Abstract
Objective
Delirium in older emergency department (ED) adults is associated with poorer long‐term physical function and cognition. We sought to evaluate if the time to and intensity of physical and/or occupational therapy (PT/OT) are associated with the duration of ED delirium into hospitalization (ED delirium duration).
Methods
This is a secondary analysis of a prospective cohort study conducted from March 2012 to November 2014 at an urban, academic, tertiary care hospital. Patients aged ≥65 years presenting to the ED and who received PT/OT during their hospitalization were included. Days from enrollment to the first PT/OT session and PT/OT duration relative to hospital length of stay (PT/OT intensity) were abstracted from the medical record. ED delirium duration was defined as the duration of delirium detected in the ED using the Brief Confusion Assessment Method. Data were analyzed using a proportional odds logistic regression adjusted for multiple variables. Adjusted odds ratios (ORs) were calculated with 95% confidence intervals (95%CI).
Results
The median log PT/OT intensity was 0.5% (interquartile range [IQR]: 0.3%, 0.9%) and was associated with shorter delirium duration (adjusted OR, 0.39; 95% CI, 0.21–0.73). The median time to the first PT/OT session was 2 days (IQR: 1, 3 days) and was not associated with delirium duration (adjusted OR, 1.02; 95% CI, 0.82–1.27).
Conclusion
In older hospitalized adults, higher PT/OT intensity may be a useful intervention to shorten delirium duration. Time to first PT/OT session was not associated with delirium duration but was initiated a full 2 days after the ED presentation.
Keywords: delirium, emergency department, occupational therapy, physical therapy
1. INTRODUCTION
1.1. Background
Delirium is an acute attention and cognition disorder that can be described as “acute brain failure.” 1 Approximately 8% to 17% of older emergency department (ED) patients present with delirium, 2 , 3 and up to 50% of older adults experience delirium during their hospital stay. 1 The longer delirium persists during hospitalization, there is an incremental worsening of cognition and function during the 6‐month period after hospital discharge. 4 Delirium also can be distressing for patients and their families. 5 The effects of delirium often prove costly and fatal. 1
1.2. Importance
Although there are some in‐hospital delirium prevention strategies in older adults, 6 there is, unfortunately, no universally accepted intervention shown to reduce delirium duration, especially in the ED setting. 7 In the ICU setting, early physical and/or occupation therapy (PT/OT) has been shown to be associated with a reduction in days with delirium. 8 , 9 , 10 However, these studies may not be generalizable to older hospitalized adults with higher comorbidity burdens and a wider spectrum of illness severity.
1.3. Goals of this investigation
We sought to determine if the time to and intensity of PT/OT (ie, the percentage of the total time spent in PT/OT relative to the hospital length of stay) is associated with a reduced duration of delirium in the ED extending into hospitalization (ED delirium duration).
2. METHODS
2.1. Study design and setting
This pilot study is a secondary analysis of the DELINEATE study (Delirium in the Emergency Department and Its Extension into Hospitalization (Delineate) Study: Effect on 6‐month Function and Cognition), 4 which was a prospective cohort study conducted at an urban, tertiary care, academic hospital. The DELINEATE study sought to characterize the extent to which delirium in the ED persisted into the hospitalization and determine if delirium duration affected 6‐month function and cognition. This study also conducted delirium assessments in the ED for the first 7 days of hospitalization. The local institutional review board reviewed and approved this study.
2.2. Selection of participants
Eligible patients were enrolled in the larger DELINEATE study between March 2012 and November 2014. 4 Participant enrollment details, including enrollment times and inclusion/exclusion criteria, can be found in the original DELINEATE publication. 4 The selection criteria from DELINEATE identified 228 eligible patients. For this secondary analysis, only the patients who received PT/OT in the ED (if they were boarding in the ED for a prolonged period of time) or the hospital were included. PT/OT was not ordered by the ED but was at the discretion of the patient's inpatient physicians. Although there is no protocol for ordering PT/OT, common indications include needs assessments, pain or mobility support, and discharge planning. 11 , 12 , 13
Research assistants (RAs) screened for delirium in the ED. All eligible patients who screened positive for delirium and 17% of randomly selected eligible patients who screened negative for delirium were enrolled in the DELINEATE study to maximize feasibility. Non‐delirious ED patients were included to represent the full spectrum of acute brain dysfunction, including patients who had features of delirium without meeting the full criteria (subsyndromal delirium). For these secondary analyses, 38.2% of non‐delirious ED patients had subsyndromal delirium.
2.3. Intervention
The primary independent variables of interest were time to the first PT/OT session and PT/OT intensity. They were abstracted from the electronic health record. Time to first PT/OT session was defined as the time from enrollment (days) to the first PT or OT evaluation. The day of the ED presentation was considered day 0. Hospital day 1 was the next day after midnight regardless of when the patient was enrolled.
The Bottom Line
Delirium is associated with enormous adverse outcomes, including higher health care use, irreversible functional decline, and increased mortality in emergency department (ED) patients, yet it is underrecognized and lacks an effective screening approach. No effective intervention for patients in the ED or after their admission to a hospital currently exists. This exploratory study by ED delirium experts borrows concepts from the ICU experience and offers promise. These pilot results should serve as an urgent catalyst for dedicated efforts to develop and test an ED‐based delirium intervention.
PT/OT intensity was calculated using the following formula:
PT/OT intensity is the percentage of time spent doing PT/OT during the hospital stay. In other words, a PT/OT intensity of 0.5% meant that 0.5% of the patient's hospital stay was spent in PT/OT. The duration of PT/OT is the sum of time spent with the patient each therapy session, as documented in the session summary note by the therapist. The rationale for using PT/OT intensity rather than duration is to account for the variability in hospital length of stay; that is, patients with a shorter hospital length of stay also would have a shorter PT/OT duration. Because PT/OT intensity was skewed, it was logarithmically transformed to normalize the data. All electronic health record data abstractions were double checked for accuracy.
2.4. Outcomes
ED delirium duration was defined as the total number of days a patient was delirious in the ED and continued throughout hospitalization. Delirium assessments were conducted in the ED 4 at the time of enrollment (0 hours) and at 3 hours. A patient was considered to be delirious in the ED (at enrollment) if the assessment was positive at either 0 or 3 hours. If both delirium assessments at enrollment were negative, then the patient was considered non‐delirious in the ED and was assigned an ED delirium of 0 days even if the patient developed delirium during hospitalization (incident delirium). Delirium assessments continued once daily for the first 7 days of hospitalization or until discharge, whichever occurred first. Assessments were conducted 7 days a week, usually in the mornings.
Trained RAs assessed delirium each day for all study participants. In non‐ventilated patients, a modified version of the Brief Confusion Assessment Method was used. This is a brief (<2 minutes) delirium assessment designed for use by non‐physicians in the ED setting. 14 In older ED patients, it has 82% to 86% sensitivity and 93% to 96% specificity for delirium as diagnosed by a psychiatrist, with a κ of 0.87, indicating excellent interobserver reliability. 14
2.5. Additional measurements
Trained RAs also collected pre‐illness functions at the time of enrollment using the Older American Resources and Services (OARS) Activities of Daily Living (ADL) questionnaire. 15 The OARS ADL scale assesses 7 basic and 7 instrumental activities of daily living, with a score range from 0 (completed dependent) to 28 (completely independent). This was ideally completed by an informant (eg, a family member) who knew the patient well. If no informant was available, the patient was allowed to complete the questionnaire if he/she had the capacity to provide consent. Delirium severity at enrollment was measured using the delirium index, which characterizes the severity of 7 delirium symptom domains with a score range from 0 (no delirium) to 21 (severe delirium). 16
A medical record review was performed to collect prior dementia diagnosis, comorbidity burden, the severity of illness, and the presence of a central nervous system diagnosis during the current admission. A patient was considered to have dementia if he or she had (1) documented dementia in the medical record, (2) a premorbid short‐form Informant Questionnaire on Cognitive Decline in the Elderly score 17 greater than a cutoff of 3.38, 18 or (3) prescribed cholinesterase inhibitors before admission. The Charlson Comorbidity Index (Charlson) was used to quantify the patient's comorbidity burden. 19 The Acute Physiology Score (APS) of the Acute Physiology and Chronic Health Evaluation II score was used to quantify the severity of the illness. 20 Two physician reviewers determined the presence of a central nervous system diagnosis (ie, meningitis, seizure, cerebrovascular accident, transient ischemic attack, intraparenchymal hemorrhage, epidural hematoma, subdural hematoma, subarachnoid hemorrhage, cerebral edema, meningitis). A third physician reviewer adjudicated any disagreement.
2.6. Data analysis
Measures of central tendency and dispersion for continuous variables were reported as medians and interquartile ranges (IQRs). Categorical variables were reported as frequencies (percentages). Proportional odds logistic regression was used to determine if time to first PT/OT session and log PT/OT intensity were associated with ED delirium duration adjusted for comorbidity burden (Charlson), illness severity (APS), baseline ADL function (OARS ADL), prior dementia diagnosis, nursing home residence, and central nervous system diagnosis during current admission. Covariates were chosen a priori based on expert opinion, literature review, and previous work. 4 , 21 We limited the multivariable regression model to 1 covariate for every 10 patients to avoid overfitting. 22 Because of the skewed nature of PT/OT intensity, it was logarithmically transformed for the multivariable model. We conducted a series of sensitivity analyses to evaluate the robustness of the multiple linear regression models. Because delirium severity may confound the relationship between time to and log PT/OT intensity with delirium duration, we reran the multivariable models with delirium severity at enrollment. We also reran the models for the subset of patients who were delirious in the ED (at enrollment) and patients not admitted to the ICU. We additionally examined if the effect of PT/OT was modified by pre‐illness functional status or prior dementia diagnosis. We prespecified a P value of 0.20 as the threshold for the presence of effect modification. 23 Adjusted odds ratios (ORs) with 95% confidence intervals (95% CIs) are reported. All statistical analyses were performed with SAS version 9.4 (SAS Institute, Cary, NC).
3. RESULTS
3.1. Characteristics of study subjects
During the study period, 3383 patients were screened for eligibility (Figure 1). A total of 130 patients met the eligibility criteria. Table 1 lists the cohort's characteristics. Participants had a median age of 76 years (IQR: 70, 83 years). A total of 16 participants (12%) were non‐White, 80 (62%) were women, and 24 (18.5%) were admitted to the ICU. Of the participants, 82 (63.1%) were delirious in the ED, with a median (IQR) ED delirium duration of 2 days (0, 5 days).
FIGURE 1.
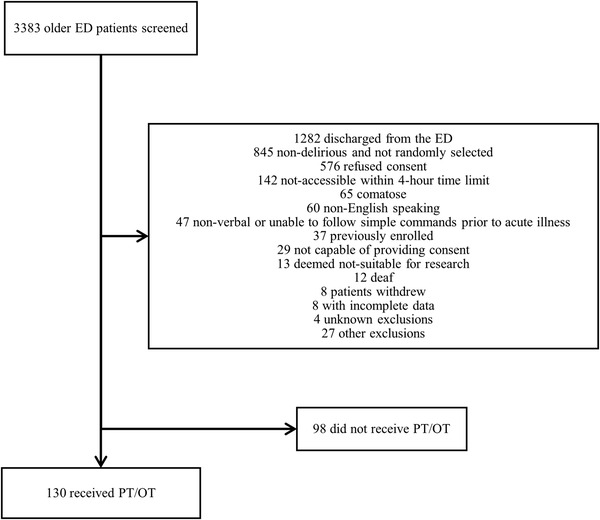
Enrollment flow diagram. ED, emergency department; PT, physical therapy. OT, occupational therapy
TABLE 1.
Participant characteristics (N = 130)
| Measure | Median (IQR) or n (%) |
|---|---|
| Age, years | 76 (63, 89) |
| Female sex | 80 (63) |
| Non‐White race | 16 (12) |
| Nursing home residence | 5 (3.89) |
| Prior dementia diagnosis | 76 (58.5) |
| Premorbid Older American Resources and Services Activities of Daily Living | 20 (6, 34) |
| Charlson Comorbidity Index | 3 (0, 10) |
| Acute Physiology Score | 13 (8, 18) |
| Delirium index | 5 (2, 9) |
| Central nervous system diagnosis during current admission | 31 (23.9) |
| Hospital length of stay | 5 (1, 9) |
| Admitted to the ICU | 24 (18.5) |
| Mechanically ventilated | 0 (0.0) |
Abbreviation: IQR, interquartile range.
Patients received a median (IQR) total PT/OT duration of 75 minutes (55, 105 minutes). The median (IQR) for log PT/OT intensity was 0.5% (0.3%, 0.9%), and the median (IQR) time to the first PT/OT session was 2 days (1, 3 days). Scatterplots for log PT/OT intensity and time to first PT/OT session are provided in Appendix Figures S1 and S2.
The OR (95% CI) for the multivariable proportional odds logistic regression can be seen in the Appendix Table. Log PT/OT intensity was significantly associated with a shorter ED delirium duration (adjusted OR, 0.39; 95% CI, 0.21–0.73) (Figure 2), but time to first PT/OT session was not (adjusted OR, 1.02; 95% CI, 0.82–1.27) (Figure 2). A proportional odds logistic regression was used and was adjusted for comorbidity burden (Charlson), illness severity (APS), baseline functional status (OARS ADL), prior dementia diagnosis, nursing home residence, and central nervous system diagnosis during current admission.
FIGURE 2.
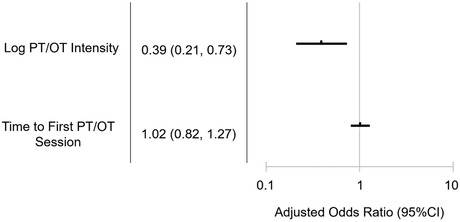
Forest plot of the adjusted odds ratios with their 95% confidence intervals (CIs) for physical therapy/occupational therapy (PT/OT) intensity and time to PT/OT on emergency department delirium duration
3.2. Sensitivity analyses
We performed several sensitivity analyses. We incorporated delirium severity as measured by the delirium index into the multivariable model. The adjusted ORs were 0.41 (95% CI, 0.22–0.79) and 0.92 (95% CI, 0.73–1.15) for log PT/OT intensity and time to first PT/OT session, respectively. We reran the model among participants who were delirious in the ED, and the adjusted ORs were 0.32 (95% CI, 0.15–0.69) and 1.16 (95% CI, 0.88–1.51), respectively. Next, we reran the model in a subset of the patients who were not admitted to the ICU, and our effect sizes did not change. The adjusted OR was 0.46 (95% CI, 0.24–0.89) for log PT/OT intensity and 1.03 (95% CI, 0.79–1.34) for time to first PT/OT session. Finally, we assessed if pre‐illness functional status and dementia modified the association between log PT/OT intensity and ED delirium duration. The pre‐illness OARS ADL × log PT/OT intensity interaction P value was 0.2351, and the pre‐illness dementia × log PT/OT intensity interaction P value was 0.7491, indicating that effect modification was unlikely. Because the time to the first PT/OT session was not significant, the effect modification was not examined for this exposure.
3.3. Limitations
This study had a few notable limitations. First, patients who received less PT/OT may have been more delirious, frail, and/or functionally impaired. Although we attempted to adjust for these covariates in the multivariable models, residual confounding likely exists. In addition, unmeasured confounders (eg, malnutrition, drug exposure during hospitalization) are also likely unaccounted for, further biasing our findings. Second, our study was limited to only patients aged ≥65 years and those who received PT/OT during their hospitalization. This study therefore may not be generalizable to younger patients or patients who did not receive PT/OT. Similarly, because all participants were from a single urban, academic, tertiary care hospital, the results may not be generalizable to other care centers. Third, it is possible that a patient with delirium in the ED had the delirium resolved before the first session of PT/OT, and this is an acknowledged weakness of our study. However, the median delirium duration was 2 days, making this scenario less likely. Fourth, we did not enroll patients on weekends or from 6:00 pm to 4:00 am, which could introduce selection bias if patients presenting at these times are different from those presenting during the enrollment times. Fifth, this was a secondary analysis, and a type 1 error (false‐positive finding) may have occurred. Conversely, our sample size was relatively small (N = 130), and the lack of association between time to the first PT/OT session and delirium duration have been secondary to a type II error (false negative finding). Sixth, almost all the PT/OT sessions were performed in the hospital setting and not the ED. This is not surprising given that PT/OT was ordered by the inpatient team and the time to first PT/OT session was 2 days. Consequently, our findings may not be generalizable to EDs that have access to PT/OT consultation. Finally, most EDs do not have access to PT/OT. However, in many US hospitals, inpatient boarding in the ED is a significant problem, and they have become de facto inpatient units. 24 If future randomized trials confirm our findings as well as find that time to first PT/OT session improves outcomes, this may prompt a change to have PT/OT readily available in the ED setting, especially if it reduces delirium duration, hospital length of stay, and overall costs.
4. DISCUSSION
The results of this study suggest that increasing PT/OT intensity during hospitalization may reduce delirium duration from ED presentation among older patients. We observed that higher intensity PT/OT was associated with a shorter ED delirium duration. Our data suggest that patients who are delirious in the ED may benefit from more intensive physical and/or occupational therapy. However, time to first PT/OT session (ie, the timeliness of PT/OT initiation) was not associated with delirium duration in the current study. Our study was exploratory. Future studies with larger sample sizes and randomized trial designs should confirm these findings and determine if higher intensity PT/OT improves delirium duration and mitigates its long‐term sequelae, such as accelerated cognitive and functional decline, among older patients. In addition, these studies should investigate if there is a minimum number of PT/OT hours (during the ED and hospital stays and postdischarge) to reduce delirium duration and long‐term outcomes while determining if there is a threshold of PT/OT duration in which its effect on outcomes plateaus. These studies should also examine if time to first session is modified by PT/OT intensity.
To our knowledge, this is the only study to assess the effect of PT and OT as a treatment for delirium in ED patients who are hospitalized. However, our results align with those of studies investigating the impact of PT/OT on delirium in ICU patients. One quality improvement project in the ICU care setting focused on improving mobilization and rehabilitation consultation frequency for patients with acute respiratory failure. 9 They found that the intervention led to a greater number of rehabilitation treatments and a significant reduction in the number of days delirious (21% days not delirious preintervention vs 53% days not delirious postintervention). 9 A randomized controlled trial evaluating delirium management in non–mechanically ventilated elderly patients in the ICU provided additional occupational therapy to the intervention group while the control group received standard delirium prevention. 10 The experimental group had shorter delirium duration (risk incidence ratios 0.15 vs 6.6) and lower incident delirium rates (3% vs 20%). 10 Schweickert et al evaluated a similar intervention in mechanically ventilated and critically ill patients. 8 They found that early exercise and mobilization via PT/OT led to a reduction in delirium duration by 2 days compared with the group who received the usual care therapy assigned by the primary team. 8 These studies provide evidence of the effectiveness of PT/OT on reducing delirium duration in ICU populations and suggest that similar effects may be achievable among older hospitalized adults.
We did not observe an association between time to first PT/OT session and ED delirium duration. However, PT/OT sessions were initiated a median of 2 full days after ED presentation. Because older hospitalized patients can rapidly lose their physiologic reserve within this short timeframe, 25 it is possible that an effect may have been observed if PT/OT was initiated earlier in the hospital course, such as in the ED. This is reflected in ICU‐based studies where PT/OT interventions initiated early in the hospital course seem to be effective, 8 whereas interventions started later did not show an effect. 26 , 27 Therefore, initiating intensive PT/OT as early as possible, such as in the ED, may potentiate its effect. This would align with the recent initiative to promote accredited geriatric EDs sponsored by the American College of Emergency Physicians that provide age‐friendly medical care known as the “4Ms”: what matters, medication, mentation, and mobility. 28
The benefits of PT/OT intervention on other outcomes, beyond delirium duration, have also been reported. Although acute hospitalization of older patients can lead to new or worsening functional impairment, 1 randomized controlled trial found that an exercise intervention reversed this effect. 29 Compared with the usual‐care group, the exercise intervention group was more likely to be functionally independent at hospital discharge. 29 The prior Schweickert et al randomized controlled trial reported similar results, with a PT/OT intervention leading to higher rates of return to pre‐illness functional status at hospital discharge compared with the control group. 8 Although this study found no difference in ICU length of stay (P = 0.08) and hospital length of stay (P = 0.93), 3 other prospective studies did show a significant reduction in both ICU and hospital length of stays with the implementation of a mobility intervention protocol. 9 , 30 , 31 In addition to the positive effects of physical activity on disease recovery, 32 these studies highlight the numerous benefits of exercise and mobility interventions during hospitalization.
In conclusion, increasing PT/OT intensity may reduce delirium duration in older ED patients who are admitted to the hospital and may be a potential intervention for delirium. Future studies should confirm this relationship between PT/OT intensity and delirium duration and further characterize it. Our study suggests that PT/OT intensity is an important factor in delirium reduction and, thus, also potentially improves long‐term outcomes for older patients.
AUTHOR CONTRIBUTIONS
Jin H. Han, E. Wesley Ely, and John F. Schnelle designed the original Delirium in the Emergency Department and Its Extension into Hospitalization (DELINEATE) study. James O. Jordano, Jin H. Han, and Sarah A. Welch designed the secondary analysis and completed data collection. Jin H. Han performed the statistical analysis. James O. Jordano and Jin H. Han wrote the primary manuscript draft. All authors provided substantial revisions.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
Supporting information
Supporting Information
Biography
James O. Jordano, BS, is an MD candidate at Vanderbilt University School of Medicine in Nashville, Tennessee, where he is pursuing a career in emergency medicine.

Jordano JO, Vasilevskis EE, Duggan MC, et al. Effect of physical and occupational therapy on delirium duration in older emergency department patients who are hospitalized. JACEP Open. 2023;4:e12857. 10.1002/emp2.12857
Meeting Presentations: This work was presented at the following: (1) Society of Academic Emergency Medicine Annual Meeting, New Orleans, LA, May 10–13, 2022, and (2) American Delirium Society Annual Conference, Indianapolis, IN, June 12–14, 2022.
Supervising Editor: Alexander X. Lo, MD, PhD.
See Editorial https://doi.org/10.1002/emp2.12900 by Alexander X. Lo in same issue.
REFERENCES
- 1. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911‐922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Han JH, Shintani A, Eden S, et al. Delirium in the emergency department: an independent predictor of death within 6 months. Ann Emerg Med. 2010;56(3):244‐252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16(3):193‐200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Han JH, Vasilevskis EE, Chandrasekhar R, et al. Delirium in the emergency department and its extension into hospitalization (DELINEATE) study: effect on 6‐month function and cognition. J Am Geriatr Soc. 2017;65(6):1333‐1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Breitbart W, Gibson C, Tremblay A. The delirium experience: delirium recall and delirium‐related distress in hospitalized patients with cancer, their spouses/caregivers, and their nurses. Psychosomatics. 2002;43(3):183‐194. [DOI] [PubMed] [Google Scholar]
- 6. Hshieh TT, Yang T, Gartaganis SL, Yue J, Inouye SK. Hospital elder life program: systematic review and meta‐analysis of effectiveness. Am J Geriatr Psychiatry. 2018;26(10):1015‐1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. AGS/NIA Delirium Conference Writing Group PC, Faculty . The American Geriatrics Society/National Institute on aging bedside‐to‐bench conference: research agenda on delirium in older adults. J Am Geriatr Soc. 2015;63(5):843‐852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373(9678):1874‐1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91(4):536‐542. [DOI] [PubMed] [Google Scholar]
- 10. Alvarez EA, Garrido MA, Tobar EA, et al. Occupational therapy for delirium management in elderly patients without mechanical ventilation in an intensive care unit: a pilot randomized clinical trial. J Crit Care. 2016;37:85‐90. [DOI] [PubMed] [Google Scholar]
- 11. Halawi MJ, Vovos TJ, Green CL, Wellman SS, Attarian DE, Bolognesi MP. Patient expectation is the most important predictor of discharge destination after primary total joint arthroplasty. J Arthroplasty. 2015;30(4):539‐542. [DOI] [PubMed] [Google Scholar]
- 12. Driessen MJ, Dekker J, Van Der Zee J, Lankhorst G. Occupational therapy in hospital based care in the Netherlands: a comparison of occupational therapy in general care (nursing homes, rehabilitation centres and general hospitals) and psychiatric care. Occup Ther Int. 1996;3(2):142‐156. [Google Scholar]
- 13. Dekker J, van Baar ME, Curfs EC, Kerssens JJ. Diagnosis and treatment in physical therapy: an investigation of their relationship. Phys Ther. 1993;73(9):568‐577. [DOI] [PubMed] [Google Scholar]
- 14. Han JH, Wilson A, Graves AJ, Shintani A, Schnelle JF, Ely EW. A quick and easy delirium assessment for nonphysician research personnel. Am J Emerg Med. 2016;34(6):1031‐1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McCusker J, Bellavance F, Cardin S, Belzile E. Validity of an activities of daily living questionnaire among older patients in the emergency department. J Clin Epidemiol. 1999;52(11):1023‐1030. [DOI] [PubMed] [Google Scholar]
- 16. McCusker J, Cole MG, Dendukuri N, Belzile E. The delirium index, a measure of the severity of delirium: new findings on reliability, validity, and responsiveness. J Am Geriatr Soc. 2004;52(10):1744‐1749. [DOI] [PubMed] [Google Scholar]
- 17. Holsinger T, Deveau J, Boustani M. Does this patient have dementia? JAMA. 2007;297(21):2391‐2404. [DOI] [PubMed] [Google Scholar]
- 18. Jorm AF. A short form of the informant questionnaire on cognitive decline in the elderly (IQCODE): development and cross‐validation. Psychol Med. 1994;24(1):145‐153. [DOI] [PubMed] [Google Scholar]
- 19. Murray SB, Bates DW, Ngo L, Ufberg JW, Shapiro NI. Charlson Index is associated with one‐year mortality in emergency department patients with suspected infection. Acad Emerg Med. 2006;13(5):530‐536. [DOI] [PubMed] [Google Scholar]
- 20. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818‐829. [PubMed] [Google Scholar]
- 21. Vasilevskis EE, Han JH, Hughes CG, Ely EW. Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol. 2012;26(3):277‐287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Springer; 2001. [Google Scholar]
- 23. Lee EC, Whitehead AL, Jacques RM, Julious SA. The statistical interpretation of pilot trials: should significance thresholds be reconsidered? BMC Med Res Methodol. 2014;14:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Medicine Io. Hospital‐based emergency care: at the breaking point. The National Academies Press; 2007. [Google Scholar]
- 25. Hirsch CH, Sommers L, Olsen A, Mullen L, Winograd CH. The natural history of functional morbidity in hospitalized older patients. J Am Geriatr Soc. 1990;38(12):1296‐1303. [DOI] [PubMed] [Google Scholar]
- 26. Morris PE, Berry MJ, Files DC, et al. Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure: a randomized clinical trial. JAMA. 2016;315(24):2694‐2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moss M, Nordon‐Craft A, Malone D, et al. A randomized trial of an intensive physical therapy program for patients with acute respiratory failure. Am J Respir Crit Care Med. 2016;193(10):1101‐1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Southerland LT, Lo AX, Biese K, et al. Concepts in practice: geriatric emergency departments. Ann Emerg Med. 2020;75(2):162‐170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Martínez‐Velilla N, Casas‐Herrero A, Zambom‐Ferraresi F, et al. Effect of exercise intervention on functional decline in very elderly patients during acute hospitalization: a randomized clinical trial. JAMA Intern Med. 2019;179(1):28‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Engel HJ, Needham DM, Morris PE, Gropper MA. ICU early mobilization: from recommendation to implementation at three medical centers. Crit Care Med. 2013;41(9):S69‐S80. [DOI] [PubMed] [Google Scholar]
- 31. Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238‐2243. [DOI] [PubMed] [Google Scholar]
- 32. Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801‐809. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


