Abstract
Purpose:
Surveillance following urinary diversion should be tailored to capture complications downstream from the initial reconstruction. Most analyses of the morbidity associated with urinary diversion are restricted to the index admission or the immediate postoperative period. We characterize the long-term medical and surgical complications and burden of health care use after urinary diversion.
Materials and Methods:
Using the 5% Medicare sample from 1998 to 2005 we identified individuals who underwent cutaneous and orthotopic continent urinary diversion, ileal conduit or other types of diversion including enterocystoplasty from physician claims for the index admission. We restricted our sample to subjects with claims 1 year before surgery and at least 2 years after the diversion. We included benign and malignant primary diagnoses, and evaluated the incidence of medical and surgical complications 2 and 5 years after surgery. We stratified complications by diversion type and compared long-term complications after urinary diversion surgery.
Results:
Of the 1,565 subjects identified 80% underwent ileal conduit urinary diversion, 7% underwent cutaneous or orthotopic continent diversion and 13% underwent other types of reconstruction. Urinary stone formation, wound complications and fistula complications were more common following continent diversion 5 years after surgery, while ureteral obstruction and renal failure/impairment were more common after ileal conduit diversion. Overall we estimated that more than 16% of patients experienced renal failure or impairment after urinary diversion.
Conclusions:
Complications are common after urinary diversion and continue to occur through 5 years postoperatively. Urolithiasis and delayed wound complications appear to occur more commonly after continent diversion than after other urinary diversions. A large proportion of patients experience renal deterioration after diversion. These results highlight the need to survey patients for the diversion related complications of cystectomy as rigorously as we monitor for cancer recurrence.
Keywords: urinary diversion, complications
Although important in the management of a number of urological diseases, urinary diversion is associated with several complications including metabolic acidosis, electrolyte imbalance, bacterial colonization, infection, urolithiasis and renal dysfunction.1–9 While complications in the immediate postoperative period have been well documented,10,11 information regarding the long-term consequences associated with urinary diversion has been limited. Thus, the impact and clinical importance of diversion related consequences have not been completely outlined.
A more complete understanding of late complications after urinary diversion may help guide surveillance care. Current surveillance recommendations do not capture the full range of diversion related health consequences.12,13 Furthermore, the risk of urinary diversion related complications may not be static as long-term exposure to persistent metabolic changes may confer downstream complications not seen during the early postoperative phase, such as changes in bone mineralization and progressive loss of renal function. Understanding these secondary health outcomes may inform surveillance practices. To address this under studied phase of care, we characterized the likelihood of and risk factors for downstream complications by studying a broad group of men and women treated with urinary diversion beyond the immediate post-diversion period.
MATERIALS AND METHODS
Data Source and Study Design
We identified our study population from a 5% sample of Medicare claims for 1998 to 2005. Medicare is a federal health services program administered and overseen by the Centers for Medicare & Medicaid Services, and it covers 97% of eligible Americans.14 Most beneficiaries are age 65 years or older, although disability related indications allow program coverage for some diseases such as renal failure. Medicare data capture billing information related to health services provided to beneficiaries such as physician visits, procedures and hospital admissions. Information regarding diagnoses and services is available through ICD diagnostic and procedure codes and HCPCS (Healthcare Common Procedure Coding System) service codes. For this study data regarding inpatient claims, outpatient provider claims, and Medicare enrollment and vital statistics were obtained from the Medicare Standard Analytical Files.
Study Population
Men and women enrolled in Medicare from 1998 to 2005 treated with urinary diversion for cancer and noncancer indications were identified for study inclusion. No age restriction was applied, although the majority of subjects were 65 years old or older, reflecting the most common enrollment criteria for the Medicare program. Individuals without Part A and B coverage and those enrolled in Medicare HMO (health maintenance organization) programs were excluded from the study to ensure complete health care claims records. The cohort was further limited to beneficiaries enrolled at least 1 year before and 2 years after diversion surgery to allow for pre-diversion comorbidity ascertainment and post-diversion followup assessment. A subgroup of study subjects with at least 5 years of followup was identified to allow for longer term measurement of health outcomes of interest.
Outcome Measures and Definitions
Demographic information including age, gender and race/ethnicity was identified from the Standard Analytical Files. Type of urinary diversion was defined according to ICD-9 procedure codes as previously described.15 Diagnostic ICD-9 codes for the indication for urinary diversion were also identified. Medical and surgical complications after urinary diversion were identified according to ICD-9 diagnosis and procedure codes as well as HCPCS service codes indicating secondary health services such as rehospitalizations and secondary surgeries. Outcomes were grouped broadly according to type of complication including stomal complications, noninfectious wound complications, infectious wound complications, other infections (eg urinary tract infections, pyelonephritis and sepsis), urinary obstruction, urolithiasis, fistula complications and renal failure/impairment (see supplementary Appendix, http://jurology.com/). Outcome measures were designed to be specific for a given group of complications based on the inclusion of health services codes indicating relatively resource intense events such as hospitalization or additional procedures. Competing comorbidities were identified from ICD-9 and HCPCS codes during the year before urinary diversion to allow for case mix adjustment using the Klabunde modification of the Charlson comorbidity index.16
Statistical Analysis
Demographic factors were compared across urinary diversion groups using chi-square tests. Complications occurring 2 and 5 years after urinary diversion were compared by diversion type using Mantel-Haenszel chi-square tests. Serious complications, defined as reoperation, sepsis and/or renal failure, were also compared across diversion groups using chi-square methods. Unadjusted and adjusted logistic regression models were then developed to identify factors associated with urinary diversion related complications. For each model the occurrence of an adverse event was treated as a binary outcome (dependent) variable and the type of urinary diversion was used as the exposure of interest.
Other clinical and demographic factors (age, gender, race/ethnicity, comorbidity, clinical indication for urinary diversion [cancer/noncancer] and year of index diversion surgery) were included in the models to adjust for case mix differences. Backward selection was used to select final reduced models and factors that were significant at p ≤0.10 were retained in reduced models. For the analysis of serious complications a composite outcome consisting of aggregated reoperation, sepsis/infection and/or renal failure/impairment events was used as the dependent variable. Statistical procedures were performed using standard statistical software (SAS® 9.1). The study was reviewed and approved by the University of California, Los Angeles and RAND Corporation institutional review board.
RESULTS
The study population consisted of 1,565 men and women treated with urinary diversion for a range of indications, corresponding to a weighted sample of 31,300 (table 1). Among the Medicare beneficiaries who underwent urinary diversion during the study period, most were older than age 65 years. Nearly half (44%) were between 65 and 74 years old, and an additional 43% were 75 years old or older. Approximately 80% were treated with an incontinent conduit diversion, while only 7% underwent a continent diversion and the remaining 13% received some other form of urinary diversion or bladder augmentation. Approximately two-thirds of the study population was male. Black men and women accounted for 6% of the study population, while Asian, Hispanic and other racial/ethnic groups accounted for 4% of the study sample. Competing health problems were common. More than half of the cohort had at least 1 major comorbidity and 23% of patients had 2 or more major comorbid conditions.
Table 1.
Demographic characteristics of patients undergoing urinary diversion
| No. Ileal Conduit (%) | No. Continent (%) | No. Other (%) | No. Totals (%) | p Value | |
|---|---|---|---|---|---|
| No. pts | 1,248 | 105 | 212 | 1,565 | |
| Age: | |||||
| Younger than 65 | 129 (10.4) | 45 (42.9) | 29 (13.7) | 203 (13.0) | <0.001 |
| 65–74 | 543 (43.5) | 44 (41.9) | 103 (48.6) | 690 (44.1) | |
| 75–84 | 522 (41.8) | 16 (15.2) | 70 (33.0) | 608 (38.8) | |
| 85+ | 54 (4.3) | 0 (0) | 10 (4.7) | 64 (4.1) | |
| Gender: | |||||
| M | 850 (68.1) | 65 (61.9) | 137 (64.6) | 1,052 (67.2) | 0.29 |
| F | 398 (31.9) | 40 (38.1) | 75 (35.4) | 513 (32.8) | |
| Race/ethnicity: | |||||
| White | 1,130 (90.5) | 91 (86.7) | 187 (88.2) | 1,408 (90.0) | 0.85 |
| Black | 71 (5.7) | 7 (6.7) | 17 (8.0) | 95 (6.1) | |
| Other | 47 (3.8) | 7 (6.6) | 8 (3.8) | 62 (3.9) | |
| Region: | |||||
| Midwest | 364 (29.2) | 33 (31.4) | 62 (29.3) | 459 (29.3) | 0.26 |
| Northeast | 246 (19.7) | 9 (8.6) | 38 (17.9) | 293 (18.7) | |
| South | 458 (36.7) | 42 (40.0) | 77 (36.3) | 577 (36.9) | |
| West | 175 (14.0) | 21 (20.0) | 34 (16.0) | 230 (14.7) | |
| Yr of surgery: | |||||
| 1998 | 162 (13.0) | 17 (16.2) | 27 (12.7) | 206 (13.2) | 0.64 |
| 1999 | 139 (11.1) | 13 (12.4) | 24 (11.3) | 176 (11.2) | |
| 2000 | 162 (13.0) | 14 (13.3) | 32 (15.1) | 208 (13.3) | |
| 2001 | 165 (13.2) | 11 (10.5) | 26 (12.3) | 202 (12.9) | |
| 2002 | 166 (13.3) | 15 (14.3) | 19 (9.0) | 200 (12.8) | |
| 2003 | 139 (11.1) | 14 (13.3) | 22 (10.4) | 175 (11.2) | |
| 2004 | 145 (11.6) | 9 (8.6) | 36 (17.0) | 190 (12.1) | |
| 2005 | 170 (13.6) | 12 (11.4) | 26 (12.3) | 208 (13.3) | |
| Primary diagnosis: | |||||
| Ca | 885 (70.9) | 37 (35.2) | 104 (49.0) | 1,026 (65.6) | <0.001 |
| NonCa | 363 (29.1) | 68 (64.8) | 108 (51.0) | 539 (34.4) | |
| Comorbidities: | |||||
| 0 | 563 (45.3) | 66 (62.9) | 105 (49.8) | 734 (47.3) | 0.03 |
| 1 | 376 (30.3) | 25 (23.8) | 60 (28.4) | 461 (29.7) | |
| 2 | 191 (15.4) | 7 (6.7) | 23 (10.9) | 221 (14.3) | |
| 3 or More | 107 (9.0) | 6 (6.6) | 22 (10.9) | 135 (8.7) | |
Table 2 displays complications according to the postoperative year in which they were encountered through 5 years of followup from the time of urinary diversion. All study subjects had a minimum of 2 years of followup. Stomal complications (stomal stenosis, parastomal hernia or need for surgical revision) occurred relatively commonly early after diversion and then decreased in frequency. Similarly, hernia complications occurred more commonly during the early phase of followup and then decreased in the later years of the study. Infectious complications such as urinary tract infections, pyelonephritis or urosepsis occurred in 27% of the study population at year 2 and then decreased to approximately 14% in subsequent years but did not vary by diversion type. Urinary obstruction was common, mainly in the form of ureteral stricture and particularly at the 2-year mark. Approximately 8% of the study population experienced obstruction by 2 years, and although the likelihood decreased in subsequent years, obstruction still impacted more than 3% of cases 5 years after urinary diversion. Although ureteral strictures were less frequent in the continent urinary diversion group at year 2, rates of stricture/obstruction were similar in subsequent years. Urolithiasis was slightly more common after continent diversion compared with ileal conduit. Deterioration in renal function affected all 3 diversion groups, with renal failure/impairment impacting more than 2% of subjects in year 2 and approximately 1% per year thereafter. Metabolic complications (eg acidosis, electrolyte imbalance) were noted in 20% of conduit cases and 13% of continent diversions 2 years after surgery.
Table 2.
Long-term complications associated with urinary diversion by interval year
| Postop Yr | No. Conduit (%) | No. Continent (%) | No. Other (%) | p Value | |||
|---|---|---|---|---|---|---|---|
| Stoma: | |||||||
| 0–2 | 43/1,248 | (3.45) | 4/105 | (3.81) | 6/212 | (2.83) | 0.87 |
| 2–3 | 8/930 | (0.86) | 0/87 | (0) | 0/160 | (0) | 0.34 |
| 3–4 | 8/707 | (1.13) | 0/71 | (0) | 2/114 | (1.75) | 0.54 |
| 4–5 | 3/544 | (0.55) | 1/56 | (1.79) | 1/94 | (1.06) | 0.53 |
| Hernia: | |||||||
| 0–2 | 52/1,248 | (4.17) | 4/105 | (3.81) | 4/212 | (1.89) | 0.28 |
| 2–3 | 12/930 | (1.29) | 3/87 | (3.45) | 1/160 | (0.63) | 0.17 |
| 3–4 | 13/707 | (1.84) | 1/71 | (1.41) | 5/114 | (4.39) | 0.20 |
| 4–5 | 4/544 | (0.74) | 1/56 | (1.79) | 2/94 | (2.13) | 0.38 |
| Wound: | |||||||
| 0–2 | 63/1,248 | (5.05) | 7/105 | (6.67) | 3/212 | (1.42) | 0.04 |
| 2–3 | 13/930 | (1.40) | 5/87 | (5.75) | 6/160 | (3.75) | 0.01 |
| 3–4 | 15/707 | (2.12) | 0/71 | (0) | 4/114 | (3.51) | 0.27 |
| 4–5 | 10/544 | (1.84) | 5/56 | (8.93) | 3/94 | (3.19) | 0.01 |
| Infection: | |||||||
| 0–2 | 339/1,248 | (27.16) | 31/105 | (29.52) | 50/212 | (23.58) | 0.45 |
| 2–3 | 123/930 | (13.23) | 13/87 | (14.94) | 23/160 | (14.38) | 0.85 |
| 3–4 | 104/707 | (14.71) | 11/71 | (15.49) | 22/114 | (19.30) | 0.45 |
| 4–5 | 75/544 | (13.79) | 18/56 | (32.14) | 18/94 | (19.15) | <0.01 |
| Urinary obstruction: | |||||||
| 0–2 | 104/1,248 | (8.33) | 3/105 | (2.86) | 10/212 | (4.72) | 0.03 |
| 2–3 | 21/930 | (2.26) | 3/87 | (3.45) | 0/160 | (0) | 0.11 |
| 3–4 | 19/707 | (2.69) | 3/71 | (4.23) | 3/114 | (2.63) | 0.75 |
| 4–5 | 21/544 | (3.86) | 2/56 | (3.57) | 2/94 | (2.13) | 0.71 |
| Urolithiasis: | |||||||
| 0–2 | 29/1,248 | (2.32) | 2/105 | (1.90) | 2/212 | (0.94) | 0.43 |
| 2–3 | 9/930 | (0.97) | 2/87 | (2.30) | 2/160 | (1.25) | 0.52 |
| 3–4 | 9/707 | (1.27) | 1/71 | (1.41) | 2/114 | (1.75) | 0.92 |
| 4–5 | 6/544 | (1.10) | 3/56 | (5.36) | 2/94 | (2.13) | 0.05 |
| Fistula: | |||||||
| 0–2 | 23/1,248 | (1.84) | 1/105 | (0.95) | 4/212 | (1.89) | 0.80 |
| 2–3 | 3/930 | (0.32) | 1/87 | (1.15) | 1/160 | (0.63) | 0.48 |
| 3–4 | 3/707 | (0.42) | 0/71 | (0) | 1/114 | (0.88) | 0.67 |
| 4–5 | 2/544 | (0.37) | 2/56 | (3.57) | 0/94 | (0) | 0.01 |
| Renal failure: | |||||||
| 0–2 | 31/1,248 | (2.48) | 3/105 | (2.86) | 4/212 | (1.89) | 0.84 |
| 2–3 | 9/930 | (0.97) | 0/87 | (0) | 4/160 | (2.50) | 0.14 |
| 3–4 | 9/707 | (1.27) | 0/71 | (0) | 6/114 | (5.26) | <0.01 |
| 4–5 | 8/544 | (1.47) | 1/56 | (1.79) | 4/94 | (4.26) | 0.18 |
| Metabolic changes/acidosis: | |||||||
| 0–2 | 242/1,248 | (19.39) | 14/105 | (13.33) | 35/212 | (16.51) | 0.22 |
| 2–3 | 73/930 | (7.85) | 10/87 | (11.49) | 15/160 | (9.38) | 0.44 |
| 3–4 | 63/707 | (8.91) | 5/71 | (7.04) | 10/114 | (8.77) | 0.87 |
| 4–5 | 47/544 | (8.64) | 8/56 | (14.29) | 10/94 | (10.64) | 0.35 |
Cumulative complications after 5 years were similar among diversion groups with a few notable exceptions (table 3). Noninfectious wound complications were prevalent and disproportionately affected the continent diversion group. Ureteral obstruction occurred in approximately 13% of diversion subjects overall (13.4% after ileal conduit, 14.3% after continent diversion). The cumulative risk of urolithiasis was lowest after ileal conduit and highest after continent reconstruction. Loss of renal function, the most concerning long-term consequence after diversion, affected more than 4% of the overall cohort, while metabolic complications occurred in more than 30% of cases. As shown in figures 1 and 2, actuarial estimates of complications were higher than cumulative rates. At 5 years Kaplan-Meier estimates of renal failure/deterioration and urolithiasis were approximately 16% and 20% or more, respectively.
Table 3.
Cumulative incidence of complications 5 years after urinary diversion
| No. Conduit (%) | No. Continent (%) | No. Other (%) | No. Totals (%) | p Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| No. pts | 544 | 56 | 94 | 694 | |||||
| Stoma | 34 | (6.25) | 5 | (8.93) | 5 | (5.32) | 44 | (6.34) | 0.67 |
| Hernia | 40 | (7.35) | 8 | (14.29) | 7 | (7.45) | 55 | (7.93) | 0.18 |
| Wound | 50 | (9.19) | 14 | (25.0) | 9 | (9.57) | 73 | (10.52) | <0.01 |
| Infection | 247 | (45.4) | 31 | (55.36) | 38 | (40.43) | 316 | (45.53) | 0.20 |
| Obstruction | 73 | (13.42) | 8 | (14.29) | 6 | (6.38) | 87 | (12.54) | 0.15 |
| Urolithiasis | 25 | (4.6) | 5 | (8.93) | 5 | (5.32) | 35 | (5.04) | 0.37 |
| Fistula | 14 | (2.57) | 4 | (7.14) | 4 | (4.26) | 22 | (3.17) | 0.14 |
| Wound infection | 42 | (7.72) | 12 | (21.43) | 9 | (9.57) | 63 | (9.08) | <0.01 |
| Renal failure | 22 | (4.04) | 2 | (3.57) | 7 | (7.45) | 31 | (4.47) | 0.32 |
| Metabolic acidosis | 170 | (31.25) | 15 | (26.79) | 21 | (22.34) | 206 | (29.68) | 0.19 |
Figure 1.
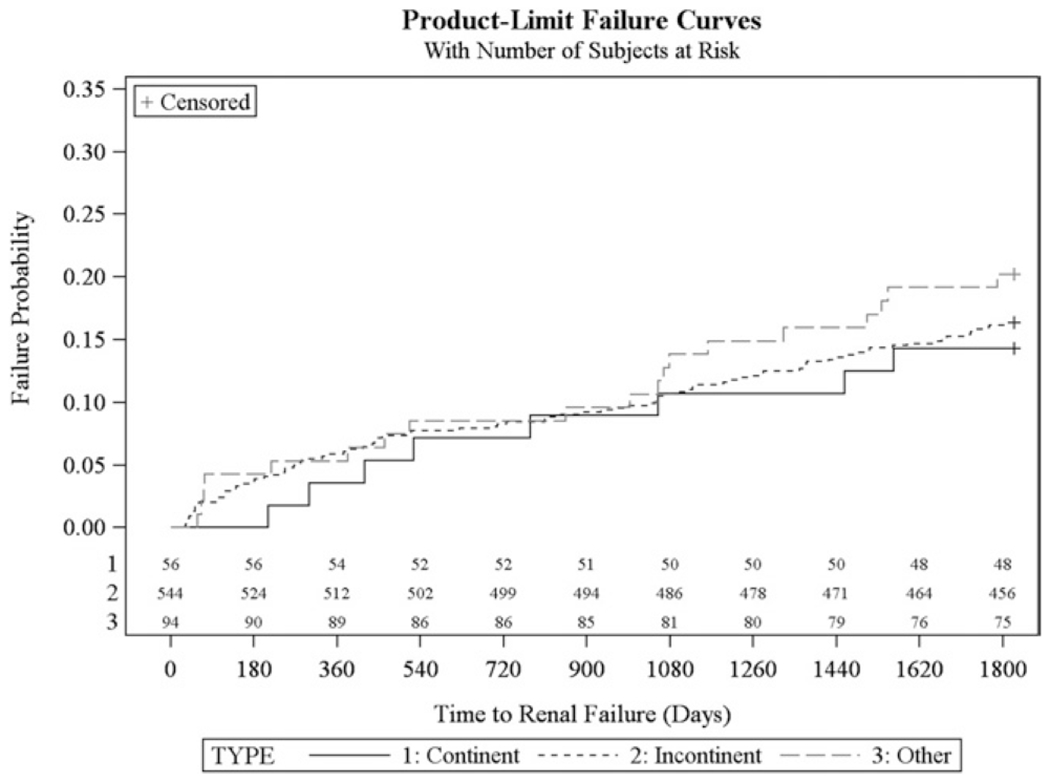
Estimated time to renal failure/renal deterioration by type of urinary diversion (log rank 0.58)
Figure 2.
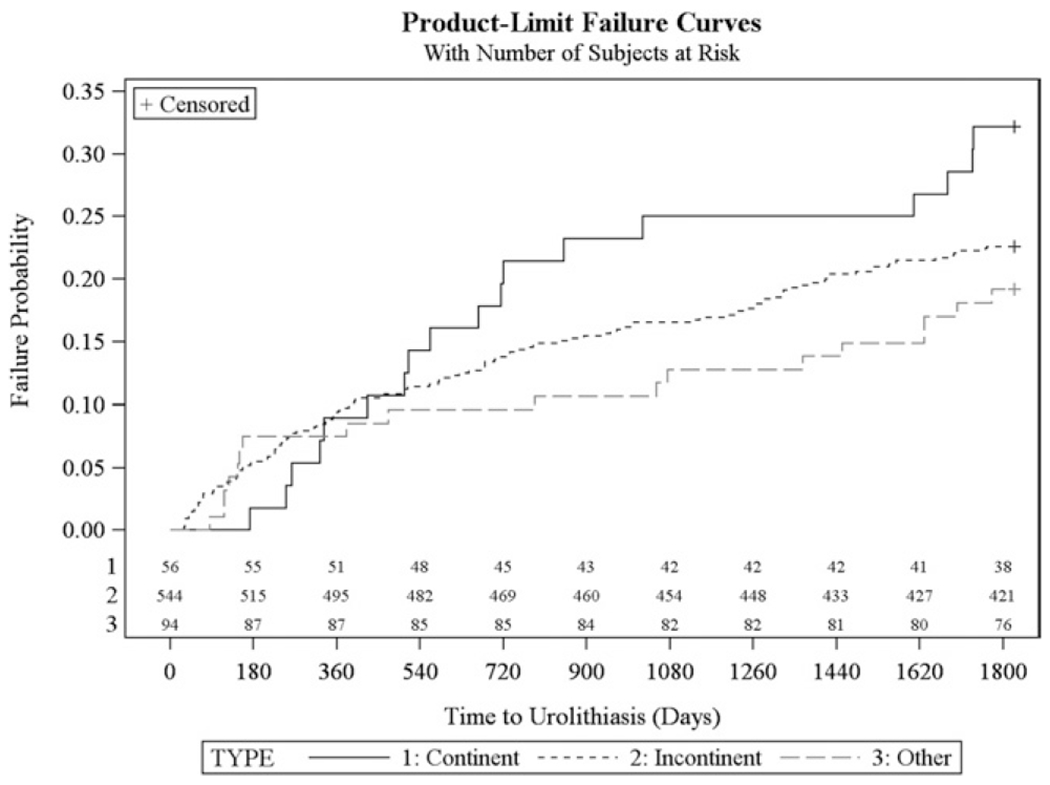
Time to urolithiasis estimates by type of urinary diversion (log rank 0.20)
Factors associated with major complications are shown in table 4. Compared with continent diversion, patients treated with ileal conduits and other types of diversion were not more or less likely to experience a major complication during the first 5 years after diversion (OR 0.85; 95% CI 0.52, 1.39 for ileal conduit vs continent diversion). Older patients did not appear to be more likely to experience a major complication, suggesting that urinary diversion may be reserved for relatively healthy octogenarians. Higher levels of competing health problems were associated with an increased likelihood of major complications during the post-diversion period (OR 2.15; 95% CI 1.36, 3.38 Charlson score 3 or greater vs Charlson score 0–1).
Table 4.
Multivariable model of factors associated with major complications following urinary diversion during 5-year study period
| OR (95% CI) | p Value | |
|---|---|---|
| Diversion type (vs continent): | ||
| Ileal conduit | 0.85 (0.52, 1.39) | 0.52 |
| Other | 0.78 (0.45, 1.36) | 0.38 |
| Age (vs 65–74 yrs): | ||
| Younger than 65 | 1.79 (1.21, 2.64) | 0.004 |
| 75–84 | 0.96 (0.75, 1.22) | 0.72 |
| 85 or Older | 1.10 (0.62, 1.95) | 0.75 |
| Female (vs male) | 1.13 (0.89, 1.44) | 0.32 |
| Race (vs white): | ||
| Black | 1.48 (0.88, 2.46) | 0.14 |
| Other | 1.04 (0.57, 1.90) | 0.89 |
| Comorbidity (vs 0–1): | ||
| Charlson score 2 | 1.26 (0.99, 1.60) | 0.06 |
| Charlson score 3 or greater | 2.15 (1.36, 3.38) | 0.001 |
| Region (vs West): | ||
| South | 0.98 (0.69, 1.38) | 0.88 |
| Northeast | 1.08 (0.73, 1.59) | 0.71 |
| Midwest | 1.11 (0.78, 1.59) | 0.55 |
| Other | 0.12 (0.01, 1.18) | 0.07 |
Serious complications defined as renal failure, reoperation or sepsis.
DISCUSSION
Patients who undergo urinary diversion face a number of complications after surgery, ranging from inconsequent metabolic acidosis to significant renal deterioration. Although prevalent, common consequences such as electrolyte abnormalities and bacterial colonization may not always result in clinical problems. For example, although bacteriuria develops in approximately 80% of patients after diversion,3,4 far fewer patients experience clinically significant infections.
Previous research in this area has largely focused on short-term outcomes. As a result, little generalizable information is available regarding the longterm consequences of diversion surgery. Our results indicate that the risk of complications after urinary diversion persists for years after surgery. For example, urinary obstruction, infection, renal deterioration and metabolic changes continued to impact a large number of patients during the later years of followup. Notably the estimated risk of renal failure/impairment 5 years after urinary diversion approached 16% (fig. 1). The cumulative incidence of other serious complications also was relatively high. Approximately 10% of patients experienced some form of wound complication, while ureteral obstruction requiring intervention affected more than 13% of our study cohort. We also found that continent diversions were associated with a greater likelihood of certain long-term complications, most notably urolithiasis. Interestingly we did not find a significant relationship between patient age and complications, possibly because older patients treated with diversion surgery are likely highly selected and may represent a relatively healthier patient group.
In the context of previous research, our results corroborate the known consequences associated with urinary diversion but also provide new insight into the persistence of complications beyond the immediate short-term period. Although immediate and short-term complications have not been shown to be different between continent and incontinent diversions,17 we noted higher rates of some long-term complications in the continent diversion group, which may relate to more pronounced metabolic changes after continent reconstruction. For example, rates of urolithiasis were greatest among patients treated with continent diversion, which has also been reported in smaller series.18 Some previous reports have suggested that ileal conduits are associated with fewer long-term complications. One study reported late complications in 39% of ileal conduit cases, compared with 63% and 59% of catheterizable pouch diversions and orthotopic neobladders, respectively.19 Other single institution series have reported ureteral strictures in approximately 13% of patients, although the majority of strictures was reported within the first year after surgery.20 Although we found a similar short-term rate, we also noted a yearly incidence of approximately 3% between years 3 and 5 after surgery resulting in a higher cumulative burden and suggesting that surveillance for progressive upper tract deterioration should continue beyond the first several postoperative years.
Although consensus recommendations endorse regular monitoring for metabolic acidosis, vitamin B12 deficiency and upper urinary tract obstruction after urinary diversion,12,13 formal evidence-based guidelines are lacking. Furthermore, little information is currently available indicating how long surveillance for these or other complications should be pursued. Our results suggest that in addition to metabolic complications and upper tract obstruction, surveillance for other consequences associated with urinary diversion such as persistent wound complications and urolithiasis should be part of the long-term followup care for this patient group. Furthermore, our results reemphasize the negative downstream consequences of ureteral obstruction, particularly in terms of renal deterioration and subsequent failure.21
Our study has several limitations. Because studies on long-term complications after urinary diversion have been limited, we chose to focus on describing the magnitude of the problem using population based data. However, our use of Medicare data may limit the applicability of our results to nonMedicare populations. Although the majority of patients who undergo cystectomy for bladder cancer are of Medicare age,22 patients with benign lower urinary tract pathology managed with urinary diversion comprise a more diverse age group. Thus, our results may be specific to older and disabled patients undergoing urinary diversion and may not extrapolate to younger, healthier patients.
In addition, although useful in describing the use of health services in a large component of the population, Medicare data lack clinical detail and can be associated with administrative coding errors. As a result, we may underestimate the true incidence of complications that arise during the post-diversion period. For example, we identified a 7% risk of stomal complications based on medical encounters required to manage this group of complications. However, the risk of stomal complications has been estimated to range from 15% to 65%, reflecting a common problem that may not always be identified by diagnostic codes or require medical intervention.23 This potential underreporting of complications may apply to other outcomes as well such as urolithiasis, in which case codes may not capture a large percentage of stone events managed conservatively or with medical expulsive therapy. However, complications that warrant medical services such as reoperation or hospitalization should be accurately characterized by our study.
We also chose to limit our analysis to beneficiaries who had at least 2 years of followup after diversion surgery. Although additional events may have occurred before the 2-year mark, we chose this time frame to focus on intermediate and long-term complications. Certainly censoring may have resulted in higher estimates. An additional complication relates to confounding. For example, the risk of renal failure may not only be linked to exposure to urinary diversion, but also to other competing health problems including aging, diabetes and hypertension.
Despite these limitations, our results indicate that the morbidity of urinary diversion persists beyond the immediate postoperative period and affects a substantial proportion of diversion cases.
CONCLUSIONS
Complications associated with urinary diversion persist beyond the first 2 years after diversion surgery. Furthermore, a substantial proportion of patients face serious late term complications such as renal deterioration and failure, supporting the need for long-term surveillance care. Additional research into the health trajectory of patients after diversion is needed to better inform surveillance recommendations and practices.
Supplementary Material
EDITORIAL COMMENT.
Gilbert et al provide an important addition to the literature on urinary diversion. By tracking longterm outcomes and showing a continued risk of complications for up to 5 years after surgery, they provide justification for continued long-term followup of these patients. As this knowledge about long-term complications is put into practice, the lack of good survivorship data for urological conditions becomes apparent. While patients may experience complications, we do not know what tests best identify issues at an early, treatable stage, and we do not know if intervention based on surveillance testing would impact patient outcomes. Initiatives for comparative effectiveness of followup care protocols are needed. Until then, the results of Gilbert et al alert us to the need to maintain a high level of suspicion for adverse functional outcomes in our patients, even many years after urinary diversion.
Footnotes
Study received institutional review board approval.
Contributor Information
Scott M. Gilbert, Department of Urology, College of Medicine, University of Florida, Gainesville, Florida
Julie Lai, RAND Corporation, Santa Monica.
Christopher S. Saigal, RAND Corporation, Santa Monica; Department of Urology, University of California, Los Angeles, Los Angeles, California
John L. Gore, Department of Urology, University of Washington, Seattle, Washington
REFERENCES
- 1.Castro JE and Ram MD: Electrolyte imbalance following ileal urinary diversion. Br J Urol 1970; 42: 29. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt JD, Hawtrey CE, Flocks RH et al. : Complications, results and problems of ileal conduit diversions. J Urol 1973; 109: 210. [DOI] [PubMed] [Google Scholar]
- 3.Thuroff JW, Alken P and Hohenfellner R: The MAINZ pouch (mixed augmentation with ileum ‘n’ zecum) for bladder augmentation and continent diversion. In: Bladder Reconstruction and Continent Urinary Diversion. Edited by King LR, Stone AF and Webster GD. Chicago: Year Book Medical Publishers; 1997; p 252. [Google Scholar]
- 4.Schwarz GR and Jeffs RD: Ileal conduit urinary diversion in children: computer analysis of followup from 2 to 16 years. J Urol 1975; 114: 285. [DOI] [PubMed] [Google Scholar]
- 5.Hagen-Cook K and Althausen AF: Early observations on 31 adults with non-refluxing colon conduits. J Urol 1979; 121: 13. [DOI] [PubMed] [Google Scholar]
- 6.Harrison AR: Clinical and metabolic observations on osteomalacia following ureterosigmoidostomy. Br J Urol 1958; 30: 455. [DOI] [PubMed] [Google Scholar]
- 7.Specht EE: Rickets following ureterosigmoidostomy and chronic hyperchloremia. A case report. J Bone Joint Surg Am 1967; 49: 1422. [PubMed] [Google Scholar]
- 8.Dretler SP: The pathogenesis of urinary tract calculi occurring after ileal conduit diversion. I. Clinical study. II. Conduit study. III. Prevention. J Urol 1973; 109: 204. [DOI] [PubMed] [Google Scholar]
- 9.Koch MO, McDougal WS, Hall MC et al. : Longterm metabolic effects of urinary diversion: a comparison of myelomeningocele patients managed by clean intermittent catheterization and urinary diversion. J Urol 1992; 147: 1343. [DOI] [PubMed] [Google Scholar]
- 10.Shabsigh A, Korets R, Vora KC et al. : Defining early morbidity of radical cystectomy for patient with bladder cancer using a standardized reporting methodology. Eur Urol 2009; 55: 164. [DOI] [PubMed] [Google Scholar]
- 11.Hautmann RE, Miller K, Steiner U et al. : The ileal neobladder: 6 years of experience with more than 200 patients. J Urol 1993; 150: 40. [DOI] [PubMed] [Google Scholar]
- 12.Fichtner J: Follow-up after urinary diversion. Urol Int 1999; 63: 40. [DOI] [PubMed] [Google Scholar]
- 13.NCCN bladder cancer guidelines. Available at www.nccn.org. Accessed September 27, 2010.
- 14.Center for Medicare & Medicaid Services (CMS). Available at www.cms.gov. Accessed November 29, 2010.
- 15.Gore JL, Saigal CS, Hanley JM et al. : Variations in reconstruction after radical cystectomy. Cancer 2006; 107: 729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klabunde CN, Potosky AL, Legler JM et al. : Development of a comorbidity index using physician claims data. J Clin Epidemiol 2000; 53: 1258. [DOI] [PubMed] [Google Scholar]
- 17.Gore JL, Yu HY, Setodji C et al. : Urinary diversion and morbidity after radical cystectomy for bladder cancer. Cancer 2010; 116: 331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knap MM, Lundbeck F and Overgaard J: Early and late treatment-related morbidity following radical cystectomy. Scand J Urol Nephrol 2004; 38: 153. [DOI] [PubMed] [Google Scholar]
- 19.Nieuwenhuijzen JA, de Vries RR, Bex A et al. : Urinary diversions after cystectomy: the association of clinical factors, complications and functional results of four different diversions. Eur Urol 2008; 53: 834. [DOI] [PubMed] [Google Scholar]
- 20.Tal R, Sivan B, Kedar D et al. : Management of benign ureteral strictures following radical cystectomy and urinary diversion for bladder cancer. J Urol 2007; 178: 538. [DOI] [PubMed] [Google Scholar]
- 21.Kristjansson A, Grubb A and Månsson W: Renal tubular dysfunction after urinary diversion. Scand J Urol Nephol 1995; 29: 407. [DOI] [PubMed] [Google Scholar]
- 22.Jemal A, Siegel R, Ward E et al. : Cancer statistics, 2009. CA Cancer J Clin 2009; 59: 225. [DOI] [PubMed] [Google Scholar]
- 23.Szymanski KM, St-Cyr D, Alam T et al. : External stoma and peristomal complications following radical cystectomy and ileal conduit diversion: a systematic review. Ostomy Wound Manage 2010; 56: 28. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


