Summary
Communicating public health guidance is key to mitigating risk during disasters and outbreaks, and ethical guidance on communication emphasizes being fully transparent. Yet, communication during the pandemic has sometimes been fraught, due in part to practical and conceptual challenges around being transparent. A particular challenge has arisen when there was both evolving scientific knowledge on COVID-19 and reticence to acknowledge that resource scarcity concerns were influencing public health recommendations. This essay uses the example of communicating public health guidance on masking in the United States to illustrate ethical challenges of developing and conveying public health guidance under twin conditions of uncertainty and resource scarcity. Such situations require balancing two key principles in public health ethics: the precautionary principle and harm reduction. Transparency remains a bedrock value to guide risk communication, but optimizing transparency requires consideration of additional ethical values in developing and implementing risk communication strategies.
Keywords: Risk communication, COVID-19, Pandemic, Transparency, Precautionary principle, Infection prevention and control
Introduction
Public adoption of risk mitigation strategies during an infectious disease outbreak depends on several factors, including perceptions of risk severity and vulnerability; the veracity, trustworthiness, and credibility of messengers; the sense of self-efficacy; and community attitudes and norms. All of these can be affected by communications from public health leaders, making communication one of the most important tools in managing risk during an outbreak.1,2 In the United States, communication efforts over the course of the coronavirus disease 2019 (COVID-19) pandemic have been marked by mixed and muddled messages, public confusion, partisan politics, and attributions of incompetence or even malice on the part of public officials—all of which contributed to less-than-optimal public adoption of simple and effective interventions such as face coverings, physical distancing, and vaccination.3 A common critique has been that public health leaders need to simply follow the cardinal ethical rule of public health communication: be transparent. But in fairness, being transparent during the pandemic has been remarkably challenging. In particular, some of the most muddled messages have come about, in part, because public health leaders have been reticent to acknowledge that both uncertain science and resource scarcity were affecting their recommendations.
In this paper, we examine both the design and communication of risk mitigation strategies for public health, which are closely intertwined in fast-moving public health emergencies. We use the example of designing and communicating guidance on masking in the US during February – July 2020 to illustrate ethical challenges facing officials seeking to transparently convey public health guidance under twin conditions of evolving science and resource shortages.
Evolving Guidance on Mask Use During the COVID-19 Pandemic
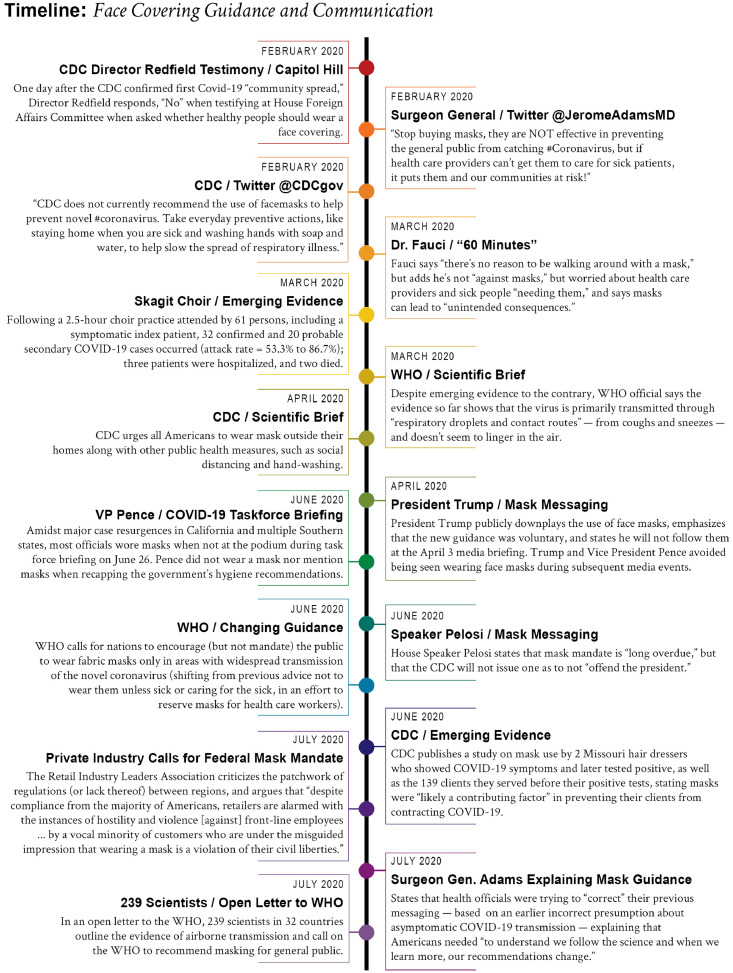
In early February 2020, the U.S. Centers for Disease Control and Prevention (CDC) recommended mask use only for health workers and individuals exhibiting COVID-19 symptoms. By late February, evidence on masking for the general public remained incomplete but had turned toward suggesting benefits, yet public health leaders elected to continue messaging that the general public need not use masks and even that they might be ineffective (Figure 1).
Figure 1.
Timeline of early public health guidance and communication for face coverings.
This approach was influenced by fears of public panic-buying of health care-grade masks,4 potentially exacerbating already severe shortages of respirators (e.g., N95 “masks” with adequate training and fit testing) in health care settings. In short, despite growing evidence that widespread use of surgical masks or respirators was the safest approach to prevent contracting and spreading the virus, inadequate supplies of masks made recommending their use to the public infeasible and possibly counterproductive. For two months, public health leaders continued to argue against mask use for the general public—a posture that later aided political opposition to masks, undermining the credibility of public health experts. During those two months, COVID-19 cases proliferated and evidence accumulated that in both pre-symptomatic and asymptomatic persons, high viral loads and virus shedding yielded both droplet and aerosolized transmission5 (Figure 1).
In a sharp turn, on April 3, 2020, the CDC urged universal mask use by the public. By mid-April, a bipartisan consensus had developed on the severity of the COVID-19 threat, with broad support for shelter-in-place recommendations. Yet, some political actors downplayed the severity of COVID-19 and the need for protective measures such as masking, and they found an opportunity in the conflicting masking messaging (Figure 1). When partisan competition emerges, including debate among political actors around health guidance, it shapes subsequent public understanding and policy support.6 Media that highlights these debates and downplays threats to population health outcomes can further delay protective behaviour by encouraging “threat dismissal.”7
This dynamic was not unique to the United States. The World Health Organization (WHO) took even longer to change its masking recommendations. By early summer of 2020, multiple studies had produced compelling evidence of virus transmission via smaller (aerosol) and larger (droplet) respiratory particles. In a July 2020 open letter to WHO, 239 scientists from 32 countries called on the agency to revise its recommendations8 to acknowledge the aerosol transmission of SARS-CoV-2 and adjust protective measure recommendations accordingly. The scientists recommended more stringent ventilation standards for indoor spaces and broad use of N95 respirators, particularly in healthcare settings.9
Several harmful consequences resulted from fragmented, contradictory, opaque, and even misinformation in messaging. The public grew increasingly distrustful of credible experts. Scientific uncertainty, which is expected in the face of a new pathogen, began to be viewed as reflecting flawed science. Arguments for and against various mitigation strategies increasingly focused on values, sometimes ignoring data altogether, and instead pitting individual freedom and rights against care for the collective. Emotional responses to the risk of disease and to these value differences led to behaviours that caused the rapid spread of the virus resulting in many excess deaths.
Public health ethical principles for designing risk mitigation strategies
A number of principles often come into play in crafting public health interventions, such as proportionality, reciprocity, solidarity and so on. But two primary ethical principles should be held in balance when designing public health recommendations under conditions of both uncertainty and scarcity.
Uncertainty often prompts the use of the precautionary principle (PP) (Table 1), because this principle encourages the implementation of risk-reducing strategies in situations involving the risk of serious harm and evolving evidence. In brief, the PP forces recognition that scientific uncertainty is common and should not preclude taking protective action. But because the PP encourages action, it can underappreciate the importance of considering whether a proposed protective action will be acceptable or possible for all stakeholders – indeed, the PP is often called upon specifically to support implementing protective actions that some stakeholders would rather not take.
Table 1.
Definitions of public health ethics principles to guide the design of risk mitigation strategies.
| Public Health Ethical Principle | Expanded Definition |
|---|---|
| Precautionary Principle (PP) | When significant risks to individuals and communities arise, but some uncertainty about the risk remains, prudent steps should be taken to mitigate the risk even as the evidence evolves. The PP places a penumbra of precaution over a number of sub-principles such as proportionality and reasonableness (risk/cost assessments, tradeoff considerations); responsibility (those creating risks should bear a greater burden of prevention); and reciprocity (shared benefit demand shared burdens).10 Intrinsic in the PP is the acknowledgement that there are ethical and practical risks of waiting for certainty before implementing safety measures, especially because certainty might never arrive. Science rarely achieves certainty and is permeated with language describing relative levels of uncertainty, exemplified by discussions of “statistical significance” and “confidence intervals” by “limitations” sections of research papers, and by frequent conclusions in science that “more research is needed.” In this light, the PP urges researchers, policymakers, and the public to make decisions based on the weight and credibility of evidence rather than awaiting elusive scientific certainty.11 |
| Harm Reduction (HR) | When a risky activity cannot reasonably be eliminated, whether because of social, political, legal, or cultural realities, steps should be taken to minimize the related harms of the risky activity, including minimizing its medical, social, and legal impacts. The HR principle is also described as a public health practice, philosophy, or social movement. The HR approach is predicated on recognizing that risky actions may be the result of forces beyond the control of an individual (such as resource shortages), and it is grounded in an approach of solidarity. Harm reduction “meets people where they are” and focuses on providing safer options when the safest option isn't realistic. While HR describes syringe and needle exchange programs and condom distributions programs, it also describes physical distancing, mask use, and privileging outdoor activities during the pandemic, all of which are HR strategies promoted in recognition that total social isolation for the duration of the pandemic is not feasible.12 |
In designing advice for the public about pandemic precautions, acceptability and feasibility are critical.10 When the threat is severe (e.g., highly transmissible virus with a high risk of mortality), guidance that is very disruptive or burdensome can be acceptable. Masking is one of the least intrusive measures among infectious disease prevention recommendations, with few secondary harms or burdens compared to interventions like sheltering-in-place, quarantine, and physical distancing.13 Still, adherence to masking guidance requires that the intended audience (whether the general public, health care workers, other essential workers and their employers) finds the information credible, perceives the risk to themselves and others, and believes that adopting the recommendations will reduce health risks.14 Early in the pandemic, this process relied on acceptance of growing evidence for the efficacy of masks for personal protection and to prevent spread, as well as acceptance of the ethical rationale for cooperating with guidance that restricts one's individual liberty (albeit in what many considered to be a modest way) to protect others from harm.
Another factor that can limit the use of the PP in designing public health guidance is resource scarcity since recommended interventions must be both acceptable and feasible. This follows the philosophical injunction that “ought implies can” (one cannot have an ethical obligation to do something that one simply cannot do). Early in the pandemic, the lack of sufficient medical-grade masks made a universal recommendation for their use inappropriate because it was not feasible, but not because masks were ineffective.
Under conditions of supply shortages, “harm reduction” becomes an important balancing principle in designing risk reduction strategies for the public. Harm reduction focuses on managing risks from activities that, for one reason or another, cannot reasonably be eliminated (Table 1). Facing shortages of medical-grade masks and respirators for workers and off-the-shelf masks for the public, public health guidance eventually focused on the use of masks made from readily available materials, including cloth (Figure 1). This was a harm reduction approach, imperfect but feasible. Additionally, where N95 respirators were recommended–for health care workers caring for patients with active COVID-19—resource scarcity forced the reuse of N95 respirators that were tested and approved for single-use only. This guidance too was grounded, often implicitly, in harm reduction.
Challenges to transparency
Once public guidance on risk mitigation is designed based on the best evidence available plus the precautionary principle, and if necessary, harm reduction needs, this guidance must then be effectively communicated to the intended audiences. Conventional wisdom is that communication with the public about actions they should take must always be guided by a principle of full and complete transparency. There are two reasons for this. First, transparency often engenders trust in public health officials, which is associated with behavioural adoption of the recommendation.15 Second, transparency provides information to assist individuals in mitigating risks.
A commitment to total transparency can be challenging when both uncertain science and shortages arise during a public health emergency. The WHO recommends that communications about emerging diseases be easy to understand, include what is known and unknown, and a disclosure that recommendations might change as new evidence emerges.16 Yet, transparently communicating the multifaceted, dynamic nature of risk and evolving science can inadvertently undermine the clarity of messages about suggested risk mitigation strategies.13,16,17
Unfettered transparency can also have unintended effects that can erode public trust. For instance, unfettered17 transparency can create a Catch-22 of risk communication, in which explanations of evolving information18 create confusion and undermine credibility. Multiple examples can illustrate the potentially detrimental effects of frequently shifting research and recommendations, such as confusion around nutrition or mammography screening guidelines leading to information uncertainty and mistrust.3 The public, perhaps especially those with limited science literacy, can perceive unfettered transparency about emerging science as lacking credibility, which carries with it the potential for less compliance with mitigation practices3 or unhelpful behaviours such as hoarding supplies.
Unfettered transparency that communicates uncertainty and risk can trigger potentially counter-productive emotional and behavioural reactions stemming from anxiety and fear. At moderate levels, anxiety can increase recommendation uptake, though only if it is coupled with self-efficacy4; however, anxiety can also increase perceived uncertainty, which is negatively associated with compliance.15 Risk perceptions also interact with factors such as attitudes about the value of the behaviours, perceptions about societal norms, and beliefs about one's ability to follow the recommendations.4,14 These factors, in turn, are influenced by and can influence trust in public health, political leaders and the media.
Perfect communications during a public health emergency marked by scientific uncertainty and serious resource shortages is perhaps impossible. While transparency provides a general rule of thumb and helps build public understanding and trust, unfettered transparency can result in several predictable adverse consequences. Designing and communicating public health strategies should therefore include explicit attention to other public health ethical principles, including the precautionary principle and harm reduction. Holding these principles in balance can help public health professionals develop more effective messages, including during situations when public health agencies must acknowledge that evolving evidence or resource shortages warrant reconsideration of prior recommendations.
Four tenets for communicating public health guidance under uncertainty and resource scarcity
Useful guidance for risk communication in public health emergencies exists, but the following are of particular importance for crafting messaging strategies when both uncertainty and resource scarcity are affecting the guidance being offered.
-
1.
Use trusted messengers. Trust is foundational to the uptake of recommendations, and mistrust is a particular threat when uncertainty and resource scarcity are affecting recommendations. Trusted messengers might not be scientific experts. Building and mobilizing a network of trusted messengers—people who are influential in their communities (e.g., changemakers, religious leaders, business leaders, health experts, athletes, and artists)—requires planning. Trusted messengers require training that respects their unique voices while preparing them to share accurate health information that encourages understanding and effective decision making while debunking mis- and dis-information.
-
2.
Give structure to uncertainty. Uncertainty is disconcerting but unavoidable during public health emergencies. It must be addressed using a structure that encourages informed decision-making and prevents the public from being misled by individuals and groups peddling false certainty.19 Instructions about current guidance should be clear while setting expectations about when and why recommendations might change.20 For instance, acknowledging the uncertainty of transmission dynamics and mask use guidance early in the pandemic should have been paired with a statement that guidance could change as the science evolved and supplies improved.
-
3.
Acknowledge the important role of values in making recommendations. Public health officials and scientists should acknowledge that values, as well as science, underlie their recommendations, especially when resources are in short supply. Transparency requires that pandemic risk communication be explicit about the values that guide decisions and the trade-offs considered in developing recommendations. Public health authorities are often criticized for not “following the science” in their recommendations, but science alone is inadequate for formulating policy. When resource shortages arise, for example, it might not be possible for the public to do what the best science recommends – transparency demands honesty when that is the case.
-
4.
Recognize that people often respond to risk information emotionally. Public health officials understand that risk information in an emergency is often interpreted through heightened emotions. Feeling threatened can prompt behaviours that raise or lower risks for self and others, and officials should address this in their communications to minimize behaviours such as supply hoarding. There are predictable emotional patterns in response to the threat of emerging infectious diseases, with fear, anger, and emotional exhaustion being prominent.18 Officials communicating risk should be familiar with behavioural research on how people respond to risk and incorporate that knowledge into risk communication strategies, weighing the impact of emotion on behaviour with values such as transparency, harm reduction, and precaution. Most importantly, manipulating or deceiving the public to avoid public panic or “for their own good” is not ethically acceptable. The apparent temptation to do so during the pandemic suggests the need for more research on how to optimize the delivery of truthful messages in ways that are most likely to prompt productive responses.
Conclusion
The COVID-19 pandemic response demonstrates the need to continue the challenging task of engaging the public in discussions that embrace uncertainty, strengthen the public's understanding of how scientific knowledge emerges and evolves, and the roles of values in policy making. What might constitute sufficient grounds to recommend a particular public health measure is not only a function of the strength of scientific evidence, but also of the magnitude and distribution of the risk, availability of resources to carry out the measure, acceptability of the measures, and other factors. Public health leaders should generally recommend precautionary measures under conditions of a serious threat, even when there is some uncertainty. But when optimal actions according to scientific evidence are not feasible to recommend, they should apply the harm reduction principle in formulating recommendations. Effective public health communication requires transparency and honesty not only about the data and the level of uncertainty but also on how these principles and other factors underpin decisions and recommendations.
Contributors
Lowe AE: Writing - Original Draft
Voo TC: Writing - Reviewing and Editing
Lee LM: Writing - Reviewing and Editing
Dineen KK: Writing - Reviewing and Editing
Ferdinand AO: Writing - Reviewing and Editing
Mohapatra S: Writing - Reviewing and Editing
Feig C: Writing - Reviewing and Editing
Brett-Major D: Writing - Reviewing and Editing
Wynia MK: Writing - Reviewing and Editing
Declaration of interests
The authors declared no conflicts of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.O'Malley P, Rainford J, Thompson A. Transparency during public health emergencies: from rhetoric to reality. Bull World Health Organ. 2009;87(8):614–618. doi: 10.2471/BLT.08.056689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vai B, Cazzetta S, Ghiglino D, et al. Risk perception and media in shaping protective behaviors: insights from the early phase of COVID-19 Italian Outbreak. Front Psychol. 2020;11(2958):563426. doi: 10.3389/fpsyg.2020.563426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gollust SE, Nagler RH, Fowler EF. The Emergence of COVID-19 in the US: a public health and political communication crisis. J Health Polit Policy Law. 2020;45(6):967–981. doi: 10.1215/03616878-8641506. [DOI] [PubMed] [Google Scholar]
- 4.Bavel JJV, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behav. 2020;4(5):460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- 5.Santarpia JL, Rivera DN, Herrera VL, et al. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci Rep. 2020;10(1):12732. doi: 10.1038/s41598-020-69286-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fowler EF, Gollust SE. The content and effect of politicized health controversies. Ann Am Acad Pol Soc Sci. 2015;658(1):155–171. [Google Scholar]
- 7.Bursztyn L, Rao A, Roth C, Yanagizawa‐Drott D. Misinformation during a pandemic. University of Chicago, Becker Friedman Institute for Economics Working Paper No. 2020‐44.
- 8.Morawska L, Milton DK. It is time to address airborne transmission of coronavirus disease 2019 (COVID-19) Clin Infect Dis. 2020;71(9):2311–2313. doi: 10.1093/cid/ciaa939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morawska L, Tang JW, Bahnfleth W, et al. How can airborne transmission of COVID-19 indoors be minimised? Environ Int. 2020;142 doi: 10.1016/j.envint.2020.105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aven T, Bouder F. The COVID-19 pandemic: how can risk science help? J Risk Res. 2020;23(7-8):849–854. [Google Scholar]
- 11.Cordner A, Brown P. Moments of uncertainty: ethical considerations and emerging contaminants. Sociol Forum (Randolph N J) 2013;28(3):469–494. doi: 10.1111/socf.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kutscher E, Greene RE. A harm-reduction approach to coronavirus disease 2019 (COVID-19)—safer socializing. JAMA Health Forum. 2020;1(6) doi: 10.1001/jamahealthforum.2020.0656. [DOI] [PubMed] [Google Scholar]
- 13.(PCSBI) PCftSoBI . PCSBI; Washington, DC: 2015. Ethics and Ebola: Public Health Planning and Response. [Google Scholar]
- 14.Duong HT, Nguyen HT, McFarlane SJ, Nguyen LTV. Risk perception and COVID-19 preventive behaviors: application of the integrative model of behavioral prediction. Soc Sci J. 2021:1–14. [Google Scholar]
- 15.Mevorach T, Cohen J, Apter A. Keep calm and stay safe: the relationship between anxiety and other psychological factors, media exposure and compliance with COVID-19 regulations. Int J Environ Res Public Health. 2021;18(6) doi: 10.3390/ijerph18062852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO. WHO Guidelines Approved by the Guidelines Review Committee . Vol. 2017. World Health Organization © World Health Organization; Geneva: 2017. (Communicating Risk in Public Health Emergencies: A WHO Guideline for Emergency Risk Communication (ERC) Policy and Practice). [PubMed] [Google Scholar]
- 17.Balog-Way DHP, McComas KA. COVID-19: reflections on trust, tradeoffs, and preparedness. J Risk Res. 2020;23(7-8):838–848. [Google Scholar]
- 18.Michelle Driedger S, Maier R, Jardine C. Damned if you do, and damned if you don't’: communicating about uncertainty and evolving science during the H1N1 influenza pandemic. J Risk Res. 2018:1–19. [Google Scholar]
- 19.Gustafson A, Rice RE. A review of the effects of uncertainty in public science communication. Public Understand Sci. 2020;29(6):614–633. doi: 10.1177/0963662520942122. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC). Crisis plus emergency risk communication manual, Chapter 1.