Background:
Research on reflexology therapy for multiple sclerosis (MS) is limited, and the evaluation is mixed. Our aim is to confirm the efficacy of reflexology therapy for MS.
Methods:
The preferred reporting items for systematic reviews and meta-analyses guidelines were followed. The search strategy was conducted in PubMed, Embase, the Cochrane Library, and the Science Citation Index. The quality of the included trials was assessed by the Cochrane Handbook. The main results were summarized and analyzed in RevMan 5.4.
Results:
A total of 11 studies were included in the final analysis. There were significant differences [mean difference (MD) –0.90, 95% confidence interval (CI) –1.37 to –0.43, heterogeneity I2 = 0%] between the Precision Reflexology and Sham Reflexology groups in visual analogue scale pain. There was a significant difference (MD –1.00, 95% CI –1.42 to –0.58, heterogeneity I2 = 93%) between the Precision Reflexology and Sham Reflexology groups on the fatigue severity scale. There was no difference between the Precision Reflexology and Sham Reflexology groups in physical function (MD 6.88, 95% CI –3.36 to 17.13, heterogeneity I2 = 31%), role disorder due to physical problems (MD 10.20, 95% CI –4.91 to 25.30, heterogeneity I2 = 0%), physical pain (MD 7.68, 95% CI –0.09 to 15.45, heterogeneity I2 = 0%), role disorder due to emotional problems (MD 3.41, 95% CI –11.55 to 18.37, heterogeneity I2 = 0%), energy (MD 3.27, 95% CI –4.32 to 10.87, heterogeneity I2 = 0%), emotional well-being (MD 1.79, 95% CI –4.76 to 8.34, heterogeneity I2 = 0%), social function (MD 5.72, 95% CI –3.48 to 14.91, heterogeneity I2 = 0%), or general health (MD 2.63, 95% CI –4.36 to 9.62, heterogeneity I2 = 0%).
Conclusions:
Reflexology therapy can be used as an effective intervention for the pain and fatigue of MS patients while improving the quality of life.
Keywords: meta-analysis, multiple sclerosis, reflexology, systematic review
1. Introduction
Multiple sclerosis (MS) is a common autoimmune inflammatory demyelination disease of the central nervous system and is the most common disease of the nervous system leading to motor disorders in young and middle-aged people in economically developed areas.[1] Its spastic symptoms can affect many functional areas, leading to gait disorders, falls, fatigue, sleep disturbances, pain, bladder dysfunction, accelerated wheelchair use, increased disability and dependency, social isolation and depression.[2] As the disease progresses, the physical disability, psychosocial adjustment, and social reintegration of patients gradually deteriorate, placing a large burden on patients, family members, and caregivers, as well as the social economy.[3] Dyskinesia often occurs in people with MS and negatively affects quality of life.[4,5]
MS patients may experience physical symptoms, cognitive impairment and psychological symptoms, such as weakness, fatigue, constipation, poor sleep, anxiety, depression, low self-esteem, pain, paresthesia and other physical or psychological effects.[6] All of these symptoms may interfere with the patient’s normal function and affect their ability to perform daily living and quality of life. Therefore, MS patients are more inclined to use complementary and alternative medicine (CAM). CAM is very popular in diseases related to central nervous system damage to control symptoms.[7] Among them, reflexology is a method of massage therapy[8] and one of the most common types of CAM. It acts on specific areas of the body to apply appropriate pressure, especially on the feet, to promote relaxation and recovery. One idea is that the technique is used to stimulate specific points in the body to improve circulation, energy, relaxation and homeostasis.[9] Another view is that reflexology works by directly pressing on specific nerve endings in the foot to stimulate relevant parts of the body to relieve certain symptoms.[10] It can be used to improve the patient’s signs and symptoms, their ability to live, and their quality of life. Reflexology is effective in reducing symptoms such as pain, fatigue, anxiety, high blood pressure, insomnia and depression.[11] At present, some researchers have gradually carried out research on the mental health and physical symptoms of MS patients, but the results of each study are controversial, and the sample sizes of the studies are small. Therefore, in this study, a meta-analysis was conducted to comprehensively evaluate the literature on the improvement of physical symptoms and mental health of MS patients with reflexology, aiming to provide a scientific basis for the clinical development of appropriate effective treatment methods to reduce physical symptoms and improve quality of life.
2. Data and methods
The systematic review and meta-analysis was performed according to the preferred reporting items for systematic reviews and meta-analysis statement. The protocol number that we registered on the PROSPERO database is CRD42022332196.
2.1. Search strategy
All references are from PubMed, Embase, the Cochrane Library and the Science Citation Index (as of June 2022). “Reflexology” AND “multiple sclerosis” were key terms used for finding relevant and qualified articles and to avoid missing appropriate articles. References of selected articles were carefully screened to ensure the reliability and validity of the meta-analysis. At the same time, we collected data only from the full published papers, not any conference abstracts.
The search terms used were reflexology and multiple sclerosis in all electronic databases, and it well balanced the search range and accuracy based on our preview testing. PubMed, Embase, the Cochrane Library and the Science Citation Index were searched. We also manually looked through the relevant trials from the references of the studies that had been included. No published conference articles were identified to determine whether they met the inclusion criteria. The language of the study was limited to English.
2.2. Eligibility criteria
At the earliest stages of our systematic review, rigid inclusion criteria were used to select relevant studies.
2.2.1. The inclusion criteria were as follows.
Study design: The study must be a randomized controlled study, not an animal study, in any language.
Subjects: All subjects were patients with clinically confirmed MS.
Intervention measures: The treatment group was given reflexology treatment, and the intervention time was not limited, while the control group was given nonreflexology treatment.
2.2.2. Articles excluded from this meta-analysis are as follows.
literature that was reported repeatedly.
non-RCT studies.
control studies of non reflexology treatment.
abstracts, lectures, cases and reviews; and.
studies in which the subject was not human.
We assessed the methodological quality using the Cochrane Collaboration’s tool for assessing risk in Review Manager 5.4.[12] To evaluate selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases, 7 items were provided by the tool. They included random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. To assess the bias, each item was answered with one of 3 replies: “low risk,” “unclear risk,” and “high risk.”[12]
2.3. Data synthesis and analysis
We assessed heterogeneity based on formal statistical testing with I2. For binary outcomes, we used Mantel–Haenszel (M-H) estimates with a fixed effect model to calculate mean differences (MDs) and their 95% confidence intervals (CIs), in which case a random effects model was performed. For continuous outcomes, inverse variance estimates were conducted with a fixed effects model to calculate standard MDs and their 95% CIs. Similarly, when significant clinical heterogeneity among studies was apparent, a random effects model was used. I2 values of more than 40% indicated that statistical heterogeneity existed. Fewer than 10 studies in the meta-analysis were deemed to have no effect method that could be used to explore publication bias.[13] When more than 10 studies were pooled for analysis, Begg’s or Egger’s funnel plot method was considered. Subgroup analysis was applied to explore the heterogeneity or between-subgroup different effects, and sensitivity analyses were also performed according to methodological quality parameters.
3. Results
3.1. Characteristics of included studies
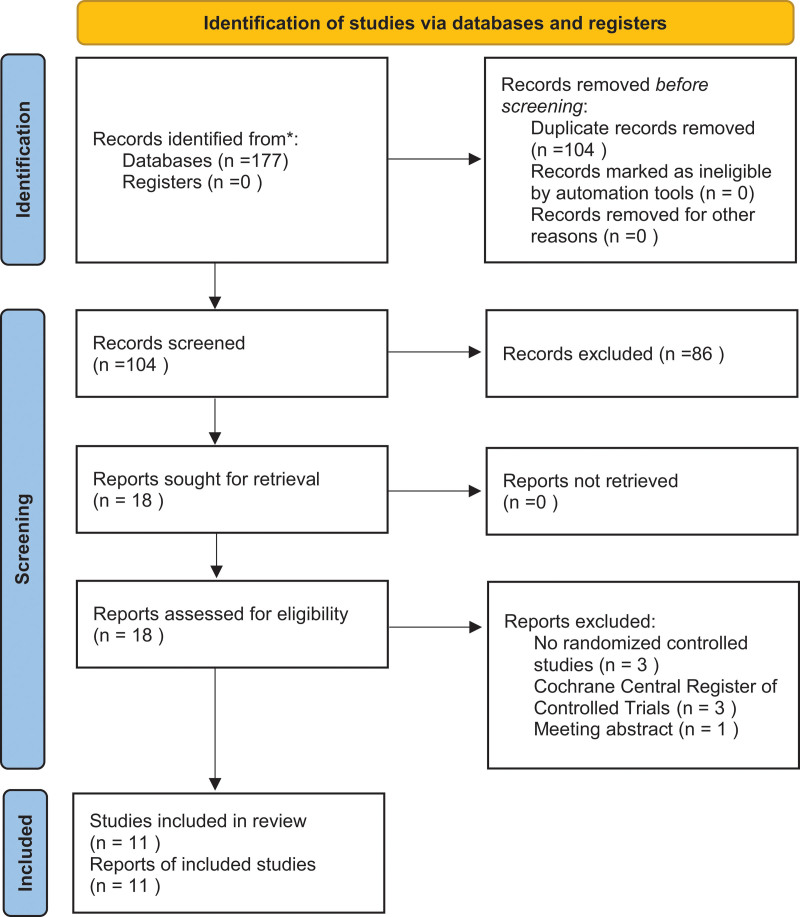
A total of 177 articles were identified through the literature search. Of the 177 published articles, 104 were considered potentially relevant. The 104 articles were independently reviewed, and 18 were included. Three of them were not randomized controlled trials, 1 was a conference abstract, and 3 were Cochrane Central Register of Controlled Trials. Therefore, a total of 11 studies were included in the final analysis (Fig. 1). In conclusion, there were comparable baseline characteristics (Table 1) between the Precision Reflexology and Sham Reflexology groups in our meta-analysis.
Figure 1.
PRISMA flow diagram. PRISMA = the preferred reporting items for systematic reviews and meta-analyses.
Table 1.
Characteristics of the studies included in this review.
| Study ID | Region (country) | Sample size (N/C) | Age, yr (N/C) | Intervention | Control | Main measurement outcome | Follow up, day |
|---|---|---|---|---|---|---|---|
| Hatice Dilek Doğan 2021 | USA | 30/30 | 36.43/39.46 | reflexology (3 sessions/week) | No reflexology made | visual analogue scale (VAS); fatigue severity scale (FSS), multiple sclerosis quality of life-54 (MSQOL-54) scale | 12 wk |
| Mahbobeh Sajadi 2020 | Iran | 33/30 | 34.52/32.12 | reflexology (twince/wk) | Foot surface massage without pressure was applied to simulate the interventions |
constipation assessment scale (CAS); stool frequency; short form (SF)36 quality of life (QOL) questionnaire | 6 wk |
| Mahbobeh Sajadi 2020 | Iran | 33/30 | - | reflexology (twince/wk) | placebo intervention | fatigue impact scale (FIS); pittsburgh sleep qual-ity index (PSQI); state-trait anxiety inventory (STAI) | 4 wk |
| Nusrat Ebrahimi 2020 | Iran | 30/30 | 32.66/32.30 | foot reflexology (3 times/wk) | foot sole massage | fatigue severity scale (FSS); stress symptom index (SSI); serum ortisol levels | 4 wk |
| CM Hughes 2009 | Northern Ireland | 35/36 | 50/53 | precision reflexology (weekly) | Sham reflexology | visual analogue scale (VAS). | 10 wk |
| Fatemeh Nazari 2015 | Iran | 25/25/25 | reflexology/relaxation/ control(34.40/ 33.90/ 34.40) | foot reflexology (twince/wk); relaxation (twince/wk) | received care and routine medical treatment | fatigue severity scale (FSS) | 4 wk |
| Mozhgan Soheili 2022 | Iran | 25/25/25 | reflexology/relaxation/ control (34.40/ 33.90/ 34.04) | reflexology(twince/wk); relaxation (twince/wk) | routine treatment | anxiety score, stress score, depression score [depression anxiety and stress scale-21 (DASS.21)] | 4 wk |
| Peter A. Mackereth 2009 | UK | 25/25 | 52.52/48.12 | reflexology (weekly) | progressive muscle relaxationPMR (weekly) | the short form 36 (SF36); general health questionnaire 28 (GHQ28); state anxiety inventory (SAI); | 6 wk |
| L Miller 2013 | UK | 10/10 | 53.6/58.1 | reflexology (once/wk) | Sham reflexology | multiple sclerosis impact scale (MSIS29); hospital anxiety and depression scale (HAD); visual analogue scale (VAS) | 8 wk |
| Fatemeh Nazari 2015 | Iran | 25/25/25 | reflexology/relaxation/ control(34.40/ 33.90/ 34.40) | reflexology (twince/wk); relaxation (twince/wk) | routine treatment | numeric rating scale (NRS) pain score | 4 wk |
| I Siev-Ner 2003 | Israel | 27/26 | 46.29/49.29 | reflexology (once/wk) | Sham treatment of nonspecific massage | paresthesias [visual analogue scale (VAS)]; urinary symptoms [American urological association (AUA) symptom score]; spastisity, muscle tone-by Ashworth score; muscle strength-by British medical research council (BMRC) scale |
11 weeks |
CAS = problem assessment scale, FIS = fatigue impact scale, FSS = fatigue severity scale, HAD = hospital anxiety and depression scale, MSIS29 = multiple sclerosis impact scale, MSQOL-54 = multiple sclerosis quality of life -54, NRS = numeric rating scale, SAI = state anxiety inventory, SSI = stress symptom index, VAS = visual analogue scale, QOL = quality of life.
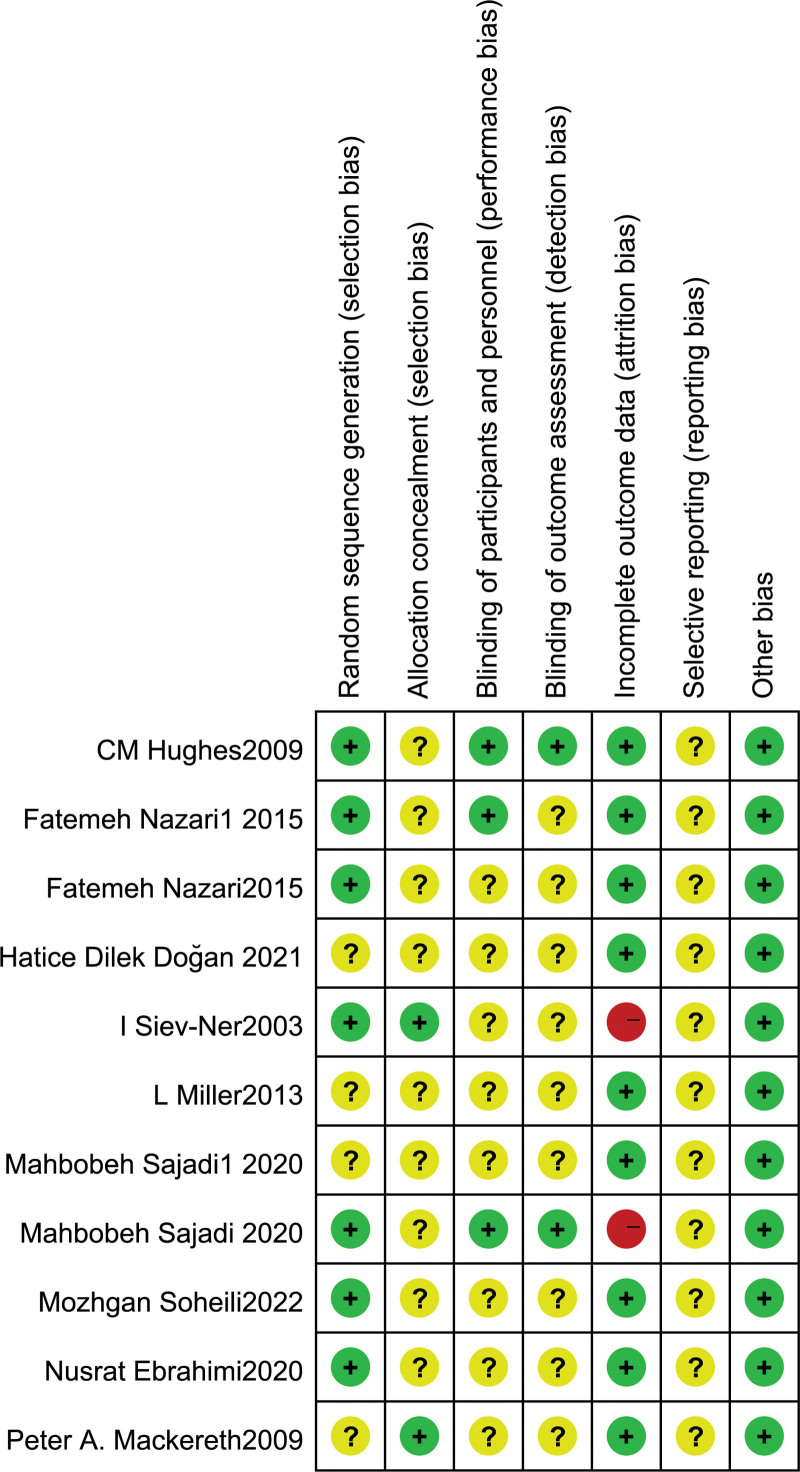
3.2. Assessing the risk of bias
There were 3 studies that could be fully assessed, and 2 were judged to be low risk of bias in all items. “Blinding of participants and personnel” was judged to be of high risk in 1 study. Two studies blinded the outcome assessors; the remaining were unclear due to missing information. Figure 2 shows all assessment results for the risk of bias.
Figure 2.
Risk of bias of included studies.
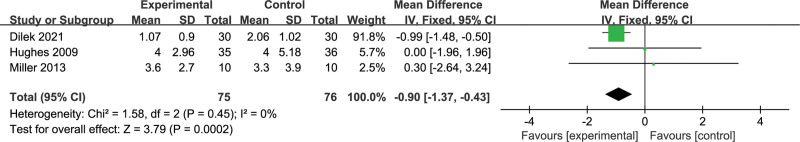
3.3. Visual analogue scale pain
Three studies reported visual analogue scale pain. The meta-analysis results for all included studies showed that there were significant differences (MD –0.90, 95% CI –1.37 to –0.43, heterogeneity I2 = 0%) between the Precision Reflexology and Sham Reflexology groups (Fig. 3). I2 values of 0% denoted that heterogeneity was negligible among studies.
Figure 3.
Forest plot for VAS pain. CI = confidence interval, RR = relative risk, VAS = visual analogue scale.
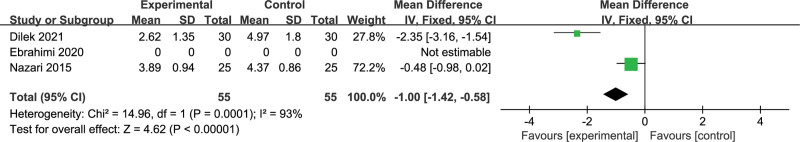
3.4. Fatigue severity scale
Three studies reported the incidence of the fatigue severity scale. The pooled analysis results suggested that there was a significant difference (MD –1.00, 95% CI –1.42 to –0.58, heterogeneity I2 = 93%) between the Precision Reflexology and Sham Reflexology groups. I2 values of 93% denoted large heterogeneity among studies (Fig. 4).
Figure 4.
Forest plot for FSS. Short form (SF) 36 quality of life (QOL). CI = confidence interval, FSS = fatigue severity scale, RR = relative risk.
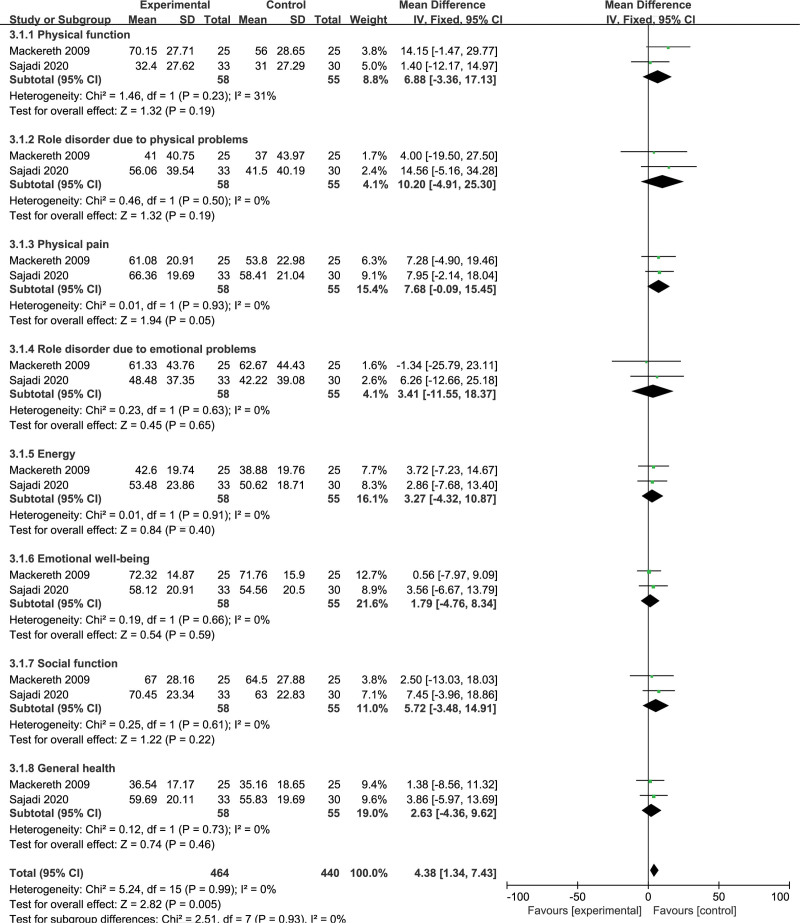
3.5. Short form 36
Two studies reported the incidence of the short form 36 quality of life. The pooled analysis results suggested that there was no difference between the Precision Reflexology and Sham Reflexology groups in physical function (MD 6.88, 95% CI –3.36 to 17.13, heterogeneity I2 = 31%), role disorder due to physical problems (MD 10.20, 95% CI –4.91 to 25.30, heterogeneity I2 = 0%), physical pain (MD 7.68, 95% CI –0.09 to 15.45, heterogeneity I2 = 0%), role disorder due to emotional problems (MD 3.41, 95% CI –11.55 to 18.37, heterogeneity I2 = 0%), energy (MD 3.27, 95% CI –4.32 to 10.87, heterogeneity I2 = 0%), emotional well-being (MD 1.79, 95% CI –4.76 to 8.34, heterogeneity I2 = 0%), social function (MD 5.72, 95% CI –3.48 to 14.91, heterogeneity I2 = 0%), and general health (MD 2.63, 95% CI –4.36 to 9.62, heterogeneity I2 = 0%). I2 values of 0% denoted that heterogeneity was negligible among studies (Fig. 5).
Figure 5.
Forest plot for short form (SF) 36 quality of life (QOL). CI = confidence interval, RR = relative risk.
3.6. Other parameters
Other parameter summaries are shown in Table 2. Quality of life was assessed monthly using the multiple sclerosis quality of life –54 scale. Dilek Doğan H[14] found that reflexology therapy was observed in the multiple sclerosis quality of life-54 scale, playing a positive role. Sajadi M[15] believes that reflexology therapy has a positive effect on MS patients on the problem assessment scale and stool frequency.
Table 2.
Other parameters.
| Study ID | Outcomes | P Value |
|---|---|---|
| Hatice Dilek Doğan 2021 | Multiple sclerosis quality of life-54 (MSQOL-54) scale | <.001 |
| Mahbobeh Sajadi 2020 | Constipation assessment scale (CAS) | .0001 |
| Stool frequency | .0001 | |
| Mahbobeh Sajadi 2020 | Fatigue impact scale (FIS) | .134 |
| Pittsburgh sleep quality index (PSQI) | .001 | |
| State-trait anxiety inventory (STAI) | .034 | |
| Nusrat Ebrahimi 2020 | Stress symptom index (SSI) | <.00001 |
| Serum ortisol levels | <.00001 | |
| Mozhgan Soheili 2022 | Anxiety score | .04 |
| Stress score | .004 | |
| Depression score [depression anxiety and stress scale-21 (DASS.21)] | .01 | |
| Peter A. Mackereth 2009 | General health questionnaire 28 (GHQ28)- severe depression | .2485 |
| GHQ28 – somatic symptoms | .9738 | |
| GHQ28 – anxiety and insomnia | .7923 | |
| GHQ28 – social dysfunction | .6809 | |
| State anxiety inventory (SAI) – state anxiety | .4378 | |
| SAI – Cortisol | .8699 | |
| SAI – systolic pressure | .9935 | |
| SAI – diastolic pressure | .6847 | |
| SAI – heart rate | .6985 | |
| L Miller 2013 | Multiple sclerosis impact scale (MSIS29) | .538 |
| Hospital anxiety and depression scale (HAD) | – | |
| HAD anxiety | .679 | |
| HAD depression | .8113 | |
| Fatemeh Nazari 2015 | Numeric rating scale (NRS) pain score | <.001 |
| I Siev-Ner 2003 | Urinary symptoms [American urological association (AUA) symptom score] | .03 |
| Spastisity, muscle tone-by Ashworth score | .03 | |
| Muscle strength-by British medical research council (BMRC) scale | .06 |
CAS = problem assessment scale, FIS = fatigue impact scale, HAD = hospital anxiety and depression scale, MSIS29 = multiple sclerosis impact scale, MSQOL-54 = multiple sclerosis quality of life-54, NRS = numeric rating scale, SAI = state anxiety inventory, SSI = stress symptom index.
Ebrahimi N[16] believes that reflexology therapy has positive effects on the stress symptom index, and serum cortisol levels showed significant improvement. Soheili M[17] found a significant decrease in the treatment group in the anxiety score, stress score, and depression score (depression anxiety and stress scale-21 (DASS.21)). Mackereth PA[18] found changes in both groups after treatment in the state anxiety inventory (SAI) – State anxiety, SAI – Cortisol, SAI – Systolic pressure, SAI – Diastolic pressure, and SAI – Heart rate. Miller L[19] also found that the multiple sclerosis impact scale, hospital anxiety and depression scale -anxiety, and hospital anxiety and depression scale-depression scores decreased significantly, but there was no significant difference between the 2 groups. Nazari F[19] observed that MS patients had significantly improved numeric rating scale pain scores. Siev-Ner I[20] also observed that MS patients showed significant improvement in urinary symptoms and severity after intervention but no significant improvement in muscle strength. Sajadi M[21] also found significant improvements in physical fatigue, sleep quality, and anxiety in the treatment group after the intervention, but the fatigue impact scale showed a decrease in fatigue levels in MS patients, but these changes were not significant.
4. Discussion
Current treatments for MS are based on immunosuppressants. However, the main problem of immunosuppressive therapy is the extensive suppression of the body’s immune function. Disease-modifying treatment, the standard treatment for MS in remission, may reduce clinical seizures and activity in patients with MS to varying degrees, but most disease-modifying treatment drugs do not affect the course of disease in advanced patients. Therefore, symptomatic treatment has become an important method for the comprehensive treatment of MS.[22] Massage therapy has been shown in many different groups and has a beneficial effect on many diseases, including prenatal depression, premature and full-term infants, autism, skin disease, arthritis and fibromyalgia pain syndrome, hypertension, asthma, autoimmune diseases such as multiple sclerosis and HIV, immune diseases such as breast cancer, and aging problems such as Parkinson’s and Alzheimer’s disease.[23]
However, studies on massage therapy for MS have had inconsistent results. Finch P et al concluded that therapeutic massage research had produced positive changes[24,25]; however, Schroeder B et al found no positive changes after using Swedish massage therapy.[26] Therefore, this study systematically evaluated the effect of reflexology therapy in the treatment of multiple sclerosis.
Our systematic review found that there are positive results in the treatment of multiple sclerosis with reflexology. Reflexology therapy for patients with multiple sclerosis can improve pain, fatigue, and quality of life. It can be used as an intervention to effectively treat the pain and fatigue of MS patients and improve the quality of life of MS patients. There are also several high-quality randomized controlled trials that have investigated the effectiveness of reflexology therapy in improving symptoms in patients with MS. This is also consistent with our conclusions.
Hatice Dilek Doğan et al[14,19,27,28] concluded that the pain score and fatigue score of patients with multiple sclerosis decreased significantly after reflexology therapy. In the evaluation of quality of life, the comprehensive scores of physical health and mental health were higher than those of the control group, and the degree of anxiety, stress and depression were significantly reduced.[17] They also showed improvement in constipation.[15] As Nusrat Ebrahimi[29] reported, reflexology therapy was also observed to affect cortisol levels, an important stimulus for reducing anxiety, stress and depression in patients with multiple sclerosis. In addition, it is effective in relieving motor, sensory and urinary symptoms in MS patients.[20] However, L Miller[30] found that reflexology therapy was effective in patients with more severe MS disabilities.
Although a total of 11 trials were included in this study, all of which were randomized controlled studies with a large sample size, there was certain heterogeneity in each study sample. Because the selected reflexology methods and follow-up times have not been unified, there may be different degrees of bias and confounding factors. We also found that the 2 articles with large heterogeneity were from different countries, and the different treatment times and frequencies in the intervention groups may also be one of the sources of heterogeneity. In addition, we also found that the selected population came from different countries. Pain, anxiety and depression are also subjective results and depend on the subjects’ self-report, so there may be potential bias in the observational results. We found that these 11 studies were all evaluated by clinicians or nurses and should be uniformly evaluated by physicians. Moreover, most studies have not reported its long-term efficacy, which requires a large number of high-quality trials combined with long-term clinical practice for observation.
The findings of this review were compared with a placebo control group for patients with MS treated with reflexology therapy. As with any systematic review, there may be selection bias, but our team used a comprehensive search strategy, including database and manual searches. However, a small portion of the data could not be included. However, we believe that most representative studies are included in the final analysis of this systematic review. Heterogeneity between studies, especially with regard to research interventions and impact scale evaluation, is a challenge. In addition, different follow-up observation times were used. In addition, the evaluators of the quality scale were physicians or nurses. Nonetheless, the study populations in all trials appear to be representative of patients seen in clinical practice. We encourage selecting clinicians or nurses in the same category as much as possible to avoid the inclusion/confusion/misunderstanding of future data.
5. Conclusions
Reflexology is a noninvasive, simple, accessible, low-cost, and uncomplicated nursing intervention that can be helpful along with other treatments to relieve problems in MS patients. The results of this study showed that reflexology therapy for patients with multiple sclerosis can improve pain, fatigue, and quality of life. It can be used as an effective intervention to effectively treat the pain and fatigue of MS patients and improve the quality of life of MS patients.
Acknowledgements
Thank all participants for their kindly help during the formation and finalization processes of the manuscript.
Author contributions
Conceptualization: Yunxiang Guan, Baoliang Wang.
Data curation: Xiaohong Ma, Zhaoyu Yuan.
Funding acquisition: Baoliang Wang.
Investigation: Baicheng Qian.
Methodology: Baicheng Qian.
Project administration: Baoliang Wang.
Resources: Yunxiang Guan.
Software: Xiaohong Ma.
Supervision: Zhaoyu Yuan.
Validation: Zhaoyu Yuan.
Visualization: Xiaohong Ma.
Writing – original draft: Xiaohong Ma.
Writing – review & editing: Xiaohong Ma.
Abbreviations:
- CAM
- alternative medicine
- CI
- confidence interval
- MD
- mean difference
- MS
- multiple sclerosis
- SAI
- state anxiety inventory
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
The authors have no ethical statement, funding and conflicts of interest to disclose.
How to cite this article: Ma X, Yuan Z, Qian B, Guan Y, Wang B. Systematic review and meta-analysis of reflexology for people with multiple sclerosis: Systematic Review and Meta-Analysis. Medicine 2023;102:5(e32661).
Contributor Information
Xiaohong Ma, Email: ma_xiaohong101687@163.com.
Zhaoyu Yuan, Email: 2817160652@qq.com.
Baicheng Qian, Email: qianbaicheng163@163.com.
Yunxiang Guan, Email: gyx77325@126.com.
References
- [1].Correale J, Gaitán MI, Ysrraelit MC, et al. Progressive multiple sclerosis: from pathogenic mechanisms to treatment. Brain. 2017;140:527–46. [DOI] [PubMed] [Google Scholar]
- [2].Milinis K, Tennant A, Young CA. Spasticity in multiple sclerosis: associations with impairments and overall quality of life. Multiple Sclerosis Rel Disord. 2016;5:34–9. [DOI] [PubMed] [Google Scholar]
- [3].Amatya B, Khan F, La Mantia L, et al. Non pharmacological interventions for spasticity in multiple sclerosis. Cochrane Database Syst Rev. 2013:Cd009974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gulick EE. Bowel management related quality of life in people with multiple sclerosis: psychometric evaluation of the QoL-BM measure. Int J Nurs Stud. 2011;48:1066–70. [DOI] [PubMed] [Google Scholar]
- [5].McClurg D, Harris F, Goodman K, et al. Abdominal massage plus advice, compared with advice only, for neurogenic bowel dysfunction in MS: a RCT. Health Technol Assess. 2018;22:1–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hyarat SY, Subih M, Rayan A, et al. Health related quality of life among patients with multiple sclerosis: the role of psychosocial adjustment to illness. Arch Psychiatr Nurs. 2019;33:11–6. [DOI] [PubMed] [Google Scholar]
- [7].Gotta M, Mayer CA, Huebner J. Use of complementary and alternative medicine in patients with multiple sclerosis in Germany. Complement Ther Med. 2018;36:113–7. [DOI] [PubMed] [Google Scholar]
- [8].Kardan M, Zarei B, BahramiTaghanaki H, et al. The effects of foot reflexology on back pain after coronary angiography: a randomized controlled trial. Complement Ther Clin Pract. 2020;38:101068. [DOI] [PubMed] [Google Scholar]
- [9].Embong NH, Soh YC, Ming LC, et al. Perspectives on reflexology: a qualitative approach. J Trad Compl Med. 2017;7:327–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Wanchai A, Armer JM. A systematic review association of reflexology in managing symptoms and side effects of breast cancer treatment. Complement Ther Clin Pract. 2020;38:101074. [DOI] [PubMed] [Google Scholar]
- [11].Dikmen HA, Terzioglu F. Effects of reflexology and progressive muscle relaxation on pain, fatigue, and quality of life during chemotherapy in gynecologic cancer patients. Pain Manag Nurs. 2019;20:47–53. [DOI] [PubMed] [Google Scholar]
- [12].Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed.). 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Uchino M, Hirose K, Bando T, et al. Randomized controlled trial of prophylactic negative-pressure wound therapy at ostomy closure for the prevention of delayed wound healing and surgical site infection in patients with ulcerative colitis. Dig Surg. 2016;33:449–54. [DOI] [PubMed] [Google Scholar]
- [14].Dilek Doğan H, Tan M. Effects of reflexology on pain, fatigue, and quality of life in multiple sclerosis patients: a clinical study. Altern Ther Health Med. 2021;27:14–22. [PubMed] [Google Scholar]
- [15].Sajadi M, Davodabady F, Naseri-Salahshour V, et al. The effect of foot reflexology on constipation and quality of life in patients with multiple sclerosis. A randomized controlled trial. Complement Ther Med. 2020;48:102270. [DOI] [PubMed] [Google Scholar]
- [16].Ebrahimi N, Loripour M, Sayadi A, et al. Effect of foot reflexology on fatigue, stress and serum cortisol levels in women with multiple sclerosis. J Evol Med Dental Sci. 2020;9:2497–501. [Google Scholar]
- [17].Soheili M, Nazari F, Shaygannejad V, et al. A comparison the effects of reflexology and relaxation on the psychological symptoms in women with multiple sclerosis. J Educ Health Promotion. 2017;6:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Mackereth PA, Booth K, Hillier VF, et al. Reflexology and progressive muscle relaxation training for people with multiple sclerosis: a crossover trial. Complement Ther Clin Pract. 2009;15:14–21. [DOI] [PubMed] [Google Scholar]
- [19].Nazari F, Soheili M, Hosseini S, et al. A comparison of the effects of reflexology and relaxation on pain in women with multiple sclerosis. J Compl Int Med. 2016;13:65–71. [DOI] [PubMed] [Google Scholar]
- [20].Siev-Ner I, Gamus D, Lerner-Geva L, et al. Reflexology treatment relieves symptoms of multiple sclerosis: a randomized controlled study. Mult Scler. 2003;9:356–61. [DOI] [PubMed] [Google Scholar]
- [21].Sajadi M, Davodabady F, Ebrahimi-Monfared M. The effect of foot reflexology on fatigue, sleep quality and anxiety in patients with multiple sclerosis: a randomized controlled trial. Arch Neurosci. 2020;7. [DOI] [PubMed] [Google Scholar]
- [22].Gold R, Oreja-Guevara C. Advances in the management of multiple sclerosis spasticity: multiple sclerosis spasticity guidelines. Expert Rev Neurother. 2013;13(12 Suppl):55–9. [DOI] [PubMed] [Google Scholar]
- [23].Field T. Massage therapy research review. Complement Ther Clin Pract. 2016;24:19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Finch P, Bessonnette S. A pragmatic investigation into the effects of massage therapy on the self efficacy of multiple sclerosis clients. J Bodywork Mov Ther. 2014;18:11–6. [DOI] [PubMed] [Google Scholar]
- [25].Negahban H, Rezaie S, Goharpey S. Massage therapy and exercise therapy in patients with multiple sclerosis: a randomized controlled pilot study. Clin Rehabil. 2013;27:1126–36. [DOI] [PubMed] [Google Scholar]
- [26].Schroeder B, Doig J, Premkumar K. The effects of massage therapy on multiple sclerosis patients’ quality of life and leg function. Evid Based Compl Altern Med. 2014;2014:1640916–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Ozdelikara A, Agcadiken Alkan S. The effects of reflexology on fatigue and anxiety in patients with multiple sclerosis. Altern Ther Health Med. 2018;24:8–13. [PubMed] [Google Scholar]
- [28].Hughes CM, Smyth S, Lowe-Strong AS. Reflexology for the treatment of pain in people with multiple sclerosis: a double-blind randomised sham-controlled clinical trial. Mult Scler. 2009;15:1329–38. [DOI] [PubMed] [Google Scholar]
- [29].Lee YM. [Effects of self-foot reflexology on stress, fatigue, skin temperature and immune response in female undergraduate students]. J Korean Acad Nursing. 2011;41:110–8. [DOI] [PubMed] [Google Scholar]
- [30].Miller L, McIntee E, Mattison P. Evaluation of the effects of reflexology on quality of life and symptomatic relief in multiple sclerosis patients with moderate to severe disability; a pilot study. Clin Rehabil. 2013;27:591–8. [DOI] [PubMed] [Google Scholar]