Summary
Background
The Radiotherapy Expansion Plan for Brazil's Unified Health System (PER-SUS) was an innovative program designed by the Ministry of Health in 2012 to provide improvements to the challenging problem of access to radiotherapy in the country. This study sought to analyze the execution and implementation of installations proposed by PER-SUS, and their capacity to address the problems of radiotherapy access in Brazil.
Methods
From the first release (February 2015) until October 2021, all PER-SUS monthly progress reports were retrospectively analyzed. The beneficiary institutions, project location, project status, project type, dates of the progress on the stages, and reasons for cancellations or possible justifications for changing the status were collected. Brazilian geographic data, health care demands, and cancer incidences were correlated. Finally, we performed an Ishikawa diagram and 5W3H methodology, aiming to better understand the findings and to yield possible ways to improve the access to radiotherapy.
Findings
After ten years, the PER-SUS project delivered nearly 50% of the planned implementation of radiotherapy equipment. There was a 17% growth in the national number of linear accelerators (LINACS) with PER-SUS, against a 32% increase in cancer incidence in Brazil in the same period. The following points were identified: a high rate of beneficiary exclusions reflecting inappropriate selection or inadequate planning; delays in execution related to bureaucratic obstacles and underestimation of the requirements (logistics/people); early closing of the equipment factory as a result of lack of project prioritization by the Government.
Interpretation
Only about 50% of PER-SUS are being carried out. However, delays and exclusions of beneficiaries were observed. The dimension of the need for radiotherapy care in Brazil is greater than considered, and might not be fully attended by PER-SUS. Geographic, epidemiological, logistical, and economic variables could be reevaluated to allow better strategic planning and improvement proposals. PER-SUS could be optimized for the next decade, by involving all stakeholders' participation, alignment, and engagement. In the future, the States and regions with a higher LINAC shortage should be prioritized to improve RT access across the country. Considering the data and the initial project deadline, PER-SUS did not achieve the pre-established goals specified by the Brazilian Government.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Keywords: Radiotherapy, Brazilian public health, Universalization
Research in context.
Evidence before this study
The Brazilian Public Healthcare System (SUS) has been providing universal access to healthcare for cancer patients under several challenging issues, including the increasing cancer incidence over time, geographic and socio-economic drawbacks, and heterogeneity of healthcare access according to region. Moreover, the availability of radiotherapy equipment is below what is necessary to meet both the current and future demands. In attempts to improve access to health and cancer treatments, specifically radiotherapy, some government initiatives have been put into practice, such as the PER-SUS (in Portuguese “Plano de Expansão da Radioterapia no Sistema Único de Saúde”, or Radiotherapy Expansion Plan for SUS). This program was launched in 2012, and little information is available as to the real impact of overcoming the aforementioned problems.
Added value of this study
The following critical points were identified from the results of this study: 1) the high rate of exclusion from institutions reflects inappropriate selection of the institutions or inadequate planning for the project; 2) the delay in execution was related to bureaucratic obstacles, as well as underestimation of the requirements for planning (logistics/people); 3) the audacious PER-SUS dimensioning did not seem to overcome the issue of oncologic care; 4) technological investment does not cover all needs; 5) the output of the teaching/research investment was not evident (no data shown), mainly due to the early closing of the factory of the company chosen to supply the PER-SUS equipment, and professional training; and 6) the closing of the equipment factory was also a consequence of inadequate planning and lack of project “protection” by the government.
Implications of all the available evidence
We believe our study makes a significant contribution to the literature because, as the findings suggest, PER-SUS can be optimized for the next decade by involving all stakeholders in participation, alignment, and engagement. Further, based on the joint data from the Brazilian Federal Court of Accounts (TCU) audit report (2018) and the Brazilian Society of Radiotherapy document published in partnership with the Dom Cabral Foundation (RT2030), radiotherapy treatment in the context of cancers is of great importance, especially in an ageing population where the prevalence of these diseases will be increasing. Therefore, the challenge of access to radiotherapy should be addressed.
Alt-text: Unlabelled box
Introduction
Brazil is a country with continental dimensions, and despite some underestimation, its cancer statistics replicate the global trend: a linear increase in the number of various types of cancer and consolidation of the most prevalent tumors in the adult population. In men, prostate, colorectal, and lung tumors account for more than 45% of the total estimated cases in 2020; in women, breast, colorectal, and cervical tumors were responsible for more than 45% of cases in 2020.1 These numbers are just the tip of the iceberg; with an increasing number of cancer cases, the treatment becomes more complex and the lack of access to healthcare is more challenging.
According to the World Health Organization (WHO), the ideal quantity and distribution of radiotherapy equipment or linear accelerator (LINAC) is one machine for every 250,000 to 300,000 people. It is also acknowledged that one machine can treat 600 patients per year.2 Additionally, the proportion of cancer patients who will need radiotherapy treatment at some point in their natural history is 60%.3 Furthermore, the epidemiological distribution of cancer cases and the ageing of the population may further increase this proportion. Thus, from the 686,000 estimated cancer cases in Brazil in 2020, the approximately 412,000 that will need radiotherapy will require 680 LINACs, Supplementary Table 1. However, in 2014, only 269 machines were available for Brazil's Unified Health System (Sistema Único de Saúde - SUS); implying 62% of the required capacity. However, only 145,000 (56% of the total SUS patients) could complete their radiation treatments by the end of 2015.4 Due to the lack of access to radiotherapy, approximately 5,000 patients died in 2016. These numbers were based on Brazilian national data considering only five cancer sites (lung, prostate, breast, cervical, and colorectal cancers).5
According to a national survey, in 2014, there were 128, 48, 35, 12, and 35 dedicated LINACs in the southeast, south, midwest, north, and northeast regions, respectively.4 In contrast, data from the Brazilian Institute of Geography and Statistics (IBGE) show that patients travel an average of 72 km from their homes to access radiotherapy services.6 Another challenge unique to cancer care and its three main specialities (surgery, systemic therapy, and radiotherapy) may be related to the disproportionate allocation of government expenditures for oncology. Data from the Ministry of Health showed that, in 2016, more than 360 million dollars were allocated to clinical oncology, 160 million to oncology surgery, and 90 million to radiation-oncology.7
Moreover, the Brazilian Federal Court of Accounts (TCU) reported that both authorization and waiting times for radiotherapy were classified as long or excessively long, in about 80% of SUS users. Less than 18% of treatments start within 30 days in Brazil, compared to 100% in Canada and 97% in the United Kingdom.8
In some attempts to improve these processes and overcome the high demand for assistance, the government launched, in 2012, Law #12732, also known as “the 60-day Law”, which required the start of cancer treatment in the SUS within a 60-day maximum period. This law was amended in 2019 to include a deadline for the initial workup (examinations and diagnosis) of up to 30 days from cancer diagnosis and initial registration.9
In May 2012, the government announced the largest public purchase of radiotherapy equipment worldwide, at that time, with the acquisition of 80 radiotherapy solutions, the implementation of a LINAC national plant, and a professional development training hub. The PER-SUS (in Portuguese: “Plano de Expansao da Radioterapia no Sistema Unico de Saúde” or Radiotherapy Expansion Plan for the Brazilian Public Healthcare System), was an audacious and innovative program that was supposedly well-designed to respect the geographic distribution and demands. In addition, it considered competition, including the submission of bids by interested companies, with policies to lower prices, reduce bureaucracy, and improve educational planning. Investments would add up to more than 110 million dollars; 32 million in equipment, projects, and inspection; and 77 million to develop radiotherapy centres. The details of this program include facility requirements, staffing, and training demands. It is important to note that much of the viability of PER-SUS was based on an essential premise: in 2012, there was a change in internal laws involving large public purchases, with financial compensation in exchange for technology transfer and professional training/qualification.
Given the magnitude of the problem of access to radiotherapy and the expected improvements with PER-SUS, we sought to analyze the execution and implementation of radiotherapy equipment and installations proposed by PER-SUS to beneficiary institutions and their capacity to address the problems of radiotherapy access in Brazil.
Methods
In this study, 77 PER-SUS monthly progress reports were retrospectively analyzed. All included documents are publicly available on the Brazilian Ministry of Health website (https://www.gov.br/saude/pt-br/acesso-a-informacao/acoes-e-programas/plano-de-expansao-da-radioterapia-no-sus) and provide data between february 2012 and october 2021. The following information was collected: names of the beneficiary institutions, project location, project status, project type, dates of the progress on the stages, and reasons for cancellations or possible justifications for changing the status.
Furthermore, Brazilian geographical data, health care demands, and cancer incidences were extracted from Brazilian databases, including estimates from the Brazilian National Cancer Institute, the Brazilian Institute of Geography and Statistics, in addition to information obtained from the Brazilian Ministry of Health website.
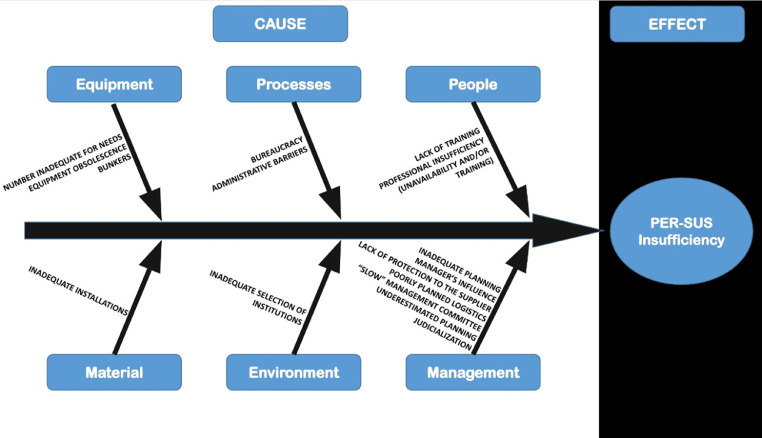
Demographic analysis, descriptive statistics, and distribution of the main variables were performed to correlate the findings. Thus, we performed a root cause analysis10 (Ishikawa diagram) and developed a checklist of actions and activities to be implemented. These were carried out by identifying and prioritizing key problems, using the 5W3H methodology, to develop a map of the situation, in support of the question to be answered by this research.
Results
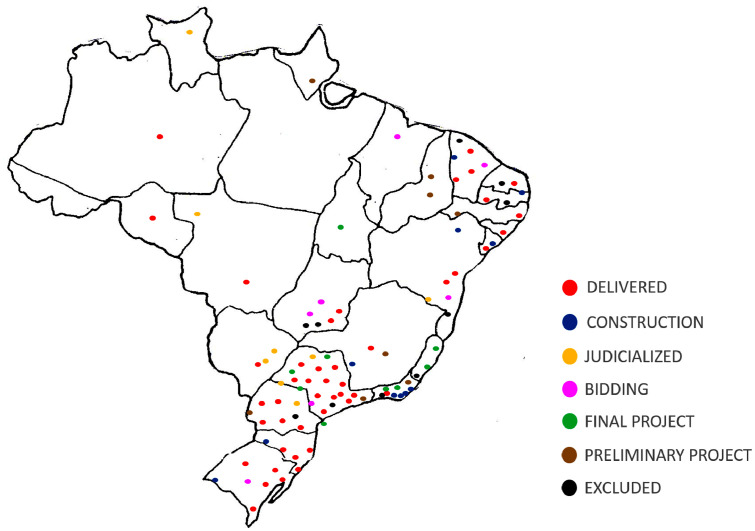
The PER-SUS project progress reports were made available on its website11 in February 2015 and updated monthly until November 2021, summing up a total of 77 documents. It is possible to determine the status of each accredited institution and the expenses. Table 1 illustrates an annual overview of the status of radiotherapy facility implantations in each beneficiary institution. Figure 1 illustrates the status of the main projects in November 2021, distributed over the Brazilian map.
Table 1.
PER-SUS project execution condition according to the year.
| Year | Documentation# | Project# | Bidding# | Construction* | Stopped construction# | Judicialized# | Delivered Projects# |
Excluded* | Total Information Available/Year | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RT expansion | New RT center | Obsolete LINAC | Empty bunker | |||||||||
| 2015 | 49 | 8 | 7 | 4 | 0 | 2 | 12 | 82 | ||||
| 2016 | 28 | 15 | 10 | 11 | 0 | 1 | 1 | 15 | 81 | |||
| 2017 | 13 | 27 | 3 | 11 | 2 | 1 | 4 | 20 | 81 | |||
| 2018 | 4 | 11 | 3 | 32 | 0 | 1 | 3 | 21 | 75 | |||
| 2019 | 7 | 15 | 10 | 26 | 9 | 1 | 10 | 24 | 113 | |||
| 2020 | 0 | 8 | 5 | 26 | 0 | 11 | 5 | 3 | 1 | 2 | 29 | 97 |
| 2021 | 0 | 10 | 5 | 14 | 0 | 11 | 3 | 8 | 4 | 5 | 29 | 89 |
Abbreviations: PER-SUS = Radiotherapy Expansion Plan for the Brazilian's Public Healthcare System; RT = radiotherapy; LINAC = linear accelerator; * Cumulative data; # Non-Cumulative data.
Footnotes: Documentation, Center in document preparation or analysis to join PER-SUS; Project, basic or executive project development; Bidding, construction BID; Stop works, construction work interrupted; Judicialized, construction stopped and waiting for judicial resolution; RT expansion, the addition of a linac to an existing RT center; New RT center, new RT center with a linac (with or without brachytherapy); Obsolete Linac, existing RT center replaced an obsolete linac for a new one; Empty bunker, institutions with an already constructed and empty treatment room receiving a linac; Excluded; centers that left PER-SUS voluntary or that were excluded.
Figure 1.
PER-SUS status in November 2021.
Abbreviation: PER-SUS = Radiotherapy Expansion Plan for the Brazilian's Public Healthcare System.
Subtracting the number of institutions whose projects were excluded from PER-SUS, the final number of equipment (if all the RT solutions were concluded) would be favorably higher in all Brazilian regions when comparing 2018 with the after PER-SUS period. It would have increased 33% (from 15 to 20 LINACS) in the Midwest region, 31% (from 70 to 92 machines) in the Northeast, 27% (from 22 to 28 LINACS) in the North region, 24% (from 79 to 98 equipment) in the South region, and 15% (from 219 to 251) in the Southeast region.
Compared to the initial 2015 project deadline,14 only approximately 50% of the expected LINACS have the license to treat cancer patients after ten years. These 44 new LINACS, as per the December 2021 PER-SUS report, represent an increase of 17% in the SUS national radiotherapy capacity. In contrast, since the introduction of the PER-SUS project, cancer incidence in Brazil increased by 32%, from 518,510 cases in 2012 to 685,960 cases in 2022.12,13 Furthermore, the rate of conclusion for each project type was: 78% (25 of 32) for the radiotherapy expansion projects, 19% (9 of 48) for the new RT centres, 50% (5 of 10) for the centres with an empty bunker, and 50% (5 of 10) for the RT sites with an obsolete LINAC.14
Our analysis identified several reasons for project delay or exclusion from the program: works halted due to inventory error (one site), judicialization (11 institutions), logistics and lack of professional availability (24 locations). Five centers requested to leave the project, while others were excluded due to contract termination (four sites) or following suggestions from the management committee (10 locations).
Bureaucratic issues
In a simple timeline, the PER-SUS processes involved the publication of an ordinance, 931/2012, and the start of activities including hospital selection criteria and selection, local management agreement, signatures of hospital adhesion terms, trading floor, development of basic and executive plans, construction bids, construction, implementation, and licensing of equipment, in selected locations.
As an illustration, the city of Campina Grande (Paraiba State) was the first location to benefit from this program. Its adhesion was consolidated in November 2012, and the operating license was approved precisely four years later. For this purpose, investments reached 1 million dollars; 500,000 dollars for construction; 450,000 dollars for equipment; 3.5 thousand dollars for the project; and 25,000 dollars for inspection.
The biggest challenges relating to the high exclusion rate of institutions were logistical problems (also during the administrative and bidding stages). For example, even though the equipment arrived with its documentation, from that point on, the following challenges were triggered: (1) The construction authorization was denied when the construction budget was greater than the equipment cost. (2) Contractors that did not honor the construction schedule, resulting in a new bid, causing delays due to new documentation, with new contracts with different service providers. (3) Changes to previously approved projects. (4) Organizational changes in institutions. (5) Decreased priority level of resources for the Ministry of Health in 2016.
It is important to highlight that, at that time (2016), attempts were made to reduce the bureaucracy and streamline processes involving PER-SUS, such as hiring both the TCU and Brazilian General Controllership (CGU) audits. This was to qualify the companies involved, package the proposals both for the bidding and works, and also include packages of the proposed services within the bidding process, under the supervision of the designated company. By 2017, more than 24 institutions were already excluded; thus, these sites had to be replaced by others. In 2018, institutions with previously available bunkers, and institutions eligible to exchange obsolete equipment became qualified for the PER-SUS project. This strategy changed the “80 deliveries” goal to 100 solutions. Unfortunately, the practical ramifications of this expansion of PER-SUS revealed further delays in the work in progress.
The choice of equipment supplier company required about 2-year from the signing of the ordinance and the signing of the contract with the designated company, in December 2013. In mid-2017, the plant in Jundiaí (São Paulo State) and a professional training centre in radiotherapy were launched. However, in September 2021, in a public statement, the company decided to terminate their services. The official allegations were related to two issues: the decree that allowed for a margin of preference for domestic products was revoked, and, more recently, the sanction of the law that proposed the reduction of taxes on imported products.
The joint data from the TCU audit report (2018) and the Brazilian Society of Radiotherapy document published in partnership with the Dom Cabral Foundation (RT203015) suggests an exponential increase in the predicted number of cases of cancer in the succeeding years, as well as the demand for radiotherapy for these patients. Table 2 illustrates the status of available equipment for the SUS in Brazil in 2018, the estimated additions of PER-SUS, and the estimated numbers of cancer cases in 2018, 2020, and 2030. It is noteworthy that despite the additional equipment from PER-SUS, available equipment will hardly be adequate to address the treatment needs; according to the WHO, 600 patients per year per machine are recommended.
Table 2.
Overview of the distribution of linear accelerators available to SUS in 2018, the corresponding data extracted from the RT2030 report and the TCU audit forecasting the 2020 and 2030 estimates of cancer cases that are candidates for radiotherapy.
| Equipment in 2018 (SUS) | Estimated addition with PER-SUS (October 2021) | Patient estimates in radiotherapy 2020 | Patient estimates in radiotherapy 2030 | |
|---|---|---|---|---|
| Midwest | 15 | 5 | 17,621 | 24,637 |
| Northeast | 64 | 22 | 62,397 | 80,475 |
| North | 20 | 6 | 15,585 | 21,959 |
| Southeast | 217 | 32 | 1,16,200 | 1,52,448 |
| South | 79 | 19 | 40,480 | 53,278 |
Abbreviation: TCU = Brazilian Federal Court of Accounts.
In addition, it is important to note that radiotherapy machines have a variable lifespan between 10 and 15 years. Despite the inclusion of new sites covered by PER-SUS in 2018, including places with obsolete equipment to be replaced, the problem of obsolescence of equipment throughout Brazil will become impactful in the short term. Data from the Ministry of Health16 predict a significant and worrying increase in the number of obsolete equipment for 2022, as shown in Table 3.9,12
Table 3.
Projection of the number of linear accelerators (LINACS) in 2018 and 2022, using the obsolescence calculation, and categorized according to their availability for the SUS and supplementary sector.
| Brazilian Census 2018 | Total LINACS in 2018 | Obsolete LINACS in 2018 |
Obsolete LINACS in 2022 |
||
|---|---|---|---|---|---|
| N | % Total | N | % Total | ||
| Total LINACS SUS | 252 | 95 | 37.7% | 127 | 50.4% |
| Total LINACS private sector | 111 | 27 | 24.3% | 35 | 31.5% |
| Total LINACS Brazil | 363 | 122 | 33.6% | 162 | 44.6% |
In addition, according to the 2018 Radiotherapy census data and RT2030 reports, the proportion of equipment that must be replaced in the next 10 years presents a worrying value of 52%, and 29 25 years-old machines are still in operation in Brazil (Tables 4 and 5). The north region had the highest percentage (68%).
Table 4.
Obsolescence of linear accelerators in Brazil.
| Equipment that should be replaced in 10 years | |
|---|---|
| North | 68% |
| Northeast | 53% |
| Midwest | 44% |
| Southeast | 43% |
| Capital SP | 49% |
| Interior SP | 56% |
| South | 57% |
| Brazil consolidated | 52% |
Abbreviation: SP = Sao Paulo (State).
Table 5.
Age of radiotherapy equipment in Brazil (2019 data).
| Date of manufacture of equipment in use in 2019 | |
|---|---|
| Until 1990 | 16 |
| 1990–1995 | 13 |
| 1996–2000 | 37 |
| 2001–2005 | 45 |
| 2006–2010 | 101 |
| 2011–2015 | 117 |
| 2016 | 18 |
| 2017 | 25 |
| 2018 | 24 |
| 2019 | 7 |
| Missing information | 6 |
| Overall, in Brazil | 409 |
The data in Table 6 was obtained from the RT2030 report and emphasized the projection for the next decade. There is still a lot of room for improvement in the provision of cancer care/radiotherapy. If the only problem needing to be overcome to address the demand for radiotherapy care in Brazil is the lack of equipment as more than 300 equipment facilities would still be required to meet the radiotherapy treatment needs for patients who are dependent on the SUS.12,17
Table 6.
The need for equipment for the next decade.
| LINAC required in 2030 | LINAC in 2018 | Replacement Required (A) | Expanded offer (B) | Total acquisition Required (A+B) | |
|---|---|---|---|---|---|
| Public | 434 | 252 | 127 | 182 | 309 |
| Private | 96 | 111 | 20 | 0 | 20 |
| Total | 530 | 363 | 147 | 182 | 329 |
Abbreviation: LINAC = linear accelerator.
In addition to the lack of equipment and its obsolescence, planning to optimize the uptime of currently active machines (530) is lacking. If we consider the number of 18 fractions times per patient as an average, all machines available in the country will need to work 16 h a day, at maximum service capacity to meet the required demand. The number of hours of equipment (uptime) presents significant variations depending on other factors, such as an adequate and constant flow of patients and reduced downtime due to maintenance.
Given the obtained results, and theoretical basis, it was possible to allocate the main factors, as well as their relationship with the problems presented by the PER-SUS project, through the use of root cause analysis (Ishikawa Diagram). It allows for a mapping of possible links between the causes, or opportunities for improvement that are appropriate to the situation (Figure 2).
Figure 2.
Ishikawa Diagram.
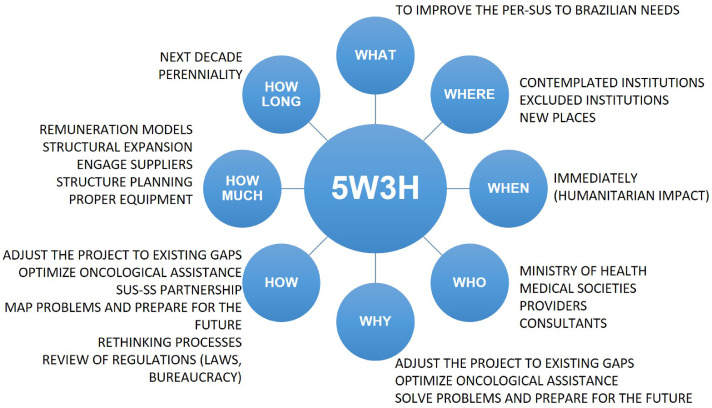
Figure 3 illustrates the initial sketch of an improvement proposal, using the 5W3H tool, aiming to optimize the PER-SUS for the Brazilian needs and to identify the most critical challenges while seekings full access to health care. It is possible to create a national plan for the distribution of equipment considering the geographic, economic, and social characteristics, as well as the epidemiological profile of each region. Moreover, it is crucial to align the priorities of the government, local managers, suppliers, and medical entities. However, quality indicators for PER-SUS are lacking, and this also needs to be considered.
Figure 3.
5W3H Matrix.
Discussion
Based on the results of this study, the following critical points were identified: The high rate of exclusion of institutions reflects inappropriate selection of the institutions or inadequate planning for the project. Moreover, the delay in execution was related to bureaucratic obstacles and underestimating the requirements for planning (logistics/people). In addition, the audacious PER-SUS dimensioning did not seem to overcome the lack of prioritization in oncologic care. Furthermore, the teaching/research and technological investment output were not evident (no data shown), mainly due to the closing of the local Varian factory. Hence, the closing of the equipment factory was also a consequence of inadequate planning and a lack of project “protection” by the government.
The RT2030 report highlighted, among others, the importance of radiotherapy treatment in the context of cancers, which are diseases that will be increasingly prevalent in an ageing population. These problems need to be adequately addressed because of their magnitude in our country.
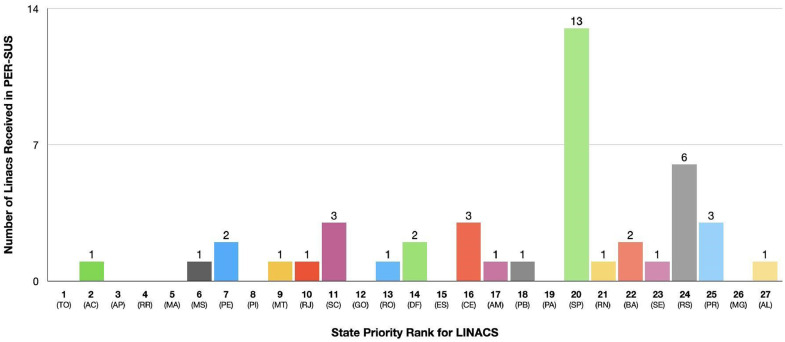
Furthermore, the inadequate prioritization of the States receiving new LINACS is another concern. Viani et al. reported that of the first 44 LINACS delivered in PER-SUS, only 6 (14%) were installed in the top 10 priority states considering the LINAC shortage index, Figure 4.18 In addition, the Midwest and North regions had a higher LINAC shortage and received only 4 (9%) and 3 (7%) of the initial 44 LINACS, respectively. On the other hand, the Northeast, South, and Southeast regions had a lower LINAC shortage and received 11 (25%), 12 (27%), and 14 (32%) of the initial 44 LINACS.
Figure 4.
Number of LINACS Received in PER-SUS against States’ Priority Rank for LINACS (reference).18
In Brazil, many of the problems associated with access to healthcare are related to geographic factors and healthcare heterogeneity. Economic and population distribution variables also influence the lack of access, as follows: First, the number of equipment available to the SUS must be interpreted differently from the number of equipment dedicated to the SUS, as many oncology centres assist patients from both the public and private health system. Second, SUS radiotherapy services do not always work at their maximum service capacity due to inadequate management of the flow of care and limited local or regional radiotherapy budget (limited monthly allowance for expenditures). Third, the standardized indications for radiotherapy according to the Brazilian Radiotherapy Society are not uniformly adopted in most health services, both supplementary and dedicated to SUS. A typical example of this situation concerns the adjuvant irradiation of patients with breast cancer, where there is strong evidence to indicate that radiotherapy performed in 5–15 daily fractions has the same effectiveness and oncological safety.19, 20, 21, 22, 23 However, many services persist in prescribing these treatments in 25 to 30 fractions, increasing the length of treatment without additional benefit to the patient or the system. Other striking examples include the ultra-hypofractionated irradiation of prostate cancer (which requires five fractions instead of 20-35, and the need for intensity-modulated radiation therapy [IMRT]) or ablative radiotherapy for early-stage lung cancer (which also requires advanced technology). This disregarding of hypofractionation might illustrate how guidelines and “standards-of-care” in the system are not being defined based on the best science/evidence available.
Thus, the lack of advanced technology and the need to deliver higher quality treatment may explain the country's low rates of short-course radiotherapy.24 Fourth, the SUS reimbursement model has not evolved with the technology and quality of radiotherapy treatments, resulting in a disproportional correlation between them. This discrepancy limits the capacity of the institutions to incorporate advanced radiotherapy techniques and to perform short treatments such as prostate and lung stereotactic body radiation therapy (SBRT) or image-guided radiotherapy, Supplementary Table 2.
It is not redundant to point out that access to radiotherapy depends directly on the country's economy, as Atun et al.25 illustrated. They were able to identify a direct and proportional relationship between access to radiotherapy and the country's economy compared with several other economies. Brazil allocates 9.5% of its GDP to health, compared to 10.8% in Canada and 9.5% in Argentina. Regarding the global per capita spending in healthcare (in 2019), Brazil allocated U$ 853.28 against U$ 5,048.37 in Canada and U$ 4312,88 in the United Kingdom. In contrast to these countries, public expenditure in Brazil represents only 40.7% of total health expenditure.26
There have been many gains from the PER-SUS assistance. In a survey by Migowski et al.,27 there was a linear increase in the number of healthcare providers that qualified for cancer treatment in Brazil between 2003 and 2018 (from 178 to 305). Furthermore, an increase in the number of chemotherapy and radiotherapy sessions between 2010 and 2017 was also observed. In the north, northeast, midwest, southeast, and south regions, these were 24%, 60%, 47%, 17%, and 47%, respectively. According to a survey by the Brazilian Radiotherapy Society in 2018, there were 383 LINACs in Brazil, with 272 available to the SUS. Despite this improvement, there is still a shortage of up to 55% for services, depending on the region.
Besides, there is a need to improve both current and future practical solutions for Brazil's healthcare problems. The EXPANDE project, which preceded PER-SUS and pledged to incorporate about 15 LINACs in SUS institutions, did little to fulfill that promise due mainly to bureaucratic, organizational, and priority changes in governments' logistical obstacles. At least four reports of institutions covered by the EXPANDE project received the equipment but could not use it because there were no professionals available to install them, and there were no bunkers prepared to receive the equipment. This finding could serve as an excellent example for the baseline and preliminary studies on PER-SUS to avoid the same obstacles.
Similarly, the regulation of new technologies in Brazil is complicated. The bureaucratization of technological incorporation for health in Brazil can be classified as one of the most complex globally. The flows of the National Commission for Incorporation of Technologies in the SUS (CONITEC)28 and National Supplemental Healthcare Agency (ANS)29 are extremely complicated for a given technology or procedure to be incorporated into the list of minimum procedures. Although safety issues are justifiable, these flows could be improved or simplified. Although radiotherapy is a safe and well-reported therapy globally, accidents involving the use of radiation in medicine (including radiotherapy) are impactful. This implies that implementing new technologies that yield faster care will require several justifications, often very difficult to obtain. In a benchmark study among equipment suppliers carried out in 2017,30 the base equipment for PER-SUS was reported at an average price of 600 thousand dollars. This lower value can be attributed to the savings from a large-scale purchase and lower technological complexity, such as a single treatment planning workstation, and the absence of a license for IMRT, and image-guidance tools. The cost for these technological upgrades could account for more than 700 thousand dollars. If an institution is willing to upgrade its equipment, it will also pay more.28 The difference between the acquisition of a “basic” equipment and another one with a “minimum package of resources” is smaller than expected.
Radiotherapy is a sphere of health extremely dependent on technological resources and professional training. The lack of quality in treatments is related to effectiveness and toxicity to patients. The term “Patient Safety” is defined by the World Health Organization as “reducing the risk of unnecessary harm associated with health care to an acceptable minimum”, and in the radiotherapy scenario, it represents a commitment by health institutions to provide quality in the treatment. The medical residency in radiotherapy in Brazil currently lasts for 4 years, and in 2019 only 28 radiation oncologists obtained their board certifications, according to a report by the Brazilian Society of Radiotherapy. Many of them will not work very far from their training places – most institutions that offer medical residency in Brazil are located in the Southeast region of the country. With the progress of PER-SUS, there were some changes in the disposition of medical residency vacancies in Brazil to compensate for this heterogeneity, which was problematic at times. In 2019, there were 206 vacancies available for medical residency in Brazil, but the occupancy rate was, unfortunately, half that amount. It would be desirable for the future to improve the quality of medical training in radiotherapy, including technical training and incentives for research. The same scenario can be applied to other components, such as medical physicists, radioprotection supervisors, radiotherapy equipment operators, nurses, dosimetrists, engineers, and healthcare managers. The lack of training centres for these professionals distributed throughout Brazil directly affects the premises for the next decade in the search for improved access to health in oncology/radiotherapy. The fact that the Varian Company has recently terminated its activities denotes the lack of equipment supply and the gap created by professional training. There is undoubtedly room and opportunity for improvements in human resources.
We would like to point out some limitations of this study. First, we performed an observational analysis of reported data referring to a project that has not yet been completed (PER-SUS) at the time this manuscript has been concluded, and possibly some of the information or even the impressions might be changed in the future. Second, some of the facts that were contextualized with our results may be underestimated (for example, some reports are from 2018, others from 2020). Third, some information collected could not be included in this article, such as estimates related individually to the benefited institutions. Finally, other parameters and direct predictors of interference in the research problem were not considered, such as changes in federal, state and municipal governments, which can change the administrative structure and even the availability of resources to institutions.12
Given several challenges described in the design and implementation of PER-SUS, we present some recommendations for the Brazilian government to consider. First, a long-term political commitment is needed to sustain integrated initiatives to expand access to universal and comprehensive cancer care, including access to radiotherapy. Second, as Brazil has a decentralized health system at the municipal level, it is crucial to strengthen inter-federative agreements and regional governance arrangements to manage the complexity of implementing the installations proposed by PER-SUS as part of the development of cancer care in all regions. Third, stable and predictable federal funding for Cancer is fundamental for addressing inequalities in funding sources, which historically has exacerbated inequalities in allocating all sorts of resources needed for cancer care in Brazil. Finally, strengthening the participatory management for the PER-SUS, involving all stakeholders in participation, alignment, and engagement, could optimize this innovative initiative for the next decade. Ideally, the entire plan should include evidence-based decisions at its core, committing the involved oncologists. Are we ready for 2030?
Conclusion
The PER-SUS project delivered nearly 50% of the proposed implementation of radiotherapy equipment after ten years. There was a 17% growth in the national number of LINACS with PER-SUS, against a 32% increase in cancer incidence in Brazil in the same period. Considering these data and the initial 2015 project deadline, PER-SUS did not achieve the pre-established goals specified by the Brazilian Government. The States and regions with a low LINACS offer should be prioritized, and the involvement of all the stakeholders is essential to overcome the challenges described in the present study and to improve access to radiotherapy with the incorporation of advanced and effective radiotherapy technologies.
Contributors
All authors contributed to the conception and design, acquisition of data, or analysis and interpretation of data; drafting of the article or revising it critically for important intellectual content, and final approval of the version to be published.
Data sharing statement
The data that support the findings of this study are publicly available, and can be reached as they are referenced in this study, especially references number: 1, 6-9, 11, 12, 13, 15-17, 28, and 29.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
All authors declare that we have no conflicts of interest in the authorship or publication of this contribution.
Acknowledgments
The authors thank the Brazilian Society of Radiotherapy and Fundação Getulio Vargas, for their encouragement.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2022.100333.
Appendix. Supplementary materials
References
- 1.INCA National Cancer Institute. Cancer treatment. 2020. Available from:https://www.inca.gov.br/sites/ufu.sti.inca.local/files/media/document/estimativa-2020-incidencia-de-cancer-no-brasil.pdf/. Accessed 1 June 2022.
- 2.World Health Organization . NCBI; 2007. Cancer control: knowledge into action: WHO guide for effective programmes: module 3: early detection.https://bit.ly/3mIGLKM Available from: [PubMed] [Google Scholar]
- 3.Ministry of Health. Ordinance no. 931 of May 10, 2012. Available from:https://bvsms.saude.gov.br/bvs/saudelegis/gm/2012/prt0931_10_05_2012.html. Accessed 9 December 2021.
- 4.Moraes F, Marta GN, Hanna SA, et al. Brazil's challenges and opportunities. Int J Radiat Oncol Biol Phys. 2015;92:707–712. doi: 10.1016/j.ijropp.2014.12.063. [DOI] [PubMed] [Google Scholar]
- 5.Mendez LC, Moraes FY, Fernandes GS, Weltman E. Cancer deaths due to lack of universal access to radiotherapy in the Brazilian public health system. Clin Oncol. 2018;30:e29–e36. doi: 10.1016/j.clon.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Siasus 2017. Available from:https://ces.ibge.gov.br/base-de-dados/metadados/ministerio-da-saude/sistema-de-informacoes-ambulatoriais-do-sus-sia-sus.html/. Accessed 9 December 2021.
- 7.Ministry of Health . 2019. Radiotherapy census.https://bit.ly/30240Wq Available from: [Google Scholar]
- 8.Federal Court of Accounts. National Oncology Care Policy. Minister Rapporteur José Jorge . Vol. 132. 2011. Operational audit report. (Operational audit report). [Google Scholar]
- 9.Ministry of Health . 2019. Radiotherapy census. Brasilia.https://bit.ly/3iYgB4A Available from: [Google Scholar]
- 10.Oribe CY. Tree diagram: the tool for the present times. 2012. Available from: https://bit.ly/3jdU2ZR. Accessed 9 December 2021.
- 11.PER-SUS - radiotherapy expansion plan in the SUS. Available from: https://www.gov.br/saude/pt-br/acesso-a-informacao/acoes-e-programas/plano-de-expansao-da-radiooterapia-no-sus/. Accessed 9 December 2021.
- 12.INCA National Cancer Institute. Estimativa 2020–2022: incidência do Câncer no Brasil. Available from: https://www.inca.gov.br/sites/ufu.sti.inca.local/files//media/document//estimativa-2020-incidencia-de-cancer-no-brasil.pdf. Accessed 1st June 2022.
- 13.INCA National Cancer Institute. Estimativa 2012: incidência do Câncer no Brasil. Available from: http://portal.saude.sp.gov.br/resources/ses/perfil/gestor/homepage/estimativas-de-incidencia-de-cancer-2012/estimativas_incidencia_cancer_2012.pdf. Accessed 1st June 2022.
- 14.Faroni LD, Rosa AA, Aran V, Ramos RS, Ferreira CG. Access of patients with lung cancer to high technology radiation treatment in Brazil. JCO Glob Oncol. 2021;7:726–733. doi: 10.1200/GO.20.00622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.SBRT. Brazilian society of radiotherapy. Radiotherapy development plan for the next decade. RT 2030. Available from: https://sbradiooterapia.com.br/wp-content/uploads/2021/08/Relatorio_Projeto_RT2030.pdf/. Accessed 9 December 2021.
- 16.Ministry of Health. Datasus. Tabnet. sd Available from: https://bit.ly/3aJNPBJ. Accessed 9 December 2021.
- 17.IBGE. Brazilian institute of geography and statistics. Projection of the population of Brazil and Federation Units. 2021. Available from: https://www.ibge.gov.br/apps/populacao/projecao/. Accessed 9 December 2021.
- 18.Viani GA, Gouveia AG, Bratti VF, et al. Prioritising locations for radiotherapy equipment in Brazil: a cross-sectional, population-based study and development of a LINAC shortage index. Lancet Oncol. 2022 doi: 10.1016/S1470-2045(22)00123-1. S1470-2045(22)00123-1. [DOI] [PubMed] [Google Scholar]
- 19.Brunt AM, Haviland JS, Wheatley DA, et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5-year efficacy and late normal tissue effects results from a multicentre, non-inferiority, randomised, phase 3 trial. Lancet. 2020;395(10237):1613–1626. doi: 10.1016/S0140-6736(20)30932-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brunt AM, Haviland JS, Sydenham M, et al. Ten-year results of FAST: a randomized controlled trial of 5-fraction whole-breast radiotherapy for early breast cancer. J Clin Oncol. 2020;38(28):3261–3272. doi: 10.1200/JCO.19.02750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.SBRT, Brazilian Society of Radiotherapy. Freitas NMA, Rosa AA, Marta GN, et al. Recommendations for hypofractionated whole-breast irradiation. Rev Assoc Med Bras (1992) 2018;64(9):770–777. doi: 10.1590/1806-9282.64.09.770. PMID: 30672995. [DOI] [PubMed] [Google Scholar]
- 22.Meattini I, Becherini C, Boersma L, et al. European society for radiotherapy and oncology advisory committee in radiation oncology practice consensus recommendations on patient selection and dose and fractionation for external beam radiotherapy in early breast cancer. Lancet Oncol. 2022;23(1):e21–e31. doi: 10.1016/S1470-2045(21)00539-8. [DOI] [PubMed] [Google Scholar]
- 23.Smith BD, Bellon JR, Blitzblau R, et al. Radiation therapy for the whole breast: executive summary of an American Society for Radiation Oncology (ASTRO) evidence-based guideline. Pract Radiat Oncol. 2018;8(3):145–152. doi: 10.1016/j.prro.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 24.Irabor OC, Swanson W, Shaukat F, et al. Can the adoption of hypofractionation guidelines expand global radiotherapy access? An analysis for breast and prostate radiotherapy. JCO Glob Oncol. 2020;6:667–678. doi: 10.1016/S1470-2045(15)00288-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Atun R, Jaffray DA, Barton MB. Expanding global access to radiotherapy. Lancet Oncol. 2015;16:1153–1186. doi: 10.1016/S1470-2045(15)00222-3. [DOI] [PubMed] [Google Scholar]
- 26.Global Health Expenditure Database (who.int). Accessed 16 February 2022.
- 27.Migowsky A, Atty ATM, Tomazelli JG, Days MBK, Garden BC. Oncology care and 30 years of the unified health system. Rev Bras Cancerol. 2018;64:247–250. https://rbc.inca.gov.br/revista/index.php/revista/article/view/84 Available from: [Google Scholar]
- 28.CONITEC. National commission for the incorporation of technologies in the unified health system. Latest news. sd Available from: https://bit.ly/3qXmCCd. Accessed 9 December 2021.
- 29.National Supplemental Health Agency. Guide to Implementing value-based compensation models. ANS, 2019. Available from: https://bit.ly/3mHAYW4. Accessed 9 December 2021.
- 30.Elekta Benchmarking 2017 (“Annual report 2017/18”). Available from: https://www.elekta.com/investors/fileadmin/reports/annual-reports/elekta-annual-report-18-en.pdf/. Accessed 4 October 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.