Key Summary Points
Aim
To study the association between atypical presentation of COVID-19, frailty and adverse outcomes, as well as the incidence of atypical presentation.
Findings
In this study, an atypical presentation of COVID-19 was significantly associated with frailty. However, patients with an atypical presentation of COVID-19 did not have worse disease outcomes.
Message
Physicians need to remain alert for COVID-19 in frail older patients, as they may present without typical complaints.
Supplementary Information
The online version contains supplementary material available at 10.1007/s41999-022-00736-z.
Keywords: COVID-19, Atypical presentation, Frailty, SARS-CoV-2, Older adults
Abstract
Purpose
Older patients with COVID-19 can present with atypical complaints, such as falls or delirium. In other diseases, such an atypical presentation is associated with worse clinical outcomes. However, it is not known whether this extends to COVID-19. We aimed to study the association between atypical presentation of COVID-19, frailty and adverse outcomes, as well as the incidence of atypical presentation.
Methods
We conducted a retrospective observational multi-center cohort study in eight hospitals in the Netherlands. We included patients aged ≥ 70 years hospitalized with COVID-19 between February 2020 until May 2020. Atypical presentation of COVID-19 was defined as presentation without fever, cough and/or dyspnea. We collected data concerning symptoms on admission, demographics and frailty parameters [e.g., Charlson Comorbidity Index (CCI) and Clinical Frailty Scale (CFS)]. Outcome data included Intensive Care Unit (ICU) admission, discharge destination and 30-day mortality.
Results
We included 780 patients, 9.5% (n = 74) of those patients had an atypical presentation. Patients with an atypical presentation were older (80 years, IQR 76–86 years; versus 79 years, IQR 74–84, p = 0.044) and were more often classified as severely frail (CFS 6–9) compared to patients with a typical presentation (47.6% vs 28.7%, p = 0.004). Overall, there was no significant difference in 30-day mortality between the two groups in univariate analysis (32.4% vs 41.5%; p = 0.173) or in multivariate analysis [OR 0.59 (95% CI 0.34–1.0); p = 0.058].
Conclusions
In this study, patients with an atypical presentation of COVID-19 were more frail compared to patients with a typical presentation. Contrary to our expectations, an atypical presentation was not associated with worse outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1007/s41999-022-00736-z.
Introduction
Over the last years, COVID-19 has affected many older patients. Older patients with COVID-19 are more susceptible to adverse outcomes like Intensive Care Unit (ICU) admission and mortality [1, 2] especially those with comorbidity and who are frail. Earlier studies have shown in-hospital mortality rates up to 60% in patients aged 65 years or older and older patients account for nearly 80% of all COVID-19-related deaths [3].
The clinical presentation of COVID-19 ranges from an asymptomatic course to a potentially fatal acute respiratory distress syndrome (ARDS). The most common clinical symptoms of COVID-19 include fever, cough and dyspnea [1, 4]. However, like in other diseases [5, 6], older patients with COVID-19 can present without any of these typical symptoms, and present instead with atypical complaints such as decreased mobility, falls or delirium [7–11]. Previous studies have shown that in general, such an atypical presentation of disease is an indicator of frailty and is associated with worse clinical outcomes, including prolonged hospitalization and death [5, 6, 12]. Therefore, we would expect that an atypical presentation of COVID-19 in older patients is an independent predictor for adverse outcomes.
However, this association between an atypical presentation of COVID-19, frailty and adverse outcomes has not been studied extensively yet [13]. So far, the few existing studies have shown conflicting results, with some showing increased mortality in older patients with an atypical presentation [14] and some showing increased mortality in older patients with a typical presentation [15], whereas others found similar mortality [16, 17]. Further, studies reporting on the incidence of atypical presentation in older patients with COVID-19 have found a wide range of results [16, 18, 19].
The aim of this study was to investigate the association between an atypical presentation of COVID-19 and frailty, and the association between an atypical presentation and adverse outcomes such as ICU admission and 30-day mortality during the first pandemic surge. Furthermore, we studied the incidence of an atypical presentation of COVID-19 in hospitalized older patients.
Methods
Study design
As part of the larger COVID-OLD study [20], we conducted a retrospective observational multi-center cohort study in eight hospitals in the Netherlands: Alrijne hospital Leiderdorp, Elisabeth-TweeSteden hospital Tilburg, Erasmus University Medical Centre Rotterdam, Gelre hospitals Apeldoorn and Zutphen, Leiden University Medical Centre Leiden, Reinier de Graaf hospital Delft, Viecuri Medical Centre Venlo, and Zaans Medical Centre Zaandam. An opt-out procedure was used for inclusion in this study, i.e., data were available for scientific research unless a patient explicitly objected. The medical ethics committee waived the necessity for formal approval of the study, as data collection followed routine practice.
Study participants
All patients aged ≥ 70 years with COVID-19, who were admitted to one of the participating hospitals between February 27th and May 15th, 2020, were included. Inclusion criteria were consistent with the COVID-OLD study [18], i.e., age ≥ 70 years and hospitalization with COVID-19. Participants were diagnosed with COVID-19 if they tested positive on a polymerase chain reaction (PCR) assay of nasopharyngeal swabs on SARS-CoV-2 or if there was radiological confirmation by computed tomography (CT) imaging of the chest, defined as a CO-RADS score of ≥ 4 [21]. Patients with a clinical diagnosis of COVID-19 (based on a strong clinical suspicion due to laboratory and radiological findings in the absence of a positive PCR) were also included. Patients who were transferred to or from another hospital were excluded because information concerning symptoms at admission or outcomes was missing.
Data collection
Data were obtained from the electronic medical records by trained (research) nurses and physicians working at the participating hospitals. The following data were collected: symptoms in the 24 h prior to admission, duration between start of symptoms and hospital admission, duration of hospital stay, respiratory rate at admission, demographic data, C-reactive protein (CRP) level at admission, tobacco use, Body Mass Index (BMI) and comorbidity according to the Charlson Comorbidity Index (CCI).
In addition, frailty parameters were collected from the electronic medical records. First, we assessed frailty using the Clinical Frailty Scale (CFS) [22]. These data were collected retrospectively from patient records. If the CFS was not explicitly stated, it was assessed by a trained clinician based on the clinical record at admission. This clinician was not blinded for symptoms at admission or outcome variables. The CFS was categorized in three groups: fit (CFS 1–3), pre-frail (CFS 4–5) and severely frail (CFS 6–9). Second, we extracted data regarding the Dutch National Safety Management System (VMS) [23]. The VMS is a risk assessment tool routinely used by trained nursing staff at hospital admission in the Netherlands for all patients aged ≥ 70 years. The instrument consists of thirteen questions regarding four domains: risk of physical impairment, falls, delirium and malnutrition [23]. Outcome data included ICU admission, discharge destination and 30-day mortality.
Patients were categorized as presenting with or without typical symptoms, based on their symptoms at admission. Typical presentation of COVID-19 was defined as having at least one of the following symptoms: fever (temperature ≥ 38 °C), cough and dyspnea. Patients were considered to have an atypical presentation of COVID-19 if the medical history contained none of the typical symptoms.
Statistical analysis
Continuous data are presented as means if distributed normally [with a standard deviation (SD)] and as medians [interquartile range (IQR)] if skewed. Categorical data are presented as numbers [n, percentages (%)]. Differences in baseline characteristics for continuous variables were assessed using the unpaired t test if normally distributed and the Mann–Whitney U test if skewed. For categorical variables, we used the Chi-squared test.
Multivariable logistic regression analysis was used with 30-day mortality as the dependent variable and the following as the independent variables: type of presentation (typical or atypical), age, sex, tobacco use, CRP, CFS and CCI total. Results are presented as odds ratio’s (OR) with 95% confidence intervals. A p value < 0.05 was considered statistically significant. Because of missing values in CFS scores, comorbidity (CCI total), tobacco use and CRP, multiple imputation techniques were performed before the multivariable logistic regression analysis. This advanced strategy deals with missing values and is generally preferred over complete case analysis [24]. We based a multiple imputation regression model on the observed values and corresponding patient’s characteristics (type of presentation (typical or atypical), age, sex, tobacco use, CRP, CFS and CCI total). This model was combined with Markov Chain Monte Carlo methods to estimate missing values according to the observed patient’s characteristics. We did not perform multiple imputation on outcome data. All statistical procedures were performed using IBM SPSS Statistics, version 24 (IBM Corp., Armonk, N.Y., USA).
Results
Baseline characteristics
835 patients aged ≥ 70 years, who were hospitalized with COVID-19, were eligible. We excluded 55 (6.6%) patients who were transferred to or from another hospital (Supplementary Fig. 1. Flowchart of patient inclusion). For baseline analysis, 780 patients aged ≥ 70 years were included.
Baseline characteristics as well as indicators of disease severity are shown in Table 1. 74 (9.5%) patients had none of the typical symptoms and were, thus, considered to have an atypical presentation. 706 (90.5%) patients had typical COVID-19 symptoms. The most common reported symptoms at presentation are listed in Supplementary Table 1. The most frequently reported atypical symptom was malaise (52.7%), followed by anorexia (51.4%), delirium (35.1%) and falls (32.4%). The median age of patients with an atypical presentation was 80 (IQR 76–86) years versus 79 (IQR 74–84) years in the group of patients with a typical presentation (p = 0.044). The proportion of men with an atypical presentation was 51.4% versus 58.9% in the group with a typical presentation (p = 0.209). Before admission, 11 (14.9%) patients with an atypical presentation and 73 (10.3%) patients with a typical presentation lived in an institution (p = 0.247). BMI was lower in the group with an atypical presentation (24.9 vs 27.4; p = < 0.001). In the group with an atypical presentation the percentage of patients with a history of depression was higher (9.5% vs 3.4%; p = 0.011). The percentage of patients with dementia was significantly higher in the group with an atypical presentation (16.2% vs 8.1%; p = 0.019).
Table 1.
Baseline characteristics
| Typical presentation of COVID-19 (n = 706) | Atypical presentation of COVID-19 (n = 74) | p value | |
|---|---|---|---|
| Demographics | |||
| Age (years), median (IQR) | 79 (10) | 80 (10) | 0.044 |
| Male sex, n (%) | 416 (58.9%) | 38 (51.4%) | 0.209 |
| Living in an institution, n (%) | 73 (10.3%)a | 11 (14.9%)b | 0.247 |
| BMI, mean (SD) | 27.4 (4.7)c | 24.9 (6.2)d | < 0.001 |
| PCR confirmed COVID-19, n (%) | 620 (88.8%)e | 62 (84.9%)f | 0.322 |
| Comorbidity | |||
| History of myocardial infarction, n (%) | 135 (19.1%)g | 10 (13.5%) | 0.236 |
| History of heart failure, n (%) | 151 (21.4%)h | 12 (16.2%) | 0.295 |
| History of diabetes mellitus, n (%) | 213 (30.2%)i | 26 (35.1%) | 0.400 |
| History of chronic obstructive pulmonary disease (COPD), n (%) | 144 (20.4%)j | 9 (12.2%) | 0.088 |
| History of hypertension, n (%) | 426 (60.3%) | 46 (62.2%) | 0.760 |
| History of malignancy, n (%) | 78 (11.0%)k | 7 (9.5%)l | 0.683 |
| History of depression, n (%) | 24 (3.4%) | 7 (9.5%) | 0.011 |
| History of smoking, n (%) | 314 (44.5%)m | 32 (43.2%)n | 0.910 |
| History of dementia, n (%) | 57 (8.1%)o | 12 (16.2%) | 0.019 |
| CCI total, median (IQR) | 2 (2)p | 2 (3)q | 0.803 |
| Disease severity indicators | |||
| Duration of symptoms until admission (days), median (IQR) | 6 (7)r | 7 (8)s | 0.940 |
| Duration of hospital stay (days), median (IQR) | 6 (7)t | 6 (7) | 0.660 |
| Respiratory rate (breaths/min), mean (SD) | 22 (6.7)u | 19 (6.1)v | < 0.001 |
| C-reactive protein (mg/L), median (IQR) | 77 (99)w | 63 (87)x | 0.010 |
IQR interquartile range, SD standard deviation
aTotal 669 (37 missing)
bTotal 71 (3 missing)
cTotal 590 (116 missing)
dTotal 55 (19 missing)
eTotal 698 (8 missing)
fTotal 73 (1 missing)
gTotal 705 (1 missing)
hTotal 705 (1 missing)
iTotal 701 (5 missing)
jTotal 704 (2 missing)
kTotal 690 (26 missing)
lTotal 71 (3 missing)
mTotal 527 (179 missing)
nTotal 53 (21 missing)
oTotal 704 (2 missing)
pTotal 691 (15 missing)
qTotal 72 (2 missing)
rTotal 648 (58 missing)
sTotal 64 (10 missing)
tTotal 704 (2 missing)
uTotal 649 (57 missing)
vTotal 71 (3 missing)
wTotal 632 (74 missing)
xTotal 67 (7 missing)
As for disease severity indicators, patients with an atypical presentation had a lower respiratory rate (19 vs 22 breaths/min; p = < 0.001) and a lower C-reactive protein level (63 vs 77 mg/L; p = 0.010) at presentation, compared to patients with a typical presentation. There was no difference in duration of symptoms until hospital admission (7 vs 6 days; p = 0.940) or duration of hospital stay (6 vs 6 days; p = 0.660) between groups.
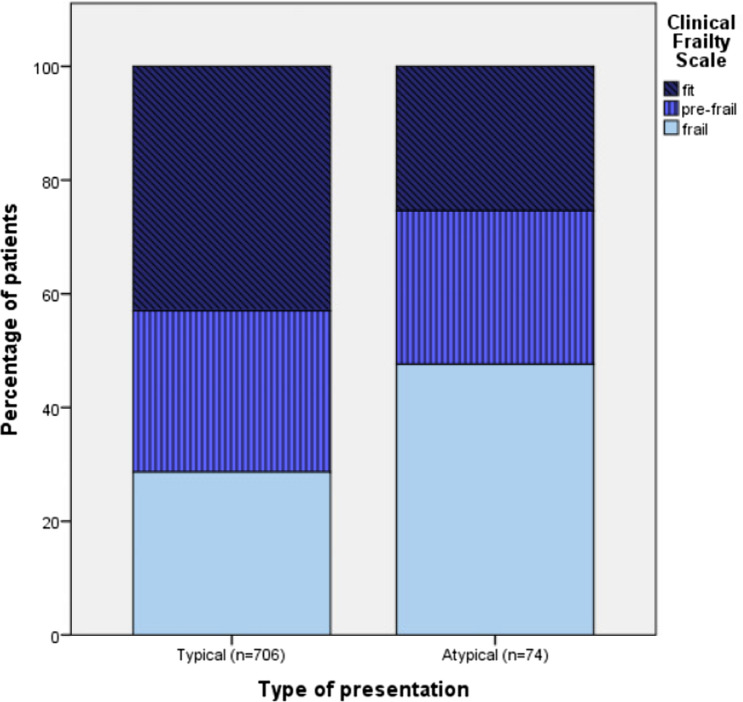
Frailty and (a)typical presentation
Table 2 presents the CFS scores and VMS scores stratified for patients with an atypical and a typical presentation. Fewer patients with an atypical presentation were classified as fit (CFS 1–3) compared to patients with a typical presentation (21.6% vs 36.1). More patients with an atypical presentation were classified as frail (CFS 6–9) compared to patients with a typical presentation (40.5% vs 24.1%) (Fig. 1). These differences were statistically significant (p = 0.004). Patients with an atypical presentation had a higher risk of physical impairment than patients with a typical presentation (44.6% vs 31.3%; p = 0.026). Furthermore, patients with an atypical presentation had a higher risk of delirium (54.1% vs 39.7%; p = 0.017), and a higher risk of falling (41.9% vs 26.1%; p = 0.004). There was no significant difference in risk of malnutrition or total CCI score between groups.
Table 2.
Frailty measurements stratified by presentation group
| Typical presentation of COVID-19 (n = 706) | Atypical presentation of COVID-19 (n = 74) | p value | |
|---|---|---|---|
| Clinical frailty scalea + b | |||
| 1–3 (fit), n (%) | 255 (43.0%) | 16 (25.4%) | 0.004 |
| 4–5 (pre-frail), n (%) | 168 (28.3%) | 17 (27.0%) | |
| 6–9 (frail), n (%) | 170 (28.7%) | 30 (47.6%) | |
| Frailty measurements (VMS) | |||
| Risk of physical impairment, n (%) | 221c (31.3%) | 33d (44.6%) | 0.026 |
| Risk of delirium, n (%) | 280e (39.7%) | 40f (54.1%) | 0.017 |
| Risk of falling, n (%) | 184g (26.1%) | 31h (41.9%) | 0.004 |
| Risk of malnutrition, n (%) | 143i (20.3%) | 21j (28.4%) | 0.145 |
aTotal typical presentation 593 (113 missing)
bTotal atypical presentation 63 (11 missing)
cTotal 613 (93 missing)
dTotal 66 (8 missing)
eTotal 620 (86 missing)
fTotal 66 (8 missing)
gTotal 600 (106 missing)
hTotal 64 (10 missing)
iTotal 594 (112 missing)
jTotal 65 (9 missing)
kTotal 691 (15 missing)
lTotal 72 (2 missing)
Fig. 1.
Clinical Frailty Scale category stratified per presentation type. Distribution of Clinical Frailty Scale (CFS) category (fit, pre-frail and frail) per presentation type. The distribution of the CFS is presented as a histogram of the percentages of patients within a given category of the CFS. Patients with an atypical presentation were less often classified as fit and more often classified as frail (p = 0.004, Chi-squared test)
Adverse outcomes
184 (23.6%) patients suffered from delirium during their hospital stay. There was no significant difference in the incidence of delirium between patients with an atypical or typical presentation (31.1% vs 22.8%; p = 0.065). During hospitalization, 82 (10.5%) patients were admitted to the ICU. Less patients with an atypical presentation were admitted to the ICU compared to patients with a typical presentation (4.1% vs 11.2%; p = 0.045). Patients with an atypical presentation were more often discharged to a nursing home (37.8% vs 23.1%; p = 0.005). However, there was no significant difference in the number of patients who were discharged to a nursing home while previously living at home (25.7% vs 17.3%; p = 0.086). 317 (40.6%) patients died within 30 days following hospital admission (Table 3). Overall, there was no statistically significant difference in 30-day mortality between patients with an atypical presentation compared to patients with a typical presentation (32.4% vs 41.5%; p = 0.173). When adjusted for age, sex, tobacco use, CRP, CFS and CCI total, there was no statistically significant difference in 30-day mortality in patients with an atypical presentation compared to patients with a typical presentation [OR 0.59 (95% CI 0.34–1.0); p = 0.058]. Univariate and multivariate estimates of baseline characteristics, geriatric measurements and 30-day mortality are shown in Table 4.
Table 3.
Outcomes of older patients with COVID-19 stratified by presentation group
| Typical presentation of COVID-19 (n = 706) | Atypical presentation of COVID-19 (n = 74) | p value | |
|---|---|---|---|
| Outcomes | |||
| 30-day mortality, n (%) | 293a (41.5%) | 24b (32.4%) | 0.173 |
| ICU admission, n (%) | 79c (11.2%) | 3d (4.1%) | 0.045 |
| Delirium during admission, n (%) | 161e (22.8%) | 23f (31.1%) | 0.065 |
| Discharge destination | |||
| Home, n (%) | 253 g (35.8%) | 23 (31.1%) | 0.401 |
| Nursing home, n (%) | 163 h (23.1%) | 28 (37.8%) | 0.005 |
| Discharge to nursing home while previously living at home, n (%) | 122i (17.3%) | 19 (25.7%) | 0.086 |
aTotal 704 (2 missing)
bTotal 72 (2 missing)
cTotal 657 (49 missing)
dTotal 72 (2 missing)
eTotal 647 (59 missing)
fTotal 65 (9 missing)
gTotal 703 (3 missing)
hTotal 703 (3 missing)
iTotal 695 (11 missing)
Table 4.
Univariable and multivariable associations of baseline characteristics and 30-day mortality
| n | Univariable model | Multivariable model | |||
|---|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | ||
| Type of presentation | |||||
| Atypical | 776 | 0.7 (0.4–1.2) | 0.175 | 0.59 (0.34–1.0) | 0.058 |
| Demographics | |||||
| Age (per year) | 780 | 1.1 (1.0–1.1) | < 0.001 | 1.0 (1.0–1.1) | 0.002 |
| Male | 776 | 1.4 (1.0–1.8) | 0.034 | 1.6 (1.2–2.1) | 0.007 |
| Living in institution | 736 | 2.3 (1.5–3.8) | < 0.001 | ||
| Comorbidity | |||||
| History of myocardial infarction | 775 | 1.8 (1.2–2.6) | 0.002 | ||
| History of heart failure | 775 | 1.2 (0.9–1.7) | 0.286 | ||
| History of diabetes mellitus | 771 | 1.6 (1.2–2.2) | 0.004 | ||
| History of chronic obstructive pulmonary disease (COPD) | 774 | 1.9 (1.3–2.7) | < 0.001 | ||
| History of hypertension | 776 | 1.2 (0.9–1.6) | 0.209 | ||
| History of malignancy | 747 | 1.2 (0.7–1.9) | 0.457 | ||
| History of depression | 776 | 0.6 (0.3–1.3) | 0.177 | ||
| History of smoking | 577 | 1.4 (1.0–2.0) | 0.042 | 0.8 (0.6–1.1) | 0.210 |
| History of dementia | 774 | 2.1 (1.3–3.4) | 0.004 | ||
| BMI | 641 | 1.0 (0.97–1.0) | 0.703 | ||
| Disease severity indicators | |||||
| Duration of symptoms until admission (days) | 776 | 0.953 (0.935–0.972) | < 0.001 | ||
| Duration of hospital stay (days) | 776 | 0.980 (0.961–0.999) | 0.038 | ||
| Respiratory rate (breaths/min) | 776 | 1.069 (1.044–1.095) | < 0.001 | ||
| C-reactive protein (mg/L) | 776 | 1.002 (1.000–1.005) | 0.024 | 1.004 (1.002–1.006) | 0.001 |
| Frailty measurements | |||||
| Clinical Frailty Scale | |||||
| 1–3 | 270 | Ref | Ref | Ref | Ref |
| 4–5 | 184 | 2.1 (1.4–3.1) | 0.000 | 1.6 (1.1–2.4) | 0.022 |
| 6–9 | 198 | 3.0 (2.1–4.5) | 0.000 | 2.2 (1.3–3.8) | 0.006 |
| Risk of physical impairment | 675 | 1.8 (1.3–2.5) | 0.000 | ||
| Risk of delirium | 683 | 2.5 (1.8–3.7) | 0.000 | 1.5 (0.9–2.3) | 0.084 |
| Risk of falling | 662 | 1.5 (1.1–2.1) | 0.013 | 1.0 (0.7–1.5) | 0.850 |
| Risk of malnutrition | 657 | 1.2 (0.8–1.7) | 0.395 | 1.0 (0.7–1.5) | 0.962 |
| CCI total | 759 | 1.2 (1.1–1.3) | 0.000 | 1.1 (1.1–1.2) | 0.001 |
OR odds ratio, CI confidence interval
Discussion
In this study, the incidence of an atypical presentation of COVID-19 in patients aged ≥ 70 years was 9.5%. Having an atypical presentation was significantly associated with frailty, as these patients were less often classified as fit (CFS 1–3), and more often classified as frail (6–9). Patients with an atypical presentation were less often admitted to the ICU. There was no significant difference in 30-day mortality; however, after adjustment for age, sex, tobacco use, CRP, CFS and CCI total there was a trend towards a lower risk of 30-day mortality in patients with an atypical presentation.
In our study, the incidence of an atypical presentation of COVID-19 among hospitalized patients aged ≥ 70 years was almost 10%. Other studies, using a similar definition of atypical presentation, have found both higher and lower incidences of an atypical presentation. This is probably due to differences in case mix, as previous studies have shown that an atypical presentation is more common in older patients [17, 25, 26], and might be more common in residents of care homes [18, 25]. Rawle et al. [18] found an incidence of an atypical presentation of 13.4% in a population that was somewhat older than our population [median age 86 (IQR 7.6) years] and included more care home residents (47.8% vs 10.8% in our study); whereas Gan et al. [16] found an incidence of 40.2% in a population with a similar age [mean age 81 (SD 8) years] that included more care home residents (27.9%). By contrast, Karlsson et al. [27] found an incidence of 3% in a somewhat older population [median age 84 (IQR 82–88)] that included more care home residents (28.4%). Therefore, age and care home residency are not the only determinants for an atypical presentation. As shown in our study, frailty is also associated with an atypical presentation, which might explain part of the variation in incidence found. In addition, these incidences were found in studies during the first phase of the pandemic, when patients with an atypical presentation may not have been tested for COVID-19, thus resulting in underdiagnosis of COVID-19. Therefore, the true incidence of an atypical presentation of COVID-19 is probably higher.
Our findings have shown that patients with an atypical presentation of COVID-19 are more frail as measured with the CFS as well as with other frailty indicators (VMS). This was in agreement with a study by Poco et al. [25] that showed that frail patients with COVID-19 were more likely to present with atypical complaints such as confusion and functional decline. In addition, in a study by Gan et al. [16], 71% of patients with an atypical presentation were frail compared to 56% in the group with a typical presentation. Last, Osuafor et al. [28] found that frail older patients were more likely to present with atypical symptoms. This strong association between frailty and atypical presentation of disease is already well known in other diseases [6, 29]. It is important to know that COVID-19 is no exception to this rule.
Overall, there was no difference in 30-day mortality between groups, even after adjustment for confounders such as age, frailty and CRP. This was unexpected, as patients with an atypical disease presentation have worse outcomes in other diseases [5, 6]. On the other hand, patients with a fatal course of COVID-19 die from pulmonary complications such as acute respiratory distress syndrome (ARDS) or pulmonary embolisms [30, 31], and are, therefore, likely to have typical pulmonary complaints. Previous studies regarding atypical presentation of COVID-19 and mortality have found conflicting results. In agreement with our study, Gan et al. [16] did not find a significant difference in hospital mortality between patients with an atypical and a typical presentation; however, they did not correct for possible confounders such as frailty and markers for disease severity. Also, Marziliano et al. [17] using a more extensive definition of atypical presentation, did not find a difference in hospital mortality after correction for confounders. By contrast, after adjustment for confounders, Knopp et al. [15] found that typical symptoms, such as fever and dyspnea in COVID-19 were associated with a higher risk of mortality and Goldberg et al. [26] found that patients with two or more typical symptoms had higher odds of 30-day mortality or intubation. In a meta-analysis by Damayanthi et al. [32] dyspnea was also found to be significantly associated with mortality. On the other hand, Poco et al. [25] found that the co-occurrence of typical COVID symptoms was associated with lower mortality, but this was no longer significant after correction for age, sex and frailty. However, the presence of fever was associated with a lower odds of mortality. Last, Pop-Vicas et al. [14] found a higher 30-day mortality in patients with an atypical presentation; however, these results should be interpreted with caution as their patients with an atypical presentation were much older. In conclusion, the existing evidence about the association of an atypical presentation with mortality is conflicting, and our study adds to this evidence base. However, it is important that, as in our study, future studies correct for confounders, such as high age, male sex, frailty and higher CRP levels as these are associated with higher mortality in patients with COVID-19 [20, 27, 32–37]. In addition, we would recommend to investigate whether there is a difference in mortality between patients that present atypically but develop fever, cough or dyspnea later in their disease trajectory and those who do not develop any typical complaints.
In our study, patients with a typical presentation were more often admitted to the ICU. Marziliano et al. [17] also found that patients who presented with typical complaints were more likely to receive ICU care. This result could be due to selection bias, as the CFS [22] was significantly higher in the group of patients with an atypical presentation, and the assessment of whether a patient should be admitted to the ICU was partly based on the frailty assessment using the CFS [38]. It could also be due to the aforementioned fact that patients with a typical presentation of COVID-19 were more likely to experience pulmonary complications, and were therefore more likely to need invasive ventilatory support.
This study is one of a limited number of studies that have focused on the association between an atypical presentation of COVID-19, frailty and adverse outcomes. This is important, as it expands the knowledge base on COVID-19 in older patients, and alerts clinicians to be vigilant for COVID-19 in frail older patients presenting without pulmonary complaints or with geriatric syndromes such as falls or delirium. Further, it was a large multi-center study, including over 700 participants who were admitted to different hospitals throughout the Netherlands, which adds to the generalizability of our study. We collected a large amount of data concerning adverse outcomes, frailty and geriatric indicators, which enabled us to correct for important confounders such as age, frailty and CRP. Our study had some limitations as well, the first being its retrospective nature, which has resulted in missing data and possibly underreporting of complaints that were not considered typical. Second, for some patients, the CFS was assessed retrospectively by clinicians not blinded for symptoms or patient outcomes, which may have led to bias. Further, there may have been selection bias as some patients presenting with atypical symptoms were probably not tested for COVID-19 and were, thus, not included in our study, which may have resulted in the inclusion of fewer patients who were frail. Last, the study was done during the first phase of the pandemic, and the virus and testing strategies have changed significantly ever since [39]. This, together with the availability of vaccines, may limit the generalizability of our results.
In this study, almost 10% of older COVID-19 patients presented without typical symptoms of COVID-19. These patients were more frail compared to patients with a typical presentation. Contrary to our expectations, these patients did not have a higher mortality rate than patients with typical symptoms. However, early identification of these patients remains essential to ensure proper isolation measures and the initiation of treatment and support. Physicians need to remain alert for COVID-19 in older patients, especially when they are frail, who present without typical complaints. Additional studies investigating an atypical presentation of COVID-19 in a fully vaccinated population might be able to further advance everyday practice.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank Annemarie Verburg and Marianne van Nistelrooij (Department of Geriatric Medicine and Centre of Excellence for Old Age Medicine, Gelre Hospitals, Apeldoorn & Zutphen, the Netherlands); Greetje Emmerik (Department of Geriatric Medicine, Reinier de Graaf Hospital, Delft, the Netherlands); Orla Smit (Department of Internal Medicine, Division of Geriatric Medicine, Zaans Medisch Centrum, Zaandam, the Netherlands); Esmee Mulder and Milou Spekreijse (Department of Geriatric Medicine, Catharina Hospital, Eindhoven, the Netherlands); and Leanne Oosterwijk (Department of Internal Medicine, Division of Geriatric Medicine, Erasmus MC, University Medical Centre Rotterdam, Rotterdam, the Netherlands) for their assistance with data collection. Furthermore, we would like to thank Marjan Wieringa (Department of Education, Office of Science, Elisabeth-TweeSteden Hospital, Tilburg, the Netherlands) for her assistance with the statistical analysis.
Author contributions
Study design: CMS, EMW, VM. Data acquisition: CMS, EMW, VM. Data Analysis: CMS, EMW. Data Interpretation: all authors. Writing and critical revision of the manuscript: all authors. Study design: CMS, EMW, VM. Data acquisition: CMS, EMW, VM. Data Analysis: CMS, EMW. Data Interpretation: all authors. Writing and critical revision of the manuscript: all authors. Study design: JVDB, SJ, CVDL, SM, HW, HS, SR. Data acquisition: JVS, EK, JVDB, DB, LB, CVD, LE, AL, RL, HM, BVM, FMR, AP, HPB, RS, PS, AW, NW, HS, SR. Data Analysis: JVS, EK, JVDB, HS, SR. Data Interpretation: JVS, EK, JVDB, SM, HPB, HS, SR. Writing the manuscript: JVS, EK, JVDB, HS, SR. Critical revision of the manuscript: all authors.
Funding
No funding was received for conducting this study.
Data availability
The data supporting the findings of this study are available upon request from the corresponding author, J.E. van Son.
Declarations
Conflict of interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The medical ethics committees of all participating hospitals waived the necessity for formal approval of the study, as data collection followed routine practice.
Informed consent
For this type of study, formal consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chen T, Rakesh Z, Mo P, Li X, Ma Z, Song S, et al. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: a single-centered, retrospective study. J Gerontol A Biol Sci Med Sci. 2020 doi: 10.1093/gerona/glaa089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centres for Disease Control and Prevention (2020) Demographic Trends of COVID-19 cases and deaths in the US reported to CDC. https://covid.cdc.gov/covid-data-tracker/#demographics. Accessed 24 July 2021
- 4.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hofman MR, van den Hanenberg F, Sierevelt IN, Tulner CR. Elderly patients with an atypical presentation of illness in the emergency department. Neth J Med. 2017;75:241–246. [PubMed] [Google Scholar]
- 6.Jarrett PG, Rockwood K, Carver D, Stolee P, Cosway S. Illness presentation in elderly patients. Arch Intern Med. 1995;155:1060–1064. doi: 10.1001/archinte.1995.00430100086010. [DOI] [PubMed] [Google Scholar]
- 7.Olde Rikkert MGM, Vingerhoets RW, van Geldorp N, de Jong E, Maas HAAM (2020) Atypical clinical picture of COVID-19 in older patients. Ned Tijdschr Geneeskd 164:D5004 [PubMed]
- 8.Hewitt J, Carter B, Vilches-Moraga A, Quinn TJ, Braude P, Verduri A, et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30146-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kennedy M, Helfand BKI, Gou RY, Gartaganis SL, Webb M, Moccia JM, et al. Delirium in Older Patients With COVID-19 Presenting to the Emergency Department. JAMA Netw Open. 2020;3:e2029540. doi: 10.1001/jamanetworkopen.2020.29540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norman RE, Stall NM, Sinha SK. Typically atypical: COVID-19 presenting as a fall in an older adult. J Am Geriatr Soc. 2020;68:E36–E37. doi: 10.1111/jgs.16526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prendki V, Tiseo G, Falcone M. Caring for older adults during the COVID-19 pandemic. Clin Microbiol Infect. 2022;28:785–791. doi: 10.1016/j.cmi.2022.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Limpawattana P, Phungoen P, Mitsungnern T, Laosuangkoon W, Tansangworn N. Atypical presentations of older adults at the emergency department and associated factors. Arch Gerontol Geriatr. 2016 doi: 10.1016/j.archger.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 13.Remelli F, Volpato S, Trevisan C. Clinical features of SARS-CoV-2 infection in older adults. Clin Geriatr Med. 2022;38:483–500. doi: 10.1016/j.cger.2022.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pop-Vicas A, Haleem A, Osman F, Fuglestad R, Shirley D, Striker R, et al. Risk factors and mortality for atypical presentation of COVID-19 infection in hospitalized patients—lessons from the early pandemic. WMJ. 2021;120:94–99. [PubMed] [Google Scholar]
- 15.Knopp P, Miles A, Webb TE, Mcloughlin BC, Mannan I, Raja N, et al. Presenting features of COVID-19 in older people: relationships with frailty, inflammation and mortality. Eur Geriatr Med. 2020 doi: 10.1007/s41999-020-00373-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gan JM, Kho J, Akhunbay-Fudge M, Choo HM, Wright M, Batt F, et al. Atypical presentation of COVID-19 in hospitalised older adults. Ir J Med Sci. 2021 doi: 10.1007/s11845-020-02372-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marziliano A, Burns E, Chauhan L, Liu Y, Makhnevich A, Zhang M, et al. Patient factors and hospital outcomes associated with atypical presentation in hospitalized older adults with COVID-19 during the first surge of the pandemic. J Gerontol A Biol Sci Med Sci. 2022 doi: 10.1093/gerona/glab171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rawle MJ, Bertfield DL, Brill SE. Atypical presentations of COVID-19 in care home residents presenting to secondary care: a UK single centre study. Aging Med. 2020 doi: 10.1002/agm2.12126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blain H, Gamon L, Tuaillon E, Pisoni A, Giacosa N, Albrand M, et al. Atypical symptoms, SARS-CoV-2 test results and immunisation rates in 456 residents from eight nursing homes facing a COVID-19 outbreak. Age Ageing. 2021 doi: 10.1093/ageing/afab050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blomaard LC, van der Linden CMJ, van der Bol JM, Jansen SWM, Polinder-Bos HA, Willems HC, et al. Frailty is associated with in-hospital mortality in older hospitalised COVID-19 patients in the Netherlands: the COVID-OLD study. Age Ageing. 2021 doi: 10.1093/ageing/afab018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prokop M, van Everdingen W, van Rees VT, Quarles van Ufford H, Stöger L, Beenen L, et al. CO-RADS: a categorical CT assessment scheme for patients suspected of having COVID-19—definition and evaluation. Radiology. 2020 doi: 10.1148/radiol.2020201473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rockwood K. A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J. 2005 doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.VMS Veiligheidsprogramma (2009) Praktijkgids kwetsbare ouderen. Utrecht
- 24.Donders ART, van der Heijden GJMG, Stijnen T, Moons KGM. Review: a gentle introduction to imputation of missing values. J Clin Epidemiol. 2006 doi: 10.1016/j.jclinepi.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 25.Poco PCE, Aliberti MJR, Dias MB, de Takahashi SF, Leonel FC, Altona M, et al. Divergent: age, frailty, and atypical presentations of COVID-19 in hospitalized patients. J Gerontol A Biol Sci Med Sci. 2021;76:e46–51. doi: 10.1093/gerona/glaa280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldberg EM, Southerland LT, Meltzer AC, Pagenhardt J, Hoopes R, Camargo CA, et al. Age-related differences in symptoms in older emergency department patients with COVID-19: prevalence and outcomes in a multicenter cohort. J Am Geriatr Soc. 2022;70:1918–1930. doi: 10.1111/jgs.17816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karlsson LK, Jakobsen LH, Hollensberg L, Ryg J, Midttun M, Frederiksen H, et al. Clinical presentation and mortality in hospitalized patients aged 80+ years with COVID-19—a retrospective cohort study. Arch Gerontol Geriatr. 2021;94:104335. doi: 10.1016/j.archger.2020.104335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osuafor CN, Davidson C, Mackett AJ, Goujon M, van der Poel L, Taylor V, et al. Clinical features, inpatient trajectories and frailty in older inpatients with COVID-19: a retrospective observational study. Geriatrics (Basel) 2021 doi: 10.3390/geriatrics6010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ellis G, Marshall T, Ritchie C. Comprehensive geriatric assessment in the emergency department. Clin Interv Aging. 2014;9:2033–2043. doi: 10.2147/CIA.S29662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tian S, Xiong Y, Liu H, Niu L, Guo J, Liao M, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020 doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Damayanthi HDWT, Prabani KIP, Weerasekara I. Factors associated for mortality of older people with COVID 19: a systematic review and meta-analysis. Gerontol Geriatr Med. 2022 doi: 10.1177/23337214211057392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pranata R, Henrina J, Lim MA, Lawrensia S, Yonas E, Vania R, et al. Clinical frailty scale and mortality in COVID-19: a systematic review and dose-response meta-analysis. Arch Gerontol Geriatr. 2021;93:104324. doi: 10.1016/j.archger.2020.104324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vrillon A, Hourregue C, Azuar J, Grosset L, Boutelier A, Tan S, et al. COVID-19 in older adults: a series of 76 patients aged 85 years and older with COVID-19. J Am Geriatr Soc. 2020;68:2735–2743. doi: 10.1111/jgs.16894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gonçalves FAR, Besen BAMP, de Lima CA, Corá AP, Pereira AJR, Perazzio SF, et al. Use and misuse of biomarkers and the role of D-dimer and C-reactive protein in the management of COVID-19: a post-hoc analysis of a prospective cohort study. Clinics (Sao Paulo) 2021;76:e3547. doi: 10.6061/clinics/2021/e3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Na YS, Kim JH, Baek MS, Kim W-Y, Baek A-R, Lee B, et al. In-hospital mortality prediction using frailty scale and severity score in elderly patients with severe COVID-19. Acute Crit Care. 2022;37:303–311. doi: 10.4266/acc.2022.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maynou L, Owen R, Konstant-Hambling R, Imam T, Arkill S, Bertfield D, et al. The association between frailty risk and COVID-19-associated all-mortality in hospitalised older people: a national cohort study. Eur Geriatr Med. 2022;13:1149–1157. doi: 10.1007/s41999-022-00668-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nederlandse Vereniging voor Intensive Care. Draaiboek Pandemie. Volume 13 2020. https://www.demedischspecialist.nl/sites/default/files/Draaiboek%20pandemie%20deel%201.pdf. Accessed 24 July 2021
- 39.Fernandes Q, Inchakalody VP, Merhi M, Mestiri S, Taib N, Moustafa AED, et al. Emerging COVID-19 variants and their impact on SARS-CoV-2 diagnosis, therapeutics and vaccines. Ann Med. 2022;54:524–540. doi: 10.1080/07853890.2022.2031274. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting the findings of this study are available upon request from the corresponding author, J.E. van Son.