Summary
Background
Geographic accessibility to healthcare services is a fundamental component in achieving universal health coverage, the central commitment of the Brazilian Unified Health System (SUS). For cancer patients, poor accessibility has been associated with inadequate treatment, worse prognosis, and poorer quality of life.
Methods
We explored nationwide healthcare data from the SUS health information systems, and mapped the geographic accessibility to cancer treatment in two time-frames: 2009–2010 and 2017–2018. We applied social network analysis (SNA) to estimate the commuting route, flow, and distances travelled by cancer patients to undergo surgical, radiotherapy, and chemotherapy treatment.
Findings
A total of 12,751,728 treatment procedures were analyzed. Overall, more than half of the patients (49·2 to 60·7%) needed to travel beyond their municipality of residence for treatment, a fact that did not change over time. Marked regional differences were observed, as patients living in the northern and midwestern regions of the country had to travel longer distances (weighted average of 296 to 870 km). Cancer care hubs and attraction poles were mostly identified in the southeast and northeast regions, with Barretos being the main hub for all types of treatment throughout time.
Interpretation
Important regional disparities in the accessibility to cancer treatment in Brazil were revealed, suggesting the need to review the distribution of specialized care in the country. The data presented here contribute to ongoing research on improving access to cancer care and can provide reference to other countries, offering relevant data for oncological and healthcare service evaluation, monitoring, and strategic planning.
Funding
This work was funded by the Oswaldo Cruz Foundation - Fiocruz (Inova - no. 8451635123 to BPF) and the National Council for Scientific and Technological Development - CNPq (no. 407060/2018–9 to BPF); Coordination for the Improvement of Higher Education Personnel – CAPES (scholarship to PCA, Finance Code 001); and Instituto Nacional de Ciência e Tecnologia de Inovação em Doenças de Populações Negligenciadas (INCT-IDPN).
Resumo
A acessibilidade geográfica aos serviços de saúde é um componente fundamental para o alcance da cobertura universal de saúde, compromisso central do Sistema Único de Saúde (SUS). Para pacientes com câncer, a baixa acessibilidade aos serviços especializados tem sido associada ao tratamento inadequado, piora no prognóstico e na qualidade de vida.
Neste estudo, dados de saúde dos sistemas de informação em saúde do SUS foram utilizados para mapear a acessibilidade geográfica ao tratamento do câncer em dois períodos: 2009–2010 e 2017–2018. Aplicamos a análise de redes sociais (ARS) para estimar os fluxos de deslocamento e as distâncias percorridas por pacientes com câncer para receberem tratamento cirúrgico, radioterápico e quimioterápico.
Um total de 12.751.728 procedimentos de tratamento foram analisados. Em geral, mais da metade dos pacientes (49,2 a 60,7%) precisaram se deslocar de seus municípios de residência para receber tratamento, fato que não mudou comparando os dois períodos de tempo analisados. Foram observadas importantes diferenças regionais no acesso. Pacientes residentes das regiões norte e centro-oeste do país tiveram que percorrer maiores distâncias para alcançar os serviços (média ponderada = 296 a 870 km). A maioria dos hubs e polos de atração para atendimento oncológico foram identificados nas regiões Sudeste e Nordeste, sendo o município de Barretos o principal hub para todos os tipos de tratamento ao longo do tempo.
As disparidades de acessibilidade para o tratamento de câncer, alertam para a necessidade de revisar a distribuição dos serviços de atenção especializada no país. A metodologia e os resultados apresentados neste estudo contribuem para as pesquisas sobre a melhoria do acesso ao tratamento do câncer e podem servir como referência para outros países, oferecendo dados relevantes para avaliação, monitoramento e planejamento estratégico de serviços oncológicos e de saúde em geral.
Keywords: Health services access, Cancer treatment, Geographic accessibility, Brazil, Social network analysis
Research in context.
Evidence before this study
There is little documented evidence on how well the Brazilian Unified Health System (SUS) is fulfilling its mission of adequately providing universal healthcare to the population. Cancer is the second leading cause of death in Brazil, and there has been increasing attention to providing patients with timely access to treatment. Searching Scopus and the SciELO regional database for publications on the geographic accessibility of cancer treatment in Brazil as of May 2021, by using “Brazil”, “cancer”, “accessibility” and “treatment” as search terms, only a few studies were identified. These were focused on breast cancer treatment and mostly limited to a single period of time.
Added value of this study
This is the first study to address the evolution of geographical accessibility to cancer treatment in Brazil. We have explored the SUS national dataset and collected more than 12 million treatment records, for all types of solid tumors in two different biennia, ten years apart. The analysis provided the most comprehensive assessment of the commuting distance required for cancer patients to receive specialized healthcare in Brazil. Through network analysis we were able to identify cancer care hubs and attraction poles to inform an evidence-based rational planning, monitoring and evaluation of SUS oncological care services in the country.
Implication of all the available evidence
Geographic accessibility of cancer treatment in Brazil has developed slowly over the past decade. Regional disparities mainly hinder patients from northern and midwestern states. The concentration of cancer care centers and the attractiveness of the southeast region indicate a need to properly balance the supply and demand for specialized care. Better planning and regulation are required to ensure wide coverage of cancer treatment, while preventing the idleness of high complexity infrastructure and specialized human resources.
Alt-text: Unlabelled box
Introduction
Access to quality healthcare services is a fundamental component in achieving Universal Health Coverage (UHC), a major health policy mandate as the world advances towards the proposed United Nations’ Sustainable Development Goals (SDGs).1 Access can be defined as the opportunity to reach and obtain appropriate health care services in situations of perceived need for care. It results from the interface between the characteristics of persons, households, social and physical environments, and the characteristics of health systems, organizations, and providers.2
Accessibility is a concept related to the characteristics of health systems that can facilitate or limit the use of health services by potential users, affecting the balance between the demand and provision of adequate services.3 Thus, health services are accessible if their specific characteristics – geographic disposition, organization, affordability, and acceptability – allow people to reach, enter and use them.3,4 Accessibility is, therefore, an important factor associated with variations in the use of health services, and represents a relevant dimension in studies on equity in health systems.5,6
Geographic accessibility reflects aspects of the spatial distribution of health services offered, which hinder or promote their utilization.3 It refers to the ease with which residents of a given area can reach services and facilities, which can be measured using different approaches.7 In this study, geographic accessibility is expressed as the physical distance between the service delivery point and the user's place of residence.8
Studies have demonstrated that poor geographical accessibility to healthcare services contributes to lower levels of service utilization, which in turn gives rise to poorer health outcomes.9 This is especially important for cancer patients, as treatment is often multimodal – involving surgery, radiotherapy, and/or chemotherapy – and may require repeated visits to healthcare facilities. When distance hinders accessibility, delayed treatment could potentially lead to suboptimal care or even premature and/or avoidable death. Increasing travel requirements for cancer patients have been associated with more advanced disease at the time of diagnosis, inadequate treatment, a worse prognosis, and a poorer quality of life.10
Social network analysis (SNA) has been increasingly used in healthcare settings, as it offers a means of understanding this complex system.11 SNA has been applied as a tool to map healthcare staff communication networks,12 factors that determine the patient's choice of surgical treatment,13 patients’ flow between hospitals14 and, patient's accessibility to health services.15, 16, 17 Through SNA, the analysis of commuting networks for treatment may reveal weaknesses in the health system organization, thereby identifying regional disparities, geographical gaps, and overloaded health centres. Assessing the distance travelled between the patients’ residence and hospital can be a useful and sensitive indicator of their difficulty in accessing healthcare.
The Brazilian Unified Health System (Sistema Único de Saúde – SUS), a tax-funded, universal health scheme,18 subsidizes cancer treatment for approximately 75% of the population.19 The primary care network is the patient's entryway to the health system, playing a decisive role in actions to promote health, prevent and track cancer. If cancer is suspected, the patient seen in the primary care unit is referred to secondary care for further investigation. Once the diagnosis is confirmed, the patient is referred to tertiary specialized care units that provide high-complexity and comprehensive care. These include (1) oncology centers (Centros de Assistência de Alta Complexidade em Oncologia – CACONs); (2) oncology units (Unidades de Assistência de Alta Complexidade em Oncologia – UNACONs); and (3) hospital complexes (general hospitals with cancer surgery and radiotherapy services). At this level, diagnostic confirmation is performed, as well as disease staging and treatment of patients diagnosed with cancer, including surgery, chemotherapy, and radiotherapy, in addition to the coordination of palliative care. Oncological treatments provided by SUS are carried out by accredited health institutions, whether public or private, for-profit or non-profit. Each treatment session is registered in the health information systems, which, among other functions, manages the recording and billing of medical procedures.
The Brazilian National Cancer Care Policy emphasizes the need to provide timely treatment near the patients’ homes, which is an enormous challenge given the growing demand.20,21 However, few studies provide evidence to support the assessment of geographic accessibility of cancer treatment, especially with a historical review to monitor its evolution over time. The shortage of data on the mapping, number of patients, and quality of cancer care is a major obstacle to creating evidence-based policies.22 By 2020, 625,000 new cases of cancer were estimated in Brazil23 and, given the increasing impact on specialized centres, the understanding of the geographic accessibility to these services can generate evidence and inform future planning and management.
In this paper, SNA was used as a strategic tool to generate data to support the evaluation, monitoring, and management of healthcare services by analyzing the commuting route, flow, and travel distance of cancer patients receiving treatment within SUS, over time. Two knowledge gaps were addressed: (i) whether SUS has been geographically accessible to provide cancer treatment, over time, and (ii) whether SNA can offer evidence for the management of health services. The paper adds value to the global discussion on improving access to cancer care,24,25 and can be used as a reference to other countries, to offer relevant data for the oncological and healthcare service evaluation, monitoring, and strategic planning.
Methods
A retrospective, cross-sectional analysis was conducted using two independent datasets, separated by 10 years. Each dataset included cancer treatment records of patients residing in one of the 5,570 municipalities located in 26 Brazilian states, in five geographical regions.26 Through SNA, the commuting route and flow of cancer patients from their place of residence to the hospital for surgical, chemotherapy, and radiotherapy treatment were mapped. The analysis only included patient records in which the pair of municipalities was different. The hubs and attraction poles with increased demand for oncological services were identified and distances travelled by patients were estimated.
To examine trends in the access to oncological services over time we collected data from two biennia: 2009–2010 and 2017–2018, to characterize two implementation phases of the National Cancer Care Policy. The “expansion phase” (2005–2012), characterized by the structuring of oncology pathways of care, focused on improving the patients’ therapeutic itinerary; and the “integration phase” (2013–2018), which focused on establishing a healthcare network model, with new standards and parameters.27
Database description
The SUS Information Technology Department (DATASUS) maintains a large set of nationwide health information systems that gather data from various aspects of the Brazilian population, including morbidity and mortality data, health services, administrative and financial data. For this study, data on surgical procedures were extracted from the SUS Hospital Information System (SIH-SUS) and data from chemotherapy and radiotherapy procedures were retrieved from the Ambulatory Information System (SIA-SUS).
SIH-SUS and SIA-SUS were developed in the 1990s and are the primary source data for hospitalizations and ambulatorial procedures of the Brazilian Ministry of Health. SIH-SUS is responsible for processing the information from Hospital Admissions Authorizations (AIHs). SIA-SUS contains all data related to ambulatorial care, including High Complexity Procedure Authorizations (APACs), required for procedures carried out by SUS-accredited institutions. Both systems have a primary focus on administration, being used as instruments to assist managers in the planning, control, billing, and auditing of health services. The systems include information on the service provided, the International Classification of Diseases code (ICD-10)28 associated with each procedure, patients’ municipality of residence, the municipality where the procedure was carried out, among other information. Both systems are updated monthly and have been widely used to support retrospective health studies in Brazil.29,30
The current study was exempted from ethical review considering that only public and aggregate data from DATASUS was used, without any individual identification.
Data extraction, processing, and validation
Data on the municipality of residence and municipality of treatment of all patients with a primary diagnosis of cancer were extracted from the DATASUS database, for two biennia, 10 years apart – January 2009 to December 2010 and January 2017 to December 2018.
AIHs for surgical procedures (SIH-SUS code 04.16), and APACs for chemotherapy (SIA-SUS codes 03.04.02 to 03.03.08), and radiotherapy (SIA-SUS code 03.04.01) were used as proxies for surgical, chemotherapy, and radiotherapy treatment. Each AIH and APAC has a specific validity that varies from 15 to 90 days (except for urgent/emergency procedures). This implies that if a patient undergoes more than one treatment procedure within 90 days, his/her trips to the treatment facility are only counted once. Given the large number of records evaluated herein (more than 12 million), we believe that a potential bias would be offset. Note that the dataset is formed by authorizations of treatment procedures (AIHs and APACs), not individual patients receiving treatment. Since each authorization is related to a single patient, the number of authorizations was used as a proxy for the number of patients.
The ICD-10 codes C00-C75, corresponding to “malignant neoplasms, stated or presumed to be primary (of specified sites)”,28 were used to filter for patients’ records with a primary diagnosis of cancer. These include patients of all ages, with cancers of the lip, oral cavity and pharynx, digestive organs, respiratory system and intrathoracic organs, bone, skin, mesothelioma and soft tissue, breast, female and male genital organs, urinary tract, eye, brain and other parts of the central nervous system, and thyroid and other endocrine glands.
A non-relational database (NoSQL) was created using the ElasticSearch software (www.elastic.co). Data extraction and loading were carried out by an extraction, transformation, and loading methodology (ETL) using the Dataiku DSS software (www.dataiku.com), in addition to the R and Python languages.31 All data were audited following DATASUS information as the gold standard. After checking and validating, the data from SIH-SUS were made available for public use at https://bigdata-metadados.icict.fiocruz.br/dataset/sistema-de-informacoes-hospitalares-do-sus-sihsus/resource/7b8a74d7–72da-4b8f-9eec-d973486c450c. After filtering for the codes of interest, the final study dataset for the two periods of time comprised of a total of 12,751,728 treatment procedures: 391,525 surgeries (3·0%), 2,841,879 radiotherapy (22·2%) and 9,518,324 chemotherapy (74·6%) procedures.
Travel distance estimates
The OSRM version 3.0.1 software package of the OpenStreetMap project (www.openstreetmap.org) was used to obtain estimates of road distances between patients’ municipality of residence (origin) and the municipality of treatment (destination). The analysis included all records in which the pair of municipalities was different. These measurements were based on the best route between the two given municipalities, derived from the centroid of each municipality, using OpenStreetMap's road network.
The weighted average distance travelled by patients was calculated by summing up the product of the travel distance between an origin/destination pair of municipalities times the number of patients travelling between them, divided by the total number of patients that had to travel to receive treatment. One-way distances travelled to the treatment facilities were grouped as up to 100, 100 to 250, 250 to 500, 500 to 1000, and more than 1000 km.
Network assembly, visualization, and analysis
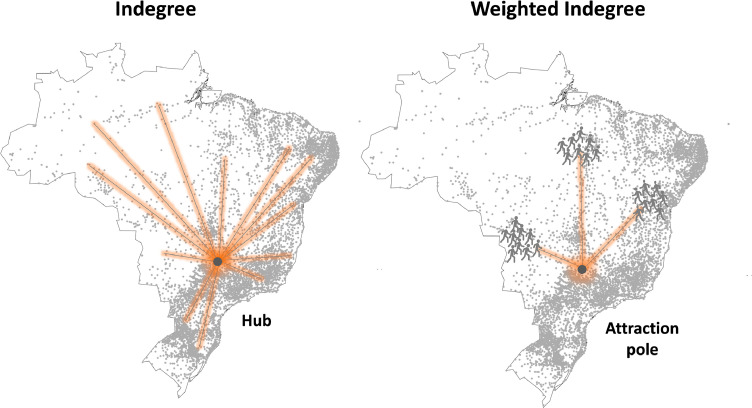
The units of analysis were the residence (origin) and treatment (destination) municipalities. The analysis only included records in which the pair of municipalities was different. A pair of origin/destination municipalities define a connection and the number of people moving between them establishes a flow. The connections between municipalities were directional (origin to destination) and asymmetrical (the origin/destination connection was not reciprocal), and weighted by the number of patients commuting between each pair of municipalities. Each municipality in the network was analyzed using the metrics described in Table 1 and illustrated in Figure 1. Network visualizations and metric calculations were done in Gephi 0.9.2 (www.gephi.org).
Table 1.
SNA metrics used in this study and their meanings.
| Metric | Definition | Meaning in this study |
|---|---|---|
| Indegree | Total number of unique connections in direction to a given node | The destination municipality is used as reference. It quantifies the number of different municipalities (origin) from which patients traveled to the municipality where the treatment was carried out (destination). A higher indegree indicates a hub for cancer care. |
| Weighted indegree | Total number of unique connections in direction to a given node, weighted by the frequency of the connections | The destination municipality and the number of patients are used as references. It quantifies the flow of patients who have traveled to the destination municipality for treatment. A higher weighted indegree indicated an attraction pole for cancer care. |
Figure 1.
Schematic representations of the SNA metrics used in this study. Indegree quantifies the number of different residence municipalities (origin) from which patients travelled to the treatment municipality (destination) (left panel). Weighted indegree quantifies the flow of patients who have travelled to the destination municipality for treatment (right panel). Indegree was used to identify hubs and weighted indegree was used to identify attraction poles of oncological treatment.
Statistical analysis
Statistical analysis was performed with Minitab Statistical Software v.20 (Minitab Inc, State College, PA, USA). Data were checked for normality in distribution and Student's t-test was applied to compare weighted average distances travelled by residents of each Brazilian state on the two time periods evaluated. The level of statistical significance was assumed at p < 0.05.
Role of the funding source
This work was funded by the Oswaldo Cruz Foundation - Fiocruz (Inova - no. 8451635123 to BPF) and the National Council for Scientific and Technological Development - CNPq (no. 407060/2018–9 to BPF); Coordination for the Improvement of Higher Education Personnel – CAPES (scholarship to PCA, Finance Code 001); and Instituto Nacional de Ciência e Tecnologia de Inovação em Doenças de Populações Negligenciadas (INCT-IDPN). The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript. All authors had full access to all the data in the study and accept the responsibility to submit it for publication.
Results
More than half of the cancer patients had to travel to receive treatment
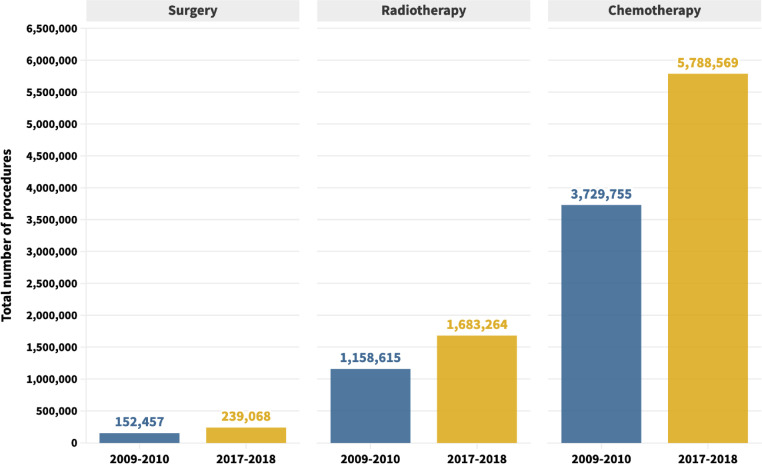
Between 2009 and 2010, 152,457 surgical, 1158,615 radiotherapy, and 3,729,755 chemotherapy procedures were performed, regardless of the need to travel (Figure 2). This number has increased 56·8% for surgeries, 45·3% for radiotherapy, and 55·2% for chemotherapy procedures in 2017–2018 (Figure 2).
Figure 2.
Total number of cancer treatment procedures carried out within SUS (2009–2010 and 2017–2018).
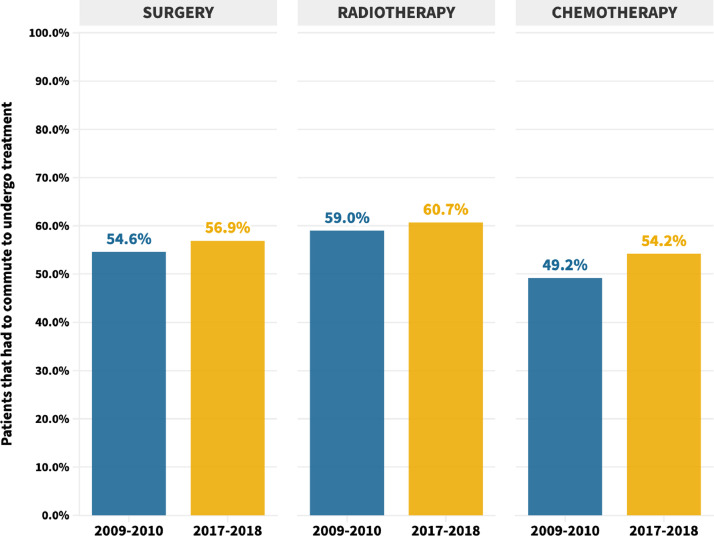
More than half of all cancer patients treated in SUS had to commute from their municipality of residence to receive treatment (Figure 3). In 2009–2010, 54·6%, 59·0% and 49·2% of the patients that received surgical, radiotherapy, or chemotherapy treatment had to commute to other municipalities, respectively. The corresponding figures for 2017–2018 slightly increased to 56·9%, 60·7%, and 54·2%, respectively (Figure 3). Interstate commuting remained relatively unchanged over time: from 2·0%, 3·3%, and 2·3% in the first biennium to 2·1%, 3·0%, and 2·3% in the second biennium, for surgeries, radiotherapy, and chemotherapy, respectively (data not shown).
Figure 3.
Percentage of patients that had to commute from their municipalities of residence to receive SUS cancer treatment.
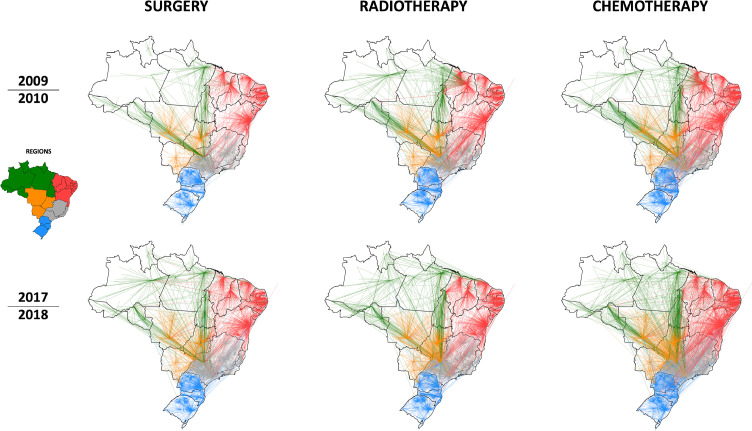
The patients’ commuting networks are shown in Figure 4. Each node is a municipality and the link between them indicates the origin/destination patient flow. The color of the link indicates the macro-region (north, northeast, midwest, southeast, or south) where the patient lived. A visual inspection of the networks revealed that patients’ commutes were mainly within regional and/or state boundaries. However, in addition to flows between the north (green links) and northeast (red links) regions, to midwest municipalities, there were obvious connections between municipalities in the north, northeast, and midwest (orange links) regions with municipalities in the southeast region (gray) (Figure 4).
Figure 4.
Commuting networks of patients that received cancer treatment within SUS. Each node is a municipality and a connection between them indicates an origin/destination flow of patients. The color of the links indicates the macro-region where the patient's municipality of residence was located: north = green; northeast = red; southeast = gray; midwest = orange; south = blue. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Marked regional accessibility inequalities have not changed over time
In 2009–2010, cancer patients who had to commute to receive treatment travelled a weighted average of 166·9 km, 167·8 km, and 139·2 km for surgical, radiotherapy, or chemotherapy treatment, respectively (Table 2). These values remained similar in 2017–2018, with 152·8 km for surgeries, 167·1 km for radiotherapy, and 139·0 km for chemotherapy. The median travel distances indicated that, in the two biennia, at least half of all cancer patients that had to commute to receive treatment within SUS travelled more than 170·3–187·3 km to receive treatment (Table 2). The three types of treatment had similar travel distance profiles over the entire period: 52·6 to 60·0% of patients had to travel less than 100 km, 26·2 to 29·3% of patients travelled between 100 and 250 km, 10·6 to 13·5% travelled from 250 to 500 km, 2·3 to 4·3% travelled from 500 to 1,000 km, and 0·8 to 1·3% travelled more than 1,000 km to receive treatment (Table 2).
Table 2.
Distances travelled by cancer patients to reach a SUS treatment facility.
| Distance travelled to receive treatment (km) |
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment type | 2009–2010 |
2017–2018 |
||||||||||||||||||
| Number of patientsa | Average (SD) | Weighted average | Median (IQR) | Max. | Min. | Number of patientsa | Average (SD) | Weighted average | Median (IQR) | Max. | Min. | |||||||||
| Surgery | 152,457 | 306·1 (473·1) |
166·9 | 170·3 (88·0–343·6) |
7,297 | 7·9 | 239,068 | 344·2 (574·7) |
152·8 | 171·4 (89·0–349·0) |
7,155 | 0·5 | ||||||||
| Radiotherapy | 1,158,615 | 333·4 (476·8) |
167·8 | 188·4 (101·4–364·9) |
5,170 | 7·9 | 1,683,264 | 341·6 (529·6) |
167·1 | 183·2 (98·5–366·8) |
6,675 | 7·9 | ||||||||
| Chemotherapy | 3,729,755 | 330·2 (493·5) |
139·2 | 181·6 (94·6–360·4) |
6,970 | 7·9 | 5,788,569 | 377·7 (588·5) |
139·0 | 187·3 (96·7–290·9) |
7,066 | 0·4 | ||||||||
| Number of patientsa,b that travelled to receive treatment |
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment type | 2009–2010 |
2017–2018 |
||||||||||||||||||
| <100 km | 100–250 km | 250–500 km | 500–1,000 km | >1,000 km | <100 km | 100–250 km | 250–500 km | 500–1,000 km | >1,000 km | |||||||||||
| Surgery | 43,727 (52·6%) |
23,989 (28·8%) |
11,083 (13·3%) |
3,591 (4·3%) |
767 (0·9%) |
77,538 (57·2%) |
37,340 (27·5%) |
14,712 (10·8%) |
4,718 (3·5%) |
1,343 (1·0%) |
||||||||||
| Radiotherapy | 358,834 (52·6%) |
199,242 (29·2%) |
92,400 (13·5%) |
23,298 (3·4%) |
8,747 (1·3%) |
538,902 (52·9%) |
299,153 (29·3%) |
130,198 (12·8%) |
39,144 (3·8%) |
12,028 (1·2%) |
||||||||||
| Chemotherapy | 1,074,055 (58·6%) |
502,308 (27·4%) |
199,387 (10·9%) |
41,303 (2·3%) |
14,665 (0·8%) |
1,875,411 (60·0%) |
818,106 (26·2%) |
330,025 (10·6%) |
78,526 (2·5%) |
24,277 (0·8%) |
||||||||||
The number of authorizations were used as proxies of the number of patients (see Methods).
Percentages are relative to the total number of patients who had to travel to receive treatment.
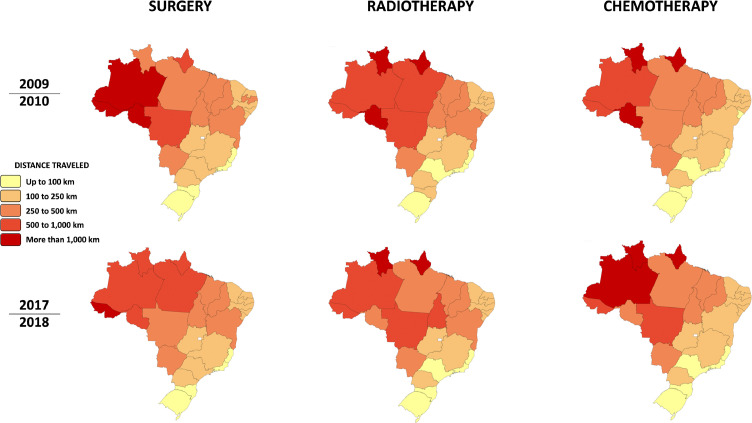
Regional analysis showed a marked difference in the weighted mean distance travelled by patients who had to commute to receive treatment according to their place of residence (Figure 5). A lighter color stripe on the right side of the map indicates residence states in which patients commuted shorter distances to be treated.
Figure 5.
Representation of weighted average distances travelled by cancer patients to receive treatment within SUS. Average road distances between each origin/destination pair were estimated and weighted according to the number of patients traveling between them. One-way distances to the treatment facilities were grouped in kilometers as: up to 100, 100 to 250, 250 to 500, 500 to 1,000, and more than 1,000 km.
In the two biennia, patients living in municipalities of the north region travelled the largest distances to be treated (Table 3). Nearly half (48%) surgical patients living in northern states travelled a weighted average distance of 612 km to receive treatment in 2017–2018. All patients living in the states of Roraima and Amapá had to commute to undergo radiotherapy, traveling a weighted average distance of more than 2,000 km, in both biennia. In both biennia, patients living in the midwest regions who had to commute to receive treatment travelled a weighted average distance of more than 300 km for radiotherapy or chemotherapy treatment. Patients living in the southeast and south regions usually travelled less: a weighted average distance ranging from 90 to 134 km over time (Table 3).
Table 3.
Number of patients, and weighted average distances travelled to receive cancer treatment by region and state of residencea.
| Region/State | SURGERY |
RADIOTHERAPY |
CHEMOTHERAPY |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009–2010 |
2017–2018 |
Change (%) | 2009–2010 |
2017–2018 |
Change (%) | 2009–2010 |
2017–2018 |
Change (%) | |||||||
| Number of patientsb,c | Distance (SD) | Number of patientsb,c | Distance (SD) | Number of patientsb,c | Distance (SD) | Number of patientsb,c | Distance (SD) | Number of patientsb,c | Distance (SD) | Number of patientsb,c | Distance (SD) | ||||
| North |
1,643 (34%) |
767 km (1,082·1) |
3,507 (48%) |
612 km (887·4) |
−9·4* |
18,841 (42%) |
870 km (912·1) |
37,834 (52%) |
702 km (964·5) |
−19·3* |
35,565 (38%) |
656 km (865·7) |
80,380 (45%) |
543 km (830·4) |
−17·1* |
| Acre | 105 (33%) |
1,183 km (1,706·1) |
112 (42%) |
1,287 km (1,757·8) |
8·8 | 1,154 (33%) |
885 km (1,063·3) |
2,203 (83%) |
871 km (788·0) |
−1·6 | 1,528 (29%) |
925 km (1,128·3) |
3714 (39%) |
800 km (992·1) |
−13·5* |
| Amazonas | 27 (1%) |
1,890 km (2,034·5) |
426 (22%) |
895 km (1,133·3) |
−52·7* | 2,074 (25%) |
749 km (882·3) |
1,457 (10%) |
875 km (1,114·4) |
16·7* | 1,867 (10%) |
852 km (1,022·5) |
2,471 (6%) |
1,327 km (1,593) |
55·7* |
| Amapá | 49 (42%) |
609 km (1,005·7) |
88 (38%) |
961 km (1,211·7) |
57·8 | 156 (100%) |
3,216 km (738·3) |
2,289 (100%) |
2,506 km (959·7) |
−22·1* | 591 (27%) |
1,396 km (2062·3) |
1656 (32%) |
2,167 km (2487) |
55·2* |
| Pará | 859 (63%) |
416 km (603·1) |
1,572 (63%) |
526 km (749·3) |
26·5* | 5,214 (29%) |
831 km (817·8) |
17,284 (52%) |
443 km (531·4) |
−46·7* | 13,640 (39%) |
397 km (576·4) |
33,747 (52%) |
448 km (595·0) |
12·7* |
| Rondônia | 257 (85%) |
2,277 km (1,038·5) |
659 (62%) |
605 km (831·1) |
−73·4* | 5,436 (64%) |
1,203 km (920·5) |
8,035 (67%) |
408 km (540·4) |
−66·1* | 8,285 (68%) |
1,282 km (924·8) |
21,134 (63%) |
490 km (588·4) |
−61·8* |
| Roraima | 28 (17%) |
403 km (701·6) |
659 (62%) |
692 km (1,158·2) |
71·8 | 397 (100%) |
2,028 km (1,914·7) |
1,143 (100%) |
3,020 km (2,263·2) |
48·9* | 372 (16%) |
2,122 km (2,082·2) |
21,134 (63%) |
3,045 km (1,839·6) |
43·5* |
| Tocantins | 318 (55%) |
297 km (369·6) |
561 (60%) |
446 km (593·9) |
50·2* | 4,410 (68%) |
365 km (224·8) |
5,423 (93%) |
569 km (452·1) |
55·9* | 9292 (56%) |
286 km (257·0) |
16,973 (63%) |
374 km (428·5) |
30·7* |
| Northeast |
19,486 (60%) |
208 km (262·6) |
31,097 (62%) |
198 km (269·2) |
−20·2* |
143,288 (61%) |
219 km (294·3) |
242,835 (62%) |
210 km (231·2) |
−4·3* |
389,182 (50%) |
191 km (264·1) |
737,630 (58%) |
184 km (217·5) |
−3·4* |
| Alagoas | 379 (47%) |
163 km (334·6) |
1,034 (51%) |
141 km (304·7) |
−13·3 | 7,678 (57%) |
154 km (267·7) |
12,822 (57%) |
104 km (203·1) |
−32·5* | 16,027 (46%) |
165 km (328·2) |
40,027 (54%) |
123 km (235·1) |
−25·6* |
| Bahia | 3,985 (59%) |
301 km (248·9) |
6,760 (56%) |
289 km (262·6) |
−4·1* | 30,228 (64%) |
266 km (257·2) |
62,296 (59%) |
275 km (252·6) |
3·5* | 83,552 (50%) |
250 km (232·9) |
180,738 (56%) |
244 km (233·3) |
−2·2* |
| Ceará | 3,079 (43%) |
178 km (187·4) |
4781 (59%) |
180 km (221·2) |
1·3 | 19,365 (45%) |
166 km (217·6) |
40,491 (59%) |
172 km (165·5) |
3·7* | 62,716 (36%) |
162 km (200·0) |
129,126 (54%) |
166 km (156·4) |
2·6* |
| Maranhão | 1,372 (58%) |
294 km (451·4) |
2,973 (58%) |
252 km (383·2) |
−14·2* | 14,504 (59%) |
340 km (384·5) |
21,747 (58%) |
239 km (302·4) |
−29·9* | 20,385 (57%) |
404 km (540·7) |
42,883 (48%) |
266 km (334·9) |
−34·1* |
| Paraíba | 1,520 (67%) |
212 km (331·8) |
2,430 (66%) |
198 km (280·3) |
−6·8 | 10,847 (62%) |
190 km (276·3) |
16,755 (64%) |
187 km (191·7) |
−1·7 | 31,843 (50%) |
206 km (275·6) |
63,736 (61%) |
187 km (215·2) |
−9·1* |
| Pernambuco | 6,364 (75%) |
138 km (192·5) |
8,448 (74%) |
131 km (198·6) |
−4·9* | 33,448 (75%) |
147 km (198·6) |
42,009 (76%) |
161 km (218·4) |
9·3* | 100,416 (61%) |
108 km (163·7) |
163,262 (66%) |
115 km (159·9) |
7·0* |
| Piauí | 1,204 (60%) |
308 km (236·2) |
1,025 (57%) |
333 km (422·5) |
8·2 | 9,010 (60%) |
288 km (210·7) |
26,142 (58%) |
299 km (188·6) |
3·8* | 22,040 (55%) |
300 km (236·5) |
41,525 (56%) |
294 km (208·3) |
−2·1* |
| Rio Grande do Norte | 1,081 (58%) |
180 km (218·6) |
3,224 (59%) |
145 km (207·0) |
−19·2* | 13,373 (64%) |
199 km (303·8) |
13,801 (59%) |
139 km (220·0) |
−30·4* | 40,108 (50%) |
178 km (290·9) |
63,272 (59%) |
153 km (210·4) |
−14·4* |
| Sergipe | 502 (65%) |
146 km (365·7) |
422 (68%) |
136 km (330·0) |
−7·1 | 4,835 (60%) |
375 km (698·2) |
6,722 (72%) |
106 km (190·2) |
−71·8* | 12,095 (55%) |
101 km (181·7) |
13,061 (70%) |
110 km (234·0) |
9·5* |
| Midwest |
4,908 (58%) |
326 km (369·8) |
9,692 (62%) |
296 km (347·6) |
−4·7* |
37,448 (62%) |
345 km (336·0) |
60,098 (66%) |
341 km (322·7) |
−1·1 |
85,153 (49%) |
306 km (287·0) |
170,978 (56%) |
319 km (350·6) |
4·3* |
| Goiás | 3,032 (60%) |
219 km (205·8) |
6061 (64%) |
213 km (232·4) |
−2·7 | 19,547 (58%) |
212 km (170·6) |
31,258 (66%) |
223 km (191·2) |
5·2* | 42,507 (51%) |
190 km (159·0) |
92,727 (62%) |
212 km (186·6) |
11·8* |
| Mato Grosso do Sul | 967 (46%) |
391 km (301·0) |
1,541 (51%) |
356 km (299·2) |
−8·8* | 7,458 (58%) |
416 km (237·2) |
11,175 (53%) |
394 km (232·1) |
−5·3* | 21,141 (38%) |
369 km (213·6) |
31,250 (41%) |
352 km (287·0) |
−4·8* |
| Mato Grosso | 909 (69%) |
609 km (612·5) |
2,090 (66%) |
489 km (527·1) |
−19·7* | 10,443 (75%) |
543 km (485·3) |
17,665 (53%) |
516 km (446·6) |
−5·0* | 21,505 (61%) |
475 km (415·8) |
47,001 (61%) |
508 km (514·3) |
6·9* |
| Southeast region |
34,918 (52%) |
134 km (139·3) |
54,861 (53%) |
109 km (131·8) |
−4·3* |
310,401 (56%) |
113 km (116·4) |
433,788 (58%) |
108 km (115·2) |
−4·2* |
884,177 (48%) |
101 km (104·9) |
1,393,691 (52%) |
96 km (124·8) |
−4·7* |
| Espírito Santo | 2,232 (58%) |
90 km (92·4) |
4,943 (74%) |
86 km (93·8) |
−4·0 | 14,696 (80%) |
93 km (105·7) |
29,084 (85%) |
90 km (95·5) |
−3·0* | 69,591 (79%) |
83 km (89·9) |
102,320 (76%) |
84 km (100·0) |
1·0 |
| Minas Gerais | 11,164 (63%) |
154 km (159·1) |
16,656 (61%) |
137 km (159·8) |
−11·3* | 97,629 (67%) |
156 km (145·2) |
165,581 (65%) |
145 km (135·7) |
−7·0* | 261,021 (57%) |
135 km (125·0) |
447,960 (60%) |
134 km (173·8) |
−1·4* |
| Rio de Janeiro | 4,199 (38%) |
79 km (68·9) |
5,602 (41%) |
76 km (85·1) |
−3·4 | 41,881 (47%) |
68 km (71·6) |
52,760 (49%) |
71 km (89·4) |
5·6* | 108,747 (40%) |
74 km (75·0) |
162,159 (43%) |
64 km (80·4) |
−12·8* |
| São Paulo | 17,323 (49%) |
139 km (138·9) |
27,660 (50%) |
102 km (123·3) |
−26·5* | 156,195 (52%) |
99 km (97·1) |
186,363 (54%) |
88 km (93·8) |
−11·7* | 444,818 (43%) |
91 km (95·2) |
681,252 (48%) |
82 km (87·3) |
−10·0* |
| South region |
22,276 (60%) |
105 km (109·8) |
36,726 (60%) |
100 km (132·6) |
−18·6* |
172,874 (56%) |
111 km (109·6) |
245,700 (65%) |
106 km (115·2) |
−4·3* |
437,847 (55%) |
96 km (94·0) |
745,543 (58%) |
90 km (107·2) |
−6·6* |
| Paraná | 10,809 (38%) |
119 km (106·4) |
18,061 (65%) |
112 km (110·0) |
−6·2* | 65,800 (68%) |
123 km (99·2) |
100,918 (65%) |
121 km (116·3) |
−1·3* | 132,668 (55%) |
115 km (103·0) |
250,387 (59%) |
107 km (106·2) |
−6·5* |
| Santa Catarina | 3,497 (59%) |
91 km (125·2) |
6,740 (59%) |
85 km (118·4) |
−6·6* | 31,998 (69%) |
118 km (138·4) |
50,219 (69%) |
100 km (132·2) |
−15·7* | 88,429 (56%) |
88 km (101·0) |
160,574 (60%) |
71 km (113·2) |
−19·5* |
| Rio Grande do Sul | 7,970 (58%) |
91 km (104·5) |
11,925 (56%) |
92 km (165·9) |
0·3 | 75,076 (65%) |
97 km (102·9) |
94,563 (63%) |
93 km (95·8) |
−4·2* | 216,750 (54%) |
87 km (83·1) |
334,582 (56%) |
85 km (103·1) |
−2·6* |
The data refer to patients who had to commute between municipalities to receive treatment.
The number of authorizations were used as proxies of the number of patients.
Percentages are relative to the total number of cancer patients, regardless of their need to travel to receive treatment.
indicates p < 0.05.
Over time, the weighted average distance travelled by patients to undergo surgery significantly decreased for residents of 12 Brazilian states (46·1%) and increased for residents of two states (7·7%). The remaining 12 states presented no significant change. Fifteen (57·7%) states presented significantly decreased weighted average distances for radiotherapy and chemotherapy. The weighted average distances travelled significantly increased over time in one state (3·8%) for radiotherapy, and nine states (34·6%) for chemotherapy (Table 3).
Patients living in Rondônia, Maranhão, Mato Grosso do Sul, Minhas Gerais, São Paulo, Paraná, and Santa Catarina significantly reduced weighted average distances travelled for all types of treatment (Table 3; Supplementary material). Patients living in Tocantins have experienced a significant increase in weighted average distances travelled for surgical (p < 0·001) and chemotherapy (p < 0·001) treatment. Patients living in Amazonas had significantly increased travel distances for radiotherapy (p = 0·001) and chemotherapy (p < 0·001) treatment, despite having significantly decreased distances travelled for surgical treatment (p = 0·018) (Table 3; Supplementary material).
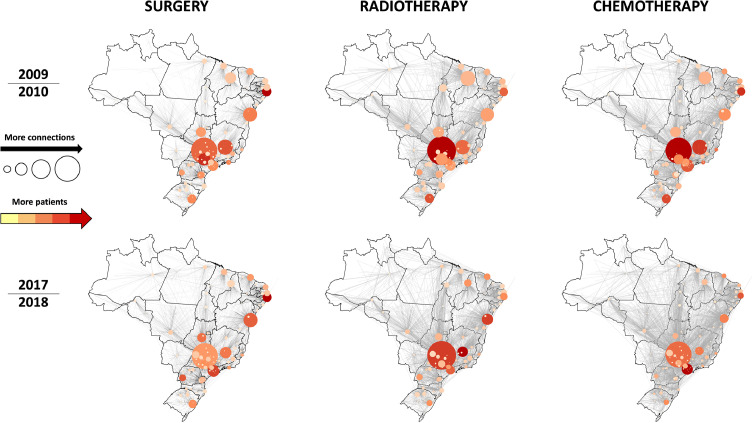
Hubs and attraction poles of oncological care were concentrated in the northeast and southeast regions
Figure 6 shows the patients’ commuting networks highlighting the municipalities of treatment. Each node is a municipality, and the size and color of each node are proportional to its indegree and weighted indegree, respectively (see Table 1 for definitions). Municipalities that had many connections with others as a destination for cancer treatment were considered hubs for cancer care. These were represented in the map with larger diameters. Municipalities that received large numbers of patients for treatment, from one or several municipalities, were considered attraction poles for cancer care. These were represented in the map with reddish colors.
Figure 6.
Hubs and attraction poles of oncological care in Brazil. Each node is a municipality and a connection between them indicates a relationship of origin/destination of patients. The diameter of the circles is proportional to the indegree: the larger the circle, the more connections with different municipalities as a treatment destination for patients. The color intensity is proportional to the weighted indegree: the darker the red, the greater the flow of patients from other municipalities.
Table 4 shows the main hubs of cancer care in both biennia. Most hubs were located in the southeast and northeast regions of Brazil. Throughout the time, Barretos (state of São Paulo) was the main hub for all types of treatment, receiving patients from 730, 948, and 1,192 different municipalities for surgery, radiotherapy, and chemotherapy, respectively. Overall, 94·3% of all patients assisted in Barretos were non-residents.
Table 4.
Ranking of treatment destination municipalities (cancer care hubs) based on the number of connections with other municipalities.
| Treatment type | Rank | Destination municipality | Region | Number of municipality connections as a treatment destination (indegree) | % of non-residents relative to the total patients assisted |
|---|---|---|---|---|---|
| SURGERY | 2009–2010 | ||||
| 1 | Barretos | SE | 636 | 95·5% | |
| 2 | Belo Horizonte | SE | 369 | 62·9% | |
| 3 | Salvador | NE | 341 | 57·9% | |
| 2017–2018 | |||||
| 1 | Barretos | SE | 730 | 91·8% | |
| 2 | Salvador | NE | 395 | 59·3% | |
| 3 | São Paulo | SE | 328 | 35·4% | |
| RADIOTHERAPY | 2009–2010 | ||||
| 1 | Barretos | SE | 749 | 95·2% | |
| 2 | Teresina | NE | 390 | 69·8% | |
| 3 | Belo Horizonte | SE | 376 | 65·6% | |
| 2017–2018 | |||||
| 1 | Barretos | SE | 948 | 94·3% | |
| 2 | Salvador | NE | 371 | 57·1% | |
| 3 | Belo Horizonte | SE | 345 | 59·7% | |
| CHEMOTHERAPY | 2009–2010 | ||||
| 1 | Barretos | SE | 811 | 95·0% | |
| 2 | Belo Horizonte | SE | 463 | 53·5% | |
| 3 | Teresina | NE | 400 | 64·1% | |
| 2017–2018 | |||||
| 1 | Barretos | SE | 1192 | 92·4% | |
| 2 | São Paulo | SE | 508 | 34·0% | |
| 3 | Salvador | NE | 402 | 54·2% | |
SE: southeast; NE: northeast.
The main attraction poles of cancer care are shown in Table 5. For surgeries, the municipality of Recife received the largest number of patients in both biennia, assisting more than 8,000 people in 2017–2018. For radiotherapy and chemotherapy, Barretos was the main attraction pole of the first biennium. In 2017–2018, other municipalities outperformed: Belo Horizonte received 42,395 patients for radiotherapy and São Paulo assisted 192,343 patients for chemotherapy, as the main attraction poles of the biennium.
Table 5.
Ranking of treatment municipalities based on the number of patients received from other municipalities (cancer care attraction poles).
| Treatment type | Rank | Destination municipality | Region | Number of non-resident patients (weighted indegree) | % of non-residents relative to the total patients assisted |
|---|---|---|---|---|---|
| SURGERY | 2009–2010 | ||||
| 1 | Recife | NE | 6,386 | 75·0% | |
| 2 | Jaú | SE | 5,302 | 91·2% | |
| 3 | Belo Horizonte | SE | 4,462 | 62·9% | |
| 2017–2018 | |||||
| 1 | Recife | NE | 8,333 | 76·0% | |
| 2 | São Paulo | SE | 6,342 | 35·4% | |
| 3 | Cascavel | S | 5,679 | 85·2% | |
| RADIOTHERAPY | 2009–2010 | ||||
| 1 | Barretos | SE | 47,664 | 95·2% | |
| 2 | Porto Alegre | S | 33,763 | 61·8% | |
| 3 | Recife | NE | 30,886 | 75·7% | |
| 2017–2018 | |||||
| 1 | Belo Horizonte | SE | 42,395 | 59·7% | |
| 2 | Barretos | SE | 39,209 | 94·3% | |
| 3 | Salvador | NE | 39,065 | 57·1% | |
| CHEMOTHERAPY | 2009–2010 | ||||
| 1 | Barretos | SE | 104,158 | 95·0% | |
| 2 | Recife | NE | 85,509 | 65·2% | |
| 3 | Belo Horizonte | SE | 83,346 | 53·5% | |
| 2017–2018 | |||||
| 1 | São Paulo | SE | 192,343 | 34·0% | |
| 2 | Recife | NE | 131,868 | 71·7% | |
| 3 | Barretos | SE | 119,591 | 92·4% | |
S: South; SE: southeast; NE: northeast.
Discussion
One of the main aspects of achieving UHC is planning catchment areas for specialized healthcare. In this study, we used SNA to estimate the commuting routes, flow, and distances travelled by cancer patients to receive surgical, radiotherapy, and chemotherapy provided by the national unified health system (SUS). To our knowledge, this is the first study to examine the evolution of cancer treatment accessibility in Brazil.
Over time, we have shown an increased number of treatment procedures. This may be due to a variety of factors, including population growth, aging, increased number of SUS-accredited hospitals, better diagnosis, availability of medical services, and better management of reference services. The great difference observed between surgery and radiotherapy/chemotherapy procedures is probably related to cancer treatment specificities. Cancer patients may undergo a single surgical procedure, and multiple sessions of radiotherapy and/or chemotherapy.
Our findings revealed that more than half of the cancer patients had to travel from their home municipalities to receive treatment and that regional accessibility disparities persisted over time, despite the decreased traveling distances observed in some states. Other low- and middle-income countries (LMICs) have also reported geographic accessibility issues.32, 33, 34 LMICs have diverse environments in terms of workforce capacity, private sector regulation, public investment, pathways of care, and a general lack of nationwide strategies for cancer care development, governance, sustainable funding, and certification.22 In Colombia, a country that also offers national healthcare coverage, the limited offer of oncology services is aggravated by ill-timed access and lack of continued care. Unlike Brazil, where different cancer treatments are usually concentrated in single healthcare units, many Colombian institutions providing oncological care offer only some specialized services (e.g. only radiotherapy), causing delays and fragmentation in the treatment of patients who need treatment combinations.34 In both countries access to cancer treatment is widely influenced by the concentration of services in large urban centers and the consequent large distances travelled by patients. The territorial extension of Brazil makes it even more important and challenging to provide a highly-coordinated multi-layered healthcare system.
The first national cancer policy in Brazil, published in 2005, emphasized the “need to structure a regionalized and hierarchical service network that guarantees comprehensive care to the population”.20 In 2013, a new national policy established the provision of timely treatment as close as possible to the patients’ homes as a guideline for the treatment of cancer patients,21 a difficult task to accomplish in a country with continental dimensions. The development of a healthcare network centered on people with chronic diseases was also included in a set of proposals to address care fragmentation.35 Furthermore, SUS provided tickets and daily subsistence subsidies for patients that do not have a reference center in their municipalities. Even though these financial resources are limited, such a policy allowed for more flexibility in meeting the needs of users.
Evaluations of cancer treatment access based on country-wide averages may not provide reliable accessibility information, particularly in geographically dispersed countries. The national median distance travelled by cancer patients who had to commute for treatment ranged from 170·3 to 188·4 km, which equates to a 3 h, one-way drive. Nonetheless, our findings demonstrated that regional disparities exist, as patients living in states of the north and midwest regions of Brazil had to travel longer distances than patients in the south, southeast and northeast regions. There is no empirical evidence to recognize what would be a reasonable distance to travel for oncological treatment. Current Ministry of Health regulations establish that high-complexity oncological services should be distributed at the ratio of one health establishment for every 500,000 inhabitants.36 A recent study pointed out a deficit of 144 CACON- or UNACON-type services for the estimated 207·7 million in 2017.37 The authors demonstrated that the distribution of cancer care facilities was heterogeneous and that health care services were concentrated in a few states, with southern states having the highest need versus supply ratio, and the northern, the lowest.37 These regional variations may also reflect the greater concentration of medical facilities along the east side of the country, population density differences,38 as well as patterns of inequality related to personal (gender, age, race/ethnicity) and socioeconomic (income, education) characteristics of individuals,39 which can limit the outcomes of egalitarian policies.
The identification of hubs and attraction poles for cancer treatment through SNA allowed mapping municipalities with high demand for healthcare services. Given their higher population density, the concentration of hubs and poles in the southeast and northeast of Brazil is expected. Even though northern Brazil has a lower population density, the possibility of establishing new cancer care centers in the north would undoubtedly improve access for a large population living in the states of Acre, Amazonas, Amapá, and Roraima, from where cancer patients had to travel more than 1,000 km to receive different types of treatment. Further research looking at coverage areas and hospital absorption capacity could contribute to this discussion.
Previous studies emphasized the long distances patients had to travel to hospitals that provided oncology services in Brazil.15,16,40,41 Several difficulties have been reported among cancer patients who had to commute for treatment, such as fatigue, long waits to return home, a lack of proper feeding, lack of financial resources to travel, and a continuous interruption of routine activities.42 Radiotherapy and chemotherapy are especially important because treatment requires frequent visits to cancer care facilities. Long travel distances to radiotherapy facilities have been linked to decreased use of radiotherapy services,43 an increased risk of mastectomy for breast cancer,44 a lower likelihood of radiotherapy use among patients with colon, rectum, lung, ovary, and prostate cancer,45 and less frequent use of palliative radiation therapy.46 Although the distance travelled by patients is not the only issue affecting patient access to oncological services, addressing this issue is critical to improving health equity and UHC. In high-income countries, such as the United States and Japan, approximately 90% of the population lives less than one hour from specialized cancer care centers47 and 80% of cancer patients have been admitted to hospitals in less than a 45 min drive from their residences.48
Cancer care offered within SUS necessarily goes through a regulation center. The structure is intended to organize cancer care according to the availability of hospital beds, patient's place of residence, and complexity of the case, optimizing the use of the health system's capacity. It also aims to reduce the waiting time for treatment and avoid large commuting distances. Considering the results presented herein, it is worth questioning the reasons why patients’ commuting flows were frequently different from those projected by health policies. In addition to the shortage of specialized cancer care centers in Brazil, the question of whether all municipalities that have high-complexity centers are prepared to serve their resident population remains. Also, it is possible that some of the reference treatment facilities may not be attractive to patients for several reasons, including transport availability and public confidence.
The high non-resident rate of patients assisted in Barretos, a city with 122,000 people, suggests that patients may seek ways of accessing services that do not necessarily follow what has been planned, articulating flows regardless of distances to ensure that they meet their real or symbolic demands.35 The Hospital de Amor, located in Barretos, is a reference center for cancer treatment that provides care directly and free of charge to cancer patients. It assists more the 1·2 million people per year, financed by donations from the community, artists, private companies, as well as government funding. The hospital is a unique example in the country: it has a competent fundraising structure, organizational culture, population credibility, support infrastructure, and good clinical results that attract people from the entire country, even without an official referral process. Understanding the factors that contribute to this increased and unbalanced patient flow towards the hubs and poles can provide useful information for strategic planning and improvement of oncological care.
Our analysis suggests that the geographical access to cancer care in Brazil did not improve over time, as the percentage of patients who had to commute for treatment remained relatively constant and regional disparities persisted over a nearly 10-years period (2009–2018). A historical analysis of the Brazilian national cancer care policy following the establishment of SUS revealed that the structuring of cancer care was maintained by stimulating the expansion of healthcare services and accreditation by sanctioning norms.27 Although the number of accredited services has grown over time, few financial investments have been made to expand the services’ offer and ensure compliance with the established rules.27 The establishment of criteria to qualify services without the allocation of financial resources favored accreditation of existing facilities that already had the infrastructure, financial resources, and personnel to meet the established requirements over expanding to new ones.37
The interpretation of our results has some limitations. Other measures of geographical accessibility, such as travel time, could have been included in the analysis, however, considering the country's relatively deficient and expensive transportation infrastructure, the distances and the need to commute from one municipality to another can be used as proxy indicators of the difficulties patients face in accessing treatment. Measurements of the cost and number of trips per patient could also add to the characterization of the problem, but this information is not easily available. Therefore, we have looked at one of the many aspects of the Brazilian cancer care network: geographic accessibility to treatment. A comprehensive analysis of the health system infrastructure network and its corresponding demand will provide additional input for planning and improving availability and accessibility.
Conclusions
The SUS's information technology architecture offers a great opportunity for the research community to gain insights into the accessibility and overall operation of the public health services. Although specialized services tend to be concentrated in healthcare networks, better planning and regulation can ensure broader coverage while preventing high-complexity infrastructure and human resources from becoming idle. The results of this study are useful in informing the oncology services and policy-makers that: (i) more than half of the cancer patients need to travel to receive treatment in a SUS's hospital; (ii) regional disparities are marked and persisted over the last decade, hindering the accessibility of patients from the northern and midwestern states of Brazil; (iii) hubs and attraction poles are concentrated in a few municipalities of the southeast and northeast regions, indicating the need to better balance the supply and demand for specialized care.
Author contributions
BPF: conceptualizations and study design, data analysis, visualization and interpretation, writing - original draft; RFS: data collection, cleaning, and validation; PCA: data analysis, statistical analysis and interpretation; FZ: supervision and writing - review and editing. All authors critically revised the manuscript and approved its final version.
Declaration of interests
The authors declare no competing interests.
Acknowledgments
Acknowledgments
This work was funded by the Oswaldo Cruz Foundation - Fiocruz (Inova no. 8451635123 to BPF) and the National Council for Scientific and Technological Development - CNPq (no. 407060/2018–9 to BPF); Coordination for the Improvement of Higher Education Personnel – CAPES (scholarship to PCA, Finance Code 001); and Instituto Nacional de Ciência e Tecnologia de Inovação em Doenças de Populações Negligenciadas (INCT-IDPN).
Data sharing statement
Data used in this manuscript is freely available from the sources mentioned in the Methods section. A spreadsheet with the compiled raw data used is available as Supplementary Material.
Editor note:The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2021.100153.
Appendix. Supplementary materials
References
- 1.United Nations . United Nations Sustainable Development; 2021. Sustainable Development Goals-United Nations.http://www.un.org/sustainabledevelopment/sustainable-development-goals/ [Google Scholar]
- 2.Levesque J.F., Harris M.F., Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donabedian A. Aspects of Medical Care Administration. Harvard University Press; Boston: 1973. Capacity to produce services in relation to need and demand. [Google Scholar]
- 4.Penchansky R., Thomas J.W. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19:127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Omrani-Khoo H., Lotfi F., Safari H., Zargar Balaye Jame S., Moghri J., Shafii M. Equity in distribution of health care resources; assessment of need and access, using three practical indicators. Iran J Public Health. 2013;42:1299–1308. [PMC free article] [PubMed] [Google Scholar]
- 6.Rosero-Bixby L. Spatial access to health care in Costa Rica and its equity: a GIS-based study. Soc Sci Med. 2004;58:1271–1284. doi: 10.1016/S0277-9536(03)00322-8. [DOI] [PubMed] [Google Scholar]
- 7.Apparicio P., Abdelmajid M., Riva M., Shearmur R. Comparing alternative approaches to measuring the geographical accessibility of urban health services: distance types and aggregation-error issues. Int J Health Geogr. 2008;7:7. doi: 10.1186/1476-072X-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peters D.H., Garg A., Bloom G., Walker D.G., Brieger W.R., Rahman M.H. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008;1136:161–171. doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- 9.Hierink F., Okiro E.A., Flahault A., Ray N. The winding road to health: a systematic scoping review on the effect of geographical accessibility to health care on infectious diseases in low- and middle-income countries. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0244921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ambroggi M., Biasini C., Giovane C.D., Fornari F., Cavanna L. Distance as a barrier to cancer diagnosis and treatment: review of the literature. Oncologist. 2015;20:1378–1385. doi: 10.1634/theoncologist.2015-0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pomare C., Long J.C., Churruca K., Ellis L.A., Braithwaite J. Social network research in health care settings: design and data collection. Soc Netw. 2019 doi: 10.1016/j.socnet.2019.11.004. published online Dec 14. [DOI] [Google Scholar]
- 12.Chambers D., Wilson P., Thompson C., Harden M. Social network analysis in healthcare settings: a systematic scoping review. PLoS ONE. 2012;7:e41911. doi: 10.1371/journal.pone.0041911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strozzi F., Garagiola E., Trucco P. Analysing the attractiveness, availability and accessibility of healthcare providers via social network analysis (SNA) Decis Support Syst. 2019;120:25–37. [Google Scholar]
- 14.Bean D.M., Stringer C., Beeknoo N., Teo J., Dobson R.J.B. Network analysis of patient flow in two UK acute care hospitals identifies key sub-networks for A&E performance. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0185912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saldanha R de F., Xavier D.R., Carnavalli K de M., Lerner K., Barcellos C. Analytical study of the breast cancer patient flow network in Brazil from 2014 to 2016. Cad de Saúde Pública. 2019;35 doi: 10.1590/0102-311x00090918. [DOI] [PubMed] [Google Scholar]
- 16.Oliveira de E.X.G., Melo E.C.P., Pinheiro R.S., Noronha C.P., Carvalho M.S. Access to cancer care: mapping hospital admissions and high-complexity outpatient care flows. The case of breast cancer. Cad de Saúde Pública. 2011;27:317–326. doi: 10.1590/s0102-311x2011000200013. [DOI] [PubMed] [Google Scholar]
- 17.Sousa L.M.O., Araújo de E.M., Miranda J.G.V. Characterization of access to normal childbirth care in Bahia State, Brazil, based on graph theory. Cad de Saúde Pública. 2017;33 doi: 10.1590/0102-311x00101616. [DOI] [PubMed] [Google Scholar]
- 18.Paim J., Travassos C., Almeida C., Bahia L., Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011;377:1778–1797. doi: 10.1016/S0140-6736(11)60054-8. [DOI] [PubMed] [Google Scholar]
- 19.Santos dos N.R. SUS, política pública de Estado: seu desenvolvimento instituído e instituinte e a busca de saídas. Ciênc saúde coletiva. 2013;18:273–280. doi: 10.1590/s1413-81232013000100028. [DOI] [PubMed] [Google Scholar]
- 20.Brazil. Ministry of health. Ordinance No. 874. Institutes the National Policy for the Prevention and Control of Cancer in the Health Care Network of People with Chronic Diseases within the scope of the Unified Health System (SUS). 2005. http://bvsms.saude.gov.br/bvs/saudelegis/gm/2013/prt0874_16_05_2013.html. Accessed July 24, 2018.
- 21.Brazil. Ministry of health. Ordinance n. 2439. Institutes the National Oncology Care Policy: Promotion, Prevention, Diagnosis, Treatment, Rehabilitation and Palliative Care, to be implemented in all federated units, respecting the competencies of the three management spheres. 2013. http://bvsms.saude.gov.br/bvs/saudelegis/gm/2005/prt2439_08_12_2005.html. Accessed July 30, 2018.
- 22.Sirohi B., Chalkidou K., Pramesh C.S., et al. Developing institutions for cancer care in low-income and middle-income countries: from cancer units to comprehensive cancer centres. Lancet Oncol. 2018;19:e395–e406. doi: 10.1016/S1470-2045(18)30342-5. [DOI] [PubMed] [Google Scholar]
- 23.INCA. Estimate/2020-cancer incidence in Brazil. Instituto Nacional de Câncer José Alencar Gomes da Silva, 2020 https://www.inca.gov.br/publicacoes/livros/estimativa-2020-incidencia-de-cancer-no-brasil. Accessed December 15, 2021.
- 24.Montag B., Khuntia D. How can we achieve equitable global access to cancer imaging and care? Lancet Oncol. 2021;22:429–430. doi: 10.1016/S1470-2045(21)00068-1. [DOI] [PubMed] [Google Scholar]
- 25.Ward Z.J., Scott A.M., Hricak H., et al. Estimating the impact of treatment and imaging modalities on 5-year net survival of 11 cancers in 200 countries: a simulation-based analysis. Lancet Oncol. 2020;21:1077–1088. doi: 10.1016/S1470-2045(20)30317-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.IBGE. Brazil cities and states. Brazilian institute of geography and statistics. https://www.ibge.gov.br/en/cities-and-states.html. Accessed September 9, 2021.
- 27.Silva da M.J.S., Lima de F.L.T., O'Dwyer G., Osorio-de-Castro C.G.S. Cancer care policy in Brazil after creation of unified health system. Rev Bras Cancerol. 2017:177–187. [Google Scholar]
- 28.World Health Organization . 2nd ed. World Health Organization; 2004. Icd-10: International Statistical Classification of Diseases and Related Health Problems:tenth revision.https://apps.who.int/iris/handle/10665/42980 Accessed March 20, 2021. [Google Scholar]
- 29.Florêncio R.B., de Araújo Fonseca L.G., da Silva V.F.D., Lima Í.N.D.F., Gualdi L.P. Diabetes mellitus hospitalization and mortality rate according to a national database in Brazil: a longitudinal study. BMC Public Health. 2021;21:403. doi: 10.1186/s12889-021-10438-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fernandes G dos S., Campos D., Ballalai A., et al. Epidemiological and clinical patterns of newly diagnosed hepatocellular carcinoma in brazil: the need for liver disease screening programs based on real-world data. J Gastrointest Canc. 2020 doi: 10.1007/s12029-020-00508-7. published online Sept 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saldanha de R.F., Bastos R.R., Barcellos C., Saldanha de R.F., Bastos R.R., Barcellos C. Microdatasus: a package for downloading and preprocessing microdata from Brazilian health informatics department (DATASUS) Cad de Saúde Pública. 2019;35 doi: 10.1590/0102-311x00032419. [DOI] [PubMed] [Google Scholar]
- 32.Ahamad A. Geographic access to cancer care: a disparity and a solution. Postgrad Med J. 2011;87:585–589. doi: 10.1136/pgmj.2010.111930. [DOI] [PubMed] [Google Scholar]
- 33.Yahya N., Sukiman N.K., Suhaimi N.A., Azmi N.A., Manan H.A. How many roads must a Malaysian walk down? Mapping the accessibility of radiotherapy facilities in Malaysia. PLoS ONE. 2019;14 doi: 10.1371/journal.pone.0213583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Vries E., Buitrago G., Quitian H., Wiesner C., Castillo J.S. Access to cancer care in Colombia, a middle-income country with universal health coverage. J Cancer Policy. 2018;15:104–112. [Google Scholar]
- 35.Viana A.L.Á., Bousquat A., Melo G.A., et al. Regionalization and health networks. Ciênc Saúde Coletiv. 2018;23:1791–1798. doi: 10.1590/1413-81232018236.05502018. [DOI] [PubMed] [Google Scholar]
- 36.Brazil. Ministry of health. Ordinance no. 140: Redefines the criteria and parameters for organization, planning, monitoring, control and evaluation of accreditated health care establishments in specialized oncology care and defines the structural, operational and human resources conditions for the accreditation of these establishments within the Unified Health System (SUS). 2014. https://bvsms.saude.gov.br/bvs/saudelegis/sas/2014/prt0140_27_02_2014.html. Accessed December 15, 2021.
- 37.Silva M.J.S., O'Dwyer G., Osorio-de-Castro C.G.S. Cancer care in Brazil: structure and geographical distribution. BMC Cancer. 2019;19:987. doi: 10.1186/s12885-019-6190-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.IBGE . Brazilian Institute of Geography and Statistics; 2021. Estimates of Resident Population For Municipalities and Federation Units.https://www.ibge.gov.br/en/statistics/social/population/18448-estimates-of-resident-population-for-municipalities-and-federation-units.html?=&t=o-que-e Accessed Sept 8. [Google Scholar]
- 39.Melo E.C.P., de Oliveira E.X.G., Chor D., Carvalho M.S., Pinheiro R.S. Inequalities in socioeconomic status and race and the odds of undergoing a mammogram in Brazil. Int J Equity Health. 2016;15:144. doi: 10.1186/s12939-016-0435-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grabois M.F., de Oliveira E.X.G., Sa Carvalho M., Grabois M.F., de Oliveira E.X.G., Sa Carvalho M. Assistencia ao cancer entre criancas e adolescentes: mapeamento dos fluxos origem-destino no Brasil. Rev de Saúde Pública. 2013;47:368–378. doi: 10.1590/S0034-8910.2013047004305. [DOI] [PubMed] [Google Scholar]
- 41.Rocha-Brischiliari S.C., Andrade L., Nihei O.K., et al. Spatial distribution of breast cancer mortality: socioeconomic disparities and access to treatment in the state of Parana, Brazil. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0205253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Teston E.F., Fukumori E.F.C., Benedetti dos G.M.S., et al. Feelings and difficulties experienced by cancer patients along the diagnostic and therapeutic itineraries. Escola Anna Nery. 2018;22 doi: 10.1590/2177-9465-ean-2018-0017. [DOI] [Google Scholar]
- 43.Liu E., Santibáñez P., Puterman M.L., et al. A quantitative analysis of the relationship between radiation therapy use and travel time. Int J Radiat Oncol Biol Phys. 2015;93:710–718. doi: 10.1016/j.ijrobp.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 44.Longacre C.F., Neprash H.T., Shippee N.D., Tuttle T.M., Virnig B.A. Travel, treatment choice, and survival among breast cancer patients: a population-based analysis. Women's Health Rep. 2021;2:1–10. doi: 10.1089/whr.2020.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jones A.P., Haynes R., Sauerzapf V., Crawford S.M., Zhao H., Forman D. Travel time to hospital and treatment for breast, colon, rectum, lung, ovary and prostate cancer. Eur J Cancer. 2008;44:992–999. doi: 10.1016/j.ejca.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 46.Lavergne M.R., Johnston G.M., Gao J., Dummer T.J., Rheaume D.E. Variation in the use of palliative radiotherapy at end of life: examining demographic, clinical, health service, and geographic factors in a population-based study. Palliat Med. 2011;25:101–110. doi: 10.1177/0269216310384900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Onega T., Duell E.J., Shi X., Wang D., Demidenko E., Goodman D. Geographic access to cancer care in the U.S. Cancer. 2008;112:909–918. doi: 10.1002/cncr.23229. [DOI] [PubMed] [Google Scholar]
- 48.Tanaka H., Ishikawa K.B., Katanoda K. Geographic Access to cancer treatment in Japan: results from a combined dataset of the patient survey and the survey of medical institutions in 2011. J Epidemiol. 2018;28:470–475. doi: 10.2188/jea.JE20170051. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.