Abstract
Objective
To examine the effect of the COVID-19 pandemic on maternal substance abuse and neonatal outcomes.
Study design
Cross-sectional observational study of neonates admitted to the NICU and born to mothers with evidence of substance abuse pre-pandemic compared to during the COVID-19 pandemic.
Result
We noted a significant increase in fentanyl (12% vs. 0.6%, p < 0.001) and tobacco use (64% vs. 33%, p < 0.001) during the pandemic compared to pre-pandemic, including an increase in fentanyl use among mothers enrolled in opioid maintenance therapy (OMT) during the pandemic (32.3% vs. 1.5%, p < 0.001). There was a significant increase in preterm births (58% vs. 48%, p = 0.022) and lower birth weight (2315 ± 815 vs. 2455 ± 861 g, p = 0.049) during pandemic.
Conclusion
There was a significant increase in maternal fentanyl use during the pandemic, even with OMT enrollment, with an increase in preterm births and lower birth weights among infants born to mothers with substance use.
Subject terms: Medical research, Health care
Introduction
The COVID-19 pandemic changed access to global maternity care with a noted reduction in antenatal care services utilized [1] even with the introduction and availability of telemedicine [2]. Occurring in parallel to the COVID-19 pandemic was the increasing incidence of opioid use/abuse. Since 2013, the United States has seen an increase in synthetic opioid-related deaths [3] with a significant rise during the COVID-19 pandemic [4].
With the ongoing COVID-19 and concomitant opioid pandemics, pregnant women with opioid use disorder (OUD) were a particularly vulnerable population. In addition to facing challenges with accessing routine and specialized care, they also experienced an increasing number of stressors (concerns with becoming infected and ill with COVID-19, employment, finances, social isolation, etc.), leading to higher rates of depression and anxiety [5–9]. While there is emerging literature regarding substance use during the COVID-19 pandemic in pregnant women, there is little to no literature discussing changes in neonatal outcomes in relation to maternal substance use, specifically opioid use, before versus during the COVID-19 pandemic.
The primary purposes of the current study were to: (1) evaluate the impact of COVID-19 on maternal substance use by comparing the two time periods (two years prior to the pandemic compared to two years into the pandemic) and (2) examine the effects of the suspected increase in maternal substance use, in particular opioid use, on neonatal outcomes.
Subjects and methods
This is a cross-sectional observational study at a level III neonatal intensive care unit (NICU) at Regional One Health (ROH) hospital in Memphis, Tennessee. ROH is a regional tertiary perinatal center and provides services to high-risk pregnancy and low-income mothers. This study was dual approved by the Institutional Review Board (IRB) of the University of Tennessee Health Science Center (UTHSC) and hospital IRB. The current data are abstracted from an ongoing observational study of maternal substance use (Study title: “Maternal Prescription, Illicit or Recreational Substance Use and Infant Outcomes—An Observational Study”). Informed consent was waived with IRB approval.
Study population
Mothers and their respective infants were included if there was a positive active or recent history of maternal substance use during the concurrent pregnancy. Maternal substance use was recorded by self-reported drug use or presence of positive results on maternal urine drug screen (recent or on admission), neonatal urine drug screen, or neonatal umbilical cord drug screen. Specifically, “substance use” referred to the use of amphetamine, cocaine, heroin, tobacco, marijuana, alcohol, other opioids, or benzodiazepines. We compared cohorts from before the start of the COVID-19 pandemic (those admitted from January 2018 to December 2019) and during the COVID-19 pandemic (those admitted from January 2020 to April 2021). Per institutional NICU guidelines, all newborns with evidence of prenatal opioid exposure, whether through onset of withdrawal symptoms or based on maternal history and/or urine drug screen, are admitted to NICU for observation for neonatal opioid withdrawal syndrome (NOWS) for 5–7 days or longer duration if treatment for withdrawal was needed. In 2007, our NICU developed internal guidelines for the management of NOWS, and no changes to the guidelines were made during the study period. A recent practice for infants born to mothers with OUD encourages the “Eat, Sleep, Console” method, breastfeeding, and rooming-in to allow mothers to bond with their infants, reduce pharmacological intervention, and decrease duration of hospital stay [10]. However, since we were not equipped to monitor maternal drug use during the infant’s stay, no rooming-in was provided. Instead, we encouraged parents and immediate designated family members to visit and stay with the infant as long and as often as their lifestyle allowed [11]. At the time of the study, institution guidelines utilized the modified Finnegan scoring (mFS) method for evaluation of infants [12]. There was no change in method of NOWS observation or treatment guidelines during the study period.
Outcomes and variables
The primary outcome measures were prevalence of maternal substance use and associated neonatal outcomes, including gestational age and birth weight, during the first two years of the COVID-19 pandemic compared to two years prior to the COVID-19 pandemic. Our secondary outcomes were changes in maternal substance use, specifically fentanyl, and correlation of its use with other substances as well as associated neonatal outcomes. Mothers with OUD were identified and information on maternal opioid maintenance therapy (OMT) was collected, including the therapy used (methadone or buprenorphine) and duration of treatment at time of delivery. Data were also collected on maternal and infant demographics, diagnosis and pharmacological treatment of NOWS, discharge weight, and length of stay.
Statistical analysis
The patients were first stratified by when they gave birth: prior to the COVID-19 pandemic versus during the COVID-19 pandemic. Data were summarized as mean and standard deviation (SD) or count and percentage. Normally distributed continuous variables were compared between the two periods using a one-way ANOVA, and categorical variables were compared using the Fisher’s Exact test. A subset was created for fentanyl positive patients and the analysis was repeated. A p-value ≤0.05 was considered statistically significant. All analyses were conducted in R version 3.6.0 (2020-02-29).
Results
We identified 330 mother-infant dyads pre-pandemic and 240 mother-infant dyads during the pandemic who met inclusion criteria. Maternal demographics are shown in Table 1.
Table 1.
Maternal demographics.
| Pre-pandemic N = 330 | During pandemic N = 240 | P value | |
|---|---|---|---|
| Mean maternal age, years | 28.5 ± 5.5 | 28.2 ± 5.5 | 0.60 |
| Highest reported education level, n (%) | 0.72 | ||
| Less than high school | 111 (35) | 87 (38) | |
| High school degree | 164 (51) | 114 (50) | |
| Some college or post-graduate | 46 (14) | 29 (13) | |
| No prenatal care, n (%) | 75 (23) | 53 (22) | 0.92 |
| Maternal employment, n (%) | 52 (16) | 43 (18) | 0.17 |
| Caesarean delivery, n (%) | 143 (43) | 120 (50) | 0.21 |
Results reported as mean ± SD or count/number n (%).
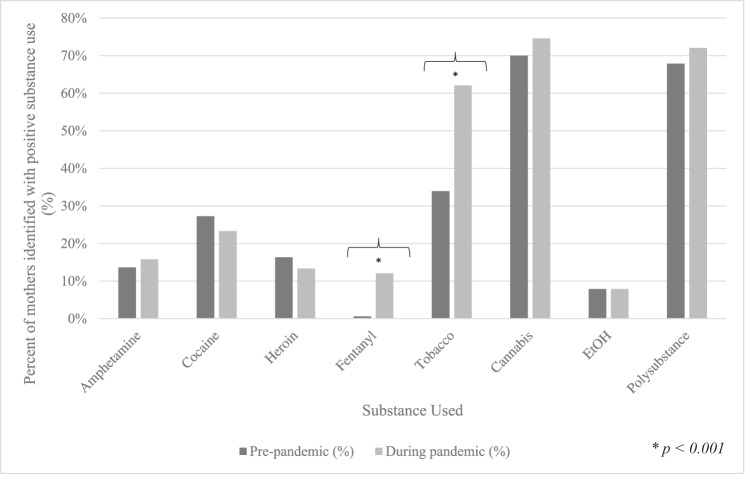
Method of detection for substance use, prevalence of maternal OMT, and infant demographics and outcomes are reported in Table 2. Figure 1 compares types of maternal substance use from pre-pandemic to during the COVID-19 pandemic. There was a significant increase in fentanyl (12.2% vs. 0.6%, p < 0.001) and tobacco use (63.5% vs. 33.4%, p < 0.001) during the pandemic compared to pre-pandemic. Fewer mothers were actively enrolled in OMT during pandemic (14% vs. 20%, p = 0.08). There was a significant increase in fentanyl use among pregnant women enrolled in OMT during the pandemic compared to pre-pandemic [32.3% (11/34) vs. 1.5% (1/66), p < 0.001]. Though there were similar mean gestational ages, the incidence of preterm birth (58% vs. 48%, p = 0.02) was significantly higher during the pandemic. Incidence of NOWS was similar during the pandemic compared to pre-pandemic.
Table 2.
Maternal substance use and infant outcomes.
| Pre-pandemic N = 330 | During pandemic N = 240 | P value | |
|---|---|---|---|
| Substance use, n (%) | |||
| Maternal self-reported use | 281 (85) | 216 (90) | 0.10 |
| Maternal UDSb | 268 (90) | 185 (90) | 0.88 |
| Infant UDSb | 144 (54) | 100 (50) | 0.40 |
| UCDSc | 247 (88) | 186 (92) | 0.18 |
| Opioid maintenance therapy, n (%) | 66 (20) | 34 (14) | 0.08 |
| Mean gestational age, weeks | 35.4 ± 4.0 | 35.0 ± 4.0 | 0.25 |
| Premature birth, n (%) | 159 (48) | 139 (58) | 0.02 |
| Male sex, n (%) | 163 (49) | 115 (52) | 0.73 |
| Median APGAR scores [IQRa] | |||
| 1 minute | 8 [6–8] | 8 [6–9] | 0.84 |
| 5 minutes | 9 [8,9] | 9 [8,9] | 0.92 |
| Mean length of stay, days | 19.6 ± 21.8 | 20.9 ± 28.3 | 0.51 |
| Mean birth weight, grams | 2455.4 ± 860.8 | 2314.8 ± 815.3 | 0.05 |
| Mean discharge weight, grams | 2748.2 ± 772.8 | 2665.4 ± 804.9 | 0.22 |
| NOWSd diagnosis, n (%) | 52 (16) | 48 (20) | 0.22 |
Results reported as mean ± SD, count/number n (%), or median [IQR]. aIQR interquartile range, bUDS urine drug screen, cUCDS umbilical cord drug screen, dNOWS neonatal opioid withdrawal syndrome.
Fig. 1. Comparison of maternal substance use pre-pandemic versus during the pandemic.
Bars are represented as the prevalence of the specific substance used out of mothers identified with overall substance use for that time period. * indicates statistical significance with p < 0.001.
Out of those who met initial inclusion criteria, there were 2 mother-infant dyads pre-pandemic and 29 mother-infant dyads during the pandemic who were further stratified into a fentanyl cohort. Maternal demographics, method of detection for substance use, and use of OMT for the fentanyl cohort can be found in Supplemental Table 1. Mean gestational ages were 34.0 ± 1.4 and 35.6 ± 3.0 (p = 0.48) and mean birth weights were 2520.0 ± 42.4 grams and 2454.4 ± 694.6 grams (p = 0.90) for pre-pandemic and during the pandemic, respectively. When looking at co-substance use, there was a significant increase in tobacco use within the fentanyl cohort (96.6% vs. 0%, p < 0.001) during the pandemic compared to pre-pandemic.
Discussion
Effect of COVID-19 on maternal substance use
One of the aims of this study was to look at changes in maternal substance use, with a focus on fentanyl use, during the COVID-19 pandemic. We did not find any statistically significant changes in cannabis, amphetamine, cocaine, and alcohol use among our patient population. Our results differ slightly from those found in literature but are also difficult to compare because of varying target populations as well as differences in local laws regarding specific substances (such as cannabis use). Young-Wolff et al. found a 25% increase in prenatal cannabis use during the pandemic in California where cannabis retailers are legal and regulated, though there was no statistically significant increase in rates before and during the pandemic [13]. Other studies have looked at substance use in relation to depression/anxiety or COVID-19 related stress, while we simply looked at substance use over time and did not specifically correlate our results to mental health. One study of Canadian pregnant women did find an increase in cannabis and tobacco use that was related COVID-19 stress, and that the substance use was more frequent in participants with financial struggles, loss of employment, or stress about receiving poor prenatal care [9]. Smith et al. identified that elevated stress and depressive symptoms was associated with an increase in number of substances used during the COVID-19 pandemic [14].
While we did not note a significant increase in other substances, we did observe a significant increase of fentanyl use during pregnancy, which is in line with national data on synthetic opioid use and overdose. According to the Centers for Disease Control and Prevention (CDC), more than 93,000 people died from drug overdoses in the US in 2020, nearly a 30% increase from 2019. Opioids accounted for approximately 75% of all overdose deaths in 2020 [15], with synthetic opioids (primarily fentanyl) acting as the main culprit with a six-fold increase from 2015 to 2020 [16, 17]. Given the concomitant opioid pandemic, it is difficult to elucidate whether the increase we noted in fentanyl use was in relation to the COVID-19 pandemic or whether it would have followed its current trajectory regardless. However, it is still important to note these trends to screen pregnant women for substance use disorders and provide adequate care, including enrollment in OMT in cases of opioid use disorder.
Effect of COVID-19 on prenatal care and OMT
The COVID-19 pandemic brought on many changes and stressors, including housing instability, financial strains, self-isolation, anxiety over health and well-being, and access to maternal health care. Telehealth use for obstetric patients was rapidly implemented especially in early stages of the pandemic [18, 19], including for the treatment of opioid use disorder [20]. Studies show that pregnant women with OUD are less likely to engage in prenatal care [21] and are at higher risk for adverse pregnancy outcomes [22]. Although not statistically significant, we did note relatively lower rates of reported enrollment in OMT during the pandemic despite similar rates of general prenatal care. In fact, Lensch et al. noted 33% fewer clinics accepting pregnant women for OUD treatment during the pandemic [23]. We did not differentiate whether our decreased enrollment was due to inability to find a treatment facility that was accepting patients, disinterest in OMT, or if it was not offered. There is also some concern that the transition from in-person to virtual therapies may have impacted attendance. McKiever et al. saw nearly a three-fold decrease in group therapy attendance rates with the shift to telehealth, as well as a trend of up-titration of OMT doses due to cravings [24].
Importantly, while we did not see a significant decrease in OMT enrollment, there was a statistically significant increase in fentanyl users among not only the pandemic cohort but also among those who were enrolled in OMT. Researchers found that use of fentanyl increased by 108% in a study of opioid agonist treatment patients in Canada [25]. Treatment of OUD with opioid agonists combined with behavioral therapy has been shown to reduce the misuse of opioids, prevent withdrawal symptoms, decrease risk of fatal and nonfatal overdose, and is associated with overall improved maternal and infant outcomes [26–28]. With this trend of increasing fentanyl use, there is an increased likelihood of adverse maternal and infant outcomes. It also presents the question of whether there is a gap or deficiency in current opioid maintenance therapy, or whether the increased rates are due to individual intent or related to stress and anxiety. Further studies should be performed to observe the cause-and-effect of this increase in fentanyl use despite OMT.
Effect of maternal substance use on neonatal outcomes
Our study is the first to report infant outcomes related to substance use during the COVID-19 pandemic compared to pre-pandemic. We found there was a significantly higher incidence of preterm birth during the COVID-19 pandemic, which differs from that reported in literature. Given the numerous potential variables and retrospective nature of this study, it is difficult to determine whether the preterm birth rate was due to maternal stress, illness, or overall health; specific drug use; or other factors. However, when looking at literature, studies show a decrease in preterm birth rates during the pandemic [29, 30]. In a study looking at association of preterm birth rate during the 2020 stay-at-home order in our state, they reported significantly lower rates compared to previous years [31]. Other studies demonstrated a decrease in preterm birth that was primarily driven by decline in Caesarean sections of induced deliveries [32]. Meanwhile, we had a significant increase in preterm birth rate with a statistically insignificant increase in number of Caesarean sections. It is unclear why our data differs from that reported in literature. One of the contributing factors may be that our regional center serves a high-risk, low-income, and inner-city population, which was shown to have overall poorer health outcomes and higher economic challenges during the pandemic.
Interestingly, when looking at the fentanyl cohorts, we did not note a significant difference in incidence of NOWS or preterm birth rate. We did see a decrease in birth weight though it was not found to be statistically significant. One of our study limitations was the small pre-pandemic fentanyl cohort (n = 2), which limited our data analysis when evaluating association of fentanyl use in our patient population with perinatal outcomes such as prematurity and birth weight. However, both preterm birth and low birth weight are well documented in literature with being associated with opioid [33, 34] and tobacco [35, 36] use during pregnancy, and use of both were observed to be increased during the pandemic. It is also well-established that fentanyl is associated with onset of withdrawal symptoms [37, 38]. There are new synthetic opioids and fentanyl analogues being illicitly manufactured and distributed which may not be routinely detected without specialized toxicology testing [39–41]. In areas of high use, practitioners should consider screening for specific toxicology. With the emergence of these drugs and variability in potency, the uncertainty of the impact on fetal and neonatal outcomes is a concern and should be something that we continue to monitor.
Our study did not include overdose-related deaths or perinatal mortality from maternal substance use because we were looking at live-born infants. However, in the U.S., there were over 90,000 drug overdose deaths in 2020, the majority of which were opioid-related [42]. Even most benzodiazepine overdose deaths involved opioids, with 66.7% involving fentanyl [43]. Fentanyl was present in more than 85% of all overdose deaths during the COVID-19 pandemic [44]. It is crucial for the well-being of mother and infant that there be readily available access to standard prenatal care as well as specialized care such as OMT to prevent or minimize the occurrence of adverse outcomes.
Patrick et al. presented several suggestions regarding the public health response to opioid use in pregnancy by improving education and increasing availability of treatment services, rather than a punitive approach [45]. Given that opioid agonist therapy in conjunction with behavioral therapy have been shown to be associated with improved maternal and infant outcomes, it would be prudent to increase public health funding towards multidisciplinary programs where women with OUD can receive generalized and specialized obstetric care, oversight of their OMT, as well as psychosocial and mental health treatment. There are currently only 19 states that have drug treatment programs specifically targeted to those who are pregnant [46]. Additionally, treatment centers that do offer these types of specific services are typically located in urban areas, so additional efforts should be made to educate providers in rural areas on management of OUD in pregnancy. Studies have shown that pregnant women with OUD may avoid seeking care due to fear of being reported and having their child taken away [21]. Yet, literature also suggests that pregnancy can be a motivator for women with OUD to seek treatment [47]. We should capitalize on this motive rather than create more barriers which is what happens with the incarceration and criminal prosecution of mother. The de-criminalization of substance use in pregnancy could be a significant measure that would encourage women to engage in prenatal care and OMT.
Limitations and next steps
There are several limitations to this study. This was a single-center study, and we have a high-risk, low-income population. As previously mentioned, when analyzing the fentanyl cohorts, we were limited by our small pre-pandemic sample size. Additionally, risk of neonatal outcomes in relation to the increase in fentanyl use needs to be further investigated, especially with respect to incidence of NOWS. We plan to further stratify data to look at preterm versus term data in relation to maternal substance use. At this time, we do not have any neonatal neurodevelopmental or neuroimaging data, but this is an ongoing study, and we are planning to look at this data and report it in near future.
Conclusions
In our study, we reported the increasing incidence of fentanyl and tobacco use during pregnancy during the COVID-19 pandemic compared to two years prior to the pandemic. There was a significant increase in fentanyl use among mothers enrolled in OMT. We also identified a significantly lower birth weight and increase in preterm birth rate during the COVID-19 pandemic, though not specifically related to fentanyl use. Our study is the first to report infant outcomes related to substance use during the COVID-19 pandemic compared to pre-pandemic. As the opioid pandemic continues, it will be important to continue monitoring its impact on neonatal outcomes as well as long-term neurodevelopmental effects.
Supplementary information
Acknowledgements
We would like to extend our thanks and gratitude to the Social Workers, especially Ms. Linda DeBaer, at the Newborn Center at Regional Medical Center in Memphis, TN for their assistance in speaking with these mothers and survey-work.
Author contributions
JL contributed to design of the study, collected the data, performed preliminary analysis, and drafted and revised the manuscript. RD conceptualized and designed the study and reviewed and revised the manuscript. TH and FLS carried out the statistical analysis. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the University of Tennessee Health Science Center (UTHSC). No consent form was required.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41372-023-01613-8.
References
- 1.Townsend R, Chmielewska B, Barratt I, Kalafat E, van der Meulen J, Gurol-Urganci I, et al. Global changes in maternity care provision during the COVID-19 pandemic: A systematic review and meta-analysis. E Clin Med. 2021;37:1–19. doi: 10.1016/j.eclinm.2021.100947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Semaan AT, Audet C, Huysmans E, Afolabi BB, Assarag B, Banke-Thomas A, et al. Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Glob Health. 2020;5:e002967. doi: 10.1136/bmjgh-2020-002967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths–United States, 2013–2019. Morb Mortal Wkly Rep. 2021;70:202–7. doi: 10.15585/mmwr.mm7006a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia GG, Stringfellow EJ, DiGennaro C, Poellinger N, Wood J, Wakeman S, et al. Opioid overdose decedent characteristics during COVID-19. Ann Med. 2022;54:1081–8. doi: 10.1080/07853890.2022.2067350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmad M, Vismara L. The psychological impact of COVID-19 pandemic on women’s mental health during pregnancy: A rapid evidence review. Int J Environ Res Public Health. 2021;18:1–15. doi: 10.3390/ijerph18137112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Basu A, Kim HH, Basaldua R, Choi KW, Charon L, Kelsall N, et al. A cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PLoS ONE. 2021;16:e0249780. doi: 10.1371/journal.pone.0249780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Czeisler ME, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic – United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049–57. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2021;377:5–13. doi: 10.1016/j.jad.2020.07.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kar P, Tomfohr-Madsen L, Giesbrecht G, Bagshawe M, Lebel C. Alcohol and substance use in pregnancy during the COVID-19 pandemic. Drug Alcohol Depend. 2021;225:1–8. doi: 10.1016/j.drugalcdep.2021.108760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grossman MR, Berkwitt AK, Osborn RR, Xu Y, Esserman DA, Shapiro ED, et al. An initiative to improve the quality of care of infants with neonatal abstinence syndrome. Pediatrics. 2017;139:e20163360. doi: 10.1542/peds.2016-3360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howard MB, Schiff DM, Penwill N, Si W, Rai A, et al. Impact of parental presence at infants’ bedside on neonatal abstinence syndrome. Hosp Pediatr. 2017;7:63–69. doi: 10.1542/hpeds.2016-0147. [DOI] [PubMed] [Google Scholar]
- 12.Pourcyrous M, Elabiad MT, Rana D, Gaston KP, DeBaer L, Dhanireddy R. Racial differences in opioid withdrawal syndrome among neonates with intrauterine opioid exposure. Pediatr Res. 2021;90:459–63. doi: 10.1038/s41390-020-01279-4. [DOI] [PubMed] [Google Scholar]
- 13.Young-Wolff KC, Ray GT, Alexeeff SE, Adams SR, Does MB, Ansley D, et al. Rates of prenatal cannabis use among pregnant women before and during the COVID-19 pandemic. JAMA. 2021;326:1745–7. doi: 10.1001/jama.2021.16328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith CL, Waters SF, Spellacy D, Burduli E, Brooks O, Carty CL, et al. Substance use and mental health in pregnant women during the COVID-19 pandemic. J Reprod Inf Physiol. 2021;40:465–78. doi: 10.1080/02646838.2021.1916815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The Commonwealth Fund. The Drug Overdose Toll in 2020 and Near Term Actions for Addressing it. Published on August 16, 2021. Accessed July 20, 2022. https://www.commonwealthfund.org/blog/2021/drug-overdose-toll-2020-and-near-term-actions-addressing-it.
- 16.National Institute on Drug Abuse. Overdose Death Rates. Published on January 29, 2021. Accessed July 20, 2022. https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates.
- 17.The Commonwealth Fund. The Spike in Drug Overdose Deaths During the COVID-19 Pandemic and Policy Options to Move Forward. Published on March 25, 2021. Accessed July 20, 2022. https://www.commonwealthfund.org/blog/2021/spike-drug-overdose-deaths-during-covid-19-pandemic-and-policy-options-move-forward.
- 18.Aziz A, Zork N, Aubey JJ, Baptiste CD, D’Alton ME, Emeruwa UN, et al. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am J Perinatol. 2020;37:800–8. doi: 10.1055/s-0040-1712121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gao C, Osmundson S, Malin BA, Chen Y. Telehealth use in the COVID-19 pandemic: A retrospective study of prenatal care. Stud Health Technol Inf. 2022;290:503–7. doi: 10.3233/SHTI220127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Uscher-Pines L, Huskamp HA, Mehrota A. Treating patients with opioid use disorder in their homes: an emerging treatment model. JAMA. 2020;324:39–40. doi: 10.1001/jama.2020.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kremer ME, Arora KS. Clinical, ethical, and legal considerations in pregnant women with opioid abuse. Obstet Gynecol. 2015;126:474–8. doi: 10.1097/AOG.0000000000000991. [DOI] [PubMed] [Google Scholar]
- 22.Whiteman VE, Salemi JL, Mogos MF, Cain MA, Aliyu MH, Salihu HM. Maternal opioid drug use during pregnancy and its impact on perinatal morbidity, mortality, and the costs of medical care in the United States. J Pregnancy. 2014;ID 906723:1–8. doi: 10.1155/2014/906723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lensch AC, Hairston E, Carter G, Jones HE. Pregnant patients using opioids: Treatment access barriers in the age of COVID-19. J Addict Med. 2022;16:e44–e47. doi: 10.1097/ADM.0000000000000826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKiever ME, Cleary EM, Schmauder T, Talley A, Hinely KA, Costantine MM, et al. Unintended consequences of the transition to telehealth for pregnancies complicated by opioid use disorder during the coronavirus 2019 pandemic. Am J Obstet Gynecol. 2020;223:770–2. doi: 10.1016/j.ajog.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morin KA, Acharya S, Eibl JK, Marsh DC. Evidence of increased fentanyl use during the COVID-19 pandemic among opioid agonist treatment patients in Ontario, Canada. Int J Drug Policy. 2021;90:1–3. doi: 10.1016/j.drugpo.2020.103088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Committee on Obstetric Practice. ACOG committee opinion no. 711: Opioid use and opioid use disorder in pregnancy. Opioid Gynecol. 2017;130:e81–e94. doi: 10.1097/AOG.0000000000002235. [DOI] [PubMed] [Google Scholar]
- 27.Jones HE, Grady KE, Tuten M. Reinforcement-based treatment improves the maternal treatment and neonatal outcomes of pregnant patients enrolled in comprehensive care treatment. Am J Addict. 2011;20:196–204. doi: 10.1111/j.1521-0391.2011.00119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tran EL, Kim SY, England LJ, Green C, Dang EP, Broussard CS, et al. The MATernaL and Infant NetworK to understand outcomes associated with treatment of opioid use disorder during pregnancy (MAT-LINK): surveillance opportunity. J Women’s Health. 2020;29:1491–9. doi: 10.1089/jwh.2020.8848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen J, Ferre C, Ouyang L, Mohamoud Y, Barfield W, Cox S, et al. Changes and geographic variation in rates of preterm birth and stillbirth during the prepandemic period and COVID-19 pandemic, according to health insurance claims in the United States. Am J Obstet Gynecol MFM. 2022;4:100508. doi: 10.1016/j.ajogmf.2021.100508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Noddin K, Bradley D, Wolfberg A. Delivery outcomes during the COVID-19 pandemic as reported in a pregnancy mobile app: retrospective cohort study. JMIR Pediatr Parent. 2021;4:e27769. doi: 10.2196/27769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harvey EM, McNeer E, McDonald MF, Shapiro-Mendoza CK, Dupont WD, Barfield W, et al. Association of preterm birth rate with COVID-19 statewide stay-at-home orders in Tennessee. JAMA Pediatr. 2021;175:635–7. doi: 10.1001/jamapediatrics.2020.6512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dench D, Joyce T, Minkoff H. United States preterm birth rate and COVID-19. Pediatrics. 2022;149:e2021055495. doi: 10.1542/peds.2021-055495. [DOI] [PubMed] [Google Scholar]
- 33.Corsi DJ, Hsu H, Fell DB, Wen SW, Walker M. Association of maternal opioid use in pregnancy with adverse perinatal outcomes in Ontario, Canada, from 2012 to 2018. JAMA Netw Open. 2020;3:e208256. doi: 10.1001/jamanetworkopen.2020.8256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Interrante JD, Scroggs SLP, Hogue CJ, Friedman JM, Reefhuis J, Jann MW, et al. Prescription opioid use during pregnancy and risk for preterm birth or term low birth weight. J Opioid Manag. 2021;17:215–25. doi: 10.5055/jom.2021.0632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ion R, Bernal AL. Smoking and preterm birth. Reprod Sci. 2015;22:918–26. doi: 10.1177/1933719114556486. [DOI] [PubMed] [Google Scholar]
- 36.Stock SJ, Bauld L. Maternal smoking and preterm birth: an unresolved health challenge. PLoS Med. 2020;17:e1003386. doi: 10.1371/journal.pmed.1003386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alipio JB, Brockett AT, Fox ME, Tennyson SS, deBettencourt CA, Francis NA, et al. enduring consequences of perinatal fentanyl exposure in mice. Addict Biol. 2021;26:e12895. doi: 10.1111/adb.12895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pacifici GM. Clinical pharmacology of fentanyl in preterm infants: a review. Pediatr Neonatol. 2015;56:143–8. doi: 10.1016/j.pedneo.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Fentanyl Encounters Data. Published on August 9, 2021. Accessed November 2, 2022. https://www.cdc.gov/drugoverdose/deaths/fentanyl-encounters/index.html.
- 40.United Nations Office on Drugs and Crime. Understanding the global opioid crisis. Global SMART Update Volume 21, March 2019.
- 41.Prekupec MP, Mansky PA, Baumann MH. Misuse of novel synthetic opioids: a deadly new trend. J Addict Med. 2017;11:256–65. doi: 10.1097/ADM.0000000000000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Auty SG, Griffith KN. Medicaid expansion and drug overdose mortality during the COVID-19 pandemic in the United States. Drug Alcohol Depend. 2022;232:1–4. doi: 10.1016/j.drugalcdep.2022.109340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu S, O’Donnell J, Gladden RM, McGlone L, Chowdhury F. Trends in nonfatal and fatal overdoses involving benzodiazepines—38 states and the District of Columbia, 2019-2020. MMWR Morb Mortal Wkly Rep. 2021;70:1136–41. doi: 10.15585/mmwr.mm7034a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DiGennaro C, Garcia GG, Stringfellow EJ, Wakeman S, Jalali MS. Changes in characteristics of drug overdose death trends during the COVID-19 pandemic. Int J Drug Policy. 2021;98:1–4. doi: 10.1016/j.drugpo.2021.103392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Patrick SW, Schiff DM, AAP COMMITTEE ON SUBSTANCE USE AND PREVENTION. A public health response to opioid use in pregnancy. Pediatrics. 2017;139:e20164070. doi: 10.1542/peds.2016-4070. [DOI] [PubMed] [Google Scholar]
- 46.Guttmacher Institute. Substance use during pregnancy. State Policies in Brief. January 1, 2023. Available at: https://www.guttmacher.org/state-policy/explore/substance-use-during-pregnancy. Accessed January 3, 2023.
- 47.Davis KJ, Yonkers KA. Making lemonade out of lemons: a case report and literature review of external pressure as an intervention with pregnant and parenting substance-using women. J Clin Psych. 2012;73:51–56. doi: 10.4088/JCP.11cr07363. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.