Abstract
Introduction
Vertebral compression fractures (VCF) are the most common low-energy fractures in older people and are associated with increased mortality. To assess mortality risk in patients suffering from VCF, we conducted a retrospective observational long-term cohort study.
Patients and Methods
The study included 270 patients. 221 patients were treated conservatively, and 49 were treated with vertebroplasty. The study group was compared to a control group of 1641 random individuals age and sex-matched. Electronic healthcare data extracted included monthly chronic medications taken regularly 3 months before hospitalisation, analgesics excluded, and date of death.
Results
Patients who suffer from VCF tend to consume more chronic medications. The mean count of chronic medication prescriptions in the 3 months before hospitalisation was 16.41 (±9.11) in the VCF group and 11.52 (± 7.17) in the control cohort (P < .0001). In univariate analysis, patients with VCF showed decreased long-term survival (P < .00). However, when controlled for age, sex, and chronic medications uptake, no significant difference was observed between the groups in a multivariate model (P = .12).
Conclusions
The study demonstrates that VCF as an independent variable has a marginal effect on mortality. The higher mortality prevalent in these patients is due to the deteriorated health status of the patients before fracture.
Keywords: osteoporosis, vertebral compression fracture, mortality, spine surgery, geriatric medicine
Introduction
Vertebral compression fractures (VCF) are the most common low-energy fractures in older people.1 Although the trauma itself is not usually associated with mortality, these fractures are associated with loss of sagittal alignment and acute and chronic back pain,2,3 leading to general physical deterioration and impaired quality of life, factors that have the potential to increase mortality.4
Medical treatment for VCF consists of bed rest, analgesia, and physiotherapy.5 Vertebral augmentation has the potential to prevent treated vertebrae from further collapse and maintain sagittal alignment. The rationale is that general health status and function go hand in hand and that post-fracture deterioration can be prevented by returning to the previous activity level as soon as possible.6 Hence, preventing the general decline and fracture-related mortality so common in the elderly. Vertebroplasty and kyphoplasty are therefore reserved as minimally invasive options for patients who suffer debilitating back pain.7 However, while the open-label trial VERTOS II (vertebroplasty vs conservative treatments in acute osteoporotic vertebral compression fractures II) and the VAPOUR (vertebroplasty for acute painful osteoporotic fractures - 2016) showed better pain relief following vertebroplasty, a randomised sham-controlled trial (VERTOS IV)2018 showed no advantage over the sham procedure for pain management of VCF. These studies focused on pain management and not long-term outcomes or mortality.8
To assess mortality risk in patients suffering from VCF, we conducted a retrospective observational long-term cohort study. We also compared the outcome in patients undergoing vertebral augmentation by vertebroplasty vs those treated by conservative management compared to an age and sex-matched control population.
Patients and Methods
Allocation of patients for the institutional orthopedic database was conducted from 2009 to 2016.15,808 patients treated in the Orthopedics Department were extracted. The database was mined to identify all patients 85 to 65 years of age who were treated for a new vertebral fracture. The records of these patients were manually verified to confirm the diagnosis of vertebral fracture. We noted whether the patient was treated conservatively or with vertebroplasty. The study was approved by the Institution Review Board of the Lady Davis Carmel Medical Center.
The verified cohorts' community electronic healthcare data were extracted, matched, and paired with each patient’s file. The extracted data included an index of general well-being and health status (the number of medications prescribed to the patient within the 3 months prior to hospitalisation) and date of death, where relevant. Our study measured the monthly chronic medications taken regularly, analgesics excluded by patients, and controls as an approximate measure of their underlying health status.
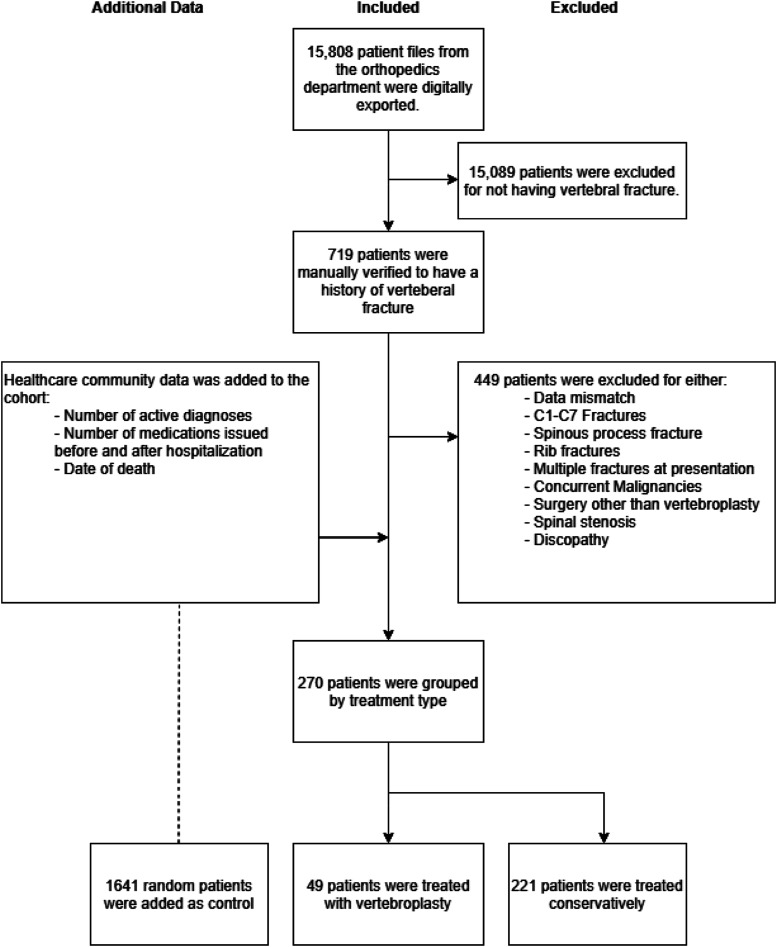
Excluded from the study were patients with C1-C7 fractures, patients who had sustained multiple trauma at the time of vertebral fracture, patients with over 1 newly diagnosed fracture, spinous or lateral process fractures, other fractures besides osteoporotic vertebral fracture and presence of intravertebral lesions, and patients with concurrent known malignancies (including multiple myelomas, carcinomas, and sarcomas), We also excluded patients who underwent spinal surgery other than vertebroplasty—the study cohort comprised 270 patients meeting all criteria (Figure 1).
Figure 1.
Inclusion and exclusion of the study population.
To compare VCF patients with general population, we extracted a control group of 1641 random individuals in the same HMO database. These were age and sex-matched to have similar parameters to the VCF cohort but without vertebral fracture.
Statistical Analysis
Clinical features between groups were evaluated using the Chi-square test, ANOVA, or Non-Parametric tests (Kruskal-Wallis or Mann-Whitney) as appropriate.
Follow-up was calculated from admission until death or until 31 October 2018. The control group was extracted to represent patients followed over a similar 10-year period (February 2008- February 2018).
The results are presented as hazard ratios and their 95% confidence intervals. Data were analysed using IBM SPSS v25.0. A 2-sided P value of <.05 was considered statistically significant. Overall survival was evaluated using a Cox proportional hazard regression model and Log Rank to compare groups.
Results
Patient Population
Demographic data are given in Table 1. The study cohort included 270 patients with VCF (63 male, 207 female). Vertebroplasty was performed in 49 (18.1%) of the VCF patients, 221 (81.9%) conservatively. Patients managed conservatively were slightly older than those undergoing vertebroplasty and those in the control cohort (76.8 ± 5.5 vs 75.8 ± 5.9 and 75.6 ± 5.9 years, P = .024).
Table 1.
Baseline Characteristics of Patients with Vertebral Fractures Conservatively and Surgically Treated and Controls.
| Group | P-value | |||||||
|---|---|---|---|---|---|---|---|---|
| Vertebroplasty | Conservative | Control | ||||||
| Mean | Count | Mean | Count | Mean | Count | |||
| Total number | 49 (2.6%) | 221 (11.6%) | 1641 (85.9%) | |||||
| Age (mean ± SD) | 75.78 (±5.89) | 76.75 (±5.53) | 75.6 (±5.89) | .024 | ||||
| Gender | Male | 12 (24.5%) | 51 (23.1%) | 418 (25.5%) | ||||
| Female | 37 (75.5%) | 170 (76.9%) | 1223 (74.5%) | .74 | ||||
| Medications taken in 3 months before hospitalization (mean ± SD)a | 17.84 (±8.62) | 16.41 (±9.02) | 11.52 (±7.17) | <.00 | ||||
aNumbers represent the mean prescriptions drawn from pharmacy 3 months prior to the fracture, analgesics excluded.
The mean count of chronic medication prescriptions in the 3 months before hospitalisation was 16.41 (±9.11) in the conservative group, 17.84 (±8 .61) in vertebroplasty patients, and 11.52 (± 7.17) in the control cohort (P < .0001). There was no difference between the conservative and vertebroplasty treated VCF groups (P = .67).
Mortality
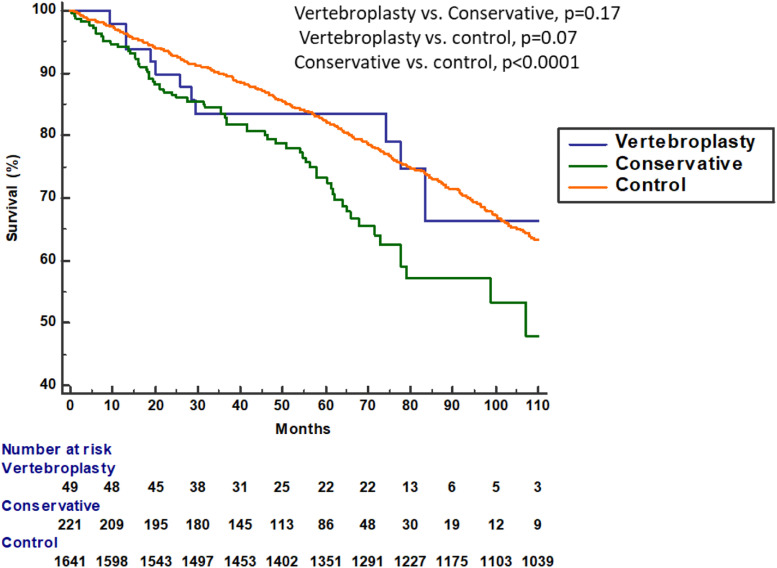
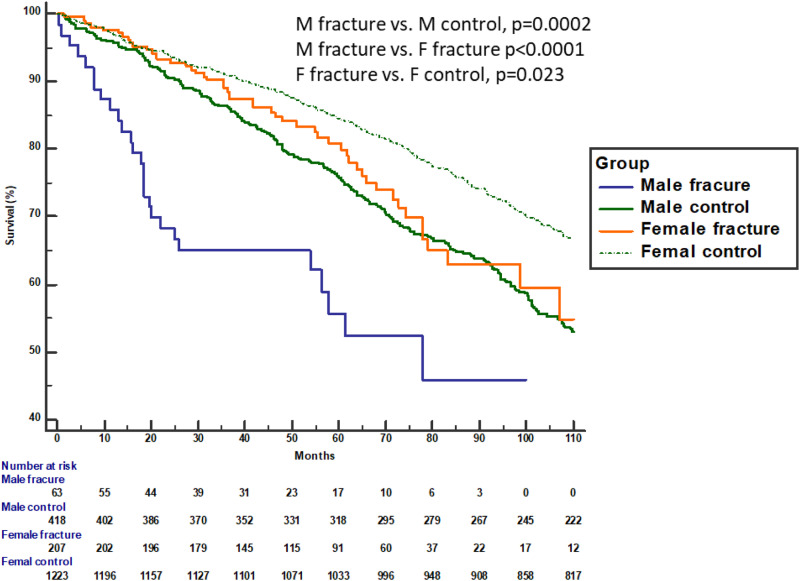
By univariate analysis, the vertebroplasty group fared better with an estimated 96 months survival period vs 85 months. In addition, the vertebroplasty group showed a reduction of 18% in mortality over 10 years compared to the conservative treatment group. However, the difference was not significant (P = .17). When analysing against the control group, it was shown that the control group survived significantly better than the conservative treatment group (P < .00). No significant difference in survival was found between the vertebroplasty and the control group (P = .78) (Figure 2). In univariate analysis, differentiating men vs women, men presented a shorter survival time than women (P < .00), as shown in Figure 3.
Figure 2.
Unadjusted Kaplan-Meier survival curve for age, sex-matched cohorts of conservative, vertebroplasty, and control cohorts.
Figure 3.
Unadjusted Kaplan-Meier survival curve for male and female age-matched cohorts of control and conservative treatment cohorts.
In a multivariate COX regression for mortality by treatment group the following hazards ratio values were found- Age HR-1.12 (Cl = 95% 1.10-1.13; <.0001) per year, Gender HR-1.53 (Cl = 95% 1.31-1.80; <.0001) for men compared to women, Chronic Medications HR-1.05 (Cl = 95% 1.04-1.06; P < .0001) per prescription drawn from pharmacy 3 months prior to the fracture event (Table 2).
Table 2.
Proportional Cox Regression Models for 10 years Mortality.
| Univariable Model | P-value | Multivariable Model | ||||||
|---|---|---|---|---|---|---|---|---|
| Mortality | ||||||||
| no = 1173 | Yes = 738 | H.R | 95%CI | H.R | 95%CI | P-value | ||
| Variables | ||||||||
| Group, n (%) | ||||||||
| Vertebroplasty | 38 (3.2) | 11 (1.5) | 1.09 | .60, 1.97 | .79 | .99 | .54, 1.80 | .97 |
| Conservative | 155 (13.2) | 66 (9.0) | 1.66 | 1.28, 2.15 | <.0001 | 1.23 | .94, 1.61 | .12 |
| Control | 980 (83.5) | 661 (89.5) | Ref | Ref | ||||
| Gender | ||||||||
| Male | 246 (51.0) | 927 (64.8) | 1.57 | 1.34, 1.83 | <.0001 | 1.53 | 1.31, 1.80 | <.0001 |
| Female | 235 (49.0) | 503 (35.2) | Ref | Ref | ||||
| Age, mean ±Std | 74.02 ± 5.64 | 78.46 ± 5.12 | 1.13 | 1.11, 1.15 | <.0001 | 1.12 | 1.10, 1.13 | <.0001 |
| Chronic medication past 3 months, mean ±Stda | 10.89 ± 6.91 | 14.41 ± 8.27 | 1.06 | 1.05, 1.07 | <.0001 | 1.05 | 1.04, 1.06 | <.0001 |
| Stratification | ||||||||
| Male | N = 246 | N = 235 | ||||||
| Group, n (%) | ||||||||
| Vertebroplasty | 9 (3.7) | 3 (1.3) | 1.34 | .43, 4.22 | .62 | 1.12b | .35, 3.60 | .85 |
| Conservative | 27 (11.0) | 24 (10.2) | 2.30 | 1.50, 3.56 | .0002 | 2.16b | 1.38, 3.38 | .001 |
| Control | 210 (85.4) | 208 (88.5) | Ref | Ref | ||||
| Female | N = 927 | N = 503 | ||||||
| Group, n (%) | ||||||||
| Vertebroplasty | 29 (3.1) | 8 (1.6) | 1.07 | .53, 2.15 | .85 | .92b | .54, 1.85 | .81 |
| Conservative | 128 (13.8) | 42 (8.3) | 1.51 | 1.09, 2.08 | .013 | .99b | .71, 1.38 | .95 |
| Control | 770 (83.1) | 453 (90.1) | Ref | Ref | ||||
95% CI = 95% confidence interval.
aNumbers represent the mean prescriptions drawn from pharmacy 3 months prior to the fracture, analgesics excluded.
bAdjusted to age and Chronic medication past 3 months.
Comparing conservative treatment to control groups, there was no significant trend for higher mortality in patients treated conservatively HR = 1.23 (Cl = 95% .94-1.61; P = .12). No difference was found between vertebroplasty and the control group regarding mortality HR = .99 (Cl = 95% .54-1.80; P = .97).
Discussion
The main findings of this study were that compared with an age and sex-matched control group, in univariate analysis, patients with VCF who were managed conservatively had decreased long-term survival. However, when controlled for age, sex, and chronic medications uptake, no significant difference was observed between the groups in a multivariate model. Lau et al9 found a mortality hazard ratio of 1.83 and 1.37 after adjustment for comorbidities, concerning our mortality hazard ratio of 1.66 (1.28-2.15 95% Cl) and an adjusted mortality hazard ratio of 1.23 (.94-1.61 95% Cl). Both studies show a trend toward increased mortality following a vertebral compression fracture; however, we see attenuation of the effect when controlled for comorbidities. This suggests that deteriorated health status before the fracture is correlated with increased mortality and not the fracture itself. Studies on the subject that do not control for comorbidities find a significant correlation between a VCF and mortality.10-13 Our study rejects that assumption.
Women do not seem to present increased mortality after a fracture as men do. This may be partially due to the higher life expectancy in women in Israel, an average of about 4 years.14 However, part of the difference is correlated to the fracture event since mortality rates in men treated conservatively were significantly higher than the men in the control group in a univariate and multivariate model. We expect men’s generally higher bone density to be protective, lowering fracture risk. A fracture that occurs in men likely demands higher energy than a fracture in women, leaving much of the men population unharmed after a minor fall, unlike women, which gives us a higher ratio of women to men who suffer from VCF.15,16 Because of this, we assume that the population of men who suffer from a fracture represents an especially frail group of men who suffer from low bone density and higher fall probability with respect to men of the same age. This group of men shows a stepwise deterioration that results in increased mortality.
Comparing interventional with conservative therapy, the data are less transparent since studies are observational. McDonald et al compared 524 patients treated with vertebroplasty to 589 patients managed conservatively over 8 years.17 They found no difference in mortality between groups and showed that vertebroplasty recipients retained higher mortality after the procedure. Another group from Albany (Kurra et al) showed no difference in survival effect in patients with a vertebral compression fracture treated by kyphoplasty, as opposed to patients treated conservatively.18 Edidin et al reported on the Medicare data set (2005-2008) of 858,978 VCF patients, comparing operated and conservatively treated VCF. The study concluded that patients in the operated cohort had a higher adjusted survival rate of 60.8% compared to 50.0% for individuals in the non-operated cohort at 4 years of follow-up, adjusted for comorbidities by the Charlson comorbidity index [hazard ratio (HR) = .63, P < .001].19,20 The conclusion is further emphasised by the fact that although a significant component of asymptomatic patients comprises the conservatively treated group, surgically treated cohort which presents symptoms demonstrates lower mortality rates. It is possible that other studies would concur if they had included a larger patient cohort. The main argument against invasive vertebroplasty and kyphoplasty as a treatment is the lack of evidence of an analgesic effect. Since conservative treatment is usually satisfactory after a few months, there is a lack of need for operative measures for pain management. While focusing on mortality, our study doesn’t have sufficient power to reach the same conclusions. However, the need for a larger cohort to gain sufficient significance suggests that the number needed to treat to achieve a mortality reduction is high, questioning the procedure’s effectiveness in that regard.
Relation to Underlying Patient Health Status
Patients with VCF were receiving, in the months preceding the fracture, some 50% more chronic medications than the control cohort, with no difference between VCF patients treated conservatively and those undergoing vertebroplasty. However indirect, in a study based on electronic health records, medication prescription data may be a reasonable method to gauge comorbidity and underlying patient health than other electronic health care references. The increased medication use in VCF patients may imply that decreased health status may be a risk factor for VCF. Falls in the elderly population are the basis for increased risk of traumatic fracture, and most authors find an association with the increased use of medications.21-25 Medications such as benzodiazepines, psychoactive drugs, vasodilators, diuretics, or adrenergic receptor blockers increase the risk of falls and, are expected to be in increased consumption in the study population.21 Kado et al conducted a prospective study on 9575 women demonstrating that women who suffer from osteoporotic vertebral fracture were more likely to have poor health status.26 Their study was cross-sectional rather than adjusted for age and gender, as in the present study.
We expected malignancies to be in higher frequency with patients suffering from vertebral fractures relative to the general population, which raises the expected mortality due to the malignancy rather than the fracture itself.27 Thus, to focus on mortality due to VCF, we excluded patients diagnosed with concurrent malignancy at the time of hospitalisation or those investigated for malignancy during their hospital stay.
Since sagittal spinal misalignment is a predictive factor for chronic pain, we expected more of it with more severe fracture patterns. However, available diagnostic and procedure codes in the record system did not allow for the characterisation of fractures. Although more severe fracture patterns may be associated with more significant trauma, we could not consider its impact on mortality. Moreover, the study did not include radiographic follow-up on patients, so the degree of sagittal misalignment could not be considered.
Potential Limitations of the Study
This was a single-centre retrospective cohort study. However, the study included patients mined from a relatively large database of over 15,000 consecutive orthopaedic patients treated for over10 years and matched to age and gender controlled group of over 1500 patients. Clinical selection bias may have influenced the findings. A slight age difference was noted between patients managed conservatively and those treated by vertebroplasty, and other unknown confounders may have influenced treatment selection. On the other hand, chronic medication usage was similar at the time of VCF in the conservative and vertebroplasty groups, suggesting a comparable level of health. A slight significant difference was noted between conservative and control groups’ ages after allocation of the control group. This is probably due to the usage of a large control cohort, and we don’t see the difference between the groups as clinically significant. It should be noted that this work includes patients with clinically manifested VCF only. We acknowledge that about two-thirds of vertebral fractures don’t present acutely.28 However, we assume that patients admitted due to their pain present with a more severe fracture and should manifest a poorer prognosis with respect to patients who are not. Since our work suggests non-inferiority of conservative management in this group, we assume the same for patients who suffer from a less severe fracture.
Electronic medical records were used to estimate underlying patient health status. We adjusted for general health status by the number of medications drawn from pharmacies, analgesics excluded. We refrained from using the Charlson comorbidity index since it would rely on the ICD-9-CM coding reference documented by the family physician. Considering the differing recording habits of medical practitioners, we expected this variable to be less reliable than the number of medications drawn from pharmacies. A similar method was explored by Häppölä et al who demonstrated that, when used alone, a data-driven medication score performs similarly to a classic comorbidity index in predicting 10 year mortality in the general ageing population.28 Because of the plethora of available drugs and generics, we could not identify medications that may lower or increase the risk of osteoporosis. Medications such as bisphosphonate s, glucocorticoids, proton pump inhibitors, and selective serotonin receptor inhibitors adjust fracture risk and may confound the data.29
In Summary
The current study demonstrates that, in women, VCF has a marginal effect on mortality, which is associated with deteriorated health prior to the fracture event. In men, however, the effect on mortality is significant.30
Regarding pain, there is a controversy over treatments such as vertebroplasty and kyphoplasty due to the lack of consensus over evidence of an analgesic effect. Conservative treatment might not demonstrate adequate results. However, the lack of solid evidence precludes recommending an operative option. On the other hand, Concerning mortality, our study shows that conservative treatment is adequate since cohorts who didn’t suffer from VCF demonstrate a similar mortality trend. Vertebroplasty wasn’t proven as a viable treatment because of that reason. Our study indicates that VCF is not a life-altering event.
Clinical Implications
This real-world cohort study suggests that patients with VCF have reduced life expectancy due to deteriorated health prior to the fracture event.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Ariel Zohar https://orcid.org/0000-0002-2669-0922
Itamar getzler https://orcid.org/0000-0001-6453-1423
References
- 1.Melton LJ. Epidemiology of spinal osteoporosis. Spine. 1997;22:2S-11S. [DOI] [PubMed] [Google Scholar]
- 2.Zhang Y-L, Shi L-T, Tang P-F, Sun ZJ, Wang YH. Correlation analysis of osteoporotic vertebral compression fractures and spinal sagittal imbalance. Orthopä. 2017;46:249-255. [DOI] [PubMed] [Google Scholar]
- 3.Ross PD. Clinical consequences of vertebral fractures. Am J Med. 1997;103:30S-42S. [DOI] [PubMed] [Google Scholar]
- 4.Smith D, Wilkie R, Croft P, McBeth J. Pain and mortality in older adults: The influence of pain phenotype. Arthritis Care Res. 2018;70:236-243. [DOI] [PubMed] [Google Scholar]
- 5.Ensrud KE, Schousboe JT. Clinical practice. Vertebral fractures. N Engl J Med. 2011;364:1634-1642. [DOI] [PubMed] [Google Scholar]
- 6.Stadhouder A, Buskens E, Vergroesen DA, Fidler MW, Nies F, Oner FC. Nonoperative treatment of thoracic and lumbar spine fractures: a prospective randomized study of different treatment options. J Orthop Trauma. 2009;23:588-594. [DOI] [PubMed] [Google Scholar]
- 7.Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine. 2000;25:923-928. [DOI] [PubMed] [Google Scholar]
- 8.Clark W, Bird P, Gonski P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016;388:1408-1416. [DOI] [PubMed] [Google Scholar]
- 9.Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am. 2008;90:1479-1486. [DOI] [PubMed] [Google Scholar]
- 10.Johnell O, Kanis JA, Odén A, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15:38-42. [DOI] [PubMed] [Google Scholar]
- 11.Puisto V, Rissanen H, Heliövaara M, Knekt P, Helenius I. Mortality in the presence of a vertebral fracture, scoliosis, or Scheuermann’s disease in the thoracic spine. Ann Epidemiol. 2008;18:595-601. [DOI] [PubMed] [Google Scholar]
- 12.Pongchaiyakul C, Nguyen ND, Jones G, Center JR, Eisman JA, Nguyen TV. Asymptomatic vertebral deformity as a major risk factor for subsequent fractures and mortality: a long-term prospective study. J Bone Miner Res. 2005;20:1349-1355. [DOI] [PubMed] [Google Scholar]
- 13.Naves M, Díaz-López JB, Gómez C. The effect of vertebral fracture as a risk factor for osteoporotic fracture and mortality in a Spanish population. Osteoporos Int. 2003;14:520-524. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization . World Health Statistics 2017: Monitoring Health for the SDGs, Sustainable Development Goals. Geneve: World Health Organization; 2017. [Google Scholar]
- 15.de Klerk G, Hegeman JH, Bronkhorst P, van der Palen J, van der Velde D, Duis HJ. The (a)-Symptomatic Vertebral Fracture. Geriatr Orthop Surg Rehabil. 2012;3:74-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Waterloo S, Ahmed LA, Center JR, et al. Prevalence of vertebral fractures in women and men in the population-based Tromsø Study. BMC Musculoskelet Disord. 2012;13:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDonald RJ, Achenbach S, Atkinson E, et al. Mortality in the vertebroplasty population. AJNR Am J Neuroradiol. 2011;32:1818-1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.KURRA S, METKAR U, LIEBERMAN IH, Lavelle WF. The effect of kyphoplasty on mortality in symptomatic vertebral compression fractures: A review. Int J Spine Surg. 2018;12:543-548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edidin AA, Ong KL, Lau E, Kurtz SM. Morbidity and mortality after vertebral fractures: comparison of vertebral augmentation and nonoperative management in the medicare population. Spine. 2015;40:1228-1241. [DOI] [PubMed] [Google Scholar]
- 20.Edidin AA, Ong KL, Lau E, Kurtz SM. Mortality risk for operated and nonoperated vertebral fracture patients in the medicare population. J Bone Miner Res. 2011;26:1617-1626. [DOI] [PubMed] [Google Scholar]
- 21.Sorock GS. Falls among the elderly: epidemiology and prevention. Am J Prev Med. 1988;4:282-288. [PubMed] [Google Scholar]
- 22.Prudham D, Evans JG. Factors associated with falls in the elderly: a community study. Age Ageing. 1981;10:141-146. [DOI] [PubMed] [Google Scholar]
- 23.Granek E, Baker SP, Abbey H, et al. Medications and diagnoses in relation to falls in a long-term care facility. J Am Geriatr Soc. 1987;35:503-511. [DOI] [PubMed] [Google Scholar]
- 24.Graafmans WC, Ooms ME, Hofstee HMA, Bezemer PD, Bouter LM, Lips P. Falls in the Elderly: A Prospective Study of Risk Factors and Risk Profiles. Am J Epidemiol. 1996;143:1129-1136. [DOI] [PubMed] [Google Scholar]
- 25.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701-1707. [DOI] [PubMed] [Google Scholar]
- 26.Kado DM. Vertebral Fractures and Mortality in Older Women: A Prospective Study. Arch Intern Med. 1999;159:1215. [DOI] [PubMed] [Google Scholar]
- 27.Saad F, Lipton A, Cook R, Chen YM, Smith M, Coleman R. Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer. 2007;110:1860-1867. [DOI] [PubMed] [Google Scholar]
- 28.Fink HA, Milavetz DL, Palermo L, et al. What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res. 2005;20:1216-1222. [DOI] [PubMed] [Google Scholar]
- 29.Häppölä P, Havulinna AS, Tasa T, et al. A data-driven medication score predicts 10-year mortality among aging adults. Sci Rep. 2020;10:15760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Panday K, Gona A, Humphrey MB. Medication-induced osteoporosis: screening and treatment strategies. Ther Adv Musculoskelet Dis. 2014;6:185-202. [DOI] [PMC free article] [PubMed] [Google Scholar]