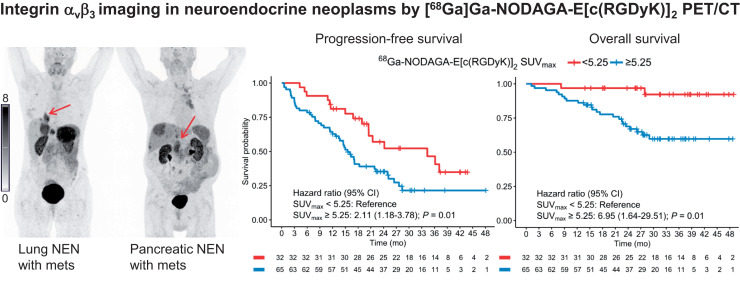
Visual Abstract
Keywords: integrin αvβ3, neuroendocrine neoplasms, PET, prognosis, molecular imaging
Abstract
Integrin αvβ3, a subtype of the arginine-glycine-aspartate (RGD)–recognizing cell surface integrins, is upregulated on endothelial cells during angiogenesis and on tumor cells. Because of involvement in tumor growth, invasiveness and metastases, and angiogenesis, integrin αvβ3 is an attractive target in cancers. In this study, we applied 68Ga-NODAGA-E[c(RGDyK)]2 for imaging of integrin αvβ3 in patients with neuroendocrine neoplasms (NENs) and its potential use for prognostication. We hypothesized that 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT would show tumor lesion uptake and that higher tumor lesion uptake was associated with a poorer prognosis. Methods: Between December 2017 and November 2020 we prospectively enrolled 113 patients with NEN of all grades (2019 World Health Organization classification) for 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT. The scan was acquired 45 min after injection of 200 MBq of 68Ga-NODAGA-E[c(RGDyK)]2. Board-certified specialists in nuclear medicine and radiology analyzed the PET/CT measuring SUVmax in tumor lesions. Positive tumor lesions were defined as those with tumor-to-liver background ≥ 2. Maximal tumor SUVmax for each patient was used as a predictor of outcome. Patients were followed for at least 1 y to assess progression-free survival and overall survival. Results: Of 113 patients enrolled in the trial, 99 underwent 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT, with 97 patients having evaluable lesions. The patients predominantly had small intestinal (64%) or pancreatic (20%) NEN and most had metastatic disease (93%). Most patients had low-grade tumors (78%), whereas 22% had high-grade tumors. During a median follow-up of 31 mo (interquartile range, 26–38 mo), 62 patients (64%) experienced disease progression and 25 (26%) patients died. In total, 76% of patients had positive tumor lesions, and of the patients with high-grade tumors 91% had positive tumor lesions. High integrin αvβ3 expression, defined as an SUVmax of at least 5.25, had a hazard ratio of 2.11 (95% CI, 1.18–3.78) and 6.95 (95% CI, 1.64–29.51) for progression-free survival and overall survival, respectively (P = 0.01 for both). Conclusion: Tumor lesion uptake of 68Ga-NODAGA-E[c(RGDyK)]2 was evident in patients with all grades of NEN. High uptake was associated with a poorer prognosis. Further studies are warranted to establish whether 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT may become a prediction tool for identification of patients eligible for treatments targeting integrin αvβ3.
Neuroendocrine neoplasms (NENs) represent a heterogeneous group of tumors originating from the neuroendocrine cells. NEN are primarily found in the gastrointestinal tract, pancreas, and lungs. Patients with NEN are often diagnosed when the disease has metastasized, yet the clinical course for these patients varies greatly. Origin of primary tumor, presence of metastases as well as tumor morphology and proliferation activity (i.e., Ki-67) are known prognostic factors (1). The 2019 World Health Organization (WHO) classification stratifies NEN into neuroendocrine tumor (NET) G1 (Ki-67 < 3%), NET G2 (Ki-67 3%–20%), NET G3 (Ki-67 > 20% and well-differentiated), and neuroendocrine carcinoma (NEC) (Ki-67 > 20% and poorly differentiated) (2). Furthermore, imaging modalities aid in diagnosis, staging, treatment selection, and follow-up for patients with NEN. In particular, PET radiotracers reflecting somatostatin receptor expression (e.g., 64Cu-DOTATATE or 68Ga-DOTATATE) and glucose metabolism (18F-FDG) are used for these purposes in addition to providing prognostic information (3,4). Finally, targeting the somatostatin receptors with peptide receptor radionuclide therapy (PRRT), for example, 177Lu-DOTATATE, has been approved for patients with NEN.
Additional tumor markers may be useful for further improvement in prognostication and ultimately identifying novel treatment targets in patients with NEN. Cell surface adhesion receptors of the integrin superfamily have been extensively investigated because their role in physiologic as well as in pathophysiologic processes, and especially in cancers (5). The subfamily of arginine-glycine-aspartate (RGD)–recognizing integrins has implications on several of hallmarks of cancer: tumor growth, invasiveness, and metastases and angiogenesis. Integrin αvβ3 is significantly upregulated on activated endothelial cells during angiogenesis but absent on quiescent endothelial cells as well as overexpressed on tumor cells in several cancers (6). NENs are generally characterized as highly vascularized tumors with overexpression of various proangiogenetic factors such as vascular endothelial growth factor (7). Previously we found, using quantitative gene expression, that the expression of integrin αvβ3 shows high variability between NENs (8). Because of its integral role in cancer, our group therefore developed and clinically translated the PET radiotracer 68Ga-NODAGA-E[c(RGDyK)]2 targeting integrin αvβ3 with high affinity (9,10).
The aim of this phase II clinical trial of 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT in patients with NEN of all grades was to further assess tumor uptake and prognostic value. We hypothesized that PET/CT with 68Ga-NODAGA-E[c(RGDyK)]2 would show accumulation in tumor lesions in patients with NEN of all grades and that the uptake of the radiotracer would be associated with progression-free survival (PFS) and overall survival (OS).
MATERIALS AND METHODS
Patients
Patients with histologically confirmed NEN were included from the Department of Endocrinology (managing low-grade NEN, Ki-67 ≤ 20%) and Department of Oncology (managing high-grade NEN, Ki-67 > 20%), Copenhagen University Hospital–Rigshospitalet, Denmark, between December 4, 2017, and November 26, 2020. Rigshospitalet is a Neuroendocrine Tumor Center of Excellence accredited by the European Neuroendocrine Tumor Society. The study was conducted in accordance with the Helsinki Declaration and Good Clinical Practice. The study was approved by the Danish Medicines Agency (EudraCT 2017-002512-14), Scientific Ethics Committee (H-17019542), and Danish Data Protection Agency (2012-58-0004), and registered on clinicaltrials.gov (NCT03271281).
Eligible patients were 18 y or older, capable of reading and understanding the patient information in Danish and giving informed consent, diagnosed with gastroenteropancreatic NEN of all grades or bronchopulmonary NEN, and had a WHO performance status of 0–2. Patients were excluded if they were pregnant or breastfeeding, had a body mass more than 140 kg, or had a history of allergic reaction attributable to compounds of chemical or biologic composition similar to 68Ga-NODAGA-E[c(RGDyK)]2 or in the case of bronchopulmonary NEN if the subtype was small cell lung cancer. After written informed consent was obtained, the patients were referred for a 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT at the first opportunity.
Image Acquisition
Data were acquired using a Biograph 128 mCT PET/CT scanner (Siemens Medical Solutions) with an axial field of view of 216 mm. On the basis of the previous phase I trial, the scans were acquired 45 min after intravenous administration of approximately 200 MBq of 68Ga-NODAGA-E[c(RGDyK)]2 ([68Ga]Ga-NODAGA-Glu[cyclo(-Arg-Gly-Asp-D-Tyr-Lys-)]2) equaling 4.4 mSv. Radiotracer were produced as previously described (9). Whole-body PET scans (mid orbita to mid thigh) were obtained with an acquisition time of 4 min per bed position. Attenuation- and scatter-corrected PET data were reconstructed iteratively using a 3-dimensional ordinary Poisson ordered-subset expectation maximization algorithm including point-spread function and time-of-flight information using the TrueX algorithm (Siemens Medical Solutions); the settings were 2 iterations, 21 subsets, 2-mm gaussian filter. A diagnostic CT scan was obtained before the PET scan with a 2-mm slice thickness, 120 kV, and a quality reference of 225 mAs modulated by the Care Dose 4D automatic exposure control system (Siemens Medical Solutions). An automatic injection system was used to administer 75 mL of an iodine-containing contrast agent (Optiray 300; Covidien) for arterial and venous phase CT.
Patients were observed for adverse events after injection of 68Ga-NODAGA-E[c(RGDyK)]2, and after discharge patients were asked to record any adverse events occurring within the first 24 h of injection. Adverse events were categorized according to Common Terminology Criteria for Adverse Events (version 5.0).
Image Analysis
Together, an experienced board-certified nuclear medicine physician and an experienced board-certified radiologist analyzed the 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT scans. The readers had access to previous imaging studies but were masked to other patient data and follow-up data. Lesions were identified on CT or PET. SUV was calculated as decay-corrected measured radioactivity concentration/(injected activity/body weight). If more than 1 lesion was present in an organ, the lesion with the highest SUVmax was noted. If no lesions were identified on PET, but lesions were visible on CT, the largest lesion (based on viable tissue within the lesion) on CT was used as guide for lesion delineation on the PET scan from which SUVmax was determined. As background reference of uptake in tumor lesions, the radiotracer uptake in normal liver tissue was measured as SUVmean. A tumor lesion–to–liver ratio (TLR) was calculated as tumor lesion SUVmax/normal liver SUVmean. A cutoff of TLR ≥ 2 was used to define positive lesions.
Follow-up
The patients were followed at the Rigshospitalet Neuroendocrine Tumor Center of Excellence with regular visits including clinical examination, blood samples, and imaging (CT, MR, ultrasound, or PET/CT). The frequency was in accordance with European Neuroendocrine Tumor Society guidelines, typically every 3–6 mo (11). The 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT was not made available for the treating physicians and thus not used to guide clinical decisions regarding treatment or follow-up. The end of follow-up was December 31, 2021, for the current study. Routine CT and or MRI were used for evaluation of PFS in accordance with RECIST (version 1.1) (12). PFS was defined as time from 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT to, if any, progression or death from any cause. If no progression or death from any cause occurred within the follow-up time period, the patient was censored at the time of last available diagnostic imaging. OS was defined as time from 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT to death by any cause. As all deaths but 2 were directly related to NEN, we refrained from analyzing disease-specific survival. Patients alive at follow-up were censored to the day of the end of follow-up (December 31, 2021).
Statistics
Continuous variables are reported as mean ± SD or median with range unless otherwise noted. Kaplan–Meier analyses were used for estimation of time to outcome (PFS and OS) and reverse Kaplan–Meier analysis was used to estimate median follow-up time. Univariate and multivariate Cox regression analyses for OS and PFS, with predictor variables being SUVmax and WHO grade, were performed to determine hazard ratio (HR) and 95% CI. We used the Cutoff Finder application to determine the optimal cutoff for SUVmax (13). A P value of less than 0.05 was considered statistically significant. R version 3.6.0 (R Foundation for Statistical Computing) was used for the analyses.
RESULTS
Patients and Image Acquisition
We prospectively included 113 patients, 14 of whom did not undergo 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT because of disease worsening (n = 4), consent withdrawal (n = 2), death before PET/CT (n = 3), logistical impossibility for PET/CT to be performed (n = 2), and infeasibility for PET/CT scanning due to COVID-19 restrictions (n = 3). Of the 99 patients scanned with PET/CT, 97 patients had evaluable lesions. The patients predominately had small intestinal (n = 62, 64%) or pancreatic (n = 19, 20%) NEN and metastatic disease (n = 90, 93%) (Table 1). Most patients had low-grade tumors (Ki-67 ≤ 20%) (n = 76, 78%), whereas 21 (22%) had high-grade tumors (Ki-67 > 20%). No patients were treatment-naïve before the PET/CT scan.
TABLE 1.
Baseline Characteristics of 97 Patients with NENs
| Baseline characteristic | Data |
|---|---|
| Median age (y) | 67 (range, 44–83) |
| Sex | |
| Female | 43 (44%) |
| Male | 54 (56%) |
| Site of primary tumor | |
| Small intestine | 62 (64%) |
| Pancreas | 19 (20%) |
| Lung | 6 (6%) |
| Colon | 6 (6%) |
| Stomach | 2 (2%) |
| Esophagus | 1 (1%) |
| Rectum | 1 (1%) |
| Metastatic disease | 90 (93%) |
| Liver metastases | 76 (79%) |
| Median Ki-67 (%) | 6 (range, 1–100) |
| 2019 World Health Organization grade | |
| NET G1 | 21 (22%) |
| NET G2 | 55 (57%) |
| NET G3 | 14 (14%) |
| NEC | 7 (7%) |
| Median time from diagnosis to PET/CT (mo) | 27 (range, 2–265) |
| Primary tumor resected | 37 (38%) |
| Ongoing treatment at PET/CT scan time | |
| Somatostatin analog | 75 (77%) |
| Interferon | 8 (8%) |
| Capecitabine/5-fluorouracil | 5 (5%) |
| Etoposide ± carboplatin | 4 (4%) |
| Streptozotocin | 4 (4%) |
| Everolimus | 3 (3%) |
| Temozolomide | 2 (2%) |
| Completed treatment before PET/CT | |
| On first line of therapy | 45 (46%) |
| Peptide receptor radionuclide therapy | 30 (31%) |
| Etoposide ± carboplatin | 16 (16%) |
| Capecitabine/5-fluorouracil | 12 (12%) |
| Temozolomide | 7 (7%) |
| Streptozotocin | 7 (7%) |
| Interferon | 6 (6%) |
| External radiation therapy | 5 (5%) |
| Liver radiofrequency ablation or embolization | 5 (5%) |
| Resection of liver metastases | 4 (4%) |
| Everolimus or sunitinib | 2 (2%) |
Patients undergoing 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT (n = 99) received a median mass dose of 18.9 (range, 7.7–49.3) μg of 68Ga-NODAGA-E[c(RGDyK)]2 and the activity dose was 193 (range, 104–226) MBq. Median time from injection to the start of PET scanning was 47 min (range, 35–86 min). Three patients experienced an adverse event: dizziness (grade 1), fall (grade 1), and infusion-related reaction to injection of CT contrast (grade 2) within 24 h of injection of 68Ga-NODAGA-E[c(RGDyK)]2. All were deemed unrelated to 68Ga-NODAGA-E[c(RGDyK)]2 injection. No grade 3–5 adverse events occurred.
Image Analysis
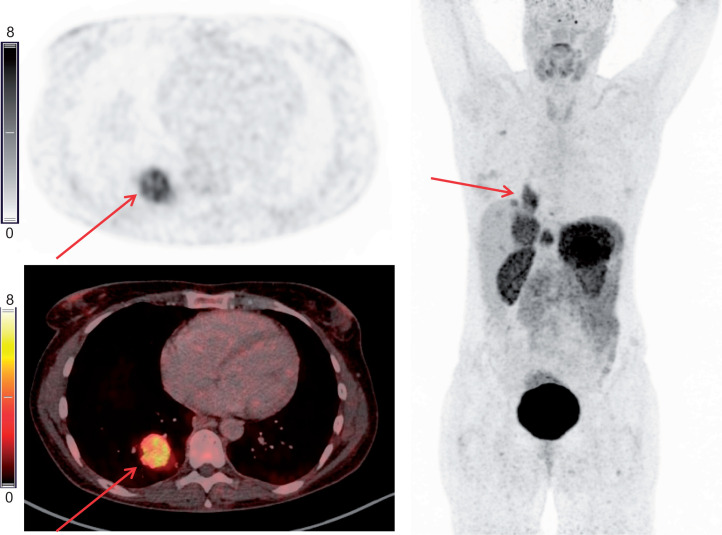
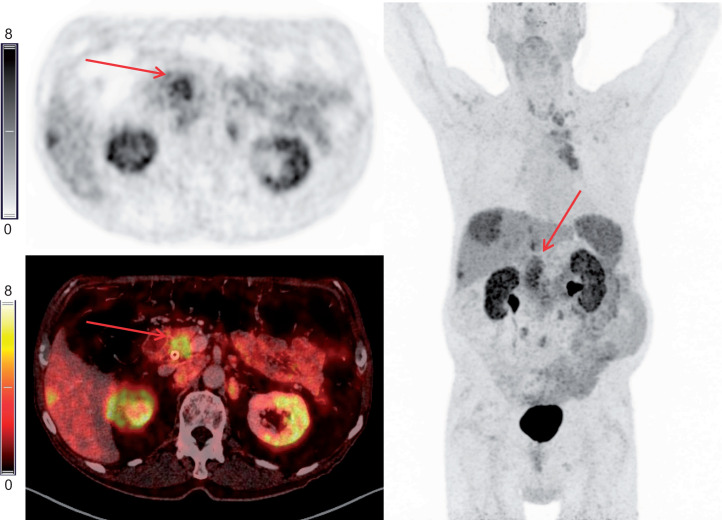
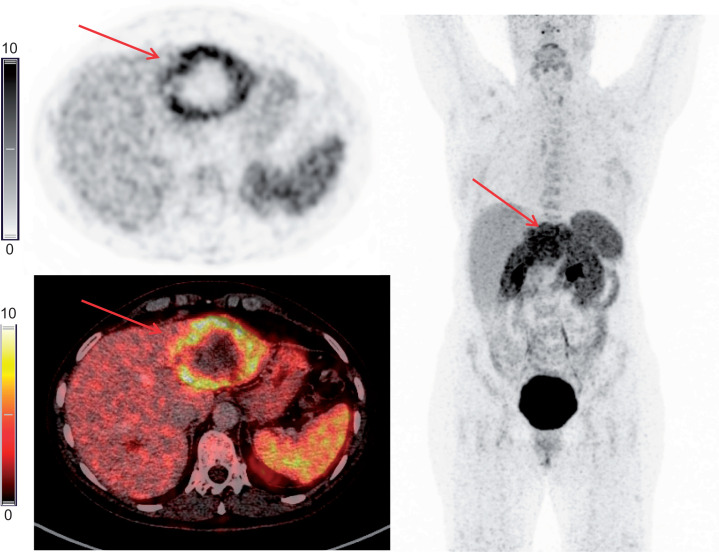
The median maximal tumor lesion SUVmax was 6.1 (range, 1.4–14.1). The mean ± SD of tumor lesion SUVmax was 6.36 ± 2.49 and the mean ± SD normal liver SUVmean was 2.41 ± 0.55. Examples of 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT are shown in Figures 1–3. When the cutoff of TLR ≥ 2 to determine positive lesions was applied, approximately two thirds of patients with NET G1 had positive lesions, which gradually increased to nearly all patients with NET G3/NEC (91%) having positive lesions (Table 2). In total, 76% of patients had positive tumor lesions.
FIGURE 1.
Example of 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT. Transaxial PET and fused PET/CT and maximum-intensity projection with color bars (unit: SUV). Patient with lung NET grade 2 (Ki-67 15%) with liver and bone metastases. Arrows point to primary tumor.
FIGURE 3.
Example of 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT. Transaxial PET and fused PET/CT and maximum-intensity projection with color bars (unit: SUV). Patient with pancreatic NET grade 2 (Ki-67 11%) with liver and lymph node metastases. Arrows point to primary tumor.
TABLE 2.
Patients with 68Ga-NODAGA-E[c(RGDyK)]2 PET–Positive Lesions (TLR ≥ 2) According to WHO Classification of NENs
| Uptake ratio | NET G1 (n = 21) | NET G2 (n = 55) | NET G3/NEC (n = 21) | All (n = 97) |
|---|---|---|---|---|
| TLR ≥ 2 | 13 (62%) | 42 (76%) | 19 (91%) | 74 (76%) |
| TLR < 2 | 8 (38%) | 13 (24%) | 2 (10%) | 23 (24%) |
A tumor was defined as positive when the TLR, measured as lesion SUVmax–to–normal liver SUVmean, was ≥ 2. Of the patients with NET G3/NEC tumors, 13 of 14 (93%) patients with NET G3 were positive and 6 of 7 (86%) patients with NEC were positive.
FIGURE 2.
Example of 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT. Transaxial PET and fused PET/CT and maximum-intensity projection with color bars (unit: SUV). Patient with gastric NET grade 2 (Ki-67 8%) with liver metastases. Arrows point to liver metastasis.
Follow-up
During a median follow-up of 31 mo (interquartile range, 26–38 mo), 62 patients (64%) experienced disease progression and 25 (26%) patients died. Overall median PFS was 18.9 mo (interquartile range, 15.5–25.1 mo). No patients were lost to follow-up. The patients’ treatments after 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT are given in Table 3. Treatment with somatostatin analog was the most frequent (80%, 78/97), and 32% (31/97) of all patients underwent PRRT during the follow-up period.
TABLE 3.
Treatments Given to Patients with NENs (n = 97) During Follow-up
| Treatment after PET/CT | n (%) |
|---|---|
| Somatostatin analog | 78 (80%) |
| Peptide receptor radionuclide therapy | 31 (32%) |
| Capecitabine/5-fluorouracil | 13 (13%) |
| Everolimus or sunitinib | 12 (12%) |
| Surgery | 11 (11%) |
| Temozolomide | 9 (9%) |
| Liver radiofrequency ablation or embolization | 9 (9%) |
| External radiation therapy | 7 (7%) |
| Etoposide ± carboplatin | 5 (5%) |
| Interferon | 5 (5%) |
| Streptozotocin | 3 (3%) |
| Docetaxel | 3 (3%) |
PFS and OS
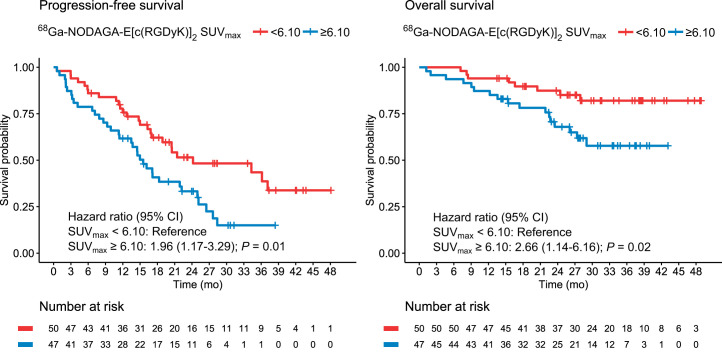
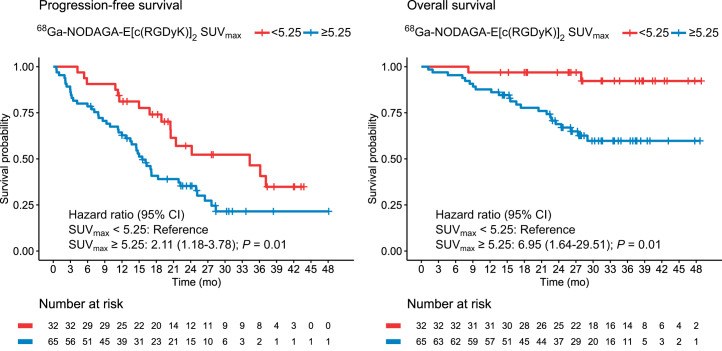
In univariate analyses, the maximal tumor SUVmax as a continuous variable was significantly associated with PFS and OS, with an HR of 1.17 (95% CI, 1.07–1.28), P < 0.001, and 1.19 (95% CI, 1.03–1.38), P = 0.02, per 1 unit increase, respectively. High integrin αvβ3 expression, defined as maximal tumor SUVmax above median (SUVmax 6.10) had an HR of 1.96 (95% CI, 1.17–3.29) and 2.66 (95% CI, 1.14–6.16) for PFS and OS, respectively (P < 0.05 for both (Fig. 4; Tables 4 and 5). Optimal cutoffs for dichotomizing maximal tumor SUVmax were assessed by Cutoff Finder for either PFS or OS as outcome (Supplemental Fig. 1; supplemental materials are available at http://jnm.snmjournals.org). When a lower cutoff of SUVmax (5.25) was used, a smaller group of patients (n = 32) with a very low risk of death could be identified (Fig. 5; Tables 6 and 7). Patients with an SUVmax above 5.25 had an HR of 2.11 (95% CI, 1.18–3.78) and 6.95 (95% CI, 1.64–29.51) for PFS and OS, respectively (P = 0.01 for both). With the cutoff of 5.25, median OS was not reached in either groups with low or groups with high SUVmax, and median PFS was 34.3 mo (20.5; upper limit not reached) for patients with low SUVmax versus 15.5 mo (13.5–22.2) for patients with high SUVmax. Furthermore, when a higher cutoff of SUVmax of 7.45 was used, the dichotomization was optimized for prediction of disease progression with an HR of 2.57 (95% CI, 1.52–4.34), P < 0.001 (Supplemental Fig. 2; Supplemental Tables 1 and 2). Patients with NET G3 and NEC had significantly worse PFS and OS as compared with patients with NET G1, whereas no difference was seen between NET G2 and NET G1 (Tables 4 and 5). In multivariate analyses including SUVmax and WHO classification (NET G3 and NEC vs. NET G1), both remained significantly associated with PFS and OS (Tables 4–7).
FIGURE 4.
Kaplan–Meier plots of 68Ga-NODAGA-E[c(RGDyK)]2 PET SUVmax dichotomized at 6.10 (median) for prediction of PFS and OS.
TABLE 4.
Uni- and Multivariate Cox Regression Analyses for PFS (SUVmax Cutoff at 6.10)
| Univariate Cox | Multivariate Cox | |||
|---|---|---|---|---|
| PFS | HR | P | HR | P |
| SUVmax | ||||
| <6.10 | Reference | — | Reference | — |
| ≥6.10 | 1.96 (1.17–3.29) | 0.01 | 1.82 (1.07–3.08) | 0.03 |
| WHO grades | ||||
| NET G1 | Reference | Reference | ||
| NET G2 | 1.25 (0.63–2.49) | 0.52 | 1.25 (0.63–2.49) | 0.52 |
| NET G3 | 4.01 (1.68–9.54) | <0.01 | 4.08 (1.70–9.77) | <0.01 |
| NEC | 7.01 (2.65–18.50) | <0.001 | 5.87 (2.21–15.61) | <0.001 |
The median SUVmax was 6.10. Data in parentheses are 95% CIs.
TABLE 5.
Uni- and Multivariate Cox Regression Analyses for OS (SUVmax Cutoff at 6.10)
| Univariate Cox | Multivariate Cox | |||
|---|---|---|---|---|
| OS | HR | P | HR | P |
| SUVmax | ||||
| <6.10 | Reference | — | Reference | — |
| ≥6.10 | 2.66 (1.14–6.16) | 0.02 | 2.59 (1.08–6.24) | 0.03 |
| WHO grades | ||||
| NET G1 | Reference | Reference | ||
| NET G2 | 1.84 (0.40–8.50) | 0.44 | 1.80 (0.39–8.35) | 0.45 |
| NET G3 | 15.99 (3.26–78.50) | <0.01 | 18.04 (3.59–90.63) | <0.001 |
| NEC | 28.46 (5.62–144.24) | <0.001 | 22.55 (4.45–114.27) | <0.001 |
The median SUVmax was 6.10. Data in parentheses are 95% CIs.
FIGURE 5.
Kaplan–Meier plots of 68Ga-NODAGA-E[c(RGDyK)]2 PET SUVmax dichotomized at 5.25 for prediction of PFS and OS.
TABLE 6.
Uni- and Multivariate Cox Regression Analyses for PFS (SUVmax Cutoff at 5.25)
| Univariate Cox | Multivariate Cox | |||
|---|---|---|---|---|
| PFS | HR | P | HR | P |
| SUVmax | ||||
| <5.25 | Reference | — | Reference | — |
| ≥5.25 | 2.11 (1.18–3.78) | 0.01 | 1.92 (1.06–3.47) | 0.03 |
| WHO grades | ||||
| NET G1 | Reference | Reference | ||
| NET G2 | 1.25 (0.63–2.49) | 0.52 | 1.22 (0.62–2.44) | 0.56 |
| NET G3 | 4.01 (1.68–9.54) | <0.01 | 3.94 (1.65–9.44) | <0.01 |
| NEC | 7.01 (2.65–18.50) | <0.001 | 5.84 (2.20–15.55) | <0.001 |
SUVmax cutoff optimized for prediction of OS was 5.25. Data in parentheses are 95% CIs.
TABLE 7.
Uni- and Multivariate Cox Regression Analyses for OS (SUVmax Cutoff at 5.25)
| Univariate Cox | Multivariate Cox | |||
|---|---|---|---|---|
| OS | HR | P | HR | P |
| SUVmax | ||||
| <5.25 | Reference | — | Reference | — |
| ≥5.25 | 6.95 (1.64–29.51) | 0.01 | 5.45 (1.26–23.60) | 0.02 |
| WHO grades | ||||
| NET G1 | Reference | Reference | ||
| NET G2 | 1.84 (0.40–8.50) | 0.44 | 1.78 (0.38–8.26) | 0.46 |
| NET G3 | 15.99 (3.26–78.50) | <0.01 | 15.67 (3.13–78.47) | <0.001 |
| NEC | 28.46 (5.62–144.24) | <0.001 | 20.23 (3.98–102.87) | <0.001 |
SUVmax cutoff optimized for prediction of OS was 5.25. Data in parentheses are 95% CIs.
DISCUSSION
The major finding of our phase II prospective study of 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT for integrin αvβ3 imaging in patients with NEN was that integrin αvβ3 expression was seen in both low- and high-grade NEN. Furthermore, we found a significant association between radiotracer uptake and both PFS and OS. When dichotomized at SUVmax 5.25, patients with higher radiotracer uptake in tumor lesion had a 2-fold higher risk of progressive disease and a 7-fold higher risk of death. These findings highlight integrin αvβ3 as an important prognostic marker in patients with NEN.
Many radiotracers using the RGD motif have been tested preclinically, with only some being further translated into clinical trials (14). In our phase I trial on 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT imaging, we included patients with NEN or breast cancer and demonstrated that administration of the radiotracer was safe and had low radiation burden and high tumor lesion uptake (9). Besides our phase I trial, no specific PET imaging studies with an RGD-based radiotracer in patients with NEN have been conducted, although combined integrin αvβ3 and somatostatin receptor targeting has been examined with 68Ga-NOTA-3P-TATE-RGD PET/CT (15). To our knowledge, the current study is the largest to be conducted with an RGD-based PET radiotracer. Other clinical trials have used RGD-based radiotracers to examine patients with, for example, breast cancer and head and neck cancers, as well as several other nononcologic applications, for example, atherosclerosis and rheumatoid arthritis (16–19).
Integrin αvβ3 is a cell surface adhesion receptor and a member of the integrin superfamily. The subfamily of integrins recognized by RGD also includes αvβ1, αvβ5, αvβ6, αvβ8, α5β1, α8β1, and αIIbβ3 (20). Integrins are involved in several physiologic and pathophysiologic pathways, for example, embryogenesis, wound healing, and angiogenesis as well as tumor growth, invasion or metastasis, and angiogenesis related to cancer. The natural ligands of integrin αvβ3 are extracellular matrix proteins such as fibronectin and vitronectin. Additionally, integrins interact with several other factors also involved in angiogenesis and invasive growth, for example, vascular endothelial growth factor and urokinase plasminogen activator receptor (5,21). An indication that integrin expression is involved in promoting the metastatic process in patients with NEN is supported by gene expression analysis in patients with pulmonary NEN. Upregulation of fibrogenic genes, including ITGAV (the gene encoding integrin αv), was related to poor differentiation and increased risk of metastases (22). However, conflicting data regarding the relation between poorer prognosis and integrin αvβ3 expression have been reported for immunohistochemical staining of gastric cancer (23) and non–small cell lung cancer (24).
Spurred by the upregulation of αvβ3 during angiogenesis, early phase clinical trials with the αvβ3/αvβ5-targeting ligand cilengitide were performed, showing modest effect on tumor growth (25,26). However, later phase II and phase III trials failed to meet expectations because of an unintended proangiogenic effect at lower concentrations while an antiangiogenetic effect was seen only at higher concentration (27). Recently, new promising pure αvβ3 ligands (TDI-4161 and TDI-3761) have been shown to circumvent the proangiogenetic effect previously seen with cilengitide (28), hence reinforcing the need for development of methods as companion diagnostics to assess in vivo the level of integrin αvβ3 expression for selection of patients for such targeted therapies.
Another possible avenue for integrin αvβ3-targeted treatments is PRRT. In patients with NEN, PRRT with 177Lu-DOTATATE, exploiting somatostatin receptor overexpression, has become an integrated part of treatment (29,30). In 2 preclinical studies, the potential of extending the use of the RGD sequence by coupling it with a radionuclide for therapy has been examined. One combined αvβ3-targeting PRRT with immune checkpoint inhibitor programmed death ligand 1 (31) and the other αvβ3-targeting PRRT with temozolomide (32). Both demonstrated additional effect of the combined therapy. Further studies of coupling imaging and PRRT in the setting of integrin αvβ3 are needed. Concerns over physiologic uptake reported in RGD-based imaging have been raised regarding PRRT (20). However, compared with dosimetry data from somatostatin-based PET radiotracers 68Ga-DOTATATE and 68Ga-DOTATOC (33), we found similar kidney, liver, spleen, and intestinal absorbed doses in our phase I trial study assessing the dosimetry of 68Ga-NODAGA-E[c(RGDyK)]2 (9). Finally, a potential advantage of αvβ3-targeting PRRT over somatostatin receptor–targeting PRRT in NEN is that in particular in high-grade tumors, somatostatin receptor expression is low or absent and therefore somatostatin receptor PRRT cannot be used. In contrast, we found a high uptake of 68Ga-NODAGA-E[c(RGDyK)]2 also in high-grade tumors (91% of patients with NET G3/NEC).
In our study, included patients predominately had small intestinal or pancreatic primary tumors and nearly all had metastatic disease with liver involvement. Hence use of 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT in other settings, for example, for assessment of newly diagnosed patients with localized disease, remains to be elucidated.
CONCLUSION
Tumor uptake of 68Ga-NODAGA-E[c(RGDyK)]2 was evident in patients both with low- and with high-grade NEN, although tumor uptake was more pronounced with increasing grade. High tumor uptake of 68Ga-NODAGA-E[c(RGDyK)]2 was associated with a poorer prognosis in patients with NEN, with a 2-fold higher risk of progression and 7-fold higher risk of death. Further studies are warranted to establish whether 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT may become a tool for risk stratification and for identification of patients eligible for treatments targeting integrin αvβ3.
DISCLOSURE
This project received funding from the European Union’s Horizon 2020 research and innovation program under grant agreements no. 670261 (ERC Advanced Grant) and 668532 (Click-It), the Lundbeck Foundation, the Novo Nordisk Foundation, the Innovation Fund Denmark, IPSEN Nordic, the Danish Cancer Society, Arvid Nilsson Foundation, the Neye Foundation, Novartis Health Care, the Research Foundation of Rigshospitalet, the Danish National Research Foundation (grant 126), the Research Council of the Capital Region of Denmark, the Danish Health Authority, the John and Birthe Meyer Foundation, the Research Council for Independent Research, and the Neuroendocrine Tumor Research Foundation. Andreas Kjaer is a Lundbeck Foundation Professor and is an inventor/holds intellectual property rights on a patent application: “68Ga- and 64Cu -NODAGA-E[c(RGDyK)]2 for use as pet tracers in the imaging of angiogenesis in humans” (WO2019091534A1). No other potential conflicts of interest relevant to this article exist.
ACKNOWLEDGEMENT
We are grateful to our dedicated colleagues at the Department of Clinical Physiology and Nuclear Medicine, Department of Endocrinology, and Department of Oncology at Rigshospitalet for assistance with patient recruitment, radiotracer production, and acquisition of PET/CT scans. We express our sincere gratitude to all the patients who participated in the study.
KEY POINTS
QUESTION: Is integrin αvβ3 expression assessed by PET evident in tumor lesions of patients with NENs and associated with prognosis?
PERTINENT FINDINGS: When 68Ga-NODAGA-E[c(RGDyK)]2 for integrin αvβ3 PET imaging was used, integrin αvβ3 was evident in tumor lesions of patients with both low- and high-grade tumors. High tumor uptake of 68Ga-NODAGA-E[c(RGDyK)]2 was associated with a poorer prognosis for both disease progression and death.
IMPLICATIONS FOR PATIENT CARE: Integrin αvβ3 is a prognostic marker and a potential treatment target in patients with NENs. 68Ga-NODAGA-E[c(RGDyK)]2 PET/CT may become a tool for risk stratification and for identification of patients eligible for treatments targeting integrin αvβ3.
REFERENCES
- 1. Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3:1335–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Digestive System Tumours. WHO Classification of Tumours. 5th ed. International Agency for Research on Cancer; 2019:16–19. [Google Scholar]
- 3. Carlsen EA, Johnbeck CB, Loft M, et al. Semiautomatic tumor delineation for evaluation of 64Cu-DOTATATE PET/CT in patients with neuroendocrine neoplasms: prognostication based on lowest lesion uptake and total tumor volume. J Nucl Med. 2021;62:1564–1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Binderup T, Knigge U, Johnbeck CB, et al. 18F-FDG PET is superior to WHO grading as a prognostic tool in neuroendocrine neoplasms and useful in guiding PRRT: a prospective 10-year follow-up study. J Nucl Med. 2021;62:808–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ludwig BS, Kessler H, Kossatz S, Reuning U. RGD-binding integrins revisited: how recently discovered functions and novel synthetic ligands (re-)shape an ever-evolving field. Cancers (Basel). 2021;13:1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nieberler M, Reuning U, Reichart F, et al. Exploring the role of RGD-recognizing integrins in cancer. Cancers (Basel). 2017;9:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cives M, Pelle E, Quaresmini D, Rizzo FM, Tucci M, Silvestris F. The tumor microenvironment in neuroendocrine tumors: biology and therapeutic implications. Neuroendocrinology. 2019;109:83–99. [DOI] [PubMed] [Google Scholar]
- 8. Oxboel J, Binderup T, Knigge U, Kjaer A. Quantitative gene-expression of the tumor angiogenesis markers vascular endothelial growth factor, integrin αV and integrin β3 in human neuroendocrine tumors. Oncol Rep. 2009;21:769–775. [PubMed] [Google Scholar]
- 9. Clausen MM, Carlsen EA, Christensen C, et al. First-in-human study of [68Ga]Ga-NODAGA-E[c(RGDyK)]2 PET for integrin alphavbeta3 imaging in patients with breast cancer and neuroendocrine neoplasms: safety, dosimetry and tumor imaging ability. Diagnostics (Basel). 2022;12:851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Oxboel J, Brandt-Larsen M, Schjoeth-Eskesen C, et al. Comparison of two new angiogenesis PET tracers 68Ga-NODAGA-E[c(RGDyK)]2 and 64Cu-NODAGA-E[c(RGDyK)]2; in vivo imaging studies in human xenograft tumors. Nucl Med Biol. 2014;41:259–267. [DOI] [PubMed] [Google Scholar]
- 11. Knigge U, Capdevila J, Bartsch DK, et al. ENETS consensus recommendations for the standards of care in neuroendocrine neoplasms: follow-up and documentation. Neuroendocrinology. 2017;105:310–319. [DOI] [PubMed] [Google Scholar]
- 12. Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–247. [DOI] [PubMed] [Google Scholar]
- 13. Budczies J, Klauschen F, Sinn BV, et al. Cutoff Finder: a comprehensive and straightforward web application enabling rapid biomarker cutoff optimization. PLoS One. 2012;7:e51862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liolios C, Sachpekidis C, Kolocouris A, Dimitrakopoulou-Strauss A, Bouziotis P. PET diagnostic molecules utilizing multimeric cyclic RGD peptide analogs for imaging integrin alphavbeta3 receptors. Molecules. 2021;26:1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zheng Y, Wang H, Tan H, et al. Evaluation of lung cancer and neuroendocrine neoplasm in a single scan by targeting both somatostatin receptor and integrin αvβ3. Clin Nucl Med. 2019;44:687–694. [DOI] [PubMed] [Google Scholar]
- 16. Dietz M, Kamani CH, Deshayes E, et al. Imaging angiogenesis in atherosclerosis in large arteries with 68Ga-NODAGA-RGD PET/CT: relationship with clinical atherosclerotic cardiovascular disease. EJNMMI Res. 2021;11:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wu J, Wang S, Zhang X, et al. 18F-Alfatide II PET/CT for identification of breast cancer: a preliminary clinical study. J Nucl Med. 2018;59:1809–1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhu Z, Yin Y, Zheng K, et al. Evaluation of synovial angiogenesis in patients with rheumatoid arthritis using 68Ga-PRGD2 PET/CT: a prospective proof-of-concept cohort study. Ann Rheum Dis. 2014;73:1269–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Durante S, Dunet V, Gorostidi F, et al. Head and neck tumors angiogenesis imaging with 68Ga-NODAGA-RGD in comparison to 18F-FDG PET/CT: a pilot study. EJNMMI Res. 2020;10:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Steiger K, Quigley NG, Groll T, et al. There is a world beyond alphavbeta3-integrin: multimeric ligands for imaging of the integrin subtypes alphavbeta6, alphavbeta8, alphavbeta3, and alpha5beta1 by positron emission tomography. EJNMMI Res. 2021;11:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mahmood N, Mihalcioiu C, Rabbani SA. Multifaceted role of the urokinase-type plasminogen activator (uPA) and its receptor (uPAR): diagnostic, prognostic, and therapeutic applications. Front Oncol. 2018;8:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Prieto TG, Machado-Rugolo J, Baldavira CM, et al. The fibrosis-targeted collagen/integrins gene profile predicts risk of metastasis in pulmonary neuroendocrine neoplasms. Front Oncol. 2021;11:706141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Böger C, Warneke VS, Behrens HM, et al. Integrins alphavbeta3 and alphavbeta5 as prognostic, diagnostic, and therapeutic targets in gastric cancer. Gastric Cancer. 2015;18:784–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Böger C, Kalthoff H, Goodman SL, Behrens H-M, Röcken C. Integrins and their ligands are expressed in non-small cell lung cancer but not correlated with parameters of disease progression. Virchows Arch. 2014;464:69–78. [DOI] [PubMed] [Google Scholar]
- 25. Nabors LB, Mikkelsen T, Hegi ME, et al. A safety run-in and randomized phase 2 study of cilengitide combined with chemoradiation for newly diagnosed glioblastoma (NABTT 0306). Cancer. 2012;118:5601–5607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Reardon DA, Fink KL, Mikkelsen T, et al. Randomized phase II study of cilengitide, an integrin-targeting arginine-glycine-aspartic acid peptide, in recurrent glioblastoma multiforme. J Clin Oncol. 2008;26:5610–5617. [DOI] [PubMed] [Google Scholar]
- 27. Stupp R, Hegi ME, Gorlia T, et al. Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma with methylated MGMT promoter (CENTRIC EORTC 26071-22072 study): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15:1100–1108. [DOI] [PubMed] [Google Scholar]
- 28. Li J, Fukase Y, Shang Y, et al. Novel pure alphaVbeta3 integrin antagonists that do not induce receptor extension, prime the receptor, or enhance angiogenesis at low concentrations. ACS Pharmacol Transl Sci. 2019;2:387–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Janson ET, Knigge U, Dam G, et al. Nordic guidelines 2021 for diagnosis and treatment of gastroenteropancreatic neuroendocrine neoplasms. Acta Oncol. 2021;60:931–941. [DOI] [PubMed] [Google Scholar]
- 30. Hope TA, Bodei L, Chan JA, et al. NANETS/SNMMI consensus statement on patient selection and appropriate use of 177Lu-DOTATATE peptide receptor radionuclide therapy. J Nucl Med. 2020;61:222–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chen H, Zhao L, Fu K, et al. Integrin alphavbeta3-targeted radionuclide therapy combined with immune checkpoint blockade immunotherapy synergistically enhances anti-tumor efficacy. Theranostics. 2019;9:7948–7960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lee SH, Choi JY, Jung JH, et al. Effect of peptide receptor radionuclide therapy in combination with temozolomide against tumor angiogenesis in a glioblastoma model. Cancers (Basel). 2021;13:5029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sandström M, Velikyan I, Garske-Román U, et al. Comparative biodistribution and radiation dosimetry of 68Ga-DOTATOC and 68Ga-DOTATATE in patients with neuroendocrine tumors. J Nucl Med. 2013;54:1755–1759. [DOI] [PubMed] [Google Scholar]