factor signalling in cardiovascular disease. Clin Exp Pharmacol Physiol 42, 1221–1224 (2015). [DOI] [PubMed] [Google Scholar]
- 20.Ross R, Glomset J, Kariya B, Harker L. A platelet-dependent serum factor that stimulates the proliferation of arterial smooth muscle cells in vitro. Proc Natl Acad Sci U S A 71, 1207–1210 (1974). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ross R, Vogel A. The platelet-derived growth factor. Cell 14, 203–210 (1978). [DOI] [PubMed] [Google Scholar]
- 22.Heldin CH, Lennartsson J, Westermark B. Involvement of platelet-derived growth factor ligands and receptors in tumorigenesis. J Intern Med 283, 16–44 (2018). [DOI] [PubMed] [Google Scholar]
- 23.Heldin CH, Westermark B. Mechanism of action and in vivo role of platelet-derived growth factor. Physiol Rev 79, 1283–1316 (1999). [DOI] [PubMed] [Google Scholar]
- 24.Kazlauskas A. PDGFs and their receptors. Gene 614, 1–7 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muhl L, et al. Neuropilin 1 binds PDGF-D and is a co-receptor in PDGF-D-PDGFRbeta signaling. J Cell Sci 130, 1365–1378 (2017). [DOI] [PubMed] [Google Scholar]
- 26.Hellstrom M, Kalen M, Lindahl P, Abramsson A, Betsholtz C. Role of PDGF-B and PDGFR-beta in recruitment of vascular smooth muscle cells and pericytes during embryonic blood vessel formation in the mouse. Development 126, 3047–3055 (1999). [DOI] [PubMed] [Google Scholar]
- 27.Holmgren L, Glaser A, Pfeifer-Ohlsson S, Ohlsson R. Angiogenesis during human extraembryonic development involves the spatiotemporal control of PDGF ligand and receptor gene expression. Development 113, 749–754 (1991). [DOI] [PubMed] [Google Scholar]
- 28.Newman AAC, et al. Multiple cell types contribute to the atherosclerotic lesion fibrous cap by PDGFRbeta and bioenergetic mechanisms. Nat Metab 3, 166–181 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coronary Artery Disease Genetics C. A genome-wide association study in Europeans and South Asians identifies five new loci for coronary artery disease. Nat Genet 43, 339–344 (2011). [DOI] [PubMed] [Google Scholar]
- 30.Miller CL, et al. Integrative functional genomics identifies regulatory mechanisms at coronary artery disease loci. Nat Commun, 12092–12108 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deloukas P, et al. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet 45, 25–33 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nikpay M, et al. A comprehensive 1,000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat Genet 47, 1121–1130 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Strawbridge RJ, et al. Carotid Intima-Media Thickness: Novel Loci, Sex-Specific Effects, and Genetic Correlations With Obesity and Glucometabolic Traits in UK Biobank. Arterioscler Thromb Vasc Biol 40, 446–461 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hartiala JA, et al. Genome-wide analysis identifies novel susceptibility loci for myocardial infarction. Eur Heart J 42, 919–933 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Consortium GT. The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science 369, 1318–1330 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Consortium GT. Human genomics. The Genotype-Tissue Expression (GTEx) pilot analysis: multitissue gene regulation in humans. Science 348, 648–660 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Borkham-Kamphorst E, Meurer SK, Van de Leur E, Haas U, Tihaa L, Weiskirchen R. PDGF-D signaling in portal myofibroblasts and hepatic stellate cells proves identical to PDGF-B via both PDGF receptor type alpha and beta. Cell Signal 27, 1305–1314 (2015). [DOI] [PubMed] [Google Scholar]
- 38.Wen X, Pique-Regi R, Luca F. Integrating molecular QTL data into genome-wide genetic association analysis: Probabilistic assessment of enrichment and colocalization. PLoS Genet 13, e1006646 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hamel AR, et al. Integrating genetic regulation and single-cell expression with GWAS prioritizes causal genes and cell types for glaucoma. medRxiv, 2022.2005.2014.22275022 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fornes O, et al. JASPAR 2020: update of the open-access database of transcription factor binding profiles. Nucleic Acids Res 48, D87–D92 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bailey TL, et al. MEME SUITE: tools for motif discovery and searching. Nucleic Acids Res 37, W202–208 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.French CR, et al. Mutation of FOXC1 and PITX2 induces cerebral small-vessel disease. The Journal of clinical investigation 124, 4877–4881 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu B, et al. Genetic Regulatory Mechanisms of Smooth Muscle Cells Map to Coronary Artery Disease Risk Loci. Am J Hum Genet 103, 377–388 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gladh H, et al. Mice Lacking Platelet-Derived Growth Factor D Display a Mild Vascular Phenotype. PLoS One 11, e0152276 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Madisen L, et al. A robust and high-throughput Cre reporting and characterization system for the whole mouse brain. Nat Neurosci 13, 133–140 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nurnberg ST, et al. Coronary Artery Disease Associated Transcription Factor TCF21 Regulates Smooth Muscle Precursor Cells That Contribute to the Fibrous Cap. PLoS Genet 11, e1005155 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Herring BP, Hoggatt AM, Burlak C, Offermanns S. Previously differentiated medial vascular smooth muscle cells contribute to neointima formation following vascular injury. Vascular cell 6, 21 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wirth A, et al. G12-G13-LARG-mediated signaling in vascular smooth muscle is required for salt-induced hypertension. Nat Med 14, 64–68 (2008). [DOI] [PubMed] [Google Scholar]
- 49.Slack MA, Gordon SM. Protease Activity in Vascular Disease. Arterioscler Thromb Vasc Biol 39, e210–e218 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Waumans Y, Baerts L, Kehoe K, Lambeir AM, De Meester I. The Dipeptidyl Peptidase Family, Prolyl Oligopeptidase, and Prolyl Carboxypeptidase in the Immune System and Inflammatory Disease, Including Atherosclerosis. Front Immunol 6, 387 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kume T. Specification of arterial, venous, and lymphatic endothelial cells during embryonic development. Histol Histopathol 25, 637–646 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Olson LE, Soriano P. PDGFRbeta signaling regulates mural cell plasticity and inhibits fat development. Dev Cell 20, 815–826 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hamzah J, et al. Vascular normalization in Rgs5-deficient tumours promotes immune destruction. Nature 453, 410–414 (2008). [DOI] [PubMed] [Google Scholar]
- 54.Lin ME, et al. Runx2 deletion in smooth muscle cells inhibits vascular osteochondrogenesis and calcification but not atherosclerotic lesion formation. Cardiovasc Res 112, 606–616 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Butler A, Hoffman P, Smibert P, Papalexi E, Satija R. Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat Biotechnol 36, 411–420 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data generated through these studies have been uploaded to the Gene Expression Omnibus (GSE214423) and will become publicly available coincident with publication of this manuscript.