Abstract
The COVID-19 pandemic has necessitated caregivers and school-aged children to adapt to ongoing changes and uncertainty. Understanding why some caregivers and school-aged children area able to adapt and others are not could be attributed to resilience. The relationships between caregiver or child resilience and socioeconomic status (SES) in the context of COVID-19 remain largely un-explored. Therefore, the purpose of this qualitative systematic review was to explore (1) what is currently known about the relationship between caregiver and child resilience in the context of COVID-19; and (2) the role of SES on caregiver or child resilience throughout the COVID-19 pandemic. Four databases (i.e., MEDLINE, Scopus, PsycINFO, and CINAHL) were systematically searched, title/abstract and full-text screening were conducted, and 17 articles met the inclusion criteria (i.e., discussed resilience of caregivers/children during COVID-19, mean age of children between 7–10, primary research/grey literature, English), including 15 peer-reviewed and two grey literature sources. Thematic analysis revealed five themes: (1) the mitigating effects of child resilience; (2) overcoming the psychological toll of the pandemic; (3) the unknown relationship: caregiver and child resilience; (4) family functioning during COVID-19; and (5) the perfect storm for socioeconomic impacts. Results from this review provide the first synthesis of the impact of the COVID-19 pandemic on the resilience of caregivers and school-aged children. Future research should conduct longitudinal data collection to understand the possible long-term impacts of the pandemic on these populations’ resilience. Understanding these impacts will be integral to assisting families in bouncing back from the long-lasting adverse circumstances caused by the COVID-19 pandemic.
Keywords: Resilience, Caregivers, School-aged children, Socioeconomic status, COVID-19
Introduction
Since December of 2019, the COVID-19 pandemic and associated public health restrictions have disrupted life for everyone (World Health Organization, 2020). These public health restrictions have impacted the lives of children as schools have vacillated between in-person and remote learning, there has been prolonged social and physical isolation, and home environments have been altered by the changing working conditions of caregivers (Carroll et al., 2020; Loades et al., 2020; Maunula et al., 2021; Suarez-Lopez et al., 2021). School-aged children have experienced some of the greatest pandemic adversities stemming from the fluctuation of remote and in-person learning with closures of schools impacting approximately 94% of the world’s student population (United Nations, 2020). These vacillations between in-person and remote learning may have contributed to anxiety, depression, and behavioural problems in children (Fegert et al., 2020). Although many hypothesized that the COVID-19 pandemic would negatively impact the mental wellbeing of school-aged children, preliminary results from cross-sectional studies have varied (Duan et al., 2020; Liang et al., 2020; Ma et al., 2021; Marques de Miranda et al., 2020; Orgilés et al., 2021; Tang et al., 2021; Xie et al., 2020; Yeasmin et al., 2020; Zhou et al., 2020). Using retrospective reports, Cost and colleagues (2021) found among a sample of 1,013 Canadian children and youth aged 6 to 18 years, 60–70% experienced declines in at least one mental health domain. Conversely, these authors also noted that the mental health of 19–31% of children did improve during the pandemic (Cost et al., 2021). These contradictory findings regarding children’s mental health during the pandemic have been documented in other studies, suggesting the effects of the pandemics on school-aged children are complex and nuanced based with emerging evidence indicating access to other social determinants of health plays a role as well (Abrams & Szefler, 2020; Maximum City, 2021).
The COVID-19 pandemic exacerbated existing inequities for families (Cusinato et al., 2020; Public Health Agency of Canada [PHAC], 2020). One such inequity is income, with reports that families with lower incomes have disproportionately experienced food insecurity, changes in working conditions, job losses, and heightened financial insecurities (Cusianto et al., 2020; Gallitto, 2020; Prime et al., 2020; SickKids, 2021). While the COVID-19 pandemic is still ongoing, research on previous pandemics demonstrated children exposed to economic hardships and traumatic events were more likely to experience anxiety, depression, and behavioural difficulties, with the effects extending years after the traumatic events occurred (Hawryluck et al., 2004; Liu et al., 2012). Moreover, income and financial strain have notable effects on overall family functioning. In a recent study on caregivers (n = 572) in the United States investigating family dynamics following economic hardships such as job and income losses, it was found that caregivers were more likely to report depressive symptoms, increased stress levels, and negative interactions with their children (e.g., increase in yelling between family members, parents quicker to lose temper) as compared to the control group (Kalil et al., 2020). Similar results were found in a study of caregivers (n = 223) in the United States by Chen and colleagues (2022) who investigated the experiences of families with school-aged children during the initial months of the pandemic. Low-income caregivers experienced more financial hardships due to the pandemic compared to their higher income counterparts. Conclusions from this study suggested that family income level impacts their ability to cope with pandemic-related challenges (Chen et al., 2022).
A family’s ability to cope when they have experienced a traumatic event, such as a pandemic, depends on their personal resources, mental health, and resilience (Bridgland et al., 2021; Coulombe et al., 2020; Cusinato et al., 2020; Li et al., 2021). Resilience can be understood as a dynamic process in which psychosocial and environmental factors interact to enable an individual to survive, grow, and thrive during adversity (Crann & Barata, 2015; Munoz et al., 2017; Prime et al., 2020). Resilience is influenced by factors such as individual characteristics, self-regulation, self-concept, family conditions, and/or community supports that promote positive outcomes or reduce negative outcomes during challenging times (Fergus & Zimmerman, 2005; Zolkoski & Bullock, 2012). Family conditions including caregiver flexibility, positive caregiver-child relationships, constructive parenting, and parental strength, have been identified as environmental factors that positively impact children’s resilience (Black & Lobo, 2008; Daks et al., 2020; Guruge et al., 2021; Torres Fernandez et al., 2013). In a recent review on family resilience during the COVID-19 pandemic, Gayatri and Irawaty (2021) reported higher family resilience was related to lower anxiety, stress, and depression symptoms among both caregivers and children (n = 165,515). Moreover, a review on parental resilience by Gavidia-Payne and colleagues (2015) concluded that resilience among parents resulted from the combination of family abilities and external factors (e.g., social support) in anticipating, perceiving, and responding to changing circumstances. The importance of family functioning and a caregiver’s ability to adapt to changing environments are necessary prerequisites for caregivers to be resilient. Despite what is known regarding factors influencing caregiver resilience (e.g., family functioning, ability to adapt), research is unclear on whether children’s resilience has been impacted throughout the pandemic. Moreover, while some authors have explored caregiver and child resilience in silo from one another (Caputi et al., 2021; Cusinato et al., 2020; Mariani Wigley et al., 2021), the relationship between a caregiver’s resilience and that of their children remains largely unexplored.
The pandemic has changed the lives of all school-aged children and their caregivers with many experiencing economic strain (Chen et al., 2022; Hawryluck et al., 2004; Kalil et al., 2020; Liu et al., 2012). Research is clear that experiencing adverse events, such as the ongoing COVID-19 pandemic, is experienced differently by individuals and this may be in part to resilience (Bridgland et al., 2021; Coulombe et al., 2020; Cusinato et al., 2020; Li et al., 2021). While studies have examined resilience among caregivers or their children distinct independently (Caputi et al., 2021; Cusinato et al., 2020; Mariani Wigley et al., 2021), few studies explore caregiver and child resilience together and fewer still nuance the effects of the pandemic based on social determinants of health (e.g., income, financial strain, employment, etc.). Specifically, the PHAC (2020) has called for research examining the intersection of social determinants of health, and the associated direct and indirect impacts of familial and child resilience in the context of COVID-19. As such the purpose of this study is to fill that gap by (1) exploring what is currently known about the relationship between caregiver and child resilience in the context of COVID-19; and (2) examining the role of SES on caregiver or child resilience throughout the COVID-19 pandemic.
Methods
A qualitative systematic review was undertaken to collage and synthesize data from the included studies to determine the status of this body of knowledge (i.e., resilience and socioeconomic status [SES]; Paré et al., 2015). Through employing typical systematic review methodologies (per Cochrane’s guidelines), we are able to provide a narrative synthesis of findings, making trends among the studies clearer (Paré et al., 2015). Ethics approval was not required for this review as all data was publicly available.
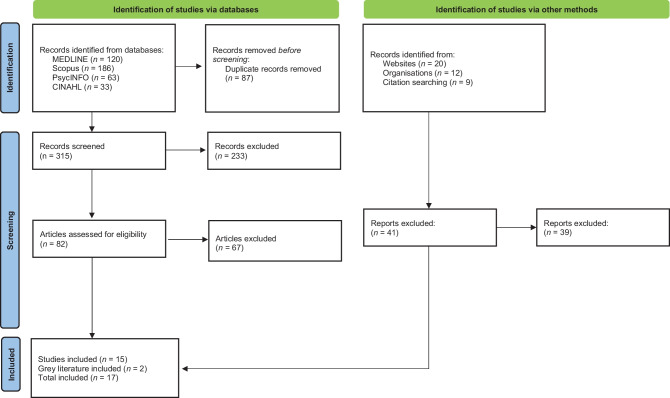
Four databases (i.e., MEDLINE, Scopus, PsycINFO, and CINAHL) were searched in March 2022 using the constructs caregivers, children, resilience, and COVID-191 (see Appendix A for complete search strategy). Grey literature searches involved systematically searching through key governmental agencies (e.g., Public Health Canada, Statistics Canada, etc.) for sources related caregiver or child resilience in the context of COVID-19. After these searches were conducted, all articles were imported into Covidence systematic review software (2021) where screening was conducted independently by two reviewers. Inclusion criteria for this review included: (1) results discussed resilience in caregivers and/or children in the context of the COVID-19 pandemic; (2) mean age of children between 7 and 10 years; (3) article classified as primary research or grey literature; and (4) written in English. The age range of 7 to 10 years was selected to capture both junior (i.e., grades K-3) and senior (i.e., grades 4–6) elementary school-aged children, given the varying ages at which children begin and end elementary school in different countries worldwide (UNESCO, 2021). Given the purpose of qualitative systematic reviews, including review studies was deemed to be beyond the scope of the current review (Paré et al., 2015). Articles needed to be written in English due to the language capabilities of both authors. Title/abstract (n = 356) and full-text (n = 123) screening were conducted in succession using the eligibility criteria outlined above (see Appendix B for rationale for excluded articles). There were no discrepancies in screening by the two reviewers. If discrepancies did arise, the reviewers planned to meet to go over the article together in detail, discussing whether the article met the outlined inclusion criteria. A total of 15 peer-reviewed studies and 2 sources of grey literature were included in the final review (see Fig. 1 for PRISMA diagram; Page et al., 2020).
Fig. 1.
PRISMA Flow Diagram
Data from all eligible articles were extracted onto a template co-designed by the research team. Extracted information included study authors, year of publication, country of origin, aims/purpose, sample size/demographics (i.e., age, gender/sex), methodology/theoretical grounding, analysis method, outcome measures, and important results (related to caregiver/child resilience or SES). No original data was modified (see Table 1 for full extraction chart).
Table 1.
Data extraction chart for included literature (n = 17)
| Author(s), Year, Country of Origin | Purpose | Sample Size, Demographics (i.e., Age, Gender/Sex) | Methodology, Theoretical Grounding, or Analysis Method | Outcome Measures | Important Results (i.e., caregiver resilience, child resilience, or SES results) |
|---|---|---|---|---|---|
| Peer-Reviewed Articles (n = 15) | |||||
|
Caputi et al., 2021 Italy |
To investigate the predictors of psychopathology in children aged 5-10 years, immediately after the national 2-month lockdown. |
n = 158 caregivers n = 158 children Age Mage caregivers = 41 (SD = 5.3) Mage children = 7.4 (SD = 1.8) Sex – Caregivers Female (93.67%) Male (6.33%) Sex – Children Female (51.90%) Male (48.10%) |
Quantitative data collected via online questionnaire during June 2020. Analyses included t-tests, correlations, and regressions. |
Children’s resilience measured by The Child and Youth Resilience Measure – Person Most Knowledgeable version (CYRM-PMK). Children’s health problems and psychological adjustment measured by The Strengths and Difficulties Questionnaire (SDQ). Parent’s resilience measured by The Adult Resilience Measure (ARM). |
- Child resilience (M = 29.868), parent resilience (M = 28.421) - Children’s resilience shows positive correlation with parental resilience (r = 0.49, p < 0.001) - Negative correlations between child resilience and total difficulties (r = -0.58, p < 0.001) - Child resilience was the only predictor of the SDQ total difficulties score (ß = -0.579, p < 0.001) - Low child resilience was a significant predictor of SDQ total difficulties (ß = -0.230, p < 0.01) |
|
Cusinato et al., 2020 Italy |
To analyze the potential risk and protective factors for parents’ and children’s well-being during a potentially traumatic event such as the COVID-19 quarantine. |
n = 463 caregivers Age Mage caregivers = 43.3 (SD = 5.88) Mage children = 9.72 (SD = 3.29) Sex – Caregivers Female (90.5%) Male (9.5%) |
Quantitative data collected via online survey from April-May 2020. Analyses included general linear models, multiple linear regression, ANOVA, t-tests, and correlations. |
Parental well-being measured by the Psychological General Well Being Index (PGWB). Children's well-being measured by the SDQ. Children's resilience measured by the CYRM. |
- Negative correlations between CYRM and all SDQ scales (values ranged from r = -0.40 to r = -0.63), except for prosocial behaviour scale (r = 0.43) - Total scores of the PGWB and CYRM-R were significant negative predictors of parental stress (respectively: ß = -0.28, t = -6.37, p < 0.001 and ß = -0.21, t = -4.17, p < 0.001) - Correlations between the CYRM-R and the PGWB were significant (values ranged from r = 0.22 to r = 0.27) |
|
Dominguez-Alvarez et al., 2020 Spain |
To examine how child coping, unique contextual conditions, and parent dispositional resilience might contribute to the children psychosocial adjustment during the extraordinary context of COVID-19 pandemic. |
n = 1004 caregivers n = 1123 children Age Mage children = 7.26 (SD = 2.39) Sex – Caregivers Female (89.5%) Male (10.5%) Sex – Children Female (50%) Male (50%) |
Quantitative data collected via online questionnaire during April 2020. Analyses included ANOVA, bivariate correlations, and multiple linear regression. |
Child coping measured by a 22-item scale developed to be context-specific. Parent resilience measured by the 10-item Connor-Davidson Resilience Scale (CD-RISC-10). SES measured through parent education, family income, and family financial solvency to face daily overheads. |
- 7-9-year-olds started to display more engaged-oriented coping strategies, including problem solving (M = 1.07, SD = 0.79), seeking understanding (M = 1.42, SD = 0.89), and seeking instrumental social support (M = 1.07, SD = 0.81) - Parent dispositional resilience was negatively correlated with child disengagement (r = -0.20, p < 0.001) and positively correlated with child engagement coping (r = 0.19, p < 0.001) - Higher SES negatively correlated with COVID-19 perceived economic impact (r = -0.39, p < 0.001) - Child engagement coping was distinctively and extensively associated to indicators of adjustment, even when controlling for other covariates assumed to be relevant (i.e., SES, parental resilience) |
|
Guruge et al., 2021 Canada |
To examine the COVID-19 related changes and challenges experienced by immigrant parents living in apartment buildings in the Greater Toronto Area of Ontario, Canada. |
n = 50 caregivers Age Age range of parents = 26-77 Gender – Caregivers Female (88%) Male (12%) |
Qualitative data collected during semi-structured interviews during summer and fall of 2020. Ecosystemic framework. Analysis informed by interpretive descriptive methodology. |
Parental-lived experiences. |
- Most parents demonstrated resilience which contributed to growth in terms of parent-child relationships - Parent-child relationships were impacted by the psychological impact of stressors such as prolonged duration at home, fears of infection, frustration and boredom, inadequate information, lack of in-person contact with classmates, friends, and teachers, lack of personal space at home, and family and financial loss |
|
Koskela et al., 2020 Finland |
To explore (1) how parents described their resilient practices; and (2) how families acted if their resilient practices conflicted with those of remote education. |
n = 316 caregivers Gender – Caregivers Female (92%) Male (7%) Do not want to say (1%) |
Qualitative data collected via online questionnaire during spring of 2020. Analysis informed by interpretative, deductive approach. |
Parental-lived experiences. |
- Parents noted multiple issues in organizing and coping with everyday life during COVID - Parents ability to reflect on situations and the shifting needs of their children promoted family resilience - Resilient practices based on personal capabilities (e.g., understanding education), family capabilities (e.g., routines), and resources outside of the family (e.g., flexible employers) - Parent/family resilient activities: recognizing/reading situations, using available resources, actively attempting to creatively solve problems at family level, reflecting on roles as facilitators for children |
|
Laufer & Bitton, 2021 Israel |
The study examined parents’ perceptions of their children’s behavioral difficulties and positive parent–child interaction during the first COVID-19 lockdown in Israel, as well as the associations among parents’ psychological distress, parents’ COVID-19–related worries, parents’ coping, and parents’ resilience. |
n = 437 caregivers Age Mage caregivers = 43.74 (SD = 8.11) Mage children = 8.47 years (SD = 5.42) Sex – Caregivers Female (73.7%) Male (26.3%) |
Quantitative data collected via online questionnaire from March-April 2020. Analyses included correlations, multiple hierarchical regressions, and parallel mediation models. |
Parental resilience measured by the 25-item Connor Davidson Resilience Scale (CD-RISC-25). Parental psychological distress measured by the short form Brief Symptom Inventory. Parental concern regarding their financial situation due to COVID-19 measured by general Likert scale questions. |
- 53.9% of parents were worried due to financial issues stemming from the pandemic - Resilience negatively related to distress (r = -0.35, p < 0.001) - Resilience mediated the relation between somatization (B = -0.23, p < 0.001), anxiety (B = -0.32, p < 0.001), and depression (B = -0.41, p < 0.001) |
|
Lim et al., 2021 Singapore |
To evaluate factors affecting psychological ill-effects and resilience of caregivers of children with developmental disabilities during the coronavirus pandemic. |
n = 107 caregivers Age Mage caregivers = 40.5 (SD = 6.0) Mage children = 7.6 years (SD = 4.1) Sex – Caregivers Female (80.4%) Male (19.6%) |
Quantitative data collected via questionnaire from May-June 2020. Analyses included univariate analysis, chi-square tests, t-tests, and logistical regression. |
Parental resilience measured by the CD-RISC-25. Parent symptoms of depression (DASS-D), anxiety (DASS-A), and stress (DASS-S) measured by the 21-item Depression, Anxiety, and Stress Scale (DASS-21). Family SES and caregiver’s perceptions of experiences and concerns during the pandemic measured by general Likert scale questions. |
- 69.2% of caregivers were worried about financial stability - The higher the caregiver’s CD-RISC-25 score, the less likely he/she would have a positive DASS-D screen (OR=0.93, p < 0.001) - Lower CD-RISC-25 scores were also associated with a positive DASS-A score (OR=0.96, p = 0.021). - Parents with a higher CD-RISC-25 score were less likely to have a positive DASS-S score (OR = 0.97, p = 0.037) |
|
Mariani Wigley et al., 2021 Italy |
To explore the role of parents’ resilience and their ability to support and promote child resilient behaviors toward child resilience and child stress-related behaviors during the COVID-19 outbreak. |
n = 166 caregivers Age Mage caregivers = 43.27 (SD = 4.20) Mage children = 8.88 (SD = 1.41) Sex – Caregivers Female (95.2%) Male (4.8%) Gender – Children Female (48.1%) Male (51.9%) |
Quantitative data collected via questionnaire from May-June 2020. Analyses included paired sample t-tests, correlations, and a sequential mediation model. |
Resilient behaviours of child taught by parent measured by the 21-item COPEWithME questionnaire. Parental resilience measured by CD-RISC 25. Child resilience measured by CYRM-PMK. Impact of COVID-19 on child well-being measured by an ad-hoc scale. |
- Mean resilience score on CD-RISC 25 = 63.78 (SD = 16.86), CYRM-PMK = 22.56 (SD = 0.59) - No significant correlation emerged between CD-RISC 25 and PMK-CYRM-R - Parental ability to teach effective strategies to cope significantly correlates with better child resilience to cope with COVID-19 (r = 0.562, p < 0.001) - Children’s stress-related behaviors observed by parents during the confinement, a higher mean score of stress-related behaviours was significantly related to poorer parental resilience (r = −0.213, p = 0.007), poorer parental ability to support and promote resilient behaviors (r = −0.319, p < 0.001), and poorer child resilience (r = −0.249, p = 0.002) - Significant negative effect of parental ability to support and promote child resilient behaviors and child stress-related behaviors during the COVID-19 outbreak (b = −0.178, p = 0.011) |
|
Marzilli et al., 2021 Italy |
To explore whether parents’ peritraumatic distress due to COVID-19 and parenting stress simply and serially mediated the effects of parents’ past traumas exposure and parental resilience on children’s psychopathological difficulties. |
n = 353 caregivers Age Mage caregivers = 42.15 (SD = 8.09) Mage children = 9.28 (SD = 4.54) Sex – Caregivers Female (64%) Male (34%) Sex – Children Female (50.7%) Male (49.3%) |
Quantitative data collected via online questionnaire from October 2020-January 2021. Analyses included correlations, hierarchical multiple regression, and sequential mediation analyses. |
Parental resilience measured by the CD-RISC. Parental peritraumatic distress symptoms due to COVID-19 measured by the COVID-19 Peritraumatic Distress Index. Stress perceived in relationship with child and on child’s emotional-behavioural functioning measured by the Parenting Stress Index-Short Form. |
- Parents’ peritraumatic distress due to COVID-19 significantly associated with resilience (r = -0.27, p < 0.01) - Parents’ resilience significantly predicted low levels of parent’s peritraumatic distress due to COVID-19 (B = -0.27, p < 0.001) and parenting stress (B = -0.24, p < 0.001) |
|
Mikocka-Walus et al., 2021 Australia |
To investigate the association between resilience and indicators of mental health in a large sample of Australian parents at the time of the COVID-19 pandemic. |
n = 2110 caregivers Age Mage caregivers = 38.25 (SD = 7.07) Gender – Caregivers Female (80.6%) Male (19.4%) |
Quantitative data collected via online questionnaire during April 2020. Analysis included hierarchical regression models. |
Parental resilience measured by The Brief Resilience Scale (BRS). Parent symptoms of depression, anxiety, and stress measured by the DASS-21. |
- Low resilience in parents was negatively correlated with anxiety (b = -0.231, p < 0.05) |
|
Nasir et al., 2021 Indonesia |
To evaluate the resilience of parents accompanying schoolchildren in online learning. |
n = 392 caregivers Age Caregiver Range = 22-42 Gender – Caregivers Female (73.65%) Male (26.35%) Gender – Children Female (53.70%) Male (46.30%) |
Quantitative data collected via online questionnaire from April-May 2021. Analysis included regression. |
Parental resilience measured by the CD-RISC-25. Parents’ socioeconomic conditions measured via demographic questionnaire. |
- Significant relationship between economic status and resilience of parents in accompanying children to participate in online learning (F = 9.010, p = 0.00) |
|
Romero et al., 2020 Spain |
To examine the effects of the Spanish confinement derived from the COVID-19 crisis on children and their families, accounting for child’s age. |
n = 1049 caregivers n = 1049 children Age Mage children = 7.26 (SD = 2.39) Gender – Caregivers Female (89.6%) Male (9.7%) Other (0.70%) Sex – Children Female (50.4%) Male (49.6%) |
Quantitative data collected via questionnaire as part of the larger Confinement Effects on Families and Children (CONFIA-20) study in April 2020. Analyses included correlations, prevalence rates of change, and a path analysis. |
Parental resilience measured by the CD-RISC-10. Child negative outcomes measured by the SDQ. Child positive outcomes measured by an ad hoc scale. SES of parents was indexed through parental level of education, based on the average of the father’s and mother’s educational level, and family economic level, based on parent-report of family income. |
- Family SES was positively related with parental resilience (r = 0.14, p < 0.001) - Parents’ dispositional resilience exerted a negative effect on perceived distress which positively affected parents’ depression and anxiety (ß = -0.40, p < 0.001) - Parents’ distress was negatively correlated with their overall resilience (ß = -0.40, p < 0.001) and correlated with conduct problems (r = 0.45, p < 0.001), emotional problems (r = 0.32, p < 0.001), and hyperactivity (r = 0.48, p < 0.001) of children |
|
Russell et al., 2022 United States |
To examine the associations between resilience, mental health and stress indicators, and parenting out- comes (caregiver burden and parent–child relationship qualities) over a 30-day period during the COVID-19 pandemic. |
n = 271 caregivers n = 95 children Age Mage caregivers = 35.29 Sex – Caregivers Female (45.8%) Male (54.2%) |
Quantitative data collected via online questionnaire from April-May 2020. Analyses included bivariate correlations, t-tests, ANOVA, and path analyses. |
Parental resilience measured by the ARM. Relationship quality measured by 15-item Child-Parent Relationship Scale. Caregiver/child stress measured by Perceived Stress Scale-Adult/Child. COVID-19 financial stressors measured by ad hoc scale. |
- Child-parent relationship conflict at the 30-day follow-up was negatively associated with baseline resilience (r = -0.25, p < 0.01; r = -0.29, p < 0.01) - Child-parent relationship closeness at the 30-day follow-up was positively associated with baseline resilience (r = 0.55, p < 0.01) - Parents whose financial needs were met reported significantly higher rates at baseline of resilience (t = -3.76, p < 0.01) - Caregiver resilience was negatively associated with parent stress (β = -0.44 and -0.55), and parent perceived child stress (β = -0.46 and -0.34), for female and male caregivers, respectively |
|
Sorkkila & Aunola, 2021 Finland |
To assess how resilience, on the one hand, and how relevant background variables on the other hand, are associated with parental burnout during the COVID-19 lockdown. |
n = 1105 caregivers Age Mage caregivers = 39.6 (SD = 7.05) Sex – Caregivers Female (88%) Male (22%) |
Quantitative data collected via online questionnaire from April-May 2020. Analyses included structural equation modelling and latent profile analysis. |
Parental resilience measured by BRS. Parental burnout measured by Parental Burnout Assessment. Financial situation measured by ad hoc scale on unemployment and perceived family income. |
- Poor financial situation significant predictor of parental burnout (r = 0.09, p < 0.01) and resilience (r = -0.20, p < 0.001) - Resilience negatively correlated with parental burnout (r = -0.48, p < 0.001), explained 19% of variation in parental burnout |
|
Touloupis, 2021 Greece |
To investigate the type of parental involvement in the homework of children during distance learning in the period of COVID-19 pandemic and the role of parents' fear of COVID-19 and resilience in their involvement in homework. |
n = 271 caregivers Sex – Caregivers Female (51.7%) Male (48.3%) Sex – Children Female (44%) Male (56%) |
Quantitative data collected via online questionnaire from March-April and November 2020. Analyses included MANOVAs, correlations, and a path analysis. |
Parental resilience measured by CD-RISC-10. Parental involvement in homework measured by ad hoc scale split into two factors: support and control. Parent’s fear of COVID-19 measured by the Fear of COVID-19 Scale (FCV-19S). |
- Negative correlation between parents’ fear of COVID-19 and resilience (r = -0.518, p < 0.01) and parental control and resilience (r = -0.301, p < 0.01) - Parental support positively correlated with resilience (r = 0.398, p < 0.01) - Parents' fear of COVID-19 indirectly and positively predicts their control in homework through their sense of resilience (Z4 = −2.39, p < .05) |
| Grey Literature (n = 2) | |||||
|
Mental Health Commission of Canada, 2021 Canada |
To provide guidance to decision makers, systems planners, and policy makers about ways to support infants, young children, and their families in light of the mental health needs emerging from or being worsened by the COVID-19 pandemic. | NA | Policy Brief |
Divided into: 1. Considerations 2. Options for Promotion and Prevention 3. Strategic Investments, Accountability, and Progress |
- Positive child development is reliant on quality relationships with parents, but parents have fewer resources available to help them cope (e.g., psychologically, financially), causing a breakdown of family relationships - Financial stress and economic insecurity affect mental health, but also parent-child relationships and parenting behaviours - Financial stress identified as one of the most frequent mental health stressors associated with COVID |
|
Public Health Agency of Canada, 2020 Canada |
To examine the state of public health in Canada and to stimulate dialogue about issues critical to the health of Canadians. | NA | Public Health Report | Direct and indirect impacts of COVID-19 on the health and well-being of people in Canada |
- Of jobs lost in March-April, employees in lower-wage jobs (i.e., lower than two-thirds of the 2019 annual median wage of $24.04) suffered the greatest losses (38%) compared to those in other jobs - These job losses disproportionately affected women with small children |
Methods of Analyses
The goal of this review was to bring together findings from the included studies as such, both numerical and thematic analyses were undertaken. Numerical analysis was used to identify the nature, distribution, and extent of studies included in this review. Thematic analysis was employed to inform our understanding of the context, related constructs, and outcomes for resilience among caregivers and children, as well as their SES during the COVID-19 pandemic. Both analyses were completed independently by the two authors, following which results were compared. First, data were synthesized by charting and sorting material from the data extraction table according to key themes. For thematic analysis, inductive content analysis according to Patton (2005), was conducted whereby emerging themes were independently identified based on all research included. Afterwards, both researchers met to compare themes and an iterative process was employed wherein emergent themes were compared to ascertain if themes were common between the dyad and final decisions were agreed upon to resolve all themes. Together, both the numerical and thematic analysis produced information highlighting consistencies and differences across studies regarding the outcomes of interest while providing an overview of the current status of the literature regarding caregiver/child resilience and SES in the context of COVID-19.
Results
Numerical Analysis
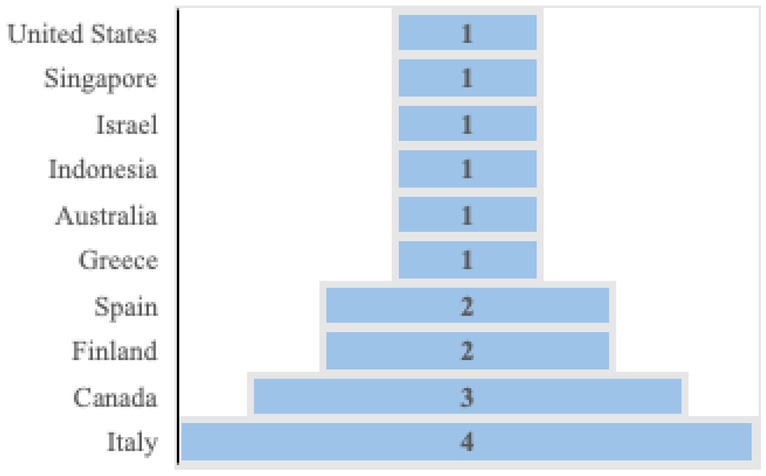
The 17 studies included in this review represented 2,425 children (Mage = 8.23) and 8,252 caregivers (Mage = 40.79). While both mothers and fathers were represented in this analysis, the majority of caregivers (80.95%) were female. Additionally, ten countries were represented in this review (see Table 2 for a full summary).
Table 2.
Country of Origin of Included Studies
Study Design
Of the 17 studies included, 13 were quantitative (Caputi et al., 2021; Cusinato et al., 2020; Dominguez-Alvarez et al., 2020; Laufer & Bitton, 2021; Lim et al., 2021; Mariani Wigley et al., 2021; Marzilli et al., 2021; Mikocka-Walus et al., 2021; Nasir et al., 2021; Romero et al., 2020; Russell et al., 2022; Sorkkila & Aunola, 2021; Touloupis, 2021), two were qualitative (Guruge et al., 2021; Koskela et al., 2020), one was a policy brief (Mental Health Commission of Canada, 2021), and one was a public health report (PHAC, 2020). The quantitative studies all used cross-sectional data collection except for Russel and colleagues (2022), who collected data at baseline and a 30-day follow-up. Two quantitative studies used retrospective data reports (Lim et al., 2021; Mactavish et al., 2021), and there were no control groups used in any of the quantitative studies. Phenomenology was used for both qualitative studies.
Outcome Measures
Caregiver resilience was measured using the CD-RISC (n = 8; Connor & Davidson, 2003), BRS (n = 2; Smith et al., 2008), and ARM (n = 2; Liebenberg & Moore, 2018), while child resilience was measured in three studies, all of which used the CYRM (Ungar & Liebenberg, 2011). Parental and/or family SES was conceptualized and measured in a variety of ways including: (1) parent education, family income, and family financial solvency to face daily overheads (Dominguez-Alvarez et al., 2020); (2) personal accounts of financial resources (Guruge et al., 2021; Koskela et al., 2020); (3) concern regarding financial situations due to the COVID-19 pandemic (Laufer & Bitton, 2021); (4) financial stability (Lim et al., 2021); (5) socioeconomic conditions (Nasir et al., 2021); (6) parental level of education, based on the average of the father’s and mother’s educational level, and family economic level, based on parent-report of family income (Romero et al., 2020); (7) COVID-19 financial stressors (Russell et al., 2022); unemployment and perceived family income (Sorkkila & Aunola, 2021); and (8) measuring the direct and indirect impacts of COVID-19 on health (PHAC, 2020).
Thematic Analysis
Thematic analysis revealed five themes related to child and caregiver resilience and SES included: (1) the mitigating effects of child resilience; (2) overcoming the psychological toll of the pandemic; (3) the unknown relationship: caregiver and child resilience; (4) family functioning during COVID-19; and (5) the perfect storm for socioeconomic impacts (for definitions of each theme see Table 3).
Table 3.
Themes and Associated Definitions
| Theme | Definition |
|---|---|
| (1) The mitigating effects of child resilience | The ability for resilience among children to mitigate negative impacts on day-to-day life resulting from the pandemic |
| (2) Overcoming the psychological toll of the pandemic | The ability for caregivers’ resilience to overcome the psychological toll of the pandemic |
| (3) The unknown relationship: Caregiver and child resilience | The contradictory findings regarding the relationship between caregiver and child resilience whereby some authors reported significant correlations between the resilience of these two groups and others reported no correlations |
| (4) Family functioning during COVID-19 | The key factors that allowed families to adapt and continue functioning during the ongoing adversities of the COVID-19 pandemic, including positive coping mechanisms, quality caregiver-child relationships, and family resilience |
| (5) The perfect storm for socioeconomic impacts | Pandemic-related impacts to socioeconomic factors (e.g., income, employment) and the role resilience played |
The Mitigating Effects of Child Resilience
A total of four studies examined child resilience and reported that childhood resilience reduced negative outcomes throughout the pandemic (Caputi et al., 2021; Cusinato et al., 2020; Dominguez-Alvarez et al., 2020; Mariani Wigley et al., 2021). Specifically, high resilience scores among children, based on the CYRM or parent-report, were associated with lower total difficulties, stress-related behaviours, and the impact of the pandemic on the overall wellbeing of children (Caputi et al., 2021; Cusinato et al., 2020; Mariani Wigley et al., 2021). Findings from these studies demonstrated children’s resilience reduced negative emotional symptoms, hyperactivity, conduct problems, and peer relationship problems (Caputi et al., 2021; Cusinato et al., 2020; Mariani Wigley et al., 2021). Furthermore, children high in resilience were more likely to engage in positive coping mechanisms responding to the pandemic, including active problem solving and seeking social support (Dominguez-Alvarez et al., 2020). Although authors from these studies only reported moderate resilience scores among their children, the benefits of resilience on mitigating pandemic-related outcomes were still found.
Overcoming the Psychological Toll of the Pandemic
Seven studies explored caregiver resilience and the psychological toll of the pandemic (Laufer & Bitton, 2021; Lim et al., 2021; Marzilli et al., 2021; Mikocka-Walus et al., 2021; Romero et al., 2020; Russell et al., 2022; Sorkkila & Aunola, 2021). Based on the overall depression, anxiety, and stress screens reported in these studies, it was evident caregivers experienced psychological distress throughout the pandemic (Laufer & Bitton, 2021; Lim et al., 2021; Marzilli et al., 2021; Mikocka-Walus et al., 2021; Romero et al., 2020; Russell et al., 2022). However, these studies reported caregiver resilience was negatively correlated to depression, anxiety, stress, and overall distress, making it likely that resilience among caregivers was an important factor in psychological toll of the pandemic. Given this relationship between resilience and psychological distress, it is unsurprising that resilience protected caregivers from burnout (Sorkkila & Aunola, 2021).
The Unknown Relationship: Caregiver and Child Resilience
Only two studies discussed the direct relationship between caregiver and child resilience and authors reported conflicting findings (Caputi et al., 2021; Mariani Wigley et al., 2021). Specifically, Caputi and colleagues (2021) noted a significant positive correlation between caregiver and child resilience (r = 0.49, p < 0.01) while Mariani Wigley and colleagues (2021) noted no significant correlation. As such, it remains unknown the relationship between caregiver and child resilience and the role it plays in the ability of families to adapt to ongoing changes during the pandemic.
Family Functioning during COVID-19
Nine studies examined factors contributing to overall family functioning during the COVID-19 pandemic including: supporting positive coping mechanisms, quality caregiver-child relationships, and family resilience (Caputi et al., 2021; Dominguez-Alvarez et al., 2020; Guruge et al., 2021; Koskela et al., 2020; Mariani Wigley et al., 2021; Mental Health Commission of Canada, 2021; Romero et al., 2020; Russell et al., 2022; Touloupis, 2021). Each of which will be discussed in turn.
Positive Coping Mechanisms
The importance of positive coping mechanisms among children (e.g., ability to regulate conduct and emotional problems) was positively correlated to caregiver resilience, with several studies addressing how caregivers can support these strategies in children (Dominguez-Alvarez et al., 2020; Romero et al., 2020; Russell et al., 2022). Supporting children to use positive coping mechanisms was found most commonly among caregivers high in resilience and low in psychological distress (Dominguez-Alvarez et al., 2020; Romero et al., 2020; Russell et al., 2022). Further, caregivers who taught positive coping mechanisms to children resulted in a positive correlation to children’s resilience (Mariani Wigley et al., 2021). Together, children employing positive coping strategies and caregivers and children being high in resilience led to lower stress-related behaviours among children and caregivers, thus improving family functioning during the pandemic.
Quality of Caregiver-Child Relationship
Despite the toll of the pandemic on families, the quality of family relationships had a positive impact on child development (Mental Health Commission of Canada, 2021). The quality of these relationships was noted as depending on support provided by caregivers, relationship closeness, and growth within caregiver-child relationships (Guruge et al., 2021; Mental Health Commission of Canada, 2021; Russell et al., 2022; Touloupis, 2021). These three aspects of family relationships were found to be positively related to caregiver resilience such that those caregivers high in resilience were able to provide higher quality relationships, resulting in benefits to child development (Guruge et al., 2021; Mental Health Commission of Canada, 2021; Russell et al., 2022; Touloupis, 2021).
Family Resilience
Family resilience, conceptualized as the ability for families to bounce back during the pandemic, was instrumental in family functioning. Families with high levels of resilience were better able to follow routines, use the resources available to them, adapt to changes, and find creative ways to problem solve – all of which contribute to families being positioned to thrive throughout the pandemic (Koskela et al., 2020).
The Perfect Storm for Socioeconomic Impacts
Ten studies highlighted how socioeconomic factors (e.g., income, employment) were impacted by the pandemic and that caregiver resilience played a role (Dominguez-Alvarez et al., 2020; Koskela et al., 2020; Laufer & Bitton, 2021; Lim et al., 2021; Mental Health Commission of Canada, 2021; Nasir et al., 2021; PHAC, 2020; Romero et al., 2020; Russell et al., 2022; Sorkkila & Aunola, 2021). The majority of caregivers were concerned about financial stability and reported psychological distress and behavioural issues among children (Laufer & Bitton, 2021; Lim et al., 2021; Mental Health Commission of Canada, 2021; PHAC, 2020). It was also reported that, compared to other adult populations, caregivers with school-aged children and those in lower-wage jobs faced a disproportionate rate of job losses (PHAC, 2020). The importance of access to external resources (e.g., flexible employers, financial support) was identified as essential to caregiver resilience (Koskela et al., 2020; Mental Health Commission, 2021). Family SES and the perceived economic impact of COVID-19 was noted by many as being a key factor determining caregivers’ resilience and the support they were able to provide to their children. Specifically, caregivers with high SES who perceived the economic impact of COVID-19 to be low reported higher resilience scores, were better able to support their children, and reported less psychological distress compared to caregivers with low SES (Dominguez-Alvarez et al., 2020; Nasir et al., 2021; Romero et al., 2020; Russell et al., 2022; Sorkkila & Aunola, 2021).
Discussion
The purpose of this systematic review was to (1) explore what is currently known about the relationship between caregiver and child resilience in the context of COVID-19; and (2) examine the role of SES on caregiver or child resilience throughout the COVID-19 pandemic. Globally, children high in resilience are better able to reduce negative outcomes throughout the pandemic (e.g., stress-related behaviours, negative emotional symptoms, peer relationship problems). Further, high resilience among caregivers was a protective factor against psychological impacts of the pandemic on caregivers such as depression, anxiety, and stress. Despite these protective benefits, it remains unknown whether the interaction between both caregiver and child resilience have played a role in these groups independently and collectively adapting to ongoing fluctuations during the pandemic. What has been established is that family functioning throughout the pandemic was dependent upon positive coping mechanisms, the quality of caregiver-child relationships, and family resilience. Finally, the SES of many families was impacted throughout the pandemic and the perceived severity of this impact fluctuated depending on the resilience of caregivers.
Similar to the findings of this review that children’s ability to positively cope and be resilient is related to family functioning, Berger and colleagues (2021) reported that children are able to be resilient during infectious disease outbreaks when parents provide ongoing support. Regarding the ongoing COVID-19 pandemic however, Lateef and co-authors (2021) have highlighted the dearth of research on the consequences of pandemics on children and youth. Future research should focus on the long-term impacts of the pandemic on the resilience and overall well-being of children to ensure that future policy decisions are supporting children with what they need to bounce back from adversities.
The psychological toll that the pandemic has had on caregivers was also highlighted in the recent review of 29 articles by Lateef and colleagues (2021) who reported that caregivers were experiencing greater levels of psychosocial problems than adults without children. Given the abundance of evidence presented in the current review surrounding the relationship between these psychological problems and the resilience of caregivers, it is likely that the resilience of caregivers may have been impacted to a greater degree than their non-parent counterparts throughout the pandemic. Based on the heightened impact of the pandemic on the psychological wellbeing and resilience of caregivers, there is a need for future policy directions to focus on supporting caregivers immediately in future iterations of the pandemic to allow caregivers the additional assistance they need above and beyond other adults to move through adverse circumstances.
Similar to the findings of this review regarding the economic burden of the pandemic on families, Prime et al. (2020) found that low-income families and those with young children have been disproportionately impacted by loss of income. Financial stressors facing caregivers were noted to be common throughout the pandemic, including high rates of unemployment, the collapse of economic markets, and inadequate financial relief packages. These economic concerns coincided with other pandemic stressors (e.g., burden on caregivers to meet educational needs of children, change in work roles/routines), resulting in higher distress among caregivers and worse behavioural adjustment among children (Gallitto, 2020; Prime et al., 2020). Future research should investigate factors that could alleviate the economic burdens facing caregivers throughout the pandemic, paying particular attention to those families of low SES.
This study is the first systematic review synthesizing what is currently known about caregiver and child resilience and SES during the COVID-19 pandemic and revealed that resilience served as a protective factor against some negative impacts of the pandemic (e.g., stress-related behaviours, anxiety, depression, perceived economic impacts). While other reviews exist in this subject area, to the authors’ knowledge this is the first to review literature pertaining to the interaction between the resilience of both caregivers and young children. Moreover, this review is differentiated by others by taking into account the impacts of SES that may have been largely disrupted throughout the COVID-19 pandemic. However, the findings of this review should be considered within the context of the limitations. The majority of the articles included in this review presented cross-sectional data limiting the ability to infer causation, accurately interpret associations, and evaluate the temporal relation between outcomes (Wang & Cheng, 2020). Given the varying ways in which economic impacts were experienced in different countries (e.g., high, middle, low income) throughout the pandemic, future research in this area should collect longitudinal data in each of these regions to provide a more fulsome picture of the economic impacts experienced by families during COVID-19. Some of the themes from this review were based on the limited number of studies that explored this topic (e.g., the unknown relationship: caregiver and child resilience; n = 2), which increases the potential of bias and therefore findings need to be cautiously interpreted and replicated in future studies. Finally, all of the data presented on child resilience is based on parent-report, despite validated scales existing that can measure resilience among this age demographic (e.g., True Resilience Scale for Children; Wagnild, 2009). As such, child resilience data is subject to implicit parental biases. Future studies should assess resilience from the perspective of children to provide a more accurate depiction of the pandemic’s impact on their resilience.
Conclusion
In the global context, this review revealed that the resilience of caregivers and their children, as well as family functioning – comprised of positive coping mechanisms, quality relationships, and family resilience – allowed families to be better able to overcome pandemic adversities. Moreover, families were better positioned to be resilient when they faced few economic hardships. Given these findings, resilience may be thought of as a ‘privilege’ that is easier to achieve when one has the resources in place to do so. Policymakers need to prioritize reducing the economic burden (i.e., job losses, financial strain) on families with young children to support families in dealing with already stressful situations. When families no longer need to worry about economic hardships, caregivers and children will be better equipped to be resilient through adverse times.
Appendix A
Database Search Strategy
| Concept | Search Terms |
|---|---|
| 1. Caregivers | 1. (caregiver* or care giver* or parent* or caretaker* or guardian*).mp. [mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] |
| 2. Children | 2. (child* or kid*).mp. [mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] |
| 3. Resilience | 3. exp Resilience, Psychological/ or Resilien*.mp |
| 4. COVID-19 |
4. COVID-19/ or exp COVID-19 Testing/ or COVID-19 Vaccines/ or SARS-CoV-2/ 5. (coronavirus/ or betacoronavirus/ or coronavirus infections/) and (disease outbreaks/ or epidemics/ or pandemics/) 6. (nCoV* or 2019nCoV or 19nCoV or COVID19* or COVID or SARS-COV-2 or SARSCOV-2 or SARS-COV2 or SARSCOV2 or SARS coronavirus 2 or Severe Acute Respiratory Syndrome Coronavirus 2 or Severe Acute Respiratory Syndrome Corona Virus 2).ti,ab,kf,nm,ot,ox,rx,px 7. (longCOVID* or postCOVID* or postcoronavirus* or postSARS*).ti,ab,kf,ot 8. ((coronavirus* or corona virus* or betacoronavirus*) adj3 (pandemic* or epidemic* or outbreak* or crisis)).ti,ab,kf,ot 9. ((Wuhan or Hubei) adj5 pneumonia).ti,ab,kf,ot 10. or/4–9 |
| 11. 1 and 2 and 3 and 10 |
Appendix B
List of Excluded Studies and Reasons for Exclusion
| Reason for Exclusion | Authors of Excluded Studies |
|---|---|
| Resilience in caregivers and/or children not discussed in results | Ajanovic et al., 2021; Ashikkali et al., 2020; Brunelli et al., 2021; Cauberghe et al., 2021; Crescentini et al., 2020; Daks et al., 2020; Erdei & Liu, 2020; Fegert et al., 2020; Johnson et al., 2021; Kamran & Naeim, 2021; Levine, 2020; Mactavish et al., 2021; Marchetti et al., 2020; Matiz et al., 2022; Nicolaidou et al., 2021; O’Keefe et al., 2021; Parrott et al., 2021; Peris & Ehrenreich-May, 2021; Rabbani et al., 2021; Roubinov et al., 2020; Schrooyen et al., 2021; Steinberg et al., 2021; A L van Tilburg et al., 2020; Vertsberger et al., 2022; White et al., 2021; Williams, 2020; Wu et al., 2021 |
| Study not conducted in the COVID-19 context | Kim et al., 2020; Pandya, 2019; Schneider et al., 2021 |
| Mean age of children outside of 7–10 range | Andres-Romero et al., 2021; Archer et al., 2021; Asscheman et al., 2021; Bates et al., 2021; Biden et al., 2021; Bryson et al., 2021; Davidson et al., 2021; Eales et al., 2021; Feng et al., 2020; Gibbons et al., 2021; Hatzichristou et al., 2021; Herbert et al., 2020; Hong et al., 2021; Iovino et al., 2021; Jungmann et al., 2021; Kohler-Dauner et al., 2021; Lawrence et al., 2021; Luthar et al., 2020; Mitra et al., 2021; Montirosso et al., 2021; Nikolaidis et al., 2021; Ruiz et al., 2020; Tang et al., 2021; Thibodeau-Nielsen et al., 2021; Tokatly Latzer et al., 2021; Tso et al., 2020; Wang et al., 2021; Wimberly et al., 2021; Wong et al., 2020; Zhang et al., 2022; |
| Article is not primary research or grey literature | Berger et al., 2021; Lateef et al., 2021; Prime et al., 2020; Reid et al., 2021; Zilberstein et al., 2021 |
Data Availability
All data generated or analyzed during this study are included in this published article.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
The Canadian Agency for Drugs and Technologies in Health (CADTH) COVID-19 search string was used in each respective database to ensure all variations of COVID literature were included in the search results. These CADTH search strings were developed and peer-reviewed by Research Information Specialists and are continuously updated as new research emerges (CADTH, 2021).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. The Lancet Respiratory Medicine. 2020;8(7):659–661. doi: 10.1016/S2213-2600(20)30234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajanovic S, Garrido-Aguirre J, Baro B, Balanza N, Varo R, Millat-Martinez P, Arias S, Fonollosa J, Perera-Lluna A, Jordan I, Munoz-Almagro C, Bonet-Carne E, Crosas-Soler A, Via E, Nafria B, Garcia-Garcia JJ, Bassat Q. How did the COVID-19 lockdown affect children and adolescent’s well-being: Spanish parents, children, and adolescents respond. Frontiers in Public Health. 2021;9(101616579):746052. doi: 10.3389/fpubh.2021.746052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andres-Romero MP, Flujas-Contreras JM, Fernandez-Torres M, Gomez-Becerra I, Sanchez-Lopez P. Analysis of psychosocial adjustment in the family during confinement: Problems and habits of children and youth and parental stress and resilience. Frontiers in Psychology. 2021;12(101550902):647645. doi: 10.3389/fpsyg.2021.647645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archer J, Reiboldt W, Claver M, Fay J. Caregiving in quarantine: Evaluating the impact of the Covid-19 pandemic on adult child informal caregivers of a parent. Gerontology & Geriatric Medicine. 2021;7(101662571):2333721421990150. doi: 10.1177/2333721421990150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashikkali L, Carroll W, Johnson C. The indirect impact of COVID-19 on child health. Paediatrics and Child Health. 2020;30(12):430–437. doi: 10.1016/j.paed.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asscheman JS, Zanolie K, Bexkens A, Bos MGN. Mood variability among early adolescents in times of social constraints: A daily diary study during the COVID-19 pandemic. Frontiers in Psychology. 2021;12(101550902):722494. doi: 10.3389/fpsyg.2021.722494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates CR, Nicholson LM, Rea EM, Hagy HA, Bohnert AM. Life interrupted: Family routines buffer stress during the COVID-19 pandemic. Journal of Child and Family Studies. 2021;9214438:1–11. doi: 10.1007/s10826-021-02063-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger E, Jamshidi N, Reupert A, Jobson L, Miko A. Review: The mental health implications for children and adolescents impacted by infectious outbreaks—A systematic review. Child and Adolescent Mental Health. 2021;26(2):157–166. doi: 10.1111/camh.12453. [DOI] [PubMed] [Google Scholar]
- Biden EJ, Greenwood CJ, Macdonald JA, Spry EA, Letcher P, Hutchinson D, Youssef GJ, McIntosh JE, Olsson CA. Preparing for future adversities: lessons from the COVID-19 pandemic in Australia for promoting relational resilience in families. Frontiers in Psychiatry. 2021;12(101545006):717811. doi: 10.3389/fpsyt.2021.717811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black K, Lobo M. A conceptual review of family resilience factors. Journal of Family Nursing. 2008;14(1):33–55. doi: 10.1177/1074840707312237. [DOI] [PubMed] [Google Scholar]
- Bridgland, V. M. E., Moeck, E. K., Green, D. M., Swain, T. L., Nayda, D. M., Matson, L. A., Hutchinson, N. P., & Takarangi, M. K. T. (2021) Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE 16(1). 10.1371/journal.pone.0240146 [DOI] [PMC free article] [PubMed]
- Brunelli, A., Silvestrini, G., Palestini, L., Vitali, P., Nanni, R., Belluzzi, A., Ciambra, R., De Logu, M., Degli Angeli, M., Dessi, F. L., Donati, D., Gaspari, L., Ghini, T., Giovannini, M., Iaia, M., Mazzini, F., Mollace, R., Nanni, V., Perra, A. P., & Marchetti, F. (2021). [Impact of the lockdown on children and families: A survey of family pediatricians within a community.]. Impatto Del Lockdown Sui Bambini e Sulle Famiglie: Un’indagine Dei Pediatri Di Famiglia All’interno Di Una Comunita., 112(3), 207–215. 10.1701/3565.35460 [DOI] [PubMed]
- Bryson H, Mensah F, Price A, Gold L, Mudiyanselage SB, Kenny B, Dakin P, Bruce T, Noble K, Kemp L, Goldfeld S. Clinical, financial and social impacts of COVID-19 and their associations with mental health for mothers and children experiencing adversity in Australia. PloS One. 2021;16(9):e0257357. doi: 10.1371/journal.pone.0257357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CADTH. (2021). CADTH COVID-19 Search Strings. Retrieved September 23, 2021. https://covid.cadth.ca/literature-searching-tools/cadth-covid-19-search-strings/
- Caputi M, Forresi B, Giani L, Michelini G, Scaini S. Italian Children’s Well-Being after Lockdown: Predictors of Psychopathological Symptoms in Times of COVID-19. International Journal of Environmental Research and Public Health. 2021;18(21):11429. doi: 10.3390/ijerph182111429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll, N., Sadowski, A., Laila, A., Hruska, V., Nixon, M., Ma, D. W. L., & Haines, J. (2020). The impact of COVID-199 on helath behaviour, stress, financial and food security among middle to high income Canadian families with young children. Nutrients, 12(2352). 10.3390/nu12082352 [DOI] [PMC free article] [PubMed]
- Cauberghe V, De Jans S, Hudders L, Vanwesenbeeck I. Children’s resilience during Covid-19 confinement. A child’s perspective-which general and media coping strategies are useful? Journal of Community Psychology. 2021;0367033:huu, 0367033. doi: 10.1002/jcop.22729. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC]. (2020). COVID-19 in racial and ethnic minority groups. Retrieved October 1, 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnicminorities.html
- Chen CY-C, Byrne E, Vélez T. Impact of the 2020 pandemic of COVID-19 on Families with School-aged Children in the United States: Roles of Income Level and Race. Journal of Family Issues. 2022;43(3):719–740. doi: 10.1177/0192513X21994153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC) Depression and Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Cost KT, Crosbie J, Anagnostou E, Birken CS, Charach A, Monga S, Kelley E, Nicolson R, Maguire JL, Burton CL, Schachar RJ, Arnold PD, Korczak DJ. Mostly worse, occasionally better: Impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. European Child & Adolescent Psychiatry. 2021 doi: 10.1007/s00787-021-01744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulombe S, Pacheco T, Cox E, Khalil C, Doucerain MM, Auger E, Meunier S. Risk and Resilience Factors During the COVID-19 Pandemic: A Snapshot of the Experiences of Canadian Workers Early on in the Crisis. Frontiers in Psychology. 2020 doi: 10.3389/fpsyg.2020.580702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covidence systematic review software. (2021). Veritas Health Innovation, Melbourne, Australia. Retrieved September 1, 2021. www.covidence.org
- Crann SE, Barata PC. The experience of resilience for adult female survivors of intimate partner violence: A phenomenological inquiry. Violence against Women. 2015 doi: 10.1177/1077801215612598. [DOI] [PubMed] [Google Scholar]
- Crescentini C, Feruglio S, Matiz A, Paschetto A, Vidal E, Cogo P, Fabbro F. Stuck outside and inside: an exploratory study on the effects of the COVID-19 outbreak on Italian parents and children’s internalizing symptoms. Frontiers in Psychology. 2020;11(101550902):586074. doi: 10.3389/fpsyg.2020.586074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Cusinato, M., Iannattone, S., Spoto, A., Poli, M., Moretti, C., Gatta, M., & Miscioscia, M. (2020). Stress, Resilience, and Well-Being in Italian Children and Their Parents during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 17(22). 10.3390/ijerph17228297 [DOI] [PMC free article] [PubMed]
- Daks JS, Peltz JS, Rogge RD. Psychological flexibility and inflexibility as sources of resiliency and risk during a pandemic: Modeling the cascade of COVID-19 stress on family systems with a contextual behavioral science lens. Journal of Contextual Behavioral Science. 2020;18(101616494):16–27. doi: 10.1016/j.jcbs.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson B, Schmidt E, Mallar C, Mahmoud F, Rothenberg W, Hernandez J, Berkovits M, Jent J, Delamater A, Natale R. Risk and resilience of well-being in caregivers of young children in response to the COVID-19 pandemic. Translational Behavioral Medicine. 2021;11(2):305–313. doi: 10.1093/tbm/ibaa124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominguez-Alvarez B, Lopez-Romero L, Isdahl-Troye A, Gomez-Fraguela JA, Romero E. Children Coping, Contextual Risk and Their Interplay During the COVID-19 Pandemic: A Spanish Case. Frontiers in Psychology. 2020;11(101550902):577763. doi: 10.3389/fpsyg.2020.577763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L, Shao X, Wang Y, Huang Y, Miao J, Yang X, Zhu G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. Journal of Affective Disorders. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eales L, Ferguson GM, Gillespie S, Smoyer S, Carlson SM. Family resilience and psychological distress in the COVID-19 pandemic: A mixed methods study. Developmental Psychology. 2021;57(10):1563–1581. doi: 10.1037/dev0001221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdei C, Liu CH. The downstream effects of COVID-19: A call for supporting family wellbeing in the NICU. Journal of Perinatology : Official Journal of the California Perinatal Association. 2020;40(9):1283–1285. doi: 10.1038/s41372-020-0745-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng, Z., Xu, L., Cheng, P., Zhang, L., Li, L.-J., & Li, W.-H. (2020). The psychological impact of COVID-19 on the families of first-line rescuers. Indian Journal of Psychiatry, 62(Suppl 3), S438–S444. 10.4103/psychiatry.IndianJPsychiatry_1057_20 [DOI] [PMC free article] [PubMed]
- Fegert, J. M., Vitiello, B., Plener, P. L., & Clemens, V. (2020). Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry Mental Health, 14(20). 10.1186/s13034-020-00329-3 [DOI] [PMC free article] [PubMed]
- Fergus S, Zimmerman MA. Adolescent resilience: A framework for understanding healthy development in the face of risk. Annual Review of Public Health. 2005;26:399–419. doi: 10.1146/annurev.publichealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- Gallitto, E. (2020). Building resilience in children during the pandemic: The role of positive parenting. Interdisciplinary Research Laboratory on the Rights of the Child (IRLRC): University of Ottawa. Retrieved October 1, 2021. https://droitcivil.uottawa.ca/interdisciplinary-research-laboratory-rights-child/building-resilience-children-during-pandemic-role-positive-parenting
- Gavidia-Payne S, Denny B, Davis K, Francis A, Jackson M. Parental resilience: A neglected construct in resilience research. Clinical Psychologist. 2015;19(3):111–121. doi: 10.1111/cp.12053. [DOI] [Google Scholar]
- Gayatri M, Irawaty DK. Family resilience during COVID-19 pandemic: A literature review. The Family Journal. 2021 doi: 10.1177/10664807211023875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons JL, Fernandez-Morales R, Maegli MA, Poelker KE. “Mi hijo es lo principal”—Guatemalan mothers navigate the COVID-19 pandemic. International Perspectives in Psychology: Research, Practice, Consultation. 2021;10(3):163–171. doi: 10.1027/2157-3891/a000017. [DOI] [Google Scholar]
- Guruge S, Lamaj P, Lee C, Ronquillo CE, Sidani S, Leung E, Ssawe A, Altenberg J, Amanzai H, Morrison L. COVID-19 restrictions: Experiences of immigrant parents in Toronto. AIMS Public Health. 2021;8(1):172–185. doi: 10.3934/publichealth.2021013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzichristou C, Georgakakou-Koutsonikou N, Lianos P, Lampropoulou A, Yfanti T. Assessing school community needs during the initial outbreak of the COVID-19 pandemic: Teacher, parent and student perceptions. School Psychology International. 2021;42(6):590–615. doi: 10.1177/01430343211041697. [DOI] [Google Scholar]
- Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerging infectious diseases. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert JS, Mitchell A, Brentnall SJ, Bird AL. Identifying rewards over difficulties buffers the impact of time in COVID-19 lockdown for parents in Australia. Frontiers in Psychology. 2020;11(101550902):606507. doi: 10.3389/fpsyg.2020.606507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong JY, Choi S, Cheatham GA. Parental stress of Korean immigrants in the U.S.: Meeting child and youth’s educational needs amid the COVID-19 pandemic. Children and Youth Services Review. 2021;127(8110100):106070. doi: 10.1016/j.childyouth.2021.106070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iovino EA, Caemmerer J, Chafouleas SM. Psychological distress and burden among family caregivers of children with and without developmental disabilities six months into the COVID-19 pandemic. Research in Developmental Disabilities. 2021;114(8709782, rid):103983. doi: 10.1016/j.ridd.2021.103983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MS, Skjerdingstad N, Ebrahimi OV, Hoffart A, Urnes Johnson S. Mechanisms of parental distress during and after the first COVID-19 lockdown phase: A two-wave longitudinal study. PloS One. 2021;16(6):e0253087. doi: 10.1371/journal.pone.0253087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jungmann T, Heinschke F, Federkeil L, Testa T, Klapproth F. Distance learning during the COVID-19 pandemic: Level of stress and coping strategies of parents with school-age children. Zeitschrift Fur Entwicklungspsychologie Und Padagogische Psychologie. 2021;53(3–4):71–81. doi: 10.1026/0049-8637/a000241. [DOI] [Google Scholar]
- Kalil, A., Mayerm S., & Shah, R. (2020). Impact of the COVID-19 crisis on family dynamics in economically vulnerable households. Becker Friedman Institute, 143.
- Kamran A, Naeim M. Managing back to school anxiety during a COVID-19 outbreak. The Journal of Nervous and Mental Disease. 2021;209(4):244–245. doi: 10.1097/NMD.0000000000001313. [DOI] [PubMed] [Google Scholar]
- Kim I, Dababnah S, Lee J. The influence of race and ethnicity on the relationship between family resilience and parenting stress in caregivers of children with autism. Journal of Autism & Developmental Disorders. 2020;50(2):650–658. doi: 10.1007/s10803-019-04269-6. [DOI] [PubMed] [Google Scholar]
- Kohler-Dauner F, Clemens V, Hildebrand K, Ziegenhain U, Fegert JM. The interplay between maternal childhood maltreatment, parental coping strategies as well as endangered parenting behavior during the current SARS-CoV-2 pandemic. Developmental Child Welfare. 2021;3(2):71–84. doi: 10.1177/25161032211014899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koskela T, Pihlainen K, Piispa-Hakala S, Vornanen R, Hämäläinen J. Parents’ Views on Family Resiliency in Sustainable Remote Schooling during the COVID-19 Outbreak in Finland. Sustainability. 2020;12(21):8844. doi: 10.3390/su12218844. [DOI] [Google Scholar]
- Lateef, R., Alaggia, R., & Collin-Vezina, D. (2021). A scoping review on psychosocial consequences of pandemics on parents and children: Planning for today and the future. Children and youth services review, 125(106002). 10.1016/j.childyouth.2021.106002 [DOI] [PMC free article] [PubMed]
- Laufer A, Bitton MS. Parents’ Perceptions of Children’s Behavioral Difficulties and the Parent-Child Interaction During the COVID-19 Lockdown. Journal of Family Issues. 2021 doi: 10.1177/0192513X211054460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence, K. C., Makhonza, L. O., & Mngomezulu, T. T. (2021). Assessing sources of resilience in orphans and vulnerable children in Amajuba District schools. South African Journal of Psychology.10.1177/00812463211062771
- Levine C. Vulnerable children in a dual epidemic. The Hastings Center Report. 2020;50(3):69–71. doi: 10.1002/hast.1140. [DOI] [PubMed] [Google Scholar]
- Liang L, Ren H, Cao R, Hu Y, Qin Z, Li C, Mei S. The effect of COVID-19 on youth mental health. Psychiatric Quarterly. 2020;91(3):841–852. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebenberg L, Moore JC. A social ecological measure of resilience for adults: The RRC-ARM. Social Indicators Research. 2018;136(1):1–19. doi: 10.1007/s11205-016-1523-y. [DOI] [Google Scholar]
- Li, F., Luo, S., Mu, W., Li, Y., Zheng, X., Xu, B., Ding, Y., Ling, P., Zhou, M., & Chen, X. (2021). Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry, 21(16). 10.1186/s12888-020-03012-1 [DOI] [PMC free article] [PubMed]
- *Lim, T. S. H., Tan, M. Y., Aishworiya, R., Kang, Y. Q., Koh, M. Y., Shen, L., & Chong, S. C. (2021). Correction to: Factors Contributing to Psychological Ill Effects and Resilience of Caregivers of Children with Developmental Disabilities During a Nationwide Lockdown During the COVID-19 Pandemic. Journal of Autism and Developmental Disorders, 7904301, hgw. 10.1007/s10803-021-05201-7 [DOI] [PMC free article] [PubMed]
- Liu, X., Kakade, M., Fuller, C. J., Fan, B., Fang, Y., Kong, J., Guan, Z., & Wu, P. (2012). Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive psychiatry, 53(1), 15–23. https://doi-org.proxy1.lib.uwo.ca/10.1016/j.comppsych.2011.02.003 [DOI] [PMC free article] [PubMed]
- Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, Linney C, McManus MN, Borwick C, Crawley E. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. Journal of the American Academy of Child & Adolescent Psychiatry. 2020;59:1218–1239. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Ebbert AM, Kumar NL. Risk and resilience during COVID-19: A new study in the Zigler paradigm of developmental science. Development and Psychopathology. 2021;33(2):565–580. doi: 10.1017/S0954579420001388. [DOI] [PubMed] [Google Scholar]
- Ma Z, Idris S, Zhang Y, Zewen L, Wali A, Ji Y, Pan Q, Baloch Z. The impact of COVID-19 pandemic outbreak on education and mental health of Chinese children aged 7–15 years: An online survey. BMC Pediatrics. 2021;21(1):95. doi: 10.1186/s12887-021-02550-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mactavish A, Mastronardi C, Menna R, Babb KA, Battaglia M, Amstadter AB, Rappaport LM. Children’s Mental Health in Southwestern Ontario during Summer 2020 of the COVID-19 Pandemic. Journal of the Canadian Academy of Child and Adolescent Psychiatry = Journal de l’Academie Canadienne de Psychiatrie de l’enfant et de l’adolescent. 2021;30(3):177–190. [PMC free article] [PubMed] [Google Scholar]
- Marchetti D, Fontanesi L, Mazza C, Di Giandomenico S, Roma P, Verrocchio MC. Parenting-related exhaustion during the Italian COVID-19 lockdown. Journal of Pediatric Psychology. 2020;45(10):1114–1123. doi: 10.1093/jpepsy/jsaa093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariani Wigley ILC, Mascheroni E, Bulletti F, Bonichini S. COPEWithME: The role of parental ability to support and promote child resilient behaviours during the COVID-19 emergency. Frontiers in Psychology. 2021 doi: 10.3389/fpsyg.2021.732745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques de Miranda D, da Silva AB, Sena Oliveira A, Simoes-e-Silva A. How is COVID-19 pandemic impacting mental health of children and adolescents? International Journal of Disaster Risk Reduction. 2020;51:101845. doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzilli E, Cerniglia L, Tambelli R, Trombini E, De Pascalis L, Babore A, Trumello C, Cimino S. The COVID-19 Pandemic and Its Impact on Families’ Mental Health: The Role Played by Parenting Stress, Parents’ Past Trauma, and Resilience. International Journal of Environmental Research and Public Health. 2021;18(21):11450. doi: 10.3390/ijerph182111450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matiz, A., Fabbro, F., Paschetto, A., Urgesi, C., Ciucci, E., Baroncelli, A., & Crescentini, C. (2022). The impact of the COVID-19 pandemic on affect, fear, and personality of primary school children measured during the second wave of infections in 2020. Frontiers in Psychiatry, 12. 10.3389/fpsyt.2021.803270 [DOI] [PMC free article] [PubMed]
- Maunula, L., Dabravolskaj, J., Maximova, K., Sim, S., Willows, N., Newton, A. S., & Veugelers, P. J. (2021). “It’s Very Stressful for Children”: Elementary School-Aged Children’s Psychological Wellbeing during COVID-19 in Canada. Children, 8(12). 10.3390/children8121185 [DOI] [PMC free article] [PubMed]
- Maximum City. (2021). COVID-19 child and youth well-being study: Canada Phase One Report. Retrieved September 23, 2021. https://maximumcity.ca/wellbeing
- *Mental Health Commission of Canada. (2021, June 25). COVID-19 and early childhood mental health: Fostering system change and resilience policy brief. Health Canada.https://mentalhealthcommission.ca/resource/covid-19-and-early-childhood-mental-health-fostering-systems-change-and-resilience-policy-brief/
- *Mikocka-Walus, A., Stokes, M., Evans, S., Olive, L., & Westrupp, E. (2021). Finding the power within and without: How can we strengthen resilience against symptoms of stress, anxiety, and depression in Australian parents during the COVID-19 pandemic?. Journal of Psychosomatic Research, 145(0376333, juv), 110433. 10.1016/j.jpsychores.2021.110433 [DOI] [PMC free article] [PubMed]
- Mitra R, Waygood EOD, Fullan J. Subjective well-being of Canadian children and youth during the COVID-19 pandemic: The role of the social and physical environment and healthy movement behaviours. Preventive Medicine Reports. 2021;23(101643766):101404. doi: 10.1016/j.pmedr.2021.101404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montirosso R, Mascheroni E, Guida E, Piazza C, Sali ME, Molteni M, Reni G. Stress symptoms and resilience factors in children with neurodevelopmental disabilities and their parents during the COVID-19 pandemic. Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association. 2021;40(7):428–438. doi: 10.1037/hea0000966. [DOI] [PubMed] [Google Scholar]
- Munoz RT, Brady S, Brown V. The psychology of resilience: A model of the relationship of locus of control to hope among survivors of intimate partner violence. Traumatology. 2017;23(1):102–111. doi: 10.1037/trm0000102. [DOI] [Google Scholar]
- Nasir A, Harianto S, Purwanto CR, Indrawait IR, Rohman M, Rahmawati PM, Putra P. The outbreak of COVID-19: Resilience and its predictors among parents of schoolchildren carrying out online learning in Indonesia. Clinical Epidemiology and Global Health. 2021 doi: 10.1016/j.cegh.2021.100890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolaidou I, Stavrou E, Leonidou G. Building primary-school children’s resilience through a web-based interactive learning environment: Quasi-experimental pre-post study. JMIR Pediatrics and Parenting. 2021;4(2):e27958. doi: 10.2196/27958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolaidis A, Paksarian D, Alexander L, Derosa J, Dunn J, Nielson DM, Droney I, Kang M, Douka I, Bromet E, Milham M, Stringaris A, Merikangas KR. The Coronavirus Health and Impact Survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Scientific Reports. 2021;11(1):8139. doi: 10.1038/s41598-021-87270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Keefe VM, Maudrie TL, Ingalls A, Kee C, Masten KL, Barlow A, Haroz EE. Development and dissemination of a strengths-based indigenous children’s storybook: “Our smallest warriors, our strongest medicine: overcoming covid-19”. Frontiers in Sociology. 2021;6(101777459):611356. doi: 10.3389/fsoc.2021.611356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés M, Espada J, Delvecchio E, Francisco R, Mazzeschi C, Pedro M, Morales A. Anxiety and depressive symptoms in children and adolescents during COVID-19 pandemic: A transcultural approach. Psicothema. 2021;33(1):125–130. doi: 10.7334/psicothema2020.287. [DOI] [PubMed] [Google Scholar]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2020). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021, 372(71). 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed]
- Pandya SP. Spiritual education programme for primary caregiver parents to build resilience in children with acute anxiety symptoms: A multicity study. Child & Family Social Work. 2019;24(2):309–320. doi: 10.1111/cfs.12616. [DOI] [Google Scholar]
- Paré G, Trudel M-C, Jaana M, Kitsiou S. Synthesizing information systems knowledge: A typology of literature reviews. Information & Management. 2015;22(2):183–199. doi: 10.1016/j.im.2014.08.008. [DOI] [Google Scholar]
- Parrott J, Armstrong LL, Watt E, Fabes R, Timlin B. Building resilience during COVID-19: Recommendations for adapting the DREAM Program—live edition to an online-live hybrid model for in-person and virtual classrooms. Frontiers in Psychology. 2021;12(101550902):647420. doi: 10.3389/fpsyg.2021.647420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton MQ. Qualitative Research. Sage; 2005. [Google Scholar]
- Peris TS, Ehrenreich-May J. The parents are not alright: A call for caregiver mental health screening during the COVID-19 pandemic. Journal of the American Academy of Child and Adolescent Psychiatry. 2021;60(6):675–677. doi: 10.1016/j.jaac.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. The American Psychologist. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- *Public Health Agency of Canada [PHAC]. (2020, October). From risk to resilience: An equity approach to COVID-19. Government of Canada. https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19.html
- Rabbani M, Haque MM, Das Dipal D, Zarif MII, Iqbal A, Schwichtenberg A, Bansal N, Soron TR, Ahmed SI, Ahamed SI. An mCARE study on patterns of risk and resilience for children with ASD in Bangladesh. Scientific Reports. 2021;11(1):21342. doi: 10.1038/s41598-021-00793-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid H, Miller WC, Esfandiari E, Mohammadi S, Rash I, Tao G, Simpson E, Leong K, Matharu P, Sakakibara B, Schmidt J, Jarus T, Forwell S, Borisoff J, Backman C, Alic A, Brooks E, Chan J, Flockhart E, Mortenson WB. The impact of COVID-19-related restrictions on social and daily activities of parents, people with disabilities, and older adults: protocol for a longitudinal. Mixed methods study. JMIR Research Protocols. 2021;10(9):e28337. doi: 10.2196/28337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Romero, E., Lopez-Romero, L., Dominguez-Alvarez, B., Villar, P., & Gomez-Fraguela, J. A. (2020). Testing the Effects of COVID-19 Confinement in Spanish Children: The Role of Parents’ Distress, Emotional Problems and Specific Parenting. International Journal of Environmental Research and Public Health, 17(19). 10.3390/ijerph17196975 [DOI] [PMC free article] [PubMed]
- Roubinov D, Bush NR, Boyce WT. How a Pandemic Could Advance the Science of Early Adversity. JAMA Pediatrics. 2020;174(12):1131–1132. doi: 10.1001/jamapediatrics.2020.2354. [DOI] [PubMed] [Google Scholar]
- Ruiz Y, Wadsworth SMM, Elias CM, Marceau K, Purcell ML, Redick TS, Richards EA, Schlesinger-Devlin E. Ultra-rapid development and deployment of a family resilience program during the COVID-19 pandemic: Lessons learned from families tackling tough times together. Journal of Military, Veteran and Family Health. 2020;6(2):35–43. doi: 10.3138/JMVFH-6.S2-CO19-0013. [DOI] [Google Scholar]
- Russell BS, Tomkunas AJ, Hutchison M, et al. The Protective Role of Parent Resilience on Mental Health and the Parent-Child Relationship During COVID-19. Child Psychiatry and Human Development. 2022;53:183–196. doi: 10.1007/s10578-021-01243-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider M, Simpson J, Zlomke K. A comparison study: Caregiver functioning and family resilience among families of children with cystic fibrosis, asthma, and healthy controls. Children’s Health Care. 2021;50(2):142–158. doi: 10.1080/02739615.2020.1842207. [DOI] [Google Scholar]
- Schrooyen, C., Soenens, B., Waterschoot, J., Vermote, B., Morbee, S., Beyers, W., Brenning, K., Dieleman, L., Van der Kaap-Deeder, J., & Vansteenkiste, M. (2021). Parental identity as a resource for parental adaptation during the COVID-19 lockdown. Journal of Family Psychology : JFP : Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 8802265, dlv. 10.1037/fam0000895 [DOI] [PubMed]
- SickKids. (2021, February 26). New research reveals impact of COVID-19 pandemic on child and youth mental health. SickKids.https://www.sickkids.ca/en/news/archive/2021/impact-of-covid-19-pandemic-on-child-youth-mental-health/
- Smith, B. W., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., & Bernard, J. (2008). The brief resilience scale: assessing the ability to bounce back. International journal of behavioral medicine, 15(3), 194–200. https://doi-org.proxy1.lib.uwo.ca/10.1080/10705500802222972 [DOI] [PubMed]
- *Sorkkila, M., & Aunola, K. (2021). Resilience and parental burnout among Finnish parents during the COVID-19 pandemic: Variable and person-oriented approaches. The Family Journal, 1–9. [DOI] [PMC free article] [PubMed]
- Steinberg, D. M., Andresen, J. A., Pahl, D. A., Licursi, M., & Rosenthal, S. L. (2021). “I’ve weathered really horrible storms long before this...”: The experiences of parents caring for children with hematological and oncological conditions during the early months of the COVID-19 pandemic in the U.S. Journal of Clinical Psychology in Medical Settings, 9435680. 10.1007/s10880-020-09760-2 [DOI] [PMC free article] [PubMed]
- Suarez-Lopez JR, Cairns MR, Sripada K, Quiros-Alcala L, Mielke HW, Eskenazi B, Etzel RA, Kordas K. COVID-19 and children’s health in the United States: Consideration of physical and social environments during the pandemic. Environmental Resilience. 2021 doi: 10.1016/j.envres.2021.111160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang S, Xiang M, Cheung T, Xiang Y. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. Journal of Affective Disorders. 2021;279:353–360. doi: 10.1016/j.jad.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokatly Latzer I, Leitner Y, Karnieli-Miller O. Core experiences of parents of children with autism during the COVID-19 pandemic lockdown. Autism : The International Journal of Research and Practice. 2021;25(4):1047–1059. doi: 10.1177/1362361320984317. [DOI] [PubMed] [Google Scholar]
- Torres Fernandez I, Schwartz JP, Chun H, Dickson G. Family resilience and parenting. In: Becvar DS, editor. Handbook of family resilience. Springer; 2013. pp. 119–136. [Google Scholar]
- Touloupis T. Parental involvement in homework of children with learning disabilities during distance learning: Relations with fear of COVID-19 and resilience. Psychology in the Schools. 2021;58(12):2345–2360. doi: 10.1002/pits.22596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNESCO. (2021). Primary school starting age (years). The World Bank: UNESCO Institute for Statistics. Retrieved September 1, 2021. https://data.worldbank.org/indicator/SE.PRM.AGES?end=2020&start=2020&view=map
- Ungar M, Liebenberg L. Assessing Resilience Across Cultures Using Mixed Methods: Construction of the Child and Youth Resilience Measure. Journal of Mixed Methods Research. 2011;5(2):126–149. doi: 10.1177/1558689811400607. [DOI] [Google Scholar]
- United Nations. (2020). Policy brief: Education during COVID-19 and beyond. Retrieved September 21, 2021. https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2020/08/sg_policy_brief_covid-19_and_education_august_2020.pdf
- van Tilburg, M. A. L., Edlynn, E., Maddaloni, M., van Kempen, K., Diaz-Gonzalez de Ferris, M., & Thomas, J. (2020). High levels of stress due to the SARS-CoV-2 pandemic among parents of children with and without chronic conditions across the USA. Children (Basel, Switzerland), 7(10). 10.3390/children7100193 [DOI] [PMC free article] [PubMed]
- Vanier Institute of the Family. (2020). Families struggle to cope with financial impacts of the COVID-19 pandemic. https://vanierinstitute.ca/families-struggle-to-cope-with-financialimpacts-of-the-covid-19-pandemic/
- Vertsberger D, Roskam I, Talmon A, van Bakel H, Hall R, Mikolajczak M, Gross JJ. Emotion regulation during the COVID-19 pandemic: Risk and resilience factors for parental burnout (IIPB) Cognition and Emotion. 2022;36(1):100–105. doi: 10.1080/02699931.2021.2005544. [DOI] [PubMed] [Google Scholar]
- Wagnild, G. (2009). A review of the resilience scale. Journal of Nursing Measurement, 17(2), 105–113.https://doi-org.proxy1.lib.uwo.ca/10.1891/1061-3749.17.2.105 [DOI] [PubMed]
- Wang X, Cheng Z. Cross-Sectional Studies: Strengths, Weaknesses, and Recommendations. Chest. 2020;158(1):65–71. doi: 10.1016/j.chest.2020.03.012. [DOI] [PubMed] [Google Scholar]
- White SW, Stoppelbein L, Scott H, Spain D. It took a pandemic: Perspectives on impact, stress, and telehealth from caregivers of people with autism. Research in Developmental Disabilities. 2021;113(8709782, rid):103938. doi: 10.1016/j.ridd.2021.103938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K. Navigating the COVID-19 pandemic: The future of children and young people. Child & Youth Services. 2020;41(3):320–322. doi: 10.1080/0145935X.2020.1835211. [DOI] [Google Scholar]
- World Health Organization. (2020, April 27). Archived: WHO Timeline – COVID-19.https://www.who.int/news/item/27-04-2020-who-timeline---covid-19
- Wu Q, Xu Y, Jedwab M. Custodial grandparent’s job loss during the COVID-19 pandemic and its relationship with parenting stress and mental health. Journal of Applied Gerontology. 2021;40(9):923–933. doi: 10.1177/07334648211006222. [DOI] [PubMed] [Google Scholar]
- Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei province, China. JAMA Pediatrics. 2020;174(9):898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeasmin S, Banik R, Hossain S, Hossain M, Mahumud R, Salma N, Hossain M. Impact of COVID-19 pandemic on the mental health of children in Bangladesh: A cross-sectional study. Children and Youth Services Review. 2020;117:105277. doi: 10.1016/j.childyouth.2020.105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zilberstein K. Debate: Coping and resilience in the time of COVID-19 and structural inequities. Child and Adolescent Mental Health. 2021;26(3):279–280. doi: 10.1111/camh.12484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S, Zhang L, Wang L, Guo Z, Wang J, Chen J, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child & Adolescent Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zolkoski SM, Bullock LM. Resilience in children and youth: A review. Children and Youth Services Review. 2012;34:2295–2303. doi: 10.1016/j.childyouth.2012.08.009. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.