Abstract
Introduction:
Diastasis recti abdominis usually occurs during pregnancy and delivery in young women with no surgical history, and can induce a severely negative body image, urogynecological symptoms, and musculoskeletal pain. However, the optimal surgical procedure for diastasis recti abdominis is undetermined, and minimally invasive surgery has not been adopted. Additionally, open repair causes scarring that is unlikely to improve negative body image and may even worsen it. We present a case of diastasis recti abdominis surgically treated using an extended-view totally extraperitoneal approach, Rives-Stoppa technique, and transversus abdominis release procedure.
Case Description:
The patient was a 29-year-old woman who delivered transvaginally two weeks before presenting with bulging of the abdominal wall. Computed tomography revealed separation of the rectus. A three-month course of conservative therapy comprising exercises to strengthen the transversus abdominis was ineffective, and the patient had newly developed abdominal pain. Therefore, we performed surgical repair using the Rives-Stoppa technique and transversus abdominis release via the extended-view totally extraperitoneal approach. The postoperative course was uneventful, with no recurrence. This procedure may be superior to other methods in terms of cosmetic appearance, preventing infection, bowel adhesion, and recurrence.
Discussion:
In the case study, the Rives-Stoppa technique and transversus abdominis release via the extended-view totally extraperitoneal approach achieved a good therapeutic outcome for diastasis recti abdominis.
Keywords: Diastasis recti abdominis, Minimally invasive surgery, Surgical retrorectus mesh
BACKGROUND
Diastasis recti abdominis (DRA) is defined as separation of the two rectus abdominis muscles along the linea alba. DRA usually occurs during pregnancy and delivery in young women with no surgical history. There is no standard procedure to treat DRA. Even with recent advances in minimally invasive surgery, laparoscopic procedures have seldom been used to treat DRA. However, laparoscopic treatment is warranted for DRA, especially with respect to cosmetic outcomes. Palanivelu et al. reported laparoscopic plication and underlay mesh reinforcement for DRA;1 however, as with ventral hernia repair, retrorectus mesh placement is thought to produce better outcomes. Therefore, we treated DRA using an extended-view totally extraperitoneal approach (eTEP), the Rives-Stoppa technique, and the transversus abdominis release (TAR) procedure in combination, as previously described in ventral hernia repair.2 This method has the advantages of laparoscopy, including a good cosmetic outcome, lower infection risk, and shorter hospital stay; it also has the advantages of the ventral hernia repair method, realizing a wide dissection space for repair and mesh placement without causing bowel adhesions that may occur with underlay mesh, which is commonly used in laparoscopic repair.
CASE PRESENTATION
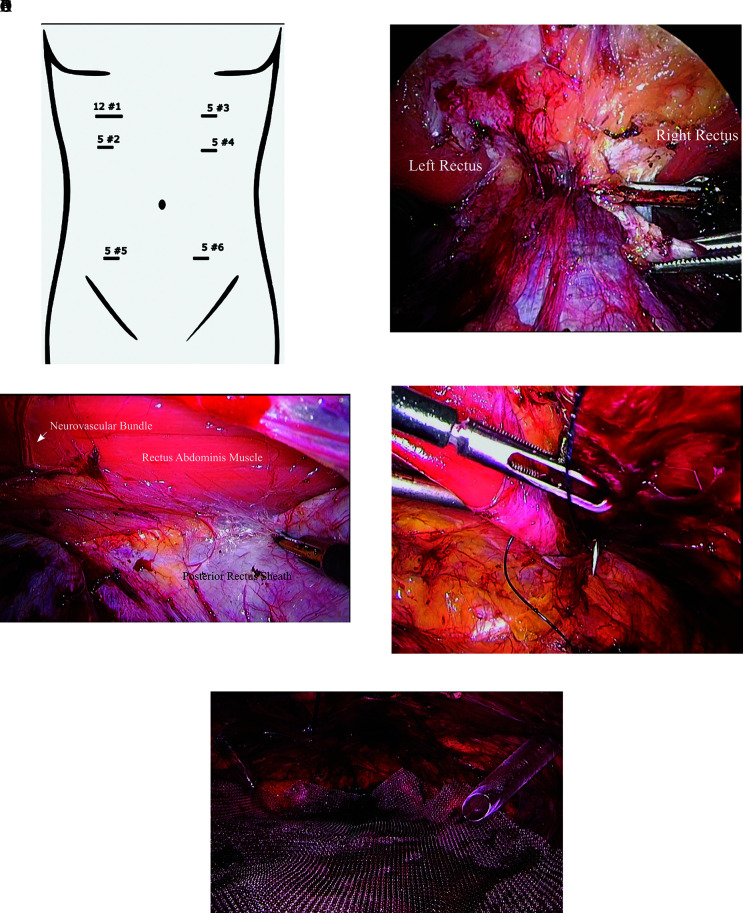
The patient was a 29-year-old woman (body weight 45 kg, body mass index 18.03 kg/m2) who delivered transvaginally two weeks before presenting with bulging of the abdominal wall. Her medical history included no specific disease, and her pregnancy history was gravida 3 and para 2. Computed tomographic and ultrasonographic examinations revealed an attenuated linea alba and separation of the rectus (Figures 1A and 1B). The distance between the two rectus abdominis muscles was 7 cm at the umbilicus, and the separation continued to 4 cm above and 4 cm below the umbilicus. Three months of conservative therapy comprising exercises to strengthen the transversus abdominis was ineffective, and the patient newly developed lower abdominal cramping and back pain at rest and had difficulty performing activities of daily living. Physical assessment, blood testing, and imaging examination ruled out other etiologies. Therefore, we decided to perform surgical treatment and selected the eTEP, Rives-Stoppa, and TAR procedure to reduce the risks of infection and hernia recurrence.
Figure 1.
Pre-operative computed tomography images of diastasis recti abdominis, A) Axial view, 6 – 7 centimeter diastasis, B) Sagittal view showing 6 – 7 centimeter diastasis.
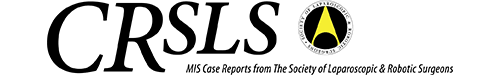
After the induction of general anesthesia and intubation, the patient was placed in the supine position. Port #1 (Kii Fios, 12 mm; Applied Medical, Rancho Santa Margarita, CA) was inserted in the right upper quadrant for the eTEP access with the optical method, and an inflation pressure of 8 cm H2O to 10 cm H2O was used to dissect the retrorectus space (Figure 2A). Port #2 (EZ trocar, 5 mm; Hakko, Nagano, Japan) was inserted into the retrorectus space. A 30-degree scope was placed through port #1. Using port #2, the right posterior rectus sheath (PRS) was released in the caudal-to-cephalad direction with an ultrasonic coagulation and cutting instrument, and inferior crossover was done from the right to left PRS. Port #3 (EZ trocar, 5 mm) was inserted and the left PRS was dissected. Port #4 (5 mm) was inserted on the left side above the umbilicus. Ports #5 and #6 (5 mm) were inserted to release the PRS caudally (Figure 2B). The bilateral TAR procedure was performed to confirm the mesh placement and tension-free rectus plication. The neurovascular bundle was identified, and the lamina of the internal oblique muscle was transected just medial to the neurovascular bundle (Figure 2C). The underlying transversus abdominis muscle was transected to release the plane posterior to the transversus abdominis muscle, achieving bilateral TAR. The extent of dissection of the retrorectus space was 3 cm from the diastasis in all directions. Following this, both sides of the rectus were plicated with barbed self-locking 2-0 V-lok suture (Figure 2D). Polypropylene mesh (30 × 21 cm Ventralight ST; Beckman and Dickinson Company, Franklin Lakes, NJ) was placed in the retrorectus/preperitoneal space (Figure 2E) and fixed by 3-0 Vicryl at the cranial, caudal, and both lateral sides. A 19-Fr silicone suction drain was placed in the retrorectus space. We used intraperitoneal mesh as the retrorectus mesh because this is the only large-sized mesh available in our hospital.
Figure 2.
Endoscopic view in the extended-view totally extraperitoneal approach with Rives-Stoppa hernia repair and transverse abdominus release, A) Port sites, B) Medial edges of both posterior rectus sheaths, C) Transverse abdominus release, D) Suturing of the linea Alba and defect, E) Polypropylene mesh placement.
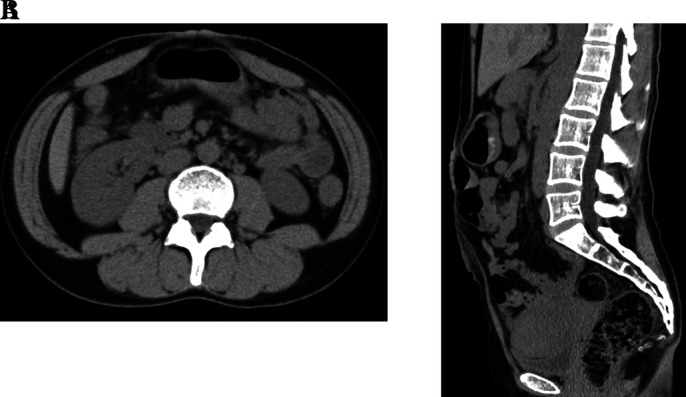
The postoperative course was uneventful. The drain was removed on postoperative day 4, and the patient was discharged on postoperative day 5. At one month after the surgery, the patient reported only slight discomfort when lifting her child; the lower abdominal cramping and back pain had disappeared, and suturing and mesh fixation pain was not induced by contraction or relaxation of the rectus abdominis. There was no recurrence seen on routine follow-up abdominal computed tomography performed 3 months after the surgery (Figure 3). One year after the surgery, the patient had not experienced DRA recurrence, and the discomfort had disappeared. Hernia recurrence mainly occurs in one year, and after one year routine follow-up the patient is counseled to return to a clinic if any clinical changes occur.
Figure 3.
Computed tomography images obtained three months postoperatively. Axial view shows no recurrence and no seroma.
DISCUSSION
DRA typically occurs after pregnancy3 and differs from ventral hernia because there is no surgical scar and the patients are young women of reproductive age. Conservative therapeutic abdominal exercises are useful in some cases. No study has assessed which abdominal exercises are most effective for DRA, but we chose exercises to strengthen the transversus abdominis, as described in previous studies.4,5 In our case, three months of conservative therapy failed to resolve the condition, and lower abdominal cramping and back pain had newly appeared. In such situations, DRA requires surgical intervention. From a cosmetic point of view, DRA treatment requires minimally invasive surgery. However, a standard surgical procedure for DRA has not been established. Laparoscopic hernia repair decreases risk of infection, but earlier studies reported an increased risk of recurrence and bowel injury for large, complicated ventral hernia compared with open surgery. More recent reports have shown outcomes of laparoscopic hernia repair that are comparable to those for open surgery; however, some cases convert to open surgery.6 To date, the implementation of laparoscopic hernia repair has been restricted by technical and topological difficulties, especially for intracorporeal repair.
Several recent studies have reported minimally invasive surgical techniques for DRA, including the Venetian blind technique,1 intracorporeal suture and underlay mesh repair, SubCutaneous OnLay endoscopic Approach (SCOLA),7 pre-aponeurotic endoscopic repair (REPA),8 the Trentino Hernia Team (THT) technique,9 suturing the rectus sheath with a linear stapler, and placing retrorectus mesh. However, the long-term outcomes of these techniques are unknown, and it is unclear which is the best procedure for DRA repair. Intracorporeal suture and underlay mesh repair may cause perioperative pain, direct mesh contact with viscera, and operability may be poor because of limitations regarding the port positions.2,10 The SCOLA and REPA techniques sometimes cause tissue ischemia and skin necrosis following the cutting or cauterizing of perforator vessels.11 The THT technique is an intraperitoneal procedure with limited port position options that result in poor operability. Performing the Rives-Stoppa and TAR procedures via the eTEP has three major advantages: retrorectus mesh placement, flexible port positioning, and adoption of a standard open surgery method in minimally invasive surgery.
Mesh repair is superior to supportive suture but carries a risk of mesh infection. In particular, the use of mesh in a young female of child-bearing age carries the risks of chronic pain in pregnancy and obstruction in future laparoscopic or open surgery. As with ventral hernia, these risks are related to mesh placement.12 Retrorectus mesh placement reportedly lowers the recurrence rate and infection rate compared with the interposition mesh procedure (which has the highest infection and recurrence rates) and the onlay procedure (which has the highest recurrence rate).12
The combination of eTEP, Rives-Stoppa, and TAR procedure resolves these difficulties. The eTEP ensures that the procedure remains minimally invasive while still enabling the surgeon to perform the Rives-Stoppa procedure, which is a standard method in ventral hernia repair. TAR is performed to achieve tension-free suturing of the hernia defect and ensure appropriate mesh placement.
For the abovementioned reasons, the combined eTEP, Rives-Stoppa, and TAR procedure is superior to other methods, such as endoscopic-assisted linea alba reconstruction, intraperitoneal onlay mesh placement, and the subcutaneous onlay laparoscopic approach. In our case, there was no infection, chronic pain, or hernia recurrence after the Rives-Stoppa retrorectus mesh placement. The advantages of combined eTEP, Rives-Stoppa, and TAR procedure have been previously described in ventral hernia repair, and our successful experience demonstrated that these advantages carry over to DRA treatment.13
The eTEP-TAR for DRA may cause port site scarring, postoperative seroma, and chronic pain during the next pregnancy. To minimize cosmetic problems, we used the smallest possible port sizes (only one 12-mm port and five 5-mm ports) and buried the sutures used to close the port site wounds. Therefore, our patient’s port site scars were almost unnoticeable. To prevent seroma, a drain was placed in the retrorectus space. Regarding the risk of chronic pain during subsequent pregnancies, although there have been several reports that both mesh and linea alba suturing without mesh caused pain in the last trimester, other reports have not found the mesh to cause pain.14,15 However, it is clear that, in DRA as in ventral hernia, suture-only repair has a higher recurrence risk than mesh repair.16 As our patient had no plans for a subsequent pregnancy, we could not confirm whether mesh repair caused pain during pregnancy. However, we speculate that mesh elasticity may influence chronic pain following surgical treatment of DRA, and adequate mesh elasticity may be useful in improving both hernia recurrence and chronic pain in the next pregnancy.
CONCLUSIONS
This case report suggests that the combined eTEP, Rives-Stoppa, and TAR procedure may be a promising minimally invasive surgical option for DRA.
Footnotes
Acknowledgements: We thank Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Disclosure: none.
Funding sources: none.
Conflict of interests: none.
Informed consent: Dr. Masahito Kinoshita declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
References:
- 1.Palanivelu C, Rangarajan M, Jategaonkar PA, Amar V, Gokul KS, Srikanth B. Laparoscopic repair of diastasis recti using the 'Venetian blinds' technique of plication with prosthetic reinforcement: a retrospective study. Hernia. 2009;13(3):287–292. [DOI] [PubMed] [Google Scholar]
- 2.Belyansky I, Daes J, Radu VG, et al. A novel approach using the enhanced-view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc. 2018;32(3):1525–1532. [DOI] [PubMed] [Google Scholar]
- 3.Nahabedian MY. Management strategies for diastasis recti. Semin Plast Surg. 2018;32(3):147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Michalska A, Rokita W, Wolder D, Pogorzelska J, Kaczmarczyk K. Diastasis recti abdominis - a review of treatment methods. Ginekol Pol. 2018;89(2):97–101. [DOI] [PubMed] [Google Scholar]
- 5.Lee D, Hodges PW. Behavior of the linea alba during a curl-up task in diastasis rectus abdominis: an observational study. J Orthop Sports Phys Ther. 2016;46(7):580–589. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Y, Zhou H, Chai Y, Cao C, Jin K, Hu Z. Laparoscopic versus open incisional and ventral hernia repair: a systematic review and meta-analysis. World J Surg. 2014;38(9):2233–2240. [DOI] [PubMed] [Google Scholar]
- 7.Claus C, Cavazzola L, Malcher F. Subcutaneous Onlay endoscopic approach (SCOLA) for midline ventral hernias associated with diastasis recti. Hernia. 2021;25(4):957–962. [DOI] [PubMed] [Google Scholar]
- 8.Juárez Muas DM. Preaponeurotic endoscopic repair (REPA) of diastasis recti associated or not to midline hernias. Surg Endosc. 2019;33(6):1777–1782. [DOI] [PubMed] [Google Scholar]
- 9.Carrara A, Catarci M, Fabris L, et al. Prospective observational study of abdominal wall reconstruction with THT technique in primary midline defects with diastasis recti: clinical and functional outcomes in 110 consecutive patients. Surg Endosc. 2021;35(9):5104–5114. [DOI] [PubMed] [Google Scholar]
- 10.Penchev D, Kotashev G, Mutafchiyski V. Endoscopic enhanced-view totally extraperitoneal retromuscular approach for ventral hernia repair. Surg Endosc. 2019;33(11):3749–3756. [DOI] [PubMed] [Google Scholar]
- 11.Chang CJ. Assessment of videoendoscopy-assisted abdominoplasty for diastasis recti patients. Biomed J. 2013;36(5):252–256. [DOI] [PubMed] [Google Scholar]
- 12.Albino FP, Patel KM, Nahabedian MY, Sosin M, Attinger CE, Bhanot P. Does mesh location matter in abdominal wall reconstruction? A systematic review of the literature and a summary of recommendations. Plast Reconstr Surg. 2013;132(5):1295–1304. [DOI] [PubMed] [Google Scholar]
- 13.Radu VG, Lica M. The endoscopic retromuscular repair of ventral hernia: the eTEP technique and early results. Hernia. 2019;23(5):945–955. [DOI] [PubMed] [Google Scholar]
- 14.Jensen KK, Henriksen NA, Jorgensen LN. Abdominal wall hernia and pregnancy: a systematic review. Hernia. 2015;19(5):689–696. Oct [DOI] [PubMed] [Google Scholar]
- 15.Mulder RJ, Stroobants WL, Roumen FJ. Pregnancy and delivery with an abdominal mesh graft. Eur J Obstet Gynecol Reprod Biol. 2004;116(2):235–236. [DOI] [PubMed] [Google Scholar]
- 16.Oma E, Jensen KK, Jorgensen LN. Increased risk of ventral hernia recurrence after pregnancy: a nationwide register-based study. Am J Surg. 2017;214(3):474–478. [DOI] [PubMed] [Google Scholar]