Abstract
Background
Arteriosclerosis and atherosclerosis are closely related with cardiovascular disease (CVD) risk. Remnant cholesterol (RC) could predict CVD. However, its effect on joint arteriosclerosis and atherosclerosis progression remains unclear. This study aims to evaluate the association of RC with joint arteriosclerosis and atherosclerosis progression trajectories in the general population.
Methods
This study collected data across five biennial surveys of the Beijing Health Management Cohort from 2010 to 2019. Multi-trajectory model was used to determine the joint arteriosclerosis and atherosclerosis progression patterns by brachial-ankle pulse wave velocity (baPWV) and ankle brachial index (ABI). We also performed discordance analyses for RC vs. low density lipoprotein cholesterol (LDL-C) using ordinal logistics model.
Results
A total of 3186 participants were included, with three clusters following distinct arteriosclerosis and atherosclerosis progression patterns identified using a multi-trajectory model. In the multivariable-adjusted ordinal logistics analyses, RC was significantly associated with baPWV and ABI progression (OR: 1.20; 95% CI: 1.13–1.28, per 10 mg/dL). For the discordance analyses, the discordant low RC group was associated with decreased risk compared to the concordant group (OR: 0.73; 95% CI: 0.60–0.89). People with a high RC level were at an increased risk of joint arteriosclerosis and atherosclerosis progression, even with optimal LDL-C.
Conclusions
RC is independently associated with joint arteriosclerosis and atherosclerosis progression beyond LDL-C. RC could be an earlier risk factor than LDL-C of arteriosclerosis and atherosclerosis in the general population.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-023-02733-w.
Keywords: Remnant cholesterol, Arteriosclerosis and atherosclerosis, Brachial-ankle pulse wave velocity, Ankle brachial index, LDL cholesterol
Background
Cardiovascular disease (CVD) has become one of the greatest threats to public health and the leading cause of mortality and health burden worldwide [1]. Systemic arteriosclerosis and atherosclerosis are robust predictors of CVD and overall death [2, 3], causing vascular damage by degenerating arterial elasticity and increasing pulse pressure [4]. Therefore, it is of significance to identify the primary risk factors and potential target(s) for the early recognition of arteriosclerosis and atherosclerosis. Brachial-ankle pulse wave velocity (baPWV) and ankle-brachial index (ABI) are two sensitive and non-invasive alternative indicators for arteriosclerosis and peripheral atherosclerosis widely used in population studies [5–7]. High baPWV and low ABI are independent predictors of cardiovascular events and mortality [6, 8]. Thus, combining the two indicators, baPWV and ABI, can comprehensively assess the CVD risk.
Abnormal lipid metabolism plays a key role in arteriosclerosis and atherosclerosis [9–12]. Lowering low-density lipoprotein cholesterol (LDL-C) primarily through statin is the leading therapy target for primary and secondary prevention of arteriosclerosis and atherosclerosis-related diseases [13, 14]. However, patients with a substantial reduction in LDL-C still have a considerable residual CVD risk [15, 16]. Atherogenic dyslipidemia, characterized by high levels of triglycerides and low concentrations of high-density lipoprotein cholesterol (HDL-C) with normal concentrations of LDL-C, is a common lipid disorder and one of the main causes of lipid-dependent residual CVD risk [17]. In view of the fact that several clinical trials found that HDL-C raising therapies did not significantly reduce the risk of CVD [18], recent research attentions have shifted to triglyceride-rich lipoproteins (TRLs). Human cells can generally degrade triglycerides but not cholesterol. Thus, we hypothesized that the cholesterol component carried on TRLs may be the main culprits for arteriosclerosis and atherosclerosis [17]. Remnant cholesterol (RC) represents the cholesterol content of TRLs, i.e., the intermediate density lipoprotein (IDL) and very low density lipoprotein (VLDL) in the fasting state. It also includes the extra chylomicron remnants in the non-fasting state [19]. There are studies showing that TRLs could penetrate through and accumulate on the arterial wall and subsequently cause foam cell formation, atherosclerosis, and low-grade inflammation [19–21]. Emerging evidence suggested that remnant cholesterol (RC) could contribute to CVD residual risk to a large extent [15, 19]. Both epidemiological and genetic studies have reported the causal association of RC with CVD and mortality [17, 20, 22–28]. Considering the progression of arteriosclerosis and atherosclerosis is an important early vascular feature in the occurrence of CVD, evidence about the association of RC with arteriosclerosis and/or atherosclerosis is still limited. Cross-sectional studies found that increased RC is significantly associated with baPWV alone [7, 29]. However, the longitudinal association of RC with the joint arteriosclerosis and atherosclerosis progression remains unclear.
Therefore, we aimed to jointly characterize the progression trajectory combining multiple examinations of baPWV and ABI during a 10-year follow-up and to evaluate the effect of RC on the arteriosclerosis and atherosclerosis progression in the general population. This study for the first time provided data about RC with joint baPWV and ABI progression for the early recognition of arteriosclerosis and atherosclerosis from a longitudinal cohort perspective.
Methods
Settings
For the current study, we used individual-level data from the Beijing Health Management Cohort (BHMC). The BHMC study was conducted based on physical examination populations from Beijing Xiaotangshan Examination Center and Beijing Physical Examination Center, which are two biggest health examination centers in Beijing, China. The participants were required to undertake regular physical examinations (height, weight, heart rate, blood pressure, ultrasound, arterial stiffness), face-to-face questionnaire survey, and blood sample collection under a uniform examination package. This cohort collected longitudinal key variables such as lipid profiles, chronic diseases status, and arterial stiffness measurements that are valuable for CVD prevention, treatment, and management. The study was approved by the Ethics Committee of Capital Medical University (grant number: 2020SY031) and Edith Cowan University (grant number: 2021-03164-WU). All participants provided written informed consent before taking part in the study.
Study design and population
We examined the association between the baseline level of RC, other lipid parameters, and joint arteriosclerosis and atherosclerosis progression, with the baseline defined as visit 1 between 2010 and 2011. The health examination during 2012 to 2013 was then defined as visit 2, 2014 to 2015 as visit 3, 2016 to 2017 as visit 4, and 2018 to 2019 as visit 5. The measurements of baPWV and ABI data were extracted from all visits. All participants aged 25 years and above without a history of CVD at baseline were initially screened for inclusion. Individual-level records with any missing data of lipid profiles or baPWV or ABI measurements were excluded. Finally, a total of 3186 individuals with three or more subsequent visits were enrolled for the final analyses.
Laboratory measurements
Fasting blood samples were stored and measured in the central laboratories of Beijing Xiaotangshan Examination Center and Beijing Physical Examination Center. Fasting glucose, serum total cholesterol, triglyceride, HDL-C, and LDL-C were directly measured using the Olympus Automatic Biochemical Analyzer (Hitachi 747; Tokyo, Japan). The coefficients of variation (CVs) were < 4.0% for triglyceride and HDL-C, < 3.0% for total cholesterol, and LDL-C and < 5.0% for fasting glucose. Non-HDL-C was calculated as total cholesterol concentration minus HDL-C. RC was defined as non-HDL-C minus the calculated LDL-C by the Martin equation [30]. The Martin-Hopkins method matches 1/180 factor by individual triglycerides and non-HDL-C levels to estimate the LDL-C level. Thus, RC could be calculated by non-HDL-C minus the estimated LDL-C level (Stata code: https://www.ldlcalculator.com/). The Martin-Hopkins method is recommended by the American Heart Association (AHA) guidelines and has been applied in many population studies. RC was alternatively estimated as non-HDL-C minus the calculated LDL-C by the Friedewald equation for triglycerides < 400 mg/dL (or non-HDL-C minus the directly measured LDL-C for triglycerides ≥ 400 mg/dL) in the sensitivity analysis. In this current study, Martin equation was used in the main analysis and Friedewald equation was adopted in the sensitivity analysis. High-sensitivity C-reactive protein (hsCRP) was also measured, as hsCRP is closely related with RC and contributes to the CVD risk [14].
Discordance definition
We used two approaches to define discordance between LDL-C and RC. First, we defined discordance by the percentile distance between RC and LDL-C. The population was classified into three groups: discordantly low RC (RC percentile < LDL-C percentile by 10 percentile units), concordant RC and LDL-C (RC percentile minus LDL-C percentile within ± 10 percentile units), and discordantly high RC (RC percentile > LDL-C percentile by 10 percentile units) following the previous study [26]. Second, we used the relevant clinical cut-off points to define discordance between LDL-C (100 and 130 mg/dL) and RC (17 and 24 mg/dL) according to the established Guideline Recommendations [31]. Third, we used the median values of LDL-C and RC as cut-off points [32, 33].
BaPWV and ABI measurements
The baPWV was measured with an Omron Colin BP-203RPE III device (Omron Health Care, Kyoto, Japan). After a minimum of 5 min rest in the supine position, four cuffs were wrapped around the bilateral brachial and ankles and then connected to a plethysmographic sensor and oscillometric pressure sensor. The final baPWV was calculated as the length between the brachium and ankle divided by the transit time between the wave front of the brachial waveform and the ankle waveform [34]. ABI was calculated using the following formula [35]: ABI = SBP of posterior tibial artery/SBP of the brachial artery. At least two acceptable measurements were performed on each side (right and left) and the difference between two measures of each side should be less than 50 cm/s for baPWV and 0.05 for ABI. The mean value of these two measurements were separately recorded for each side. The maximum value of baPWV on the left and right sides was used. The minimum value of ABI on the left and right sides was used in the analysis.
Other covariates
The demographic characteristics, smoking status, history of diseases, and medication uses were collected at baseline survey via a standard questionnaire by our trained staff. Smoking status was divided into current smoking or not. Anthropometric measurements were performed. Body mass index (BMI) was calculated as weight (in kilograms)/height squared (in meters squared). Overweight and obesity was defined as BMI ≥ 24.0 kg/m2 and ≥ 28.0 kg/m2 according to the BMI standard for Asian subjects [36]. Systolic blood pressure and diastolic blood pressure were presented as the average of two measurements on the right arm using a sphygmomanometer after resting for at least 10 min. Hypertension status was defined as systolic pressure ≥ 140 mmHg or diastolic pressure ≥ 90 mmHg, self-reported diagnosis history of hypertension, or use of antihypertensive medication [37]. Type 2 diabetes was defined as fasting glucose ≥ 7.0 mmol/L or using any glucose-lowering medication or self-reported diagnosis history of diabetes [38]. In this current study, there was no type 1 diabetes reported. Lipid-lowering medication referred to any use of statins or fibrates in this study.
Statistical analysis
Statistical analysis was conducted from May to December 2021. The baseline characteristics of the study population by arteriosclerosis and atherosclerosis progression clusters were described, using medians (25th–75th percentiles) for continuous variables and frequencies (proportions) for categorical variables. The differences were compared by Kruskal-Wallis test or chi-squared test between three groups, as appropriate.
We estimated the joint progression trajectories of arteriosclerosis and atherosclerosis across the five biennial visits by baPWV and ABI, using group-based multi-trajectory modeling [39]. We fitted the joint changes of baPWV and ABI with age as the time-scale following previous studies [40, 41]. The group-based multi-trajectory model allows the identification of clusters of individuals following similar patterns through multiple visits using multi-variables. Varied models were considered to choose the optimal number of distinct groups and trajectory shape parameters (e.g., linear, quadratic, cubic) based on Bayesian information criteria (BIC) and Akaike information criterion (AIC). Sufficient sample sizes in each multi-trajectory group (> 5% of the sample) and clinical interpretation are important additional elements when determining the best model. Furthermore, we fitted the progression trajectory of baPWV and ABI separately using group-based trajectory modeling.
Unadjusted and adjusted ordinal logistics models were used to assess the associations of baseline lipid profiles (considered as both continuous and categorical variables) with arteriosclerosis and atherosclerosis progression clusters. Adjustments were made for age, sex, BMI, smoking status, systolic blood pressure, hypertension, diabetes, antihypertensive medication, and lipid-lowering treatment. Using the same models, we assessed the association of RC and LDL-C concordant/discordant groups with baPWV and ABI progression using the difference in percentile units, clinical cut-off points, and medians of RC and LDL-C. Finally, we performed three sensitivity analyses by excluding individuals on lipid-lowering therapy (n = 634), additionally adjusting for hsCRP (available in 2358 of 3186 individuals) and further adjusting for the change of systolic blood pressure during the follow-up period to explore the stability of our findings.
The group-based trajectory modeling technique was implemented using Proc Traj in Stata software version 14 (STATA Corp., TX, US). All other statistical analyses were performed with R software version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria). Two-sided p < 0.05 was considered statistically significant.
Results
Characteristics
The baseline characteristics of the participants are shown in Additional file 1: Table S1. Of 3186 individuals, the median (P25-P75) of age was 65.0 (57.0,75.0) years; 2445 (76.7%) were male; 829 (26.0%) with hypertension; and 337 (10.6%) with diabetes. Median levels were RC: 23.35 mg/dL, LDL-C: 114.86 mg/dL, non-HDL-C: 128.26 mg/dL; HDL-C: 48.52 mg/dL. The percentage of concordant RC and LDL-C was 23.5%, while 40.1% had discordantly low RC, and 36.4% had discordantly high RC. Proportions of concordance/discordance among individuals according to LDL-C clinical cut-off points are presented in Additional file 2: Fig. S1.
Clusters of arteriosclerosis and atherosclerosis progression
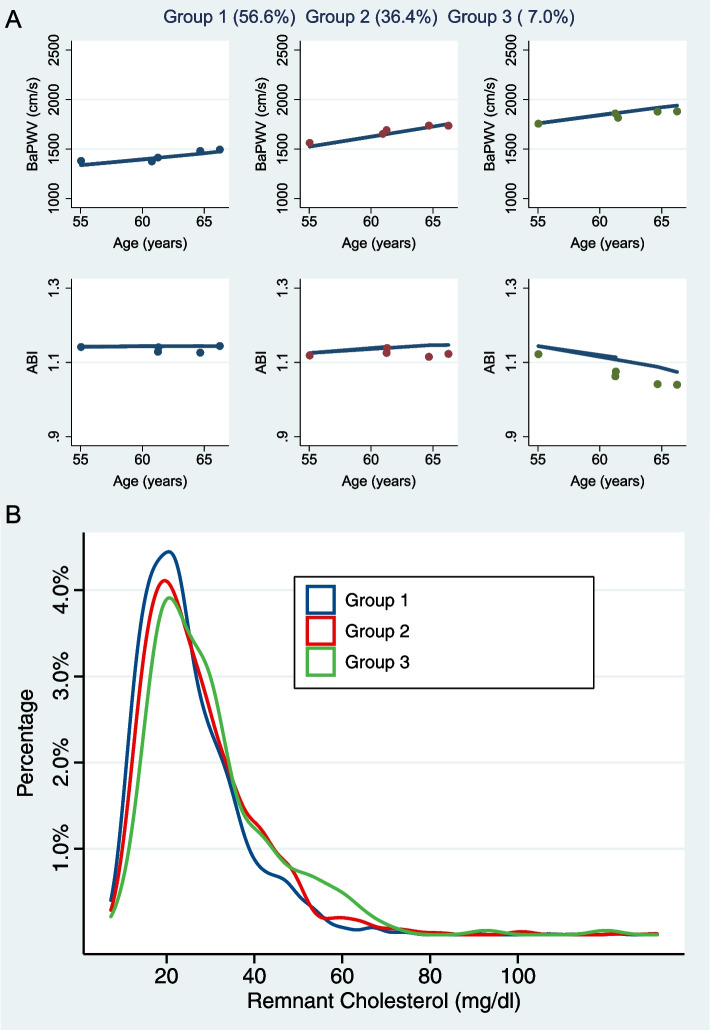
Using the criteria mentioned above, we determined three clusters using the multi-trajectory model as stable baPWV/stable ABI (group 1: 56.6%), increasing baPWV/stable ABI (group 2: 36.4%), and increasing baPWV/decreasing ABI (group 3: 7.0%). The procedure of choosing the optimal group number and shape parameter for the final model was shown in Additional file 1: Table S2. Thus, the three groups represented a gradually increased risk of joint arteriosclerosis and atherosclerosis progression. Figure 1A shows the longitudinal joint trajectories of baPWV and ABI, and the percentages for each group. The characteristics of the three clusters are shown in Table 1. The RC (medians: 22.6 vs. 24.4 vs. 26.9 mg/dL, p < 0.001) and HDL-C (medians: 49.6 vs. 47.6 vs. 44.6 mg/dL, p < 0.001) were significantly distributed in three groups, whereas there were no significant differences for LDL-C (medians: 115.1 vs. 114.3 vs. 113.5 mg/dL, p = 0.852), or non-HDL-C (medians: 127.6 vs. 128.5 vs. 131.1 mg/dL, p = 0.208). The RC distribution according to the joint progression clusters is shown in Fig. 1B. We also derived a multi-group propensity score weighting model to infer the casual differences of lipid profiles. In the matched multi-trajectory clusters, RC concentrations were still significantly higher in group 2 and group 3, compared to group 1 (Additional file 1: Table S3). In addition, we fitted the progression trajectories of baPWV and ABI separately (Additional file 2: Fig. S2).
Fig. 1.
The distribution of remnant cholesterol among groups of arteriosclerosis and atherosclerosis progression clustered by multi-trajectory model. A Joint arteriosclerosis and atherosclerosis progression patterns clustered by multi-trajectory model. B Density distribution of remnant cholesterol in trajectory groups. Dots show group-specific mean observed levels, and solid lines represent fitted trajectories. baPWV, brachial-ankle pulse wave velocity; ABI, ankle-brachial index
Table 1.
Characteristics in multi-trajectory groups of joint baPWV and ABI
| Group 1d (n = 1802) | Group 2 (n = 1160) | Group 3 (n = 224) | |
|---|---|---|---|
| Age, years | 64.00 [56.00, 73.00] | 66.00 [58.00, 76.00] | 66.00 [56.00, 77.00] |
| Female sex, n (%) | 473 (26.2) | 238 (20.5) | 30 (13.4) |
| BMI, kg/m2 | 25.16 [23.29, 27.26] | 25.48 [23.82, 27.25] | 25.55 [23.87, 27.48] |
| BMI group, n (%) | |||
| 24.0 kg/m2 | 576 (33.4) | 300 (27.1) | 58 (27.4) |
| 24.0–27.9 kg/m2 | 837 (48.5) | 617 (55.7) | 111 (52.4) |
| ≥ 28.0 kg/m2 | 314 (18.2) | 191 (17.2) | 43 (20.3) |
| Current smoker, n (%) | 432 (24.0) | 280 (24.1) | 45 (20.1) |
| SBP, mmHg | 122.81 (15.91) | 132.80 (16.47) | 139.47 (17.04) |
| SBP change, mmHg | 4.61 (23.55) | 5.31 (22.97) | 9.81 (25.62) |
| Hypertension, n (%) b | 413 (22.9) | 345 (29.7) | 71 (31.7) |
| Diabetes, n (%) c | 153 (8.5) | 138 (11.9) | 46 (20.5) |
| Antihypertensive medication, n (%) | 386 (21.4) | 328 (28.3) | 64 (28.6) |
| Lipid-lowering medication use, n (%) | 352 (19.5) | 241 (20.8) | 41 (18.3) |
| Triglycerides, mg/dL | 113.09 [85.28, 152.94] | 121.83 [91.90, 168.42] | 134.56 [99.51, 179.19] |
| RC, mg/dL | 22.60 [17.06, 30.51] | 24.37 [18.38, 33.59] | 26.91 [19.91, 35.19] |
| LDL-C, mg/dL | 115.06 [97.42, 133.23] | 114.26 [97.29, 135.44] | 113.52 [94.60, 131.08] |
| HDL-C, mg/dL | 49.64 [42.61, 58.69] | 47.55 [40.98, 55.29] | 44.58 [39.80, 51.24] |
| Non-HDL-C, mg/dL | 127.64 [109.15, 146.36] | 128.51 [108.82, 151.06] | 131.11 [108.74, 149.44] |
| hsCRP, mg/L d | 0.76 [0.46, 1.42] | 0.90 [0.52, 1.72] | 1.01 [0.58, 1.92] |
Continuous variables are reported as median (25th–75th percentile). Medians and proportions were compared using Kruskal–Wallis or chi-squared test
SI conversion factor: To convert RC, LDL-C, HDL-C, non-HDL-C to mmol/L, multiply by 0.02586; TG, multiply by 0.01129
Abbreviations: CI Confidence interval, BMI Body mass index, SBP Systolic blood pressure, DBP Diastolic blood pressure, RC Remnant cholesterol, LDL-C Low-density lipoprotein cholesterol, HDL-C High-density lipoprotein cholesterol, hsCRP High-sensitivity C-reactive protein
aHypertension defined as SBP ≥ 140 mmHg or DBP ≥ 90 mmHg, self-reported diagnosis history of hypertension or use of antihypertensive medication
bDiabetes defined as fasting glucose ≥ 7.0 mmol/L or using any glucose-lowering medication or self-reported diagnosis history of diabetes
chsCRP data only available in a part of overall population (2358 of 3186 subjects)
dGroup 1 represents the stable baPWV/stable ABI, group 2 represents increasing baPWV/stable ABI, and group 3 represents increasing baPWV/decreasing ABI
Association of lipid profiles with baPWV and ABI progression
In the current study, RC was weakly correlated with LDL-C (β = 0.061, p < 0.05) but moderately correlated with triglycerides (β = 0.792, p < 0.001) and HDL-C (β = − 0.461, p < 0.001) after adjusting for age and sex (Additional file 1: Table S4). The scatter plots between RC and LDL-C are presented in Additional file 2: Fig. S3.
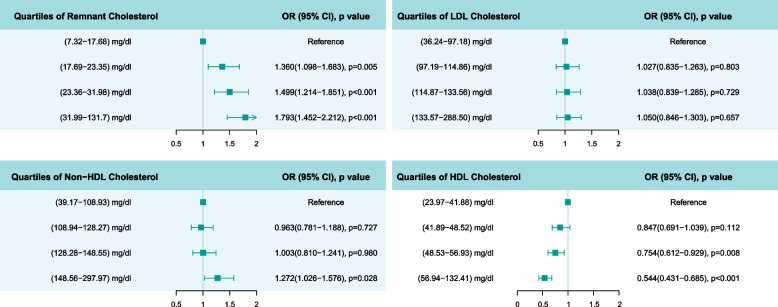
In the ordinal logistics models, we observed significant associations of triglycerides, RC, HDL-C, and non-HDL-C with joint baPWV and ABI progression (Table 2). The adjusted OR (95% CI) were 1.029 (1.019–1.039) for triglycerides per 10 mg/dL increase, 1.203 (1.132–1.278) for RC per 10 mg/dL increase, 0.905 (0.872–0.939) for HDL-C per 5 mg/dL increase, and 1.043 (1.016–1.070) for non-HDL-C per 10 mg/dL increase, respectively. The OR values of other covariates in the adjusted model are shown in Additional file 1: Table S5. We further examined the association of the quartile of lipid profiles with the joint baPWV and ABI progression trajectories (Fig. 2).
Table 2.
Association of baseline lipid profiles with the increase of baPWV along with a decreasing ABI
| Unadjusted odds ratio (95% CI) | p value | Adjusted odds ratio (95% CI) | p value | |
|---|---|---|---|---|
| Triglycerides, + 10 mg/dL | 1.030 (1.021–1.039) | < 0.001 | 1.029 (1.019–1.039) | < 0.001 |
| RC, + 10 mg/dL | 1.207 (1.143–1.275) | < 0.001 | 1.203 (1.132–1.278) | < 0.001 |
| LDL-C, + 10 mg/dL | 1.007 (0.982–1.033) | 0.585 | 1.025 (0.996–1.054) | 0.091 |
| HDL-C, + 5 mg/dL | 0.894 (0.867–0.922) | < 0.001 | 0.905 (0.872–0.939) | < 0.001 |
| Non-HDL-C, + 10 mg/dL | 1.029 (1.005–1.053) | 0.018 | 1.043 (1.016–1.070) | < 0.001 |
Odds ratio (OR) was estimated by ordinal logistics regression models adjusted for age, sex, body mass index, smoking status, systolic blood pressure, hypertension, diabetes, antihypertensive medication, and lipid-lowering treatment
Abbreviations: CI Confidence interval, RC Remnant cholesterol, LDL-C Low-density lipoprotein cholesterol, HDL-C High-density lipoprotein cholesterol
Fig. 2.
Association of cholesterol components with arteriosclerosis and atherosclerosis progression. Odds ratios (95% CI) were estimated by ordinal logistics regression models adjusted for age, sex, body mass index, smoking status, systolic pressure, hypertension, diabetes, antihypertensive medication, and lipid-lowering treatment
The associations of lipid profiles with separate baPWV and ABI progression trajectories are shown in Additional file 1: Table S6. We also observed significant associations of RC (per 10 mg/dL increase) with a higher level of baPWV and a lower level of ABI, and the adjusted OR were 1.154 (1.033–1.201) and 1.206 (1.114–1.301), respectively.
Discordance analysis of RC and LDL-C
Compared to the concordant group, the discordantly low RC had a significant decreased risk of joint arteriosclerosis and atherosclerosis progression after adjusting the common CVD risk factors (adjusted OR: 0.733; 95% CI: 0.604–0.889). However, we did not observe a significantly increased risk in the discordantly high RC group (adjusted OR: 0.989; 95% CI: 0.816–1.199). At the cut-off points of 130 mg/dL for LDL-C and 24 mg/dL for RC, those with high RC (≥ 24 mg/dL) and low LDL-C (< 130 mg/dL) had an increased risk of arteriosclerosis and atherosclerosis progression (adjusted OR: 1.445; 95% CI: 1.210–1.725), compared to the group with both low RC (< 24 mg/dL) and LDL-C (< 130 mg/dL). Notably, individuals with low RC (< 24 mg/dL) and high LDL-C (≥ 130 mg/dL) had a borderline increased risk (adjusted OR: 1.276; 95% CI: 1.000–1.628). In addition, consistent results were observed when using the clinical cut-off points of 100 mg/dL for LDL-C and 17 mg/dL for RC (Table 3), and the median values for LDL-C (114.86 mg/dL) and RC (23.35 mg/dL) (Additional file 1: Table S7).
Table 3.
Odds ratios (95% confidence interval) for the increasing baPWV along with decreasing ABI across LDL-C vs. remnant cholesterol concordant/discordant groups and according to clinical cut-off points
| Unadjusted odds ratio (95% CI) | Adjusted odds ratio (95% CI) | |
|---|---|---|
| RC percentile minus LDL-C percentile | ||
| Concordant (within 10 percentiles), n = 749 | Reference | Reference |
| Discordantly low RC, n = 1277 | 0.701 (0.586–0.837) | 0.733 (0.604–0.889) |
| Discordantly high RC, n = 1160 | 1.017 (0.85–1.217) | 0.989 (0.816–1.199) |
| Cutpoints: LDL-C 130 mg/dL; RC 24 mg/dL | ||
| LDL-C < 130 mg/dL and RC < 24 mg/dL, n = 1273 | Reference | Reference |
| LDL-C ≥ 130 mg/dL and RC < 24 mg/dL, n = 393 | 1.229 (0.981–1.539) | 1.276 (1.000–1.628) |
| LDL-C < 130 mg/dL and RC ≥ 24 mg/dL, n = 986 | 1.378 (1.169–1.626) | 1.445 (1.210–1.725) |
| LDL-C ≥ 130 mg/dL and RC ≥ 24 mg/dL, n = 534 | 1.689 (1.385–2.06) | 1.599 (1.289–1.983) |
| Cutpoints: LDL-C 100 mg/dL; RC 17 mg/dL | ||
| LDL-C < 100 mg/dL and RC < 17 mg/dL, n = 301 | Reference | Reference |
| LDL-C ≥ 100 mg/dL and RC < 17 mg/dL, n = 395 | 1.569 (1.154–2.132) | 1.348 (0.966–1.879) |
| LDL-C < 100 mg/dL and RC ≥ 17 mg/dL, n = 610 | 1.686 (1.281–2.218) | 1.604 (1.190–2.161) |
| LDL-C ≥ 100 mg/dL and RC ≥ 17 mg/dL, n = 1880 | 2.025 (1.601–2.561) | 1.899 (1.464–2.463) |
Odds ratio (OR) was estimated by ordinal logistics regression models adjusted for age, sex, body mass index, smoking status, systolic blood pressure, hypertension, diabetes, antihypertensive medication, lipid-lowering treatment
Abbreviations: CI Confidence interval, RC Remnant cholesterol, LDL-C Low-density lipoprotein cholesterol, HDL-C High-density lipoprotein cholesterol
(i) Concordant was defined as RC percentile and LDL-C percentile within ± 10 percentile units; (ii) discordantly low RC was defined as LDL-C percentile > RC percentile by 10 percentile units; and (iii) discordantly high RC was defined as RC percentile > LDL-C percentile by 10 percentile units
Sensitivity analyses
We observed consistent results after excluding individuals with lipid-lowering medication use or additionally adjusting for hsCRP level and the change of systolic blood pressure during the follow-up period (Table 4). In addition, we performed subgroup analyses, and the associations of RC with joint arteriosclerosis and atherosclerosis progression remained consistent when stratified by age, sex, BMI level, hypertension, and diabetes status (Additional file 1: Table S8). We further calculated the alternative RC concentration using the Friedewald formula, and the association results were almost consistent (Additional file 1: Table S9).
Table 4.
Associations of remnant cholesterol with the increasing baPWV along with decreasing ABI beyond LDL-C in sensitivity analyses
| Adjusted odds ratio (95% CI) | |||
|---|---|---|---|
| Sensitivity analysis I | Sensitivity analysis II | Sensitivity analysis III | |
| RC concentration, + 10 mg/dL | 1.220 (1.141–1.304) | 1.176 (1.090–1.269) | 1.256 (1.179–1.337) |
| Quartiles of RC | |||
| Quartile 1 | Reference | Reference | Reference |
| Quartile 2 | 1.251 (0.980–1.597) | 1.311 (1.024–1.679) | 1.398 (1.125–1.737) |
| Quartile 3 | 1.305 (1.017–1.675) | 1.582 (1.239–2.020) | 1.521 (1.228–1.884) |
| Quartile 4 | 1.862 (1.448–2.394) | 1.951 (1.527–2.493) | 1.789 (1.443–2.217) |
| RC percentile minus LDL-C percentile | |||
| Concordant | Reference | Reference | Reference |
| Discordantly low RC | 0.726 (0.585–0.901) | 0.747 (0.598–0.934) | 0.708 (0.583–0.862) |
| Discordantly high RC | 1.047 (0.839–1.306) | 0.979 (0.785–1.221) | 0.970 (0.798–1.179) |
| Cut-off: LDL-C 130 mg/dL; RC 24 mg/dL | |||
| LDL-C < 130 mg/dL and RC < 24 mg/dL | Reference | Reference | Reference |
| LDL-C ≥ 130 mg/dL and RC < 24 mg/dL | 1.672 (1.085–2.578) | 1.307 (0.896–1.907) | 1.190 (0.928–1.525) |
| LDL-C < 130 mg/dL and RC ≥ 24 mg/dL | 1.446 (1.170–1.787) | 1.395 (1.111–1.753) | 1.381 (1.154–1.652) |
| LDL-C ≥ 130 mg/dL and RC ≥ 24 mg/dL | 1.559 (1.255–1.937) | 1.385 (1.115–1.720) | 1.606 (1.291–1.997) |
| Cut-off: LDL-C 100 mg/dL; RC 17 mg/dL | |||
| LDL-C < 100 mg/dL and RC < 17 mg/dL | Reference | Reference | Reference |
| LDL-C ≥ 100 mg/dL and RC < 17 mg/dL | 1.561 (1.07–2.277) | 1.259 (0.876–1.810) | 1.233 (0.879–1.728) |
| LDL-C < 100 mg/dL and RC ≥ 17 mg/dL | 1.595 (1.154–2.205) | 1.587 (1.129–2.231) | 1.551 (1.146–2.100) |
| LDL-C ≥ 100 mg/dL and RC ≥ 17 mg/dL | 2.026 (1.522–2.696) | 1.784 (1.331–2.391) | 1.940 (1.489–2.527) |
Odds ratio (OR) was estimated by ordinal logistics regression models adjusted for age, sex, body mass index, smoking status, SBP, hypertension, diabetes, antihypertensive medication, lipid-lowering treatment
Abbreviations: CI Confidence interval, RC Remnant cholesterol, LDL-C Low-density lipoprotein cholesterol, HDL-C High-density lipoprotein cholesterol, SBP Systolic blood pressure
(i) Concordant was defined as RC percentile and LDL-C percentile within ± 10 percentile units; (ii) discordantly low RC was defined as LDL-C percentile > RC percentile by 10 percentile units; and (iii) discordantly high RC was defined as RC percentile > LDL-C percentile by 10 percentile units
Sensitivity analysis I: Individuals (n = 634) on lipid-lowering medication (referring to statins and fibrates) excluded from the analysis
Sensitivity analysis II: High-sensitivity C-reactive protein (hsCRP) was additionally adjusted
Sensitivity analysis III: Change of systolic blood pressure during the follow-up period was additionally adjusted
Discussion
In this cohort study, we identified clusters representing distinct patterns of joint arteriosclerosis and atherosclerosis progression using a group-based multi-trajectory method (see Fig. 1). This method clusters distinct trajectory patterns considering more than one variable and is able to depict the joint progression of intra-correlated measurements. The baPWV measures the arterial stiffness level, and it is closely related with age and other CVD risk factors, while ABI as a noninvasive detection measure is widely used to diagnose peripheral artery disease in clinical practice [42]. We chose the optimal number (set as 3) of distinct groups and trajectory shape parameters (set as 2) based on BIC and AIC and identified three trajectory groups following distinct patterns of joint baPWV and ABI changes during a 10-years follow-up (all fitted p value < 0.001). Group 1 was characterized by stable baPWV and ABI, while group 2 showed a stable ABI but a steeper increase of baPWV, and group 3 had a strong increase of baPWV up to 2000 cm/s along with a decreasing ABI. Individuals with unfavorable joint changes of baPWV and ABI had higher blood pressure, BMI, triglycerides, hsCRP, and lower HDL-C and were more likely to suffer from diabetes. Combining the two indicators for trajectory analysis could identify high-risk groups of CVD and improve the early primary prevention of CVD.
We found that higher RC was significantly associated with the joint and separate arteriosclerosis and atherosclerosis progressions measured by baPWV and ABI after adjusting for traditional confounding factors and LDL-C. In addition, discordance analyses revealed that increased RC level differentiates individuals at a higher risk of arteriosclerosis and atherosclerosis progression, even in people with an optimal LDL-C level. Our findings are consistent with most previous studies. A longitudinal study reported that higher levels of RC, but not LDL-C, were associated with major adverse cardiovascular events independent of other risk factors among overweight or obese subjects at high cardiovascular risk [17]. Similar findings were observed that RC could predict atherosclerotic CVD beyond LDL-C [26]. Our study supplemented the evidence about RC and subclinical indicators of CVD risk in the general population. We found that RC, rather than LDL-C, was significantly associated with the 10-year joint progression of arteriosclerosis and atherosclerosis. Only two cross-sectional studies reported that RC was associated with higher baPWV alone [7, 29]. Our founding extended the data on the longitudinal association between RC and arterial stiffness. A Copenhagen study found that higher level of RC at baseline increased the risk of incident peripheral arterial disease [27]. Our study fitted multi-trajectories to describe the 10-year joint progression of arteriosclerosis and peripheral atherosclerosis. We revealed the relationship between RC and the joint progression of baPWV and ABI for the first time from the perspective of early primary prevention of CVD.
In real-world clinical practice, LDL-C is commonly considered as the primary therapy target both in the primary and secondary prevention of adverse CVD [43]. The fact is that after reducing LDL-C to recommended levels, there still exists a considerable residual risk of CVD and adverse outcomes [11]. This residual risk has been partly recognized as a result of the common lipid disorder characterized by high circulating triglycerides and low HDL-C with normal concentrations of LDL-C [44]. However, randomized controlled trials with HDL-C as a therapeutic target reported that the use of HDL-C modifying treatments had no significant effect on CVD [18]. A prospective cohort study among 15.8 million adults found that both low and high levels of HDL-C were associated with increased mortality from CVD, supporting that high HDL-C is not necessarily a sign of optimal cardiovascular health [45]. Thus, recent research focused on TRLs and the embedded cholesterol component [26]. Triglycerides can be easily metabolized in most cells [46]. Thus, it is hypothesized that the harmful component in TRLs is cholesterol rather than triglycerides [46], which was validated in our discordance analyses. Our results revealed that RC plays a key role in the pathological arteriosclerosis and atherosclerosis progression, even in patients with optimal LDL-C levels. In addition, RC yielded greater risk for arteriosclerosis and atherosclerosis progression than triglycerides. Previous study indicated that RC could increase the risk of CVD regardless of LDL-C level through discordance analyses [17, 26]. BaPWV and ABI are two validated predictive factors for CVD, which have potential to be more widely used as early markers of the primary prevention strategies for CVD [47]. Our conclusions extended these prior findings and confirmed the association of RC with joint arteriosclerosis and atherosclerosis progression. Interestingly, we found that the discordant low RC group was associated with decreased risk of arteriosclerosis and atherosclerosis, which may provide a time window for early CVD prevention, even for those with optimal LDL-C levels.
Although the exact mechanisms underlying the association of RC with arteriosclerosis and atherosclerosis still need to be established, several potential biological pathways can be proposed. Like low-density lipoprotein, particles containing RC in the blood flow accumulate through the endodermis and are absorbed by macrophages and smooth muscle cells, forming foam cells, which eventually become part of atherosclerotic plaques [48]. Due to the relatively large size of remnant lipoproteins compared with LDL, RC is more easily trapped and taken up by macrophages than LDL-C, leading to a faster formation of foam cells and arterial damage [49]. Our study also found that RC, not LDL-C, was significantly associated with the joint arteriosclerosis and atherosclerosis progression, indicating the atherogenic effect of RC. In addition, higher RC level was regarded as a risk factor of endothelial dysfunction, which may mediate the progression of arteriosclerosis and atherosclerosis [50]. Finally, genetic evidence indicated that elevated RC was associated with low-grade inflammation, thus promoting the progression of coronary burden, arterial stiffness, and atherosclerosis [20]. Of note, the results remained significant after additionally adjusting for hsCRP in our analysis (see Table 4), which indicated that the underlying mechanism remains to be further clarified.
There has been an increasing clinical interest in RC targeted interventions. Several studies showed that liraglutide, high-dose n-3 fatty acid supplementation, particularly icosapent ethyl and peroxisome proliferator-activated receptor alpha modulators could serve as novel candidates to reduce RC level [25, 51, 52]. However, the reported clinical benefits of RC-lowering therapy were distinct. A recent study suggested that using icosapent ethyl could reduce the concentrations of atherogenic remnant particle-cholesterol and concomitantly lessen the occurrence of certain cardiovascular events independent of statin treatment [51]. Another randomized controlled trial performed in patients with type 2 diabetes found that the incidence of cardiovascular events was not lower among those receiving pemafibrate, although pemafibrate could lower RC levels [53]. Notably, a randomized crossover study in patients of hyperlipidemia, atorvastatin, and simvastatin significantly reduced RC levels in addition to LDL-C. This may be another potential mechanism to explain the cardiovascular benefits from statins [54]. Future research should further explore more RC targeted interventions to slow down the progression of arteriosclerosis and atherosclerosis, thus reducing cardiovascular risk.
Limitations
This cohort design with multiple surveys supplements the evidence about the longitudinal association of RC with joint arteriosclerosis and atherosclerosis progression using an innovative multi-trajectory modeling technique [39, 55]. However, the results should be interpreted in the context of limitations. First, RC concentration was not directly measured but obtained by calculation, which may deviate from the actual level. However, the calculated RC is closely correlated with the directly measured RC and is widely used in population studies [27, 56]. Second, the baPWV measures the stiffness of the elastic aorta and the muscular arteries, but only aortic stiffness is more closely related with CVD risk [57]. However, a meta-analysis showed that the measurement of baPWV could enhance the efficacy of predicting cardiovascular events, which was comparable with the Framingham risk score in 14,673 Japanese participants [58], indicating that baPWV level reflects the CVD risk, especially in the Asian population. In this current study, the cfPWV data were not available, and we were unable to compare the results between baPWV and cfPWV. Third, although we adjusted for some confounding factors, there is still a possibility of residual confounding bias. For example, the data of fish oil supplement were not collected in this study, which could have an effect on the RC level. Finally, the observed results require further validation in other populations.
Conclusions
This longitudinal study indicated that RC is an early risk factor of the joint arteriosclerosis and atherosclerosis progressions independent of LDL-C in the general population, providing new evidence on the necessity of monitoring RC for promoting cardiovascular health. RC may serve as a potential prevention and intervention target of arteriosclerosis and atherosclerosis, even in people with an optimal LDL-C level.
Supplementary Information
Additional file 1: Table S1. Baseline characteristics in male and female. Table S2. Diagnostic criteria for choosing the group number and shape parameter of the final multi-trajectory model. Table S3. Lipid component levels in the matched multi-trajectory groups. Table S4. Partial correlation matrix of lipid profiles and vascular measures adjusted for age and sex. Table S5. Full regression results of associations of remnant cholesterol and covariates with arteriosclerosis and atherosclerosis progression. Table S6. Associations of lipid profiles with separate baPWV and ABI trajectories. Table S7. Risk for arteriosclerosis and atherosclerosis progression according to the median and individualized cutpoints across LDL-C and remnant cholesterol. Table S8. Subgroup analysis of associations between remnant cholesterol level and arteriosclerosis and atherosclerosis progression in terms of age, sex, BMI, hypertension and diabetes. Table S9. Associations of alternative remnant cholesterol with arteriosclerosis and atherosclerosis progression beyond LDL-C.
Additional file 2: Fig. S1. Proportions of concordance/discordance among individuals according to LDL-C clinical cutpoints. Fig. S2. Progression trajectories of separate baPWV and ABI. Fig. S3. The scatter plots between remnant cholesterol and LDL cholesterol stratified by age and sex.
Acknowledgements
We thank all the staff and participants of the Beijing Health Management Cohort for their invaluable contributions.
Abbreviations
- RC
Remnant cholesterol
- CVD
Cardiovascular disease
- BHMC
Beijing Health Management Cohort
- baPWV
Brachial-ankle pulse wave velocity
- ABI
Ankle brachial index
- LDL-C
Low density lipoprotein cholesterol
- TRLs
Triglyceride-rich lipoproteins
- IDL
Intermediate density lipoprotein
- VLDL
Very low density lipoprotein
- hsCRP
High-sensitivity C-reactive protein
- cIMT
Carotid intima-media thickness
Authors’ contributions
WW, XHG, and LXT had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: XHG, WW, and LXT; acquisition, analysis, or interpretation of the data: XLM, YL, HYP, ZH, XPK, ZWL, and XL; drafting of the manuscript: ZYW, JQW, and HPZ; critical revision of the manuscript for important intellectual content: ZYW, WW, XHG, and LXT. The authors read and approved the final manuscript.
Funding
Our work was funded by the National Natural Science Foundation of China (numbers: 81872708 and 82073668 to Lixin Tao) and the China Scholarship Council (number: 201908110447 to Zhiyuan Wu). The funding sources had no role in the study design, data collection, analysis and interpretation of the data, writing of the report, and in the decision to submit the paper for publication.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author (Wei Wang, Lixin Tao and Xiuhua Guo) on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committees of Capital Medical University (grant number: 2020SY031) and Edith Cowan University (grant number: 2021-03164-WU). All participants gave informed consent to participate before taking part.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhiyuan Wu and Jinqi Wang are first co-authors.
Zhiyuan Wu and Jinqi Wang analyzed the data and drafted the manuscript together.
Contributor Information
Jinqi Wang, Email: wangjinqi@ccmu.edu.cn.
Haiping Zhang, Email: yeszhang09@163.com.
Huiying Pan, Email: panhuiying526@163.com.
Zhiwei Li, Email: 15128472546@163.com.
Yue Liu, Email: mugglesblue@163.com.
Xinlei Miao, Email: miaoxinlei1030@163.com.
Ze Han, Email: hz18843113362@163.com.
Xiaoping Kang, Email: kanspin910@126.com.
Xia Li, Email: wuxiaozhi@ccmu.edu.cn, Email: x.li2@latrobe.edu.au.
Xiuhua Guo, Email: statguo@ccmu.edu.cn.
Lixin Tao, Email: taolixin@ccmu.edu.cn.
Wei Wang, Email: wei.wang@ecu.edu.au.
References
- 1.Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–212. doi: 10.1038/s41569-018-0119-4. [DOI] [PubMed] [Google Scholar]
- 2.Wilson J, Webb AJS. Systolic blood pressure and longitudinal progression of arterial stiffness: a quantitative meta-analysis. J Am Heart Assoc. 2020;9(17):e017804. doi: 10.1161/JAHA.120.017804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z, Zhou D, Liu Y, Li Z, Wang J, Han Z, Miao X, Liu X, Li X, Wang W, et al. Association of TyG index and TG/HDL-C ratio with arterial stiffness progression in a non-normotensive population. Cardiovasc Diabetol. 2021;20(1):134. doi: 10.1186/s12933-021-01330-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu S, Xu L, Wu M, Chen S, Wang Y, Tian Y. Association between triglyceride-glucose index and risk of arterial stiffness: a cohort study. Cardiovasc Diabetol. 2021;20(1):146. doi: 10.1186/s12933-021-01342-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun D, Liu Y, Zhang J, Liu J, Wu Z, Liu M, Li X, Guo X, Tao L. Long-term effects of fine particulate matter exposure on the progression of arterial stiffness. Environ Health. 2021;20(1):2. doi: 10.1186/s12940-020-00688-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kinjo Y, Ishida A, Kinjo K, Ohya Y. A high normal ankle-brachial index combined with a high pulse wave velocity is associated with cerebral microbleeds. J Hypertens. 2016;34(8):1586–1593. doi: 10.1097/HJH.0000000000000993. [DOI] [PubMed] [Google Scholar]
- 7.Wang Z, Li M, Xie J, Gong J, Liu N. Association between remnant cholesterol and arterial stiffness: a secondary analysis based on a cross-sectional study. J Clin Hypertens (Greenwich) 2022;24(1):26–37. doi: 10.1111/jch.14384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsu PC, Lee WH, Tsai WC, Chen YC, Chu CY, Yen HW, Lin TH, Voon WC, Lai WT, Sheu SH, et al. Comparison between estimated and brachial-ankle pulse wave velocity for cardiovascular and overall mortality prediction. J Clin Hypertens (Greenwich) 2021;23(1):106–113. doi: 10.1111/jch.14124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhan B, Huang X, Wang J, Qin X, Zhang J, Cao J, Song Y, Liu L, Li P, Yang R, et al. Association between lipid profiles and arterial stiffness in Chinese patients with hypertension: insights from the CSPPT. Angiology. 2019;70(6):515–522. doi: 10.1177/0003319718823341. [DOI] [PubMed] [Google Scholar]
- 10.Wen J, Huang Y, Lu Y, Yuan H. Associations of non-high-density lipoprotein cholesterol, triglycerides and the total cholesterol/HDL-c ratio with arterial stiffness independent of low-density lipoprotein cholesterol in a Chinese population. Hypertens Res. 2019;42(8):1223–1230. doi: 10.1038/s41440-019-0251-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sekizuka H, Hoshide S, Kabutoya T, Kario K. Determining the relationship between triglycerides and arterial stiffness in cardiovascular risk patients without low-density lipoprotein cholesterol-lowering therapy. Int Heart J. 2021;62(6):1320–1327. doi: 10.1536/ihj.21-309. [DOI] [PubMed] [Google Scholar]
- 12.Hartz J, Krauss RM, Göttsater M, Melander O, Nilsson P, Mietus-Snyder M. Lipoprotein particle predictors of arterial stiffness after 17 years of follow up: the Malmö Diet and Cancer Study. Int J Vasc Med. 2020;2020:4219180. doi: 10.1155/2020/4219180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stone NJ, Robinson JG, Lichtenstein AH, BaireyMerz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–2934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, Simes J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sandesara PB, Virani SS, Fazio S, Shapiro MD. The forgotten lipids: triglycerides, remnant cholesterol, and atherosclerotic cardiovascular disease risk. Endocr Rev. 2019;40(2):537–557. doi: 10.1210/er.2018-00184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoogeveen RC, Ballantyne CM. Residual cardiovascular risk at low LDL: remnants, lipoprotein(a), and inflammation. Clin Chem. 2021;67(1):143–153. doi: 10.1093/clinchem/hvaa252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castañer O, Pintó X, Subirana I, Amor AJ, Ros E, Hernáez Á, Martínez-González M, Corella D, Salas-Salvadó J, Estruch R, et al. Remnant cholesterol, not LDL cholesterol, is associated with incident cardiovascular disease. J Am Coll Cardiol. 2020;76(23):2712–2724. doi: 10.1016/j.jacc.2020.10.008. [DOI] [PubMed] [Google Scholar]
- 18.Riaz H, Khan SU, Rahman H, Shah NP, Kaluski E, Lincoff AM, Nissen SE. Effects of high-density lipoprotein targeting treatments on cardiovascular outcomes: a systematic review and meta-analysis. Eur J Prev Cardiol. 2019;26(5):533–543. doi: 10.1177/2047487318816495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Varbo A, Nordestgaard BG. Remnant lipoproteins. Curr Opin Lipidol. 2017;28(4):300–307. doi: 10.1097/MOL.0000000000000429. [DOI] [PubMed] [Google Scholar]
- 20.Varbo A, Benn M, Tybjærg-Hansen A, Nordestgaard BG. Elevated remnant cholesterol causes both low-grade inflammation and ischemic heart disease, whereas elevated low-density lipoprotein cholesterol causes ischemic heart disease without inflammation. Circulation. 2013;128(12):1298–1309. doi: 10.1161/CIRCULATIONAHA.113.003008. [DOI] [PubMed] [Google Scholar]
- 21.Twickler TB, Dallinga-Thie GM, Cohn JS, Chapman MJ. Elevated remnant-like particle cholesterol concentration: a characteristic feature of the atherogenic lipoprotein phenotype. Circulation. 2004;109(16):1918–1925. doi: 10.1161/01.CIR.0000125278.58527.F3. [DOI] [PubMed] [Google Scholar]
- 22.Kaltoft M, Langsted A, Nordestgaard BG. Triglycerides and remnant cholesterol associated with risk of aortic valve stenosis: Mendelian randomization in the Copenhagen General Population Study. Eur Heart J. 2020;41(24):2288–2299. doi: 10.1093/eurheartj/ehaa172. [DOI] [PubMed] [Google Scholar]
- 23.Varbo A, Benn M, Tybjærg-Hansen A, Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013;61(4):427–436. doi: 10.1016/j.jacc.2012.08.1026. [DOI] [PubMed] [Google Scholar]
- 24.Yu D, Wang Z, Zhang X, Qu B, Cai Y, Ma S, Zhao Z, Simmons D. Remnant cholesterol and cardiovascular mortality in patients with type 2 diabetes and incident diabetic nephropathy. J Clin Endocrinol Metab. 2021;106(12):3546–3554. doi: 10.1210/clinem/dgab533. [DOI] [PubMed] [Google Scholar]
- 25.Cao YX, Zhang HW, Jin JL, Liu HH, Zhang Y, Gao Y, Guo YL, Wu NQ, Hua Q, Li YF, et al. The longitudinal association of remnant cholesterol with cardiovascular outcomes in patients with diabetes and pre-diabetes. Cardiovasc Diabetol. 2020;19(1):104. doi: 10.1186/s12933-020-01076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quispe R, Martin SS, Michos ED, Lamba I, Blumenthal RS, Saeed A, Lima J, Puri R, Nomura S, Tsai M, et al. Remnant cholesterol predicts cardiovascular disease beyond LDL and ApoB: a primary prevention study. Eur Heart J. 2021;42(42):4324–4332. doi: 10.1093/eurheartj/ehab432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wadström BN, Wulff AB, Pedersen KM, Jensen GB, Nordestgaard BG: Elevated remnant cholesterol increases the risk of peripheral artery disease, myocardial infarction, and ischaemic stroke: a cohort-based study. Eur Heart J 2021. [DOI] [PubMed]
- 28.Varbo A, Nordestgaard BG. Remnant cholesterol and risk of ischemic stroke in 112,512 individuals from the general population. Ann Neurol. 2019;85(4):550–559. doi: 10.1002/ana.25432. [DOI] [PubMed] [Google Scholar]
- 29.Liu J, Fan F, Liu B, Li K, Jiang Y, Jia J, Chen C, Zheng B, Zhang Y. Association between remnant cholesterol and arterial stiffness in a Chinese community-based population: a cross-sectional study. Front Cardiovasc Med. 2022;9:993097. doi: 10.3389/fcvm.2022.993097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Faridi KF, Quispe R, Martin SS, Hendrani AD, Joshi PH, Brinton EA, Cruz DE, Banach M, Toth PP, Kulkarni K, et al. Comparing different assessments of remnant lipoprotein cholesterol: the very large database of lipids. J Clin Lipidol. 2019;13(4):634–644. doi: 10.1016/j.jacl.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 31.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):e285–e350. doi: 10.1016/j.jacc.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 32.Quispe R, Elshazly MB, Zhao D, Toth PP, Puri R, Virani SS, Blumenthal RS, Martin SS, Jones SR, Michos ED. Total cholesterol/HDL-cholesterol ratio discordance with LDL-cholesterol and non-HDL-cholesterol and incidence of atherosclerotic cardiovascular disease in primary prevention: the ARIC study. Eur J Prev Cardiol. 2020;27(15):1597–1605. doi: 10.1177/2047487319862401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mora S, Buring JE, Ridker PM. Discordance of low-density lipoprotein (LDL) cholesterol with alternative LDL-related measures and future coronary events. Circulation. 2014;129(5):553–561. doi: 10.1161/CIRCULATIONAHA.113.005873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, Koji Y, Hori S, Yamamoto Y. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res. 2002;25(3):359–364. doi: 10.1291/hypres.25.359. [DOI] [PubMed] [Google Scholar]
- 35.Collins TC, Ewing SK, Diem SJ, Taylor BC, Orwoll ES, Cummings SR, Strotmeyer ES, Ensrud KE. Peripheral arterial disease is associated with higher rates of hip bone loss and increased fracture risk in older men. Circulation. 2009;119(17):2305–2312. doi: 10.1161/CIRCULATIONAHA.108.820993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.He W, Li Q, Yang M, Jiao J, Ma X, Zhou Y, Song A, Heymsfield SB, Zhang S, Zhu S. Lower BMI cutoffs to define overweight and obesity in China. Obesity (Silver Spring) 2015;23(3):684–691. doi: 10.1002/oby.20995. [DOI] [PubMed] [Google Scholar]
- 37.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. Jama. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 38.Standards of Medical Care in Diabetes-2020 Abridged for Primary Care Providers. Clin Diabetes 2020, 38(1):10-38. [DOI] [PMC free article] [PubMed]
- 39.Nagin DS, Jones BL, Passos VL, Tremblay RE. Group-based multi-trajectory modeling. Stat Methods Med Res. 2018;27(7):2015–2023. doi: 10.1177/0962280216673085. [DOI] [PubMed] [Google Scholar]
- 40.Bui DS, Lodge CJ, Burgess JA, Lowe AJ, Perret J, Bui MQ, Bowatte G, Gurrin L, Johns DP, Thompson BR, et al. Childhood predictors of lung function trajectories and future COPD risk: a prospective cohort study from the first to the sixth decade of life. Lancet Respir Med. 2018;6(7):535–544. doi: 10.1016/S2213-2600(18)30100-0. [DOI] [PubMed] [Google Scholar]
- 41.Li H, Li C, Wang A, Qi Y, Feng W, Hou C, Tao L, Liu X, Li X, Wang W, et al. Associations between social and intellectual activities with cognitive trajectories in Chinese middle-aged and older adults: a nationally representative cohort study. Alzheimers Res Ther. 2020;12(1):115. doi: 10.1186/s13195-020-00691-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK, Golzarian J, Gornik HL, Halperin JL, Jaff MR, et al. 2011 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Peripheral Artery Disease (updating the 2005 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2011;58(19):2020–2045. doi: 10.1016/j.jacc.2011.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082–e1143. doi: 10.1161/CIR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sirimarco G, Labreuche J, Bruckert E, Goldstein LB, Fox KM, Rothwell PM, Amarenco P. Atherogenic dyslipidemia and residual cardiovascular risk in statin-treated patients. Stroke. 2014;45(5):1429–1436. doi: 10.1161/STROKEAHA.113.004229. [DOI] [PubMed] [Google Scholar]
- 45.Yi SW, Park HB, Jung MH, Yi JJ, Ohrr H. High-density lipoprotein cholesterol and cardiovascular mortality: a prospective cohort study among 15.8 million adults. Eur J Prev Cardiol. 2022;29(5):844–854. doi: 10.1093/eurjpc/zwab230. [DOI] [PubMed] [Google Scholar]
- 46.Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. 2014;384(9943):626–635. doi: 10.1016/S0140-6736(14)61177-6. [DOI] [PubMed] [Google Scholar]
- 47.Maeda Y, Inoguchi T, Etoh E, Kodama Y, Sasaki S, Sonoda N, Nawata H, Shimabukuro M, Takayanagi R. Brachial-ankle pulse wave velocity predicts all-cause mortality and cardiovascular events in patients with diabetes: the Kyushu Prevention Study of Atherosclerosis. Diabetes Care. 2014;37(8):2383–2390. doi: 10.2337/dc13-1886. [DOI] [PubMed] [Google Scholar]
- 48.Nordestgaard BG. Triglyceride-rich lipoproteins and atherosclerotic cardiovascular disease: new insights from epidemiology, genetics, and biology. Circ Res. 2016;118(4):547–563. doi: 10.1161/CIRCRESAHA.115.306249. [DOI] [PubMed] [Google Scholar]
- 49.Miller YI, Choi SH, Fang L, Tsimikas S. Lipoprotein modification and macrophage uptake: role of pathologic cholesterol transport in atherogenesis. Subcell Biochem. 2010;51:229–251. doi: 10.1007/978-90-481-8622-8_8. [DOI] [PubMed] [Google Scholar]
- 50.Nakamura T, Takano H, Umetani K, Kawabata K, Obata JE, Kitta Y, Kodama Y, Mende A, Ichigi Y, Fujioka D, et al. Remnant lipoproteinemia is a risk factor for endothelial vasomotor dysfunction and coronary artery disease in metabolic syndrome. Atherosclerosis. 2005;181(2):321–327. doi: 10.1016/j.atherosclerosis.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 51.Chapman MJ, Zamorano JL, Parhofer KG. Reducing residual cardiovascular risk in Europe: therapeutic implications of European medicines agency approval of icosapent ethyl/eicosapentaenoic acid. Pharmacol Ther. 2022;237:108172. doi: 10.1016/j.pharmthera.2022.108172. [DOI] [PubMed] [Google Scholar]
- 52.Peradze N, Farr OM, Perakakis N, Lázaro I, Sala-Vila A, Mantzoros CS. Short-term treatment with high dose liraglutide improves lipid and lipoprotein profile and changes hormonal mediators of lipid metabolism in obese patients with no overt type 2 diabetes mellitus: a randomized, placebo-controlled, cross-over, double-blind clinical trial. Cardiovasc Diabetol. 2019;18(1):141. doi: 10.1186/s12933-019-0945-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Das Pradhan A, Glynn RJ, Fruchart JC, MacFadyen JG, Zaharris ES, Everett BM, Campbell SE, Oshima R, Amarenco P, Blom DJ, et al. Triglyceride lowering with pemafibrate to reduce cardiovascular risk. N Engl J Med. 2022;387(21):1923–1934. doi: 10.1056/NEJMoa2210645. [DOI] [PubMed] [Google Scholar]
- 54.Stein DT, Devaraj S, Balis D, Adams-Huet B, Jialal I. Effect of statin therapy on remnant lipoprotein cholesterol levels in patients with combined hyperlipidemia. Arterioscler Thromb Vasc Biol. 2001;21(12):2026–2031. doi: 10.1161/hq1201.100259. [DOI] [PubMed] [Google Scholar]
- 55.Koohi F, Khalili D, Mansournia MA, Hadaegh F, Soori H. Multi-trajectories of lipid indices with incident cardiovascular disease, heart failure, and all-cause mortality: 23 years follow-up of two US cohort studies. J Transl Med. 2021;19(1):286. doi: 10.1186/s12967-021-02966-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Varbo A, Nordestgaard BG. Directly measured vs. calculated remnant cholesterol identifies additional overlooked individuals in the general population at higher risk of myocardial infarction. Eur Heart J. 2021;42(47):4833–4843. doi: 10.1093/eurheartj/ehab293. [DOI] [PubMed] [Google Scholar]
- 57.Kim ED, Ballew SH, Tanaka H, Heiss G, Coresh J, Matsushita K. Short-term prognostic impact of arterial stiffness in older adults without prevalent cardiovascular disease. Hypertension. 2019;74(6):1373–1382. doi: 10.1161/HYPERTENSIONAHA.119.13496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ohkuma T, Ninomiya T, Tomiyama H, Kario K, Hoshide S, Kita Y, Inoguchi T, Maeda Y, Kohara K, Tabara Y, et al. Brachial-ankle pulse wave velocity and the risk prediction of cardiovascular disease: an individual participant data meta-analysis. Hypertension. 2017;69(6):1045–1052. doi: 10.1161/HYPERTENSIONAHA.117.09097. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Baseline characteristics in male and female. Table S2. Diagnostic criteria for choosing the group number and shape parameter of the final multi-trajectory model. Table S3. Lipid component levels in the matched multi-trajectory groups. Table S4. Partial correlation matrix of lipid profiles and vascular measures adjusted for age and sex. Table S5. Full regression results of associations of remnant cholesterol and covariates with arteriosclerosis and atherosclerosis progression. Table S6. Associations of lipid profiles with separate baPWV and ABI trajectories. Table S7. Risk for arteriosclerosis and atherosclerosis progression according to the median and individualized cutpoints across LDL-C and remnant cholesterol. Table S8. Subgroup analysis of associations between remnant cholesterol level and arteriosclerosis and atherosclerosis progression in terms of age, sex, BMI, hypertension and diabetes. Table S9. Associations of alternative remnant cholesterol with arteriosclerosis and atherosclerosis progression beyond LDL-C.
Additional file 2: Fig. S1. Proportions of concordance/discordance among individuals according to LDL-C clinical cutpoints. Fig. S2. Progression trajectories of separate baPWV and ABI. Fig. S3. The scatter plots between remnant cholesterol and LDL cholesterol stratified by age and sex.