To the Editor:
Cholera was absent from Haiti until an inadvertent introduction by United Nations security forces in October 2010. The ensuing epidemic sickened 820,000 and caused 9,792 reported deaths1. The last cholera case in Haiti was recorded in January 2019, and in February 2022, Haiti was declared to have eliminated cholera2. In late September of 2022, a new outbreak began in Port-au-Prince and rapidly expanded to 9,317 suspected cases by mid-November of which >800 were confirmed by culture3. Here, we present genomic and phenotypic analysis of the Vibrio cholerae isolated from a stool sample collected on September 30th, 2022 of an index case – a child who presented with watery diarrhea and severe dehydration – to begin to address the origins of the epidemic.
The 2022 V. cholerae isolate shares phenotypes with the 2010 outbreak strain. Both strains are V. cholerae serogroup O1 of the Ogawa serotype and have similar antibiograms, including resistance to trimethoprim/sulfamethoxazole and low-level resistance to ciprofloxacin (Supp. Table 1,2). This resistance profile is consistent among 130 isolates from the current outbreak, suggesting that the strain isolated from the index case is representative of the ongoing epidemic.
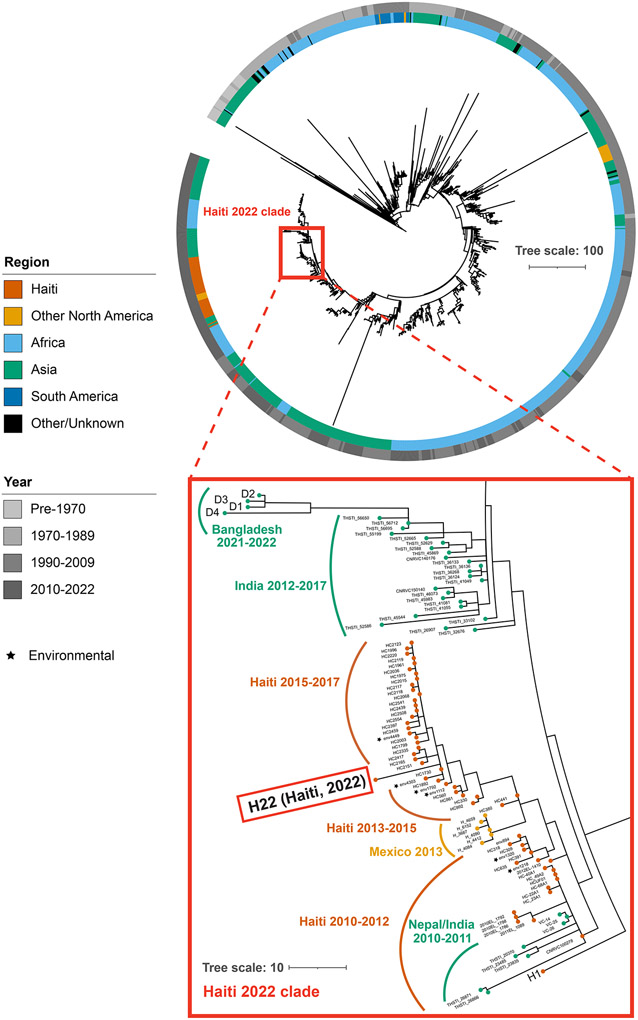
To decipher the relationship between the current outbreak strain and other toxigenic O1 El Tor strains from the ongoing seventh pandemic of cholera, we sequenced the 9/30/2022 isolate, along with four 2021-2022 isolates from Dhaka, Bangladesh (Supp. Table 2). Phylogenetic analyses of >1,200 isolates revealed that the 2022 Haiti isolate is closely related to 2010 Nepal isolates that were the origin of the initial outbreak. The 2022 isolate belongs to a subclade of Haiti V. cholerae isolates originating in 2013 during the previous epidemic and is divergent from 2013 strains from Mexico that were thought to have spread from Haiti, as well as currently circulating Bangladesh isolates. Haiti 2022 and Haiti 2010 isolates have identical ctxB (ctxB7) and other virulence factors (Supp. Table 3) and produce similar quantities of cholera toxin (Supp. Figure 1).
These analyses suggest that the reemergence of cholera in Haiti is caused, at least in part, by a descendant of the V. cholerae strain that gave rise to the 2010 epidemic. However, no cases of cholera were confirmed between 2019 and 2022 despite ongoing surveillance. Several explanations for the recrudescence of this strain are possible. The first is that toxigenic V. cholerae O1 persisted in Haiti through sub-clinical human infection and has recurred in the setting of waning population immunity coupled with a crisis in lack of clean water and sanitation. Another non-exclusive possibility is that this V. cholerae strain has persisted in environmental reservoirs. Finally, since the Haiti outbreak was ultimately transmitted to other countries in Latin America4, a third less likely explanation, given the phylogenetic evidence and absence of recent cholera cases in the region, is that the current strain could have been reintroduced to Haiti from a nearby country. These findings, along with the resurgence of cholera in several parts of the world5 despite available tools, suggest that cholera control and prevention efforts must be redoubled.
Supplementary Material
Figure 1.
Phylogenetic tree of 7th pandemic Vibrio cholerae. (Top) A phylogenetic tree of non-recombinogenic regions from 1,270 strains of O1 El Tor 7th pandemic V. cholerae. Tracks represent continent (inner) and year (outer) of isolation. Tree scale represents single-nucleotide polymorphisms (SNPs) per genome. (Bottom) Inset focused on the Haiti clade along with recent Asian isolates.
Acknowledgments
This work is funded by NIH R01AI-04237 and HHMI (MKW), NIH F30AI160911-01 and NIH T32GM007753 (DHFR), NIH R01HD102540 (JBH), and NIH R01AI099243 (LCI).
Footnotes
Publisher's Disclaimer: This is an Author Accepted Manuscript, which is the version after external peer review and before publication in the Journal. The publisher’s version of record, which includes all New England Journal of Medicine editing and enhancements, is available at https://www.nejm.org/doi/full/10.1056/NEJMc2213908.
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
Contributor Information
Daniel H. F. Rubin, Brigham and Women’s Hospital Boston, MA
Franz G. Zingl, Brigham and Women’s Hospital Boston, MA
Deborah R. Leitner, Brigham and Women’s Hospital Boston, MA
Ralph Ternier, Zanmi Lasante Croix-des-Bouquets, Haiti
Valusnor Compere, Laboratoire National de Santé Publique Port-au-Prince, Haiti
Samson Marseille, Laboratoire National de Santé Publique Port-au-Prince, Haiti
Damien Slater, Massachusetts General Hospital Boston, MA
Jason B. Harris, Massachusetts General Hospital Boston, MA
Fahima Chowdhury, International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B) Dhaka, Bangladesh
Firdausi Qadri, International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B) Dhaka, Bangladesh
Jacques Boncy, Laboratoire National de Santé Publique Port-au-Prince, Haiti
Louise C. Ivers, Massachusetts General Hospital Boston, MA
Matthew K. Waldor, Brigham and Women’s Hospital Boston, MA
References
- 1.World Health Organization. Cholera - Haiti: 12 October 2022. 2022. [Google Scholar]
- 2.Haïti Ministère de la Communication. 4 février 2019 – 4 février 2022 – trois (3) ans SANS CHOLÉRA en Haïti. Siteweb Officiel du Ministère de la Communication; 2022. [Google Scholar]
- 3.Haïti Ministère de Lasanté Publique et de la Population. Situtation Épidémiologique du Choléra, 19 Octobre 2022, Haïti. 2022. [Google Scholar]
- 4.Dorman MJ, Domman D, Poklepovich T, et al. Genomics of the Argentinian cholera epidemic elucidate the contrasting dynamics of epidemic and endemic Vibrio cholerae. Nature communications 2020;11(1):4918. (In eng). DOI: 10.1038/s41467-020-18647-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Shortage of cholera vaccines leads to temporary suspension of two-dose strategy, as cases rise worldwide - 19 October 2022. 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.