Abstract
Hypertension is a global public health problem which affects the physical and mental health of individuals. The management of hypertension is a long‐term process that requires the cooperation of both doctors and patients, and the blood pressure variability is closely related to the clinical prognosis. In recent years, the development of telemedicine has promoted better blood pressure monitoring and management for patients, as well as better medical intervention and health education for patients by medical staff. This article provides a review of remote blood pressure monitoring and management.
Keywords: blood pressure, home blood pressure monitoring, hypertension, telemedicine, remote blood pressure monitoring
1. INTRODUCTION
Hypertension is the most common chronic disease and a major risk factor for cardiovascular disease, stroke, kidney failure, and other diseases. It has a serious impact on global public health. In 2019, the number of people with hypertension worldwide exceeded 1.2 billion. 1 According to a national hypertension survey of 451 755 adults in China from 2012 to 2015, the prevalence, awareness, treatment, and control rates of hypertension were 23.2%, 46.9%, 40.7%, and 15.3%, respectively. 2 One study reported an insignificant decrease in the average blood pressure of hypertensive patients worldwide during 1975–2015. 3 The low control rates of hypertension may be associated with poor drug adherence, autonomic dysfunction, excess sympathetic activity, excess dietary sodium, fluctuations in body weight, atherosclerosis due to aging, sleep disorders, and nonprescription drugs (such as Nonsteroidal Antiinflammatory Drugs (NSAIDs) and some cold remedies). 4 Currently, blood pressure management mostly includes pharmacological treatment and lifestyle interventions. 5 Blood pressure monitoring includes monitoring office blood pressure, ambulatory blood pressure, and home blood pressure, among which home blood pressure monitoring is crucial for the long‐term management of hypertension. 6 , 7 , 8 Home blood pressure monitoring can be used to detect white coat hypertension and masked hypertension as well as assess baseline blood pressure levels and increase patients’ self‐management ability and compliance with other interventions. In recent years, several studies have been conducted on home blood pressure monitoring methods, among which blood pressure monitoring and management via remote electronic devices are popular. 9 , 10
2. BLOOD PRESSURE MONITORING METHODS AND DEVICES
With the rapid development of telecommunication technology, internet technology has gradually been applied to various fields of social work with the advantages of being timely, efficient, fast, and easy, and it has become an increasingly indispensable part of the tedious workflow in various fields. Chronic diseases such as hypertension can be managed systematically, meticulously, and effectively and its management can be standardized with the support of internet technology, involving several chronic disease management aspects such as remote online consultation, remote blood pressure monitoring, remote blood pressure assessment, remote medication guidance, remote dietary guidance, remote health education, and prognosis follow‐up. Email, smartphone applications, and other means can be used to provide information regarding the patient's hypertension condition to the doctor. Thus, the analysis of the effect of antihypertensive drug treatment and the patient's lifestyle and other conditions can be individualized, and patients can receive timely treatment advice and health education via the corresponding platform. The use of internet technology for the monitoring and management of hypertension has many advantages; however, there are also some limitations (Table 1).
TABLE 1.
Advantages and disadvantages of remote blood pressure monitoring
| Advantages | Disadvantages |
|---|---|
| • Detection of white‐coat and masked hypertension | • Higher cost than office blood pressure and ambulatory blood pressure |
| • Measurement in daily activities | • User training required |
| • Assessment of daytime blood pressure | • Nighttime blood pressure assessment is less effective |
| • Assessing the effects of anti‐hypertensive drugs | • Poor morning blood pressure surge assessment |
| • Facilitates long‐term follow‐up of hypertension | • Assessment of duration of drug action is not as good as ambulatory blood pressure |
| • Improve patient compliance | • May cause anxiety and too frequent monitoring |
| • Improve hypertension control rates | • Some patients adjust their own medications based on blood pressure readings |
| • Predict cardiovascular events | • Some patients are measured only while sitting at home and do not reflect daily activities |
| • Cost‐effectiveness | • Inequity due to the costs of technologies |
| • Better for long‐term BP control | • The digital divide |
Blood pressure monitoring methods can be divided into two types: invasive monitoring and noninvasive monitoring. Invasive monitoring involves placing the pressure sensor into the arterial blood vessels to detect pressure changes. This method can directly and continuously measure the blood pressure value in the arteries, and the measured data are also the most accurate. However, because of the invasive nature, it is only indicated for patients undergoing major surgery.
In contrast, noninvasive monitoring methods include auscultation andoscillometric methods, oscillometric measurement at the wrist, the applanation tonometry method, and photoplethysmography as well as measuring the pulse transit time. 11 According to these blood pressure monitoring methods, the current remote blood pressure monitoring devices mainly include upper‐arm electronic automatic devices (wired or wireless), smartphone applications with external wireless blood pressure monitors, smartphones acting as sleeveless blood pressure monitors, smart watches, smart bracelets, and finger photoplethysmography. Data can be transferred via smartphones, home centers, smart boxes, tablets, desktop computers, laptops, etc. 12 The blood pressure results can be sent directly to mobile terminal devices or computer storage centers, where the monitoring data can be observed and evaluated in real‐time; simultaneously, remote interventions can be provided to patients, including medication adjustment and health guidance.
Patients transmit their blood pressure monitoring values to the management platform using blood pressure monitors with data transmission function and cell phone APPs, which are recorded through the network system. Clinical pharmacists and doctors use the data summarized by the system and the medical visit records to instruct patients to perform blood pressure monitoring or enter the treatment plan adjustment phase through various communication methods such as SMS, Email, and telephone. In addition, standard workflows for patient enrollment registration, drug titration, and maintenance treatment can be developed, and tasks can be automatically assigned by the system. For example, for patients who meet the enrollment criteria, the system reminds them to take sufficient blood pressure measurements and then arranges for pharmacists and doctors to guide them to enter the titration phase, and then makes treatment decisions based on the patient's medical history, blood pressure measurements, and clinical guidelines. The system will automatically remind the patient to perform regular monitoring during the maintenance phase of drug therapy and arrange for the patient to continue the original treatment regimen or titrate again based on the monitoring results (Figure 1).
FIGURE 1.

Workflow of remote blood pressure monitoring
3. EFFECTIVENESS OF REMOTE BLOOD PRESSURE MONITORING
In recent years, several studies have demonstrated the feasibility and effectiveness of remote blood pressure monitoring. The TASMINH2 study showed that after 12 months of follow‐up, blood pressure decreased in both the non‐self‐administered and self‐administered groups, with an average decrease of 12.8 mmHg systolic and 3.4 mmHg diastolic in the non‐self‐administered group and 18.3 mmHg systolic and 7.7 mmHg diastolic in the self‐administered group. 13 Self‐management is the ability to manage psychosocial and lifestyle factors in addition to symptom monitoring, blood pressure monitoring, and medication adherence. 14 Recently, several studies have demonstrated that remote monitoring can better enhance self‐management in patients with hypertension. 15 , 16 , 17 Lu and colleagues recruited 432 patients for remote blood pressure monitoring and management, worked with public health nurses in public health care centers, and eventually, 408 patients completed data collection. Their study showed a mean reduction in systolic blood pressure of 22.1 mmHg in patients after 1 year. 18 In addition, a recent meta‐analysis that included 18 articles on remote blood pressure monitoring (all randomized controlled trials) showed that the weighted mean blood pressure decreased by 7.07 points (SBP) and 5.07 points (DBP) in the intervention group compared with 3.11 points (SBP) and 3.13 points (DBP) in the control group. 19 , 20
A recent study found that remote blood pressure monitoring and management significantly improved blood pressure control in patients with acute ischemic stroke, whereas intensive blood pressure management reduced stroke recurrence by 22%. 20 , 21
Some researchers have used telemetric blood pressure monitoring for the monitoring of blood pressure and screening for complications during pregnancy. Their results suggest that telemetric blood pressure monitoring may help in the management and improvement of hypertension during pregnancy, but most of the evidence is limited to assessing the feasibility of the trial and maternal satisfaction. 22 , 23 Hoppe and colleagues showed that remote blood pressure monitoring and management reduced readmission rates at six weeks postpartum in patients with hypertension during pregnancy. 24 , 25 In contrast, the results of the BUMP 1 Randomized Clinical Trial, published in 2022, showed that remote blood pressure self‐monitoring did not have a more significant detection rate compared with usual care in pregnant women at a higher risk of pre‐eclampsia. 26 Results from the BUMP 2 Randomized Clinical Trial in the same year showed that in pregnant women with chronic or gestational hypertension, remote monitoring of blood pressure did not significantly improve blood pressure control rates compared with usual care. 27 The feasibility and safety of remote blood pressure monitoring and management were both confirmed in the above clinical trials, but its effectiveness needs to be further evaluated in additional studies.
Hypertension is a chronic disease that accompanies patients throughout their lives. Our goal is long‐term management of blood pressure and improvement of prognosis. In the current studies, the follow‐up time was mostly within 1 year, and we expect more studies to prove the effectiveness and safety of remote blood pressure in long‐term management.
4. BLOOD PRESSURE AND TARGET ORGAN DAMAGE
Hypertension can damage target organs, including the heart, brain, and kidneys, resulting in acute and chronic cardiovascular diseases, stroke, renal insufficiency, and even renal failure. This can seriously affect the health and quality of life of patients, of which blood pressure variability (BPV) is a crucial assessment indicator. The concept of BPV first appeared in the 18th century, and it refers to the fluctuation of blood pressure over time. Many studies have shown that BPV is inextricably linked to blood pressure and can lead to cardiovascular diseases, such as coronary artery disease and stroke, independently of blood pressure. With the discovery of the close correlation between BPV and clinical prognosis, hypertension treatment has changed from lowering mean blood pressure to lowering BPV, which can help protect target organs, improving patient prognosis. 28 , 29 , 30 According to the time‐domain index, BPV is divided into ultra‐short‐time variability (variability during the cardiac cycle, also called immediate variability), short‐time variability (BPV within 24 h), medium‐time variability (BPV over several consecutive days or weeks), and long‐time variability (BPV over several months and during a long‐term follow‐up). According to the frequency‐domain index, BPV is divided into high‐frequency variability (.15–.30 Hz), low‐frequency variability (.04–.15 Hz), and very low‐frequency variation (<.04 Hz). BPV can be divided into systolic, diastolic, and pulse pressure variability according to blood pressure components. Furthermore, BPV can be divided into physiological, pathological, and drug‐induced variability according to the cause of occurrence. Physiologic variation is blood pressure variation in normal people, usually manifested as dipper‐pattern blood pressure and morning blood pressure surge. Dipper‐pattern blood pressure is a certain circadian rhythm, that is, 10%–20% decrease in blood pressure at night than at daytime. A morning blood pressure surge is when the body changes from sleep to wakefulness and starts routine activities, the blood pressure will rise rapidly from a relatively low level to a relatively high level to meet bodily needs. Such regular changes in blood pressure are important for protecting target organs, such as the heart, brain, and kidneys. Pathological blood pressure variation is an increase in BPV, which can occur when arterial elasticity is reduced, blood volume is increased, and neuroendocrine regulation is impaired. The main types are non‐dipper pattern (nighttime blood pressure is <10% lower than daytime blood pressure), extreme‐dipper pattern (nighttime blood pressure is >20% lower than daytime blood pressure), reverse‐dipper pattern (nighttime blood pressure higher than daytime blood pressure), and morning blood pressure surge. The main indicators for assessing BPV are standard deviation, coefficient of variation, variation independent of mean, and average real variability. Exercise, psychological and mental stress, smoking, and alcohol consumption can cause rapid changes in blood pressure (Figure 2). 11 Furthermore, morning blood pressure surge is associated with various forms of target organ damage, including an increased risk of stroke and cerebral hemorrhage. 31 , 32 , 33 , 34 , 35 , 36 , 37 In contrast, reverse‐dipper and non‐dipper patterns increase the risk of target organ damage and cardiovascular events. 38 , 39 , 40 , 41 , 42 Thus, the accurate detection of factors causing rapid changes in blood pressure in daily life can lead to necessary interventions to reduce cardiovascular risk and adverse cardiovascular and cerebrovascular events. With a remote blood‐pressure monitoring system, more blood pressure data can be collected from patients to assess their BPV, predict the risk of cardiovascular and cerebrovascular diseases, guide medication, and improve lifestyle to better control blood pressure as well as to improve prognosis and the quality of life of patients.
FIGURE 2.
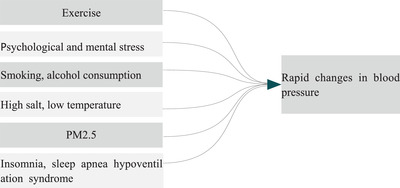
Common factors that cause rapid changes in blood pressure
5. CONCLUSIONS
The economic burden on individuals and countries has increased considerably because of the persistently high prevalence of hypertension, and without new surveillance and management methods, this trend will not decline. Simultaneously, the coronavirus disease 2019 (COVID‐19) outbreak in recent years has severely increased the global economic burden, and as the pandemic is still recurring, accessing care is difficult for many patients with chronic diseases. Cardiovascular diseases, especially hypertension, are a common co‐morbidity in COVID‐19, increasing the risk of adverse outcomes. 43 Telemedicine can potentially improve this situation. East Japan used a remote blood pressure monitoring system in one affected town after a major earthquake, effectively controlling home blood pressure in hypertensive patients and minimizing seasonal blood pressure variations over a period following the disaster. 44 In addition, remote blood pressure monitoring can also help better control blood pressure in rural and low‐income population. 45
Remote blood‐pressure monitoring can improve the self‐management ability and quality of life of hypertensive patients, reducing treatment and care costs. Such a system is especially suitable for patient groups where outpatient follow‐up is difficult or where follow‐up awareness is less and treatment compliance is poor. In addition to blood pressure monitoring, such a remote monitoring system can also monitor vital signs, including temperature, electrocardiogram, and blood sugar levels, benefitting the management of more diseases. However, the development of telemedicine also has many problems: (1) The imperfect blood pressure monitoring equipment and the purchase and maintenance of infrastructure, including computer hardware and related software; secondly, the security and privacy of data transmission, as well as the cost of related personnel; (2) The poor level of informatics skills of doctors or patients is an important barrier to telemedicine, especially for the elderly, and some people with poor health and cognitive impairment, or limited digital literacy; (3) Hypertension is a lifelong disease, and long‐term management of blood pressure is crucial. Some patients who lack motivation and lack understanding of the clinical use of telemedicine are difficult to adhere to remote blood pressure monitoring and self‐management. 46 , 47
We believe that through continuous improvement and perfection, telemedicine will bring great benefits to mankind.
AUTHOR CONTRIBUTIONS
Yan Li, Yi Jiang, and Yuping Tang: Conception and design; Data analysis and interpretation; Manuscript writing; and Final approval of manuscript.
CONFLICT OF INTEREST
We declared no conflict of interest.
ACKNOWLEDGMENTS
The authors would like to thank all the reviewers who participated in the review. The funding is provided by the Joint Medical Research Project of Chongqing Municipal Science and the Technology Bureau and Health Commission (2021MSXM159). Scientific Research Project of Chongqing Municipal Sports Bureau(C202108).
Li Y, Jiang Y, Tang Y. Is remote blood pressure monitoring and management a better approach for patients with hypertension? A narrative review. J Clin Hypertens. 2023;25:121–126. 10.1111/jch.14624
Contributor Information
Yi Jiang, Email: jiangyi@cqu.edu.cn.
Yuping Tang, Email: 542004538@qq.com.
REFERENCES
- 1. Bin Z, Rodrigo MC, Goodarz D, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population‐representative studies with 104 million participants. Lancet. 2021;398(10304):957‐980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang ZW, Chen Z, Zhang LF, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018;137(22):2344‐2356. [DOI] [PubMed] [Google Scholar]
- 3. Bin Z, James B, Mariachiara DC, et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population‐based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Michael AW. Blood pressure variability and cardiovascular prognosis: implications for clinical practice. Eur Heart J. 2017;38(37):2823‐2826. [DOI] [PubMed] [Google Scholar]
- 5. Unger T, Borghi C, Charchar F, et al. 2020 International society of hypertension global hypertension Practice Guidelines. Hypertension. 2020;75(6):1334‐1357. [DOI] [PubMed] [Google Scholar]
- 6. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American college of Cardiology/American heart association task force on clinical practice guidelines. Circulation. 2018;138(17):e426‐e483. [DOI] [PubMed] [Google Scholar]
- 7. Parati G, Stergiou GS, Asmar R, et al. European society of hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens. 2010;24:779‐785. [DOI] [PubMed] [Google Scholar]
- 8. Williams B, Mancia G, Spiering W, et al. 2018 Practice guidelines for the management of arterial hypertension of the european society of hypertension and the european society of cardiology: ESH/ESC task force for the management of arterial hypertension. J Hypertens. 2018;36:2284‐2309. [DOI] [PubMed] [Google Scholar]
- 9. Brown CN. A better way to evaluate remote monitoring programs in chronic disease care: receiver operating characteristic analysis. Telemed J E Healt. 2014;20(12):1143‐1149. [DOI] [PubMed] [Google Scholar]
- 10. Stupplebeen DA, Pirkle CM, Sentell TL, et al. Self‐measured blood pressure monitoring: program planning, implementation, and lessons learned from 5 federally qualified health centers in Hawai'i. Prev Chronic Dis. 2020;17:E47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kario K. Management of hypertension in the digital era: small wearable monitoring devices for remote blood pressure monitoring. Hypertension. 2020;76(3):640‐650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Omboni S. Connected health in hypertension management. Front Cardiovasc Med. 2019;6:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bray EP, Jones MI, Banting M, et al. Performance and persistence of a blood pressure self‐management intervention: telemonitoring and self‐management in hypertension (TASMINH2) trial. J Hum Hypertens. 2015;29(7):436‐441. [DOI] [PubMed] [Google Scholar]
- 14. Bodenheimer T, Lorig K, Holman H, et al. Patient self‐management of chronic disease in primary care. JAMA. 2002;288(19):2469‐2475. [DOI] [PubMed] [Google Scholar]
- 15. McKoy J, Fitzner K, Margetts M, et al. Are telehealth technologies for hypertension are and self‐management effective or simply risky and costly? Popul Health Manag. 2015;18(3):192‐202. [DOI] [PubMed] [Google Scholar]
- 16. Park MJ, Kim HS, Kim KS. Cellular phone and internet‐based individual intervention on blood pressure and obesity in obese patients with hypertension. Int J Med Inform. 2009;78(10):704‐710. [DOI] [PubMed] [Google Scholar]
- 17. Senesael E, Borgermans L, Van De Vijver E, et al. Effectiveness of a quality improvement intervention targeting cardiovascular risk factors: are patients responsive to information and encouragement by mail or post? Vasc Health Risk Manag. 2013;9:13‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lu JF, Chen CM, Hsu CY. Effect of home telehealth care on blood pressure control: a public healthcare centre model. J Telemed Telecare. 2019;25(1):35‐45. [DOI] [PubMed] [Google Scholar]
- 19. Kalagara R, Chennareddy S, Scaggiante J, et al. Blood pressure management through application‐based telehealth platforms: a systematic review and meta‐analysis. J Hypertens. 2022;40(7):1249‐1256. [DOI] [PubMed] [Google Scholar]
- 20. Kitagawa K, Yamamoto Y, Arima H, et al. Effect of standard vs intensive blood pressure control on the risk of recurrent stroke. JAMA Neurol. 2019;76(11):1309‐1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kim BJ, Park JM, Park TH, et al. Remote blood pressure monitoring and behavioral intensification for stroke: a randomized controlled feasibility trial. PLoS One. 2020;15(3):e0229483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rivera RO, Olmo A, Muñoz R, et al. Mobile health solutions for hypertensive disorders in pregnancy: scoping literature review. JMIR mHealth and uHealth. 2018;6(5):e130‐e130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pealing LM, Tucker KL, Mackillop LH, et al. A randomised controlled trial of blood pressure self‐monitoring in the management of hypertensive pregnancy. OPTIMUM‐BP: a feasibility trial. Pregnancy Hypertens. 2019;18:141‐149. [DOI] [PubMed] [Google Scholar]
- 24. Hoppe KK, Thomas N, Zernick M, et al. Telehealth with remote blood pressure monitoring compared with standard care for postpartum hypertension. AM J Obstet Gynecol. 2020;223(4):585‐588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hoppe KK, Williams M, Thomas N, et al. Telehealth with remote blood pressure monitoring for postpartum hypertension: a prospective single‐cohort feasibility study. Pregnancy Hypertens. 2019;15:171‐176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tucker KL, Mort S, Yu LM, et al. Effect of self‐monitoring of blood pressure on diagnosis of hypertension during higher‐risk pregnancy:the BUMP 1 randomized clinical trial. JAMA. 2022;327(17):1656‐1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chappell LC, Tucker KL, Galal U, et al. Effect of self‐monitoring of blood pressure on blood pressure control in pregnant individuals with chronic or gestational hypertension:the BUMP 2 randomized clinical trial. JAMA. 2022;327(17):1666‐1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stevens SL, Wood S, Koshiaris C, et al. Blood pressure variability and cardiovascular disease: systematic review and meta‐analysis. BMJ. 2016;354:i4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Asayama K, Schutte R, Li Y, et al. Blood pressure variability in risk stratification: what does it add? Clin Exp Pharmacol Physiol. 2014;41(1):1‐8. [DOI] [PubMed] [Google Scholar]
- 30. Parati G, Stergiou GS, Dolan E, et al. Blood pressure variability: clinical relevance and application. J Clin Hypertens. 2018;20(7):1133‐1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yano Y, Hoshide S, Inokuchi T, et al. Association between morning blood pressure surge and cardiovascular remodeling in treated elderly hypertensive subjects. AM J Hypertens. 2009;22(11):1177‐1182. [DOI] [PubMed] [Google Scholar]
- 32. Shimizu M, Ishikawa J, Yano Y, et al. The relationship between the morning blood pressure surge and low‐grade inflammation on silent cerebral infarct and clinical stroke events. Atherosclerosis. 2011;219(1):316‐321. [DOI] [PubMed] [Google Scholar]
- 33. Kuwajima I, Mitani K, Miyao M, et al. Cardiac implications of the morning surge in blood pressure in elderly hypertensive patients: relation to arising time. AM J Hypertens. 1995;8(1):29‐33. [DOI] [PubMed] [Google Scholar]
- 34. Chen CT, Li Y, Zhang J, et al. Association between ambulatory systolic blood pressure during the day and asymptomatic intracranial arterial stenosis. Hypertension. 2014;63(1):61‐67. [DOI] [PubMed] [Google Scholar]
- 35. Kaneda R, Kario K, Hoshide S, et al. Morning blood pressure hyper‐reactivity is an independent predictor for hypertensive cardiac hypertrophy in a community‐dwelling population. AM J Hypertens. 2005;18(12):1528‐1533. [DOI] [PubMed] [Google Scholar]
- 36. Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives. Circulation. 2003;107(10):1401‐1406. [DOI] [PubMed] [Google Scholar]
- 37. Metoki H, Ohkubo T, Kikuya M, et al. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the ohasama study. Hypertension. 2006;47(2):149‐154. [DOI] [PubMed] [Google Scholar]
- 38. Acciaroli G, Facchinetti A, Pillonetto G, Sparacino G. Non‐invasive continuous‐time blood pressure estimation from a single channel PPG signal using regularized ARX models. Conf Proc IEEE Eng Med Biol Soc. 2018:3630‐3633. [DOI] [PubMed] [Google Scholar]
- 39. Komori T, Eguchi K, Saito T, et al. Riser pattern is a novel predictor of adverse events in heart failure patients with preserved ejection fraction. Circ J. 2017;81(2):220‐226. [DOI] [PubMed] [Google Scholar]
- 40. Komori T, Eguchi K, Saito T, et al. Riser pattern: another determinant of heart failure with preserved ejection fraction. J Clin Hypertens. 2016;18(10):994‐999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hoshide S. Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community‐dwelling normotensives. AM J Hypertens. 2003;16(6):434‐438. [DOI] [PubMed] [Google Scholar]
- 42. Kario K. Nocturnal hypertension: new technology and evidence. Hypertension. 2018;71(6):997‐1009. [DOI] [PubMed] [Google Scholar]
- 43. Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with COVID‐19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Nishizawa M, Hoshide S, Okawara Y, et al. Strict blood pressure control achieved using an ICT‐based home blood pressure monitoring system in a catastrophically damaged area after a disaster. J Clin Hypertens. 2017;19(1):26‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Clark RD, Woods J, Zhang YX, et al. Home blood pressure telemonitoring with remote hypertension management in a rural and low‐income population. Hypertension. 2021;78(6):1927‐1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Khan NA, Stergiou GS, Omboni S, et al. Virtual management of hypertension: lessons from the COVID‐19 pandemic‐International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. J Hypertens. 2022;40(8):1435‐1448. [DOI] [PubMed] [Google Scholar]
- 47. Omboni S, McManus RJ, Bosworth HB, et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension: an international expert position paper. Hypertension. 2020;76(5):1368‐1383. [DOI] [PubMed] [Google Scholar]


