Abstract
Physical distancing and face masks remain frontline prevention strategies due to suboptimal vaccine uptake and the highly infectious COVID-19 variants. Communities of color are disproportionately impacted by a chronic disease burden that places them at higher risk of severe COVID-19 disease. Therefore, they can greatly benefit from face mask use and physical distancing, especially if the individual(s) have not received the vaccine. We applied the Health Belief Model to explore barriers and motivators influencing physical distancing and face mask use among high-risk, Black American subgroups during the early COVID-19 pandemic stages. We conducted 62 semi-structured interviews among four Black American subgroups: young adults, individuals with underlying medical conditions, essential workers, and parents. Thematic analysis, guided by the Health Belief Model, yielded six themes: (1) Knowledge on Face Mask Use and Physical Distancing, (2) Perceived Susceptibility and Severity Varies by Subgroup, (3) Experience with and Perceived Self-Efficacy to Engage in Preventive Behavior, (4) Perceived Benefits to engaging in preventive behaviors, (5) Perceived Barriers to engage in preventive behaviors, and (6) Cues to action to increase participation. Each subgroup’s unique experience informed multilevel, tailored approaches that can be used by health promotion practitioners to improve face mask use and physical distancing among uniquely vulnerable Black American subgroups in the current and future pandemic.
Keywords: face mask use, physical distancing, social distancing, COVID-19, SARS-CoV-2, health communication, behavior change, disaster and emergency preparedness, cultural competence, health promotion, Black/African American, social determinants of health, behavior change theory, health equity, program planning and evaluation, health communication
The COVID-19 pandemic continues to disproportionately impact Black Americans and other racial/ethnic minority groups (Luck et al., 2022). Black Americans are almost four times more likely to be hospitalized and three times more likely to die compared with White Americans (Centers for Disease Control and Prevention [CDC], 2022). The vaccine remains the best preventive tool against COVID-19 (CDC, 2022), yet rates remain suboptimal. In July 2022, approximately 78% of the U.S. population had received one dose, but only 67% were fully vaccinated. Among Black Americans, only 49% received one dose and 43% were fully vaccinated (CDC, 2022). While perceptions and attitudes play a major role in uptake (Padamsee et al., 2022), inequities in social determinants of health (e.g., poor vaccine education and geographical access) exacerbate current vaccine rates (AlShurman et al., 2021). Therefore, face mask use and physical distancing remain important in the comprehensive strategy to mitigate the spread of COVID-19.
Face mask use and physical distancing have been investigated across several studies, and many were inclusive of Black Americans (Jimenez et al., 2021; O’ Conor et al., 2020). In a national study, Block et al. (2020) found that 67% of Black Americans stayed at least 6 feet away from others in public, and 65% wore a mask when outside and around others. Kahn and Money (2021) also found that African Americans were more likely to report mask-related social identity threats from the public and police compared with White Americans. This led to police avoidance or decreased face mask use in the early pandemic phases. Subgroups of Black Americans are uniquely vulnerable to COVID-19, and their attitudes toward face mask use and physical distancing warrant being studied. Young adults are less likely to get vaccinated yet have a history of engaging in high-risk behaviors (Dai et al., 2022). Individuals with underlying medical conditions (UMC) are at increased risk of severe COVID-19 disease, and vaccine efficacy is lower compared to immunocompetent individuals (Galmiche et al., 2022). Minority children, including Black children, are more likely to die from COVID-19 compared with White children (Feldstein et al., 2021). Essential workers have high-risk jobs in which Black Americans and Latinos are overrepresented (Hawkins, 2020). Investigating these subgroups’ perspectives on face mask use and physical distancing is necessary to inform tailored, public health prevention strategies.
Few studies have explored factors associated with face mask use and physical distancing among Black American subgroups. Among individuals with UMCs, O’Conor et al. (2020) reported Black adults were less likely to practice physical distancing compared with White adults during the pandemic onset. Essential workers were also less likely to report face mask use and physical distancing compared with their counterparts (Roberts et al., 2020). In addition, Heerman et al. (2022) found that Black parents’ health care access and health behaviors were associated with fear, anxiety, and stress. They also had major disruptions in their daily activities. Parents across all communities found it challenging to educate their children about preventive behaviors (Esposito & Principi, 2020). In conjunction, Black and Asian young adults reported increased COVID-19 victimization and negative effects on their mental health compared with their peers (Fisher et al., 2022). Yet, little to no information is known about Black young adults’ experience with preventive behaviors. To our knowledge, few qualitative studies (Jimenez et al., 2021) have provided a deeper understanding of knowledge and attitudes toward facemask use and physical distancing among uniquely vulnerable Black American subgroups.
The Health Belief Model (HBM) is used to guide and test public health interventions by considering the motivating factors that shape behavior, including perceived confidence to act (i.e., self-efficacy) and modifying factors (e.g., knowledge; Glanz et al., 2008). It states individuals are more likely to engage in behaviors when: (1) perceived susceptibility to disease exists; (2) the outcomes related to the disease are perceived severe; and (3) perceived benefits associated with the behavior outweigh the risks of taking action. A few studies have used the model to explore COVID-19 intervention strategies (Alagili & Bamashmous, 2021; Callow et al., 2020). For example, in a cross-sectional study among older adults, a major finding by Callow and colleagues (2020), was perceived severity of COVID-19 and perceived benefits of physical distancing positively impacted attitudes toward physical distancing while perceived barriers negatively impacted attitudes toward physical distancing. Alagili and Bamashmous (2021) similarly found that perceived benefits, perceived barriers, and cues to action were associated with adherence to COVID-19 preventive behaviors in a cross-sectional study among adults.
The objective of this study was to explore perceptions and attitudes toward face mask use and physical distancing in the early onset of the COVID-19 pandemic among uniquely vulnerable Black American subgroups. Each subgroup’s unique experience will inform multilevel, tailored approaches to improve face mask use and physical distancing in the current and future pandemic.
Method
Study Design, Sample, and Recruitment
We used a phenomenological, qualitative study design to explore attitudes and practices related to face masks and physical distancing among a purposive sample of Black Americans in the United States during the first 6 months of the pandemic. We aimed to recruit a minimum of 60 participants, or 15 per subgroup. Across studies, six to 12 interviews are a necessary number of participants to reach saturation (Hagaman & Wutich, 2017). According to Creswell (1998), a qualitative, phenomenological study requires up to 10 long interviews to reach saturation. Recruitment strategies included email, existing databases, word-of-mouth, and flyers. Participants were either contacted from an existing database of participants who agreed to participate in follow-up studies, or they contacted the research team using the contact information on the flyer.
An individual was excluded if they did not meet the following inclusion criteria: (1) English-speaking; (2) Black; (3) older than 18 years; and (4) a member of the following subgroups: parent with a child under 18, young adult (age 18–30), individual with a UMC, or an essential worker. An individual with an UMC has a condition such as cancer or sickle cell disease that increases susceptibility to severe COVID-19 disease (Galmiche et al., 2022). We sought a range of medical conditions (e.g., lung diseases, cardiovascular diseases, autoimmune diseases) to understand the experiences of people living with chronic diseases during the pandemic and highlighted their unique issues or concerns with wearing a face mask and physical distancing. The U.S. Department of Homeland Security (2020) states an essential worker “conducts a range of operations and services that are typically essential to continue critical infrastructure operations.” Examples included teachers, food service workers, public health and medical professionals, and public service workers. This study was approved by the Institutional Review Board at Meharry Medical College.
Procedures
Data collection took place between July and September 2020. Before the interview, participants completed a brief, sociodemographic screener. Verbal consent was obtained before the interviews, which lasted 45 to 90 min. The facilitator’s guide queried participants’ level of engagement in physical distancing and face mask adherence along with facilitators, barriers, and strategies to increase use. Each participant received a US$30 e-gift card. All sessions were audio-recorded and transcribed using the online, video conferencing platform Zoom. The research team listened to the audio while reviewing the transcript to ensure accuracy. Data analysis was conducted after all interviews were completed.
Analysis
SPSS version 28 software was used to conduct frequencies, percentages, cross-tabulations, and analysis of variance on survey data. Inductive, thematic analysis was used to analyze qualitative, interview data. Senior author J.C.E., a trained qualitative researcher, first created a priori codes guided by the HBM and the literature studying face mask use and physical distancing across populations. Three trained team members used the a priori codes to code transcripts. See Table 1 for the applied definition of each construct. Emerging codes were added to the listing until coding saturation was met. Each code was put into a category (i.e., axial coding). Codes were then compared and a consensus was reached on discrepancies. Themes were developed using the existing codes and categories. Rigor was established using peer debriefing, in which one outside researcher trained in qualitative research reviewed and provided feedback on the methodology including the interview protocol at the design stage. This individual also provided feedback on how the results were presented in the article. We also used rich, thick descriptions of the data including interviewee quotes to provide a detailed account of patterns and context of the cultural and social relationships influencing the engagement of preventive behavior among uniquely vulnerable Black American subgroups.
Table 1.
Health Belief Model Construct Definitions
| Behavioral theory | Construct | Brief definition |
|---|---|---|
| Health Belief Model | Perceived susceptibility | Beliefs regarding the chance of getting SARs-CoV-2 (i.e., virus that causes COVID-19) |
| Perceived severity | Beliefs regarding how serious the consequences of COVID-19 | |
| Perceived benefits | Beliefs regarding the efficacy of face masks and physical distance to reduce the risk or seriousness of COVID-19 | |
| Perceived barriers | Beliefs regarding the tangible and psychological costs of wearing facemask and physical distancing | |
| Cues to action | Strategies to activate an individual’s readiness for face mask use and physical distancing to reduce the risk of COVID-19 | |
| Self-efficacy | An individual’s confidence in their ability to wear face mask and practice physical distancing to overcome barriers to reduce the risk of COVID-19 |
Source: Adapted from Glanz et al. (2008).
Results
We conducted 62 semi-structured interviews. See Table 2 for demographics. When exploring sociodemographics by preventive behavior, there was a significant difference in face mask use by gender (χ2 = 5.367; p = .021) and a marginally significant difference in physical distancing by subgroup (F = 3.804; p = .056; Results not shown). We describe six HBM-related themes and the Supplementary File provides sample quotes from participants by subgroup and behavior.
Table 2.
Sociodemographics by Face Mask-Wearing and Physical Distancing, N = 62
| Face masks yes, all the time | Face masks yes, sometimes/None | Physical distance yes, all the time | Physical distance yes, sometimes/none | |||||
|---|---|---|---|---|---|---|---|---|
| Participant Characteristics | M | SD | M | SD | M | SD | M | SD |
| Age | 41.30 | 14.69 | 36.08 | 10.56 | 43.63 | 14.94 | 35.96 | 11.74 |
| N | % | N | % | N | % | N | % | |
| Gender | ||||||||
| Male (N = 19) | 12 | 24.0 | 7 | 58.3 | 10 | 28.6 | 9 | 33.3 |
| Female (N = 33) | 38 | 76.0 | 5 | 41.7 | 25 | 71.4 | 18 | 66.7 |
| Category | ||||||||
| Essential Worker (N = 16) | 13 | 26.0 | 3 | 25.0 | 10 | 28.6 | 6 | 22.2 |
| Underlying Medical Condition (N = 15) | 14 | 28.0 | 1 | 8.3 | 13 | 37.1 | 2 | 7.4 |
| Young Adults (N = 15) | 9 | 18.0 | 6 | 50.0 | 5 | 14.3 | 10 | 37.0 |
| Parents (N = 16) | 14 | 28.0 | 2 | 16.7 | 7 | 20.0 | 9 | 33.3 |
| Education | ||||||||
| Some College or less (N = 22) | 15 | 30.0 | 7 | 58.3 | 12 | 34.3 | 10 | 37.0 |
| Associates Degree or more (N = 40) | 35 | 70.0 | 5 | 41.7 | 23 | 65.7 | 17 | 63.0 |
| Income | ||||||||
| Less than $40,000 (N = 20) | 15 | 30.0 | 5 | 41.7 | 9 | 25.7 | 11 | 40.7 |
| $40,001-$80,000 (N = 17) | 15 | 30.0 | 2 | 16.7 | 11 | 31.4 | 6 | 22.2 |
| More than $80,000 (N = 16) | 13 | 26.0 | 3 | 25.0 | 9 | 25.7 | 7 | 25.9 |
| Do not want to answer (N = 9) | 7 | 14.0 | 2 | 16.7 | 6 | 17.1 | 3 | 11.1 |
Note. Race/Ethnicity demographics are not included in Table 2, as 100% of the study sample was Black Americans. There was a significant difference in face mask use by gender (p = .021).
Theme 1: Knowledge of Face Mask Use and Physical Distancing
Most participants across subgroups defined physical distance as the minimum distance of 6 feet between individuals. They also emphasized that small or closed public spaces should be avoided along with touching others. In addition, many stated physical distancing required wearing a face mask in public. Using a face mask was defined as wearing a mask that covered the mouth and nose, and wearing a face mask below the nose was not the proper use. Many also discussed the different types of mask styles and materials.
Theme 2: Perceived Susceptibility and Severity Varies by Subgroups
Overall, the degree of perceived susceptibility and severity of COVID-19 disease while engaging in these behaviors varied by subgroup. Most participants perceived these behaviors as strategies to lower their risk of contracting, being hospitalized, and/or dying from COVID-19. Hence, they were viewed as protective behaviors to “flatten the curve.” A few participants were skeptical of the ability of face masks to lower COVID-19 transmission. This was due to the limited guidance from public health officials about the effectiveness of specific materials and optimal mask styles. Young adults cited they were less concerned about the severity of SARS-CoV-2 if they did not wear a mask compared with other subgroups. As a result, most stated that it was a personal choice and continued engagement with their social circles without mask use. Some parents were unsure or perceived their children as low risk and did not need a mask based on the media and public health guidance.
For physical distancing, mostly parents and those with a UMC expressed minimizing activities that placed them and/or their household at higher risk. They were content with staying home and engaging in routine preventive practices (e.g., respecting personal space and hand washing). They also expressed the desire for other community members to take the pandemic seriously and engage in these behaviors to demonstrate empathy. They specifically stated they were perplexed by the behaviors of their family, coworkers, and/or government officials when they blatantly disregarded public health guidance through acts of selfishness in their decision-making.
Subsequently, many participants from all subgroups had empathy for individuals who continued to physically engage with their close social group due to mental health issues (e.g., depression or anxiety) caused by the pandemic despite the risk. However, there were negative connotations associated with people who blatantly disregarded the safety precautions and jeopardized the community’s health. They were viewed as “selfish,” “disrespectful,” “privileged,” “dirty,” “protecting their constitutional rights,” or having a particular political ideology due to government officials’ stance on COVID-19 issues.
Theme 3: Experiences and Perceived Self-Efficacy to Engage in Preventive Behavior
Physical distancing and wearing face masks had positive and negative effects on participants’ home and work lives. Participants across subgroups described using the time at home to work on personal projects and professional goals. However, this increased household tension and frustration in some instances. As a result, people spent more time in their own spaces or only interacted during certain times (e.g., mealtime). For face masks, all participants expressed difficulty in securing face masks for themselves and/or child(ren) in the initial pandemic stages. Participants either used materials in their homes (e.g., handkerchiefs) to make masks or acquired them from family and friends. However, as mask access and variety increased, many observed more improper mask use (i.e., mask-wearing below the nose) or use of masks that were perceived as ineffective.
For face mask adherence by subgroup, many essential workers stated their job required and/or provided face masks. Nonetheless, they complained some coworkers did not comply with the requirement or they only complied when management was present. Comparatively, parents’ experiences were characterized by their interactions with their children. For example, a few discussed educating their children about the proper use and appropriate time to not wear a mask (e.g., lunch), especially when they were at school. Some parents found that their children often reminded them about the proper etiquette of physical distancing and face mask use. In addition, a few participants with a UMC expressed wearing face masks in their home or placing themselves in a “silo” or isolated environment, practices developed prepandemic. Conversely, most young adults stated they could access masks but admitted they did not always wear them as they had a “trusted” circle of friends or did not worry about COVID-19. A few young adults stated they took wearing a mask more seriously around individuals who were concerned about contracting COVID-19 or were at higher risk of serious disease.
For physical distancing by subgroups, participants with a UMC continued to interact with people who practiced physical distancing or stayed in their “silo” due to essential workers in the home. Parents and their children transitioned to virtual learning which had both positive and negative effects on their child’s schooling and also on parents’ work–life balance. Students experienced falling behind due to the need for one-on-one teaching or accelerating because they could focus more while at home. Parents discussed finding a work routine that allowed them to balance their job obligations and manage their children’s schoolwork. Also, essential workers stated the lack of physical distancing created fear of contracting COVID-19. For example, teachers struggled with limiting physical interaction with small children as they like to display affection through physical touch. Contrarily, some young adults did not and were unwilling to follow the physical distancing guidelines. All participants in each subgroup perceived physical distancing as difficult because it forced isolation from loved ones and their community. Many varied in their degree of willingness to risk COVID exposure for social interaction. However, a few acknowledged COVID-19 risks could not be avoided due to health care necessities, socialization desires, and/or living in a multigenerational home.
Theme 4: Perceived Benefits of Engaging in Preventive Behavior
Lowering COVID-19 transmission and mortality rates were motivating factors to practice physical distancing and face mask use across all subgroups. Many wanted to protect themselves from COVID-19 and health-related complications. Participants were concerned about the long-term effects of COVID-19 and its lasting effect on their well-being. They, especially essential workers, wanted to protect their community including family members, social networks, and vulnerable populations (i.e., older adults and those with a UMC). Young adults particularly wanted to protect their family members by physical distancing as they were still engaging in high-risk behaviors. Finally, many perceived a long-term benefit would include being able to return to “normal” once cases decreased.
Theme 5: Perceived Barriers to Engage in Preventive Behavior
The meaning of “social” distancing was unclear to a few participants due to poor communication from political and government officials. Some mentioned the term had a “negative connotation” within the community. Numerous participants from all subgroups were unable to practice physical distance due to multigenerational households and the desire/need for social engagement and support. Others expressed that physical distancing was detrimental to their relationships and mental health. Participants across subgroups admitted they continued to physically interact with their social group(s). Furthermore, some participants perceived the selfishness of others to not have physical distance as a significant barrier.
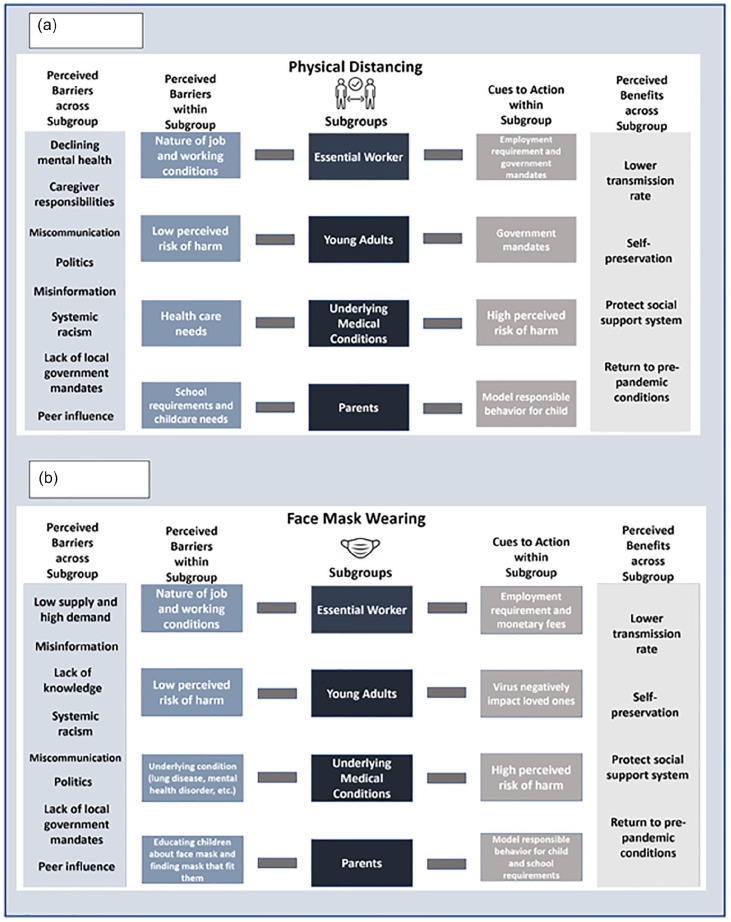
All participants expressed a lack of access to masks in the early pandemic stage. When masks became available, the “fit” of the mask became an issue. A few participants with UMC such as asthma, claustrophobia, or sensitive skin had issues with wearing a mask for long periods of time. There was fear of “breathing in too much carbon dioxide.” Some participants discussed how masks interfered with their daily activities or work duties (e.g., foggy glasses, too hot, breathing difficulty). Some participants discussed the negative connotations associated with wearing a face mask (i.e., perceived as “super safe” or an “uncomfortable safe person”). This dictated the way people interacted with their families and support systems. In addition, participants, specifically young adult males and parents with boys, were also concerned about racial profiling (i.e., harassment by police during face mask use in public). They described how the murder of George Floyd heightened their fear of mask-wearing, especially when recalling the countless other lives lost when racially profiled. The Black Lives Matter protests exacerbated their decreased trust levels in the police and criminal law system. Specifically, participants stated their distrust of law enforcement was due to a history of structural and institutional racism in the form of police brutality and unjust enforcement of laws. In that instance, the risk of wearing a mask in public outweighed the benefits because they perceived an experience with the police as more deadly than COVID-19. Other barriers included the politicization of face masks and inconsistent messaging by government officials. Figure 1 summarizes the benefits and barriers of engagement in these behaviors across subgroups.
Figure 1.
Perceived Benefits, Cues to Action and Barriers to Physical Distancing and Face Mask Use Within and Across Black American Subgroups. Figure 1a highlights barriers and motivators to physical distancing within and across each subgroup. Figure 1b explores motivators and barriers to face mask use within and across each subgroup.
Theme 6: Cues to Action to Increase Participation
Many participants cited the need for tailored education on the benefits of face mask use and physical distancing. Some participants also wanted to know how to identify appropriate masks or engage in physical distancing techniques in indoor and outdoor environments. Participants, especially parents and those with UMCs, wanted the term “physical distancing” to replace “social distancing” so the language would reflect the action being recommended and avoid confusion. In addition, parents were also motivated by their children to be good role models because they wanted them to understand the seriousness of the pandemic. Those with UMCs highlighted understanding their increased risk of severe disease was a cue to action. For face mask adherence, a recommendation was to offer fines for those who did not comply with mandates. In addition, many stated job requirements were a cue to action. In addition, young adults and those with a UMC mentioned government mandates and recommendations from trusted sources as motivating factors.
Discussion
In the early pandemic stages, participants across subgroups reported they understood the meaning of physical distancing and how to wear facemasks. The majority of participants also reported wearing facemasks and physical distancing all the time with men being less likely to wear masks. This is consistent with a study by Czeisler et al. (2020) where the majority of Americans supported physical distancing (88%) and stay-at-home ordinances (80%) in May 2020. Weiss and Paasche-Orlow (2020) also found that African Americans were the least knowledgeable about COVID-19-related topics including preventive behaviors in the early pandemic stages; however, they were more likely to engage in preventive behaviors compared with White Americans. This study also noted differences across education and income irrespective of race. However, our study found no significant difference in education or income by facemask use or physical distancing. These findings suggest other factors (e.g., communication) could be influential in engagement in these preventive behaviors.
Most participants perceived themselves as susceptible to COVID-19 and understood the severity of the disease. They also highlighted the effectiveness of face mask use and physical distancing in prevention. This supports their positive views toward physical distancing and facemask use although physical distancing specifically strained relationships. Bateman et al. (2021) found similar results stating physical distancing had harmful effects on mental health and stress management in the Black community in the early pandemic stages. Our results also shed light on the mental toll associated with facemasks and physical distancing across subgroups. Peer pressure and racial discrimination were commonly cited as emotional factors, especially in young adults, influencing their decision to wear a facemask and practice physical distancing. Fisher et al. (2022) study further found that heightened systemic racism and victimization linked to the COVID-19 pandemic increased depression and anxiety in racial minority young adults.
All subgroups perceived their self-efficacy to access masks and engage in physical distancing as difficult in the early pandemic stage. However, access to facemasks improved over time. A new yet unsurprising finding was those with UMC were more apt to wear facemasks and physically distance themselves compared with other subgroups although some may experience more issues related to breathing or anxiety. At the same time, young adults were more willing to engage in higher-risk activities (e.g., no facemask use in subgroups) similar to the study by Lou et al. (2021). Of interest, many participants and/or families had limited access to masks. They described how they either had people in their social circle provide masks or they bought or made masks for their family. This reflects collectivism, which places more emphasis on relationships (e.g., family) and their interconnectedness and not the individual (Lukwago et al., 2001; White & Parham, 1990). In our study, young adults displayed behavior that may suggest they perceive the individual as more important but understood the importance of physical distancing from loved ones due to their behaviors.
Worldwide collectivism was displayed during the Black Lives Matter Movement in the summer of 2020 due to the murder of George Floyd by police. Black families witnessed rampant racism, particularly racial profiling, which was a commonly cited barrier to facemask use among young male adults and parents with sons. Christiani et al. (2022) confirmed these findings by demonstrating Black people perceived wearing particular types of masks (i.e., bandanas or homemade clothes) as threatening to their life due to the racial climate. Kajeepeta et al. (2022) found that police in New York City targeted African Americans more when they enforced mask mandates in the summer of 2020 similar to “stop and frisk” outcomes. It resulted in higher COVID-19 criminal court summonses along with public health and nuisance arrests for African Americans. This speaks to the larger conversation about the need to combat racism in the fight to increase adherence to mask and physical distancing.
Strengths and Limitations
A major strength is this study evaluates the perspective of physical distancing and face mask use among vulnerable, Black American subgroups to develop effective, grass-root strategies to increase engagement and adherence. However, this study does have limitations. First, the data cannot be generalized to the entire Black community. Second, this study does not capture lived experiences of all subgroups within the Black community (i.e., older people and children). Third, opinions might have changed over time with changes in the stages of the pandemic so views may not reflect current opinions. Last, researcher bias can distort data analysis and interpretation; however, our research protocol implemented techniques (i.e., investigator triangulation, subgroup consensus) to minimize interference.
Implications for Practice
Table 3 provides recommendations to increase face mask use and physical distancing among Black Americans. Participants acknowledged the significance of practicing physical distancing and wearing a facemask in public spaces. However, many multilevel factors contributed to their adherence to public health mandates. At the individual and interpersonal levels, participants: (a) varied in knowledge levels and opinions about facemasks; (b) were influenced by politics, and (c) feared being shamed by their social circle. Friends, coworkers, and family were some of the biggest influences on behavior in our study. Future efforts should focus on addressing negative aspects of face mask use and physical distancing to increase acceptability while promoting a culture of empathy and respect of choice. Research should quantitatively explore face mask use and physical distancing among these uniquely vulnerable groups. In addition, research efforts should explore content, preferred sources, and channels to provide this information to the Black community, and investigate if educational and accessible needs differ by subgroup.
Table 3.
Recommendations to Increase Face Masks Use and Physical Distancing Among Black Americans
| • [Individual Level] Increase acceptability of face mask use and physical distancing. Increase access to face mask use via outreach. • [Interpersonal Level] Promote empathy and respect from family, peers, and colleagues and not “mask-shaming” or pressure to socialize as it relates to engagement in face mask use and physical distancing. • [Community Level] Mobilize the public health workforce (researchers, healthcare workers, and community-based organizations, etc.) to educate communities on COVID-19-related topics including transmission, prevention, and disparities in health outcomes to understand COVID-19 risks and potential health outcomes with scenarios representing each subgroup. • [Community Level] Train frontline workers (e.g., police officers, health care providers) on trauma-informed and restorative justice practices to engage communities, especially during pandemics or other public health crises, with the intent to reduce harm and maximize the effect. • [Policy Level] Advocate for policy development and/or change that promotes equity in social determinants of health and antiracism in public health and healthcare. The political climate and systemic factors such as racism and socioeconomic status must be considered when recommendations are being drafted. Potential target areas include, but are not limited to: ○ Allot funding to dispense masks at places such as schools, jobs, colleges, and healthcare offices. ○ Develop community health worker programs to educate the community on face mask etiquette and physical distancing in multigenerational housing. ○ Invest in public health research to further explore strategies to increase engagement in facemask use, physical distancing, and other preventive behaviors ○ Mobilize grass-root organizations and local businesses to dispense masks. ○ Increase livable wages to financially access masks or provide free access to masks. ○ Encourage mask mandates and strategies to promote physical distancing in social spaces. |
The COVID-19 pandemic continues to demonstrate why a well-funded and diverse public health workforce is critical to implementing an equitable yet fair public health response. A public health workforce may include, but is not limited to, local and state public health departments, community-based organizations, community health workers, and public health researchers. On the community level, each plays a key role in collecting and disseminating information about disease prevention, transmission, and health disparities. Our study highlights the need for tailored, meaningful outreach and communication to high-risk populations or subgroups to increase adherence to facemask use and physical distancing in the Black community. Any plan should include a trauma-informed approach, which involves community involvement and feedback to maximize positive behavior change and reduce unintended harm and distrust.
Policy determines public health funding and influences the mobilization of community resources, such as access to facemasks. As aforementioned, mask mandates and physical distancing guidance were implemented during the onset of the pandemic and proved to be effective measures to reduce cases, hospitalizations, and deaths. However, the Black community still faced significant barriers due to the impact structural and institutional racism have on other determinants of health (e.g., low-paying wages, lack of access to quality health care, being unhoused, police violence, and medical distrust). Policy development and change, rooted in the data and stories of the communities they are designed to protect, will contribute to increasing adherence to facemasks and physical distancing. Efforts to eradicate inequities should also result in antiracist policies that address social determinants of health (e.g., education, criminal law, and health care).
Supplemental Material
Supplemental material, sj-docx-1-hpp-10.1177_15248399221151176 for Understanding Physical Distancing and Face Mask Use Across High-Risk African American Subgroups During the COVID-19 Pandemic: Application of Health Belief Model by Jamal Moss, Leah Alexander, Iman Barré, Imari Parham, Taneisha Gillyard, Jamaine Davis and Jennifer Cunningham-Erves in Health Promotion Practice
Footnotes
Authors’ Note: The authors would like to thank the members of the African American community for their valuable insights on their lived experiences during the COVID-19 pandemic. This work was supported by the National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA) (Award Number: 5UL1TR0002243-03).
Consent to Participate: Informed consent was obtained from all study participants.
Data Availability Statement: Due to the confidentiality agreements, supporting data cannot be made openly available.
ORCID iD: Jennifer Cunningham-Erves  https://orcid.org/0000-0002-7780-9874
https://orcid.org/0000-0002-7780-9874
Supplemental Material: Supplemental material for this article is available online at https://journals.sagepub.com/home/hpp.
References
- Alagili D. E., Bamashmous M. (2021). The Health Belief Model as an explanatory framework for COVID-19 prevention practices. Journal of Infection and Public Health, 14(10), 1398–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AlShurman B. A., Khan A. F., Mac C., Majeed M., Butt Z. A. (2021). What demographic, social, and contextual factors influence the intention to use COVID-19 vaccines: A scoping review. International Journal of Environmental Research and Public Health, 18(17), Article 9342. 10.3390/ijerph18179342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateman L. B., Schoenberger Y. M., Hansen B., Osborne T. N., Okoro G. C., Speights K. M., Fouad M. N. (2021). Confronting COVID-19 in under-resourced, African American neighborhoods: A qualitative study examining community member and stakeholders’ perceptions. Ethnicity & Health, 26(1), 49–67. 10.1080/13557858.2021.1873250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block R., Jr., Berg A., Lennon R. P., Miller E. L., Nunez-Smith M. (2020). African American adherence to COVID-19 public health recommendations. Health Literacy Research and Practice, 4(3), e166–e170. 10.3928/24748307-20200707-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callow M. A., Callow D. D., Smith C. (2020). Older adults’ intention to socially isolate once COVID-19 stay-at-home orders are replaced with “safer-at-home” public health advisories: A survey of respondents in Maryland. Journal of Applied Gerontology, 39(11), 1175–1183. 10.1177/0733464820944704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2022). CDC covid data tracker. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic
- Christiani L., Clark C., Greene S., Hetherington M., Wager E. (2022). Masks and racial stereotypes in a pandemic: The case for surgical masks. The Journal of Race, Ethnicity, and Politics, 7, 185-202. 10.1017/rep.2021.9 [DOI] [Google Scholar]
- Creswell J. (1998). Qualitative inquiry and research design: Choosing among five traditions. SAGE. [Google Scholar]
- Czeisler M. É., Tynan M. A., Howard M. E., Honeycutt S., Fulmer E. B., Kidder D. P., Robbins R., Barger L. K., Facer-Childs E. R., Baldwin G., Rajaratnam S., Czeisler C. A. (2020). Public attitudes, behaviors, and beliefs related to COVID-19, stay—at—home orders, nonessential business closures, and public health guidance—United States, New York City, and Los Angeles, May 5-12, 2020. MMWR: Morbidity and Mortality Weekly Report, 69(24), 751–758. 10.15585/mmwr.mm6924e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H., Barrington-Trimis J. L., Unger J. B., Baezconde-Garbanati L., Leventhal A. M. (2022). Patterns and mediators of racial and ethnic disparities in COVID-19 vaccine hesitancy among young adults. Preventive Medicine, 159, Article 107077. 10.1016/j.ypmed.2022.107077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito S., Principi N. (2020). To mask or not to mask children to overcome COVID-19. European Journal of Pediatrics, 179(8), 1267–1270. 10.1007/s00431-020-03674-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldstein L. R., Tenforde M. W., Friedman K. G., Newhams M., Rose E. B., Dapul H., Soma V. L., Maddux A. B., Mourani P. M., Bowens C., Maamari M., Hall M. W., Riggs B. J., Giuliano J. S., Jr., Singh A. R., Li S., Kong M., Schuster J. E., McLaughlin G. E., . . . Overcoming COVID-19 Investigators. (2021). Characteristics and outcomes of U.S. children and adolescents with multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. Journal of the American Medical Association, 325(11), 1074–1087. 10.1001/jama.2021.2091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher C. B., Tao X., Yip T. (2022). The effects of COVID-19 victimization distress and racial bias on mental health among AIAN, Asian, Black, and Latinx young adults. Cultural Diversity & Ethnic Minority Psychology. Advance online publication. 10.1037/cdp0000539 [DOI] [PubMed]
- Galmiche S., Luong Nguyen L. B., Tartour E., de Lamballerie X., Wittkop L., Loubet P., Launay O. (2022). Immunological and clinical efficacy of COVID-19 vaccines in immunocompromised populations: A systematic review. Clinical Microbiology and Infection, 28(2), 163–177. 10.1016/j.cmi.2021.09.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K., Rimer B. K., Viswanath K. (2008). Health behavior and health education: Theory, research and practice. Jossey-Bass. [Google Scholar]
- Hagaman A. K., Wutich A. (2017). How many interviews are enough to identify metathemes in multisited and cross-cultural research? Another perspective on Guest, Bunce, and Johnson’s (2006) landmark study. Field Methods, 29(1), 23–41. 10.1177/1525822X16640447 [DOI] [Google Scholar]
- Hawkins D. (2020). Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. American Journal of Industrial Medicine, 63(9), 817–820. 10.1002/ajim.23145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heerman W. J., Gross R., Lampkin J., Nmoh A., Eatwell S., Delamater A. M., Sanders L., Rothman R. L., Yin H. S., Perrin E. M., Flower K. B. (2022). How COVID-19 impacted child and family health and healthcare: A mixed-methods study incorporating family voices. Translational Behavioral Medicine, 12(3), 466–479. 10.1093/tbm/ibab166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez M. E., Rivera-Núñez Z., Crabtree B. F., Hill D., Pellerano M. B., Devance D., Macenat M., Lima D., Martinez Alcaraz E., Ferrante J. M., Barrett E. S., Blaser M. J., Panettieri R. A., Jr., Hudson S. V. (2021). Black and Latinx community perspectives on COVID-19 mitigation behaviors, testing, and vaccines. JAMA Network Open, 4(7), Article e2117074. 10.1001/jamanetworkopen.2021.17074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn K. B., Money E. E. L. (2021). (Un)masking threat: Racial minorities experience race-based social identity threat wearing face masks during COVID-19. Group Processes & Intergroup Relations, 25(4), 871–891. 10.1177/1368430221998781 [DOI] [Google Scholar]
- Kajeepeta S., Bruzelius E., Ho J. Z., Prins S. J. (2022). Policing the pandemic: Estimating spatial and racialized inequities in New York City police enforcement of COVID-19 mandates. Critical Public Health, 32(1), 56–67. 10.1080/09581596.2021.1987387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luck A. N., Preston S. H., Elo I. T., Stokes A. C. (2022). The unequal burden of the Covid-19 pandemic: Capturing racial/ethnic disparities in US cause-specific mortality. SSM—Population Health, 17, Article 101012. 10.1016/j.ssmph.2021.101012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukwago S. N., Kreuter M. W., Bucholtz D. C., Holt C. L., Clark E. M. (2001). Development and validation of brief scales to measure collectivism, religiosity, racial pride, and time orientation in urban African American women. Family & Community Health, 24(3), 63–71. 10.1097/00003727-200110000-00008 [DOI] [PubMed] [Google Scholar]
- Luo Y., Cheng Y., Sui M. (2021). The Moderating Effects of Perceived Severity on the Generational Gap in Preventive Behaviors during the COVID-19 Pandemic in the U.S. International journal of environmental research and public health, 18(4), 2011. 10.3390/ijerph18042011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’ Conor R., Opsasnick L., Benavente J. Y., Russell A. M., Wismer G., Eifler M., Marino D., Curtis L. M., Arvanitis M., Lindquist L., Persell S. D., Bailey S. C., Wolf M. S. (2020). Knowledge and behaviors of adults with underlying health conditions during the onset of the COVID-19 U.S. Outbreak: The Chicago COVID-19 Comorbidities Survey. Journal of Community Health, 45(6), 1149–1157. 10.1007/s10900-020-00906-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padamsee T. J., Bond R. M., Dixon G. N., Hovick S. R., Na K., Nisbet E. C., Wegener D. T., Garrett R. K. (2022). Changes in COVID-19 vaccine hesitancy among Black and White individuals in the U.S. JAMA Network Open, 5(1), Article e2144470. 10.1001/jamanetworkopen.2021.44470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts J. D., Dickinson K. L., Koebele E., Neuberger L., Banacos N., Blanch-Hartigan D., Welton-Mitchell C., Birkland T. A. (2020). Clinicians, cooks, and cashiers: Examining health equity and the COVID-19 risks to essential workers. Toxicology and Industrial Health, 36(9), 689–702. 10.1177/0748233720970439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Homeland Security. (2020). Identifying critical infrastructure during COVID-19. Cybersecurity and Infrastructure Security Agency. https://www.cisa.gov/identifying-critical-infrastructure-during-covid-19
- Weiss B. D., Paasche-Orlow M. K. (2020). Disparities in adherence to COVID-19 public health recommendations. Health Literacy Research and Practice, 4(3), e171–e173. 10.3928/24748307-20200723-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White J. L., Parham T. A. (1990). The psychology of blacks: An African-American perspective. Prentice Hall. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-hpp-10.1177_15248399221151176 for Understanding Physical Distancing and Face Mask Use Across High-Risk African American Subgroups During the COVID-19 Pandemic: Application of Health Belief Model by Jamal Moss, Leah Alexander, Iman Barré, Imari Parham, Taneisha Gillyard, Jamaine Davis and Jennifer Cunningham-Erves in Health Promotion Practice