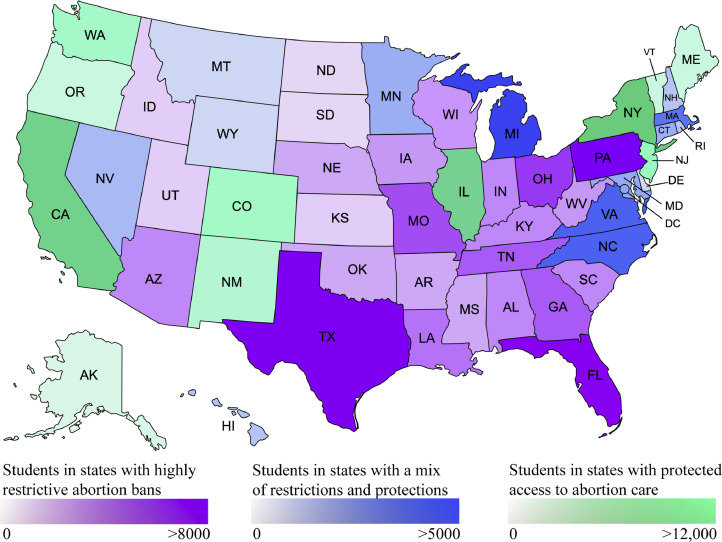
On June 24, 2022, the U.S. Supreme Court, in Dobbs v Jackson Women's Health Organisation, overturned the federal right to abortion established in Roe v Wade. This decision jeopardises the physical and psychological health of millions of pregnant people and their families. It also has profound implications for medical education and will fundamentally reshape the knowledge, skills, and quality of care provided by future physicians. Under Dobbs, 70.77% of the 129,295 US medical students1,2 will have their training restricted by state laws: 66,088 (51.11%) in states with highly restrictive abortion bans and 25,412 (19.65%) in states with a mix of restrictions and protections. Only 37,795 (29.23%) medical students will train in protected states (Figure 1).3
Figure 1.
Medical student enrollment in the United States and legal status of abortion under Dobbs.
Total student enrollment in medical schools in 2021–2022 (n=129,295). Medical students located in states with restrictive abortion laws (n = 91,500; 70.77%). 66,088 (51.11%) are located in states with highly restrictive abortion bans, 25,412 (19.65%) are located in states with a mix of restrictions and protections, and 37,795 (29.23%) are located in states with protected access to abortion care.
Dobbs impairs medical students’ ability to learn and provide safe, evidence-based clinical care to patients. Medical school teaches us pathophysiology, anatomy, and ethical clinical decision making, equipping us with a foundation to provide factual, ethical counselling for patients to make decisions about their own health. In addition to unintended pregnancy, abortion is medically indicated for pregnancy complications including placental abruption, infection, ectopic pregnancy, and eclampsia. The same medications and surgical techniques utilised for abortion also treat obstetric complications; students without abortion training will be limited in the skills necessary to manage these. Rates and severity of complications from unsafe abortion attempts will increase where abortion access is limited,4 and physicians in these regions will not be trained in their treatment. Without adequate education, long-term quality of reproductive healthcare in the U.S. will deteriorate.
Medical schools must educate students about all topics in healthcare, including abortion.5 Lack of education propagates misconceptions surrounding those who seek abortion. If students cannot observe abortion services, false beliefs surrounding abortion grow, further alienating individuals who choose abortion to improve their health.6 This precipitates polarized discourse, which is detrimental to a field reliant upon team-centred care.
Abortion care discourse is particularly important for teaching professionalism and deconstructing biases.6 Students need to learn to reflect on the relationship between personal beliefs and obligations as a medical professional, particularly when these diverge. Abortion training improves metrics of respect for patient privacy and autonomy, commitment to ethical principles, professionalism, and humanism.5 It challenges students’ existing viewpoints, encouraging them to scrutinize their biases about the reasons patients seek care and respect patients’ decisions about their care.5,6 Education including patient-centred discussion of sensitive topics is crucial to developing a patient-physician relationship based on trust and medical ethics. Eliminating abortion education will prevent future physicians from providing comprehensive family planning counselling and following fundamental bioethical principles of patient autonomy and non-maleficence. Students learning within this rigid practice, grounded not in medical best practices but in fear, will observe a blunted version of “shared-decision making”.7 To give true informed consent, a patient must understand all options, including those which a provider may not personally support. The patient-physician relationship is a social contract: we put the rights and interests of our patients above our own.8 It is paradoxical for a medical school to instill the principles of medical ethics while simultaneously refraining from providing students with the tools to implement them when treating patients.
Medical students with no option but to carry a pregnancy to term, may have to take a leave of absence, require childcare during clerkships, or forgo completing their medical degree to raise the child. This will contribute to the current physician shortage in the U.S., further limiting healthcare access. In rural regions, where healthcare resources are already disproportionately limited, this will be a particularly salient problem. 4,9 Dobbs may exacerbate these disparities because some students have anecdotally expressed their decision not to pursue clinical training or practice in states that outlaw or greatly limit abortions in favour of a more comprehensive education.10 To protect both their own and their patients’ reproductive health, students may cluster in states where abortion remains accessible, further exacerbating inequities in healthcare. Consequently, physician shortages and school enrolment in states with abortion bans will worsen.9
Fundamentally, abortion is a medical treatment which patients should have the right to choose during shared decision-making conversations with their providers. This is harmed by legislative interference. Abortion education is essential in preparing future physicians to preserve the sanctity of the patient-physician relationship, provide medically accurate clinical recommendations, and comprehensively manage all aspects of necessary healthcare. In the face of Dobbs, we as learners and educators must work together to ensure all medical schools develop or expand their abortion curricula in all ways possible to mitigate the inevitable adverse impacts on patients seeking safe and unbiased pregnancy-related care.
Contributors
Ariana M. Traub: conceptualisation of manuscript, drafted the original manuscript, created the figure, contributed to the literature search, and reviewed, edited and revised the manuscript.
Kellen Mermin-Bunnell: drafted the original manuscript, contributed to the literature search, and reviewed, edited, and revised the manuscript, data, and figure.
Priyasha Pareek: drafted the original manuscript, contributed to the literature search, and reviewed and edited the manuscript.
Sonya Williams: collected the data, contributed to the literature search, and reviewed and edited the manuscript.
Natalie Connell: collected the data, contributed to the literature search, and reviewed, edited, and revised the manuscript.
Jennifer F. Kawwass and Carrie Cwiak: reviewed and provided substantial editing to the manuscript.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
We declare no competing interests.
Ms. Traub has nothing to disclose.
Ms. Mermin-Bunnell has nothing to disclose.
Ms. Pareek has nothing to disclose.
Ms. Williams has nothing to disclose.
Ms. Connell has nothing to disclose.
Dr. Kawwass has nothing to disclose.
Dr. Cwiak has nothing to disclose.
Funding
None
References
- 1.Association of American Medical Colleges. FACTS: enrollment, graduates, and MD-PhD Data. 2021. https://www.aamc.org/data-reports/students-residents/interactive-data/2021-facts-enrollment-graduates-and-md-phd-data. Accessed 2 July 2022.
- 2.American Association of Colleges of Osteopathic Medicine. Reports on student enrollment. https://www.aacom.org/reports-programs-initiatives/aacom-reports/student-enrollment. Accessed 2 July 2022.
- 3.Guttmacher Institute. Interactive map: US abortion policies and access after Roe. https://states.guttmacher.org/policies/. Accessed 2 July 2022.
- 4.Harris LH. Navigating loss of abortion services - a large academic medical center prepares for the overturn of Roe v. Wade. N Engl J Med. 2022;386:2061–2064. doi: 10.1056/NEJMp2206246. [DOI] [PubMed] [Google Scholar]
- 5.Merz AA, Janiak E, Mokashi M, et al. “We're called upon to be nonjudgmental” a qualitative exploration of United States medical students' discussions of abortion as a reflection of their professionalism. Contraception. 2022;106:57–63. doi: 10.1016/j.contraception.2021.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Burns RM, Shaw KA. Standardizing abortion education: What medical schools can learn from residency programs. Curr Opin Obstet Gynecol. 2020;32(6):387–392. doi: 10.1097/GCO.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 7.Chen M, Lindley A, Kimport K, Dehlendorf C. An in-depth analysis of the use of shared decision making in contraceptive counseling. Contraception. 2019;99(3):187–191. doi: 10.1016/j.contraception.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 8.Cruess R.L., Cruess S.R. Expectations and obligations: professionalism and medicine's social contract with society. Perspect Biol Med. 2008;51(4):579–598. doi: 10.1353/pbm.0.0045. [DOI] [PubMed] [Google Scholar]
- 9.Vinekar K, Karlapudi A, Nathan L, Turk JK, Rible R, Steinauer J. Projected implications of overturning Roe v Wade on abortion training in U.S. obstetrics and gynecology residency programs. Obstet Gynecol. 2022:10–1097. doi: 10.1097/AOG.0000000000004832. https://journals.lww.com/greenjournal/fulltext/9900/projected_implications_of_overturning_ roe_v_wade.449.aspx [DOI] [PubMed] [Google Scholar]
- 10.Giglio ME, Magalski GR, Doan YP, Bowman S. Abortion training in medical education — implications of the Supreme Court's upcoming decision. N Engl J Med. 2022;386(8):707–709. doi: 10.1056/NEJMp2117368. [DOI] [PubMed] [Google Scholar]