Abstract
A variety of reduction labiaplasty techniques have been introduced to date, but no single technique will offer the optimal solution for every patient. Rather, the technique should be chosen based on anatomical, configurational, and technical considerations, as well as on patients' personal preferences regarded maintenance of the labial rim, maintenance of labial sensitivity, and prevention of iatrogenic thickening of the labium. We reviewed, defined, and assessed labial configurational variety, neurovascular supply, reduction techniques, and patient's preferences as the considerations relevant to the choice of labiaplasty technique. Based on this review, an algorithm was constructed that leads to a choice of reduction technique through five decisions to be made regarding (1) resection or (partial) retention of the labial free rim, (2) the measure of required labial width reduction, (3) labial vascular status, (4) prevention of iatrogenic labial thickening, and (5) preservation of labial sensibility. The choice of techniques includes edge trimming, central spindle form de-epithelialization or full-thickness resection, and three modifications of the wedge resection or de-epithelialization technique. These three modifications comprised a modified anterior resection or de-epithelialization combined with posterior flap transposition, a custom flask resection or de-epithelialization, and a modified posterior wedge resection or de-epithelialization combined with anterior flap transposition. Use of the five decisional steps and the inclusion of modifications of all three conventional reduction techniques offer an improved algorithm for the choice of labioplasty technique.
Keywords: algorithm, female, vulva, cosmetic surgery, review
Introduction
Despite the reservations harbored by various physicians and behavioral therapists regarding female genital aesthetic surgery, 1 2 3 labia minora reduction has become a mainstream treatment in economically flourishing societies. 3 The number of registered labiaplasties in the United States, for example, has increased sevenfold over the last decade, from 2142 in 2011 to 14,386 in 2020. 4 Parallel to the increase, a variety of labiaplasty techniques have been developed, presented, and reflected on. Because all have their advantages and limitations, no single one technique will offer the optimal solution for every patient. 5 6 7 8 9 10 Rather, the technique should be chosen in accordance with the expectations and anatomical features of each individual patient. 5 10 11 12 13 14
To date, some classifications have been presented to guide this choice, most of them based on labia minora width measurement, 15 labial configuration, 10 13 16 or a combination of both. 8 17 Only very few authors actually paired the various classes with various labiaplasty techniques, thereby offering a true algorithm. 6 10 18 None of these algorithms incorporated patients' preferences regarded maintenance of the labial free rim, maintenance of labial sensitivity, and prevention of iatrogenic thickening of the labium. Still, any one of these considerations may be of particular interest to the patient.
The purpose of this study was to elucidate these considerations and establish an algorithm for choice of labia minora reduction technique based on them. To do so, we found we had to (re-)define some of the terms used regarding labiaplasty. The terms width and length , 10 14 19 20 21 for instance, are used inconsistently for what would in French medical literature and stereometrically be referred to as “height.” 22 23 24 Furthermore, we (re-)assessed the considerations relevant to the choice of labiaplasty technique.
Definitions
Anteriorly, each labium minus divides into a lateral and a medial skin fold. The bilateral medial folds unite at the clitoral glans to form the clitoral frenulum, whereas both lateral folds unite over the clitoris to form the clitoral hood, or prepuce. Likewise, both minor labia are often connected with each other posteriorly, rounding the vaginal introitus as the labial frenulum, or fourchette. In a strict sense, the length of a labium minus should thus be measured from the median at the clitoral hood anteriorly, to the median at the fourchette posteriorly. 24 Still, for this work we defined the length relevant for labiaplasty as the measurement along the free rim of the labium minus from the point of transition of frenulum to labium anteriorly to the point where the fourchette leaves the medial aspect of the labium majus posteriorly ( Fig. 1 ). 25 26
Fig. 1.
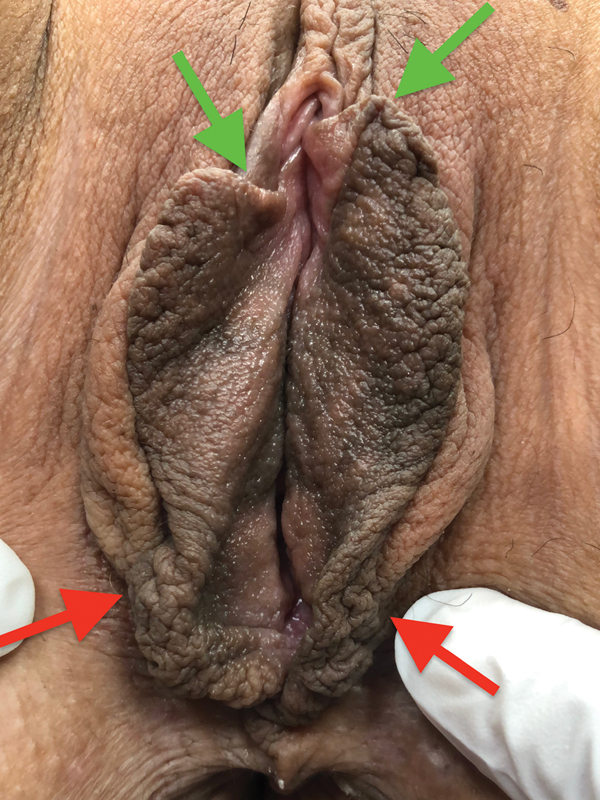
The clinically relevant length for labiaplasty was defined as the measurement along the free rim of the minor labium from the frenulum division anteriorly (green arrows) to the point where the fourchette leaves the medial aspect of the major labium posteriorly (red arrows).
The width of the labium minus was defined as the distance from its lateral base where the labium minus borders the labium majus in the interlabial sulcus, to the outer most part of its free rim when not stretched. The measure of protrusion of the labium minus past the labium majus, however, is clinically more relevant for labiaplasty. The thickness of the labium minus was defined as the mediolateral distance between the medial and lateral skin surface of the labium.
In cases where skin folds extend anteriorly from the labium minus proper to longitudinally run lateral and parallel to the clitoral hood, these folds were regarded as the paralabial folds ( plis paranymphéaux ) recorded by Jayle, in 1918. 22 These seem to correspond with the “secondary labia,” 27 “accessory labia,” 19 “redundant lateral labium,” 28 or “lateral hood folds.” 29 These are not to be confused with a relative surplus of prepuce 13 18 28 that may occur in combination with, or apart from paralabial folds ( Fig. 2 ). Finally, longitudinal skin folds extending posteriorly past the point where the fourchette leaves the labium majus are referred to as commissural folds ( plis commissureaux ). 22 For reasons of comprehensibility, our algorithm is restricted to the choice of technique of labia minora reduction. Thus, possible correction of the clitoral hood, posterior fourchette, paralabial folds, or commissural folds are to be considered separately when applicable.
Fig. 2.
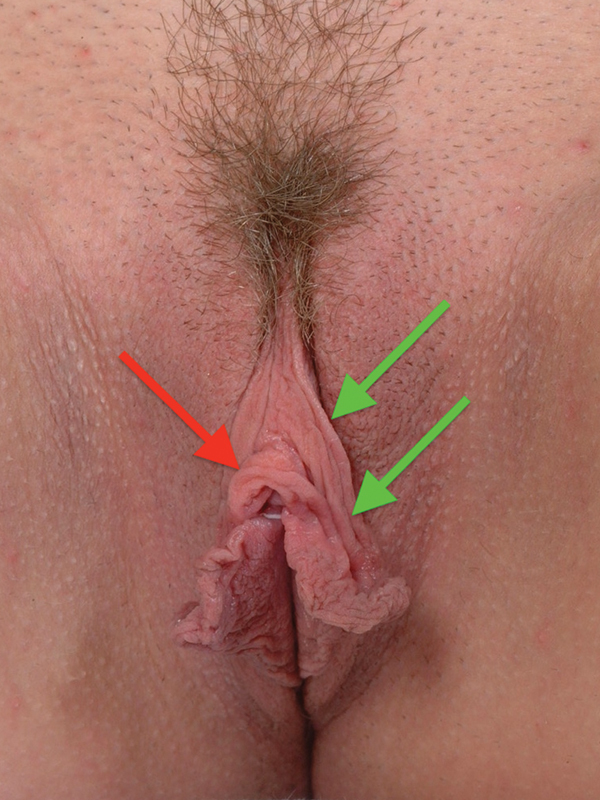
A relative surplus of preputium (red arrow) is not to be confused with paralabial folds (both green arrows).
Patient's Considerations
Patients and physicians may consciously or subconsciously differ in opinion as to the aesthetics of labia minora. 5 10 14 20 28 30 31 Like holds true for all aesthetic considerations, cultural influences (e.g., peers, media, art) largely define accepted standards of normality. 13 20 26 32 Most women in Western culture perceive a symmetrical vulva with minor labia and a clitoral hood tucked inside the major labia as normal. 10 32 Still, the surgeon needs to assess whether the patient wants her minor labia to sit flush with , or entirely hidden by the major labia. 33 Yurteri-Kaplan et al, 32 furthermore, suggested an age-related difference in patients' expectations. They found younger women to perceive the nongaping introitus featured by popular media as normal, whereas older women may desire restoration of prior individual appearance and anatomy. Moreover, some women prefer to have a darker pigmented free edge removed because they associate it with an aged appearance, 30 whereas others prefer to keep this natural aesthetic. 7 Significant pigmentation variation from the labia free rim inward, furthermore, may warrant edge preservation particularly in women of color. 29 Because of the wide spectrum of patient considerations and expectations, every patient's aesthetic or functional goals ought to be identified before a surgical technique can be decided on. 7 10 16 21 29 34 38
Configurational Considerations
Even though the request to rid the patient from any protrusion of the labium minus past the major labium may appear simple, the surgeon also has to consider the variation in labium minus configuration. 8 14 16 35 This configuration may be classified according to the location of the protrusion or relative surplus of tissue. 6 8 9 18 35 36 As such, we differentiate between predominately anterior protrusion, 8 10 14 18 30 35 predominately middle protrusion, 10 30 35 predominately posterior protrusion, 10 35 and anteroposteriorly generalized protrusion. 8 18 30
Anatomical Considerations
Accurate understanding of the labial neurovascular system may improve the surgical approach and outcome of labium reduction. 24 37 38 Salmon has been the first to record the labial vascular system by his meticulous and systematic radiographic studies of the integumental vascularization, in 1936. 39 He found the anterior one-third of the labia minora to be perfused by a branch deriving from the external pudendal artery and the posterior two-thirds by small internal pudendal branches that run perpendicular to the labial long axis ( Fig. 3 ). He recorded the two systems to anastomose and form an arcade along the labial free rim. 39
Fig. 3.

In 1936, Michel Salmon recorded the anterior one-third of the minor labia to be perfused by a branch deriving from the external pudendal artery and the posterior two-thirds by small internal pudendal branches that run perpendicular to the labial long axis. The two systems anastomose to form an arcade along the labial free rim. Note that central arteries may bilaterally be observed running to the most protruding part of the labial free rim. (Reproduced by kind permission from G.I. Taylor and M.N. Tempest, editors. Michel Salmon's Arteries of the Skin. London, UK: Churchill Livingstone; 1988).
In accordance with Salmon's radiographic study, Georgiou et al 36 more recently identified one dominant central , and three lesser arteries to originate from the internal pudendal system in 9 specimens. This central artery ran up to the labial free rim to continue along it in anterior direction and anastomose with external pudendal branches. These findings, in turn, were generally supported by a translabial illumination study by Kaya et al. 9 These authors, however, stressed that the position of the central artery predominately depends on the localization of maximum labial protrusion, rather than it being centrally located in all cases. 9 Hence, their observations appear to oppose Alter's stressing the importance of excising the most enlarged part of the labium minus, 40 as this will significantly reduce the remaining labial vascularization.
Georgiou et al, 36 furthermore, observed that the labial arteries run superficially under the skin, thus refuting the central core vascularization of the labium minus conceptualized by Heusse et al 23 and supported by the observations by Ginger et al. 37 Consequently, they warned that central de-epithelialization techniques present some risk of labial ischemia as the vessels may be injured. 36
Still, Ginger et al 37 concluded that the number of vascular structures in the minor labia is much more than what would be expected to maintain baseline vascular sufficiency for such small skin folds. This is supported by the lack of ischemia after splitting of the inner and outer aspect of the labium to allow opposite transplantation of each, in 70 metaidoioplasties. 41 In other words, labial vascularization is rich and its local interruption will seldom result in ischemia in women without potential circulatory risk factors such as tobacco abuse, diabetes mellitus, or other vascular disorders. 6 28 42 43 In heavy smokers and other women at risk, preoperative cold light assisted labial transillumination may be helpful to assess and map the labial vascular supply. 9
The sensory innervation of the labium minus may be a point of more concern. Internal and external pudendal nerve branches innervating the labium minus accompany the vascular ramifications and tend to course most readily along the free rim of the labium. 37 44 Labial innervation is unidirectional and its transection may result in loss of sensibility in part of the labium possibly affecting sexual function or, 10 28 worse, in neuroma formation along the suture line. 25 Because both the pudendal labial innervation and the dorsal clitoral innervation seem to convers to the clitoral frenulum, surgeon and patient alike ought to accept this frenulum to be a surgical no go area . It is our experience, in women as in men, that incising the frenulum easily results in neuroma formation with symptoms that are near impossible to treat.
Technical Considerations
Edge resection, wedge excision, and central de-epithelialization have been recognized, modified, and combined over the last four decennia as the three principal techniques for labial reduction ( Fig. 4 ). It is generally agreed that no reduction technique should decrease the remaining labial width to less than 1 cm measured from the interlabial sulcus. 10 11 20 29 31 45 46 Suspension of the lateral most tip of the minor labium may help plan and execute the reduction. 21 31 38
Fig. 4.
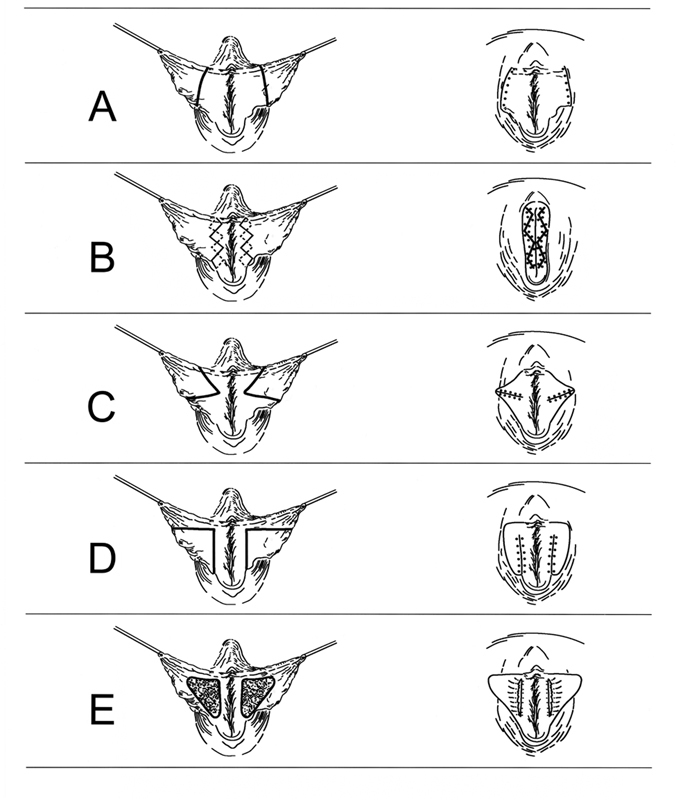
Edge resection, wedge excision, and central de-epithelialization are the three principal techniques for minor labial reduction. (A) Edge resection or trimming involves the straightforward amputation of protuberant tissues. Note that it additionally reduces the labial free rim length. (B) Straight amputation has been modified to a running W-resection to ensure a more robust and natural appearing rim after reduction. (C) Wedge excision involves the resection of a triangular part of skin at both the lateral and medial aspect of the labium minus. Note that it may correct a surplus of labial free rim length but only partly corrects labial width. (D) The initially central wedge excision has been modified to the dorsal wedge excision and anterior flap technique. Note that this modification also lowers the labial width and that the resulting scar runs less conspicuously along the base of the labium minus. (E) Central de-epithelialization involves the partial skinning of the medial and lateral aspects of the labium from its introital base, respectively, the interlabial sulcus outward. It may also be executed as a full-thickness resection or fenestration . Note that this will not reduce the labium free rim length.
Edge resection or trimming involves the straightforward amputation of protuberant tissues. It additionally reduces the labial free rim length ( Fig. 4A ) and is adaptable to virtually any labial size or shape. 29 It removes the possibly pigmented or corrugated free edge of the labium. Of the three principal techniques, trimming features the smallest risk of dehiscence. It potentially increases the risk of tenderness during sexual intercourse and scar contracture, 6 but such sequences have never been validated. 29 46 Straight amputation has been modified to a running W-resection to ensure a more robust and natural appearing rim postoperatively ( Fig. 4B ). 31 45
Wedge excision basically involves the resection of a triangular part of skin at both the lateral and medial aspect of the labium. The base of the triangle is located along the rim of the most protruding part of the labium. 12 30 The top of the triangle to be excised is pointing toward the interlabial sulcus on the lateral aspect and toward Hart's line on the medial aspect. Wedge resection may correct a surplus of labial length but only partly corrects labial width ( Fig. 4C ). 11 It saves the appearance of the remaining parts of the free labial edge. This may result in an abrupt transition of a more bulky, pigmented, or corrugated anterior edge to a finer and less pigmented posterior edge. 28 Likewise, an abrupt change of pigmentation may occur along the perpendicular scar, particularly on the medial aspect of the labium minus. 12 28 Alter's central wedge excision technique has been modified to the dorsal wedge excision and anterior flap technique by Rouzier et al. 47 The resulting scar then runs posterior and less conspicuous along the base of the labium minus. Munhoz et al, 5 Smarrito, 18 and Yang and Hengshu 10 further modified the anterior flap design to additionally reduce labial width ( Fig. 4D ). Of the three principal techniques, full-thickness wedge excision features the greatest wound dehiscence risk with reported prevalences of 7 to 14%. 5 47 Consequently, Alter more recently advocated restricting the technique to wedge de-epithelialization rather than full-thickness resection. 28
Central de-epithelialization involves the partial skinning of the medial and lateral aspects of the labium from its introital base, respectively, the interlabial sulcus outward ( Fig. 4E ). 11 This will decrease labial width but not the length of its free rim, which potentially results in festooning of the rim. 12 28 Central de-epithelialization may result in a longitudinal line of abrupt change of coloration where the epithelium is reapproximated and some authors have argued that the longitudinal scar created by this technique may distort the labia. 12 31 Again, the latter sequence has not been validated to date. 46 De-epithelialization techniques, in general, are applied to save the neurovascular supply. They also save all, or part, of the subcutaneous bulk and likely result in telescoping 48 of the remaining labial tissues and increased thickness of all but the least protruding minor labia. 6 12 28 29 46 48 Additionally, such telescoping may increase the risk of wound dehiscence. When done as a full-thickness resection rather than a de-epithelialization, 13 42 however, wound dehiscence will even result in fenestration. 42 Furthermore, the risk of loss of neurovascular supply to the free rim then lurks. 12
Combined wedge excision and central de-epithelialization was suggested as a bidimensional technique 48 and as custom flask labiaplasty . 35 Comparable addition of medial anterior and posterior triangular wedges to be excised perpendicular to the principal wedge had already been suggested by Alter, as early as 1998, 30 and this may be considered the full-thickness equivalent of the custom flask labiaplasty. Smarrito 18 and Yang and Hengshu 10 introduced three further modifications of the wedge excision design, whereas Jiang et al 34 reported combining a medial wedge excision with a partial edge resection. With these combined techniques, the authors tried to prevent remaining labial protrusion, 10 18 30 34 35 48 festooning of remaining labial rim length, 10 18 34 35 48 free rim alteration, 10 18 48 loss of neurovascular supply, 34 35 and wound dehiscence. 34
Algorithmic Decisional Steps
We propose to start the choice of labiaplasty technique by establishing whether or not the free rim of the labium is to be resected partially, entirely, or not at all ( Fig. 5 ). This may be of particular interest in women who present with labial asymmetry. In these, it has to be decided whether to reduce only the wider labium and preserve the entire rim to optimally match the contralateral one, or perform an asymmetrical bilateral reduction that may include bilateral (partial) rim resection. Reasons for entire resection include unwanted pigmentation and a corrugated appearance of the rim. Preservation of the entire rim is preferred to prevent a scar crossing the rim or a sudden change of pigmentation between its anterior and posterior parts. Partial rim resection may be indicated in cases where unwanted corrugation, pigmentation, or protrusion is restricted to part of the rim.
Fig. 5.
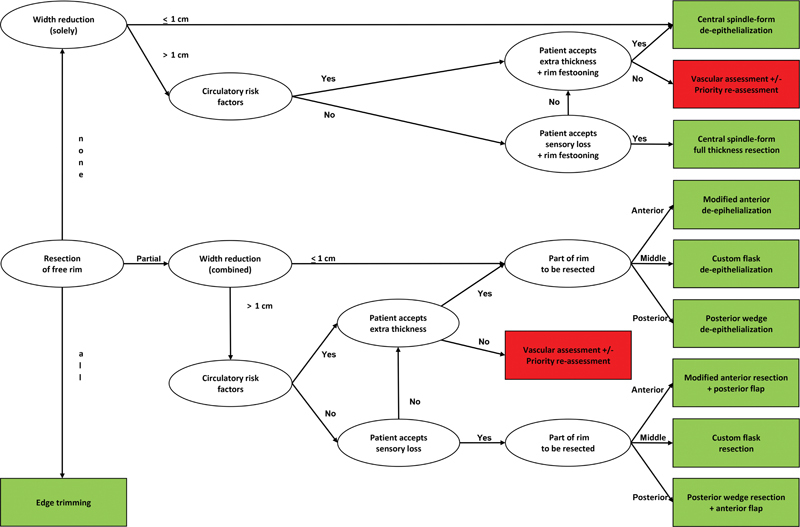
Flowchart of the proposed algorithm for the choice of reduction labiaplasty technique.
Second, the width to be resected needs be considered in candidates for (partial) rim preservation. Obviously, this width to be resected equals the labial width with which the woman presents, minus the width that is preferred by her. In cases where this width of resection is limited to 1 cm, the reduction may be done by de-epithelialization without the risk of conspicuous thickening of the labium. More extended reductions de-epithelialization tends to result in such thickening.
Next, circulatory risk factors are to be assessed and weighed. To reduce postoperative ischemic complications such as wound dehiscence and partial necrosis, de-epithelialization techniques are to be preferred over excision in heavy smokers and otherwise vascular compromised women. This implies that vascular compromised women in whom the intended width reduction is more than 1 cm are to accept iatrogenic thickening of their labium. Furthermore, possible festooning of the rim is to be accepted in such women in whom the entire rim is preserved. In cases where this is not accepted, preoperative labial transillumination may help design a safer resection. 9
In non-vascular compromised women in whom the intended width reduction is more than 1 cm, on the other hand, the risk of loss of labial sensitivity associated with central excisional techniques has to be weighed against the risk of labial thickening associated with de-epithelialization techniques.
Last, the technique for labiaplasty is paired to the location of the corrugation, pigmentation, or protrusion to be resected in candidates for partial rim resection.
Algorithmic Choice of Labiaplasty Technique
The outcome of the decisional steps of our algorithm includes edge resection according to Maas and Hage and Solanki et al 31 45 ( Fig. 6A ), central de-epithelialization or fenestration ( Fig. 6B ), according to Choi and Kim, 11 da Cunha et al, 13 and Laub, 42 and one out of three modifications of wedge resection or de-epithelialization. These modifications are:
Fig. 6.
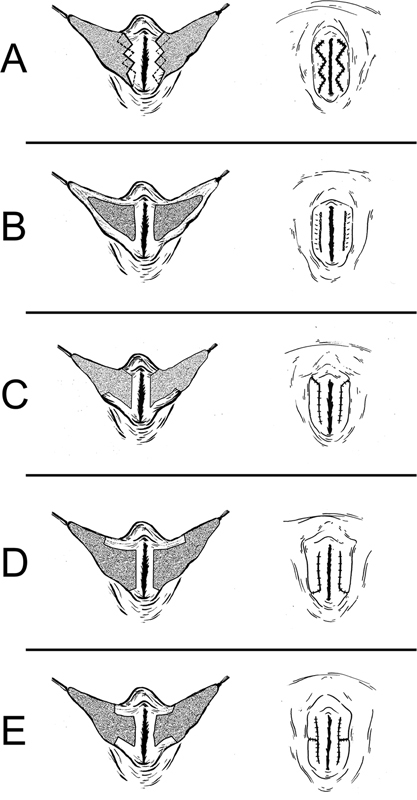
Artist impression of preoperative markings (left) and postoperative outcome (right) of each of the techniques included in the algorithm. The shaded area on the left side represents the part of the labia to be de-epithelialized or resected prior to: (A) Running W-resection of the labial rim; (B) Central de-epithelialization or fenestration. Note that this will not reduce the labium free rim length; (C) Modified anterior wedge de-epithelialization or resection combined with posterior flap transposition; (D) Posterior wedge de-epithelialization or resection combined with anterior flap transposition; (E) Custom flask de-epithelialization or full-thickness resection.
- Modified anterior wedge resection combined with posterior flap transposition according to Yang and Hengshu's method A, 10 and its de-epithelialization execution according to Alter 28 ( Fig. 6C );
- Posterior wedge resection combined with anterior flap transposition according to Munhoz et al, 5 Smarrito's Lambda technique, 18 and Yang and Hengshu's method C, 10 and its de-epithelialization modification according to Tremp et al 38 ( Fig. 6D );
- Custom flask de-epithelialization according to Gonzalez et al 35 and its full-thickness resection modification as proposed by Alter, 30 in cases of predominately middle disfigurement or protrusion ( Fig. 6E ).
Preoperative and postoperative clinical examples of each of these techniques have amply been illustrated in the original publications by the various authors. 5 11 18 28 31 35 38 45
The Algorithm in Historical Perspective
To date, only three groups of authors offered a true algorithm for choice of labiaplasty technique by pairing various classes of labial features with various reduction techniques. 6 10 18 As such, Ellsworth et al 6 adopted the classification based on absolute labial width as proposed by Franco and Franco 15 for their choice of technique. They applied the central de-epithelialization technique according to Choi and Kim 11 to reduce labia presenting with up to 4 cm (Franco Classes 1 and 2) and the inferior wedge technique according to Munhoz et al 5 in labia over 6 cm wide (Franco Class 4). Franco Class 3 labia (of 4–6 cm width) was preferably treated by lazy-S edge trimming according to Felicio, 49 but the inferior wedge technique was applied in those women who preferred to retain the natural labial edge. 6 Hence, their algorithm was based exclusively on absolute labial measurements, disregarding configurational variations and remaining protrusion associated with wedge resection.
Smarrito 18 used a classification based on the location of the relative surplus of tissue as applied previously by Gonzalez et al 35 and González, 8 and subsequently by Kaya et al 9 and Hamori and Stuzin. 16 He distinguished type I with anterior third redundancy; type II with middle third redundancy; and type III with posterior third redundancy. An anterior redundancy was treated by an incision along the posterior half of the labial rim, after which the protruding anterior part was folded dorsally to be sutured to the incised edge of the lower, most posterior part of the labium. Middle third redundancies were treated with a slightly modified posterior wedge technique, 47 whereas Smarrito combined his Lambda posterior resection and anterior flap technique for a posterior redundancy. 18 Thus, the anterior half of the labial rim was used to replace the resected posterior rim in all patients, regardless of its appearance or patients' preferences.
Yang and Hengshu 10 introduced a more extensive classification system according to the location of labial redundancy. They distinguished six configurational types: 1—anterior protrusion; 2—central protrusion; 3—posterior protrusion; 4—redundant anterior–posterior labial length; 5—generalized width and length redundancy; and 6—labial protrusion combined with preputial redundancy. To treat types 1 to 5, the authors suggested three different techniques of reduction: A—full labial resection except for a posteriorly based, rectangular edge flap that was used to replace all of the excised tissue for types 1 and 5 redundancies; B—full labial resection except for both an anterior and a posteriorly based rectangular edge flap that were used to replace all of the excised tissue for a type 2 redundancy; C—full labial resection except for an anteriorly based, triangular edge flap that was used to replace all of the excised tissue for types 3, 4, and 5 redundancies. For type 6 combined labial and preputial redundancy, the authors suggested two additional techniques. 10 Hence, their algorithm was based solely on the presenting labial configuration without consideration of labial color and texture, 21 46 or postoperative rim appearance, labial sensitivity, and pigmentation changes.
The algorithm we propose is based on individualized anatomical, configurational, and personal considerations, which can be applied unilaterally or bilaterally. In this algorithm, normative classifications of labial width are ignored. From the available normative datasets on labia minora width measurements 19 27 33 may be concluded that normal labial width varies enormously. Kreklau et al, 50 furthermore, observed a negative correlation between body mass index and labia minora width and Gress 24 stressed how the level of the interlabial sulcus can vary in relation to the vestibulum. Therefore, absolute width measurement cannot be used as a possible base for surgical decisions. 18 Rather, the request often concerns any measure of protrusion of the labia minora beyond the labia majora. 8 20 46 In the vast majority of women, this request is aesthetically driven. 29 30 47 Some of these women may be reassured by explaining that their labial features are within a normal range and loose interest in labiaplasty (the so-called desisters ), but an increasing number of them will persist in their wish for labiaplasty despite such explanation (the persisters ). 33 Like rhinoplasty, mammaplasty, and lipofilling that all usually adjust features that are within a normal range, reduction labiaplasty has become one possibility in an ever increasing array of aesthetic operations.
Given this, it is our task to improve and extend our techniques and assure that each individual patient obtains an optimal result. 10 29 The labiaplasty surgeon can no longer hide behind the adage to use the one technique you are most confident with because of the various, possibly conflicting, considerations present in each patient. 10 Consequently, the surgeon working with our proposed algorithm is required to master modifications of all three conventional reduction techniques, each to be executed either by excision or by de-epithelialization.
Potential Pitfalls of Reduction Labiaplasty
Although the minor labia are usually the focus of patients' concerns, achieving a desirable cosmetic outcome may require additional external genital alterations. When not discussed, failure to concurrently address an explicit clitoral hood may result in the patient complaining of a masculine, penile appearance. 29 40 On the other hand, unsolicited concurrent reduction in the clitoral hood or posterior fourchette may result in aesthetic disappointment or, worse, in complaints or disorders of sexual function. Hence, it is wise to evaluate the entire anatomic region—minor labia, major labia, clitoral hood, perineum, and mons pubis—during the consultation of women seeking labiaplasties. 24 29 Any involvement of the clitoral prepuce and posterior fourchette, in particular, needs to be considered preoperatively. Reduction in the prepuce may be achieved by separate longitudinal, 17 transverse, 29 or combined longitudinal and transverse resections, 42 or by extension of the design of reduction of the lateral labial aspect toward the prepuce. 13 28 29 Even though some authors record that reduction in the fourchette can be performed equally simple by direct resection, 10 17 18 others regard the fourchette a surgical no go area . 11 20 30 46 We consider fourchette trimming to feature the risk of contracture of a scar that crosses transversely over the posterior introitus which, in turn, may obliterate the introitus. Therefore, we advocate including multiple Z-plasties when preforming posterior fourchette trimming.
Future Perspectives and Conclusion
Future algorithms may be additionally proposed for the assessment and treatment of the other female genital structures. Still, the decision on technique for the reduction in the labium proper can best be reached separately from considerations regarding the other aspects of female genital aesthetic surgery. We feel that the five steps to be considered and the inclusion of modifications of all three conventional reduction techniques in the algorithm offer an improvement over previously presented algorithms.
Funding Statement
Funding None.
Conflict of Interest None declared.
Research Involving Human Participants
This article does not contain any studies with humans performed by any of the authors.
Research Involving Animals
This article does not contain any studies with animals performed by any of the authors.
Patient Consent
Informed consent was obtained from the individual participants of whom photographs were included in the study.
Ethical Approval
The Institutional Review Board confirmed that no ethical approval is needed for this review study.
Authors' Contributions
M.L. contributed to the conceptualization, investigation, data curation, methodology, and formal analysis of the study, and to the visualization and writing of the original draft and final manuscript. He accepts full accountability for all aspects of the work.
J.J.H. contributed to the project administration, conceptualization, investigation, methodology, formal analysis, and supervision of the study, and to writing the original draft and final manuscript. He accepts full accountability for all aspects of the work.
R.B.K. contributed to the conceptualization, formal analysis and interpretation of data, and to the writing of the original draft and final manuscript. He accepts full accountability for all aspects of the work.
F.A. contributed to the project administration, the conceptualization, resources, investigation, methodology, formal analysis and supervision of the study, and to writing the original draft and final manuscript. He accepts full accountability for all aspects of the work.
References
- 1.Vieira-Baptista P, Almeida G, Bogliatto F. International Society for the Study of Vulvovaginal Disease recommendations regarding female cosmetic genital surgery. J Low Genit Tract Dis. 2018;22(04):415–434. doi: 10.1097/LGT.0000000000000412. [DOI] [PubMed] [Google Scholar]
- 2.Chibnall K, McDonald K, Kirkman M. Pathologising diversity: medical websites offering female genital cosmetic surgery in Australia. Cult Health Sex. 2020;22(01):64–80. doi: 10.1080/13691058.2019.1574029. [DOI] [PubMed] [Google Scholar]
- 3.Boddy J. Re-thinking the zero tolerance approach to FGM/C: the debate around female genital cosmetic surgery. Curr Sex Health Rep. 2020;12:302–313. [Google Scholar]
- 4.Society T A.The Aesthetic Plastic Surgery National Databank Statistics 2020 2021 Accessed September 28, 2022, at:https://cdn.theaestheticsociety.org/media/statistics/aestheticplasticsurgerynationaldatabank-2020stats.pdf
- 5.Munhoz A M, Filassi J R, Ricci M D. Aesthetic labia minora reduction with inferior wedge resection and superior pedicle flap reconstruction. Plast Reconstr Surg. 2006;118(05):1237–1247. doi: 10.1097/01.prs.0000237003.24294.04. [DOI] [PubMed] [Google Scholar]
- 6.Ellsworth W A, Rizvi M, Lypka M. Techniques for labia minora reduction: an algorithmic approach. Aesthetic Plast Surg. 2010;34(01):105–110. doi: 10.1007/s00266-009-9454-5. [DOI] [PubMed] [Google Scholar]
- 7.Ellsworth W A, Rizvi M, Smith B, Cohen B, Dinh T. Labia minora reduction: guidelines for procedure choice. Plast Reconstr Surg. 2010;125(05):216e–217e. doi: 10.1097/PRS.0b013e3181d62a3d. [DOI] [PubMed] [Google Scholar]
- 8.González P I. Classification of hypertrophy of labia minora: consideration of a multiple component approach. Surg Technol Int. 2015;27:191–194. [PubMed] [Google Scholar]
- 9.Kaya A E, Dogan O, Yassa M, Basbug A, Çalışkan E. A novel technique for mapping the vascularity of labia minora prior to labiaplasty: cold light illumination. Geburtshilfe Frauenheilkd. 2018;78(08):775–784. doi: 10.1055/a-0647-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang E, Hengshu Z. Individualized surgical treatment of different types of labia minora hypertrophy. Aesthetic Plast Surg. 2020;44(02):579–585. doi: 10.1007/s00266-019-01545-9. [DOI] [PubMed] [Google Scholar]
- 11.Choi H Y, Kim K T.A new method for aesthetic reduction of labia minora (the deepithelialized reduction of labioplasty) Plast Reconstr Surg 200010501419–422., discussion 423–424 [DOI] [PubMed] [Google Scholar]
- 12.Giraldo F, González C, de Haro F.Central wedge nymphectomy with a 90-degree Z-plasty for aesthetic reduction of the labia minora Plast Reconstr Surg 2004113061820–1825., discussion 1826–1827 [DOI] [PubMed] [Google Scholar]
- 13.da Cunha F I, da Silva L M, de Araújo Costa L, Paes Vasconcelos F R, Trombetta Amaral G. Nymphoplasty: classification and technical refinements. Rev Bras Cir Plást. 2011;26:507–511. [Google Scholar]
- 14.Furnas H J, Canales F L, Pedreira R A, Comer C, Lin S J, Banwell P E. The safe practice of female genital plastic surgery. Plast Reconstr Surg Glob Open. 2021;9(07):e3660. doi: 10.1097/GOX.0000000000003660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franco T, Franco D. Hipertrofia de ninfas. J Bras Ginecol. 1993;103:163–165. [Google Scholar]
- 16.Hamori C A, Stuzin J M. Female cosmetic genital surgery. Plast Reconstr Surg. 2018;141(04):916–918. doi: 10.1097/PRS.0000000000004263. [DOI] [PubMed] [Google Scholar]
- 17.Chang P, Salisbury M A, Narsete T, Buckspan R, Derrick D, Ersek R A. Vaginal labiaplasty: defense of the simple “clip and snip” and a new classification system. Aesthetic Plast Surg. 2013;37(05):887–891. doi: 10.1007/s00266-013-0150-0. [DOI] [PubMed] [Google Scholar]
- 18.Smarrito S. Classification of labia minora hypertrophy: a retrospective study of 100 patient cases. JPRAS Open. 2017;13:81–91. [Google Scholar]
- 19.Dickinson R L.The Vulva and BreastA Topographical Hand Atlas of Human Sex Anatomy. 2nd edition.Baltimore, USA: Williams Wilkins; 194940–70. [Google Scholar]
- 20.Hodgkinson D J, Hait G. Aesthetic vaginal labioplasty. Plast Reconstr Surg. 1984;74(03):414–416. doi: 10.1097/00006534-198409000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Filho O P, Ely J B, Lee K H, Paulo E M. Labiaplasty with stable labia minora retraction-butterfly-like approach. Plast Reconstr Surg Glob Open. 2020;8(04):e2664. doi: 10.1097/GOX.0000000000002664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jayle F., IIILes nymphes ou petites lèvresLa gynécologie, Tome 1 - Lánatomie morphologique de la femme.Paris: Masson; 1918365–95. [Google Scholar]
- 23.Heusse J-L, Cousin-Verhoest S, Aillet S, Watier É. Mise au point sur les techniques de nymphoplastie de réduction. Ann Chir Plast. 2009;54:126–134. doi: 10.1016/j.anplas.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Gress S.Aesthetic and functional labiaplastyCham, Switzerland: Springer Nature; 2017. Accessed September 28, 2022, athttps://link.springer.com/content/pdf/10.1007%2F978-3-319-60222-6.pdf [Google Scholar]
- 25.Lloyd J, Crouch N S, Minto C L, Liao L M, Creighton S M. Female genital appearance: “normality” unfolds. BJOG. 2005;112(05):643–646. doi: 10.1111/j.1471-0528.2004.00517.x. [DOI] [PubMed] [Google Scholar]
- 26.Lykkebo A W, Drue H C, Lam J UH, Guldberg R. The size of labia minora and perception of genital appearance: a cross-sectional study. J Low Genit Tract Dis. 2017;21(03):198–203. doi: 10.1097/LGT.0000000000000308. [DOI] [PubMed] [Google Scholar]
- 27.Bergh R. Symbolae ad cognitionem genitalium externorum foemineorum II. Monatshefte für praktische Dermatologie. 1897;24:74–86. [Google Scholar]
- 28.Alter G J. Aesthetic labia minora and clitoral hood reduction using extended central wedge resection. Plast Reconstr Surg. 2008;122(06):1780–1789. doi: 10.1097/PRS.0b013e31818a9b25. [DOI] [PubMed] [Google Scholar]
- 29.Hunter J G. Labia minora, labia majora, and clitoral hood alteration: experience-based recommendations. Aesthet Surg J. 2016;36(01):71–79. doi: 10.1093/asj/sjv092. [DOI] [PubMed] [Google Scholar]
- 30.Alter G J. A new technique for aesthetic labia minora reduction. Ann Plast Surg. 1998;40(03):287–290. doi: 10.1097/00000637-199803000-00016. [DOI] [PubMed] [Google Scholar]
- 31.Maas S M, Hage J J. Functional and aesthetic labia minora reduction. Plast Reconstr Surg. 2000;105(04):1453–1456. doi: 10.1097/00006534-200004040-00030. [DOI] [PubMed] [Google Scholar]
- 32.Yurteri-Kaplan L A, Antosh D D, Sokol A I. Interest in cosmetic vulvar surgery and perception of vulvar appearance. Am J Obstet Gynecol. 2012;207(05):4280–4.28E9. doi: 10.1016/j.ajog.2012.06.056. [DOI] [PubMed] [Google Scholar]
- 33.Hayes J A, Temple-Smith M J. What is the anatomical basis of labiaplasty? A review of normative datasets for female genital anatomy. Aust N Z J Obstet Gynaecol. 2021;61(03):331–338. doi: 10.1111/ajo.13298. [DOI] [PubMed] [Google Scholar]
- 34.Jiang X, Chen S, Qu S. A new modified labiaplasty combined with wedge de-epithelialization on the medial side and edge resection. Aesthetic Plast Surg. 2021;45(04):1869–1876. doi: 10.1007/s00266-021-02137-2. [DOI] [PubMed] [Google Scholar]
- 35.Gonzalez F, Dass D, Almeida B. Custom flask labiaplasty. Ann Plast Surg. 2015;75(03):266–271. doi: 10.1097/SAP.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 36.Georgiou C A, Benatar M, Dumas P. A cadaveric study of the arterial blood supply of the labia minora. Plast Reconstr Surg. 2015;136(01):167–178. doi: 10.1097/PRS.0000000000001394. [DOI] [PubMed] [Google Scholar]
- 37.Ginger V A, Cold C J, Yang C C. Structure and innervation of the labia minora: more than minor skin folds. Female Pelvic Med Reconstr Surg. 2011;17(04):180–183. doi: 10.1097/SPV.0b013e318221f835. [DOI] [PubMed] [Google Scholar]
- 38.Tremp M, Oranges C M, Schaefer D J, Waldkircher N J, Schleh A C, Kalbermatten D F. The butterfly technique: a retrospective study for labia minora reduction using an integrated approach. Plast Reconstr Surg Glob Open. 2021;9(09):e3810. doi: 10.1097/GOX.0000000000003810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salmon M. London, UK: Churchill Livingstone; 1988. The trunk. In: Taylor GI, Tempest MN, eds. Arteries of the Skin; pp. 85–128. [Google Scholar]
- 40.Alter G J. Aesthetic labia minora reduction with inferior wedge resection and superior pedicle flap reconstruction. Plast Reconstr Surg. 2007;120(01):358–359. doi: 10.1097/01.prs.0000264588.97000.dd. [DOI] [PubMed] [Google Scholar]
- 41.Hage J J, van Turnhout A A. Long-term outcome of metaidoioplasty in 70 female-to-male transsexuals. Ann Plast Surg. 2006;57(03):312–316. doi: 10.1097/01.sap.0000221625.38212.2e. [DOI] [PubMed] [Google Scholar]
- 42.Laub D R. A new method for aesthetic reduction of labia minora (the de-epithelialized reduction labioplasty) by H.Y. Choi and K.T. Kim - Discussion. Plast Reconstr Surg. 2000;105:423–424. doi: 10.1097/00006534-200001000-00067. [DOI] [PubMed] [Google Scholar]
- 43.Bucknor A, Chen A D, Egeler S. Labiaplasty: indications and predictors of postoperative sequelae in 451 consecutive cases. Aesthet Surg J. 2018;38(06):644–653. doi: 10.1093/asj/sjx241. [DOI] [PubMed] [Google Scholar]
- 44.Kelishadi S S, Omar R, Herring N. The safe labiaplasty: a study of nerve density in labia minora and its implications. Aesthet Surg J. 2016;36(06):705–709. doi: 10.1093/asj/sjw002. [DOI] [PubMed] [Google Scholar]
- 45.Solanki N S, Tejero-Trujeque R, Stevens-King A, Malata C M. Aesthetic and functional reduction of the labia minora using the Maas and Hage technique. J Plast Reconstr Aesthet Surg. 2010;63(07):1181–1185. doi: 10.1016/j.bjps.2009.05.053. [DOI] [PubMed] [Google Scholar]
- 46.Motakef S, Rodriguez-Feliz J, Chung M T, Ingargiola M J, Wong V W, Patel A. Vaginal labiaplasty: current practices and a simplified classification system for labial protrusion. Plast Reconstr Surg. 2015;135(03):774–788. doi: 10.1097/PRS.0000000000001000. [DOI] [PubMed] [Google Scholar]
- 47.Rouzier R, Louis-Sylvestre C, Paniel B J, Haddad B.Hypertrophy of labia minora: experience with 163 reductions Am J Obstet Gynecol 2000182(1 Pt 1):35–40. [DOI] [PubMed] [Google Scholar]
- 48.Mayer H F, de Elizalde M LB, Duh N, Loustau H D. Bidimensional labia minora reduction. Eur J Plast Surg. 2011;34:345–350. [Google Scholar]
- 49.Felicio YdeA. Labial surgery. Aesthet Surg J. 2007;27(03):322–328. doi: 10.1016/j.asj.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 50.Kreklau A, Vâz I, Oehme F. Measurements of a ‘normal vulva’ in women aged 15-84: a cross-sectional prospective single-centre study. BJOG. 2018;125(13):1656–1661. doi: 10.1111/1471-0528.15387. [DOI] [PubMed] [Google Scholar]


