Summary
Background
To fight against the rising incidence of syphilis, the Brazilian Ministry of Health (MoH) launched the “Syphilis No!” Project (SNP), with specific resources funded by a parliamentary amendment. Then, in 2018, a national rapid response started to be implemented on the Brazilian Unified Health System (SUS, Sistema Único de Saúde) in two strategic lines (1) to reinforce SUS's universal actions and (2) to implement specific ones to 100 municipalities chosen by the MoH as priorities for syphilis congenital response. In 2015, such localities represented 6895% of congenital syphilis cases in Brazil. In this context, SNP has implemented actions to strengthen epidemiological surveillance of acquired syphilis and congenital syphilis by instituting an integrated and collaborative response through health services networks and reinforcing interstate relations.
Methods
A quasi-experimental study using time series analysis was conducted to assess immediate impacts and changes to the trend in national congenital syphilis before and after the project, from September 2016 to December 2019. Data were assessed considering rates of congenital syphilis per 1,000 live births in all priority municipalities (n=100) covered by the project and in non-priority municipalities (n=5,470) from all five macro-regions of Brazil.
Findings
Priority municipalities showed a greater reduction (change in trend) in comparison to non-priority. The linear regression model revealed trend changes after the intervention, with both groups of municipalities showing a drop in the average monthly number of cases per 1,000 live births, with a reduction of -0·21 (CI 95% -0·33 to -0·09; p=0·0011) in priority municipalities and of -0·10 (CI 95% -0.19 to -0.02; p=0·0216) in non-priority municipalities.
Interpretation
The study using ITS provides important evidence on the direction, timing, and magnitude of the effects of interventions introduced as part of the SNP on congenital syphilis in Brazil. Our results suggest that the Syphilis No! Project influenced the trends of congenital syphilis in Brazil from 2018, with higher reductions achieved in the priority municipalities.
Funding
The research is funded by a grant to the Syphilis No! Project from Brazilian Ministry of Health (Project Number: 54/2017). The funders had no role in study design, analysis, decision to publish, or preparation of the manuscript.
Keywords: public health, policy, interrupted time series, segmented regression analysis, notifiable disease, syphilis
Research in Context.
Evidence before this study
We searched PubMed for articles published up to Oct 1, 2021, using the terms "syphilis" AND ("temporal analysis" OR "time series" OR "regression methods") AND "public health", with no language restrictions. Our search identified six studies. Four of them report analysis of syphilis data in Brazil from a time series perspective, with different settings, showing the syphilis incidence rates increasing from 2007 to 2016 and the challenge of the Brazilian Ministry of Health to reduce the three forms of syphilis (in pregnancy, congenital and acquired). Apart from these studies, China reported that syphilis incidence rates have increased three-fold from 2005 to 2012 and time series analysis was an effective tool for modelling the historical and future incidence.
Added value of this study
We used interrupted time series to examine trends before and after the introduction of a public intervention project in Brazil in order to reduce acquired syphilis, syphilis in pregnant women, and congenital syphilis by expanding coverage of diagnosis (through rapid testing), and timely and appropriate treatment of pregnant women and sexual partners in prenatal care, childbirth, or abortion situations. Data were assessed considering rates of congenital syphilis per 1,000 live births in all priority municipalities (n=100) covered by the project and in non-priority municipalities (n=5,470) from all five macro-regions of Brazil.
Our interrupted time series data indicate changes in trends towards reduction or stabilization in almost all regions (North, Northeast, South, and Southeast). This effect may be attributed to the project's universal actions, that is, general interventions that were designed and implemented in all Brazilian states and municipalities.
Implication of all the available evidence
In recent years (2010-2019) it is the first time we can see a change in the course of congenital syphilis in Brazil. The effects of the intervention at the national level reveals statistically significant trend changes in monthly rates of congenital syphilis in Brazil and shows rate variations by region.
Alt-text: Unlabelled box
Introduction
Congenital syphilis (mother-to-child transmission or vertical transmission of syphilis of syphilis) causes damage to the fetus if the mother's infection is not detected and properly treated during pregnancy. The World Health Organization (WHO) estimates that each year 930,000 pregnant women have probable active syphilis worldwide each year. It results in approximately 350,000 adverse birth outcomes, including 143,000 early fetal deaths/stillbirths, 62,000 neonatal deaths, 44,000 premature/low-birthweight babies, and 102,000 infected infants.1,2
The Pan American Health Organization (PAHO) Member States, supported by WHO, in 2010 approved the Strategy and Plan of Action for the Elimination of Mother-to-Child Transmission of HIV and Congenital Syphilis. The strategy was set to reduce the incidence of congenital syphilis to ≤ 0·5 cases per 1,000 live births by 2015.3 Nonetheless, Brazil did not reach the congenital syphilis elimination goal, which led a resurgence of acquired syphilis, syphilis in pregnant women and congenital syphilis across the country. In 2010, 6,949 cases of congenital syphilis were reported to the Brazilian Ministry of Health (2·4/1,000 live births), whereas, in 2015, this case count increased to 19,647 (6·5/1,000 live births) accounting for a growth rate of 170·83%.4
To fight the syphilis epidemic in Brazil, in October of 2016, the Ministry of Health (MoH) issued the Strategic Actions Agenda for Reducing Syphilis in Brazil.5 This agenda established a list of priorities aimed in collaboration with PAHO and other institutions such as universities, international agencies, and state and municipal representatives. Furthermore, such agenda prompted a parliamentary amendment with specific resources to implement a national rapid response in Brazil's Unified Health System (SUS, Sistema Único de Saúde).
The Brazilian Ministry of Health invited state and municipal health managers to fight syphilis through the “Syphilis No!” Project—that included the “Applied Research for Intelligent Integration Aimed at Strengthening Healthcare Networks for Rapid Response to Syphilis”—to reduce acquired syphilis, syphilis in pregnant women, and congenital syphilis by expanding coverage of diagnosis (through rapid testing), and timely and proper treatment of pregnant women and sexual partners in prenatal care, childbirth, or abortion situations. Through the Project, the syphilis epidemic has been faced up through two strategic lines: (1) reinforcing universal actions of SUS and (2) implementing specific ones to 100 municipalities chosen by the MoH as priorities for syphilis congenital response, as in 2015 they represented 68·95% of the number of congenital syphilis cases in Brazil.
The universal line of intervention included acquiring and distributing testing and treatment supplies (crystalline and benzathine penicillin), enhancing the STI laboratories network and the situation rooms for epidemiological surveillance, educommunication strategies,6 social interventions, and awareness campaigns performed to face syphilis in that period. At the same time, institutional support was granted to the priority municipalities, where Research and Intervention Supporters (RIS) carried out specific work with local health managers. Hence, this work provided technical cooperation to strengthen prevention actions aimed at reducing the vertical transmission of syphilis, such as implementing committees focused on investigating syphilis cases and reinforcing local planning of response on the project's axis, among others. The details of the project interventions and relevant timelines are presented in Appendix (Figures A1 to A5).
The purpose of this study is to use interrupted time series to estimate intervention effects over time by comparing rates of congenital syphilis per 1,000 live births in the priority municipalities (n=100) covered by the Syphilis No! Project and in non-priority municipalities (n=5,470) in the five macro-regions of Brazil: North, Northeast, South, Southeast, and Midwest.
Methods
Considering that a randomized controlled trial (RCT) is infeasible to be performed in this study, we used a quasi-experimental research design with interrupted time series (ITS) analysis. Such design enables comparisons in population health outcomes before, during and after an intervention within a clearly defined span.7 ITS is a good approach for evaluating longitudinal effects of health interventions.8,9 Besides, it can be used as a statistical method for estimating intervention effects of a policy change on an outcome of interest.10 The ITS design and the use of segmented regression analysis enables evaluation of immediate impact and slope associated with a policy intervention while controlling the overall trend in the rate of the outcome of interest.10
This study was performed through a multidimensional, flexible, and adaptive framework aimed at discovery and temporal analysis of public health interventions. It was implemented using the Hermes system,11,12 which manages a complete data life cycle13 by 1) acquiring data from several external sources in different formats; 2) cleaning data for standardization and error removal; 3) transforming it into specific models; 4) publishing a dashboard; 5) preserving data as a structured database.
Use of data sources
The Hermes system was used to collect congenital syphilis data from the Notifiable Diseases Information System (SINAN, Sistema de Informação de Agravos de Notificação), provided by the Brazilian MoH. These data represent the total number of notified cases per municipality, given by month and year. The vital records of live births by municipality for each year, were retrieved from the Health Informatics Department of the Brazilian Ministry of Health (DATASUS) and used calculate monthly average live per municipality per year. Hermes derived the rates of congenital syphilis cases by dividing monthly cases per municipality by live births.
Priority vs non-priority municipalities
Brazil has 5,570 municipalities spread over five macro-regions—North, Northeast, South, Southeast and Midwest. Monthly rates per municipality were used to categorise municipalities into priority and non-priority.
The MoH classified the project as a tool with two lines for inducing response on syphilis: universal and specific actions. Thus, priority municipalities (n=100) were defined on population and epidemiological criteria, namely: the 27 capitals, in addition to municipalities in metropolitan regions with more than 100,000 inhabitants that had, in 2015, the highest rates of both congenital syphilis incidence in children under one year of age and perinatal mortality. The priority municipalities represented 68·95% of the total congenital syphilis cases in Brazil. Other municipalities (n=5,470) were categorised as non-priority. Appendix (Figure A6) provides geographic, demographic and socio-economic characteristics of the five regions and presents the geographic location of 100 priority and 5,470 non-priority municipalities.
The priority municipalities received support and technical cooperation from the project's network of Research and Intervention Supporters. Their work focused on the municipalities' needs within the axis of the project, as it was monitored through the “LUES” platform,14 made available by the project. The supporters entered on the “LUES” platform all of their technical cooperation activities to health teams and local managers of priority municipalities on a monthly basis for supporting actions to prevent mother-to-child transmission (MTCT) of syphilis.
Statistical analysis
A quasi-experimental design was applied to analyze the time series data using a segmented linear regression model in the R software, adapted to exchange data with Hermes in order to assess the immediate impact and change in trend of national congenital syphilis rates pre and post the SNP intervention. What is more, May of 2018 was considered the intervention start time point for implementing the Syphilis No! Project. Appendix provides R code used in this analysis.
Data must be collected regularly over time and at equally spaced intervals to perform a segmented regression analysis.9,15 To avoid any bias related to the Covid-19 pandemic, December of 2019 was defined as the end date for the data collection, totaling 20 months pre-intervention (Sep/2016 to Apr/2018) and 20 months post-intervention (May/2018 to Dec/2019).
A linear relationship between time and the outcome within each segment was assumed, considering segmented regression models fit a least squares regression line for each segment of the independent variable (time), p < 0·05 was considered statistically significant. Thus, the next step in the analysis was to estimate the magnitude of the intervention and test the statistical significance of immediate impact and trend rates.
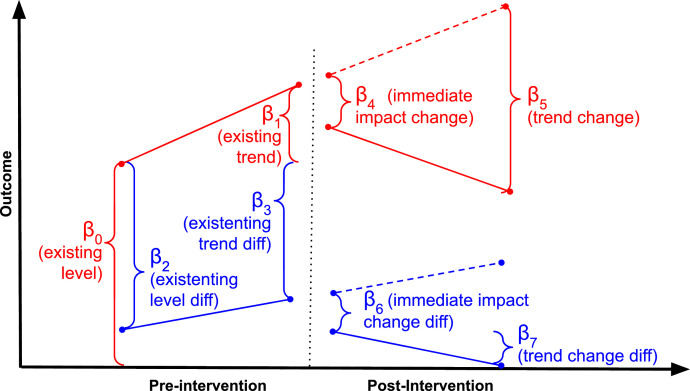
The regression model used to fit these data is straightforward. outcomet = β0 + β1 *t + β2 * priorityt + β3 * priorityt * i + β4 * post-interventiont + β5 * (t - TI) * post-interventiont + β6 * post-interventiont * priorityt + β7 * post-interventiont * t * priorityt + εt
Where β0 is the baseline outcome for the non-priority group; β1 is the pre-existing trend in the outcome of interest for the priority non-group; β2 is the baseline difference between non-priority and priority groups; β3 is the difference in trend between non-priority and priority group before intervention; β4 is the immediate impact in the priority group; β5 is the trend change in the priority group; β6 is the difference in the immediate impact change between the non-priority and priority after intervention, and β7 is the difference in trend change between the non-priority and priority group after intervention. Priority variable is coded 1 for priority and 0 for non-priority. The t variable is only an increment that counts up from 1 to 40 over the entire period. The post-intervention variable was set to be 0 before the intervention and 1 after. TI is constant that represents the intervention moment, in this case is equal to 20. Figure 1 represents the model, including the immediate impact and trend change.
Figure 1.
Interrupted time-series parameterized as a segmented regression model, including the immediate impact and trend change. The solid lines represent the observed values, and dotted lines indicate the counterfactual for the post-intervention period.
Ordinary Least Squares (OLS) regression analysis assumes that error terms associated with each observation are uncorrelated. Correctly inspecting autocorrelation terms can avoid underestimated standard errors and overestimated significance of the effects of an intervention.15 In the case of this study, a Durbin-Watson test was used to investigate the presence of autocorrelation, in addition to residual plots, Auto Correlation Function (ACF) plots, and partial-ACF plots. Autocorrelation was not detected in the statistical tests.
R-squared is a statistical measure of how close the data are to the fitted regression line. It is also known as the coefficient of determination or the coefficient of multiple determination for multiple regression. It was used in this research's model to determine how close the data are to the model and how it is presented in the results. R-squared is a value between 0 and 1, where 0 indicates that the model explains none of the variability of the response data around its mean, and 1 indicates that the model explains all the variability of the response data around its mean.
Outliers are extreme values that do not seem to fit in the time series. If the outlier reflects an anticipatory or short-term history effect, the data point can be explicitly modeled. Alternatively, if the outlier is an unambiguous clear consequence of the intervention, it can be treated as a regular data point to evaluate its impact. A preliminary analysis was performed, and a single outlier was identified in the Midwest region after the intervention (July 2018). The Moving Average (MA) method was used to smooth the data for the purpose of explaining temporal trends. The MA used was of order three, which provides only a smoothing with the two months (before and after) the calculated observation. After this process, no outlier remained.
The regression models obtained for each group (priority and non-priority municipalities), using data from the pre- and post-intervention periods (May 2018), were compared with the counterfactual for the post-intervention period considering the trend observed before the intervention. The counterfactual enables a comparison between the observed change and what would have happened had the intervention not taken place. The regression model parameters were obtained by point and interval estimation using 95% of confidence.
Role of the funding source
The funders had no role in study design, data collection, data analysis, interpretation, decision to publish, or preparation of the manuscript.
Results
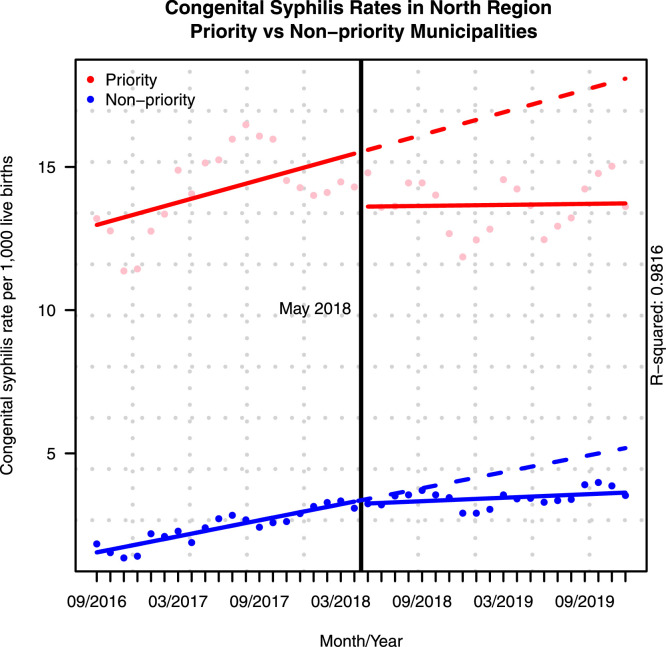
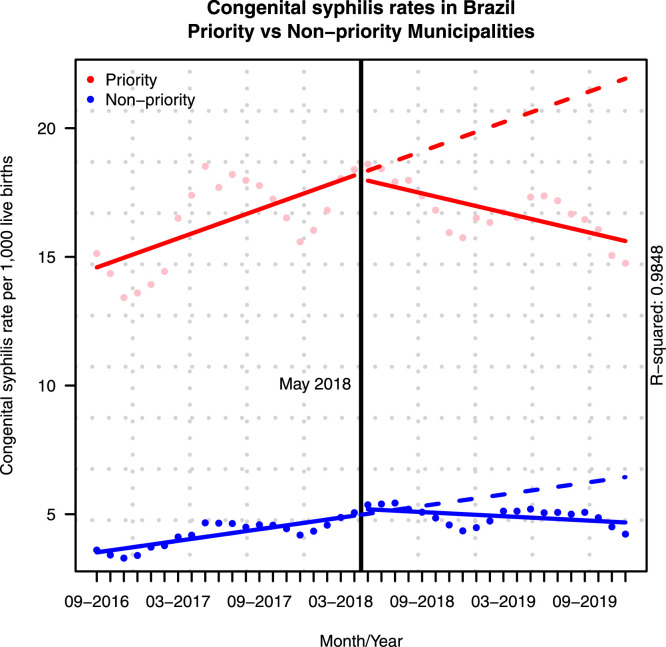
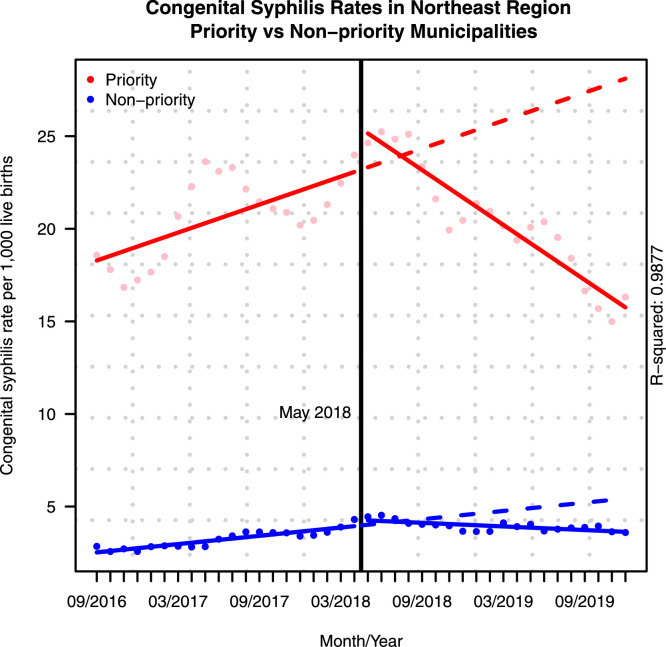
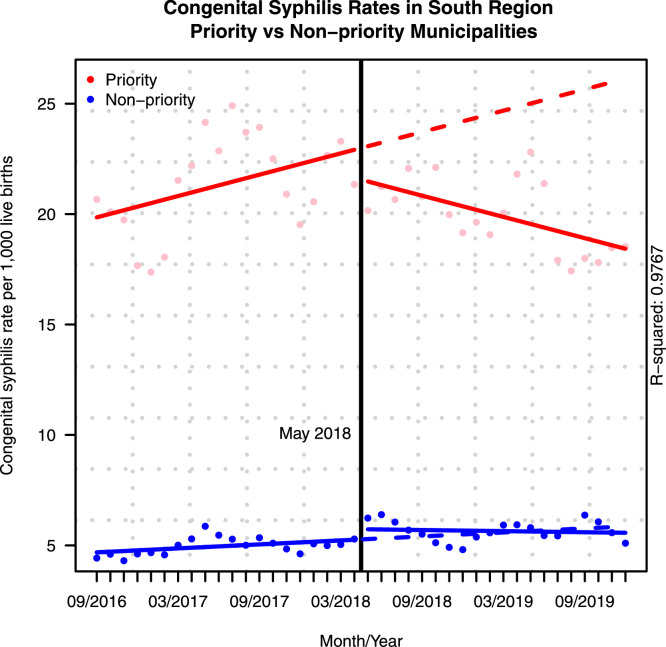
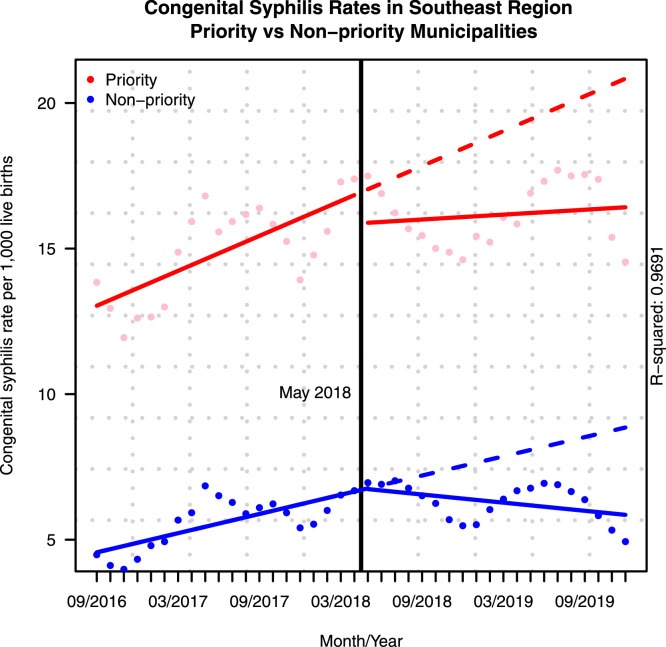
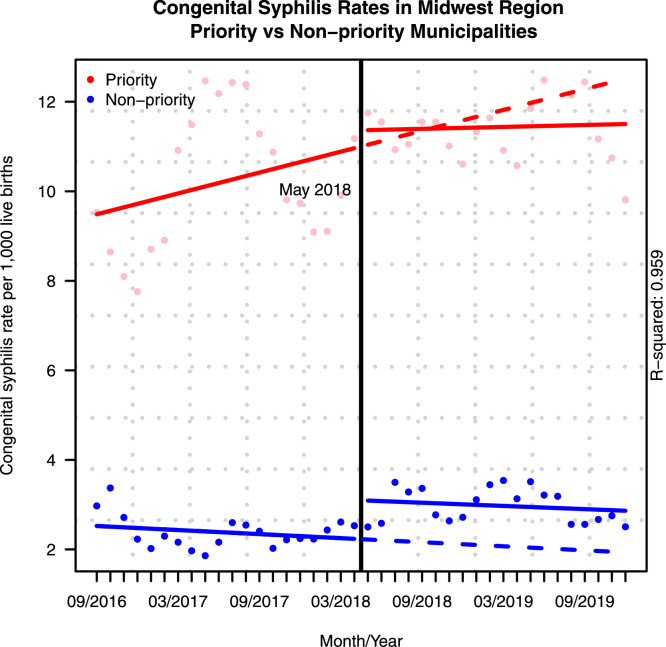
Results of the time series analysis comparing rates of congenital syphilis per 1,000 live births in the priority municipalities and non-priority municipalities are presented in Table 1 and Figures 2 to 7. The red dots represent the monthly rates of cases in priority municipalities and the blue dots in non-priority ones. The continuous lines indicate the regression models obtained for each group (priority and non-priority), using data from the pre- and post-intervention periods (May 2018). Moreover, the dotted lines indicate the counterfactual for the post-intervention period using the data trend observed before the intervention. Table 2 presents this comparison considering the last month of the analyzed period (20th month, December of 2019).
Table 1.
Results of the time series analysis comparing rates of congenital syphilis per 1,000 live births between priority and non-priority municipalities.
| North |
Northeast |
South |
Southeast |
Midwest |
Brazil |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| value (CI 95%) |
p-value | value (CI 95%) |
p-value | value (CI 95%) | p-value | value (CI 95%) | p-value | value (CI 95%) | p-value | value (CI 95%) | p-value | |
| Pre-Intervention | ||||||||||||
| Intercept | 1·45 (0·71 to 2·19) |
<0·001 | 2·45 (1·51 to 3·39) |
<0·001 | 4·65 (3·49 to 5·82) |
<0·001 | 4·45 (3·61 to 5·30) |
<0·001 | 2·54 (1·71 to 3·37) |
<0·001 | 3·44 (2·71 to 4·17) |
<0·001 |
| Differential between groups | 11·39 (10·35 to 12·44) |
<0·001 | 15·58 (14·25 to 16·91) |
<0·001 | 15·04 (13·39 to 16·68) |
<0·001 | 8·38 (7·18 to 9·58) |
<0·001 | 6·87 (5·70 to 8·04) |
<0·001 | 10·96 (9·92 to 12·00) |
<0·001 |
| Trend in priority group | 0·04 (-0·05 to 0·13) |
0·393 | 0·18 (0·07 to 0·29) |
0·002 | 0·13 (-0·01 to 0·27) |
0·062 | 0·09 (-0·01 to 0·19) |
0·077 | 0·09 (-0·01 to 0·19) |
0·063 | 0·11 (0·03 to 0·20) |
0·011 |
| Trend in non-priority group | 0·09 (0·03 to 0·16) |
0·004 | 0·07 (0·00 to 0·15) |
0·062 | 0·03 (-0·07 to 0·13) |
0·539 | 0·11 (0·04 to 0·18) |
0·003 | -0·02 (-0·08 to 0·05) |
0·665 | 0·08 (0·01 to 0·14) |
0·017 |
| Post-Intervention | ||||||||||||
| Immediate impact in priority group | -1·77 (-3·20 to -0·34) |
0·016 | 2·23 (0·42 to 4·05) |
0·016 | -1·76 (-4·00 to 0·49) |
0·123 | -1·11 (-2·75 to 0·53) |
0·181 | -0·47 (-2·07 to 1·13) |
0·560 | -0·36 (-1·77 to 1·06) |
0·618 |
| Immediate impact in non-priority group | -0·09 (-1·10 to 0·92) |
0·865 | 0·34 (-0·94 to 1·62) |
0·598 | 0·48 (-1·11 to 2·07) |
0·548 | 0·13 (-1·03 to 1·29) |
0·822 | 0·87 (-0·26 to 2·00) |
0·131 | 0·28 (-0·72 to 1·28) |
0·583 |
| Change in trend in priority group | -0·05 (-0·18 to 0·07) |
0·407 | -0·64 (-0·80 to -0·48) |
<0·001 | -0·28 (-0·48 to -0·09) |
0·005 | -0·02 (-0·16 to 0·13) |
0·827 | -0·07 (-0·21 to 0·06) |
0·291 | -0·21 (-0·33 to -0·09) |
0·001 |
| Change in trend in non-priority group | -0·07 (-0·16 to 0·01) |
0·099 | -0·11 (-0·22 to 0·00) |
0·058 | -0·04 (-0·18 to 0·10) |
0·579 | -0·16 (-0·26 to -0·06) |
0·003 | 0·00 (-0·09 to 0·10) |
0·949 | -0·10 (-0·19 to -0·02) |
0·021 |
| R2 | 0·9816 | 0·9877 | 0·9767 | 0·9691 | 0·9590 | 0·9848 | ||||||
Figure 2.
Changes in congenital syphilis rates in the North region 20 months before and after the intervention.
Figure 7.
Changes in congenital syphilis rates in Brazil 20 months before and after the intervention.
Table 2.
Comparison between the post-intervention outcome and the counterfactual in the last month of the analyzed period.
| Priority municipalities |
Non-priority municipalities |
|||||
|---|---|---|---|---|---|---|
| Region | Counterfactual | Observed | Difference (%) | Counterfactual | Observed | Difference (%) |
| North | 18·08 | 13·73 | 24·09 | 5·11 | 3·63 | 28·97 |
| Northeast | 28·11 | 15·75 | 43·95 | 5·33 | 3·63 | 31·79 |
| South | 26·13 | 18·43 | 29·48 | 5·82 | 5·57 | 4·27 |
| Southeast | 20·84 | 16·42 | 21·21 | 8·70 | 5·85 | 32·69 |
| Midwest | 12·52 | 11·50 | 8·11 | 1·94 | 2·86 | -47·86 |
| Brazil | 21·93 | 15·61 | 28·79 | 6·34 | 4·68 | 26·20 |
These results describe the intervention effects in detail for each region, separately. That is because it captures the regionalized influence of the Unified Health System governance—which is interfederative, with clear attributions at local, state, and federal levels. In this sense, as Primary Health Care (PHC) is a responsibility of municipalities, evidence that the SNP effects can vary across regions can be captured.
For the North region of Brazil, in Figure 2 and Table 1 (column 2), for both priority and non-priority municipalities, there was a reduction in the monthly rate of congenital syphilis cases in the post-intervention period. The monthly average reduction was -1·77 cases per 1,000 live births in priority municipalities and -009 per 1,000 live births in non-priority municipalities, as shown in Table 1. In addition, the estimated linear regression models for each situation show changes in the monthly average trends, with a -0·05 reduction in the priority municipalities and a -0·07 reduction for the non-priority ones.
The counterfactual presented in Table 2 shows that for the priority municipalities the model estimated 18·08 cases per 1,000 live births at the end of the 20th month without intervention. In comparison, with intervention, 13·73 cases were observed for the same time point, indicating a decline of 24·09%. In the non-priority municipalities, the model estimated 5·11 monthly cases per 1,000 live births in the 20th month. The observed value with the intervention was 3·63 per 1,000 live births, which represents a fall of 28·97%.
Figure 3 and Table 1 (column 3) display the results for the Northeast region, where an increasing of 2·23 cases per 1,000 live births in immediate impact can be observed post-intervention in priority locations. There was also a 0·34 reduction in cases for non-priority municipalities. A change in trend can be observed for both groups. Non-priority municipalities reversed the upward trend with a monthly slope of -0·11 cases per 1,000 live births. Meanwhile, priority municipalities showed a slope of -0·64 cases per thousand live births post intervention.
Figure 3.
Changes in congenital syphilis rates in the Northeast region 20 months before and after the intervention.
Regarding the counterfactual (Table 2) for this region, at the end of the span analyzed in priority municipalities and without intervention, the model estimated 28·11 cases per 1,000 live births, compared to 15·75 cases observed after intervention (a drop of 43·95% for this group). In non-priority municipalities, the model estimated 5·33 cases in the last month of data collection, while the actual value with the intervention was 3·63 per 1,000 live births, a decline of 31·79%.
As represented in Figure 4 and Table 1 (column 4), priority municipalities in the South region showed a sharp drop to -1·76 monthly cases per 1,000 live births, and a trend change of -0·28 monthly cases per 1,000 live births. Conversely, in the non-priority municipalities there was an increase of 0·48 in monthly cases per 1,000 live births and a minor trend change of -0·04 monthly cases per 1,000 live births.
Figure 4.
Changes in congenital syphilis rates in the South region 20 months before and after the intervention.
The model estimated 26·13 cases per 1,000 live births if no intervention had taken place in the priority municipalities from the South region. The actual value with intervention, was 18·42 cases per 1,000 live births, representing a decline of 29·48%. A slight decrease of 4·27% was observed for non-priority municipalities with an estimated 5·82 counterfactual cases and 5·57 actual cases per 1,000 live births.
The non-priority municipalities in the Southeast region (Figure 5 and Table 1, column 5) went through an increase of 0·13 monthly cases per 1,000 live births and a change in trend with a decrease of -0·16 monthly cases. Whereas the priority municipalities experienced a -1·11 reduction in monthly cases and slightly declining trend of -0·02 monthly cases.
Figure 5.
Changes in congenital syphilis rates in the Southeast region 20 months before and after the intervention.
The counterfactual for this region projected an estimated 20·84 cases per 1,000 live births in priority municipalities (Table 2) in the absence of intervention. However, a reduction of 21·21% to 16·42 cases per 1,000 live births was observed. In the Southeast regions's non-priority municipalities, the counterfactual was 8·70 cases against 5·85 actual cases per 1,000 live births, with a 32·69% reduction in the post-intervention period.
In the Midwest region (Figure 6 and Table 1, column 6), there was a reduction of -0·47 monthly cases in the priority municipalities following the interventions, but an increase of 0·87 monthly cases in the non-priority municipalities. There was a reversal of the trend in the priority municipalities from 0·09 monthly cases per 1,000 live births pre-intervention to -0·07 post interventions. Conversely, in non-priority locations, there was a reversal of the trend in the opposite direction. In this manner, a downward trend of -0·02 monthly cases before intervention changed to 0·00 in the post-intervention period.
Figure 6.
Changes in congenital syphilis rates in the Midwest region 20 months before and after the intervention.
The counterfactual for the post-intervention period in priority municipalities was 12·52 cases per 1,000 live births at the end of the period (Table 2), compared to 16·42 actual cases, which represents a fall of 21·21%. By contrast, the comparison between the counterfactual (1·94) and actual (2·86) cases per 1,000 live births for the non-priority municipalities revealed a 47·86% increase.
The combined analysis of the national data reveals a decline in the immediate impact of congenital syphilis post-intervention, with an average monthly reduction of -0·36 cases per 1,000 live births in the priority municipalities. Conversely, there was an increase of 0·28 cases per 1,000 live births in non-priority municipalities. In the linear regression model, examination of the trends for both groups following the intervention, reveals a decrease in the growth of the average number of cases per 1,000 live births. Hence, there was a reduction of -0·21 in priority municipalities and of -0·10 in non-priority ones, as depicted in Figure 7 and Table 1 (column 7).
For priority municipalities, the combined analysis also indicates a reduction of 28·79% in the number of cases in the last month of the analyzed period (Table 2) when compared the counterfactual of 21·93 with the actual number of 15·61 cases per 1,000 live births. In the non-priority municipalities, there was a drop of 26·20%. Accordingly, it went from 6·34 counterfactual cases to 4·68 actual cases per 1,000 live births.
As to congenital syphilis in priority and non-priority municipalities, the most remarkable differences were found in the Northeast (15·58 per 1,000 live births) and South (15·04 per 1,000 live births) regions, followed by the North (11·39 cases per 1,000 live births), Southeast (8·38 cases per 1,000 live births) and Midwest (6·87 cases per 1,000 live births).
Discussion
The findings indicate a statistically significant reduction in the trend of congenital syphilis cases in Brazil in the 20 months following the Syphilis No! Project interventions. Additionally, the results reveal that priority municipalities experienced a more significant reduction in congenital syphilis cases when compared to other Brazilian municipalities with a greater reduction in the trend.
For priority municipalities, the project's impact on changing the course of congenital syphilis trends was more evident. Unlike the other four Brazilian regions, the most significant change in the growth trend was observed in the Northeast, which showed a sharp drop. Furthermore, decreasing post-intervention trends were observed in the Northeast and South regions. Meanwhile, there was stabilization of the trend in the North. Finally, no changes in trends were found for the South and Midwest regions.
Controlling congenital syphilis depends partly on the capacity of primary health care systems to accommodate the largest number of infected pregnant women and effectively implement treatment algorithms.16 Municipalities with increasing rates of syphilis in pregnant women may indicate a greater ability to control the epidemic for congenital syphilis. Although plausible, this relationship cannot be directly correlated. In other words, many factors can still impact the welcoming and proper treatment of a pregnant person with syphilis (e.g., the administration of penicillin in PHC).17
In the latest evaluations of the quality program of PHC in Brazil, it was identified that the Northeast region held the lowest percentage in the administration of penicillin in the country. The drug administration did not exceed 40% of diagnosed cases of syphilis.18 Then, the insufficient use of penicillin, possibly owed to its supply shortage,19 was normalized in 2017. Moreover, there is also a hypothesis that the resistance of health workers to administer penicillin in pregnant women during prenatal care in PHC contributed to a reduced administration.
As to the comprehensive care axis of SUS, one of the project's actions was to act vigorously in implementing the treatment algorithm for syphilis in pregnant women. That included intervention actions in priority municipalities to promote educational activities for penicillin use in PHC. Thus, the sharpest change in congenital syphilis trends in the Northeast may have resulted from improved treatment of pregnant women with syphilis through the use of penicillin in PHC.
The Northeast of Brazil, where the diagnosis and monitoring of syphilis did not follow the diagnosis, treatment, and notification algorithm featured in the Clinical Protocol and Therapeutic Guidelines (PCDT),20 was one of the few regions where the rates of congenital syphilis were higher than those of syphilis in pregnant women.21 This fact may have contributed to the intensification of RIS interventions that strengthen continuing health training actions, focusing on PCDT. These hypotheses need yet to be tested, but the project's four intervention axes have likely had different effects across different health service networks.
In general, the congenital syphilis epidemic has been identified in several parts of the world, mainly in low-income and middle-income countries.22,23 In Brazil, a study by Santos and colleagues,21 aimed to evaluate trends in congenital syphilis in Brazil in key municipalities from 2007 to 2017, found significant growth trend, with AAPC of 15·75%. Our results concur with these findings and point to an increase in congenital syphilis levels until 2018 when the Syphilis No! Project was effectively implemented.
One of the Project's goals was to reduce congenital syphilis by providing strategic training plan to local management and through the activities performed by RIS in technical areas, whose actions include the axes of i) management and governance, ii) surveillance, iii) comprehensive care, and iv) education and awareness strengthening in priority municipalities.18 The specific actions performed by RIS were the evaluation of the health plans and programs of the municipal health secretariats; the strengthening of vertical transmission investigation committees; the reinforcement of strategic information systems for health surveillance and notification triage; and the operationalization of the line of care for children exposed to syphilis.24
This study's results suggest that the Project's actions influenced the reversal and significant reduction in congenital syphilis trends in Brazil from the year 2018. This reduction was verified at the hospital level by Andrade and colleagues.25 Hence, the researchers conducted a study that evaluated the impact of the Syphilis No! Project in reducing hospitalizations for congenital syphilis in priority municipalities. Their findings revealed that the Project significantly reduced hospital admissions for congenital syphilis, corroborating the changes in the trends of new cases observed in our study.
The counterfactual results revealed that the project was able to reverse the expected projections of congenital syphilis cases. Although the interrupted time series analysis suggests greater reductions in priority areas than non-priority areas, it is important to note that the percentage reductions were similar for these two groups of areas. Further, the results in this study reinforce that the reduction of congenital syphilis did not occur equitably in all five regions of Brazil, even though the project was implemented at a national level. Brazil is a socially and culturally diverse country of continental dimensions. Although it has a healthcare system like SUS, with universal health coverage, there are considerable differences in socioeconomic inequalities,26,27 and resourcing and capabilities of health service in each region28,29 with significant socioeconomic vulnerabilities that influence the response to infectious diseases.30
The changes in the level of cases and trends in the non-priority municipalities which did not receive RIS or specific awareness actions could also be attributed to the spillover effects of the Syphilis No! Project, which was a nationally prominent project and well known in the Unified Health System. The results also unveil changes in trends towards reduction or stabilization in almost all regions (North, Northeast, South, and Southeast). Moreover, when analyzing the impact of the educommunication actions of the SNP, with emphasis on the motto “test, treat, and cure”, Pinto and colleagues12 concluded there was a consistent increase in searches on the topic of syphilis on search engines, as well as increased use of the online learning system by health workers. Given that, it can be inferred that the global actions of the project in the educommunication axis were able to modify, to a lesser extent, the trends of congenital syphilis in non-priority locations.
No impact of the project's universal actions was observed in non-priority municipalities in the Midwest region. Only universal actions of the project were offered to such groups. Those were: mass awareness campaigns to encourage prevention, diagnosis, and treatment, in addition to universal distribution of testing and treatment resources, the instrumentation of situation rooms, and the development of studies and applied research.24 Probably, the actions related to educommunication did not reach their primary objective in this region. Consequently, those activities have not obtained the optimal engagement of local managers and health teams also.
Our study has several limitations. One of them is the absence of measurement on the effects of each intervention axis of the Syphilis No! Project concerning the observed trend changes. Although the recognition of the global effect of the project has been adequately verified, the different levels of installed capacity of epidemiological surveillance in health in the evaluated municipalities may have made it difficult to read and compare the four axes of the project. Future studies that control the level of development of the surveillance system in each location and other health care quality indicators may indicate which actions of the project had the most significant impact. Furthermore, it is natural that the limitation of the study design itself did not capture other effects, such as the influence of differences in socio-regional development, which could impact post-intervention trends.
Of note, this is a quasi-experimental study. Therefore, it is not an experiment in which we would have control over the variables. The reduction in trend observed in some cases was probably influenced by factors beyond the influence of the project. Furthermore, since syphilis is an epidemic in Brazil, the rates were high in some regions. These values were expected to be reduced given the “regression toward the mean” phenomenon. However, this effect could not be measured precisely because the study design did not include a control group, typical of experimental studies.
Another point is that in 2017 MoH changed the case definition criteria for notification of congenital syphilis, which can usually impact the information system and generate underreporting. However, we assume that the new case definition could not significantly change the mathematical models presented in this study. Another limitation of this study is that it was not possible to obtain the exact number of monthly live births. These data were calculated based on the number of annual live births per city, presented by the MoH. Nevertheless, the good amount of data and the high rate of country representation helped to reduce the impact of this limitation.
Notwithstanding these limitations, the findings of our study—which has used statistical tests to verify the effects of an interventions at the national level—indicate that the course of congenital syphilis in Brazil, comparing pre- and post-intervention periods, reveals statistically significant trend changes in monthly rates of disease in Brazil. It also reveals rate variations by region. Furthermore, with only 20 months of the project's implementation, a drop in reported cases per 1,000 live births can be observed in most country regions.
These findings provide an opportunity and direction for future studies on the specific actions implemented by RIS in each state and region by the Syphilis No! Project and examine how the results will change over time following adverse effects and interruptions posed by Covid-19 on the health system.
Declaration of interests
No relevant conflicts of interest.
Acknowledgments
Author's contributions
Conceptualization: RP, LS, RV
Methodology: RP, LS, RV, GS, MS
Software: RP, LS, RV, GS, MS
Validation: RP, LS, GS, TL, CO, MS, AM, ACO, VK, RA, RV
Formal analysis: RP, GS, MS, VK, RA, RV
Investigation: RP, LS, GS, MS, RA, RV
Resources: RP, LS, GS, RV
Data Curation: RP, LS, RV
Writing – original draft preparation: RP
Writing – review and editing: RP, LS, GS, TL, CO, MS, AM, ACO, VK, RA, RV
Visualization: RP, LS, GS, TL, CO, MS, AM, ACO, VK, RA, RV
Supervision: LS, GS, MS, AM, ACO, VK, RA, RV
Project administration: RV
Funding acquisition: RV
Funding
The research is funded by a grant to the Syphilis No! Project from Brazilian Ministry of Health (Project Number: 54/2017). The funders had no role in study design, analysis, decision to publish, or preparation of the manuscript.
Data sharing statement
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2021.100163.
Appendix. Supplementary materials
References
- 1.World Health Organization . World Health Organization; 2017. WHO guideline on syphilis screening and treatment for pregnant women. [PubMed] [Google Scholar]
- 2.World Health Organization . December 2017. WHO — shortages of benzathine penicillin. how big is the problem? and why it matters.https://www.who.int/reproductivehealth/shortages-benzathine-penicillin/en/ (Accessed on 11/05/2021) [Google Scholar]
- 3.Alonso González M. PAHO; 2010. Regional initiative for the elimination of mother-to-child transmission of HIV and congenital syphilis in Latin America and the Caribbean: regional monitoring strategy. [Google Scholar]
- 4.Brasil Ministério da Saúde. Secretaria de Vigilância em Saúde. Boletim epidemiológico - Sífilis. Brasília (DF), (Especial):1–44, 2019.
- 5.Brasil Ministério da Saúde. Secretaria de Vigilância em Saúde. Strategic actions agenda for reducing syphilis in Brazil. Brasília (DF), 2017.
- 6.Valentim RA, Oliveira AC, Dias AD, Olieveira ED, Valentim JL, Moreira JA, Coutinho KD, Trindade SM, Bonfim MA. Educommunication as a strategy to face Syphilis: an analysis of the open educational resources available at AVASUS. Brazilian Journal of Sexually Transmitted Diseases. 2021:1–5. [Google Scholar]
- 7.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. International journal of epidemiology. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cook TD, Campbell DT, Shadish W. Houghton Mifflin; Boston, MA: 2002. Experimental and quasi-experimental designs for generalized causal inference. [Google Scholar]
- 9.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. Journal of clinical pharmacy and therapeutics. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 10.Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Academic pediatrics. 2013;13(6):S38–S44. doi: 10.1016/j.acap.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 11.Pinto R, Silva L, Valentim R, Oliveira C, Lacerda J, Silva R, Paiva J, Kumar V. In2020 IEEE 20th International Conference on Advanced Learning Technologies (ICALT. IEEE; 2020. Assessing the Impact of Public Health Campaigns Through Epidemiological, Communication and Education Indicators; pp. 147–149. [Google Scholar]
- 12.de Morais Pinto R, de Medeiros Valentim RA, Fernandes da Silva L, Santos Lima TGFM, Kumar V, Pereira de Oliveira CA, Martins Gomes de Gusmão C, de Paiva JC, de Andrade I. Vol. 21. BMC Public Health; 2021. pp. 1–3. (Analyzing the reach of public health campaigns based on multidimensional aspects: the case of the syphilis epidemic in Brazil). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berman F, Rutenbar R, Hailpern B, Christensen H, Davidson S, Estrin D, Franklin M, Martonosi M, Raghavan P, Stodden V, Szalay AS. Realizing the potential of data science. Communications of the ACM. 2018;61(4):67–72. doi: 10.1145/3188721. [DOI] [Google Scholar]
- 14.Lucas MC, de Carvalho AL, de Souza EC, Melo CM, dos Santos Crives MN. A experiência de apoio institucional no projeto de resposta rápida ao enfrentamento da sífilis nas redes de atenção à saúde. Revista Brasileira de Inovação Tecnológica em Saúde-ISSN: 2236-1103. 2019:17. [Google Scholar]
- 15.Carroll N. Proceedings of the Western Users of SAS Software 2008 Conference. 2008. Application of segmented regression analysis to the Kaiser Permanente Colorado critical drug interaction program; pp. 5–7. [Google Scholar]
- 16.Rac MW, Revell PA, Eppes CS. Syphilis during pregnancy: a preventable threat to maternal-fetal health. American journal of obstetrics and gynecology. 2017 Apr 1;216(4):352–363. doi: 10.1016/j.ajog.2016.11.1052. [DOI] [PubMed] [Google Scholar]
- 17.Moline HR, Smith JF., Jr The continuing threat of syphilis in pregnancy. Current Opinion in Obstetrics and Gynecology. 2016;28(2):101–104. doi: 10.1097/GCO.0000000000000258. [DOI] [PubMed] [Google Scholar]
- 18.Figueiredo DC, Figueiredo AM, Souza TK, Tavares G, Vianna RP. Relationship between the supply of syphilis diagnosis and treatment in primary care and incidence of gestational and congenital syphilis. Cadernos de Saúde Pública. 2020;36(3) doi: 10.1590/0102-311X00074519. [DOI] [PubMed] [Google Scholar]
- 19.Chaves LA, Chaves GC, Vianna MN, Oliveira MA. Desabastecimento de medicamentos na literatura científica da saúde: uma revisão narrativa. PHYSIS: revista de saúde coletiva. 2019;29 [Google Scholar]
- 20.de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis D. Protocolo clínico e diretrizes terapêuticas para atenção integral às pessoas com infecções sexualmente transmissíveis (IST). http://www.aids.gov.br/pt-br/pub/2015/protocolo-clinico-e-diretrizes-terapeuticas-para-atencao-integral-pessoas-com-infeccoes (2015). (Accessed on 14/07/2021).
- 21.Marques dos Santos M, Lopes AK, Roncalli AG, Lima KC. Trends of syphilis in Brazil: a growth portrait of the treponemic epidemic. Plos One. 2020;15(4) doi: 10.1371/journal.pone.0231029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Korenromp EL, Rowley J, Alonso M, Mello MB, Wijesooriya NS, Mahiané SG, Ishikawa N, Le LV, Newman-Owiredu M, Nagelkerke N, Newman L. Global burden of maternal and congenital syphilis and associated adverse birth outcomes—Estimates for 2016 and progress since 2012. PloS one. 2019;14(2) doi: 10.1371/journal.pone.0211720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newman L, Kamb M, Hawkes S, Gomez G, Say L, Seuc A, Broutet N. Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. PLoS medicine. 2013;10(2) doi: 10.1371/journal.pmed.1001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis D. Agenda de ações estratégicas para redução da sífilis congênita. http://www.aids.gov.br/pt-br/pub/2016/agenda-de-acoes-estrategicas-para-reducao-da-sifilis-congenita (2016). (Accessed on 03/07/2021).
- 25.de Andrade IG, de Medeiros Valentim RA, de Oliveira CA. The influence of the No Syphilis Project on congenital syphilis admissions between 2018 and 2019. Brazilian Journal of Sexually Transmitted Diseases. 2020:1–6. [Google Scholar]
- 26.Massuda A, Hone T, Leles FA, de Castro MC, Atun R. The Brazilian health system at crossroads: progress, crisis and resilience. BMJ global health. 2018;3(4) doi: 10.1136/bmjgh-2018-000829. https://gh.bmj.com/content/3/4/e000829 URL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Castro MC, Massuda A, Almeida G, Menezes-Filho NA, Andrade MV, de Souza Noronha KV, Rocha R, Macinko J, Hone T, Tasca R, Giovanella L. Brazil's unified health system: the first 30 years and prospects for the future. The lancet. 2019;394(10195):345–356. doi: 10.1016/S0140-6736(19)31243-7. [DOI] [PubMed] [Google Scholar]
- 28.Oliveira AP, Gabriel M, Poz MR, Dussault G. Challenges for ensuring availability and accessibility to health care services under Brazil's Unified Health System (SUS) Ciência & Saúde Coletiva. 2017;22:1165–1180. doi: 10.1590/1413-81232017224.31382016. [DOI] [PubMed] [Google Scholar]
- 29.Cecilio LC, Reis AA. Notes on persistent challenges for basic health care in Brazil. Cadernos de Saúde Pública. 2018;34 doi: 10.1590/0102-311X00056917. [DOI] [PubMed] [Google Scholar]
- 30.Rocha R, Atun R, Massuda A, Rache B, Spinola P, Nunes L, Lago M, Castro MC. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. The Lancet Global Health. 2021 doi: 10.1016/S2214-109X(21)00081-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.