Abstract
Objective:
Cooling devices (CDs) worn under personal protective equipment (PPE) can alleviate some of the heat stress faced by health care workers responding to the Ebola outbreak in West Africa.
Methods:
Six healthy, young individuals were tested while wearing 4 different CDs or no cooling (control) under PPE in an environmental chamber (32°C/92% relative humidity) while walking (3 METs, 2.5 mph, 0% grade) on a treadmill for 60 minutes. Exercise was preceded by a 15-minute stabilization period and a 15-minute donning period.
Results:
The control condition resulted in a significantly higher rectal temperature (Tre) at the end of the exercise than did all CD conditions (CD1, P = 0.004; CD2, P = 0.01; CD3, P = 0.000; CD4, P = 0.000) with CD1 and CD2 resulting in a higher Tre than CD3 and CD4 (P < 0.05). The control condition resulted in a higher heart rate (HR) at the end of exercise than did the CD3 (P = 0.01) and CD4 (P = 0.009) conditions, whereas the HR of the CD1 and CD2 conditions was higher than that of the CD3 and CD4 conditions (P < 0.05). Weight loss in the control condition was higher than in the CD3 (P = 0.003) and CD4 (P = 0.01) conditions. Significant differences in subjective measurements of thermal stress were found across conditions and time.
Conclusions:
Use of CDs can be advantageous in decreasing the negative physiological and subjective responses to the heat stress encountered by health care workers wearing PPE in hot and humid environments.
Keywords: environmental exposure, extreme heat, emergency preparedness, disease outbreaks, emergency medicine
Risk for heat-stress-related injuries is increased greatly for occupations that require wearing of impermeable or nonporous personal protective equipment (PPE) while working in hot and humid environments.1,2 One of several possible examples of such an occupation is health care workers (HCWs) who have been called to respond to the Ebola outbreak in West Africa. While heightened transmission-based precautions for HCWs treating Ebola patients provide elevated protection from pathogens, these precautions require additional layers of PPE that can increase the burden of heat stress. Additionally, respiratory protection must be used to protect HCWs from potential pathogen transmission during aerosol-generating medical procedures. The hot, humid environmental conditions in West Africa are such that heat-stress-related injuries must be considered when recommending and using PPE for extended work shifts to maximize HCW safety. The Centers for Disease Control and Prevention (CDC) has recently recommended that HCWs treating Ebola patients should use fluid-resistant or impermeable gowns or coveralls for optimal protection from Ebola virus transmission.3 These additional, impermeable layers decrease the body’s homeostatic ability to carry out physiological cooling strategies through sweat evaporation, convection, and radiation. In addition, PPE can increase the HCW’s workload and heat production as a result of the added weight of the entire ensemble, which adds an additional 3.8 to 4.2 kg depending on the combination used. These factors contribute to reports of HCWs only being physically able to wear PPE for short, limited periods of approximately 40 working minutes before requiring a rest break to avoid heat stress.4,5 In order to provide continuous care to a large number of patients, more HCWs would be required to fill the gaps created by necessary breaks in shift work. Frequent breaks in HCW shift work, to allow for cooling, require frequent donning and doffing of potentially contaminated PPE and increase the risk of pathogen transmission from the PPE to the HCW. Also, single-use PPE is in limited supply, and providing new PPE for frequent shift work is not economical or practical in an emergency effort such as the Ebola outbreak.
It is important to understand and create ways to improve PPE to decrease the potential of heat stress and heat-stress-related injuries. Possible improvements in PPE can be achieved through a greater understanding of the balance between fabric permeability and the associated heat load. It is generally understood that with greater impermeability of a fabric comes increased heat load.2 Secondary to alterations in the PPE fabric characteristics and garments chosen, cooling strategies can be considered for use during work. Such strategies can include cooling devices (CDs) that are worn underneath the PPE garments throughout the working hours. A CD in this text refers to a cooling vest that includes the vest itself as well as the cooling medium such as ice packs or water circulation hoses. CDs may help to slow the increase in core temperature while using PPE in a hot and humid environment, which could allow workers to work more safely for longer periods of time. It is, however, important to understand the characteristics of CDs in achieving this goal as many CD options exist. Different CDs have varying properties that must be considered, such as weight, cooling material, cooling effectiveness, field practicality, and ergonomics.
The purpose of this study was to test the physiological impact of the use of 4 different CDs, in conjunction with PPE, during low-intensity exercise (mimicking the work intensity of HCWs involved in patient care) in a hot and humid environment similar to the ambient conditions of West Africa.
METHODS
Subjects
Six healthy male subjects completed a general health screening conducted by a licensed physician and were cleared for exercise testing (mean height, 1.84 ± 0.09 m; weight, 75.05 ± 10.27 kg; body mass index [in kg/m2], 22.15 ± 2.31). The study was approved by the National Institute for Occupational Safety and Health’s (NIOSH) Human Subjects Review Board and written informed consent was obtained prior to study participation. All subjects were given orientation to the testing protocol, the purpose of the study, and any potential risks involved with their participation before beginning testing. Subjects were instructed to abstain from alcohol, caffeine, and strenuous exercise for at least 24 hours before their test visit. Female subjects were excluded to limit a potential confounding effect due to gender variation from menstrual cycling on the small sample size.
Testing Protocol
Each of the 6 participants was tested a total of 5 times, once for each condition: 4 different cooling devices (CD1, CD2, CD3, and CD4) and 1 control condition. A PPE ensemble recommended for use in West Africa during the Ebola outbreak was worn during each test. The ensemble consisted of medical scrubs, socks and rubber boots, Tychem QC highly impermeable coverall (DuPont, Wilmington, DE), Médecins Sans Frontières custom-made Tyvek (DuPont) hood with integrated splash-resistant surgical mask, rubber surgical apron, splash-resistant goggles, surgical nitrile inner gloves, heavy-duty nitrile outer gloves, duckbill N95 filtering face piece respirator (model 46828; Kimberly Clark, Irving, TX), and fluid-resistant surgical cap (KCH69240; Kimberly Clark). Each test was completed within environmental conditions that represented conditions of many areas of West Africa affected by the Ebola outbreak. The exercise protocol consisted of 60 minutes of continuous treadmill walking (3 METs, 2.5 mph, 0% grade) in an environmental chamber set at 32°C, 92% relative humidity. This exercise intensity was chosen to represent the working intensity seen in HCWs during patient care, such as walking, standing, and carrying light objects. Each testing session consisted of a 15-minute pre-exercise stabilization period, a 15-minute CD and PPE donning period, and a 60-minute exercise period. During the stabilization period, each subject was instructed to sit quietly in a chair as the environmental conditions were stabilized. Each subject’s test was separated by at least a 48-hour washout period to minimize confounding effects of heat acclimation, dehydration, or fatigue. All subjects were un-acclimated to exertion in the heat prior to testing. If predetermined termination criteria were met during exercise (rectal temperature [Tre] ≥ 39.5°C, heart rate [HR] ≥ 95%,HRmax > 2 minutes, volitional fatigue [rating of perceived exertion ≥ 19], subject’s desire to stop), the testing was stopped immediately and the subject was asked to complete the testing protocol for that same CD on the next visit.
Testing Devices
Four different CDs were tested on each subject. The testing order of the CDs was randomized to minimize possible effects of testing order on outcome variables. The 4 CDs consisted of an upper body vest with different cooling materials (ice, phase-change materials [PCMs], or circulating water). The CDs tested were all size medium, which accommodated an appropriate fit for all test subjects. All CDs were worn underneath PPE but over standard medical scrubs.
CD1 was a cotton vest shell with a thermal liner, 4 pockets (2 in front, 2 in back) for cooling packs, and 4 PCM cooling packs (34.25 cm × 15.25 cm). The ready-to-use weight was 2.78 kg.
CD2 was a polyester vest outer shell with a mesh inner shell, 22 pockets for holding cooling packs, and 22 PCM cooling packs (12.75 cm × 7 cm). The ready-to-use weight was 2.24 kg.
CD3 was a cotton shell vest with 5 pockets for cooling packs and 5 gel ice packs (34.25 cm × 12.75 cm). The ready-to-use weight was 2.78 kg.
CD4 was a cotton shell vest with tubing routed throughout vest and a backpack with pump, battery, and semi-frozen water supply. CD4 used a battery-operated pump to deliver cold water from a partially frozen reservoir of water through tubing within the vest. The ready-to-use weight was 7.15 kg.
Test Measurements
Seminude weight (kg) was measured both before and after exercise to evaluate sweating weight loss throughout testing. Tre was monitored by using a rectal thermistor (model REF-4491; YSI Temperature, Dayton, OH) inserted 13 cm beyond the anal sphincter.
HR was measured continuously by using the Zephyr Bio-Harness 3 (Zephyr Technology Corp, Annapolis, MD). Five subjective variables were obtained every 15 minutes throughout exercise and recovery: heat sensation, thermal comfort, rating of perceived exertion (RPE), breathing comfort, and wetness. Heat sensation was measured on a scale of 4 to −4 (where 4 = very hot, 0 = neutral, and −4 = very cold).6,7 Thermal comfort was measured on a scale of 1 to 4 (where 1 = not uncomfortable and 4 = very uncomfortable).8 RPE was measured by use of the Borg 6–20 exertional scale.9 Breathing comfort was measured by using a scale of 1 to 7 (where 1 = no discomfort and 7 = intolerable discomfort). Subjective wetness was measured by using a scale of 1 to 5 (where 1 = dry and 5 = soaked). A posttest questionnaire was given to each participant to identify the specific ease of use and comfort characteristics of each CD (Table 1).
TABLE 1.
Subjective Questionnairea
| Q1. How easily did you don/doff the PPE? | (Scale: 1–7; 1: very easy, 7: very difficult) |
| Q2. How easily did you don/doff the CD? | (Scale: 1–7; 1: very easy, 7: very difficult) |
| Q3. If any, identify PPE or CD component limiting donning/doffing. | |
| Q4. How heavy was the PPE (and CD) when performing the work? | (Scale: 1–5; 1: very light, 5: extremely heavy) |
| Q5. How did the PPE (and CD) fit? | (Scale: 1–5; 1: very tight, 5: very loose) |
| Q6. How much did the PPE (and CD) restrict your freedom of movement when performing the work? | (Scale: 1–5; 1: no interference, 5: extreme interference) |
| Q7. How would you rate overall wearing comfort of the PPE (and CD)? | (Scale: 1–5; 1: comfortable, 5: extremely uncomfortable) |
| Q8. If any, identify PPE or CD component limiting fit, movement, or wearing comfort. |
Abbreviations: CD, cooling device; PPE, personal protective equipment.
Statistical Analysis
Each measurement variable was calculated for mean and standard deviation for 3 time periods: stabilization, start of exercise, and end of exercise. Two-way repeated-measures ANOVA was used to determine main effects of time in each condition. Time points of start of exercise, end of exercise, and end of recovery were considered for Tre, HR, and all subjective measurements. Significant differences in mean weight loss across ensembles were tested by using a paired t-test. The least significant difference method was used to evaluate individual differences across conditions in post hoc pairwise comparisons. The alpha level was set at P < 0.05 for all tests.
Predicted time to reach Tre = 39.0°C, the temperature over 1 hour at which decrements in simple mental performance is noted,10 was calculated by using the continuously measured Tre data throughout the testing protocol. A polynomial trend line was then created to extend the measured values out in greater duration and solve for time when Tre = 39.0°C for each condition.
RESULTS
As shown in Figure 1, average Tre was greatest (38.86 ± 0.42°C) in the control condition at the end of exercise. A main effect of time and condition was found on Tre (P = 0.000 for both). Post hoc pairwise comparisons revealed that, at the end of exercise, the control condition resulted in a significantly higher Tre than did the CD1 (38.26 ± 0.34°C, P = 0.004), CD2 (38.43 ± 0.37°C, P = 0.01), CD3 (37.94 ± 0.43°C, P = 0.000), and CD4 (37.87 ± 0.43°C, P = 0.000) conditions. The CD1 condition resulted in a significantly higher Tre at the end of exercise than did the CD3 (P = 0.01) and CD4 (P = 0.004) conditions. The CD2 condition resulted in a significantly higher Tre at the end of exercise than did the CD3 (P = 0.02) and CD4 (P = 0.006) conditions.
FIGURE 1.
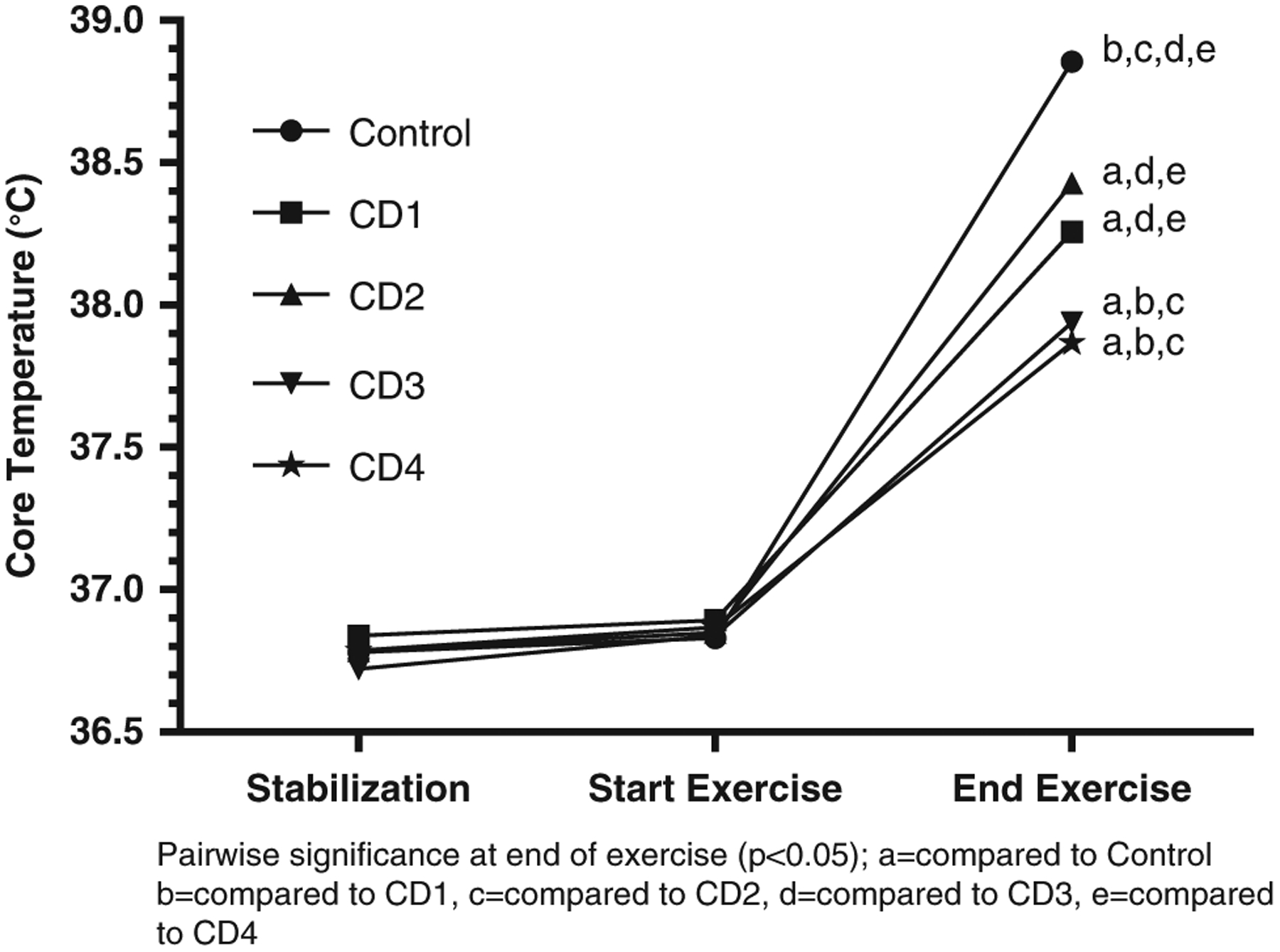
Average Core Temperature (Tre).
Abbreviation: CD, cooling device.
Using the continuous Tre information, a predicted time to reach Tre = 39.0°C was calculated for each condition and is shown in Table 2. The control condition was predicted to have the shortest time to Tre = 39.0°C with a predicted time of 63.86 minutes. The longest predicted time to Tre = 39.0°C was shown in the CD4 condition with a predicted time of 93.93 minutes. All CD conditions showed an increased time to Tre = 39.0°C compared with the control condition.
TABLE 2.
Predicted Exercise Time in Minutes to Tre = 39°Ca
| Condition | Predicted Time (minutes) |
|---|---|
| Control | 63.86 |
| CD1 | 81.86 |
| CD2 | 78.37 |
| CD3 | 79.77 |
| CD4 | 93.93 |
Abbreviations: CD, cooling device; Tre, rectal temperature.
Main effects of time (P = 0.000) and condition (P = 0.006) were also found on HR. Figure 2 shows HR across 3 time points separated by CD condition. Post hoc pairwise comparisons revealed significant individual differences across conditions. All significant pairwise differences were found at the end-of-exercise time point across conditions. The control condition resulted in a significantly higher HR (163.17 ± 13.33 bpm) than did the CD3 (134.83 ± 17.24 bpm, P = 0.01) and CD4 (129.00 ± 12.70 bpm, P = 0.009) conditions. The CD1 condition resulted in a significantly higher HR (148.67 ± 8.71 bpm) than did the CD3 (P = 0.04) and CD4 (P = 0.008) conditions. The CD2 condition resulted in a significantly higher HR (157.67 ± 17.60 bpm) than did the CD3 (P = 0.03) and CD4 (P = 0.02) conditions.
FIGURE 2.
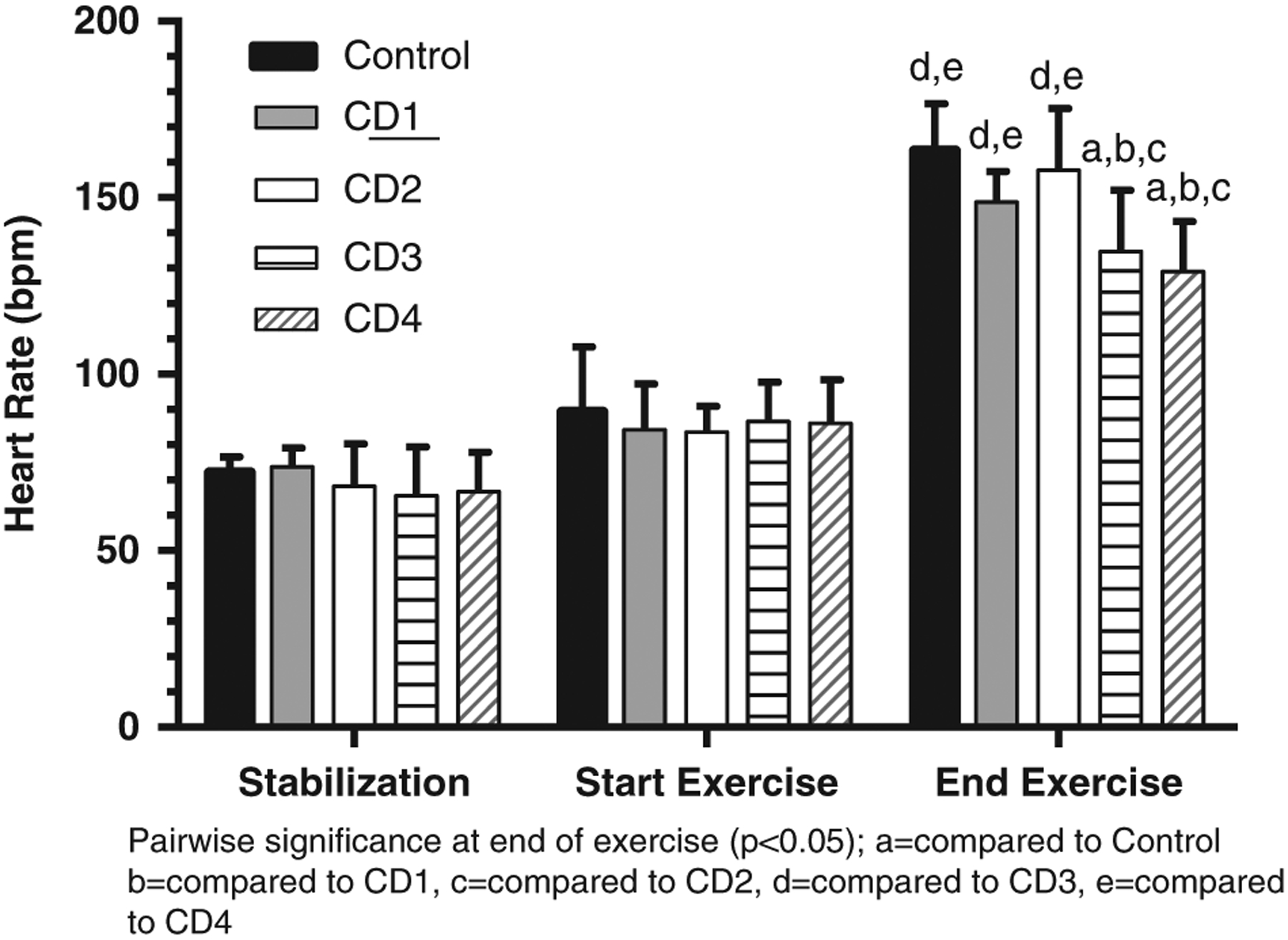
Average Heart Rate.
Abbreviation: CD, cooling device.
Figure 3 compares average weight loss across all 5 conditions. A repeated-measures ANOVA revealed a significant difference across the 5 devices (P = 0.000). Post hoc comparisons showed that weight loss in the control condition (1.34 ± 0.36 kg) was significantly higher than in the CD3 (1.00 ± 0.31 kg, P = 0.003) and CD4 (0.91 ± 0.26 kg, P = 0.01) conditions. Weight loss in the CD1 condition (1.18 ± 0.34 kg) was significantly higher than in the CD3 (P = 0.03) and CD4 (P = 0.03) conditions. Weight loss in the CD2 condition (1.26 ± 0.31 kg) was significantly higher than in the CD3 (P = 0.003) and CD4 (P = 0.004) conditions. Weight loss in the CD3 condition was significantly lower than in the control (P = 0.003), CD1 (P = 0.03), and CD2 (0.003) conditions. Weight loss in the CD4 condition was significantly lower than in the control (P = 0.012), CD1 (P = 0.039), and CD2 (0.004) conditions.
FIGURE 3.
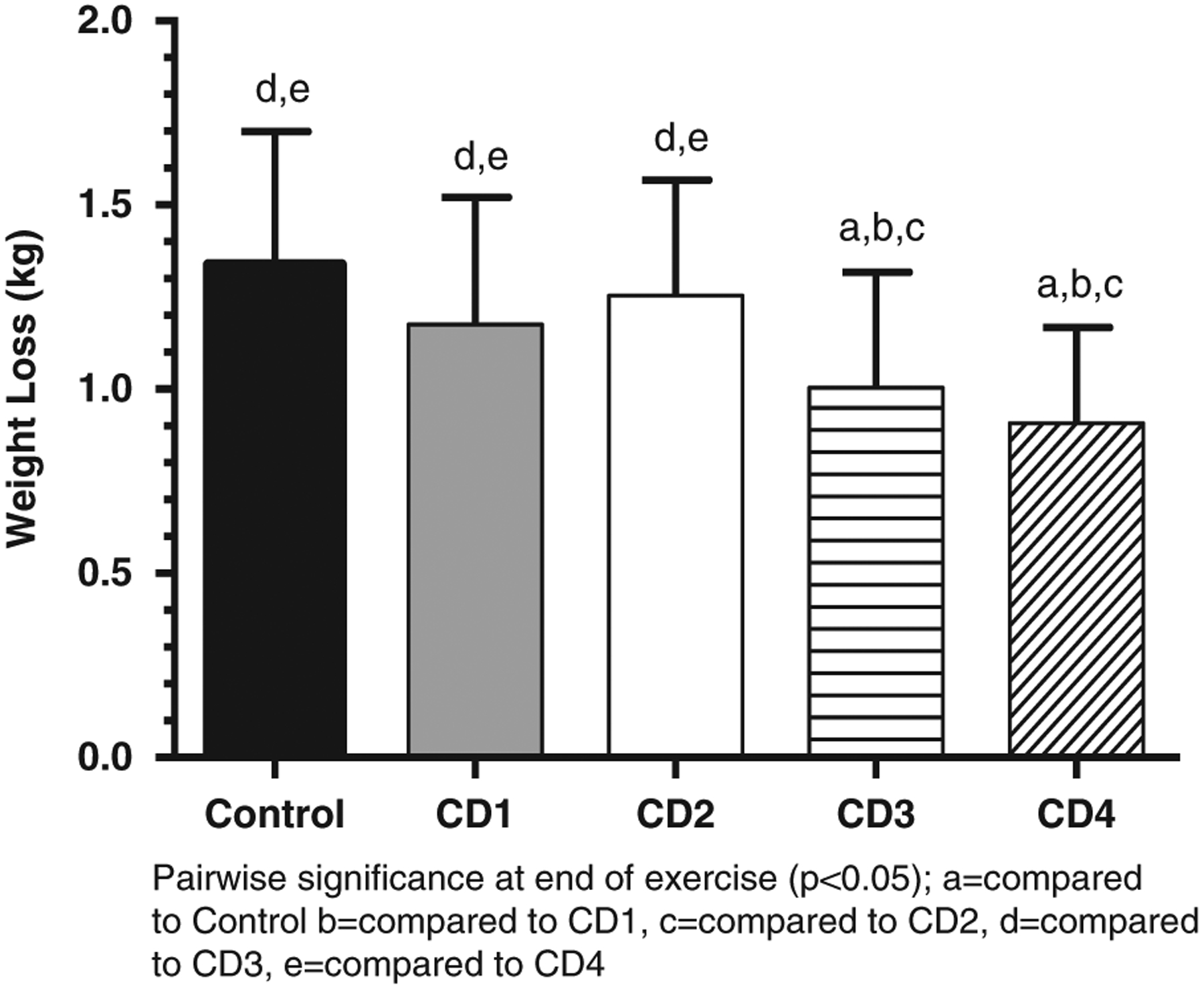
Average Weight Loss.
Abbreviation: CD, cooling device.
The results of the subjective measurement variables are shown in Table 3. Main effects of time on heat sensation, thermal comfort, RPE, breathing comfort, and wetness were found (P = 0.000 for each parameter). Main effects of condition on heat sensation, thermal comfort, RPE, breathing comfort, and wetness were found (P = 0.003, P = 0.013, P = 0.000, P = 0.018, P = 0.004, respectively). Specific pairwise comparisons are shown in Table 3.
TABLE 3.
Subjective Measurements of Comfort and Heat Stressa
| Stabilization, Average ± SD | Start of Exercise, Average ± SD | End of Exercise, Average ± SD | |
|---|---|---|---|
| Heat Sensation | |||
| Control | 0.33 ± 0.82 | 1.50 ± 0.84 | 3.83 ± 0.41e,f |
| CD1 | −0.33 ± 0.82 | 1.00 ± 0.63 | 3.50 ± 0.55e,f |
| CD2 | −0.50 ± 0.84 | 1.33 ± 0.52f | 3.50 ± 0.55e,f |
| CD3 | −0.17 ± 0.98 | −0.67 ± 2.42 | 2.67 ± 0.52b,c,d |
| CD4 | −0.67 ± 1.03 | 0.17 ± 1.47d | 2.83 ± 0.75b,c,d |
| Thermal Comfort | |||
| Control | 1.00 ± 0.00 | 1.83 ± 0.98 | 3.50 ± 0.55c,e,f |
| CD1 | 1.00 ± 0.00 | 1.33 ± 0.52 | 3.17 ± 0.4b,e,f |
| CD2 | 1.00 ± 0.00 | 1.50 ± 0.55 | 3.50 ± 0.55e,f |
| CD3 | 1.00 ± 0.00 | 1.67 ± 0.52 | 2.67 ± 0.52b,c,d |
| CD4 | 1.00 ± 0.00 | 1.50 ± 0.84 | 3.00 ± 0.63b,c,d |
| RPE | |||
| Control | 6.33 ± 0.82 | 7.33 ± 1.97 | 15.83 ± 3.60c,e,f |
| CD1 | 6.17 ± 0.41 | 6.83 ± 1.60 | 14.00 ± 2.97b,e,f |
| CD2 | 6.00 ± 0.00 | 6.83 ± 0.75 | 14.50 ± 3.39e,f |
| CD3 | 6.17 ± 0.41 | 6.67 ± 0.82 | 12.17 ± 2.32b,c,d |
| CD4 | 6.17 ± 0.41 | 7.33 ± 2.16 | 12.50 ± 2.59b,c,d |
| Breathing Comfort | |||
| Control | 1.00 ± 0.00 | 1.83 ± 1.17 | 5.17 ± 0.98c,e,f |
| CD1 | 1.00 ± 0.00 | 1.50 ± 0.55 | 4.33 ± 0.82b,e |
| CD2 | 1.00 ± 0.00 | 1.67 ± 0.52 | 4.67 ± 1.03e |
| CD3 | 1.00 ± 0.00 | 1.83 ± 0.75 | 3.33 ± 0.52b,c,d |
| CD4 | 1.00 ± 0.00 | 1.67 ± 0.52 | 3.67 ± 1.03b |
| Wetness | |||
| Control | 1.00 ± 0.00 | 1.67 ± 0.82 | 4.83 ± 0.41f |
| CD1 | 1.00 ± 0.00 | 1.83 ± 0.41 | 4.83 ± 0.41f |
| CD2 | 1.00 ± 0.00 | 1.33 ± 0.52 | 5.00 ± 0.00f |
| CD3 | 1.00 ± 0.00 | 1.33 ± 0.52 | 4.50 ± 0.84 |
| CD4 | 1.00 ± 0.00 | 1.33 ± 0.52 | 4.00 ± 0.89b,c,d |
Abbreviations: CD, cooling device; RPE, rating of perceived exertion.
Pairwise significance (P < 0.05): bcompared to control, ccompared to CD1, dcompared to CD2, ecompared to CD3, fcompared to CD4.
DISCUSSION
The physiologic stress response to light-intensity exercise in a hot and humid environment while wearing PPE similar to that used while fighting the Ebola epidemic in West Africa was attenuated by using a CD. The increase in core temperature over time was less extreme in the CD conditions, which resulted in an extended predicted time to reach Tre = 39.0°C. Also, the HR response to exercise was decreased in the CD conditions compared with the control. Lower HR during exercise is directly related to lower energy expenditure, and therefore, heat production. These results show that the ultimate goal of increased work duration in this type of environment before exhaustion will likely be achieved. This extended predicted time translates into potentially longer, higher-performance, and safer shifts for HCWs. Weight loss was lower in all CD conditions compared with the control. Because this weight loss is due to sweat, the decreased weight loss in CD conditions may assist in the maintenance of hydration during exercise and rehydration requirements following exercise. CD4 seemed to perform the best, physiologically, despite its greater weight. The physiologic response was supported by the subjective measurements as well. Compared to the control condition, the CDs helped to decrease heat sensation, decrease RPE, and increase breathing comfort at the end of exercise. These improved subjective responses to acute exercise while wearing a CD may allow the user to be more comfortable working in such extreme conditions. However, it is important for HCWs to be properly trained and knowledgeable about potential limitations when using a CD.
The CDs used in this analysis consisted of ice packs, PCM, or chilled liquid circulation. These systems each have limitations in operating time, as the materials will warm during use, causing cooling packs and ice or liquid to change phase or melt. While the use of a CD may attenuate the physiological stress response to exercise in the heat, core temperature may eventually still reach unsafe levels owing to the finite working time of the CD. Education of HCWs on the proper working time of individual CDs is important. It is evident from the Tre, HR, and time to reach Tre that each CD possesses varying working time properties that must be understood. Advantages of less energy expenditure burden with a lighter weight CD may also result in decreased attenuation of core temperature increase such as in CD1, CD2, and CD3. However, the increased weight of CD4 may be offset by greater attenuation of core temperature increases. Although it has been shown in this analysis that, generally, the ice pack–based (CD3) and circulating liquid (CD4) devices performed the best, practical limitations of these types of CDs compared to others must be considered. Both of these CDs require a frozen water source and therefore electricity to run a freezer and to charge the batteries. Electricity may not always be available in emergency response situations, which would, in turn, make these devices unusable. On the other hand, CD1 and CD2 are PCM-based devices whose packs can be activated simply by submerging the packs in cold water (45 minutes at <14°C for CD1 and <28°C until elements are solid for CD2) and would not necessarily require electricity to activate.
Along with the aforementioned various physiological-based positive and negative attributes to each CD, wearer-based perceptions must also be considered for making the best possible choice, as perceptions influence a HCW’s decision to use PPE or PPE-related garments.11 One thing that should be considered in choosing or developing an optimal CD is the material composition. Material composition is an important issue, even though the CD is worn under an impermeable garment where evaporation does not exist. Fabric composition, porosity, and fit all affect breathability, and, in turn, the body’s capacity to sweat. Polyester is known to be either moisture-wicking or moisture-trapping, both of which are less suitable for warmer temperatures. Moisture-trapping polyester can trap sweat against the skin, not allowing the moisture to evaporate properly. Moisture-wicking polyester keeps the sweat off the skin by wicking it to the surface of the garment, not allowing the body to naturally cool through sweat evaporation. On the other hand, cotton provides more breathability through porosity and contact with sweat on the skin, allowing for cooling to occur via evaporation. Interestingly, because evaporation does not exist under impermeable coveralls, all 6 subjects tested reported feeling that CD2 was “not cooling,” “ineffective,” and “warm” after only 10, 15, and 20 minutes, respectively, of wear underneath the PPE ensemble. One subject reported feeling as if “sweat was not able to escape, making it very warm, very quickly.” CD2 was the only CD made up of a polyester shell, which may have acted somewhat as a sweat-trapping device. Contrastingly, CD1, CD3, and CD4 all comprised a cotton shell and subjects provided no comments involving the perception of the other CDs in a similar manner. CD2 was the second tightest-fitting device, which also potentially contributed to the increased heat sensation and weight loss, as seen through evaporative sweat loss when compared to the other CDs.
Along with fabric considerations, ease of use and wear is not only important for wearing comfort and functionality, but also increases the intuitiveness of the device. This is essential when working in the field during an epidemic where training and education on PPE and CDs may be limited. Although CD4 was the bulkiest and most restricting on range of motion and freedom of movement owing to the heavy backpack housing the circulating water tank, it was also rated by subjects as being one of the loosest fitting (overall). This is especially important for a HCW because it could be of benefit in improved donning and doffing procedures. The CD that was rated as the most difficult to don was CD2, which included 22 PCM packs that had to be placed in the appropriate mesh pockets before donning. Subjects reported the gel-ice-based CD3 being the easiest to don, having the least interference on range of motion and freedom of movement, but also reported it to be the tightest-fitting cooling device. The tight fit of CD3 also resulted in visible skin discoloration from the ice packs closely contacting the skin (separated by a layer of standard medical scrubs) on one subject that may have indicated dermal vascular effects. However, no negative comments were made on this finding by any of the 6 subjects. The different properties of the CDs make it clear that no single CD should be used in every situation. An educated decision about which type to use should be driven by physiological and practical implications.
The use of a CD decreases the thermoregulatory and cardiovascular strain on the wearer during low-work-rate exercise in a hot and humid environment. Data from the current study on the use of a CD during exercise in a hot environment correlate with previous such studies that have shown a moderation of the increase in core temperature and improved endurance performance.12–14 Additionally, it has been shown that HR response and cardiovascular strain are increased during exercise in a hot and humid environment and that this is attenuated with the use of a CD.13–16 Weight loss has also been shown to be reduced when using a CD during exercise in the heat.16,17 Previously, PCM CDs have been reported to offer a cooling effect that is “quick and strong,” mimicking the results seen in this study.18,19
The strengths of the study include the design, which allowed for comparison of several of the readily available types of CDs which offer a variety of costs and benefits. PCM devices, ice pack–based devices, and a circulating liquid device were all evaluated, resulting in data that can easily be used for comparison purposes. Human subject testing, rather than simulated measurements, enhanced the reliability of the data.
Study limitations included the small number of subjects tested (n = 6); however, all subjects were experienced PPE users, which increased the consistency of the data. Owing to the strenuous nature of the environmental conditions and exercise-induced heat stress, the study utilized fit and healthy men who may not accurately mirror the fitness level and gender of typical HCWs. Furthermore, the exercise trials involved continuous activity (treadmill walking) that may not accurately reflect the typically intermittent activities and related energy expenditures of HCWs. The exercise protocol was also not repeated multiple times throughout 1 day on each subject such as may be seen in an actual working environment. The study also consisted of males only, even though the gender distribution of the health workforce shows that 74.2% of HCWs are female.20
Further investigation of the physiological impact of circulating-water CDs is warranted, including research that further examines the physiological impact of these CDs in active precooling studies with the same PPE ensemble described previously. Additional research regarding possible postural and ergonomic burdens on the user would be useful to more holistically assess the practical implementation of CDs in the workforce.
CONCLUSION
Compared to the control condition, all CDs attenuated the increase in core temperature, lowered the HR response to exercise, and decreased weight loss following a 60-minute exercise bout in a hot and humid environment. Three of the 5 measured subjective responses (heat sensation, RPE, and breathing comfort) were improved at the end of exercise with the addition of the CD. The positive effects, across all CDs, were of different magnitudes for each device, and therefore better education and training on expectations of protection for individual devices should be a prelude to their use. To ensure the most effective delivery of health care to infectious diseases patients, in hot and humid environments and other work requiring PPE use in extreme environments, CDs can be advantageous in decreasing the negative physiological and subjective responses to heat stress, thus extending safe working time.
Acknowledgments
The authors are sincerely grateful for the technical and experimental support in conducting the present study from NIOSH’s Emergency Preparedness and Response Office (Chad Dowell and Lisa Delaney), the CDC Foundation, Susan Lovasic (DuPont), and the in-depth review and helpful comments from Randy Sakowitz and Douglas Frost. The US Agency for International Development (USAID) is thanked for raising awareness of the need for this research and their role in assisting in the selection of the cooling devices tested.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health. Mention of company names or products does not constitute endorsement by NIOSH.
REFERENCES
- 1.de Almeida R, Veiga MM, de Castro MDF, et al. Thermal comfort and personal protective equipment (PPE). Work. 2011;41:4979–4982. [DOI] [PubMed] [Google Scholar]
- 2.Havenith G, den Hartog E, Martini S. Heat stress in chemical protective clothing: porosity and vapour resistance. Ergonomics. 2011;54(5): 497–507. 10.1080/00140139.2011.558638. [DOI] [PubMed] [Google Scholar]
- 3.Guidance on Personal Protective Equipment (PPE) To Be Used By Healthcare Workers during Management of Patients with Confirmed Ebola or Persons under Investigation (PUIs) for Ebola Who Are Clinically Unstable or Have Bleeding, Vomiting, or Diarrhea in US Hospitals, Including Procedures for Donning and Doffing PPE. Centers for Disease Control and Prevention website. http://www.cdc.gov/vhf/ebola/healthcareus/ppe/guidance.html. Last updated August 27, 2015. Accessed [Google Scholar]
- 4.Chertow DS, Kleine C, Edwards JK, et al. Ebola virus disease in West Africa—clinical manifestations and management. N Engl J Med. 2014;371(22):2054–2057. 10.1056/NEJMp1413084. [DOI] [PubMed] [Google Scholar]
- 5.Wolz A Face to face with Ebola—an emergency care center in Sierra Leone. N Engl J Med. 2014;371(12):1081–1083. 10.1056/NEJMp1410179. [DOI] [PubMed] [Google Scholar]
- 6.Coca A, DiLeo T, Kim JH, et al. Baseline evaluation with a sweating thermal manikin of personal protective ensembles recommended for use in West Africa. Disaster Med Public Health Prep. 2015;9(05):536–542. 10.1017/dmp.2015.97. [DOI] [PubMed] [Google Scholar]
- 7.International Organization for Standardisation. 10551, Ergonomics of the Thermal Environment–Assessment of the Influence of the Thermal Environment Using Subjective Judgment Scales. Geneva: International Organization for Standardisation; 1995. [Google Scholar]
- 8.International Organization for Standardisation. 7730, Ergonomics of the Thermal Environment–Analytical Determination and Interpretation of Thermal Comfort Using Calculation of the PMV and PPD Indices and Local Thermal Comfort Criteria. Geneva: International Organization for Standardisation; 2005. [Google Scholar]
- 9.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. 10.1249/00005768-198205000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Hancock P, Vasmatzidis I. Effects of heat stress on cognitive performance: the current state of knowledge. Int J Hyperthermia. 2003;19(3):355–372. 10.1080/0265673021000054630. [DOI] [PubMed] [Google Scholar]
- 11.Gralton J, Rawlinson WD, McLaws ML. Health care workers’ perceptions predicts uptake of personal protective equipment. Am J Infect Control. 2013;41(1):2–7. 10.1016/j.ajic.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 12.Chou C, Tochihara Y, Kim T. Physiological and subjective responses to cooling devices on firefighting protective clothing. Eur J Appl Physiol. 2008;104(2):369–374. 10.1007/s00421-007-0665-7. [DOI] [PubMed] [Google Scholar]
- 13.Hasegawa H, Takatori T, Komura T, et al. Wearing a cooling jacket during exercise reduces thermal strain and improves endurance exercise performance in a warm environment. J Strength Cond Res. 2005; 19(1):122–128. [DOI] [PubMed] [Google Scholar]
- 14.Kenny GP, Schissler AR, Stapleton J, et al. Ice cooling vest on tolerance for exercise under uncompensable heat stress. J Occup Environ Hyg. 2011;8(8):484–491. 10.1080/15459624.2011.596043. [DOI] [PubMed] [Google Scholar]
- 15.Lefferts WK, Heffernan KS, Hultquist EM, et al. Vascular and central hemodynamic changes following exercise-induced heat stress. Vasc Med. 2015;20(3):222–229. 10.1177/1358863X14566430. [DOI] [PubMed] [Google Scholar]
- 16.Smolander J, Kuklane K, Gavhed D, et al. Effectiveness of a light-weight ice-vest for body cooling while wearing fire fighter’s protective clothing in the heat. Int J Occup Saf Ergon. 2004;10(2):111–117. 10.1080/10803548.2004.11076599. [DOI] [PubMed] [Google Scholar]
- 17.Fehling PC, Haller JM, Lefferts WK, et al. Effect of exercise, heat stress and dehydration on myocardial performance. Occup Med. 2015; 65(4):317–323. 10.1093/occmed/kqv015. [DOI] [PubMed] [Google Scholar]
- 18.Gao C, Kuklane K, Holmér I. Cooling vests with phase change material packs: the effects of temperature gradient, mass and covering area. Ergonomics. 2010;53(5):716–723. 10.1080/00140130903581649. [DOI] [PubMed] [Google Scholar]
- 19.Holmer I Protective clothing in hot environments. Ind Health. 2006; 44(3):404–413. 10.2486/indhealth.44.404. [DOI] [PubMed] [Google Scholar]
- 20.US Bureau of Labor Statistics. Women in the Labor Force: a Databook. https://www.bls.gov/opub/reports/womens-databook/archive/women-in-the-labor-force-a-databook-2015.pdf. Published December 2015. Accessed February 13, 2017.


