Abstract
Background
During the COVID-19 pandemic Chinese international students were reported to experience racism, food security issues and social isolation. However, no study has investigated the prevalence of these issues and the potential for worsening mental health in this population group during the pandemic. Therefore, this study aimed to examine the effect of this pandemic on the mental health of Chinese international students living in Australia and China, and the protective effect of social support.
Methods
Data were extracted from a survey of Australian university students (April–June 2019) and follow-up during the pandemic (Sept-Oct 2020). The prevalence of anxiety, major depression and pandemic-related stressors was reported. Multivariable logistic regression was used to assess the association between country of residence, social support (baseline/follow-up), and follow-up self-reported mental health.
Results
With the pandemic, there was a substantial increase in the prevalence of anxiety (24.7 % vs 45.7 %) and major depression (22.1 % vs 43.8 %). Major depression was less likely to be reported by international students in China (34.8 %) than in Australia (46.3 %). Students with high social support during the pandemic were less likely to report major depression (Adjusted OR:0.15 [95 % CI 0.06,0.34]), although this effect was not observed longitudinally (Adjusted OR:1.03 [95 % CI 0.58,1.83]).
Limitation
Post pandemic improvement in mental health cannot be assessed.
Conclusion
The pandemic appeared to have had a strong negative effect on Chinese international university students' mental health. Those living in Australia were more likely to experience poorer mental health, highlighting the need for increased support to this group.
Keywords: Depression, Anxiety, COVID-19 related stress, Social support, Chinese international student
1. Introduction
The widely and rapidly spreading Coronavirus Disease 2019 (COVID-19) has become a global public health issue and the effect on mental health in many countries has been widely reported (Batra et al., 2021; Wu et al., 2021; Xiong et al., 2020). In Australia, the setting of this study, an increase in the use of mental health services during the pandemic has been observed, with a 21.8 % increase in mental health related prescriptions between January 1st and September 19th, 2021 over 2019 levels (Australian Institute of Health and Welfare, 2021). Internationally, university students are a population that has experienced multiple stressors during the pandemic; studies conducted during previous epidemics have found that individuals experiencing multiple epidemic related stressors were more likely to suffer from mental health problems than those experiencing fewer stressors (Liu et al., 2012; Main et al., 2011).
The specific stressors faced by university students during the pandemic have included university closures and transition to online-only study (Batra et al., 2021; Copeland et al., 2021; Salimi et al., 2021), loss of peer interaction, and increased level of loneliness (Hamza et al., 2020; Sahu, 2020; Son et al., 2020). A meta-analysis of 27 studies covering 90,879 university students from 15 different countries, assessed the prevalence of psychological issues in this population during the COVID-19 pandemic (Batra et al., 2021). The study found that 31.2 % of students experienced depression and 39.4 % of students reported anxiety during the pandemic (Batra et al., 2021), although no pre-pandemic comparison was made in this study. Studies that have compared to pre-pandemic mental health levels have found an increase in prevalence with the pandemic although estimates vary dramatically (Meda et al., 2021; Toth et al., 2021).
One group that has faced additional stressors in Australia is Chinese international students (Zhai and Du, 2020). The Australian Federal Government imposed border restrictions on any travellers who had left or transited through mainland China in late January 2020 (ABC News, 2020), precluding many from entry into the country. This led to considerable disruption for thousands of Chinese international students coming to Australia for their study. The potential impacts on these students included, substantially reduced connection with their university and peers, and heightened financial stress due to ongoing payment of tuition fees without the immersive educational experience (Xiao, 2021). At the same time, some students from China were unable to leave Australia and return home to family (Chen et al., 2020; Sahu, 2020). Loss of casual employment for this group also resulted in food insecurity and housing issues (Alan et al., 2020; Fronek et al., 2021) and as temporary residents, they were not eligible for government relief packages (Bolton, 2020). Additionally, racial discrimination towards Chinese nationals during the pandemic has been recognized as a stressor for some Chinese international students living abroad (Xia and Duan, 2020) at a time when xenophobia and sinophobia have been reported as increasing (Litam, 2020). Hence, Chinese international students living in Australia and in China may have experienced a unique set of stressors than other international students. It is yet to be explored whether one group was more impacted than the other in terms of mental health.
The combination of stressors related to COVID-19, along with pre-existing challenges, have placed Chinese international students in a more vulnerable position with possible impacts on mental health (Chen et al., 2020; Zhai and Du, 2020). However, to the best of our knowledge, there are no published quantitative studies focusing on the mental health of Chinese international students in Australia during the COVID-19 pandemic.
1.1. Social support as a buffer
Social support has been found to play a key role in helping individuals coping with distress and may mitigate the risks to mental health (Gariépy et al., 2016; Hefner and Eisenberg, 2009). Several studies have demonstrated the protective effect of social support on mental health when facing challenging environments (Li et al., 2020; Qi et al., 2020; Ye et al., 2020). A study of 7143 college students living in China during the pandemic found that those with high levels of social support were less likely to experience anxiety during the COVID-19 pandemic, compared to those with lower levels of social support (Cao et al., 2020). While this study sheds light on the relationship between social support and mental health among Chinese university students, it was conducted with students living and studying in their country of origin and was therefore unable to examine several of the stressors mentioned above that may be unique to Chinese students studying in Australia. Furthermore, as the study was cross-sectional, changes in mental health over time and the effects of longer-term social support could not be observed.
To address the above limitations, the aims of this current study were to: (1) examine changes in mental health among Chinese international students studying in Australia from before to during the pandemic; and (2) compare prevalence of anxiety, major depression, and COVID-19 related stressors during the COVID-19 pandemic between Chinese international students living in Australia and those living in China/internationally. The results of this study may provide information about the potential longer-term impacts of the COVID-19 pandemic on Chinese international students' mental health as well as the usefulness of building social support to buffer the impacts of high stress situations.
2. Method
2.1. Study setting and sample
The present study examined two waves of data collected through the “Towards a Health Promoting University” study (Sanci et al., 2022), which was based at a single tertiary educational institute in Melbourne, Australia. The baseline survey (Wave 1) was conducted between 2 April to 3 June 2019. All students who were enrolled at the institution in March/April 2019, and who were over 18 years old were invited to participate in this survey (Sanci et al., 2022). Students enrolled in non-award courses, cross-institutional or exchange programs, and whose status was ‘not admitted’ were excluded. In order to investigate the impact of the COVID-19 pandemic on university student mental health and wellbeing, a follow-up survey was conducted from 22 September to 20 October in 2020 (Wave 2) when Melbourne was in the midst of a second strict lockdown due to the global pandemic, which lasted for 112 days. Students who were still enrolled at the same institution in September 2020 and who had completed at least one section of the Wave 1 survey were eligible for the study and were invited via an e-mail to complete the Wave 2 survey. In total, 56,375 students were invited to participate in the Wave 1 survey, and 14,880 (26.4 %) students completed at least one section. After excluding 5869 students who had already left the institution by 2020, 9011 eligible students were invited to the Wave 2 survey, and 4297 (47.7 %) students completed it. The present study was approved by the University of Melbourne Medicine and Dentistry Human Ethics Sub-Committee (Ethics ID: 2057722).
For the present study, only data from Chinese international students who continued at the university across 2019 and 2020 were examined. Students who indicated their residential status as ‘international student’, country of birth as ‘mainland China’ and fee payment type as ‘overseas full fee and scholarship’ were defined as being Chinese international students.
2.2. Measures
2.2.1. Demographics
Information on participant age, gender (male/female/self-described), course level (undergraduate/masters/other postgraduate/graduate research) and financial difficulties (Yes/No) was collected at Wave 1. Financial difficulties were assessed in the Wave 1 survey by two questions ‘In the last 12 months, were there any times that you ran out of food and could not afford to buy more’ and ‘In the last 12 months, were there any times you could not afford to buy medicine’. Students who answered ‘yes’ to either question were identified as having financial difficulties.
2.2.2. Country of residence
Students were asked about their country of residence in the Wave 2 survey. For the purposes of this study, students from China were divided into those currently living in Australia and those currently living internationally (either in China or another country) during the study period. Students currently living internationally were classified with those currently living in China as it was assumed that both groups may have returned to their family of origin (primary support location).
2.2.3. Major depression
Depressive symptoms experienced over the previous two weeks were assessed in both the Wave 1 and Wave 2 surveys, using the short version of the Patient Health Questionnaire (PHQ-2) (Kroenke et al., 2003). This measure comprises two items (loss of interest; feeling depressed) assessed on a four-point scale ranging from 0 (not at all) to 3 (nearly every day). A depression scale score is calculated as the sum of the items. Validation of the PHQ-2 has been investigated in a large sample of Australian general practice patients, where a score of three or greater was found to have 91 % sensitivity and 78 % specificity for detecting probable major depressive disorder (Carey et al., 2016). In the present study we adopted this approach and used a scale score of three or more as a cut-off for probable major depression.
2.2.4. Anxiety
Anxiety symptoms over the previous two weeks were assessed in both Wave 1 and 2 surveys, using the two-item Generalized Anxiety Disorder Questionnaire (GAD-2) (Kroenke et al., 2007). Each item (feeling anxious; unable to stop worrying) was rated on a scale of 0 (not at all) to 3 (nearly every day), with scale scores ranging from 0 to 6. In this study, we used a score of three or more as a cut off to identify probable anxiety (Plummer et al., 2016). Validation of the GAD-2 has been investigated in a systematic review, where a score of three or greater was found to have 76 % sensitivity and 81 % specificity for identifying probable generalized anxiety disorder (Plummer et al., 2016).
2.2.5. Social support
Social support was measured in both Wave 1 and Wave 2 surveys using the 6-item Medical Outcomes Study Social Support Survey (MOS-SSS-6). The MOS-SSS-6 includes four subscales: tangible support, affectionate support, positive social interaction and emotional/informational support. Each item has a 5-point response, ranging from 1 (none of the time) to 5 (all of the time). This scale has high internal consistency with Cronbach's alpha 0.70 and scale reliability 0.89 (Holden et al., 2014). Continuous results are presented and to aid interpretation results are also presented with the score categorised into low social support (score ≤ 15), medium (score of 16 to 23), and high social support (score ≥ 24). These categorizations were developed in a study with a Chinese population (Ni et al., 2020).
2.2.6. Pandemic-related stressors
Pandemic-related stressors were measured in the Wave 2 survey using a set of 10 questions devised by the research team that asked participants to nominate whether various areas of life had changed during the COVID-19 pandemic. The following areas were included: homesickness, coping with study, confidence in future job prospects, racial discrimination, connection to university peers, connection with friends, relationship with family, financial positions, access to paid work, and finding suitable accommodation/living arrangements. These areas were chosen based on the issues raised in previous surveys and qualitative reports of student experiences during the COVID-19 pandemic. Participants were presented with six response options (Much worse than before, Somewhat worse than before, Unchanged, Somewhat better than before, Much better than before, Not applicable). For analyses, these six options were combined into three categories (Worse than before/Unchanged/Better than before) to aid interpretation.
2.3. Statistical analyses
Descriptive statistical analysis was conducted to illustrate the demographic characteristics of the sample at each assessment stage. Prevalence and 95 % confidence intervals (95 % CIs) were calculated for each categorical variable (i) anxiety, (ii) major depression, and (iii) pandemic-related stressors at each assessment stage, and separately for Chinese international students (i) currently residing in China and other countries, and (ii) those currently residing in Australia. Multivariable logistic regression analyses were conducted to assess the association between social support (Wave 1/Wave 2) and mental health status (Wave 2); with adjustment for potential confounders (including age, gender, financial difficulties, Wave 1 major depression/anxiety, Wave 1 social support, country of residence, and current living status). In the analysis of the association between country of residence (Wave 2) and mental health status (Wave 2) adjustments for age, gender and Wave 1 mental health status were made. Confounding factors were identified based on previous literature and direct acyclic graphs were generated (Supplementary Figs. 1 & 2).
In a sensitivity analysis, to investigate the effect of loss to follow up in the Wave 2 survey, inverse probability weighting (IPW) was used to calculate the weighted prevalence and weighted measures of effect of social support on mental health. The weighted prevalence was used to reflect the distribution of mental health outcomes and pandemic-related stressors for the possible participants (who have been invited to the Wave 2 survey) rather than only those who completed the Wave 2 survey. To calculate the reweighted prevalence, a missingness model was developed. In this logistic regression model the baseline self-reported level of support received from university (A lot/Not at all), experience of ethnic discrimination (Yes/No), feeling stress to succeed (Yes/No), and perceived self-confidence (Yes/No) were identified as predictors of missingness. A Hosmer and Lemeshow's goodness-of-fit test was utilised to assess the model fit. From the model, we calculated the propensity for each participant to be to participate. The sample was then reweighted using the inverse of the propensity score.
All analyses were conducted using STATA16.
3. Results
3.1. Participants
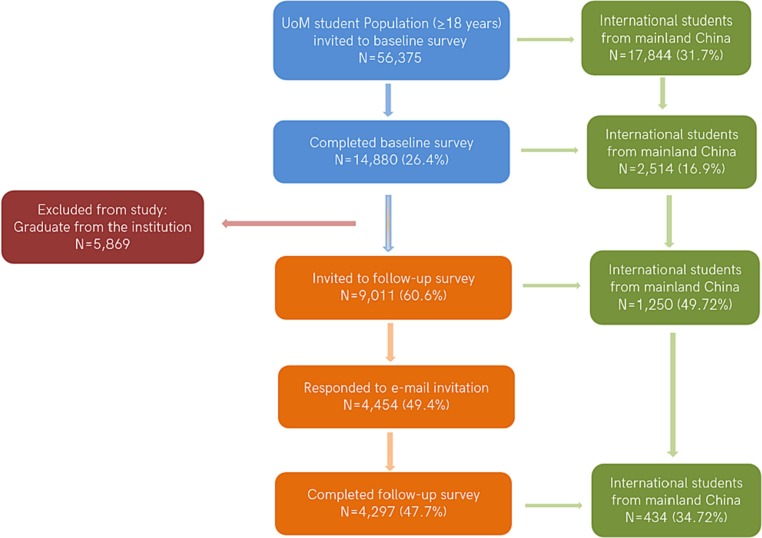
From 17,884 Chinese international students studying at the participating institution at Wave 1, 2514(16.9 %) completed at least one section of the survey. By Wave 2, approximately half this group (1250 students) were continuing at the University and eligible to participate in Wave 2. Of these, 34.7 % (n = 434) completed the Wave 2 survey (Fig. 1 ).
Fig. 1.
Participants in the Wave 1 & Wave 2 survey.
Comparison was made between the overall Chinese international student population from the participating institute and the subsample of students taking part in the present study (Table 1 ). The mean age of Chinese international students who took part in the Wave 2 survey (n = 4,34) was slightly higher than the mean age of Chinese international students in the overall university population (21.7 years vs 20.4 years). The proportion of female students taking part in the Wave 2 survey was slightly higher than the proportion of females in the overall student population (68.6 % vs 62.4 %). Meanwhile, undergraduate and younger students were more likely to be invited and participate in the Wave 2 survey (as their degree is three-years compared to two-years for postgraduate students) (Table 1). During the time of the Wave 1 survey, all Chinese international students studying at the university were currently living in Australia, whilst at Wave 2 there were 97 (22.4 %, 95%CI:18.5 % ∼ 26.6 %) students living in China or another oversea country.
Table 1.
Demographics of Chinese international students.
| Institution population (2019) |
Wave 1 sample (2019) |
Students invited to Wave 2 (2020) |
Wave 2 sample (2020) |
||||
|---|---|---|---|---|---|---|---|
| n = 17,844 | n = 2514 | n missing (%) | n = 1250 | n missing (%) | n = 434 | n missing (%) | |
| Mean Age (SD) | 20.4 (0.30) | 22.6 (2.80) | 21.8 (2.87) | 21.7 (2.89) | |||
| Gender (% of total) | 34 (1.4 %) | 24 (1.9 %) | 7 (1.6 %) | ||||
| Female | 11,132 (62.4 %) | 1690 (68.2 %) | 818 (66.7 %) | 293 (68.6 %) | |||
| Male | 6709 (37.6 %) | 789 (31.8 %) | 408 (33.3 %) | 134 (31.4 %) | |||
| Self-described | 3 (0.02 %) | 1 (0.04 %) | 0 | 0 | |||
| Course level (% of total) | 70 (2.8 %) | 36 (2.9 %) | 6 (1.4 %) | ||||
| Undergraduate | 6847 (38.4 %) | 935 (38.3 %) | 644 (53.1 %) | 238 (55.6 %) | |||
| Masters (coursework) | 10,320 (57.8 %) | 1355 (55.4 %) | 474 (39.0 %) | 152 (35.5 %) | |||
| Other postgraduate | 145 (0.8 %) | 22 (0.9 %) | 7 (0.6 %) | 3 (0.7 %) | |||
| Graduate Research | 532 (3.0 %) | 132 (5.4 %) | 89 (7.3 %) | 35 (8.2 %) | |||
| Wave 1 financial difficulties (% of total) | 421 (16.8 %) | 225 (18.0 %) | 54 (12.4 %) | ||||
| Yes | / | 159 (7.6 %) | 79 (7.7 %) | 28 (7.4 %) | |||
| No | / | 1934 (92.4 %) | 946 (92.3 %) | 352 (92.6 %) | |||
3.2. Prevalence of major depression and anxiety at Wave 1 and 2
The prevalence of reported major depression was observed to substantially increase from 22.7 % (95 % CI: 18.7 % ∼ 27.3 %) at Wave 1 to 43.8 % (95 % CI: 39.1 % ∼ 48.6 %) at Wave 2 (Table 2 ). Similarly, there was a marked increase in the prevalence of anxiety from Wave 1 (26.5 %, 95 % CI: 22.3 % ∼ 31.3 %) to Wave 2 (45.7 %, 95 % CI: 41.0 % ∼ 50.5 %). Weighted prevalence of major depression and anxiety at Wave 2, estimated through sensitivity analyses remained high (major depression: 42.7 %, 95 % CI: 37.4 % ∼ 48.1 %; anxiety: 44.0 %, 95 % CI: 38.7 % ∼ 49.4 %). Overall, the weighted prevalence of major depression and anxiety were seen to be 1.8 to 2 times higher than the prevalence of major depression and anxiety in the Wave 1 survey.
Table 2.
Comparison of major depression and anxiety among Chinese international students (Wave 12019/Wave 22020).
| Wave 1 results for those invited to participate in Wave 2 (2019) |
Wave 1 results for those participating in Wave 2 (2019) |
Wave 2 results (2020) |
|||||
|---|---|---|---|---|---|---|---|
| Observed prevalence |
Weighted prevalence (95 % CI) |
||||||
| n = 1250 | 95 % CI | n = 434 | 95 % CI | n = 434 | 95 % CI | n = 348 | |
| Major depression (% of total) | |||||||
| Yes | 219 (22.1 %) | [19.7 %,24.8 %] | 84 (22.7 %) | [18.7 %,27.3 %] | 183 (43.8 %) | [39.1 %,48.6 %] | 42.7 % [37.4 %,48.1 %] |
| No | 770 (77.9 %) | [75.2 %,80.3 %] | 286 (77.3 %) | [72.7 %,81.3 %] | 235 (56.2 %) | [51.2 %,60.9 %] | 57.3 % [51.9 %,62.6 %] |
| Missing | 261 (20.9 %) | 64 (14.8 %) | 16 (3.7 %) | ||||
| Anxiety (% of total) | |||||||
| Yes | 241 (24.7 %) | [22.1 %,27.5 %] | 98 (26.5 %) | [22.3 %,31.3 %] | 191 (45.7 %) | [41.0 %,50.5 %] | 44.0 % [38.7 %,49.4 %] |
| No | 735 (75.3 %) | [72.5 %,77.9 %] | 271 (73.4 %) | [68.7 %,77.7 %] | 227 (54.3 %) | [49.5 %,59.0 %] | 56.0 % [50.6 %,61.3 %] |
| Missing | 274 (21.9 %) | 65 (15.0 %) | 16 (3.7 %) | ||||
3.3. Pandemic-related stressors
The details of reported pandemic-related stressors can be found in Table 3 . In regard to health and wellbeing issues, confidence in future job prospects and coping with study were identified as the top two stressors (Table 3). In terms of connection and relationship issues, 73.9 % (95 % CI: 69.4 % ∼ 77.9 %) to 82.6 % (95 % CI: 78.7 % ∼ 86.0 %) of participants reported it was more difficult for them to connect with friends and university peers during the pandemic. Regarding improvements in stressors during the COVID-19 pandemic, 27.1 % (95 % CI: 23.0 % ∼ 31.6 %) of participants thought their relationship with family improved during the COVID-19 pandemic, while 55.1 % (95 % CI: 50.3 % ∼ 59.9 %) stated this relationship did not change. In regard to financial and housing issues, over three quarters of participants believed that it was more difficult for them to get access to paid work during the COVID-19 pandemic. Meanwhile, 68.2 % (95 % CI: 63.4 % ∼ 72.5 %) of participants stated that their financial position was worse than before. In the sensitivity analysis, the weighted prevalence of each stressor did not materially change from the unweighted estimates.
Table 3.
Wave 2 pandemic-related stressors reported by Chinese international students.
| Pandemic-related stressors | n = 434 | n missing (%) | Observed prevalence % (95 % CI) | Weighted prevalence % (95 % CI) |
|---|---|---|---|---|
| Health and wellbeing issues (% of total) | ||||
| Confidence in future job prospects | 25 (5.8 %) | |||
| Worse than before | 334 | 81.7 [77.6,85.1] | 80.7 [75.9,84.6] | |
| Unchanged | 62 | 15.2 [12.0,19.0] | 15.6 [12.1,20.0] | |
| Better than before | 13 | 3.2 [1.9,5.4] | 3.7 [2.1,6.5] | |
| Coping with study | 24 (5.5 %) | |||
| Worse than before | 296 | 72.2 [67.6,76.3] | 71.1 [65.8,75.8] | |
| Unchanged | 71 | 17.3 [13.9,21.3] | 18.3 [14.4,22.9] | |
| Better than before | 43 | 10.5 [7.9,13.9] | 10.7 [7.7,14.6] | |
| Racial discrimination | 41 (9.5 %) | |||
| Worse than before | 206 | 52.4 [47.5,57.3] | 49.9 [44.4,55.5] | |
| Unchanged | 174 | 44.3 [39.4,49.2] | 46.3 [40.7,51.9] | |
| Better than before | 13 | 3.3 [1.9,5.6] | 3.8 [2.1,6.7] | |
| Homesickness | 38 (8.8 %) | |||
| Worse than before | 200 | 50.5 [45.6,55.4] | 49.0 [43.5,54.6] | |
| Unchanged | 157 | 39.7 [34.9,44.6] | 40.5 [35.1,46.1] | |
| Better than before | 39 | 9.9 [7.3,13.2] | 10.5 [7.5,14.5] | |
| Connection and relationship issues (% of total) | ||||
| Connection to University peers | 25 (5.8 %) | |||
| Worse than before | 338 | 82.6 [78.7,86.0] | 82.3 [77.6,86.1] | |
| Unchanged | 56 | 13.7 [10.7,17.4] | 14.3 [10.8,18.7] | |
| Better than before | 15 | 3.7 [2.2,6.0] | 3.5 [1.9,6.1] | |
| Connection with friends | 24 (5.5 %) | |||
| Worse than before | 303 | 73.9 [69.4,77.9] | 73.0 [67.8,77.7] | |
| Unchanged | 74 | 18.1 [14.6,22.1] | 19.6 [15.5,24.5] | |
| Better than before | 33 | 8.1 [5.8,11.1] | 7.4 [5.0,10.7] | |
| Relationship with family | 24 (5.5 %) | |||
| Worse than before | 73 | 17.8 [14.4,21.8] | 19.1 [15.1,23.9] | |
| Unchanged | 226 | 55.1 [50.3,59.9] | 55.5 [50.0,60.9] | |
| Better than before | 111 | 27.1 [23.0,31.6] | 25.4 [21.0,30.5] | |
| Financial and housing issues (% of total) | ||||
| Access to paid work | 66 (15.2 %) | |||
| Worse than before | 287 | 78.0 [73.5,81.9] | 78.2 [73.0,82.7] | |
| Unchanged | 69 | 18.8 [15.1,23.1] | 18.7 [14.5,23.7] | |
| Better than before | 12 | 3.26 [1.9,5.7] | 3.1 [1.6,5.8] | |
| Financial positions | 29 (6.7 %) | |||
| Worse than before | 276 | 68.2 [63.4,72.5] | 68.3 [63.0,73.2] | |
| Unchanged | 113 | 27.9 [23.7,32.5] | 27.3 [22.7,32.4] | |
| Better than before | 16 | 4.0 [2.4,6.4] | 4.5 [2.7,7.3] | |
| Finding suitable accommodation/living arrangements | 51 (11.8 %) | |||
| Worse than before | 141 | 36.8 [32.1,41.8] | 37.7 [32.3,43.5] | |
| Unchanged | 202 | 52.7 [47.7,57.7] | 52.6 [46.8,58.2] | |
| Better than before | 40 | 10.4 [7.8,13.9] | 9.8 [6.9,13.7] | |
3.4. Country of residence, mental health, and pandemic-related stressors
For the 97 students residing in China and other countries at Wave 2, the prevalence of major depression in the Wave 2 survey was 34.8 % (95 % CI: 25.7 % ∼ 45.2 %), whereas the prevalence of major depression for Chinese students who were living in Australia was 46.3 % (95 % CI: 41.0 % ∼ 51.8 %) (Table 4 ). For students residing in China and other countries, the prevalence of anxiety was 41.3 % (95 % CI: 31.6 % ∼ 51.7 %), whilst for Chinese students living in Australia, the prevalence of anxiety was slightly higher (46.9 %; 95 % CI: 41.6 % ∼ 52.4 %). In the adjusted multivariable logistic regression analysis, we did not find a strong association between country of residence and Wave 2 major depression (Adjusted OR: 0.67, 95 % CI: 0.39– 1.15, p-value: 0.144) or anxiety (Adjusted OR: 0.90, 95 % CI: 0.52– 1.55, p-value: 0.707) (Table 4).
Table 4.
Association between pandemic country of residence (Australia versus currently in China & other countries) and major depression/anxiety (Wave 22020).
| Observed prevalence % (95 % CI) |
Weighted prevalence % (95 % CI) |
Adjusted OR (95 % CI) |
p-value |
Weighted Adjusted OR (95 % CI) |
p-value |
|
|---|---|---|---|---|---|---|
| n = 418 | n = 349 | |||||
| Depression | ||||||
| Students currently in Australia (n = 334) | 46.3 [41.0,51.8] | 45.4 [39.4,51.5] | Reference group | – | Reference group | – |
| Students currently in China & Other countries (n = 97) | 34.8 [25.7,45.2] | 33.0 [22.9,45.0] | 0.67 [0.39,1.15](2) | 0.144 | 0.68 [0.38,1.22] | 0.196 |
| Anxiety | – | |||||
| Students currently in Australia (n = 334) | 46.9 [41.6,52.4] | 46.3 [40.3,52.5] | Reference group | – | Reference group | – |
| Students currently in China & Other countries (n = 97) | 41.3 [31.6,51.7] | 35.6 [25.4,47.4] | 0.90 [0.52,1.55](3) | 0.707 | 0.78 [0.43,1.39] | 0.392 |
(1) Missing Australia: 8 (2.4 %), China and other countries: 5 (5.2 %).
(2) After adjusting for age, gender, Wave 1 depression presence.
(3) After adjusting for age, gender, Wave 1 anxiety presence.
The top five pandemic-related stressors among students residing in China and students living in Australia were similar. For students living in China, difficulty connecting with university peers (85.6 %) was the most prevalent stressor during the COVID-19 pandemic (Supplementary Table 1). Meanwhile, for students living in Australia, lack of confidence in future job prospects (83.0 %) was the most prevalent stressor during the COVID-19 pandemic (Supplementary Table 2).
3.5. Social support and psychological symptoms
Table 5 shows the association between social support (Wave 1/Wave 2) and major depression/anxiety (Wave 2). After including all potential confounders in the model, the cross-sectional multifactorial logistic regression analysis results show that high social support during the COVID-19 pandemic (Wave 2) was strongly associated with a decreased risk of reporting major depression in Wave 2 (Table 5). The odds ratio of 0.18 (95 % CI: 0.07– 0.43; p-value<0.001) indicated that students with high social support during the COVID-19 pandemic were 82 % less likely to report major depression in Wave 2 comparing to those students with low social support during the pandemic. Students who had high social support during the COVID-19 pandemic had a 0.28 (95 % CI: 0.13– 0.62; p-value = 0.002) decreased odds of reporting anxiety in Wave 2 when compared to those who had low social support during the pandemic. With each increasing unit of social support on the MOS-SSS-6, there was a decreased odds of major depression (Adjusted OR:0.90, 95 % CI:0.85– 0.94; p-value<0.001) and anxiety (Adjusted OR:0.91, 95 % CI: 0.87– 0.96; p-value:0.001).
Table 5.
Logistic regression analysis of the association between social support (Wave 1 2019/Wave 2 2020) and major depression/anxiety (Wave 2 2020)
| Major depression | ||||||
|---|---|---|---|---|---|---|
| No (%) |
Yes (%) |
Adjusted OR (95 % CI) |
p-value |
Weighted Adjusted OR (95 % CI) |
p-value |
|
| n = 342 | ||||||
| Social support wave 1 mean (SD)(1) | 18.03 (6.50) | 17.99 (6.42) | 1.00 [0.97, 1.04] | 0.813 | 1.01 [0.97,1.04] | 0.642 |
| Categorised | ||||||
| Low | 87 (56.1 %) | 68 (43.9 %) | Reference group | – | Reference group | – |
| Medium | 64 (56.1 %) | 50 (43.9 %) | 1.17 [0.71,1.95] | 0.539 | 1.29 [0.77,2.18] | 0.335 |
| High | 44 (55.0 %) | 36 (45.0 %) | 1.03 [0.58,1.83] | 0.915 | 1.09 [0.60,1.96] | 0.781 |
| Total | 195 (55.9 %) | 154 (44.1 %) | ||||
| n = 340 | ||||||
| Social support wave 2 mean (SD) (2) | 19.90 (6.46) | 16.73 (5.73) | 0.89 [0.85, 0.94] | <0.001 | 0.90 [0.85, 0.94] | <0.001 |
| Categorised | ||||||
| Low | 78 (45.6 %) | 93 (54.3 %) | Reference group | – | Reference group | – |
| Medium | 79 (53.7 %) | 68 (46.3 %) | 0.61 [0.35,1.05] | 0.076 | 0.63 [0.36,1.11] | 0.111 |
| High | 78 (78.0 %) | 22 (22.0 %) | 0.15 [0.06,0.34] | <0.001 | 0.18 [0.07,0.43] | <0.001 |
| Total | 235 (56.2 %) | 183 (43.8 %) | ||||
| Anxiety | ||||||
| n = 342 | ||||||
| Social support wave 1 mean (SD)(3) | 18.02 (6.43) | 18.00 (6.52) | 1.01 [0.97, 1.04] | 0.775 | 1.00 [0.97,1.04] | 0.892 |
| Categorised | ||||||
| Low | 81 (52.3 %) | 74 (47.7 %) | Reference group | – | Reference group | – |
| Medium | 62 (54.4 %) | 52 (45.6 %) | 1.01 [0.60,1.70] | 0.962 | 1.00 [0.58,1.72] | 0.996 |
| High | 44 (55.0 %) | 36 (45.0 %) | 0.91 [0.51,1.63] | 0.747 | 0.91 [0.51,1.63] | 0.743 |
| Total | 187 (53.6 %) | 162 (46.4 %) | ||||
| n = 340 | ||||||
| Social support wave 2 mean (SD)(4) | 19.78 (6.31) | 17.01 (6.07) | 0.91 [0.86, 0.95] | <0.001 | 0.91 [0.87,0.96] | 0.001 |
| Categorised | ||||||
| Low | 78 (45.6 %) | 93 (54.4 %) | Reference group | – | Reference group | – |
| Medium | 77 (52.4 %) | 70 (47.6 %) | 0.70 [0.40,1.21] | 0.196 | 0.69 [0.39,1.21] | 0.190 |
| High | 72 (72.0 %) | 28 (28.0 %) | 0.28 [0.13,0.62] | 0.002 | 0.34 [0.14,0.79] | 0.012 |
| Total | 227 (54.3 %) | 191 (45.7 %) | ||||
(1) After adjusting for age, gender, financial difficulties, Wave 1 depression presence.
(2) After adjusting for age, gender, current living status, current living country, Wave 1 social support level, Wave 1 depression presence.
(3) After adjusting for age, gender, financial difficulties, Wave 1 anxiety presence.
(4) After adjusting for age, gender, current living status, current living country, Wave 1 social support level, Wave 1 anxiety presence.
With the sensitivity IPW analysis, the weighted odds ratio of major depression and anxiety for students who had high social support during the pandemic compared to those with low social support was slightly increased. However, the association between high social support during the pandemic and lower odds of major depression and anxiety in Wave 2 remained the same.
We did not find evidence of an association between Wave 1 social support and Wave 2 major depression/anxiety in longitudinal adjusted analyses (Table 5).
4. Discussion
4.1. Main findings
To our knowledge, this study is the first to use longitudinal data to examine mental health status, and the effect of social support amongst Chinese international students during the pandemic. This study highlights the major psychological challenges and stressors faced by Chinese international students, with the reported prevalence of major depression and anxiety during the pandemic almost double pre-pandemic levels. The prevalence of mental health issues was higher for Chinese international students living in Australia during the pandemic than for those living in China during the pandemic, although there was less strong evidence for a difference with the smaller sample size. Meanwhile, Chinese international students experienced considerable financial, social connection and wellbeing stressors during the pandemic. Additionally, this study indicated that Chinese international students with more social support during the COVID-19 pandemic were less likely to experience major depression and anxiety.
Our findings are consistent with previous studies on the wider population of university students, which have found high prevalence of major depression and anxiety during the COVID-19 pandemic (Cao et al., 2020; Chirikov et al., 2020; Dodd et al., 2021). We found that there was a substantial increase in mental health issues for Chinese international students and that the prevalence of major depression and anxiety during the pandemic was slightly higher among those students who were currently living in Australia. It is possible that, compared with those students living in China, Chinese students living in Australia were away from traditional family support (Forbes-Mewett, 2020) and facing more stress, such as racial discrimination (Zhai and Du, 2020), homesickness (Chai, 2020) and financial difficulties (Dodd et al., 2021), and thus tended to experience poorer mental health during the COVID-19 pandemic. It is also worth noting that the Wave 2 survey was conducted during a strict lockdown period in Melbourne, while China has eased some restrictions at that time. A previous study has found that the prevalence of mental health symptoms was lower after a COVID-19 related quarantine was lifted compared to rates during periods of lockdown (Wathelet et al., 2022), which may also explain the differential results by country of residence that we found in this study. Overall, there was weaker evidence of an association between country of residence and mental health status during the pandemic, however the samples sizes for this comparison were small and may thus have impacted statistical power. Thus, these hypotheses still require further investigation.
4.2. Pandemic-related stressors among Chinese international students
This study also found Chinese international students faced various stressors during the COVID-19 pandemic, including difficulty connecting with university peers and friends, access to paid work, coping with study, and lower confidence in future job opportunities. This finding is in line with previous studies in a general population of university students, which found students reported more stress from online study, graduation and future job prospects, as well as difficulties maintaining the connection with university peers during the COVID-19 pandemic (Dodd et al., 2021; Hamza et al., 2020). It is also worth noting that over a quarter of participants indicated that their relationship with family had improved during the pandemic, while previous research found that the COVID-19 pandemic might have a disruptive effect on family relationships (Prime et al., 2020). This might be attributed to the high value placed on family orientation in China (Xia and Duan, 2020). Research has indeed identified that Chinese international students tend to rely on their families for support when dealing with difficult issues (Ling and Tran, 2015). Another possible reason might be that the COVID-19 pandemic has made people begin to realize the fragility of life (Zhang et al., 2020), which may in turn increase their contact with their families.
4.3. Effect of social support on psychological symptoms
The current study indicated that higher social support during the COVID-19 pandemic was associated with a lower likelihood of reporting major depression and anxiety. This finding is in accordance with previous studies demonstrating that social support has a protective effect on mental health among young adults in acute and large-scale pandemic situations (Grey et al., 2020; Li et al., 2020; Liu et al., 2020). A possible explanation for this might be that family members and friends protect against mental health issues of young adults by providing support and demonstrating empathy (Qi et al., 2020). Moreover, social support can provide resources for individuals to help them dealing with stressors and reducing maladaptive coping strategies under such epidemic circumstance (Li et al., 2020). However, it is important to note that in the present study this association was not found longitudinally, hence there is a possibility that the lower levels of mental health caused a decrease in seeking of social contact or reporting of social support by students (Kiely et al., 2021).
4.4. Strengths and limitations
This study has several notable strengths. First, it is the first study using longitudinal data to assess the association between social support and psychological symptoms among Chinese international students during the COVID-19 pandemic. By using the longitudinal data, we were able to compare over time the changes in major depression and anxiety. Second, this study used validated scales (e.g., PHQ-2, GAD-2, and MOS-SSS-6) to measure psychological symptoms and social support level, which increases the internal validity of the study. Additionally, we used inverse probability weighting to help address potential attrition bias. We reported the prevalence of major depression, anxiety, pandemic-related stressors, as well as the odds of major depression and anxiety after weighting for factors that were associated with non-participation. In addition, the demographic characteristics of this study sample are similar to the university's Chinese international student population, which indicates the study results are likely representative of the wider Chinese international student population.
This study also has some limitations that need to be highlighted. Firstly, social support during the COVID-19 pandemic and mental health status were assessed at the same time in 2020. Thus, we are not able to examine the temporal relationship between these two variables, and ongoing longitudinal studies would be needed to assess this. Secondly, the relatively small sample size at Wave 2 prohibits us from separately evaluating the effect of social support on mental health among students currently in China and students currently in Australia. Meanwhile, we only have cross-sectional data regarding students' country of residence. Therefore, we cannot attribute currently living country as a causative factor for major depression and anxiety in this study. It may be that mental health issues were a factor in the decision to live in China/overseas or Australia during the pandemic. Third, as with many other observational studies, we were not able to measure all potential confounders in this study. For instance, personality traits (e.g., neuroticism and extraversion) can be a potential confounder that affects the association between social support and psychological symptoms (Fyrand et al., 1997; Lara et al., 1997). Future studies could include personality traits as a potential confounder in the analysis.
4.5. Implications and recommendations
As the first study examining the pandemic-related stressors, psychological symptoms and their relationship with social support among Chinese international students during the COVID-19 pandemic, this study has important implications for universities and other educational institutions. First of all, given that Chinese international students reported an extremely high prevalence of pandemic-related stressors, major depression and anxiety during the pandemic, counseling services could consider using the online platform and social media to share self-help strategies to assist Chinese international students build positive coping strategies and maintain good mental health; such platforms can also reach students living internationally. Our study also found that Chinese international students felt less confident in future job markets during the COVID-19 pandemic than before. Therefore, universities could design specific career programs for Chinese international students to help them planning for their future careers and competing for graduate jobs. Of note, this concern was issued for Chinese international students prior to the pandemic (Nachatar Singh, 2020) and were then exacerbated by the pandemic. Post pandemic these issues are highly likely to continue without intervention.
In addition, this study found social support during the COVID-19 pandemic was negatively associated with major depression and anxiety. Previous studies also indicate that individuals with low social support satisfaction are more likely to suffer from mental health problems (Harandi et al., 2017). Moreover, a study on social capital showed that receiving social support from local community members could help increase the sense of belonging, reduce negative effects of loneliness, and promote effective behavioural responses to the pandemic (Stevenson et al., 2021). This local community support is a factor that may not have been experienced by Chinese international students in Australia. Therefore, universities could consider designing programs to help Chinese international students build connections and create informal social support networks during challenging times by organizing online activities, such as regular student-staff catch up sessions, as universities play a crucial role in providing students with opportunities to interact with staff and other students (Ye et al., 2020).
Although some of the issues explored in this study, such as financial stress due to loss of work and stress imposed by border closures may be specific to those countries which had certain pandemic restrictions in place, other implications, such as the ongoing importance of social support and the use of online platforms and social media to build connections and networks remain relevant as a global issue.
5. Conclusion
The present study used longitudinal data to examine Chinese international student mental health before and during the COVID-19 pandemic. The study results demonstrate that Chinese international students experienced many pandemic-related stressors and reported high levels of major depression and anxiety symptoms during the pandemic. These issues appeared heightened for students living in Australia. The major issues identified were prevalent prior to the pandemic and are likely to continue post pandemic. These findings could be used by universities and other educational institutions to develop effective interventions to help Chinese international students cope with this acute and large-scale epidemic.
Funding
We received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest
None.
Acknowledgments
Acknowledgements
We would like to acknowledge that this study is associated with a larger study conducted by the University of Melbourne in partnership with the Bupa Foundation. The authors would like to acknowledge Patty Chondros (Department of General Practice) to provide statistical support for this study. We are also thankful to the thousands of students who responded to the survey invitation and provided the data presented in this study.
CRediT authorship contribution statement
Author TK: designed the study, conducted the analysis, and wrote the initial draft of the manuscript
Author LS & NR & IW: provided comments on the draft of manuscript
Author WL & MR: provided substantial feedback and guidance on the study design, analysis and multiple iteration of the manuscript
Appendix A. Supplementay data
Supplementary material
References
- ABC News Australians told not to travel to mainland China due to coronavirus threat, border restrictions tightened considerably. 2020. https://www.abc.net.au/news/2020-02-01/australians-told-not-to-travel-to-china-due-to-coronavirus/11920742
- Alan M., Catherine H., Shaun W., et al. 2020. The experience of international students before and during COVID-19: housing, work, study and wellbeing. doi:APO-307336. [Google Scholar]
- Australian Institute of Health and Welfare Mental health services in Australia. 2021. https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia
- Batra K., Sharma M., Batra R., Singh T.P., Schvaneveldt N. Assessing the psychological impact of COVID-19 among college students: an evidence of 15 countries. Healthcare. 2021;9(2) doi: 10.3390/healthcare9020222. (Basel) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton R. Financial Review; 2020. Struggling international students don't get any JobSeekers.https://www.afr.com/work-and-careers/education/struggling-international-students-don-t-get-any-jobkeepers-20200413-p54j8r [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey M., Boyes A., Noble N., Waller A., Inder K. Validation of the PHQ-2 against the PHQ-9 for detecting depression in a large sample of Australian general practice patients. Aust. J. Prim. Health. 2016;22(3):262–266. doi: 10.1071/py14149. [DOI] [PubMed] [Google Scholar]
- Chai S. The study of mental health of overseas students during COVID-19. Int.J.Educ.Manag. 2020;5(3):230–231. http://ij-em.com/Papers/Vol%205,%20No%203%20(IJEM%202020).pdf#page=236 http://ij-em.com/Papers/Vol%205,%20No%203%20(IJEM%202020).pdf#page=236. [Google Scholar]
- Chen J.H., Li Y., Wu A.M.S., Tong K.K. The overlooked minority: mental health of international students worldwide under the COVID-19 pandemic and beyond. Asian J. Psychiatr. 2020;54 doi: 10.1016/j.ajp.2020.102333. 102333-102333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirikov I., Soria K.M., Horgos B., Jones-White D. SERU Consortium, U. o. C.-. Berkeley, & U. o. Minnesota; 2020. Undergraduate And Graduate Students' Mental Health During the COVID-19 Pandemic. [Google Scholar]
- Copeland W.E., McGinnis E., Bai Y., Adams Z., Nardone H., Devadanam V., Rettew J., Hudziak J.J. Impact of COVID-19 pandemic on college student mental health and wellness. J. Am. Acad. Child Adolesc. Psychiatry. 2021;60(1):134–141.e132. doi: 10.1016/j.jaac.2020.08.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd R.H., Dadaczynski K., Okan O., McCaffery K.J., Pickles K. Psychological wellbeing and academic experience of university students in Australia during COVID-19. Int. J. Environ. Res. Public Health. 2021;18(3) doi: 10.3390/ijerph18030866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes-Mewett H. International Education Association of Australia; 2020. The impact of COVID-19 on international student mental health.https://www.ieaa.org.au/blog/the-impact-of-covid-19-on-international-student-mental-health [Google Scholar]
- Fronek P., Briggs L., Liang J., Gallagher H., Doherty A., Charles B., McDonald S. Australian Social Work Academics respond to international students in crisis during COVID-19. Front. Educ. 2021;6:51. doi: 10.3389/feduc.2021.637583. https://www.frontiersin.org/article/10.3389/feduc.2021.637583. [DOI] [Google Scholar]
- Fyrand L., Wichstrøm L., Moum T., Glennås A., Kvien T.K. The impact of personality and social support on mental health for female patients with rheumatoid arthritis. Soc. Indic. Res. 1997;40(3):285–298. http://www.jstor.org/stable/27522248 http://www.jstor.org/stable/27522248. [Google Scholar]
- Gariépy G., Honkaniemi H., Quesnel-Vallée A. Social support and protection from depression: systematic review of current findings in Western countries. Br. J. Psychiatry. 2016;209(4):284–293. doi: 10.1192/bjp.bp.115.169094. [DOI] [PubMed] [Google Scholar]
- Grey I., Arora T., Thomas J., Saneh A., Tohme P., Abi-Habib R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza C.A., Ewing L., Heath N.L., Goldstein A.L. Educational Publishing Foundation; 2020. When Social Isolation Is Nothing New: A Longitudinal Study Psychological Distress During COVID-19 Among University Students With And Without Preexisting Mental Health Concerns. [DOI] [Google Scholar]
- Harandi T.F., Taghinasab M.M., Nayeri T.D. The correlation of social support with mental health: a meta-analysis. Electron. Physician. 2017;9(9):5212–5222. doi: 10.19082/5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hefner J., Eisenberg D. Social support and mental health among college students. Am. J. Orthopsychiatry. 2009;79(4):491–499. doi: 10.1037/a0016918. [DOI] [PubMed] [Google Scholar]
- Holden L., Lee C., Hockey R., Ware R.S., Dobson A.J. Validation of the MOS Social Support Survey 6-item (MOS-SSS-6) measure with two large population-based samples of Australian women. Qual. Life Res. 2014;23(10):2849–2853. doi: 10.1007/s11136-014-0741-5. [DOI] [PubMed] [Google Scholar]
- Kiely K.M., Sutherland G., Butterworth P., Reavley N.J. Age and gender differences in the reciprocal relationship between social connectedness and mental health. Soc. Psychiatry Psychiatr. Epidemiol. 2021;56(6):1069–1081. doi: 10.1007/s00127-020-01960-3. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med. Care. 2003;41(11):1284–1292. doi: 10.1097/01.Mlr.0000093487.78664.3c. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Monahan P.O., Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Lara M.E., Leader J., Klein D.N. The association between social support and course of depression: is it confounded with personality? J. Abnorm. Psychol. 1997;106(3):478–482. doi: 10.1037//0021-843x.106.3.478. [DOI] [PubMed] [Google Scholar]
- Li X., Wu H., Meng F., Li L., Wang Y., Zhou M. Relations of COVID-19-related stressors and social support with Chinese college students' psychological response during the COVID-19 pandemic. Front. Psychiatry. 2020;11:1084. doi: 10.3389/fpsyt.2020.551315. https://www.frontiersin.org/article/10.3389/fpsyt.2020.551315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling C., Tran L.T. Chinese international students in Australia: an insight into their help and information seeking manners. Int.Educ.J. 2015;14(1):42–56. [Google Scholar]
- Litam S.D. "Take Your Kung-Flu Back to Wuhan": Counseling Asians, Asian Americans, and Pacific Islanders with race-based trauma related to COVID-19. Prof. Couns. 2020;10:144–156. doi: 10.15241/sdal.10.2.144. [DOI] [Google Scholar]
- Liu X., Kakade M., Fuller C.J., Fan B., Fang Y., Kong J., Guan Z., Wu P. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry. 2012;53(1):15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113172. 113172-113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main A., Zhou Q., Ma Y., Luecken L.J., Liu X. Relations of SARS-related stressors and coping to Chinese college students' psychological adjustment during the 2003 Beijing SARS epidemic. J. Couns. Psychol. 2011;58(3):410–423. doi: 10.1037/a0023632. [DOI] [PubMed] [Google Scholar]
- Meda N., Pardini S., Slongo I., Bodini L., Zordan M.A., Rigobello P., Visioli F., Novara C. Students' mental health problems before, during, and after COVID-19 lockdown in Italy. J. Psychiatr. Res. 2021;134:69–77. doi: 10.1016/j.jpsychires.2020.12.045. [DOI] [PubMed] [Google Scholar]
- Nachatar Singh J.K. Challenges in obtaining employment in China: lived experiences of Australian Chinese graduates. Aust. J. Career Dev. 2020;29(3):153–163. doi: 10.1177/1038416220947085. [DOI] [Google Scholar]
- Ni M.Y., Yang L., Leung C.M.C., Li N., Yao X.I., Wang Y., Leung G.M., Cowling B.J., Liao Q. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Ment. Health. 2020;7(5) doi: 10.2196/19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Qi M., Zhou S.J., Guo Z.C., Zhang L.G., Min H.J., Li X.M., Chen J.X. The effect of social support on mental health in Chinese adolescents during the outbreak of COVID-19. J. Adolesc. Health. 2020 doi: 10.1016/j.jadohealth.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus. 2020;12(4) doi: 10.7759/cureus.7541. e7541-e7541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salimi N., Gere B., Talley W., Irioogbe B. College students mental health challenges: concerns and considerations in the COVID-19 pandemic. J. Coll. Stud. Psychother. 2021;1–13 doi: 10.1080/87568225.2021.1890298. [DOI] [Google Scholar]
- Sanci L., Williams I., Russell M., Chondros P., Duncan A.-M., Tarzia L., Peter D., Lim M.S.Y., Tomyn A., Minas H. Towards a health promoting university: descriptive findings on health, wellbeing and academic performance amongst university students in Australia. BMC Public Health. 2022;22(1):2430. doi: 10.1186/s12889-022-14690-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son C., Hegde S., Smith A., Wang X., Sasangohar F. Effects of COVID-19 on college students' mental health in the United States: interview survey study. J. Med. Internet Res. 2020;22(9) doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson C., Wakefield J.R.H., Felsner I., Drury J., Costa S. Collectively coping with coronavirus: local community identification predicts giving support and lockdown adherence during the COVID-19 pandemic. Br. J. Soc. Psychol. 2021;60(4):1403–1418. doi: 10.1111/bjso.12457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth E., Faherty T., Mazaheri A., Raymond J.E. Changes to student mental health during the COVID-19 pandemic. PsychArchives. 2021 doi: 10.23668/PSYCHARCHIVES.4635. [DOI] [Google Scholar]
- Wathelet M., Vincent C., Fovet T., Notredame C.E., Habran E., Martignène N., Baubet T., Vaiva G., D'Hondt F. Evolution in French university students' mental health one month after the first COVID-19 related quarantine: results from the COSAMe survey. Front. Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.868369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia M., Duan C. Stress coping of Chinese international students in face of COVID 19 pandemic: cultural characteristics. Int. J. Ment. Health Promot. 2020;22(3) doi: 10.32604/IJMHP.2020.011117. [DOI] [Google Scholar]
- Xiao B. ABC News; 2021. Chinese students graduate from Australian universities, but some have never set foot on campus due to COVID.https://www.abc.net.au/news/2021-08-24/chinese-international-students-australia-pandemic-graduates/100399338 [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Z., Yang X., Zeng C., Wang Y., Shen Z., Li X., Lin D. Resilience, social support, and coping as mediators between COVID-19-related stressful experiences and acute stress disorder among college students in China. Appl. Psychol. Health Well Being. 2020 doi: 10.1111/aphw.12211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai Y., Du X. Mental health care for international Chinese students affected by the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4) doi: 10.1016/s2215-0366(20)30089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Zhang H., Ma X., Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int. J. Environ. Res. Public Health. 2020;17(10) doi: 10.3390/ijerph17103722. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material