Abstract
Background
In patients with ulcerative colitis (UC) and Crohn’s disease (CD), this research examined the following: prevalence of fecal urgency (hereafter urgency), association of urgency with inflammatory bowel disease (IBD) symptoms and fecal calprotectin, and association between well-being and urgency.
Methods
In this cross-sectional study from the Study of a Prospective Adult Research Cohort with IBD, urgency was categorized as none, mild, and moderate-severe. We examined the prevalence of urgency, association of urgency with IBD symptoms and fecal calprotectin (in a subset) using multinomial logistic regression, and association of well-being (not feeling well vs generally well) with urgency using logistic regression.
Results
Among 576 UC patients, 31.4% reported mild and 28.1% moderate-severe urgency. Among 1330 CD patients, 33.8% reported mild and 31.4% moderate-severe urgency. In UC, moderate-severe urgency was associated with: increased average bowel movements/day [odds ratio (OR) 1.23; 95% confidence interval: 1.09, 1.23], increased stool frequency relative to normal (OR, 9.95; 95% CI: 3.21, 30.87), rectal bleeding (OR, 3.36; 95% CI: 1.79, 6.34), moderate-severe abdominal pain (OR, 17.5; 95% CI: 5.38, 56.89), and calprotectin ≥ 250 μg/g (OR, 4.36; 95% CI: 1.50, 12.66). In CD, moderate-severe urgency was associated with: increased average bowel movements/day (OR, 1.23; 95% CI: 1.14, 1.34), increased stool frequency relative to normal (OR, 7.57; 95% CI: 3.30, 17.34), rectal bleeding (OR, 1.77; 95% CI: 1.13, 2.78), and moderate-severe abdominal pain (OR, 7.52; 95% CI: 4.31, 13.14). Reduced well-being was associated with moderate-severe urgency in both UC (OR, 4.20; 95% CI: 1.69, 20.40) and CD patients (OR, 2.52; 95% CI: 1.51, 4.22).
Conclusions
Urgency was common and associated with symptoms and biomarkers suggesting active IBD and reduced well-being.
Keywords: fecal urgency, IBD, well-being, IBD, UC, CD
Introduction
Inflammatory bowel disease (IBD) is a chronic disease characterized by intestinal inflammation and a major cause of morbidity and healthcare utilization in the United States.1 IBD includes ulcerative colitis (UC) and Crohn’s disease (CD), which is differentiated primarily based on the location of the inflammation, histopathology and formation of strictures, fistula, and abscess.2 Common IBD symptoms include diarrhea, abdominal pain, gastrointestinal bleeding, weight loss, and malnutrition. Fecal urgency, the sense of urgency to have a bowel movement, is also commonly reported by patients with IBD but has been relatively neglected in the scientific literature despite its significant impact on patients’ quality of life.3 A 2016 Delphi survey of Nurses European Crohn’s and Colitis Organization identified fecal urgency in IBD patients as one of the top 5 research priorities.4
More than 50% of IBD patients experience some form of fecal urgency.5 A cross-sectional analysis reported that approximately 83% of UC and 74% of CD patients experience fecal urgency.6 Fecal urgency can negatively impact emotional, psychological, and social functioning.7, 8 Affected patients report higher levels of anxiety, depression, and are more likely to be confined home.7–9 Despite the high burden of fecal urgency in IBD patients, data on the prevalence and correlates of fecal urgency in IBD patients remain limited. In this research, the authors sought to examine the following in UC and CD patients: (1) prevalence of fecal urgency, (2) association of fecal urgency with IBD symptoms and with fecal calprotectin, and (3) association between well-being and fecal urgency.
Materials and Methods
Data Source
Data for this study were obtained from the IBD Plexus platform of the Crohn’s & Colitis Foundation. This cross-sectional study used data from the Study of a Prospective Adult Research Cohort with IBD (SPARC IBD). The SPARC IBD is a multicenter prospective cohort registry of well-phenotyped IBD patients initiated by the Crohn’s & Colitis Foundation in November 2016. The registry includes adult patients aged 18 years or older with CD, UC, or unclassified IBD who are cared for at 17 centers across the United States. Data in SPARC IBD are collected from an IBD Smartform embedded in the Epic electronic health record system, which includes information regarding current symptoms, surgical history, cancer/dysplasia history, medication history, laboratory data, imaging/diagnostic procedures, disease phenotype, and extraintestinal manifestations. These data are linked with biosamples, coded diagnoses from electronic medical records, and patient-reported outcome data. The study also captures data from routine care. The SPARC IBD protocol does not include a prespecified schedule for office visits or endoscopic procedures after enrollment. Our analysis utilized symptom and fecal calprotectin data collected at the time of enrollment in the SPARC IBD study and results from the first colonoscopy completed after enrollment.
Study Population
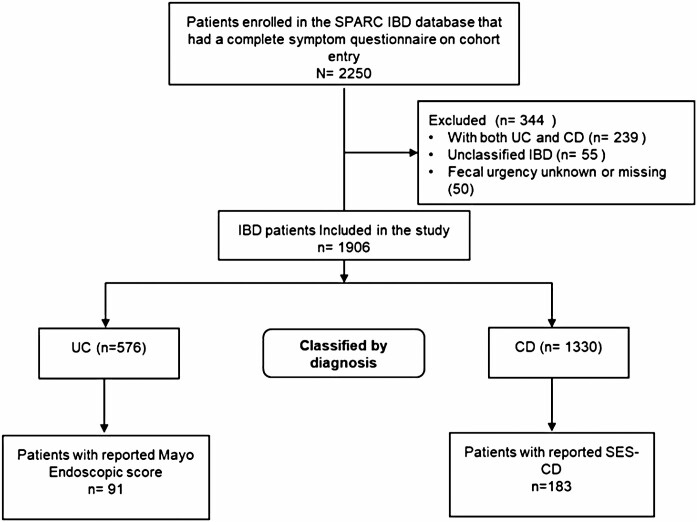
The study population consisted of 2250 patients enrolled in the SPARC IBD database between 2017 and 2019 who had a completed baseline symptom questionnaire and/or IBD Smartform with data on urgency symptoms at cohort entry (Figure 1). Patients with a diagnosis of both UC and CD (n = 239), IBD unclassified (n = 55), and those with unknown or missing fecal urgency status at their enrollment visit (n = 50) were excluded from this analysis. Thus, the remaining 1906 patients with CD or UC who completed the patient symptom questionnaire at enrollment into SPARC IBD and had a valid response to the fecal urgency question formed the analytic sample.
Figure 1.
Flow diagram of the study population. Abbreviations: CD, Crohn’s disease; IBD, inflammatory bowel disease; UC, ulcerative colitis.
Variables Definitions
Fecal urgency was assessed using the question, “Over the last week, how much urgency have you had before bowel movements?” The fecal urgency response scale options were none (I can wait 15 minutes or longer to have a bowel movement), mild (I need to get to the bathroom within 5-15 minutes), moderate (I need to get to the bathroom within 2-5 minutes), moderately severe (I need to get to the bathroom in less than 2 minutes), and too severe (Sometimes I am unable to make it to the bathroom in time). Because relatively few patients reported moderate, moderately severe, and severe urgency, these patients were combined into a “moderate-severe” fecal urgency group.
Factors potentially associated with fecal urgency that were explored for all IBD patients included age, sex, IBD disease duration, average bowel movements per day stool frequency relative to normal when the patient is well, presence of rectal bleeding, and severity of abdominal pain. Additional factors explored among only CD patients include whether disease involves the rectum and perianal disease status. Patient-reported general well-being is measured in SPARC IBD as generally well, slightly under par, poor, very poor, or terrible. Patients reporting slightly under par, poor, very poor, or terrible well-being were re-categorized as “not feeling well.” The definitions and source files for each of these variables are summarized in Supplementary Table S1.
Laboratory and Endoscopic Data
In a subset of the cohort who completed an office visit at enrollment and had biosample data available, we categorized fecal calprotectin concentration as < 50 μg/g, ≥ 50 μg/g but < 250 μg/g, and ≥ 250 μg/g. Missing calprotectin was generally due to the lack of receipt of a stool sample from the participant at the time of enrollment. Similarly, we examined the Simple Endoscopic Score for Crohn Disease (SES-CD) and Mayo Endoscopic Score for UC disease activity for a subset of the cohort who underwent colonoscopy or sigmoidoscopy after enrollment.10, 11 The SES-CD score is calculated based on an assessment of 5 segments of the bowel (rectum, descending colon, transverse colon, ascending colon, and ileum). The extent of ulceration, size of ulceration, the extent of inflammation, and stenosis are assessed within each bowel segment and assigned a severity score between 0 and 3, and the final score is calculated as the sum of the individual scores.10 The Mayo Endoscopic Score assesses the activity of UC by assigning a score between 0 and 3 to represent inactive, mild, moderate, or severe disease.
Statistical Analysis
Separately for UC and CD, we summarized patients’ demographics and clinical characteristics stratified by fecal urgency level (none, mild, and moderate-severe) as means and standard deviations for continuous variables and frequencies and proportions for categorical variables. We conducted all of the following analyses separately in UC and CD patients:
a) Prevalence of fecal urgency among UC and CD patients in SPARC IBD
We reported the total number and proportion of patients in SPARC IBD who reported fecal urgency including mild and moderate-severe urgency in both UC and CD patients.
b) Association between fecal urgency and IBD symptoms
Because fecal urgency was categorized as a 3-level variable, we used multinomial logistic regression models to identify IBD symptoms and characteristics associated with different levels of fecal urgency (none, mild, and moderate-severe) in UC and CD patients. Each model treated fecal urgency as the dependent variable and considered the following independent variables: demographic variables (age and gender) and IBD symptoms (average bowel movement per day, disease duration, stool frequency, bleeding frequency, and abdominal pain). Perianal disease status and rectal disease involvement were 2 additional factors considered for CD patients. We retained variables in the final model based on the forward variable selection using Akaike’s Information Criteria (AIC).
In a subset of the primary cohorts with complete fecal calprotectin level, we used multinomial logistic regression models to examine the association of fecal urgency (dependent variable) and fecal calprotectin (independent variable) while adjusting for age and gender in the models. We did not adjust these models for IBD symptoms as the bowel inflammation measured by calprotectin would likely be colinear with fecal urgency.
c) Association between well-being and fecal urgency
Logistic regression was used to assess the association between patient-reported well-being (not feeling well vs generally well) and fecal urgency in CD and UC. Models treated well-being as the dependent variable and included age, sex, average bowel movement per day, bleeding frequency, stool frequency, abdominal pain, and fecal urgency as independent variables.
Association between endoscopic assessment and fecal urgency
Due to the limited availability of endoscopy data with concurrent fecal urgency assessments, we conducted a separate analysis to test the association between endoscopic assessments and fecal urgency. A subset of the SPARC IBD cohort who reported fecal urgency scores within 60 days prior to their colonoscopy or sigmoidoscopy was examined. Kruskal-Wallis tests were used to compare the distribution of SES-CD scores across fecal urgency levels among CD patients and the distribution of Mayo endoscopic scores across fecal urgency levels among UC patients.
All statistical analyses were performed using SAS 9.4 (SAS Institute Inc.).
Ethical Considerations
This study was approved by the Institutional Review Board at the University of Pennsylvania.
Results
Patient Population
Prevalence and characteristics of fecal urgency in UC cohort
Of the 576 UC patients, 59.5% reported no fecal urgency, 31.4% reported mild fecal urgency, and 28.1% moderate-severe fecal urgency (Table 1). Compared with UC patients who reported no fecal urgency, UC patients with moderate-severe fecal urgency were older (mean age, 45 years vs 42 years) and more likely to report more than 4 stools above their normal per day (35% vs 3%), most or all liquid stool consistency (10% vs 1%), presence of bleeding (56% vs 16%), and moderate-severe abdominal pain (37% vs 2%).
Table 1.
Demographics and clinical characteristics of ulcerative colitis and Crohn’s disease patients who responded to fecal urgency question in SPARC IBD
| Ulcerative colitis (n = 576) | Crohn’s disease (n = 1330) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Urgency level | ||||||||||||
| None | Mild | Moderate-severe | None | Mild | Moderate-severe | |||||||
| n | 233 | 181 | 162 | 464 | 449 | 417 | ||||||
| Demographics | n (%) unless otherwise indicated | |||||||||||
| Age, mean (± SD) | 42.3 | (14.3) | 43.4 | (15.3) | 45.3 | (15.3) | 39.7 | (13.6) | 41.7 | (14.5) | 44.1 | (14.4) |
| Gender (male) | 136 | (58.4) | 82 | (45.6) | 79 | (48.5) | 249 | (53.9) | 191 | (42.4) | 140 | (33.5) |
| Average bowel movements per day | 2.5 | (1.9) | 2.9 | (2.1) | 5.2 | (4.3) | 2.5 | (2.0) | 3.1 | (2.1) | 5.8 | (3.7) |
| Disease duration, mean (± SD) | 12.4 | (8.9) | 14 | (11.5) | 12.6 | (11.4) | 14.7 | (10.3) | 15.9 | (9.7) | 16.4 | (10.2) |
| Perianal disease | — | — | — | — | — | — | 76 | (16.5) | 68 | (15.1) | 81 | (19.4) |
| Disease involving the rectum | — | — | — | — | — | — | 123 | (26.6) | 105 | (23.4) | 111 | (26.6) |
| Stool frequency | ||||||||||||
| Normal | 189 | (81.1) | 125 | (69.1) | 42 | (25.9) | 361 | (77.8) | 285 | (63.5) | 147 | (35.3) |
| 1-2 stools > normal | 24 | (10.3) | 28 | (15.5) | 34 | (21.0) | 74 | (15.9) | 102 | (22.7) | 95 | (22.8) |
| 3-4 stools > normal | 13 | (5.6) | 17 | (9.4) | 29 | (17.9) | 19 | (4.1) | 49 | (10.9) | 75 | (18.0) |
| >4 stools > normal | 6 | (2.6) | 11 | (6.1) | 56 | (34.6) | 9 | (1.9) | 13 | (2.9) | 99 | (23.7) |
| Bleeding frequency | ||||||||||||
| None | 195 | (83.7) | 145 | (80.1) | 71 | (43.8) | 415 | (89.4) | 373 | (83.1) | 296 | (71.0) |
| Visible blood less than half of the time | 28 | (12.0) | 24 | (13.3) | 48 | (29.6) | 39 | (8.4) | 60 | (13.4) | 88 | (21.1) |
| Visible blood half of the time or more | 7 | (3.0) | 11 | (6.1) | 32 | (19.8) | 9 | (1.9) | 16 | (3.6) | 27 | (6.5) |
| Passing blood alone | 1 | (0.4) | 1 | (0.6) | 10 | (6.2) | 1 | (0.2) | - | - | 5 | (1.2) |
| Abdominal pain | ||||||||||||
| None | 182 | (78.1) | 106 | (58.6) | 48 | (29.6) | 325 | (70.0) | 227 | (50.6) | 134 | (32.1) |
| Mild | 47 | (20.2) | 57 | (31.5) | 54 | (33.3) | 111 | (23.9) | 162 | (36.1) | 161 | (38.6) |
| Moderate-severe | 4 | (1.7) | 17 | (9.4) | 60 | (37.0) | 28 | (6.0) | 60 | (13.4) | 122 | (29.3) |
| Fecal calprotectin in a subset of the cohort, n | 87 | 70 | 54 | 139 | 167 | 131 | ||||||
| < 50 μg/g | 71 | (81.6) | 46 | (65.7) | 26 | (48.2) | 115 | (82.7) | 130 | (77.8) | 93 | (71.0) |
| ≥ 50 μg/g but < 250 μg/g | 7 | (8.1) | 16 | (22.9) | 18 | (33.3) | 17 | (12.2) | 25 | (15.0) | 26 | (19.9) |
| ≥ 250 μg/g | 9 | (10.3) | 8 | (11.4) | 10 | (18.5) | 7 | (5.0) | 12 | (7.2) | 12 | (9.2) |
| Endoscopic disease activity scores in a subset of the cohort, n | 48 | 57 | 70 | 22 | 21 | 29 | ||||||
| SES_CD, mean (± SD)a | 3.3 | 3.7 | 3.6 | 6.0 | 3.6 | 4.6 | — | — | — | — | — | — |
| SES-CD, rectum, mean (± SD)a | 0.6 | 1.4 | 0.8 | 2.2 | 0.6 | 1.4 | — | — | — | — | — | — |
| Mayo score among UC, mean (± SD)a | — | — | — | — | — | — | 1.2 | 1.3 | 1.1 | 1.3 | 1.5 | 1.2 |
Abbreviations: SES-CD, simple endoscopic score for Crohn disease; UC, ulcerative colitis. Percent missing for stool frequency (<1%), bleeding frequency (<1%), and pain (<1%).
a P-values for disease activity scores: SES-CD (0.89), SES-CD rectum score (0.86), and Mayo score (0.04); values were considered significant if they were ≤ 0.05.
Prevalence and characteristics of fecal urgency in CD cohort
Of the 1330 CD patients, 65% reported fecal urgency, 33.8% mild fecal urgency, and 31.4% moderate-severe fecal urgency (Table 1). Compared with CD patients without fecal urgency, CD patients who reported moderate-severe fecal urgency were older (mean age, 44 years vs 40 years) and more likely to report having > 4 stools per day greater than normal (24% vs 2%), most or all liquid stools (16% vs 6%), presence of bleeding (29% vs 11%), and moderate-severe abdominal pain (29% vs 6%).
Factors Associated With Fecal Urgency in UC Patients
The multinomial logistic regression fitted for UC patients demonstrated that increased average bowel movements per day (odds ratio [OR], 1.23; 95% confidence interval [CI]: 1.09, 1.23), presence of bleeding (OR, 3.36; 95% CI: 1.79, 6.34), any level of increased stool frequency relative to normal (OR for ≥ 4 stools per day, 9.95; 95% CI: 3.21, 30.87), and any abdominal pain (OR for moderate-severe abdominal pain, 17.50; 95% CI: 5.38, 65.89) are associated with a higher likelihood of moderate-severe fecal urgency compared with no fecal urgency. Similar but less strong associations were observed for stool frequency and abdominal pain with mild fecal urgency relative to no fecal urgency (Table 2). The analysis of the subset of patients with biosample data available showed that increased fecal calprotectin level is associated with a higher likelihood of mild or moderate-severe fecal urgency compared with no urgency (OR for fecal calprotectin ≥ 250 μg/g, mild urgency 1.53; 95% CI: 0.54, 4.37; OR for moderate-severe urgency 4.36; 95% CI: 1.50, 12.66) (Table 3).
Table 2.
Factors associated with fecal urgency among patients with ulcerative colitis and Crohn’s disease in SPARC IBDa
| Ulcerative colitis | Crohn’s disease | |||
|---|---|---|---|---|
| Mild | Moderate-severe | Mild | Moderate-severe | |
| Odds ratio (95% confidence interval) | Odds ratio (95% confidence interval) | |||
| Age | 1.01 (1.00, 1.02) | 1.03 (1.01, 1.05) | 1.01 (1.00, 1.02) | 1.03 (1.01, 1.03) |
| Female | 1.76 (1.14, 2.70) | 1.38 (0.78, 2.42) | 1.41 (1.06, 1.88) | 2.05 (1.45, 2.87) |
| Average bowel movements per day | 1.10 (0.98, 1.23) | 1.23 (1.09, 1.23) | 1.11 (1.03, 1.20) | 1.23 (1.14, 1.34) |
| Presence of bleeding | 1.02 (0.57, 1.85) | 3.36 (1.79, 6.34) | 1.34 (0.88, 2.03) | 1.77 (1.13, 2.78) |
| Stool frequency | ||||
| 1-2 stools > normal | 1.27 (0.66, 2.43) | 4.04 (1.96, 8.32) | 1.54 (1.07, 2.23) | 2.31 (1.53, 3.49) |
| 3-4 stools > normal | 2.05 (0.88, 4.75) | 6.14 (2.51, 15.06) | 2.42 (1.32, 4.42) | 5.01 (2.71, 9.27) |
| >4 stools > normal | 1.97 (0.60, 6.46) | 9.95 (3.21, 30.87) | 0.99 (0.38, 2.61) | 7.57(3.30, 17.34) |
| Abdominal pain | ||||
| Mild | 1.89 (1.16, 3.08) | 2.98 (1.61, 5.54) | 1.85 (1.34, 2.56) | 2.27 (1.56, 3.32) |
| Moderate-severe | 5.11 (1.60, 16.35) | 17.50 (5.38, 56.89) | 3.09 (1.78, 5.37) | 7.52 (4.31, 13.14) |
Abbreviation: SPARC IBD, Study of a Prospective Adult Research Cohort with IBD. Reference categories: fecal urgency (none), sex (male), stool frequency (normal), bleeding frequency (none), and abdominal pain (none).
aBased on the forward variable selection using Akaike’s Information Criteria.
Table 3.
Association of fecal urgency with calprotectin level among patients with ulcerative colitis and Crohn’s disease
| Ulcerative colitisa (n = 211) | Crohn’s diseasea (n = 437) | |||
|---|---|---|---|---|
| Mild | Moderate-severe | Mild | Moderate-severe | |
| Odds ratio (95% confidence interval) | Odds ratio (95% confidence interval) | |||
| Fecal calprotectin | ||||
| ≥ 50 μg/g but < 250 μg/g | 3.80 (1.43, 10.12) | 8.84 (3.18, 24.66) | 1.32 (0.68, 2.59) | 1.90 (0.96, 3.78) |
| ≥ 250 μg/g | 1.53 (0.54, 4.37) | 4.36 (1.50, 12.66) | 1.59 (0.60, 4.20) | 2.33 (0.87, 6.28) |
Reference category: fecal calprotectin (<50 μg/g).
aBoth models were adjusted for age and sex.
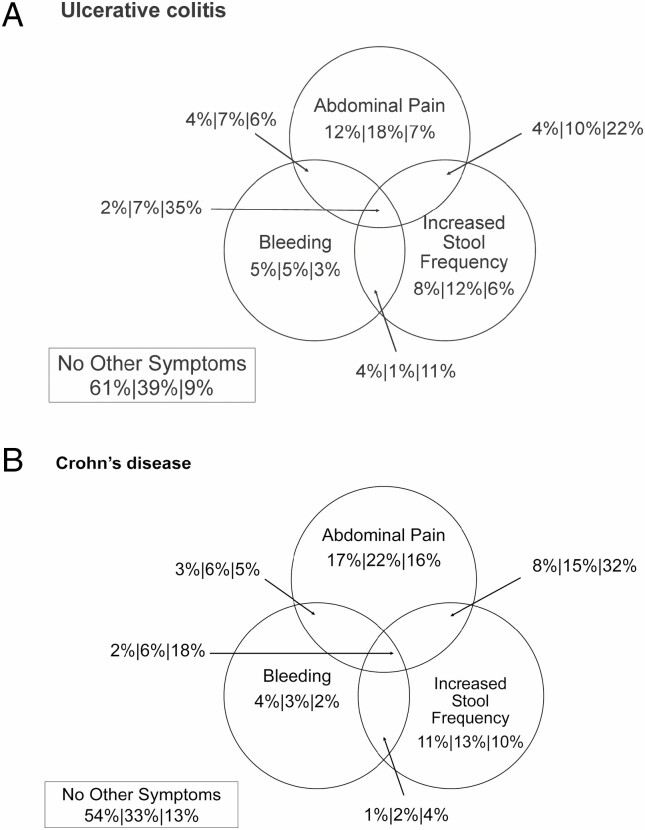
Despite these associations between fecal urgency and IBD symptoms, many patients were observed to experience fecal urgency independent of the symptoms examined. Approximately, 39% of UC patients with mild fecal urgency and 9% of patients with moderate-severe fecal urgency reported normal bowel frequency, no bleeding, and no abdominal pain. Similarly, 18% of patients with mild fecal urgency and 7% of patients with moderate-severe fecal urgency reported abdominal pain as their only symptom (Figure 2, Panel A). Fecal calprotectin was available for 39 UC patients with fecal urgency but no additional symptoms. Among these patients, 26 had fecal calprotectin <50 μg/g (67%), 7 had 50-249 μg/g (18%), and 6 had ≥250 μg/g (15%).
Figure 2.
Percentage of UC patients (Panel A) and CD patients (Panel B), with no, mild, and moderate-severe fecal urgency experiencing the given combination of symptoms.
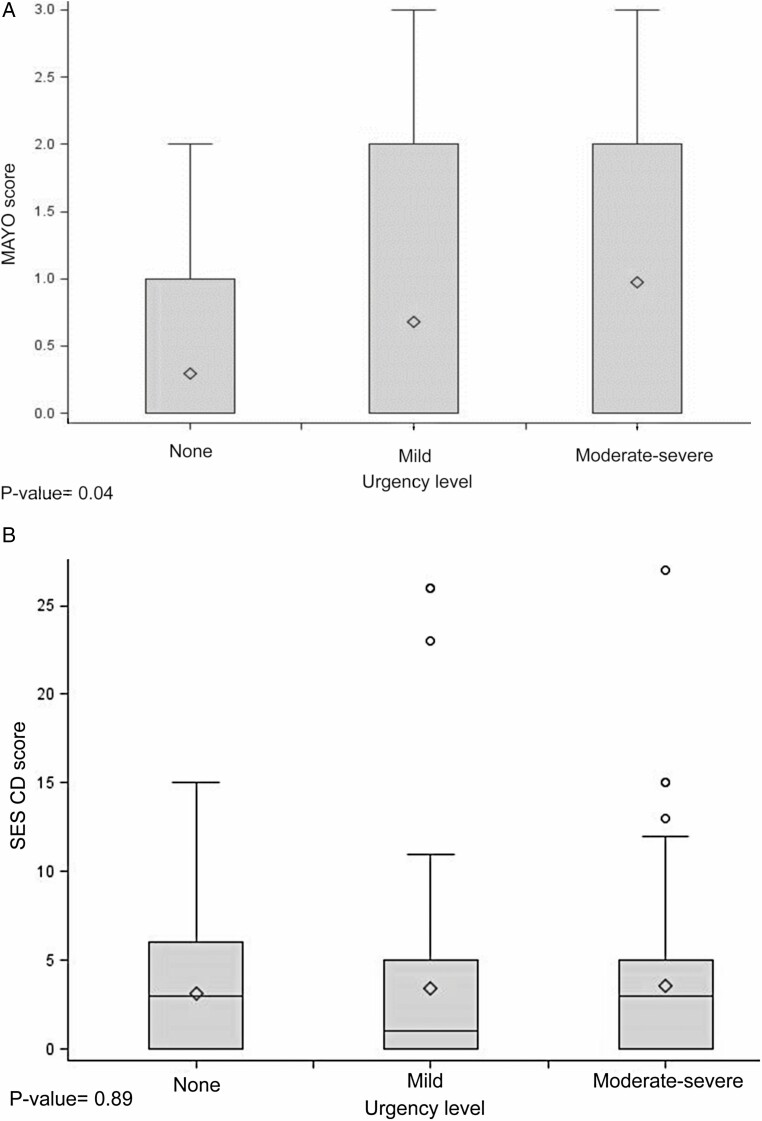
The endoscopic assessment was reported in 91 UC patients. We found that a higher Mayo endoscopic score was significantly associated with higher levels of mild or moderate-severe fecal urgency among patients with UC (P = .04) (Table 1 and Figure 3, Panel A). Among UC patients with fecal urgency with normal stool frequency, no bleeding, and no abdominal pain, the mean endoscopic Mayo score was 0.5 (± 0.9).
Figure 3.
Association of fecal urgency with MAYO score among patients with UC and SES-CD score among patients with Crohn’s disease. (A) MAYO score among UC patients and (B) SES-CD among CD patients. *P-value based on the results from Kruskal-Wallis test. The lower and upper edges of the box are located at the 25th and 75th percentile, respectively; the diamond shape (♢) marks the mean; the circle shape (○) marks extreme values; the whiskers extend as the minimum and maximum values which are within 1.5 times the interquartile range. Abbreviations: SES-CD, simple endoscopic score for Crohn disease; UC, ulcerative colitis.
Factors Associated With Fecal Urgency in CD Patients
The multinomial logistic regression fitted for CD patients demonstrated that increased average bowel movements per day (OR, 1.23; 95% CI: 1.14, 1.34), presence of bleeding (OR, 1.77; 95% CI: 1.13, 2.87), increased stool frequency relative to normal (OR for ≥ 4 stools per day, 7.57; 95% CI: 3.30, 17.34), and abdominal pain (OR for moderate-severe abdominal pain, 7.52; 95% CI: 4.31, 13.14) are associated with a higher likelihood of moderate-severe fecal urgency compared with no fecal urgency. Similar but less strong associations were observed for stool frequency and abdominal pain with mild fecal urgency relative to no fecal urgency (Table 2). Fecal calprotectin concentration was not seen to be predictive of mild or moderate to severe urgency in CD. Approximately, 33% of CD patients with mild fecal urgency and 13% of patients with moderate-severe fecal urgency reported normal bowel frequency, no bleeding, and no abdominal pain. Similarly, 22% of patients with mild fecal urgency and 16% of patients with moderate-severe fecal urgency reported abdominal pain as their only symptom (Figure 2, Panel B). Fecal calprotectin was available in 78 patients with fecal urgency but no other symptoms. Among these patients, 54 (69%) had fecal calprotectin <50 μg/g, 16 (21%) had 50-249 μg/g, and 8 (10%) had ≥250 μg/g.
Among CD patients, the endoscopic assessment was reported in 183 patients. The distribution of total SES-CD (P = .89) and SES-CD rectal subscore (P = .86) was not significantly different across fecal urgency levels among patients with CD (Table 1 and Figure 3, Panel B). The mean total SES-CD score and SES-CD rectum subscore among patients with fecal urgency but with normal stool frequency, no bleeding, and no abdominal pain were 2.7 (± 3.5) and 0.5 (± 1.1), respectively.
Association of well-being and fecal urgency in UC and CD patients
After adjusting for age and IBD symptoms, the presence of fecal urgency in UC patients was significantly associated with feeling not-well (OR for mild fecal urgency 2.33, 95% CI: 1.10, 4.96; OR for moderate-severe fecal urgency 4.20, 95% CI: 1.69, 10.40) (Table 4). Similarly, after adjusting for age and IBD symptoms, the presence of fecal urgency in CD patients was significantly associated with feeling not-well (OR for mild fecal urgency 1.55, 95% CI: 0.96, 2.50; OR for moderate-severe fecal urgency 2.52, 95% CI: 1.51, 3.92) (Table 4).
Table 4.
Association between well-being and fecal urgency among ulcerative colitis and Crohn’s disease patients
| Ulcerative colitis | Crohn’s disease | |
|---|---|---|
| Variable | Odds ratio (95% confidence interval) | |
| Urgency level | ||
| Mild | 2.33 (1.10, 4.96) | 1.55 (0.96, 2.50) |
| Moderate-severe | 4.20 (1.69, 10.40) | 2.52 (1.51, 4.22) |
| Age | 1.01 (0.99, 1.04) | 1.01 (1.00, 1.03) |
| Female | 1.00 (0.53, 1.90) | 0.78 (0.52, 1.18) |
| Average bowel movements per day | 1.05 (0.93, 1.20) | 1.10 (1.01, 1.21) |
| Presence of bleeding | 1.54 (0.72, 3.33) | 2.35 (1.41, 3.92) |
| Stool frequency | ||
| 1-2 stools > normal | 4.18 (1.78, 9.79) | 2.54 (1.59, 4.06) |
| 3-4 stools > normal | 4.33 (1.48, 12.66) | 2.46 (1.35, 4.50) |
| >4 stools > normal | 3.08 (0.79, 12.00) | 3.40 (1.39, 8.36) |
| Abdominal pain | ||
| Mild | 3.19 (1.57, 6.46) | 3.28 (2.12, 5.09) |
| Moderate-severe | 3.87 (1.12, 13.41) | 9.47 (5.27, 16.99) |
Reference categories: well-being (generally well), sex (male), stool frequency (normal), bleeding frequency (none), and abdominal pain (none).
Discussion
In this cross-sectional analysis of patients enrolled in SPARC IBD, we found that fecal urgency is common among IBD patients. Six in 10 patients reported fecal urgency of any degree with 3 out of 10 having moderate-severe urgency. These results were consistent between UC and CD patients. Fecal urgency was associated with increased stool frequency relative to normal, presence of bleeding, average bowel movement per day, and abdominal pain in both UC and CD patients. Moderate-severe fecal urgency was generally more strongly associated with the other symptoms and inflammatory markers than mild fecal urgency. Further, we found that fecal urgency was associated with reduced well-being in patients with UC and CD, again with stronger associations with moderate-severe fecal urgency. This is consistent with prior studies suggesting a higher level of anxiety and depression among those affected by fecal urgency.7–9
Despite advancements in treatment and management of IBD, a substantial number of patients experience fecal urgency. The proportion of patients reporting fecal urgency in this study (60%) is significantly higher than that reported in the general population (3%).8 A few other studies have also observed a high prevalence of fecal urgency in patients with IBD. In one study of UC, a prevalence of fecal urgency up to 85% was reported.12 Another analysis that evaluated the stool patterns and symptoms of 72 IBD patients who were hospitalized found that 67% of those with CD and 84% of those with UC reported fecal urgency.5
Data on characteristics of patients with fecal urgency in IBD are scarce. In the current study, we found that abdominal pain, presence of rectal bleeding, high stool frequency, and higher average bowel movements per day were associated with fecal urgency. These symptoms and signs are generally consistent with active IBD. However, some patients have persistent symptoms despite resolution of inflammation as assessed by fecal calprotectin and lower endoscopy. Abdominal pain was strongly associated with fecal urgency. Those with moderate-severe abdominal pain had more than 8–18-fold higher odds of reporting moderate-severe urgency. Abdominal pain is very common in IBD, particularly CD.13Although clinicians routinely examine changes in stool frequency or consistency when evaluating fecal urgency, abdominal pain may be overlooked.13 To our knowledge, an association between the severity of fecal urgency and abdominal pain has not previously been assessed. The magnitude of association in the current study suggests that incorporating abdominal pain severity in the routine evaluation of IBD patients with fecal urgency is warranted. However, treating abdominal pain with analgesics, including opioids, may not be the optimal treatment choice in this population as narcotic use among patients with IBD has been associated with adverse outcomes.14 Rather, a search for the underlying etiology of the abdominal pain, particularly ongoing inflammation, appears indicated.
Fecal calprotectin is a simple and inexpensive test that correlates with histologic and endoscopic disease activity.15 Although fecal calprotectin has been shown to be a useful tool in the diagnosis, monitoring, and prediction of relapse in IBD patients, to our knowledge, evidence on the association of fecal urgency and fecal calprotectin level has not been previously reported. We also confirmed the hypothesized association between endoscopic disease activity severity and fecal urgency in UC. While SES-CD was not associated with fecal urgency among CD patients in this study, this finding is not surprising as the correlation of endoscopy findings and symptoms in CD has previously been documented to be weak.16 We hypothesized that the rectal subscore of SES-CD may be more strongly associated with fecal urgency but that was not apparent in this population. Nonetheless, findings of positive correlations of fecal urgency with calprotectin, Mayo endoscopic score, and symptoms common in active IBD suggest that evaluating for inflammation should be the first step of evaluating patients who complain of fecal urgency. Interestingly, a large proportion of patients without other symptoms reported fecal urgency. Among these, the fecal calprotectin data demonstrated that 10%–15% of those patients had fecal calprotectin levels ≥250 μg/g. This suggests the potential for otherwise subclinical inflammation in a subset. Whether resolution of that inflammation would resolve the fecal urgency needs to be assessed in future studies.
Although this study was not able to fully explore the reasons for fecal urgency in those without other symptoms and normal concentration of fecal calprotectin, there are several potential causes. A proportion of those patients may have undiagnosed irritable bowel syndrome (IBS) in addition to IBD and may benefit from therapies used to treat IBS. Other patients may have developed a reflexive sense of urgency resulting from previously having long periods with inflammation that was causing fecal urgency. These patients might benefit from biofeedback or other similar approaches. Finally, some patients may have scarring from prior inflammation that leads to reduced rectal compliance. We hypothesized that were this true, duration since diagnosis with IBD would be associated with fecal urgency, but we did not observe such an association in this study. Future research should explore these hypotheses given the impact of fecal urgency on quality of life.
Our study has several limitations. First, due to the cross-sectional nature of the data, we were not able to establish temporality in the association between fecal urgency and risk factors. Second, the population under study is largely derived from tertiary care academic centers and may limit the generalizability of the results to the broader IBD population. Nonetheless, the SPARC IBD population has advantages over clinical trial populations as the cohort includes a range of disease activity and patients were not selected for enrollment based on disease severity or urgency level. Third, the fecal urgency score developed in the current study was not previously validated, although the score showed a good correlation with symptom severity and general well-being. Fourth, the study may have been underpowered to assess the association of fecal urgency with SES-CD. Although not available in all patients, the fecal samples for calprotectin were collected as part of the research protocol rather than as part of clinical care. As such, there is less likelihood of bias due to collection predominantly in patients reporting symptoms. The symptoms reported in the current study are subject to misclassification. If this is non-differential, we may have underestimated the magnitude of the associations. This should not affect objective measurements, such as calprotectin or endoscopic score measurements. Given that these more objective makers produced similar findings to that of symptoms, it is less likely that differential misclassification bias produced spurious associations. Finally, fecal calprotectin and endoscopic activity data were only available for a subset of patients, and associations with fecal urgency may not extrapolate to the entire IBD population. Further research may be necessary to verify these initial findings.
Conclusions
To conclude, we have demonstrated that fecal urgency is common in IBD patients enrolled in SPARC IBD and is associated with reduced well-being. Fecal urgency was associated with other signs and symptoms that characterize active IBD, including elevated fecal calprotectin, Mayo endoscopic score, abdominal pain, rectal bleeding, average bowel movement per day, and stool frequency. However, a subset of patients with fecal urgency had no other symptoms, and many had normal fecal calprotectin, suggesting alternative etiologies and the need for different management approaches.
Supplementary Material
Contributor Information
Ghadeer K Dawwas, Center for Clinical Epidemiology and Biostatistics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, USA; Center for Pharmacoepidemiology Research and Training, Department of Biostatistics, Epidemiology, and Informatics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, USA; Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
Hamzeh Jajeh, Ohio State University, Lima, Ohio.
Mingyang Shan, Eli Lilly and Company, Indianapolis, Indiana, USA.
April N Naegeli, Eli Lilly and Company, Indianapolis, Indiana, USA.
Theresa Hunter, Eli Lilly and Company, Indianapolis, Indiana, USA.
James D Lewis, Center for Clinical Epidemiology and Biostatistics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, USA; Center for Pharmacoepidemiology Research and Training, Department of Biostatistics, Epidemiology, and Informatics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, USA; Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia, Pennsylvania, USA; Division of Gastroenterology and Hepatology, Perelman School of Medicine, University of Pennsylvania , Philadelphia, Pennsylvania, USA.
Funding
This work was funded by R25-DK108711 and P30-DK050306.
Conflicts of Interest
M.S., A.N.N., and T.H. are full-time employees of Eli Lilly and Company.
Data Availability
People interested in accessing SPARC IBD data for research should contact the Crohn’s & Colitis Foundation.
References
- 1. Longobardi T, Jacobs P, Bernstein CN. Utilization of health care resources by individuals with inflammatory bowel disease in the united states: a profile of time since diagnosis. Am J Gastroenterol. 2004;99(4):650–655. doi: 10.1111/j.1572-0241.2004.04132.x [DOI] [PubMed] [Google Scholar]
- 2. Panaccione R. Mechanisms of inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2013;9(8):529–532. [PMC free article] [PubMed] [Google Scholar]
- 3. Walter S, Hjortswang H, Holmgren K, Hallbook O. Association between bowel symptoms, symptom severity, and quality of life in Swedish patients with fecal incontinence. Scand J Gastroenterol. 2011;46(1):6–12. doi: 10.3109/00365521.2010.513059 [DOI] [PubMed] [Google Scholar]
- 4. Dibley L, Bager P, Czuber-Dochan W, et al. Identification of research priorities for inflammatory bowel disease nursing in Europe: a nurses-European Crohn’s and Colitis Organisation Delphi Survey. J Crohns Colitis. 2017;11(3):353–359. doi: 10.1093/ecco-jcc/jjw164 [DOI] [PubMed] [Google Scholar]
- 5. Petryszyn PW, Paradowski L. Stool patterns and symptoms of disordered anorectal function in patients with inflammatory bowel diseases. Adv Clin Exp Med. 2018;27(6):813–818. doi: 10.17219/acem/68986 [DOI] [PubMed] [Google Scholar]
- 6. Nobrega VG, Silva INN, Brito BS, Silva J, Silva MCMD, Santana GO. The onset of clinical manifestations in inflammatory bowel disease patients. Arq Gastroenterol. 2018;55(3):290–295. doi: 10.1590/s0004-2803.201800000-73 [DOI] [PubMed] [Google Scholar]
- 7. Singh P, Takazawa E, Rangan V, et al. Fecal urgency is common in constipated patients and is associated with anxiety. Neurogastroenterol Motil. 2019;31(4):e13545. doi: 10.1111/nmo.13545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rangan V, Mitsuhashi S, Singh P, et al. Risk factors for fecal urgency among individuals with and without diarrhea, based on data from the National Health and Nutrition Examination Survey. Clin Gastroenterol Hepatol. 2018;16(9):1450–1458.e2. doi: 10.1016/j.cgh.2018.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Drossman DA, Sandler RS, Broom CM, McKee DC. Urgency and fecal soiling in people with bowel dysfunction. Dig Dis Sci. 1986;31(11):1221–1225. doi: 10.1007/BF01296523 [DOI] [PubMed] [Google Scholar]
- 10. Sipponen T, Nuutinen H, Turunen U, Farkkila M. Endoscopic evaluation of Crohn’s disease activity: comparison of the CDEIS and the SES-CD. Inflamm Bowel Dis. 2010;16(12):2131–2136. doi: 10.1002/ibd.21300 [DOI] [PubMed] [Google Scholar]
- 11. D′Haens G, Sandborn WJ, Feagan BG, et al. A review of activity indices and efficacy end points for clinical trials of medical therapy in adults with ulcerative colitis. Gastroenterology. 2007;132(2):763–786. doi: 10.1053/j.gastro.2006.12.038 [DOI] [PubMed] [Google Scholar]
- 12. Rao SS, Holdsworth CD, Read NW. Symptoms and stool patterns in patients with ulcerative colitis. Gut. 1988;29(3):342–345. doi: 10.1136/gut.29.3.342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zeitz J, Ak M, Muller-Mottet S, et al. Pain in IBD patients: very frequent and frequently insufficiently taken into account. PLoS One. 2016;11(6):e0156666. doi: 10.1371/journal.pone.0156666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lichtenstein GR, Feagan BG, Cohen RD, et al. Serious infection and mortality in patients with Crohn’s disease: more than 5 years of follow-up in the TREAT registry. Am J Gastroenterol. 2012;107(9):1409–1422. doi: 10.1038/ajg.2012.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alibrahim B, Aljasser MI, Salh B. Fecal calprotectin use in inflammatory bowel disease and beyond: a mini-review. Can J Gastroenterol Hepatol. 2015;29(3):157–163. doi: 10.1155/2015/950286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lewis JD, Rutgeerts P, Feagan BG, et al. Correlation of stool frequency and abdominal pain measures with simple endoscopic score for Crohn’s disease. Inflamm Bowel Dis. 2020;26(2):304–313. doi: 10.1093/ibd/izz241 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
People interested in accessing SPARC IBD data for research should contact the Crohn’s & Colitis Foundation.