Abstract
Rationale:
Psychological well-being is associated with better cardiovascular health, but the underlying mechanisms are unclear.
Objective:
This study investigates one possible mechanism by examining psychological well-being’s prospective association with lipid levels, focusing on high-density lipoprotein cholesterol (HDL-C).
Methods:
Participants were 4,757 healthy men and women ages ≥50 from the English Longitudinal Study of Ageing with clinical data from three times, three to five years apart. Psychological well-being was assessed at baseline using the Control, Autonomy, Satisfaction, and Pleasure scale; HDL-C, triglycerides, and total cholesterol were assayed from blood samples. Descriptive statistics and linear mixed models were used to examine associations between psychological well-being and lipid levels over time; the latter controlled for confounders and health behaviours.
Results:
In descriptive analyses, HDL-C levels were initially higher in people with greater psychological well-being. Among those who met recommended levels of HDL-C at baseline, fewer individuals with higher versus lower psychological well-being dropped below HDL-C recommendations over time. Mixed models indicated that HDL-C increased over time (β=0.64; 95% CI = 0.58 to 0.69) and higher baseline psychological well-being was associated with higher baseline HDL-C (β=0.51; 95% CI = 0.03 to 0.99). A significant well-being by time interaction indicated individuals with higher versus lower well-being exhibited a more rapid rate of increase in HDL-C over follow-up. Higher psychological well-being was also significantly associated with lower triglycerides, but main effects for both HDL-C and triglycerides were attenuated after accounting for health behaviours.
Conclusion:
Higher psychological well-being is associated with healthier HDL-C levels; these effects may compound over time. This protective effect may be partly explained by health behaviours.
Keywords: well-being, lipids, high-density lipoprotein cholesterol, triglycerides, English Longitudinal Study of Ageing
Introduction
Cardiovascular disease is the leading cause of death globally (WHO, 2017). The burden of cardiovascular disease is particularly high among older adults (WHO, 2008), so research to understand mechanisms of health promotion is particularly urgent in this important demographic. Most research to date has focused on risk factors in this population with less work identifying potential protective factors. Psychological well-being may be one such protective factor and is defined as having positive feelings and thoughts (Boehm & Kubzansky, 2012). Common indicators of psychological well-being include positive emotion and life satisfaction. Research has documented consistent associations between psychological well-being and greater cardiovascular health (Boehm & Kubzansky, 2012). Psychological well-being could be related to reduced risk of myocardial infarction, heart failure, and stroke by promoting biological or behavioural processes that foster healthy functioning (Farrelly, 2012). Identifying factors that support optimal functioning may inform approaches to health beyond simply studying risk factors that accelerate deterioration (Kubzansky, Boehm, & Segerstrom, 2015). High-density lipoprotein cholesterol (HDL-C), in particular, has been identified as a marker of a restorative process because HDL-C removes harmful cholesterol from blood vessels (Sacks & Jensen, 2018). As such, higher levels of HDL-C are desired for optimal cardiovascular health.
HDL-C is posited to be a pathway linking psychological well-being with cardiovascular health. Greater psychological well-being could lead to longer periods of healthy functioning that serve as opportunities for the body to accumulate reserves of HDL-C and other biological markers that contribute to restoration and health maintenance (Kubzansky, Boehm, & Segerstrom, 2015). Evidence also shows that low HDL-C levels can predict adverse cardiovascular events even in individuals treated who undergo statin therapy and have very low levels (i.e., healthy levels) of low-density lipoprotein cholesterol (LDL-C) (Boekholdt et al., 2013). Moreover, a growing body of research suggest s higher HDL-C levels predict survival and cardiovascular health independent of other lipids (Rader & Hovingh, 2014; Rye & Barter, 2014). Past research suggests that an association is plausible between healthier lipids and psychological well-being and related constructs. One study found that higher optimism was associated with higher HDL-C levels (Boehm, Williams, Rimm, Ryff, & Kubzansky, 2013); another found that higher perceived control was related to higher HDL-C (Infurna & Gerstorf, 2014). However, both studies were cross-sectional, so the direction of effects could not be determined as healthier biological functioning could lead to higher psychological well-being. Furthermore, longitudinal research is needed regarding how psychological well-being may relate to changes in lipid profiles as individuals grow into older age.
To address these outstanding questions, this study assessed the relationship of psychological well-being with changes in lipid levels over time among English men and women aged 50 and older. Primary models focused on HDL-C, with secondary analyses examining triglycerides and total cholesterol, which represent deteriorative processes (Boehm & Kubzansky, 2012). Higher versus lower psychological well-being was hypothesized to be associated with a healthier lipid profile over time, which was formally tested in models controlling for relevant covariates such as socioeconomic status. Prior work has linked depression with both lipids (Van Reedt Dortland, Giltay, van Veen, Zitman, & Penninx, 2013) and worse psychological well-being (Ryff, 2014), so these analyses also controlled for depression status to evaluate independent effects of psychological well-being. Finally, this study assessed whether observed associations between psychological well-being and lipid trajectories could be partly due to health behaviours. Previous research has found evidence of dose-response relationships between psychological well-being and cardiovascular events and mortality (Rozanski, 2014; Kim, Smith, & Kubzansky, 2014). Thus, following prior work in this area, this study considered associations with psychological well-being as either a continuous or a categorical variable (Kubzansky, Winning, & Kawachi, 2014) to assess the possibility of threshold versus more monotonic effects. To date, this longitudinal study is the first to investigate how psychological well-being may be related to lipid trajectories over time.
Methods
Participants
Data were from the English Longitudinal Study of Ageing (ELSA), a nationally representative cohort study of the community-dwelling English population aged 50 and older. The sample was recruited from households that participated in the Health Survey for England (HSE; an annual national cross-sectional health survey) in 1998, 1999, and 2001 (Steptoe, Breeze, Banks, & Nazroo, 2013). All HSE households with at least one person ≥50 years old who had consented to be re-contacted were eligible for inclusion in the ELSA cohort. The first ELSA interview in 2002–03 (Wave 1) included 11,391 men and women considered to be core ELSA members. Follow-up interviews occurred in 2004–05 (Wave 2), 2006–07 (Wave 3), 2008–09 (Wave 4), 2010–11 (Wave 5), and 2012–13 (Wave 6); response rates ranged from 73%−82% (Steptoe, Breeze, Banks, & Nazroo, 2013).
Health examinations were performed by nurses in conjunction with interviews conducted at Waves 2, 4, and 6. Because lipids were assessed only during health examinations, the overall analytic sample was limited to respondents who had at least one exam in these three waves, with covariates taken from Wave 2 (considered baseline for the present study) or later. During Wave 2, 8,780 total core members were interviewed (504 core members died by Wave 2). Analyses were further restricted to individuals who reported no doctor-diagnosed angina, heart attack, congestive heart failure, or stroke at study baseline, and who had complete data on psychological well-being and all other covariates at that time (Supplemental Figure S1). The primary analytic samples included 4,756 individuals with at least one measure of HDL-C, and 4,757 individuals with at least one measure of triglycerides and total cholesterol. An additional analysis considered only a subsample of individuals with healthy lipid levels at study baseline and who also had HDL-C measurements at all three waves (N=1,765).
ELSA was approved by various ethics committees including the London Multicentre Research Ethics Committee. Informed consent was obtained from all participants. Due to the use of de-identified data, the present study was designated as exempt research by the Institutional Review Boards at the authors’ institutions.
Assessment of Psychological Well-Being
Psychological well-being was assessed with items from the 19-item Control, Autonomy, Satisfaction, Pleasure (CASP-19) scale, which was designed to assess psychological well-being in older individuals. Originally developed and validated in 264 people in the United Kingdom ages 65–75, the CASP-19 is a summative scale covering four domains of psychological well-being: control, autonomy, pleasure and self-realization (Hyde, Wiggins, Higgs, & Blane, 2003). Higher scores represent greater psychological well-being. The CASP-19 demonstrates good internal consistency, and factor analysis has indicated the four facets load on a single underlying factor (Hyde, Wiggins, Higgs, & Blane, 2003; Wiggins, Netuveli, Hyde, Higgs, & Blane, 2008). Other work has demonstrated it has good concurrent validity in the ELSA cohort (Howel, 2012).
For this study, two health-related items were removed (“My age prevents me from doing the things I would like to,” “My health stops me from doing things I want to do”) to limit possible confounding. Thus, a modified scale (referred to as the CASP-17) was used from Wave 2 for all analyses (α=0.87). If participants completed at least 9 of the 17 items, missing values were imputed with the mean value of non-missing items (N=387; 245 [63.3%] missed one item and 50 [12.9%] missed two). Analyses considered CASP-17 as a continuous variable (mean=39.5; SD=7.28; range 0–51), which was standardized (mean=0; SD=1) to facilitate interpretation, and also a tertiled categorical variable (following past recommendations and based on the distribution of scores in the sample; low 0–37.2, moderate 37.4–43.7, and high 44–51) to assess possible discontinuous effects (Kubzansky, Winning, & Kawachi, 2014).
Assessment of Lipid Measures
Blood samples were collected at Waves 2, 4, and 6 by trained nurses. Respondents were asked to fast before their nurse visit if they were under 80 years old, did not have diabetes, and were otherwise able to do so. Lipid levels were measured for all blood samples, regardless of fasting status. Analysis of the blood data was done in the Royal Victoria Infirmary (Newcastle-upon-Tyne, UK). Details of the blood analysis, internal quality control, and external quality assessment for the laboratory are described in the 2004 HSE technical report (Graig, Deverill, & Pickering, 2006). HDL-C was analysed using a direct method (no precipitation) and triglycerides were measured using an enzymatic assay on an Olympus 640 analyser. Total cholesterol was analysed using the cholesterol oxidase assay method. LDL-C was not considered since it was derived using the Friedewald equation and thus not suitable for nonfasting samples. As only 65% of the blood samples were taken while participants were fasting, fasting status was included as a covariate in analyses.
Assessment of Covariates
Potential confounders were self-reported at baseline (Wave 2), except fasting status and high cholesterol diagnosis, which were time-updated. Age was recorded as a continuous variable in years, with participants over age 90 assigned the value of 91 by ELSA data managers to preserve confidentiality. Gender was categorized as male or female; race as White or non-White. Socioeconomic status was assessed by educational attainment (university degree or equivalent, higher education but not university degree, A-level [national school exam at age 18, high school equivalent], O-level [national school exam at age 16], or less than O-level) and total weekly income (continuous variable). Self-reported doctor-diagnoses of high cholesterol and depression (yes/no) were obtained during the interviews. High cholesterol diagnosis was used as proxy for cholesterol medication use, as the latter information was not available at Wave 2.
Potential explanatory variables including health behaviours and related factors were also assessed at baseline. Body mass index (BMI; kilograms/meters2) was measured during the health examination by study staff. Information on cigarette smoking status (current smoker, former smoker, or never smoker) and physical activity level (sedentary/low or moderate/high) was assessed during interviews. Physical activity was assessed with a series of questions regarding the frequency and intensity of participants’ physical activity during leisure time and at work. Three separate questions asked how often participants took part in sports or activities that were vigorous, moderately energetic, and mildly energetic. A fourth question asked about the level of physical activity in an individual’s main job. Responses to all four questions were categorized by ELSA data managers into four rank ordered categories (sedentary, low, moderate, and high) to reflect classifications used in the Allied Dunbar Survey of Fitness (UK Activity and Health Research, 1992). For ease of analysis, this variable was further dichotomized to represent sedentary/low or moderate/high physical activity. Alcohol intake was assessed by asking how often the respondent had an alcoholic drink during the last 12 months. Responses included almost every day; 5–6 days a week; 3–4 days a week; 1–2 days a week; 1–2 days a month; once every couple of months; once or twice a year; and not at all. Due to the monotonic and linear relationship between categories of alcohol intake and mean lipid levels, alcohol intake was treated as linear, with higher values denoting more frequent intake.
Statistical Analyses
First, baseline (Wave 2) characteristics were examined across psychological well-being tertiles in the largest analytic sample (N=4,757). Second, in a subsample of 1,765 individuals with healthy HDL-C levels (≥40 mg/dL, Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults, 2001) at the Wave 2 baseline and HDL-C measurements at all three waves, mean HDL-C levels were assessed at each time point according to psychological well-being tertiles. These analyses further identified the percentage of those individuals whose HDL-C levels dropped below recommended levels (<40 mg/dL) over the follow-up period.
Third, to evaluate patterns of change more rigorously, linear mixed models with random intercepts assessed the association between baseline psychological well-being and HDL-C over time (measured in years as a continuous variable). These analyses were done in the full analytic sample (N=4,756). The interaction between psychological well-being and time was included to assess if rate of change in HDL-C level differed depending on initial levels of psychological well-being. Mean time between lipid assessments was 4.17 years (SD=1.19). A set of four models was fitted that adjusted first for baseline age, gender, and race; second, that added baseline income and education; third, that added baseline doctor-diagnosed depression, doctor-diagnosed high cholesterol, and fasting status (the latter two were time-updated); finally, that further adjusted for baseline BMI, alcohol intake, smoking status, and physical activity. An additional model adjusted for time-updated health behaviours instead of baseline behaviours to preclude the possibility of healthy behaviours leading to higher psychological well-being. Secondary analyses evaluated, with the same set of models, psychological well-being’s relationship with changes in triglycerides and total cholesterol (N=4,757), which represent deteriorative biological processes.
To account for the likelihood that healthier individuals are more likely to undergo exams at subsequent waves (revisits), a propensity score was used to create inverse probabilities of multiple exams. This revisit propensity score was calculated from a logistic regression as the probability of having two or three exams, given all relevant factors at baseline including age, gender, race, income, education, high cholesterol diagnosis, depression diagnosis, BMI, alcohol intake, smoking status, and physical activity. This score was included in all mixed models to account for possible selection bias in analyses using repeated measures (Hogan & Lancaster, 2004).
To address concerns that other factors related to the likelihood of having repeated exams might affect lipid levels, a sensitivity analysis was performed with the mixed models. Participants with only one measurement of HDL-C, triglycerides, or total cholesterol were removed in the respective samples, and the primary analysis was repeated with the remaining participants. To evaluate gender differences in lipid levels which may modify associations (Heiss et al., 1980), interaction terms were included between gender and psychological well-being in all models. Finally, to assess whether psychological states such as well-being or ill-being may change over time and thereby affect lipid levels, primary mixed models were rerun specifying both psychological well-being and depression diagnosis as time-updated variables. All analyses were conducted using SAS statistical package version 9.4 (SAS Institute, Inc, Cary, NC), and statistical significance was set at p < 0.05, two-tailed.
Results
Descriptive Analyses
Participants were on average 64.5 years old (SD=8.75, range 50–91 years old) at baseline. There were 2,077 men and 2,680 women (56.3%), and most were White (98.9%). Individuals who were included versus excluded in the analysis had significantly higher psychological well-being and were younger at baseline. Included versus excluded individuals also had higher income, were more educated, less likely to report a high cholesterol diagnosis, and more likely to be never smokers and physically active (Supplemental Table S1). Relative to participants with low psychological well-being at Wave 2, those with higher levels earned higher incomes, were more highly educated, were less likely to report high cholesterol and depression diagnoses, had lower BMI, and were more likely to be White, never smokers, and engage in moderate or high physical activity (Table 1). Although those with higher versus lower psychological well-being reported drinking significantly more alcohol, the overall range of alcohol consumption was limited, and most individuals reported drinking alcohol only 1–2 days per week. There were no significant gender differences in levels of psychological well-being.
Table 1.
Baseline (Wave 2) covariates by tertiles of psychological well-being in the largest analytic sample. Values are either mean (SD) or N (%). N=4,757
| Overall | Psychological Well-Being Tertile at Wave 2 | p | |||
|---|---|---|---|---|---|
| Lowa | Moderateb | Highc | |||
| Age | 64.5 (8.75) | 64.7 (9.27) | 64.7 (8.75) | 64.2 (8.22) | 0.14 |
| Income | 299.3 (237.4) | 249.8 (168.9) | 304.9 (229.5) | 342.4 (287.8) | <0.001 |
| Gender | |||||
| Male | 2077 (43.7) | 720 (45.4) | 669 (43.1) | 688 (42.4) | 0.22 |
| Female | 2680 (56.3) | 865 (54.6) | 882 (56.9) | 933 (57.6) | |
| Race | |||||
| White | 4705 (98.9) | 1560 (98.4) | 1535 (99.0) | 1610 (99.3) | 0.025 |
| Non-white | 52 (1.09) | 25 (1.58) | 16 (1.03) | 11 (0.68) | |
| Education | |||||
| University degree | 669 (14.1) | 158 (9.97) | 223 (14.4) | 288 (17.8) | <0.001 |
| Higher education, no degree | 631 (13.3) | 179 (11.3) | 207 (13.4) | 245 (15.1) | |
| A-level | 335 (7.04) | 109 (6.88) | 111 (7.16) | 115 (7.09) | |
| O-level | 941 (19.8) | 295 (18.6) | 324 (20.9) | 322 (19.9) | |
| Less than O-level | 2181 (45.9) | 844 (53.3) | 686 (44.2) | 651 (40.2) | |
| High cholesterol dx | |||||
| Yes | 800 (16.8) | 297 (18.7) | 247 (15.9) | 256 (15.8) | 0.050 |
| No | 3957 (83.2) | 1288 (81.3) | 1304 (84.1) | 1365 (84.2) | |
| Depression dx | |||||
| Yes | 340 (7.15) | 190 (12.0) | 92 (5.93) | 58 (3.58) | <0.001 |
| No | 4417 (92.9) | 1395 (88.0) | 1459 (94.1) | 1563 (96.4) | |
| Body mass index (kg/m2) | 27.7 (4.76) | 28.0 (5.09) | 27.7 (4.67) | 27.5 (4.49) | 0.040 |
| Alcohol intake d | 4.96 (2.12) | 4.62 (2.20) | 5.01 (2.07) | 5.25 (2.05) | <0.001 |
| Smoking status | |||||
| Never | 1874 (39.4) | 585 (36.9) | 604 (38.9) | 685 (42.3) | <0.001 |
| Former | 2236 (47.0) | 717 (45.2) | 753 (48.6) | 766 (47.3) | |
| Current | 647 (13.6) | 283 (17.9) | 194 (12.5) | 170 (10.5) | |
| Physical activity | |||||
| Sedentary / low | 1052 (22.1) | 498 (31.4) | 327 (21.1) | 227 (14.0) | <0.001 |
| Moderate / high | 3705 (77.9) | 1087 (68.6) | 1224 (78.9) | 1394 (86.0) | |
| HDL-C (mg/dL) | 60.1 (14.9) | 58.9 (14.6) | 59.8 (14.8) | 61.4 (15.1) | 0.0003 |
| Triglycerides (mg/dL) | 159.4 (101.8) | 165.5 (100.7) | 160.4 (106.3) | 152.5 (98.0) | 0.0049 |
| Total cholesterol (mg/dL) | 235.1 (44.5) | 234.0 (43.4) | 233.3 (46.3) | 237.8 (43.7) | 0.0222 |
Note. CASP-17 = modified version of the 19-item Control, Autonomy, Satisfaction, Pleasure scale; dx = diagnosis
CASP-17≤37.2; N=1585 (33.3%)
37.4≤CASP-17≤43.7; N=1551 (32.6%)
CASP-17≥44; N=1621 (34.1%)
Alcohol intake was assessed by asking how often the respondent had an alcoholic drink during the last 12 months (almost every day; five or six days a week; three or four days a week; once or twice a week; once or twice a month; once every couple of months; once or twice a year; not at all). Responses were treated as a linear variable; higher values denote more frequent intake.
At baseline, unadjusted mean HDL-C levels were 58.9 (SD=14.6) for the lowest psychological well-being tertile, 59.8 (SD=14.8) for the middle tertile, and 61.4 (SD=15.1) for the highest tertile (p=0.0003). For the full analytic sample, Figure 1 shows unadjusted mean HDL-C levels at each wave by baseline psychological well-being tertile. When considering only the subsample of individuals with healthy HDL-C levels at baseline and HDL-C assessments at all three waves, a notable pattern emerged in HDL-C levels over follow-up according to baseline psychological well-being tertile. More participants in the lower two versus the highest tertile of psychological well-being became unhealthy (i.e., no longer met recommended levels) during the follow-up period, and the pattern appeared graded. For example, among the 545 participants in the lowest tertile, 46 (8.44%) became unhealthy whereas among the 595 participants in the middle tertile, 32 (5.38%) became unhealthy, and among the 625 participants in the highest tertile, only 28 (4.48%) became unhealthy.
Figure 1.
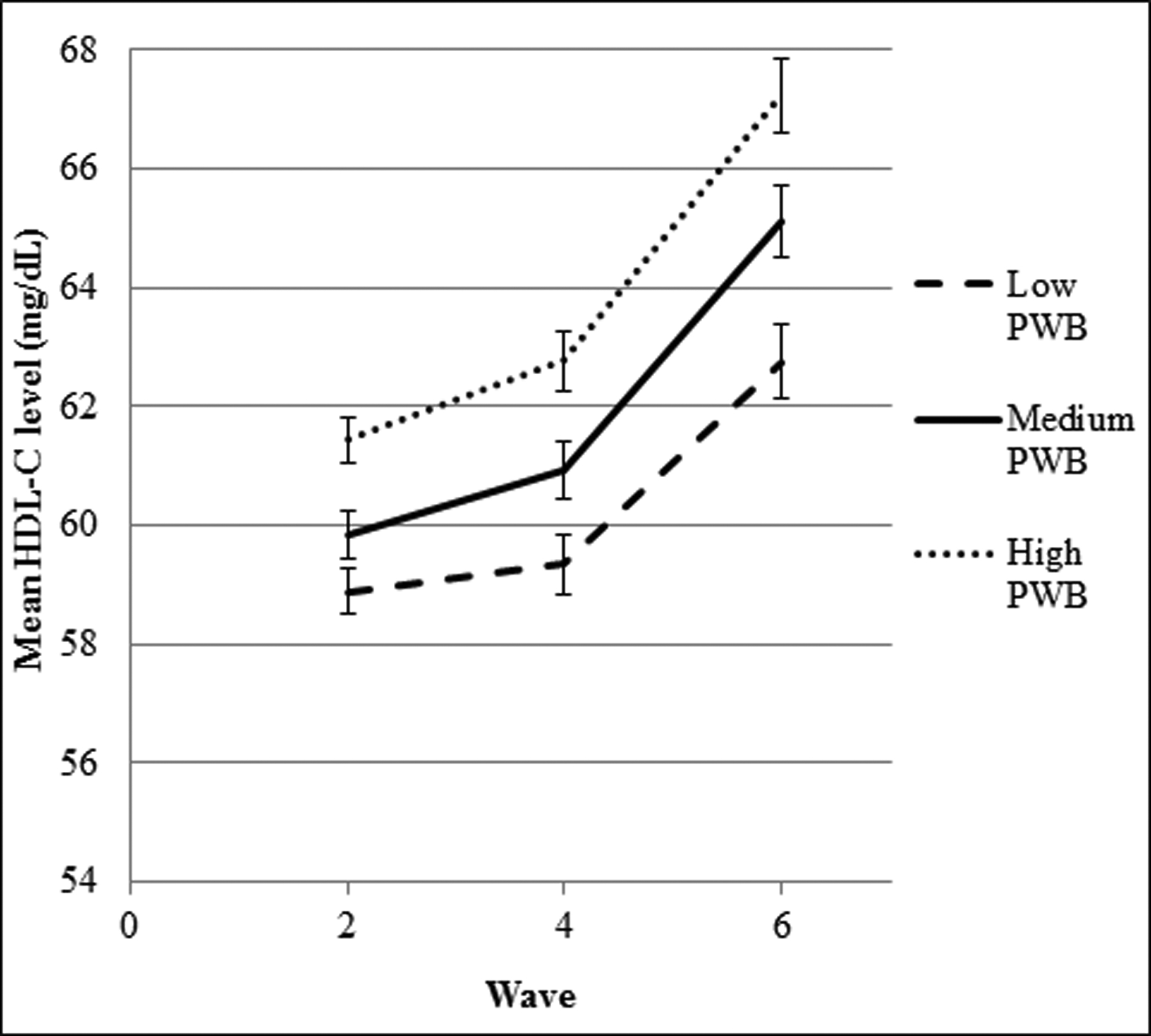
Graph of mean high-density lipoprotein cholesterol (HDL-C) over time by baseline (Wave 2) tertile of psychological well-being (PWB) in the analytic sample (N=4,756). Error bars denote the standard error.
Psychological Well-Being and Changes in HDL-C and Other Lipids over Time
In minimally-adjusted linear mixed models, baseline psychological well-being was positively associated with higher baseline HDL-C (β=1.00 for every SD increase in well-being; 95% CI = 0.53 to1.47; Table 2). HDL-C increased over time (β=0.55; 95% CI = 0.50 to 0.61). In addition, the interaction between psychological well-being and time was significant and positive (β=0.08; 95% CI = 0.03 to 0.14), indicating that HDL-C increased at a faster rate among individuals with higher versus lower psychological well-being. These associations persisted after adjusting for sociodemographic characteristics, high cholesterol and depression diagnosis, and fasting status. After adjusting for health behaviours, however, the main effect of psychological well-being was no longer significant, although the interaction between psychological well-being and time remained significant (β=0.07; 95% CI = 0.02 to 0.13).
Table 2.
Linear mixed models showing change in HDL-C over time, using psychological well-being as a continuous variable. Values are β (95% confidence interval). All covariates are obtained at Wave 2 unless otherwise indicated (N=4,756).
| Model 1 β (95% CI) |
Model 2 β (95% CI) |
Model 3 β (95% CI) |
Model 4 β (95% CI) |
|
|---|---|---|---|---|
| Psychological well-being (standardized) | 1.00 (0.53, 1.47)* | 0.60 (0.13, 1.07)* | 0.51 (0.03, 0.99)* | −0.16 (−0.61, 0.30) |
| Time (per year) | 0.55 (0.50, 0.61)* | 0.55 (0.50, 0.60)* | 0.64 (0.58, 0.69)* | 0.62 (0.56, 0.68)* |
| Psychological well-being*Time Interaction | 0.08 (0.03, 0.14)* | 0.08 (0.02, 0.14)* | 0.07 (0.02, 0.13)* | 0.07 (0.02, 0.13)* |
| Age (per year) | 0.01 (−0.04, 0.05) | 0.08 (0.03, 0.12)* | 0.12 (0.07, 0.17)* | 0.07 (0.02, 0.12)* |
| Gender (women as ref) | −11.1 (−11.9, −10.2)* | −11.7 (−12.6, −10.9)* | −11.8 (−12.6, −11.0)* | −12.9 (−13.7, −12.1)* |
| Race (White as ref) | 3.10 (−0.80, 6.99) | 2.81 (−1.04, 6.67) | 2.97 (−0.87, 6.81) | 4.98 (1.40, 8.56)* |
| Income (standardized) | 0.94 (0.44, 1.44)* | 0.90 (0.40, 1.40)* | 0.43 (−0.04, 0.90)† | |
| Education (less than O-level as ref) | ||||
| University degree | 5.70 (4.36, 7.03)* | 5.69 (4.36, 7.03)* | 2.54 (1.27, 3.81)* | |
| Higher education, no degree | 2.54 (1.25, 3.82)* | 2.49 (1.21, 3.76)* | 0.95 (−0.24, 2.15) | |
| A-level | 2.10 (0.44, 3.75)* | 2.07 (0.42, 3.72)* | 0.83 (−0.71, 2.36) | |
| O-level | 2.31 (1.21, 3.42)* | 2.30 (1.20, 3.40)* | 0.61 (−0.42, 1.65) | |
| High cholesterol dxa (no dx as ref) | −1.49 (−2.07, −0.92)* | −1.28 (−1.84, −0.72)* | ||
| Fasting statusa (nonfasting as ref) | 2.34 (1.89, 2.79)* | 2.15 (1.71, 2.59)* | ||
| Depression dx (no dx as ref) | −0.25 (−1.86, 1.35) | −0.10 (−1.59, 1.40) | ||
| Body mass index (per kg/m2) | −0.81 (−0.89, −0.73)* | |||
| Alcohol intake | 1.53 (1.34, 1.72)* | |||
| Smoking status (never smoker as ref) | ||||
| Former | −0.38 (−1.20, 0.44) | |||
| Current | −2.85 (−4.05, −1.66)* | |||
| Moderate/high physical activity (sedentary/low as ref) | 0.98 (0.03, 1.92)* |
Note. HDL-C = high-density lipoprotein cholesterol; ref = reference; dx = diagnosis
Time-updated (taken concurrent with lipid measure)
p < 0.05,
p < 0.10
Findings were similar with tertiled psychological well-being and suggested a dose-response relationship (Table 3). Individuals with moderate versus low levels of psychological well-being had non-significantly higher baseline HDL-C in the minimally-adjusted model. However, individuals in the highest tertile had significantly higher baseline HDL-C, and this effect persisted after adjusting for sociodemographic characteristics, high cholesterol and depression diagnosis, and fasting status (β=1.12; 95% CI = 0.05 to 2.20). The interaction between tertiled psychological well-being and time was also significant for both high and moderate versus low psychological well-being, with the magnitude of the effect for the highest tertile greater than that for the moderate tertile. After adjusting for health behaviours, the main effect of tertiled psychological well-being again was no longer significant; the interaction between moderate psychological well-being and time was marginally significant; and the interaction between high psychological well-being and time was statistically significant. For all models presented in Tables 2 and 3, variance estimates of the intercept were statistically significant, indicating between-person differences in the extent to which individuals differed in baseline lipid levels and supporting the use of a random intercept model.
Table 3.
Linear mixed models showing change in HDL-C over time, using psychological well-being as a tertiled categorical variable. Values are β (95% confidence interval) (N=4,756).
| Model 1 β (95% CI) |
Model 2 β (95% CI) |
Model 3 β (95% CI) |
Model 4 β (95% CI) |
|
|---|---|---|---|---|
| Psychological well-being (low as ref) | ||||
| Moderate | 0.61 (−0.47, 1.69) | 0.04 (−1.03, 1.12) | −0.07 (−1.14, 1.01) | −0.79 (−1.81, 0.22) |
| High | 2.21 (1.15, 3.28)* | 1.33 (0.26, 2.40)* | 1.12 (0.05, 2.20)* | −0.10 (−1.13, 0.92) |
| Time (per year) | 0.44 (0.35, 0.53)* | 0.44 (0.35, 0.53)* | 0.54 (0.44, 0.63)* | 0.52 (0.43, 0.61)* |
| Psychological well-being*time interaction (low × time as ref) | ||||
| Moderate × time | 0.16 (0.03, 0.28)* | 0.15 (0.02, 0.28)* | 0.13 (0.01, 0.26)* | 0.13 (−0.001, 0.25)† |
| High × time | 0.21 (0.09, 0.34)* | 0.21 (0.08, 0.34)* | 0.20 (0.07, 0.32)* | 0.20 (0.08, 0.33)* |
Note. HDL-C = high-density lipoprotein cholesterol; ref = reference
Model 1 adjusted for baseline (Wave 2) age, gender, and race.
Model 2 additionally adjusted for baseline income and education.
Model 3 additionally adjusted for time-updated high cholesterol diagnosis, time-updated fasting status, and baseline depression diagnosis.
Model 4 additionally adjusted for baseline body mass index, alcohol intake, smoking status, and physical activity.
p < 0.05,
p < 0.10
Psychological well-being (as a continuous variable) was negatively associated with triglycerides, even after adjusting for sociodemographic characteristics, high cholesterol and depression diagnosis, and fasting status (β=−4.20; 95% CI = −7.03 to −1.37). Triglycerides decreased over time (β=−4.52; 95% CI = −4.95 to −4.08), and the interaction between psychological well-being and time was not significant. The main effect of psychological well-being was substantially attenuated after adjusting for health behaviours (β=−1.84; 95% CI = −4.65 to 0.97). The main effect of psychological well-being on total cholesterol was not significant in any model. Although total cholesterol also decreased significantly over time, the interaction term between psychological well-being and time was not significant in any model.
To mitigate concerns that healthy behaviours might lead to higher psychological well-being rather than vice versa, the linear mixed models were re-run with time-updated health behaviours taken from the wave immediately prior to the wave in which lipids were assessed. Results were similar to those from analyses using only baseline behaviours, with an attenuation of psychological well-being’s effects after including behaviours in the models.
Additional Analyses
In sensitivity analyses that removed individuals with only one lipid measurement from the mixed models (3,282 individuals remained in the HDL-C analysis; 3,283 in the triglycerides and cholesterol analyses), results were qualitatively similar for triglycerides and total cholesterol. For HDL-C, results were also similar; however, the main effect of psychological well-being did not reach statistical significance in the model adjusting for sociodemographics, high cholesterol and depression diagnosis, and fasting status (β=0.53; 95% CI = −0.06 to 1.12). Given the similar effect estimate with a smaller sample size, this attenuation could be attributable to lack of power.
In the minimally-adjusted mixed model for HDL-C with interaction terms between gender, psychological well-being, and time, the three-way interaction was not significant. The gender by psychological well-being interaction was not significant as well. However, the gender by time interaction was significant (β=−0.13 for males versus females; 95% CI = −0.24 to −0.03), indicating that HDL-C increased at a slower rate over time for men versus women. Results for triglycerides and total cholesterol also showed that only the gender by time interaction was significant, in that triglycerides and total cholesterol decreased faster over time in men than women. This pattern persisted even after adjusting for all covariates.
Mixed models for HDL-C with time-updated psychological well-being and time-updated depression (Supplemental Table S2) showed attenuated main effects of psychological well-being on HDL-C, but significant interactions between psychological well-being and time in all models. Models produced similar results to the original analyses for triglycerides and total cholesterol. Furthermore, the CASP-17 had an intraclass correlation of 0.66 in the analytic sample, and the Pearson correlation coefficients for psychological well-being between persons at any two time points over Waves 2, 4, and 6 ranged from 0.61 to 0.71. These results suggest well-being was relatively stable over time.
Discussion
To the investigators’ knowledge, this study is the first to examine the associations between psychological well-being and changes in objectively measured HDL-C (and other lipid) levels over time. Somewhat surprisingly, HDL-C increased over the follow-up period while triglycerides and total cholesterol decreased; but this result has been previously documented in ELSA (Banks, Nazroo, & Steptoe, 2014). Another study in the Framingham Heart Offspring Cohort also found similar increases in HDL-C and decreases in triglycerides over time (Ingelsson et al., 2009). Authors in that study hypothesized that certain secular dietary changes, including a reduction in total fats and particularly saturated fats, could result in enzymatic activity that leads to both an increased formation of HDL-C and a reduction in triglycerides. While the Framingham study included individuals who were an average of 10 years younger than those in the present study, similar physiologic or behaviour-related changes could continue operating into older ages.
In the present study, individuals with the highest versus lowest baseline levels of psychological well-being had the healthiest HDL-C and were less likely to show declines below recommended HDL-C levels. Moreover, higher psychological well-being was associated with healthier HDL-C trajectories. Those in the highest versus lowest tertile experienced a significantly faster rate of increase in HDL-C over time, with HDL-C levels that were, on average, a little over 3 mg/dL higher after 10 years of follow-up, controlling for a broad range of covariates. Analyses with tertiled psychological well-being were consistent with those using the continuous measure of psychological well-being and showed a possible dose-response relationship; these findings echo previous research that has found a graded relationship between one specific facet of psychological well-being—optimism—and reduced incidence of heart failure (Kim, Smith, & Kubzansky, 2014). Higher psychological well-being was also associated with healthier triglyceride levels. Although some research suggests that psychological well-being is related to different health-related biological mechanisms in men versus women (Steptoe, Demakakos, de Oliveira, & Wardle, 2012), there was no evidence of gender differences in associations between psychological well-being and changes in lipids over time.
Although the effect sizes found in this study were relatively small, previous research has reported that decreases in BMI, moderate alcohol consumption, and decreases in sedentary time have similarly sized associations with HDL-C (Cooper et al., 2011; Holmes et al., 2014; Rahilly-Tierney, Sesso, Djoussé, & Gaziano, 2011). Evidence suggests that a 1 mg/dl increase in HDL-C is associated with a 2–3% decrease in cardiovascular risk (Gordon et al., 1989). Thus, even the seemingly small difference in HDL-C that individuals with high versus low levels of psychological well-being showed (on average 3 mg/dL) could give rise to different trajectories in HDL-C across longer periods of time. If psychological well-being is associated with healthier HDL-C and, in turn, reduces the burden of cardiovascular disease by 6–9%, then these associations would be meaningful at the population level, where millions of people worldwide are burdened by cardiovascular disease.
In this study, associations between psychological well-being and HDL-C were attenuated after accounting for BMI and health-related behaviours, which is consistent with the speculation that health behaviours lie on the pathway linking psychological well-being and healthy HDL-C (Kubzansky, Boehm, & Segerstrom, 2015; Boehm, Williams, Rimm, Ryff, & Kubzansky, 2013). This finding may have occurred because individuals with higher psychological well-being have more energy and motivation to engage in healthy habits and have the psychological resources to make healthier behavioural choices. This reasoning is supported by empirical evidence. For example, one study of individuals with coronary heart disease reported that associations between positive affect and improved survival were largely mediated by physical activity (Hoen, Denollet, de Jonge, & Whooley, 2013). Another study found that associations between higher positive affect or life satisfaction and lower C-reactive protein, another biomarker of cardiovascular health, may be mediated by exercise and BMI (Ironson, Banerjee, Fitch, & Krause, 2018). Prior research also indicates that psychological well-being is related to lower prevalence of smoking, more physical activity, and better medication adherence (Grant, Wardle, & Steptoe, 2009; Sin, Moskowitz, & Whooley, 2015). Furthermore, one prospective study in ELSA found robust associations between initial psychological well-being and physical activity over time but limited evidence of reverse causality (Kim, Kubzansky, Soo, & Boehm, 2016). The present study supports the possibility that psychological well-being could precede the health behaviours that may serve as mechanisms between the well-being and lipid association.
Health behaviours could also be associated with healthier lipid profiles and decreased cardiovascular risk through a variety of biological mechanisms or changes in biomarker synthesis, metabolism, or clearance (Van Gaal, Mertens, & De Block, 2006). For example, physical inactivity may be associated with unhealthy HDL-C levels via changes in insulin resistance and glucose metabolism (Wannamethee, Shaper, & Alberti, 2000); cigarette smoking has shown associations with lipids by contributing to atherosclerotic changes and narrowing of the vascular lumen (U.S. Department of Health and Human Services, 2010).
Although changes in health behaviours are associated with changes in lipids (Rahilly-Tierney, Sesso, Djoussé, & Gaziano, 2011), identifying upstream determinants of behavioural risk and protective factors is critical. Cardiovascular medicine has called for a primordial approach to prevention in which the focus is on stopping risk factors from becoming established. Once risk factors are in place they can be persistent, difficult to eradicate, and impose substantial elevation in lifetime risk of cardiovascular disease (Lloyd-Jones et al., 2010). Identifying assets or factors that promote health more generally may also be more efficient than targeting single risk factors since such assets could serve as upstream determinants of many proximate factors. Prior work has suggested that psychological well-being, like other cognitive or personality attributes, is moderately plastic and can change (Mroczek, 2014). Other work has shown that aspects of psychological well-being are modifiable with strategies such as expressing gratitude or engaging in cognitive behavioural therapy (Boehm, Vie, & Kubzansky, 2012). Future research could explore whether psychological well-being may provide a novel target for intervention with potentially beneficial effects for both psychological and physical health.
Limitations
This study has some limitations. The analytic sample consisted of a homogeneous group of almost entirely white English men and women over age 50; thus, generalizability is limited with regard to other races, nationalities, and ages. Individuals in the sample also had higher psychological well-being and were younger, more socioeconomically advantaged, and healthier at baseline compared to those who were excluded. More disadvantaged and less healthy individuals may have dropped out of the study at disproportionate rates compared to their healthier counterparts, thereby contributing less data to the mixed-models analysis. However, revisit propensity scores were used to weight these models and account for this selective drop out, and sensitivity analyses excluding participants with one lipid measure did not significantly alter the findings. Also, data on cholesterol medication was not available at this study’s baseline. While doctor diagnosis of high cholesterol was used as a proxy, this variable may not fully capture changes in lipid levels due to pharmacological intervention. Finally, relationships between psychological well-being and health behaviours are likely bidirectional; however, due to limited follow-up, analyses did not formally test for mediation of the psychological well-being and lipid relationship. Future research should assess if health behaviours mediate the relation between psychological well-being and health-related biomarkers, and which behaviours, if any, are primarily responsible.
These limitations are balanced by strengths including a prospective design that involved up to 9 years of follow-up and excluded people with pre-existing cardiovascular disease. In addition, health-related items were excluded from the psychological well-being measure because such items could bias associations if unhealthy lipid levels were indicative of subclinical or new cardiovascular disease. Analyses also accounted for the possibility of selective drop-out and controlled for depression and high-cholesterol diagnoses. Thus, effects of psychological well-being may be independent from the influence of poor health and persist even when individuals may be taking measures to reduce high lipid levels, either by medication or behavioural change.
Conclusion
This study’s findings indicated that higher psychological well-being was associated with healthier HDL-C trajectories in older people. Evidence has linked subjective measures of psychological well-being to improved cardiovascular health and increased longevity (Steptoe, Deaton, & Stone, 2015). These analyses expand upon this literature by providing a mechanism for this association, specifically that psychological well-being is associated with healthier trajectories of HDL-C levels across time. As opposed to simply preventing the occurrence of disease or ill health, psychological well-being could play a role in actively stimulating biological processes that help to restore, recover, and enhance physical function (Boehm & Kubzansky, 2012). The current study shows that higher psychological well-being is related to healthier biological function (as characterized by HDL-C), which may lead to improved health not simply by avoiding disease but by actively promoting cardiovascular health.
Supplementary Material
Research Highlights.
First longitudinal study to examine psychological well-being and lipid trajectories.
Psychological well-being is associated with healthier lipids in older adults.
Protective effects may partly be explained by health behaviours.
Lipids may represent one mechanism linking well-being with health and longevity.
Funding
This work was supported by the National Institute on Aging (R03AG046342) and the National Cancer Institute (3R25CA057711) at the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the views of the National Institutes of Health.
Footnotes
Other declarations of interest: none
References
- Banks J, Nazroo J, & Steptoe A (2014). The dynamics of ageing: Evidence from the English Longitudinal Study of Ageing 2002–12 (Wave 6). The Institute for Fiscal Studies: English Longitudinal Study of Ageing. Retrieved from http://www.elsa-project.ac.uk/publicationDetails/id/7411 [Google Scholar]
- Boehm JK, & Kubzansky LD (2012). The heart’s content: the association between positive psychological well-being and cardiovascular health. Psychological Bulletin, 138, 655–691. 10.1037/a0027448 [DOI] [PubMed] [Google Scholar]
- Boehm JK, Vie LL, & Kubzansky LD (2012). The promise of well-being interventions for improving health risk behaviors. Current Cardiovascular Risk Reports, 6, 511–519. 10.1007/s12170-012-0273-x [DOI] [Google Scholar]
- Boehm JK, Williams DR, Rimm EB, Ryff C, & Kubzansky LD (2013). Relation between optimism and lipids in midlife. The American Journal of Cardiology, 111, 1425–1431. 10.1016/j.amjcard.2013.01.292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boekholdt SM, Arsenault BJ, Hovingh GK, Mora S, Pedersen TR, Larosa JC, … Kastelein JJ (2013). Levels and changes of HDL cholesterol and apolipoprotein A-I in relation to risk of cardiovascular events among statin-treated patients: a meta-analysis. Circulation, 128, 1504–1512. 10.1161/CIRCULATIONAHA.113.002670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper AR, Sebire S, Montgomery AA, Peters TJ, Sharp DJ, Jackson N, … Andrews RC (2011). Sedentary time, breaks in sedentary time and metabolic variables in people with newly diagnosed type 2 diabetes. Diabetologia, 55, 589–599. 10.1007/s00125-011-2408-x [DOI] [PubMed] [Google Scholar]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. (2001). Executive summary of the third report of the National Cholesterol Education Program (NCEP). JAMA, 285, 2486–2497. 10.1001/jama.285.19.2486 [DOI] [PubMed] [Google Scholar]
- Farrelly C (2012). “Positive biology” as a new paradigm for the medical sciences. EMBO Reports, 13, 186–188. 10.1038/embor.2011.256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, … Tyroler HA (1989). High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation, 79, 8–15. 10.1161/01.CIR.79.1.8 [DOI] [PubMed] [Google Scholar]
- Graig R, Deverill C, & Pickering K (2006). Quality control of blood saliva and urine analytes. In Health survey for England 2004, Methodology and documentation, vol 2 (pp. 34–41). London: The Information Centre. [Google Scholar]
- Grant N, Wardle J, & Steptoe A (2009). The relationship between life satisfaction and health behavior: a cross-cultural analysis of young adults. International Journal of Behavioral Medicine, 16, 259–268. 10.1007/s12529-009-9032-x [DOI] [PubMed] [Google Scholar]
- Heiss G, Tamir I, Davis CE, Tyroler HA, Rifkand BM, Schonfeld G, … Frantz ID (1980). Lipoprotein-cholesterol distributions in selected North American populations: the lipid research clinics program prevalence study. Circulation, 61, 302–315. 10.1161/01.CIR.61.2.302 [DOI] [PubMed] [Google Scholar]
- Hoen PW, Denollet J, de Jonge P, & Whooley MA (2013). Positive affect and survival in patients with stable coronary heart disease: findings from the Heart and Soul Study. The Journal of Clinical Psychiatry, 74, 716–722. 10.4088/JCP.12m08022 [DOI] [PubMed] [Google Scholar]
- Hogan JW, & Lancaster T (2004). Instrumental variables and inverse probability weighting for causal inference from longitudinal observational studies. Statistical Methods in Medical Research, 13, 17–48. 10.1191/0962280204sm351ra [DOI] [PubMed] [Google Scholar]
- Holmes MV, Lange LA, Palmer T, Lanktree MB, North KE, Almoguera B, … Keating BJ (2014). Causal effects of body mass index on cardiometabolic traits and events: a Mendelian randomization analysis. The American Journal of Human Genetics, 94, 198–208. 10.1016/j.ajhg.2013.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howel D (2012). Interpreting and evaluating the CASP-19 quality of life measure in older people. Age and Ageing, 41, 612–617. 10.1093/ageing/afs023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde M, Wiggins RD, Higgs P, & Blane DB (2003). A measure of quality of life in early old age: the theory, development and properties of a needs satisfaction model (CASP-19). Aging & Mental Health, 7, 186–194. 10.1080/1360786031000101157 [DOI] [PubMed] [Google Scholar]
- Infurna FJ, & Gerstorf D (2014). Perceived control relates to better functional health and lower cardio-metabolic risk: the mediating role of physical activity. Health Psychology, 33, 85–94. 10.1037/a0030208 [DOI] [PubMed] [Google Scholar]
- Ironson G, Banerjee N, Fitch C, & Krause N Positive emotional well-being, health behaviors, and inflammation measured by C-Reactive Protein. Social Science & Medicine, 197, 235–243. 10.1016/j.socscimed.2017.06.020. [DOI] [PubMed] [Google Scholar]
- Kim ES, Smith J, & Kubzansky LD (2014). A prospective study of the association between dispositional optimism and incident heart failure. Circulation: Heart Failure, 7, 394–400. 10.1161/CIRCHEARTFAILURE.113.000644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim ES, Kubzansky LD, Soo J, & Boehm JK (2016). Maintaining healthy behavior: a prospective study of psychological well-being and physical activity. Annals of Behavioral Medicine. 10.1007/s12160-016-9856-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubzansky LD, Winning A, & Kawachi I (2014). Affective states and health. In Berkman LF, Glymour MM, & Kawachi I (Eds.), Social epidemiology: New perspectives on social determinants of global population health, 2nd (pp. 320–364). New York: Oxford University Press. [Google Scholar]
- Kubzansky LD, Boehm JK, & Segerstrom SC (2015). Positive psychological functioning and the biology of health. Social and Personality Psychology Compass, 9, 645–660. 10.1111/spc3.12224 [DOI] [Google Scholar]
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, … American Heart Association Strategic Planning Task Force and Statistics Committee. (2010). Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation, 121, 586–613. 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- Mroczek DK (2014). Personality plasticity, healthy aging, and interventions. Developmental Psychology, 50, 1470–1474. 10.1037/a0036028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rader DJ, & Hovingh GK (2014). HDL and cardiovascular disease. The Lancet, 384, 618–625. 10.1016/S0140-6736(14)61217-4 [DOI] [PubMed] [Google Scholar]
- Rahilly-Tierney C, Sesso HD, Djoussé L, & Gaziano JM (2011). Lifestyle changes and 14-year change in high-density lipoprotein cholesterol in a cohort of male physicians. American Heart Journal, 161, 712–718. 10.1016/j.ahj.2010.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal R (1990). How are we doing in soft psychology? American Psychologist, 45, 775–777. 10.1037/0003-066X.45.6.775 [DOI] [Google Scholar]
- Rozanski A (2014). Behavioral cardiology: current advances and future directions. Journal of the American College of Cardiology, 64, 100–110. 10.1016/j.jacc.2014.03.047 [DOI] [PubMed] [Google Scholar]
- Rye KA, & Barter PJ (2014). Cardioprotective functions of HDLs. Journal of Lipid Research, 55, 168–179. 10.1194/jlr.R039297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff CD (2014). Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychotherapy and Psychosomatics, 83, 10–28. 10.1159/000353263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks FM, & Jensen MK (2018). From high-density lipoprotein cholesterol to measurements of function: prospects for the development of tests for high-density lipoprotein functionality in cardiovascular disease. Arteriosclerosis, Thrombosis, and Vascular Biology. Advance online publication. 10.1161/ATVBAHA.117.307025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin NL, Moskowitz JT, & Whooley MA (2015). Positive affect and health behaviors across 5 years in patients with coronary heart disease: the Heart and Soul Study. Psychosomatic Medicine, 77, 1058–1066. 10.1097/PSY.0000000000000238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [Dataset] Steptoe A, Breeze E, Banks J, & Nazroo J (2013). Cohort profile: the English Longitudinal Study of Ageing. International Journal of Epidemiology, 42, 1640–1648. 10.1093/ije/dys168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Deaton A, & Stone AA (2015). Subjective wellbeing, health, and ageing. Lancet, 385, 640–648. 10.1016/S0140-6736(13)61489-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Demakakos P, de Oliveira C, & Wardle J (2012). Distinctive biological correlates of positive psychological well-being in older men and women. Psychosomatic Medicine, 74, 501–508. 10.1097/PSY.0b013e31824f82c8 [DOI] [PubMed] [Google Scholar]
- UK Activity and Health Research. (1992). Allied Dunbar National Fitness Survey: main findings. London: Sports Council and Health Education Authority. [Google Scholar]
- U.S. Department of Health and Human Services. (2010). How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK53017/ [PubMed] [Google Scholar]
- Van Gaal LF, Mertens IL, & De Block CE (2006). Mechanisms linking obesity with cardiovascular disease. Nature, 444, 875–880. 10.1038/nature05487 [DOI] [PubMed] [Google Scholar]
- Van Reedt Dortland AK, Giltay EJ, van Veen T, Zitman FG, & Penninx BW (2013). Longitudinal relationship of depressive and anxiety symptoms with dyslipidemia and abdominal obesity. Psychosomatic Medicine, 75, 83–89. 10.1097/PSY.0b013e318274d30f. Epub 2012 Nov 28. [DOI] [PubMed] [Google Scholar]
- Wannamethee SG, Shaper AG, & Alberti KG (2000). Physical activity, metabolic factors, and the incidence of coronary heart disease and type 2 diabetes. Archives of Internal Medicine, 160, 2108–2116. 10.1001/archinte.160.14.2108 [DOI] [PubMed] [Google Scholar]
- WHO. (2008). The global burden of disease: 2004 update. Retrieved from http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/
- WHO. (2017). Cardiovascular diseases (CVDs). Retrieved from http://www.who.int/mediacentre/factsheets/fs317/en/
- Wiggins RD, Netuveli G, Hyde M, Higgs P, & Blane D (2008). The evaluation of a self-enumerated scale of quality of life (CASP-19) in the context of research on ageing: a combination of exploratory and confirmatory approaches. Social Indicators Research, 89, 61–77. 10.1007/s11205-007-9220-5 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


