Summary
Background
In the United States, abortion access is often more limited for people who live in states with few abortion facilities and restrictive abortion legislation. Pregnant people seeking an abortion thus often travel to access care.
Methods
We calculated state-specific abortion rate (number of abortions per thousand women ages 15 to 44) and percentage of patients leaving for abortion care using CDC 2017 Abortion Surveillance data, the Guttmacher Institute's Abortion Provider Census and Pregnancies, Births and Abortions in the United States report, and US Census data. We categorized percent leaving by abortion policy landscape using the Guttmacher Institute's classification of state abortion laws, and by facility density (number of abortion facilities per million women ages 15 to 44), calculated using Census and Guttmacher data. We ran correlational tests between each of our variables (percent leaving, facility density, and policy environment), as well as between percent leaving and facility density within policy environment.
Findings
In 2017, an average of 8% of US patients left their state of residence for abortion care. Percent leaving varied widely by state: 74% left Wyoming, 57% left South Carolina, and 56% left Missouri, while 13 states had fewer than 4% of patients leaving. States with more restrictive laws averaged 12% of patients leaving, while states with middle ground or supportive laws averaged 10% and 3% leaving, respectively. Pairwise correlations between percent leaving, facility density, and policy score were all statistically significant, though correlations between percent leaving and facility density within policy environment were not.
Interpretation
Many patients travel across state lines for abortion care. While patients may leave for a range of reasons, restrictive state-level abortion policy and facility scarcity are associated with patients leaving their state of residence.
Funding
This study was supported by a philanthropic foundation that makes grants anonymously.
Research in context.
Evidence before this study
Studies conducted in individual facilities, states, and regions illuminate that people who live in states with few facilities or restrictive abortion legislation may need to leave their state of residence.
Added value of this study
This study makes novel use of data from the US Centers for Disease Control and Prevention on abortions by state of occurrence and state of patient residence to calculate the number and percent of patients leaving their state of residence for abortion care. We contextualize these findings by categorizing states by policy environment and facility density (number of abortion facilities per million women ages 15–44).
Implications of all the available evidence
Many patients travel across state lines for abortion care. Restrictive state-level abortion policy as well as abortion facility scarcity may play a role in patients needing to leave their state of residence.
Alt-text: Unlabelled box
Introduction
In 1973, the United States (US) Supreme Court legalized abortion throughout the country with its landmark Roe v. Wade ruling.1 Nevertheless, abortion in the US remains highly regulated at the state level, with states in the Midwest and South enacting the largest number of laws that regulate abortion. Laws impact both health care provision and access. Some laws regulate clinics or providers (limits to where abortions can take place, who can perform abortions, and what procedures can be used), and others regulate patients (waiting periods and insurance restrictions).2,3 Almost all abortion care in the US (95%) is provided in standalone facilities (as opposed to hospitals, private practices, or OB-GYN clinics).3 In states with restrictive laws, abortion care is increasingly concentrated in smaller numbers of facilities.3
Access to abortion care in the US thus varies widely depending on the specific state policy context. Policies that target abortion providers (as opposed to those seeking abortions),4 such as hospital transfer agreements, facility size requirements, and limitations on allowable distance to hospitals, force abortion facilities to meet requirements that are medically unnecessary3 and may cause them to close5 or lead to abortion care churn: “clinic-level instability of abortion care services and chronic uncertainty about potential closure or changes in services.”6 Closures and churn can create abortion deserts from which individuals may need to travel further to access abortion care.7,8 Cartwright et al. identified 27 abortion deserts in 2017, where patients would need to travel over 100 miles to reach an abortion facility.9 Policies such as mandatory waiting periods and gestational limits also create barriers for abortion seekers via increased time and transportation cost, and the need to travel for care past their closest facilities’ gestational limit.10 As a result of the accumulation of barriers, the experience of seeking abortion care, particularly for those who must travel, can be arduous.11,12
We turn to the question of how states differ in the extent to which patients leave their state of residence to access care. While leaving one's state is not necessarily burdensome (e.g., sometimes one's closest abortion facility may be across state lines), interrogating how people leave their home state for care allows for a fuller understanding of the ways in which differences between state policy contexts influence interstate travel. In this project, we describe the percentage of state residents who leave each state to have an abortion using 2017 data from the US Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute. We examine differences in the percent leaving by restrictiveness of the state's abortion policy environment, as well as by its abortion facility density (defined as the number of abortion facilities per million women of reproductive age).
Methods
Data
We rely on data from five sources for our analysis of interstate travel for abortion care. Our first main source of abortion data is the CDC's 2017 annual Abortion Surveillance report13 (the most recent year for which data is available across all abortion count sources in this analysis). The number of abortions, by both state of pregnant person's residence and state of occurrence, are collected by the CDC from state health departments of the location of occurrence. State provision of this information to the CDC is voluntary, and states differ in the reporting requirements that facilitate collection of this data.14 Totals by state of occurrence reported by the CDC include those with both known and unknown residence status. Because states may differ in their reporting requirements, comparison of abortions by occurrence between states is difficult, and counts reported by some states may be different from the actual number of abortions taking place there. Additionally, in 2017, four states (California, Maryland, New Hampshire, and Wyoming) either did not report to the CDC, or did not conform to reporting requirements. Nonetheless, the ability to cross-compare state of occurrence and state of patient residence makes the CDC data both unique and valuable as an analytic source. We therefore use a second, more reliable, source of data to account for some of the reporting variation issues.
Our second main source of abortion data comes from the Guttmacher Institute's 2017 Abortion Provider Census.15 The Abortion Provider Census is an ongoing survey of all health care facilities known or suspected to be providing abortions in the US. 2017 data on number of abortions by state of occurrence were collected between January 2018 and March 2019. The Guttmacher Institute estimates that the abortion providers that did not participate perform fewer than 30 abortions per year and thus have minimal impact on the total number of abortions. Our third main source of abortion data comes from the Guttmacher Institute’s report on trends in pregnancies, abortions, and births from 1973 to 2017.33 These data are compiled by the Guttmacher Institute based on their own Abortion Provider Census alongside the CDC’s surveillance data as well as data gathered directly from state health departments.
Because the Guttmacher survey collects data from health care facilities directly, we consider these data to be more accurate and more consistently comparable across states than data from the CDC; however, we cannot use this data alone to examine percent leaving, since neither of these reports provide a cross-comparison of abortions by state of occurrence and residence. Our analysis section below describes our combined use of these three datasets to calculate percent leaving. Additionally, we calculate facility densities using the number of health care facilities known to be providing abortions by state from the Abortion Provider Census report.
Fourth, we use data from the US Census16 to identify the number of women of reproductive age (aged 15–44). We use these data for calculating the abortion rate by state of residence (number of abortions among state residents per 1000 women aged 15–44 in that state) and facility density (number of facilities per million women aged 15–44). Calculating abortion rate and facility density allows a comparison of abortion utilization and presence of facilities between states that differ in population size.
Fifth, to further contextualize our findings, we draw from the Guttmacher Institute's policy analysis, State Abortion Policy Landscape,17 which classifies states as being “hostile,” “middle ground,” or “supportive” of abortion based on the prevalence of restrictions and protective policies at the state level across several policy snapshots. The Guttmacher analysis was conducted in August 2019, representing the policy analysis closest in time to 2017 (the previous policy analysis from the Guttmacher Institute is from 2010). The policy analysis assigns states “-1” for each of six abortion restrictions in effect (unconstitutional abortion bans, two trips required for abortion, restricted Medicaid coverage, parental involvement required, and clinic regulations, e.g., ambulatory surgical center standards or admitting privileges), and a “+1” for each of six protective policies in effect (state constitution protects abortion rights, state law protects abortion rights, Medicaid coverage for abortion, advanced practice clinician provision of abortion, health insurance plans must cover abortion, and access to abortion clinics protected). Scores are then summed, such that states with a -6 would have all six abortion restriction types in effect, and states with a +6 would have all six abortion protective policy types in effect. States with scores ranging from -6 to -2 are reported by Guttmacher to be hostile, -1 to +1 are middle ground, and +2 to +6 are supportive. We assign a -1 to Washington, DC, which was not included in the Guttmacher abortion policy report, based on Guttmacher's assessment of DC in September 2019, which states that it had just one abortion-related law: “Public funding is available for abortion only in cases of life endangerment, rape or incest” (i.e., Medicaid coverage was restricted).
Analysis
For our primary analysis, we calculate by state: the percent of patients leaving their state of residence for an abortion; the abortion rate (abortions per 1000 women aged 15–44) among residents; and the facility density (number of abortion facilities per million women aged 15–44). We also calculate the US pooled mean for percent leaving, abortion rate, and facility density. Finally, we present the pooled mean percent leaving and facility density by the policy landscape category (hostile, middle ground, or supportive) of the state of residence.
To calculate percent leaving, we use a combination of the CDC and Guttmacher datasets (see Table A1 for additional information). For the 46 states (plus DC) that reported to the CDC in 2017, we divide the number of patients from a state that received care in that state (a) by the total number of abortions that took place in that state (b), giving a percent () of abortions within each state that are performed on residents of that state. Next, we multiply this percent by the more reliable Guttmacher counts of total number of abortions for each state of occurrence (c) and round to the nearest whole number to give an adjusted count of the number of abortions taking place within a state, among state residents (). By subtracting this value from the Guttmacher total number of abortions among residents of each state (d), we are left with an estimate of the number of patients that leave their state for care (). Finally, dividing this by the total number of abortions among state residents, we have the percent of patients who leave their home state for care:
For the four states that do not report to the CDC or do not follow reporting requirements, we do not have data on the number of patients who stay within the state for care. Instead, we use CDC data to calculate the percent of patients from each of these states who had abortions in any of the non-missing states, and then apply these percentages to the Guttmacher counts, as above (see Table A2).
Additionally, we calculate the number and percent of patients going to and from each of these three policy categories. To do so, we once again rely on a combination of CDC and Guttmacher data. Similar to our calculation of number leaving for the four “missing” states, we first calculate the percent of abortions taking place within each state, from each state of residence individually, using CDC data. We then use Guttmacher totals of abortions by state of occurrence to calculate an adjusted number of abortions for each combination of state of occurrence and state of residence. Finally, we use these adjusted numbers to calculate the number of patients going to and coming from each policy environment.
Finally, in order to further investigate the relationships between percent leaving, policy landscape, and facility density, we run correlational tests between all three of our main variables, as well as between percent leaving and facility density within policy category.
All analyses conducted in Stata 16 (StataCorp, College Station, TX); map created using ArcGIS Pro (Esri, Redlands, CA).
Role of the funding source
This study was supported by a philanthropic foundation that makes grants anonymously. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
In 2017, an average of 8% of patients left their state of residence for abortion care (Table 1).
Table 1.
Number of abortions, abortion rate, facility density, abortion policy score, out of state abortions, and percent leaving by state of residence, 2017.
| State of residence | No. abortions among state residents | Abortion ratea among state residents | Facility densityb | Abortion policy score | No. abortions obtained out of state | % abortions obtained out of state |
|---|---|---|---|---|---|---|
| Alabama | 7660 | 8.0 | 5.2 | -5 | 2397 | 31.3% |
| Alaska | 1420 | 9.6 | 27.2 | 2 | 178 | 12.5% |
| Arizona | 13270 | 10.1 | 6.1 | -6 | 1065 | 8.0% |
| Arkansas | 3710 | 6.4 | 5.2 | -6 | 876 | 23.6% |
| California | 131380 | 16.3 | 20.0 | 6 | 142 | 0.1% |
| Colorado | 11100 | 10.1 | 16.3 | 0 | 157 | 1.4% |
| Connecticut | 11950 | 17.6 | 38.3 | 3 | 374 | 3.1% |
| Delaware | 2770 | 15.4 | 22.2 | -1 | 1094 | 39.5% |
| District of Columbia | 3930 | 21.8 | 22.2 | -1 | 1904 | 48.4% |
| Florida | 68640 | 18.3 | 17.4 | -2 | 439 | 0.6% |
| Georgia | 32520 | 15.3 | 7.1 | -3 | 1618 | 5.0% |
| Hawaii | 3220 | 12.1 | 15.0 | 4 | 63 | 2.0% |
| Idaho | 1790 | 5.6 | 9.4 | -3 | 550 | 30.7% |
| Illinois | 37770 | 14.7 | 9.7 | 3 | 2641 | 7.0% |
| Indiana | 10270 | 7.9 | 4.6 | -6 | 3159 | 30.8% |
| Iowa | 3650 | 6.2 | 13.6 | -2 | 389 | 10.7% |
| Kansas | 3520 | 6.3 | 7.2 | -3 | 108 | 3.1% |
| Kentucky | 4780 | 5.6 | 1.2 | -5 | 1994 | 41.7% |
| Louisiana | 9280 | 9.9 | 4.3 | -6 | 764 | 8.2% |
| Maine | 2050 | 8.8 | 68.6 | 1 | 109 | 5.3% |
| Maryland | 26940 | 22.5 | 20.9 | 2 | 2492 | 9.3% |
| Massachusetts | 18880 | 13.7 | 13.8 | 1 | 1037 | 5.5% |
| Michigan | 26130 | 13.9 | 11.2 | -3 | 338 | 1.3% |
| Minnesota | 10100 | 9.6 | 6.6 | 2 | 354 | 3.5% |
| Mississippi | 4930 | 8.2 | 1.7 | -6 | 2505 | 50.8% |
| Missouri | 9690 | 8.3 | 2.6 | -6 | 5440 | 56.1% |
| Montana | 1510 | 8.1 | 26.7 | 3 | 78 | 5.2% |
| Nebraska | 2250 | 6.1 | 8.2 | -4 | 444 | 19.7% |
| Nevada | 9620 | 16.8 | 12.2 | 0 | 488 | 5.1% |
| New Hampshire | 2330 | 9.6 | 16.5 | -1 | 208 | 8.9% |
| New Jersey | 47010 | 27.4 | 23.9 | 3 | 1507 | 3.2% |
| New Mexico | 3830 | 9.6 | 15.1 | 3 | 361 | 9.4% |
| New York | 103060 | 25.6 | 28.1 | 4 | 4127 | 4.0% |
| North Carolina | 25060 | 12.6 | 7.0 | -4 | 1030 | 4.1% |
| North Dakota | 970 | 6.7 | 6.9 | -5 | 127 | 13.1% |
| Ohio | 20560 | 9.3 | 4.1 | -5 | 1192 | 5.8% |
| Oklahoma | 4780 | 6.3 | 5.2 | -5 | 333 | 7.0% |
| Oregon | 8950 | 11.4 | 20.4 | 4 | 267 | 3.0% |
| Pennsylvania | 33910 | 14.1 | 7.5 | -4 | 4501 | 13.3% |
| Rhode Island | 3280 | 15.7 | 9.6 | 0 | 300 | 9.1% |
| South Carolina | 11380 | 12.0 | 4.2 | -5 | 6536 | 57.4% |
| South Dakota | 750 | 4.8 | 6.3 | -6 | 324 | 43.2% |
| Tennessee | 11060 | 8.5 | 6.2 | -5 | 1361 | 12.3% |
| Texas | 56340 | 9.8 | 3.7 | -5 | 2122 | 3.8% |
| Utah | 3020 | 4.6 | 4.6 | -5 | 198 | 6.6% |
| Vermont | 1140 | 9.9 | 52.2 | 3 | 68 | 6.0% |
| Virginia | 20290 | 12.1 | 9.5 | -4 | 4114 | 20.3% |
| Washington | 17760 | 12.5 | 28.2 | 4 | 942 | 5.3% |
| West Virginia | 2380 | 7.2 | 3.0 | -4 | 1109 | 46.6% |
| Wisconsin | 7540 | 7.0 | 2.8 | -4 | 1375 | 18.2% |
| Wyoming | 720 | 6.6 | 18.2 | -2 | 536 | 74.4% |
| TOTAL | 860850 | 13.6 | 12.7 | -2 | 65835 | 7.6% |
Abortion rate is the abortions per 1000 women aged 15–44 in state of residence.
Facility density is the number of abortion facilities per million women aged 15–44.
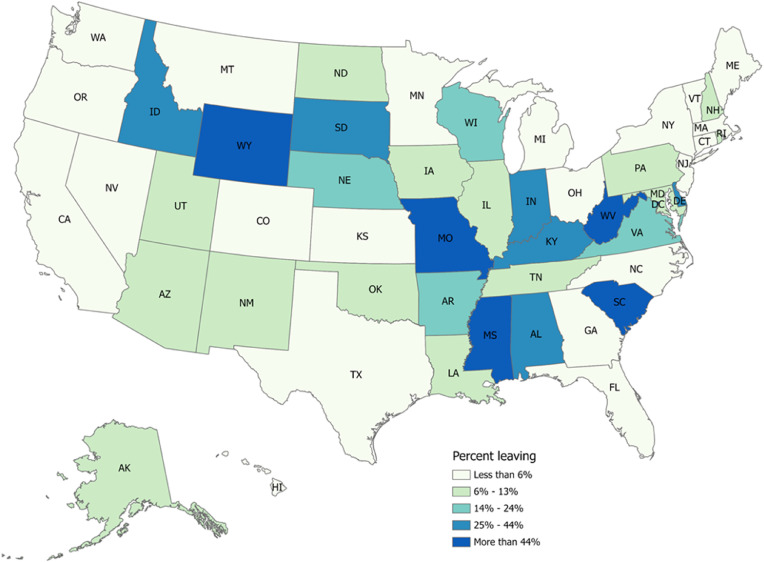
An average percent leaving of 8% belies the wide range in percent of patients crossing state lines for abortion care (Figure 1). In 12 states, more than a quarter of patients traveled out of state, while 13 states had fewer than 4% of patients leaving (Table 1). In four states–Mississippi, Missouri, South Carolina, and Wyoming—more than half of patients left their state.
Figure 1.
Percent of patients leaving state of residence for abortion care in 2017 for 50 states plus DC. Note: natural breaks for categorization determined using the Jenks method.
Categorizing states by the policy landscape shows differences in percent leaving by abortion policy scores (Table 2). States with hostile policies (N = 29) average 12% leaving, while middle ground states (N = 8) and states with supportive policies states (N = 14) average 10% and 3% leaving, respectively. The highest percent leaving, 36%, are those with a -1 abortion policy score, though this is largely driven by the high percent of patients leaving the small geographic areas of Delaware (40%) and the District of Columbia (48%); the seven states with a -6 policy score average 27% leaving.
Table 2.
Number of abortions, abortion rate, facility density, out of state abortions, and percent leave by abortion policy score, 2017.
| Abortion policy score | Number of states | No. abortions among state residents | Abortion ratea among state residents | Facility densityb | No. abortions obtained out of state | Percent of out-of-state abortions | Average facility density | Average percent leaving | States | |
|---|---|---|---|---|---|---|---|---|---|---|
| Hostile (29) | -6 | 7 | 51900 | 8.6 | 4.3 | 14133 | 27.2% | 6.9 | 11.7% | Arizona, Arkansas, Indiana, Louisiana, Mississippi, Missouri, South Dakota |
| -5 | 9 | 120550 | 8.9 | 4.1 | 16260 | 13.5% | Alabama, Kentucky, North Dakota, Ohio, Oklahoma, South Carolina, Tennessee, Texas, Utah | |||
| -4 | 6 | 91430 | 11.6 | 7.0 | 12573 | 13.8% | Nebraska, North Carolina, Pennsylvania, Virginia, West Virginia, Wisconsin | |||
| -3 | 4 | 63960 | 13.1 | 8.8 | 2614 | 4.1% | Georgia, Idaho, Kansas, Michigan | |||
| -2 | 3 | 73010 | 16.4 | 16.9 | 1364 | 1.9% | Florida, Iowa, Wyoming | |||
| Middle Ground (8) | -1 | 3 | 9030 | 15.0 | 19.9 | 3206 | 35.5% | 18.1 | 9.8% | Delaware, District of Columbia, New Hampshire |
| 0 | 3 | 24000 | 12.7 | 14.3 | 945 | 3.9% | Colorado, Nevada, Rhode Island | |||
| 1 | 2 | 20930 | 13.0 | 21.8 | 1146 | 5.5% | Maine, Massachusetts | |||
| Supportive (14) | 2 | 3 | 38460 | 16.0 | 15.0 | 3024 | 7.9% | 21.2 | 3.3% | Alaska, Maryland, Minnesota |
| 3 | 6 | 103210 | 18.2 | 19.2 | 5029 | 4.9% | Connecticut, Illinois, Montana, New Jersey, New Mexico, Vermont | |||
| 4 | 4 | 132990 | 20.5 | 26.6 | 5399 | 4.1% | Hawaii, New York, Oregon, Washington | |||
| 5 | 0 | – | – | – | – | – | – | |||
| 6 | 1 | 131380 | 16.3 | 20.0 | 142 | 0.1% | California | |||
| TOTAL | 51 | 860850 | 13.6 | 12.7 | 65835 | 7.6% |
Abortion rate is the abortions per 1000 women aged 15–44 in state of residence.
Facility density is the number of abortion facilities per million women aged 15–44.
Examining patterns of patient flow from one policy category to another (Table 3) shows that of all patients who leave their state of residence, 39% both reside in and go to a state with hostile policy designation for abortion care. Overall, 71% of patients leaving their state of residence are coming from states with hostile policies, and 43% of those leaving are going to states with hostile policies.
Table 3.
Number and percent of patients going to and coming from each abortion policy category.
| No. (%) of pts going to hostile states | No. (%) of pts going to middle ground states | No. (%) of pts going to supportive states | TOTAL | |
|---|---|---|---|---|
| No. (%) of pts leaving hostile states | 25471 (39%) | 2601 (4%) | 8803 (13%) | 46944 (71%) |
| No. (%) of pts leaving middle ground states | 777 (8%) | 549 (1%) | 589 (1%) | 5297 (8%) |
| No. (%) of pts leaving supportive states | 1933 (3%) | 2375 (4%) | 2828 (4%) | 13594 (21%) |
| TOTAL | 28181 (43%) | 5525 (8%) | 12220 (19%) | 65835 (100%) |
Facility density ranges widely, from 68·6 facilities per million women aged 15–44 in Maine, 52·2 in Vermont, and 38·3 in Connecticut, to 2·6 in Missouri, 1·7 in Mississippi, and 1·2 in Kentucky (Table 1). States with hostile policies averaged the lowest facility density (6·9), while states with supportive policies averaged the highest (21·2) (Table 2).
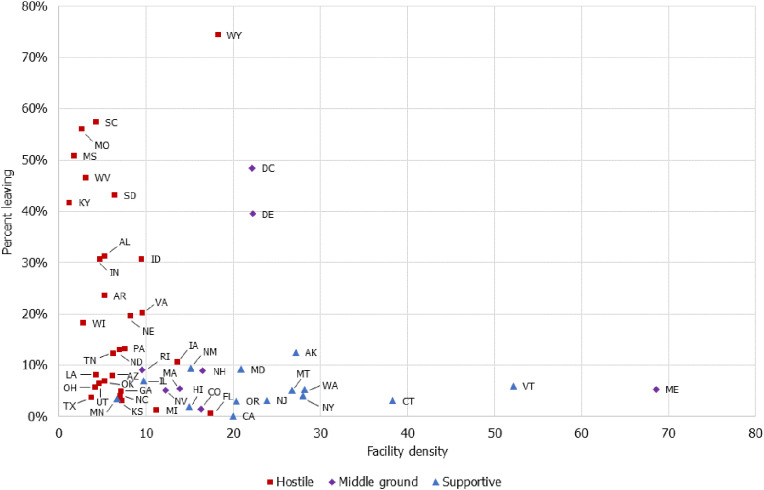
When facility density, percent leaving, and policy environment are plotted together (Figure 2), we observe that those states with a lower facility density tended to have a higher percentage of patients leaving. Spearman rank correlations show all three measures (facility density, percent leaving, and policy environment) to be statistically significantly related as well, indicating that percent leaving is associated with facility density, facility density is associated with policy environment, and percent leaving is associated with policy environment: ρleave,facility = −0.41, p = 0.0025; ρleave,score = −0.55, p < 0.001; and ρscore,facility = −0.85, p < 0.001. Within policy environment strata, correlations between percent leaving and facility density are no longer statistically significant at p < 0.05 (ρhostile = −0.31, p = 0.10; ρmiddle = 0.24, p = 0.57 and ρsupportive = 0.15, p = 0.60), indicating that within a single policy environment, percent leaving is not associated with facility density.
Figure 2.
Scatterplot of facility density against percent leaving state of residence for abortion, by abortion policy category in 2017.
Discussion
Our analysis of data from the CDC shows that substantial numbers of people, more than 65,000, or nearly 8% of all people who have an abortion in the US, travel out of state for abortion care. While prior research from facilities, states, and regions reflects similar patterns of patient travel,11,18,19 this study is the first to comprehensively examine interstate travel across all 50 states (plus DC) together with variation in facility density and policy environments.
Abortion patients may leave their state for care for many reasons, including state restrictions related to gestational limits,20 waiting periods,21 and parental notification requirements or judicial bypass processes,22 as well as if a clinic out of state is more conveniently located, has a shorter wait time, or has another characteristics preferred by the patient.18,23 In our study, we found that a higher percentage of people living in states with policies more hostile to abortion travel out of state for abortion care (12%) than those living in states with protected access (3%), suggesting that restrictive abortion policy may be one of the factors related to patients leaving their state for care. The plurality (39%) of those who leave their state for abortion care leave a state with a restrictive policy environment and obtain their abortion in another state with a restrictive environment. This finding illuminates the fact that many patients who leave their state for care live in and near states with hostile designation, due to the clustering of policy environment by geography. Additionally, this finding highlights that a simple determination of ‘restrictiveness’ may ignore geographic nuance in access to abortion care. Geography influences the location where some patients obtain abortions; they may leave their state of residence to access the closest facility,18 a factor that changes as facilities in a state close.5,24 Others have described the experiences of living in abortion deserts,7 and high percentages of women live in counties without an abortion facility.15
Examining percent leaving, policy category, and facility density concurrently, we see that states with hostile policy designation tend to have a lower facility density, yet are associated with a range of percent leaving. Similarly, states with supportive policy designation have consistently low levels of percent leaving, while having a range of facility densities. The pattern revealed in the scatterplot suggests that having a low facility density is a necessary, though not sufficient, condition for having high percent leaving. Correlational analyses of these three variables suggest that the relationship between percent leaving and facility density differs across, but not within, policy environments. The only exception may be that within states considered to be hostile, lower facility density is associated with a higher percent leaving at p = 0.1. In all, states with hostile policies have both a lower facility density as well as a higher percent leaving. Abortion restrictions make it harder for existing facilities to remain in operation and discourage new health care facilities from taking on abortion care.3 It is possible that restrictive policy environments in combination with low facility density leads to more leaving, and that restrictive environments drive low facility density in places where demand then cannot be met. Our analysis does not include the physical size of states, and future researchers may want to consider that the experience of leaving a state differs by its size: leaving Texas can involve more driving than leaving Delaware.
Our findings are limited by the CDC data which are not inclusive of reliable, consistent counts of abortions and percent leaving for all states. However, by adjusting counts by the more reliable data from the Guttmacher Institute, we can leverage the unique characteristics of the CDC data along with the completeness of the Guttmacher data. In calculating the number of patients leaving from the four states that do not report or fail to follow reporting guidelines, we rely on counts from surrounding states that do provide this information. Notably, if patients from one of these “missing” states traveled to another “missing” state, those patients would be missing from leave counts. The true number (and percent) leaving for these four states may thus be higher than our estimates; though given geographic distribution, the number of patients missing for this reason is likely relatively small. Similarly, our analysis of which abortion policy environments patients are going to and from lacks data on patients going to California, Maryland, New Hampshire, and Wyoming. These four states represent all three policy environments (California is supportive, Maryland and New Hampshire are middle ground, and Wyoming is hostile). In addition, given the large number of abortions taking place in California (approximately 15% of all abortions in the US) it is likely that there are more patients traveling to supportive states than is represented in our findings. Uncounted travel from hostile to supportive is especially likely when measuring travel from states surrounding California, including Nevada which is considered middle ground and Arizona which is considered hostile.
Additionally, while our analysis of state policy environment and facility density comprise two sets of reasons that patients may leave their state of residence, this data cannot speak directly to why any one patient travels for care. Facility density is a crude measure of access. While a facility may exist, its presence in a state does not mean that it has the capacity to see people in a timely way, that it is physically accessible to people who seek care, or that it has the type of care people need. While we note an association between facility density and percent leaving their state for abortion, the limitations about what facility density represents precludes our ability to attribute degree of leaving to facility density. Furthermore, additional research assessing patient perspectives, like Cohen and Joffe's work,12 is necessary for further understanding why patients travel, with special attention to those leaving their home states. Furthermore, this data cannot be used to distinguish between subgroups of patients who are either more likely to have an abortion, or to travel for care. Additional attention to the demographics of patients who leave for care will be important to understand the inequitable distribution of burdens on patients of color and low-income patients who want abortion care.
Finally, because patient counts represent those individuals seeking an abortion who were able to obtain care at a facility, this analysis entirely misses those who traveled for care but were not able to receive it, or those who would have traveled but did not have the resources to reach a facility. Our analysis does not consider abortions that were undertaken outside of the formal medical system.
Nonetheless, the present study makes novel use of data provided by the CDC on number of abortions by state of occurrence alongside state of patient residence. While other data describing abortion rates by state of occurrence15 and residence33 individually is available, they do not provide the cross-comparison of state of occurrence and state of patient residence necessary for analyzing the number and percent of patients leaving each state. Given the state-level variation in abortion policy2,3,25 and disparity in abortion facility proximity to women of reproductive age,15 analysis of this data is both important and timely.
Negative impacts of needing to travel for abortions are well documented. These include delays to care21 (and as care is delayed, patients face some increased risk of complication from their abortion)26 as well as increased cost.27 Similarly, low facility density may result in longer wait times and facility congestion, where facilities may not be able to meet the demand of a relatively high number of patients.28 These burdens are particularly meaningful for those who have low incomes, are traveling further due to living in rural areas or abortion deserts, or experience other intersecting forms of structural oppression (for example related to race, gender, sexuality, or ability) that limit access to holistic reproductive healthcare.29 We note that several states have facilities near their borders, suggesting that that travel from one state to another may not represent a meaningful distance in travel, and may be best for a patient seeking abortion care. Future research could focus on states with border facilities to examine driving distance and facility congestion in combination with interstate travel.
While some people who live near the border of their state will leave their state for abortion care while still staying close to home, for those living in larger states, crossing state lines may be more of a burden. Beyond the challenges due to travel itself, leaving one's state of residence for an abortion illuminates other public health burdens. Health insurance through Medicaid can only be used within the state of residence, and private insurance plans may have geographic limits; traveling out of state may preclude use of health insurance for abortion. Having to travel to another state for a standard procedure like abortion may also increase patient's anxiety and add additional strain on their resources. Abortion care is highly stigmatized,30,31 and that stigma is reinforced when services are limited or unavailable such that a person travels away from their home state to access the care.
State restrictions that necessitate travel for abortion care, and lack of available in-state abortion facilities, represent burdens for patients attempting to access abortion care. Furthermore, as the right to abortion under Roe v. Wade becomes increasingly threatened,32 further examination of ways to facilitate access to care, including to non-adjacent states, remains vitally important.
Contributors
Smith is the lead author and contributed to the literature search, analysis, data curation, administration, writing, and reviewing of the manuscript.
Muzyczka contributed to the literature search, writing, and reviewing of the manuscript.
Chakraborty contributed to the analysis, figure creation, writing, and reviewing of the manuscript.
Johns-Wolfe contributed to figure creation.
Higgins contributed to the conceptualization, literature search, and writing of the manuscript.
Bessett contributed to the conceptualization, literature search, supervision, writing, reviewing of the manuscript, and funding acquisition for the project.
Norris contributed to the conceptualization, literature search, analysis, supervision, writing, reviewing of the manuscript, and funding acquisition for the project.
Data sharing statement
This study uses publicly available data from the CDC (https://www.cdc.gov/reproductivehealth/data_stats/abortion.htm), the US Census (https://data.census.gov/), and the Guttmacher Institute (https://www.guttmacher.org/report/abortion-incidence-service-availability-us-2017, https://www.guttmacher.org/report/pregnancies-births-abortions-in-united-states-1973-2017, and https://www.guttmacher.org/article/2019/08/state-abortion-policy-landscape-hostile-supportive).
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
The authors have no conflicts of interest to disclose.
Acknowledgments
We thank Rachel Jones, Whitney Rice, Ushma Upadhyay, Kari White, and Amy Williamson for their input on earlier versions of this manuscript.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2022.100214.
Appendix. Supplementary materials
References
- 1.Library of Congress. US. Reports: Roe v. Wade, 410 U.S. 113 (1973). Library of Congress, Washington, DC. 20540 USA. Published 1973. Accessed July 6, 2021. https://www.loc.gov/item/usrep410113/
- 2.Guttmacher Institute . Guttmacher Institute; 2021. An Overview of Abortion Laws.https://www.guttmacher.org/state-policy/explore/overview-abortion-laws Accessed January 9, 2019. [Google Scholar]
- 3.Guttmacher Institute . Guttmacher Institute; 2021. Targeted Regulation of Abortion Providers.https://www.guttmacher.org/state-policy/explore/targeted-regulation-abortion-providers Accessed August 20, 2021. [Google Scholar]
- 4.Medoff M.H., Dennis C. TRAp abortion laws and partisan political party control of state government. Am J Econ Sociol. 2011;70(4):951–973. doi: 10.1111/j.1536-7150.2011.00794.x. [DOI] [PubMed] [Google Scholar]
- 5.Raifman S., Sierra G., Grossman D., et al. Border-state abortions increased for Texas residents after House Bill 2. Contraception. 2021;104(3):314–318. doi: 10.1016/j.contraception.2021.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGowan M.L., Norris A.H., Bessett D. Care churn — why keeping clinic doors open isn't enough to ensure access to abortion. N Engl J Med. 2020;383(6):508–510. doi: 10.1056/NEJMp2013466. [DOI] [PubMed] [Google Scholar]
- 7.Hennessy-Fiske M. Los Angeles Times; 2016. Crossing the “Abortion Desert”: Women Increasingly Travel out of Their States for the Procedure.https://www.latimes.com/nation/la-na-adv-abortion-traveler-20160530-snap-story.html [Google Scholar]
- 8.Bearak J.M., Burke K.L., Jones R.K. Disparities and change over time in distance women would need to travel to have an abortion in the USA: a spatial analysis. Lancet Public Health. 2017;2(11):e493–e500. doi: 10.1016/S2468-2667(17)30158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cartwright A.F., Karunaratne M., Barr-Walker J., Johns N.E., Upadhyay U.D. Identifying national availability of abortion care and distance from major US cities: systematic online search. J Med Internet Res. 2018;20(5) doi: 10.2196/jmir.9717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones RK, Jerman J. Time to appointment and delays in accessing care among U.S. abortion patients. Published online August 9, 2016. Accessed July 29, 2021. https://www.guttmacher.org/report/delays-in-accessing-care-among-us-abortion-patients
- 11.Barr-Walker J., Jayaweera R., Ramirez A.M., Gerdts C. Experiences of women who travel for abortion: a mixed methods systematic review. PLoS One. 2019;14(4):1026. doi: 10.1371/journal.pone.0209991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen D.S., Joffe C. University of California Press; 2021. Obstacle Course: The Everyday Struggle to Get an Abortion in America. [Google Scholar]
- 13.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; 2020. CDCs Abortion Surveillance System FAQs | CDC.https://www.cdc.gov/reproductivehealth/data_stats/abortion.htm Accessed March 22, 2021. [Google Scholar]
- 14.Guttmacher Institute. Abortion Reporting Requirements. Published November 1, 2021. Accessed November 24, 2021. Guttmacher Institute https://www.guttmacher.org/state-policy/explore/abortion-reporting-requirements
- 15.Jones R.K., Witwer E., Jerman J. Guttmacher Institute; 2019. Abortion Incidence and Service Availability in the United States, 2017. [DOI] [Google Scholar]
- 16.United States Census Bureau. 2014-2018 ACS Demographic and Housing Estimates. United States Census Bureau. Published 2021. Accessed March 22, 2021. https://data.census.gov/
- 17.Nash E. State abortion policy landscape: from hostile to supportive; 2021. Accessed May 12, 2021. https://www.guttmacher.org/article/2019/08/state-abortion-policy-landscape-hostile-supportive
- 18.Fuentes L., Jerman J. distance traveled to obtain clinical abortion care in the United States and reasons for clinic choice. J Womens Health. 2019;28(12):1623–1631. doi: 10.1089/jwh.2018.7496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones R.K., Jerman J. How far did US women travel for abortion services in 2008? J Womens Health. 2013;22(8):706–713. doi: 10.1089/jwh.2013.4283. [DOI] [PubMed] [Google Scholar]
- 20.Upadhyay U.D., Weitz T.A., Jones R.K., Barar R.E., Foster D.G. Denial of abortion because of provider gestational age limits in the United States. Am J Public Health. 2014;104(9):1687–1694. doi: 10.2105/AJPH.2013.301378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finer L.B., Frohwirth L.F., Dauphinee L.A., Singh S., Moore A.M. Timing of steps and reasons for delays in obtaining abortions in the United States. Contraception. 2006;74(4):334–344. doi: 10.1016/j.contraception.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 22.Dennis A, Henshaw SK, Joyce TJ, Finer LB, Blanchard K. The impact of laws requiring parental involvement for abortion: a literature review. Published online March 18, 2009. Accessed July 29, 2021. https://www.guttmacher.org/report/impact-laws-requiring-parental-involvement-abortion-literature-review
- 23.Heymann O., Odum T., Norris A.H., Bessett D. Selecting an abortion clinic: the role of social myths and risk perception in seeking abortion care. J Health Soc Behav. 2021 doi: 10.1177/00221465211044413. [DOI] [PubMed] [Google Scholar]
- 24.Gerdts C., Fuentes L., Grossman D., White K. Impact of clinic closures on women obtaining abortion services after implementation of a restrictive law in Texas. Am J Public Health. 2021;106(5) doi: 10.2105/AJPH.2016.303134. Accessed April 19. https://ajph.aphapublications.org/doi/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.NARAL. Who decides? The Status of women's reproductive rights in the United States; 2019. Accessed February 3, 2020. https://www.prochoiceamerica.org/report/2019-who-decides-the-status-of-womens-reproductive-rights-in-the-united-states/
- 26.Zane S., Creanga A.A., Berg C.J., et al. Abortion-related mortality in the United States 1998–2010. Obstet Gynecol. 2015;126(2):258–265. doi: 10.1097/AOG.0000000000000945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones R.K., Upadhyay U.D., Weitz T.A. At what cost? Payment for abortion care by U.S. women. Womens Health Issues. 2013;23(3):e173–e178. doi: 10.1016/j.whi.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 28.Lindo J.M., Myers C.K., Schlosser A., Cunningham S. How far is too far? New evidence on abortion clinic closures, access, and abortions. J Hum Resour. 2020;55(4) doi: 10.3368/jhr.55.4.1217-9254r3. N.PAG-N.PAG. [DOI] [Google Scholar]
- 29.Ross L., Solinger R. University of California Press; 2017. Reproductive Justice.https://www.ucpress.edu/book.php?isbn=9780520288201 Accessed October 6, 2018. [Google Scholar]
- 30.Norris A., Bessett D., Steinberg J.R., Kavanaugh M.L., De Zordo S., Becker D. Abortion stigma: a reconceptualization of constituents, causes, and consequences. Womens Health Issues. 2011;21(3):S49–S54. doi: 10.1016/j.whi.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 31.Hanschmidt F., Linde K., Hilbert A., Riedel-Heller S.G., Kersting A. Abortion stigma: a systematic review. Perspect Sex Reprod Health. 2016;48(4):169–177. doi: 10.1363/48e8516. [DOI] [PubMed] [Google Scholar]
- 32.Myers C., Jones R., Upadhyay U. Predicted changes in abortion access and incidence in a post-roe world. Contraception. 2019;100(5):367–373. doi: 10.1016/j.contraception.2019.07.139. [DOI] [PubMed] [Google Scholar]
- 33.Maddow-Zimet Isaac, Kost Kathryn. Pregnancies, Births and Abortions in the United States, 1973–2017: National and State Trends by Age. Guttmacher Institute. 2021 doi: 10.1363/2021.32709. https://www.guttmacher.org/report/pregnancies-births-abortions-in-united-states-1973-2017 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.