Summary
Background
Cirrhosis is a public health threat associated with high mortality. Alcoholic Liver Disease (ALD) is the leading cause in Latin America and Metabolic Associated Fatty Liver Disease (MAFLD) in western countries. In Mexico, ALD and chronic Hepatitis C Virus infection (HCV) were the most frequent aetiologies during the past decades. We aimed to describe the trends in the aetiologies of cirrhosis in a middle-income country.
Methods
We performed a retrospective cohort study including patients diagnosed with cirrhosis between 2000 and 2019 from six different tertiary care hospitals in central Mexico. We collected information regarding cirrhosis etiology, year of diagnosis, hepatocellular carcinoma development, liver transplantation, and death. We illustrated the change in the tendencies of cirrhosis aetiologies by displaying the proportional incidence of each etiology over time stratified by age and gender, and we compared these proportions over time using chi square tests.
Findings
Overall, 4,584 patients were included. In 2019, MAFLD was the most frequent cirrhosis etiology (30%), followed by ALD (24%) and HCV (23%). During the study period, MAFLD became the leading etiology, ALD remained second, and HCV passed from first to fourth. When analysed by gender, ALD was the leading etiology for men and MAFLD for women. The annual incidence of HCC was 3·84 cases/100 persons-year, the median survival after diagnosis was 12·1 years, and seven percent underwent LT.
Interpretation
Increased alcohol consumption and the obesity epidemic have caused a transition in the aetiologies of cirrhosis in Mexico. Public health policies must be tailored accordingly to mitigate the burden of alcohol and metabolic conditions in developing countries.
Funding
None.
Keywords: Cirrhosis, MAFLD, Hepatocellular carcinoma, Hepatitis C Virus, Alcohol liver disease, Liver transplantation
Research in Context.
Evidence before this study
Cirrhosis is a public health threat that leads to high costs and deaths. Hepatitis C Virus related policies directed at screening, prevention, and granting universal access to direct-acting antivirals, along with a rising prevalence of chronic metabolic diseases, have shifted the aetiologies of cirrhosis worldwide from infectious to metabolic conditions in high-income countries. Previous reports suggest this change will also occur in developing countries; however, it has not been confirmed yet.
Added value of this study
This is the largest cohort study in Latin America that evaluates the changing trends in the aetiologies of cirrhosis over the past 20 years in Mexican patients. MAFLD has become the leading cause of cirrhosis, ALD remains an important cause, and cases secondary to HCV infection have decreased dramatically. Like developed countries, the primary driver to this epidemiological shift seems to be a rise in the prevalence of metabolic syndrome and its components.
Implication of all the available evidence
The most common causes of cirrhosis in developing countries are preventable. Therefore, an accurate description of the different aetiologies is required to tailor public health policies to mitigate their burden. Screening, early diagnosis, and treatment of metabolic comorbidities might prevent patients from developing MAFLD and progressing to inflammation, fibrosis, and cirrhosis. Developing strategies to reduce alcohol consumption is also critical, as it remains a frequent cause of cirrhosis. Finally, because liver transplantation remains the only effective treatment for cirrhosis, healthcare policies that guarantee better access to these procedures in developing countries are also required.
Alt-text: Unlabelled box
Introduction
Cirrhosis is the final pathological stage of various chronic liver diseases. It is a public health threat causing over 1 million deaths per year worldwide and around 1·5 million years of potential life lost in the US, a high burden of premature deaths.1,2 The most common aetiologies are hepatitis B virus (HBV), hepatitis C virus (HCV), alcohol-related liver disease (ALD), and metabolic-associated fatty liver disease (MAFLD).3 Alcohol is the leading cause of cirrhosis in Latin America and Africa, while the prevalence of MAFLD is increasing in western countries.3, 4, 5
The discovery of direct-acting antivirals (DAA) and the implementation of current HBV vaccination policies have shifted the epidemiology of cirrhosis worldwide.3 HCV has become less prevalent in high-income countries and it is expected to drop even further as the access to treatment increases.6 However, the true extent of the problem remains unknown in many parts of the globe, as there are no strategies to prevent and diagnose liver disease.4 Healthcare systems need to accurately assess the causes of cirrhosis to elaborate public health policies to reduce their burden, as most of the cases are preventable.
In Mexico, ALD and HCV were the most frequent causes of cirrhosis during the past decade.7 The rise and awareness in metabolic and autoimmune diseases, along with more widespread use of HCV targeted therapies might be causing similar shifts to those seen in high-income countries.4,7
We aimed to describe the changes in the trends of cirrhosis aetiologies over the past 20 years in Mexico, by retrieving information from six hospitals in central Mexico (Mexico City and State of Mexico), as well as hepatocellular carcinoma prevalence by aetiology, frequency of liver transplantation, and overall mortality.
We consider that an accurate assessment is vital to set clinical, research, and policy-making priorities to face this public health threat.
Methods
Study design and patient data
A retrospective, multicenter, cohort study was performed including patients diagnosed with cirrhosis between 2000 and 2019 from six hospitals in the metropolitan area of Mexico (Mexico City and State of Mexico). Information was retrieved from clinical charts and analysed by the coordinating centre. The six hospitals included were: Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (Centre A, Mexico City), Hospital General Dr Manuel Gea González (Centre B, Mexico City), Instituto de Seguridad Social del Estado de México y Municipios (Centre C, State of Mexico), Hospital General de México (Centre D, Mexico City), Centro Médico Nacional La Raza (Centre E, Mexico City), and Centro Médico Lic. Adolfo López Mateos (Centre F, Mexico City). Of these, Centres A, D, and E are currently considered active performing liver transplant centres, and Centres A and D are considered national reference hospitals.
Included patients were adults aged 18 years or older, diagnosed with liver cirrhosis by conventional methods (medical history, liver biochemistry, imaging and/or endoscopy when appropriate) and with an identifiable aetiology according to clinical records. ICD-10 codes were used to identify cirrhosis, hepatocellular carcinoma, and liver transplantation. Patients were excluded if they were younger than 18 years old at the time of diagnosis or if their information regarding gender was unavailable.
For each patient, we collected: age at diagnosis, gender, cirrhosis aetiology, year of diagnosis, Child-Pugh score and prior decompensations, development of hepatocellular carcinoma, time to liver transplantation, time to death, and time of follow-up. Aetiology was retrieved according to clinical charts and categorized according to ICD-10 codes as follows: Alcoholic liver disease (ALD), chronic hepatitis C virus infection (HCV), and autoimmune diseases (autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis and overlap syndromes). Other aetiologies included less prevalent causes of cirrhosis such as (but not limited to) alpha-1 antitrypsin deficiency (A1AD), Wilson's disease, hereditary hemochromatosis, chronic hepatitis B infection. MAFLD was considered as the aetiology according to previously published consensus:8 Patients must have had any history of liver steatosis prior or at the time of cirrhosis diagnosis, and meet any of the ATP-III criteria: overweight or obesity (BMI 25 kg/m2 or higher); type 2 Diabetes Mellitus; or at least two metabolic abnormalities (waist circumference >102 cm for men, > 88 cm for women, blood pressure > 130/85 mmHg, triglycerides >150 mg/dL, HDL <40 mg/dL for men and <50 mg/dL for women, prediabetes, HOMA index >2·5). Following the MAFLD consensus, patients previously diagnosed with “cryptogenic aetiology” were considered under the MAFLD umbrella. Hepatocellular carcinoma (HCC) was considered present or absent according to clinical charts, and exact dates of diagnosis could not be retrieved.
The protocol was approved by the institutional review board at each participating centre.
Statistics
Categorical variables are summarized in frequency and percentages and numerical variables in mean and standard deviation or median and interquartile range as appropriate. Baseline characteristics are compared by gender using a Pearson chi-square test if categorical or using a t-test that allows for heteroscedasticity if numerical.
To illustrate the change in the tendencies of cirrhosis aetiologies over time we displayed the proportional incidence of each aetiology over time stratified by age group (< 45 years, 46 – 59 years, and > 60 years) and gender, and we compare these proportions over time using chi-square tests.
The mean annual incidence of HCC is estimated overall, within aetiology groups and by gender. Since the exact time of HCC diagnosis was not recorded in the dataset, we considered that each patient who developed HCC stayed at risk during half of his/her follow-up time. For the same reason, we did not compare these mean annual incidences by subgroups.
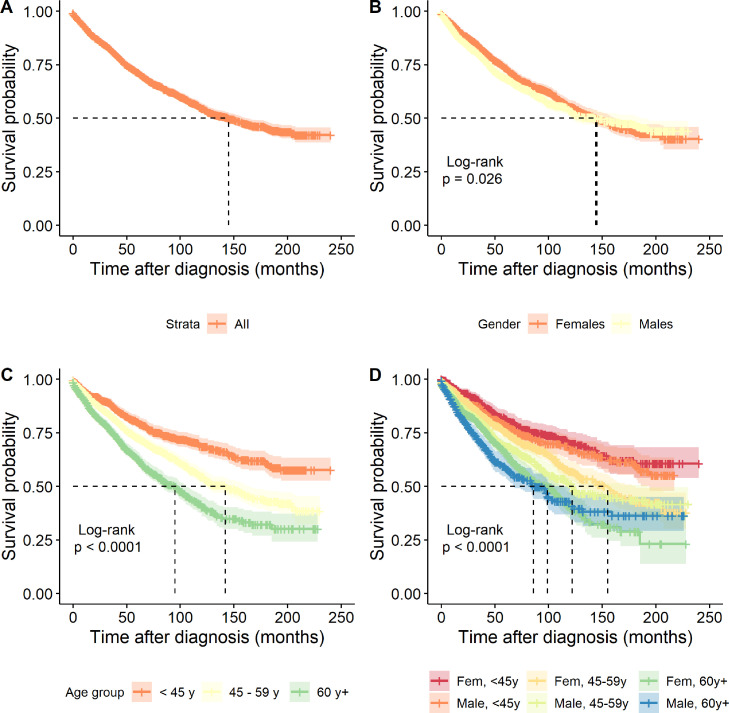
The survival after diagnosis was estimated using the Kaplan-Meier method and was compared by gender and by age groups using the log-rank test.
The statistical analysis was performed using R version 4·0·2.
Role of the funding source
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sector.
Results
Cohort construction
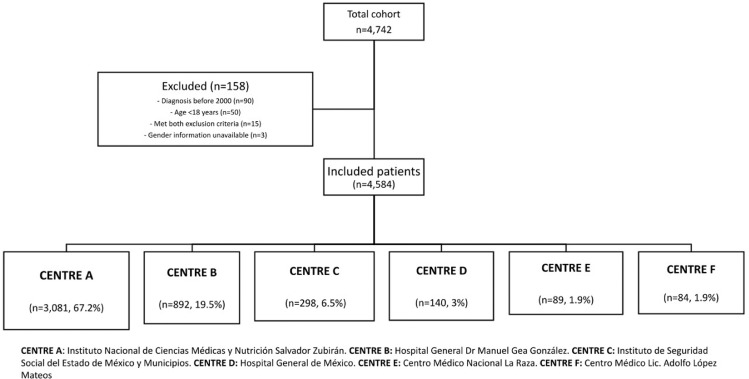
A total of 4742 patients were retrieved from the hospital records, from whom 158 were excluded, leaving a final cohort of 4584 patients. Two hospitals from Mexico City contributed to 86% of the cohort. Centre A, a national reference hospital, contributed two-thirds of the cohort (3081 patients). Centre B, a secondary care hospital, contributed a fifth of the cohort (892 patients). The general flowchart of this cohort is shown in Fig. 1. The specific contributions of each hospital in the entire cohort, according to age, gender, and aetiology of the patients are shown in Fig. S1 and Table S1.
Figure 1.
Flowchart of the present cohort. CENTRE A: Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán. CENTRE B: Hospital General Dr Manuel Gea González. CENTRE C: Instituto de Seguridad Social del Estado de México y Municipios. CENTRE D: Hospital General de México. CENTRE E: Centro Médico Nacional La Raza. CENTRE F: Centro Médico Lic. Adolfo López Mateos.
Baseline characteristics
Baseline characteristics of the cohort are presented in Table 1. The average age was 53 years (SD 13 years) and 55% were female (n = 2560). Overall, MAFLD/Cryptogenic was the most common aetiology (30%) followed by ALD (24%) and HCV (23%). By the time of diagnosis, 77% had at least one prior episode of decompensation, and the mean Child-Pugh score was 7 points (IQR 6–9).
Table 1.
Baseline features and outcomes overall and by gender.
| Feature | n | Overall (n = 4584) | Females (n = 2560) | Males (n = 2024) | P-value† |
|---|---|---|---|---|---|
| Age (years), mean (SD) | 4584 | 53 (13) | 54 (13) | 52 (13) | <0.001 |
| Centre, n (%) | 4584 | ||||
| A | 3081 (67%) | 1751 (68%) | 1330 (66%) | < 0.001 | |
| B | 892 (19%) | 406 (16%) | 486 (24%) | ||
| C | 298 (6·6%) | 194 (7·6%) | 104 (5·1%) | ||
| D | 140 (3·1%) | 91 (3·6%) | 49 (2·4%) | ||
| E | 89 (1·9%) | 60 (2·3%) | 29 (1·4%) | ||
| F | 84 (1·8%) | 58 (2·3%) | 26 (1·3%) | ||
| Cirrhosis aetiology, n (%) | 4584 | ||||
| MAFLD/Cryptogenic | 1373 (30%) | 839 (33%) | 534 (26%) | <0.001 | |
| Alcohol | 1110 (24%) | 294 (11%) | 816 (40%) | ||
| Hepatitis C Virus | 1058 (23%) | 664 (26%) | 394 (19%) | ||
| Autoimmunity | 787 (17%) | 640 (25%) | 147 (7·3%) | ||
| Other | 256 (5·6%) | 123 (4·8%) | 133 (6·6%) | ||
| Child-Pugh score at diagnosis, median (range) | 4583 | 7 (6, 9) | 7 (6, 8) | 8 (6, 9) | <0.001 |
| Prior decompensations, n (%) | 4525 | 3473 (77%) | 1855 (74%) | 1618 (81%) | <0.001 |
| Outcomes | |||||
| Follow-up (months), median (IQR) | 4584 | 38 (14, 77) | 42 (17, 82) | 33 (12, 72) | <0.001 |
| Hepatocellular carcinoma, n (%) | 3155 | 547 (17%) | 282 (16%) | 265 (19%) | 0.018 |
| Liver transplant, n (%) | 4584 | 340 (7·4%) | 169 (6·6%) | 171 (8·4%) | 0.018 |
| Death, n (%) | 4584 | 1290 (28%) | 718 (28%) | 572 (28%) | 0.9 |
MAFLD: Metabolic Associated Fatty Liver Disease; CENTRE A: Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán; CENTRE B: Hospital General Dr Manuel Gea González; CENTRE C: Instituto de Seguridad Social del Estado de México y Municipios; CENTRE D: Hospital General de México; CENTRE E: Centro Médico Nacional La Raza; CENTRE F: Centro Médico Lic. Adolfo López Mateos.
†t-test or Pearson's chi-squared test.
Aetiologies transition
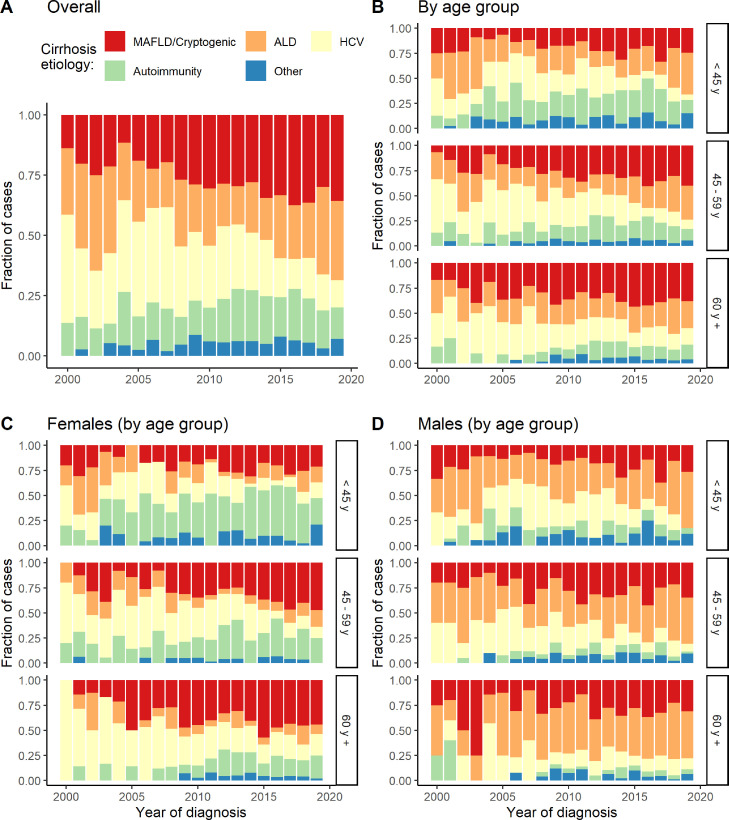
The cirrhosis aetiology trends from 2000 to 2019 are summarized in Fig. 2A. MAFLD passed from being the third cause of cirrhosis, responsible for 14% of incident cases in 2000, to becoming the leading cause since 2012, responsible for 36% of incident cases in 2019. On the other hand, HCV passed from being the leading cause of cirrhosis in 2000, responsible for 45% of incident cases, to becoming the fourth cause since 2016, responsible for 11% of incident cases in 2019.
Figure 2.
Proportional incidence of cirrhosis aetiology over time. A. Overall; B. By age groups; C. Females by age groups; D. Males by age groups.
ALD: Alcoholic Liver Disease; HCV: Hepatitis C Virus; MAFLD: Metabolic Associated Fatty Liver Disease. Other: hepatitis B virus, secondary biliary cirrhosis, hemochromatosis, metabolic (alpha-1 antitrypsin deficiency, Wilson Disease), cardiac cirrhosis, porphyria, congenital hepatic fibrosis, biliary atresia, Budd-Chiari syndrome, Caroli disease, Von Meyenburg disease, lysosomal acid lipase deficiency.
ALD was the second cause of cirrhosis in 2000, responsible for 28% of incident cases, and passed to be the third or fourth cause between 2006 and 2017 and returned to be the second leading cause in 2019, responsible for 33% of incident cases. During the entire follow-up, autoimmunity fluctuated between being the third or fourth cause of cirrhosis, responsible for 16% of incident cases per year, on average. All these changes in the cirrhosis aetiologies over time were statistically significant (see Table 2).
Table 2.
P values for comparing the cirrhosis aetiology distribution over time overall, by gender, by age group, and by combinations of them.
| Gender/Age group | < 45 y | 46 – 59 y | 60 y + | Overall |
|---|---|---|---|---|
| Females | < 0.001 | < 0.001 | 0.001 | < 0.001 |
| Males | 0.004 | 0.008 | 0.402 | < 0.001 |
| Overall | < 0.001 | < 0.001 | 0.002 | < 0.001 |
Cirrhosis aetiologies by age groups
The transition of cirrhosis aetiologies by age group is shown in Fig. 2B. It is worth noting that HCV was the leading cause of cirrhosis in 2000 amongst the three age groups (37·5% in <45 years, 53·3% in 45–59 years, and 33·3% in >60 years) but continuously declined during the entire period until 2019, reaching 5·7% in <45 years, 9·1% in 45–59 years and 16·5% in >60 years. Moreover, MAFLD has shown a continuous rise in its frequency, particularly in patients older than 45 years. ALD remained steady during the study period for those older than 45 years, but it became the most common aetiology in 2019 for those younger than 45 years (41·5%). Autoimmunity has remained as a frequent aetiology (second or third) in patients younger than 45 years, and third in the 45–59 years group. These changes in the aetiologies trends over time were also statistically significant (see Table 2).
Cirrhosis aetiologies by gender
Differences in aetiologies by gender, stratified by age group, are shown in Fig. 2C and D. MAFLD has become the leading aetiology of cirrhosis in women (responsible for 6% of incident cases in 2000 and 41% in 2019) and the second cause of cirrhosis in men (responsible for 25% of incident cases in 2000 and 31% in 2019). On the other side, ALD has become more common in men (responsible for 42% of incident cases in 2000 and 49% in 2019) and less common in women (responsible for 18% in 2000 and 13% in 2019). ALD has been the leading cause of cirrhosis in men during the entire period from 2000 to 2019.
HCV passed from being the leading cause of cirrhosis for both genders in 2000, responsible for 59% of the incident cases in women and 25% in men, to become the third cause in 2019, responsible for 17% in women and 7% in men. Despite that the autoimmunity trend has remained steady when analysing the entire cohort, it has behaved differently by gender. In men, autoimmunity represented 8% of incident cases in 2000 and 4% in 2019. Conversely, for women, this aetiology was responsible for 18% of cases in 2000 and 24% in 2019, becoming the second leading cause of cirrhosis since 2011. Except for 60-year-old men or older, all these changes in the cirrhosis aetiologies over time were statistically significant (see Table 2).
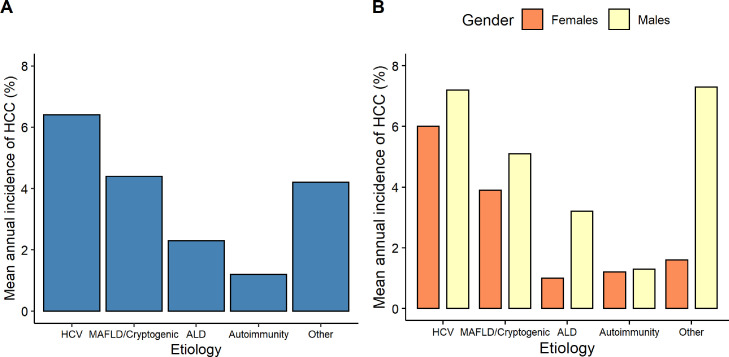
Hepatocellular carcinoma
Information was available in 3155 patients from whom 17% (n = 547) developed HCC with an approximate mean time at risk of 4.51 years, leading to an approximate mean annual incidence of 3·84% (3·84 incident cases/100 person-year) in our cohort. In patients who developed HCC, HCV was the leading aetiology of cirrhosis (mean annual incidence 6·4%), followed by MAFLD/Cryptogenic and ALD (mean annual incidences of 4·4% and 2·3%, respectively).
The mean annual incidence of HCC was distinct when compared by gender and cirrhosis aetiologies. In the female population, HCV was the most common aetiology of cirrhosis that led to HCC, followed by MALFD/Cryptogenic and ALD (mean annual incidence of 6·0%, 3·9%, and 1·0%, respectively). Conversely, for the male population, the other aetiologies group was the most commonly associated with HCC, followed by HCV and MAFLD/Cryptogenic (mean annual incidence of 7·3%, 7·2%, and 5·1% respectively). Fig. 3 summarizes the mean annual incidences of the entire cohort and divided by gender.
Figure 3.
Mean annual incidence of Hepatocellular carcinoma according to cirrhosis aetiology. A. Overall. B. By gender.
ALD: Alcoholic Liver Disease; HCV: Hepatitis C Virus; MAFLD: Metabolic Associated Fatty Liver Disease. Other: hepatitis B virus, secondary biliary cirrhosis, hemochromatosis, metabolic (alpha-1 antitrypsin deficiency, Wilson Disease), cardiac cirrhosis, porphyria, congenital hepatic fibrosis, biliary atresia, Budd-Chiari syndrome, Caroli disease, Von Meyenburg disease, lysosomal acid lipase deficiency.
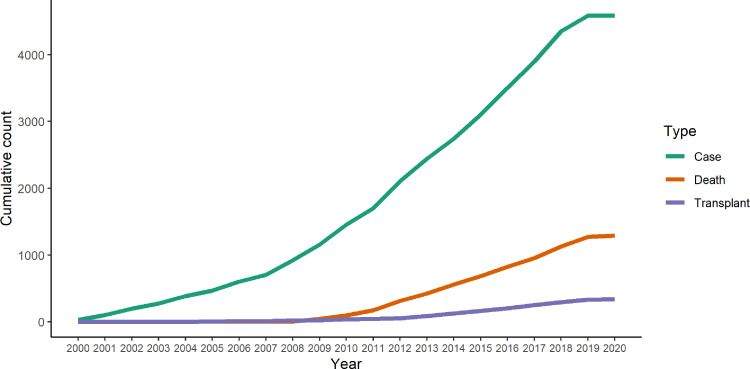
Liver transplantation (LT) incidence and mortality
During follow-up 340 patients (7·4%) underwent LT, 169 women and 171 men, and 1290 (28%) died, 718 women and 572 men (Table 1). Data regarding LT and death are summarized in Fig. 4.
Figure 4.
Cumulative liver transplantation and death in our cohort.
The median survival after diagnosis for the overall population was 12·1 years, 95% CI 10·8 - 13·4 (Fig. 5A), and it was higher for males (12 years, 95% CI 10.0 - 15.5) compared with females (12·08 years, 95% CI 10·7 – 13·4) (p = 0·026) (Fig. 5B). The survival probability was significantly higher in the <45 years group (median survival not reached) when compared to the 45–59 years and ≥60 years groups (median survival of 11·8 years, 95% CI 10·2 – 13·5 and 7·91 years, 95% CI 6·91 – 8·57, respectively) (p < 0·0001) (Fig. 5C). The overall survival according to gender and the three different age categories is shown in Fig. 5D.
Figure 5.
Survival probability after diagnosis of cirrhosis in the present cohort. A. Overall; B. By gender; C. By age groups; D. Stratified by gender and age groups.
Discussion
This study illustrates the impact of metabolic conditions in the trends of cirrhosis aetiologies in the last two decades. To our knowledge, this is the largest cohort of patients diagnosed with cirrhosis from Latin America. Similar to developed countries,9 MAFLD has become the leading cause of cirrhosis; ALD has remained, on average, the second most common cause; HCV has steadily declined over the last decade, and autoimmune aetiologies have slightly increased in women. These findings are different from those reported by Mendez-Sanchez et al. in a cohort of 1210 patients in Mexico City during January 2012 and December 201;77 they found HCV and ALD as the leading causes of cirrhosis and an increasing trend in the cases of MAFLD.
The prevalence of obesity has increased in Mexico during the last decades. The National Health and Nutrition Examination Surveys carried out in 2000 (ENSA 2000) and 2018–19 (ENSANUT 2018–19) showed that the prevalence of obesity increased from 25% in 2000 to 36% in 2019, and the prevalence of morbid obesity from 2% to 4%.10,11 Furthermore, a National Survey in 2003 estimated that metabolic syndrome affects one-fifth of the population and a 2018 meta-analysis estimates that this has risen to 36% according to the ATP-III criteria.12,13 This is problematic as one-third of patients with MAFLD will progress to a more active disease, of whom 10–15% will progress to cirrhosis.14,15 Studies in the Mexican population showed that 17% of patients with steatohepatitis will develop cirrhosis.16 This supports our findings; the increase in metabolic comorbidities over the last decades might have been the main driver of the transition in the leading cirrhosis aetiology. Besides metabolic syndrome; cultural, socioeconomic, dietary and exercise habits, and genetics also play a role in the development and progression of this disease. Patatin-like phospholipase domain-containing protein 3 (PNPLA3) gene polymorphisms have been associated with MAFLD severity and prognosis, and Genome-wide association studies have confirmed this association in Mexican-American populations.17 Previous information from the Mexican population has shown an overall frequency of 77% for a MAFLD-risk allele.18 Despite the burden it represents to global health systems, little progress has been done in the public health response.19 A recent survey conducted in Mexican gastroenterology fellows revealed that 22% of them are unaware of the global prevalence of MAFLD and 29% do not believe it is a potentially severe disease.20 Public health policies to raise awareness and to prevent MAFLD progression with proper screening as well as strategies to improve lifestyle in the population are required.
ALD is the leading cause of liver-related deaths in Asia, Eastern Europe, and Latin America, and might cause up to 30% of the cases of HCC in countries with high consumption of alcohol.21,22 The National Survey on Drug, Alcohol, and Tobacco Use reported that daily alcohol consumption in adolescents and adults increased from 0·8% to 2·9%, in 2011 and 2016, respectively.23 This may explain the growing proportion of ALD-related cirrhosis cases we observed. Despite the increasing prevalence of alcohol consumption, alcohol use disorders remain underdiagnosed and undertreated. Effective pharmacological and psychosocial interventions, as well as proven policies, might reduce this burden.24
HCV remains one of the leading causes of cirrhosis and HCC, causing over 400,000 liver-related deaths in 2015.3 However, the advent of DAAs has turned this infection curable, reducing the prevalence and complications of HCV worldwide.25,26 An European model projects that cured patients will exceed the viremic patients in number by 2021.6 In our cohort, HCV cases began to decline before the introduction of DAAs, with a higher reduction after the approval of these treatments in 2015. Our findings are in accordance with other Liver Units worldwide,9,25 In 2015, the prevalence of HCV in Mexico was estimated to be 0·4%, and if the current trend continues, HCV will no longer be one of the primary causes of cirrhosis.27 Despite the optimism, several factors challenge the eradication of HCV: treatment access is limited due to its high cost, and many patients remain undiagnosed with a latent risk of liver fibrosis that otherwise could be reversible.6,28 To reduce the morbidity and mortality secondary to HCV, governments must develop screening programs and improve access to treatment.
The incidence of HCC has risen in the last decades and nowadays constitutes the fourth leading cause of death by cancer worldwide, and the fifth and ninth most diagnosed cancer in men and women, respectively.29 In Mexico, liver cancer is the fourth cause of death by cancer, and the eighth-most diagnosed cancer in men and women.29 Despite that HCV and ALD remain the leading causes of HCC, cases attributable to MAFLD are increasing.30 HCV is the main aetiology associated with HCC in our patients, followed by MAFLD and ALD. Following the trend we observed for cirrhosis, we anticipate the causes of HCC will shift to metabolic conditions in the near future.
Even though liver diseases represent the fifth cause of death in Mexican adults and the second cause in the economically active population, Mexico only performs between 150 and 240 LT per year, one of the lowest numbers of LT per million in Latin America.31,32 In our cohort, only 7·4% (n = 340) underwent LT, and 3·8 patients died for every patient who received a transplant during a period of 20 years. As of April 23, 2020, 328 patients are on the waiting list for a LT in Mexico.30 This contrasts with developing countries; for example, in the US, 10,500 patients are added to the waiting list and 6800 transplants are performed per year, on average.30 The Centro Nacional de Trasplante in Mexico has 84 approved centres for liver transplantation in Mexico. Still, only 7 performed more than ten transplants per year in 2019.33 Our findings confirm that even in referral centres, the proportion of patients with end-stage liver disease undergoing transplantation remains dismally low. The latter could be explained by delayed diagnoses and patients not being evaluated in LT centres.
Despite being the largest cohort described in Latin America, this study has some limitations. First, because the information was collected from hospitals located in Central Mexico (Mexico City and State of Mexico), it does not constitute a representative sample of the Mexican population. However, it might be a representative sample of the metropolitan area of Mexico City and nearby States since the participating hospitals are reference centres of all the existing public healthcare systems in Mexico. Second, we grouped MAFLD and cryptogenic cirrhosis into the same category, which could overestimate the cases of MAFLD; however, MAFLD has been previously recognized as the most common cause of cryptogenic cirrhosis. Third, because of the retrospective nature of our study, we had to rely on the information available on the records; however, it is the largest cohort described in a developing country. Finally, the provided mean annual incidences of HCC are not accurate since we did not record the exact time of diagnosis in those who developed HCC, however, we consider that these values are good approximations and can be used to make comparisons with other studies.
Conclusion
Similar to other countries, Mexico is facing a transition in the aetiology of cirrhosis mainly driven by an increase in metabolic conditions and the advent of direct-acting antivirals. During the last two decades, MAFLD passed from third to first place as leading causes of cirrhosis. HCV aetiology passed from first to fourth place, while ALD remained the second cause. Although all these causes are preventable, little progress has been made in our country. Appropriate knowledge of the current trends in cirrhosis aetiologies can guide researchers, policymakers, and clinicians towards reducing the burden of liver diseases.
Acknowledgments
Contributors
Conceptualization AG-Ch, IG-J, AG-Ch, AO-M. Data Collection LCCh-G, OJ-L, JC-G, JDD-G, MSG-H, GM-L, VMP-Z, MC-B, OJC-Q, FIG-J, JAR-L, LT-Y, JFS-A, JAA-R, AB-S, MD-H, AKV-V. Writing – Original Draft JR-M, MS-R. Writing – Review & Editing AO-M, MSG-H, LT-Y, JAA-R, IR. Formal Analysis AO-M. Verified Underlying Data AO-M, IG-J. Supervision IG-J.
Funding
None.
Data sharing statement
A de-identified dataset is available from the corresponding author upon reasonable request.
Declaration of interests
The authors have no conflict of interest to disclose.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2021.100151.
Appendix. Supplementary materials
References
- 1.Asrani S.K., Devarbhavi H., Eaton J., Kamath P.S. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151–171. doi: 10.1016/j.jhep.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 2.Paik J.M., Golabi P., Biswas R., Alqahtani S., Venkatesan C., Younossi Z.M. Nonalcoholic fatty liver disease and alcoholic liver disease are major drivers of liver mortality in the United States. Hepatol Commun. 2020;4(6):890–903. doi: 10.1002/hep4.1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moon A.M., Singal A.G., Tapper E.B. Contemporary epidemiology of chronic liver disease and cirrhosis. Clin Gastroenterol Hepatol. 2020;18(12):2650–2666. doi: 10.1016/j.cgh.2019.07.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marcellin P., Kutala B.K. Liver diseases: a major, neglected global public health problem requiring urgent actions and large-scale screening. Liver Int. 2018;38:2–6. doi: 10.1111/liv.13682. December 2017. [DOI] [PubMed] [Google Scholar]
- 5.Stein E., Cruz-Lemini M., Altamirano J., et al. Heavy daily alcohol intake at the population level predicts the weight of alcohol in cirrhosis burden worldwide. J Hepatol. 2016;65(5):998–1005. doi: 10.1016/j.jhep.2016.06.018. [DOI] [PubMed] [Google Scholar]
- 6.Chen Q., Ayer T., Bethea E., et al. Changes in hepatitis C burden and treatment trends in Europe during the era of direct-acting antivirals: a modelling study. BMJ Open. 2019;9(6):1–11. doi: 10.1136/bmjopen-2018-026726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Méndez-Sánchez N., Zamarripa-Dorsey F., Panduro A., et al. Current trends of liver cirrhosis in Mexico: similitudes and differences with other world regions. World J Clin Cases. 2018;6(15):922–930. doi: 10.12998/wjcc.v6.i15.922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eslam M., Sanyal A.J., George J. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020 doi: 10.1053/j.gastro.2019.11.312. Published online. [DOI] [PubMed] [Google Scholar]
- 9.Wong R.J., Singal A.K. Trends in liver disease etiology among adults awaiting liver transplantation in the United States, 2014-2019. JAMA Netw open. 2020;3(2) doi: 10.1001/jamanetworkopen.2019.20294. [DOI] [PubMed] [Google Scholar]
- 10.Barquera S., Hernández-barrera L., Trejo-valdivia B. Obesidad en México, prevalencia y tendencias en adultos. Ensanut. 2020;62(6) doi: 10.21149/11630. 2018-19. [DOI] [PubMed] [Google Scholar]
- 11.Olaiz G., Rojas R., Barquera S., et al. Encuesta Nacional de Salud. Tomo 2. La salud de los adultos. Instituto Nacional de Salud Pública; Cuernavaca, Morelos, Mexico: 2003. [Google Scholar]
- 12.Aguilar-Salinas C.A., Rojas R., Gómez-Pérez F.J., et al. High prevalence of metabolic syndrome in Mexico. Arch Med Res. 2004;35(1):76–81. doi: 10.1016/j.arcmed.2003.06.006. [DOI] [PubMed] [Google Scholar]
- 13.Gutiérrez-Solis A.L., Datta Banik S., Méndez-González R.M. Prevalence of metabolic syndrome in mexico: a systematic review and meta-analysis. Metab Syndr Relat Disord. 2018;16(8):395–405. doi: 10.1089/met.2017.0157. [DOI] [PubMed] [Google Scholar]
- 14.Araújo A.R., Rosso N., Bedogni G., Tiribelli C., Bellentani S. Global epidemiology of non-alcoholic fatty liver disease/non-alcoholic steatohepatitis: what we need in the future. Liver Int. 2018;38:47–51. doi: 10.1111/liv.13643. November 2017. [DOI] [PubMed] [Google Scholar]
- 15.Divella R., Mazzocca A., Daniele A., Sabbà C., P. A. Obesity, Nonalcoholic fatty liver disease and adipocytokines network in promotion of cancer. 2019;15. 10.7150/ijbs.29599 [DOI] [PMC free article] [PubMed]
- 16.Bernal-Reyes R., Castro-Narro G., Malé-Velázquez R., et al. The Mexican consensus on nonalcoholic fatty liver disease. Rev Gastroenterol Mex. 2019;84(1):69–99. doi: 10.1016/j.rgmx.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 17.Young K.A., Xiang A.H. Genome-wide association study identifies loci for liver enzyme concentrations in Mexican Americans : the GUARDIAN consortium. 2019;00(00):1–7. 10.1002/oby.22527 [DOI] [PMC free article] [PubMed]
- 18.Martínez L.A., Larrieta E., Calva J.J., Kershenobich D., Torre A. The expression of PNPLA3 polymorphism could be the key for severe liver disease in NAFLD in hispanic population. Ann Hepatol. 2019;16(6):909–915. doi: 10.5604/01.3001.0010.5282. [DOI] [PubMed] [Google Scholar]
- 19.Lazarus J.V., Colombo M., Cortez-Pinto H., et al. NAFLD – sounding the alarm on a silent epidemic. Nat Rev Gastroenterol Hepatol. 2020;17(7):377–379. doi: 10.1038/s41575-020-0315-7. [DOI] [PubMed] [Google Scholar]
- 20.Mendez-Sanchez N., Diaz-Orozco L., Cordova-Gallardo J. Redefinition of fatty liver disease from NAFLD to MAFLD raised disease awareness: mexican experience. J Hepatol. 2021 doi: 10.1016/j.jhep.2021.04.021. Published online. [DOI] [PubMed] [Google Scholar]
- 21.Sepanlou S.G., Safiri S., Bisignano C., et al. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Gastroenterol Hepatol. 2020;5(3):245–266. doi: 10.1016/S2468-1253(19)30349-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ganne-carrié N., Nahon P. Hepatocellular carcinoma in the setting of alcohol-related liver disease. 2019;70. 10.1016/j.jhep.2018.10.008 [DOI] [PubMed]
- 23.Escobar E.R., Gamiño M.N.B., Salazar R.M., et al. National trends in alcohol consumption in Mexico: results of the national survey on drug, alcohol and tobacco consumption 2016-2017. Salud Ment. 2018;41(1):7–16. doi: 10.17711/SM.0185-3325.2018.003. [DOI] [Google Scholar]
- 24.Carvalho A.F., Heilig M., Perez A., Probst C., Rehm J. Alcohol use disorders. Lancet. 2019;394(10200):781–792. doi: 10.1016/S0140-6736(19)31775-1. [DOI] [PubMed] [Google Scholar]
- 25.Crespo J., Cuadrado A., Perelló C., et al. Epidemiology of hepatitis C virus infection in a country with universal access to direct-acting antiviral agents: data for designing a cost-effective elimination policy in Spain. J Viral Hepat. 2020;27(4):360–370. doi: 10.1111/jvh.13238. [DOI] [PubMed] [Google Scholar]
- 26.Park H., Wang W., Henry L., Nelson D.R. Impact of all-oral direct-acting antivirals on clinical and economic outcomes in patients with chronic hepatitis C in the United States. Hepatology. 2019;69(3):1032–1045. doi: 10.1002/hep.30303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blach S., Zeuzem S., Manns M., et al. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol. 2017;2(3):161–176. doi: 10.1016/S2468-1253(16)30181-9. [DOI] [PubMed] [Google Scholar]
- 28.Marciano S., Haddad L., Borzi S.M., et al. Access to direct-acting antivirals for the treatment of hepatitis C in a country with limited resources. Rev Gastroenterol Mex. 2018;83(2):208–211. doi: 10.1016/j.rgmx.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 29.Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F (2020). Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. Published 2020. Available from: https://gco.iarc.fr/today (accessed July 25, 2021).
- 30.Caines A., Selim R., Salgia R. The Changing Global Epidemiology of Hepatocellular Carcinoma. Clin Liver Dis. 2020;24(4):535–547. doi: 10.1016/j.cld.2020.06.001. [DOI] [PubMed] [Google Scholar]
- 31.INEGI Instituto Nacional de Estadística, Geografía e Informática. Características de las defunciones registradas en méxico durante enero a agosto de 2020. 2021. Available from: https://www.inegi.org.mx/contenidos/saladeprensa/boletines/2021/EstSociodemo/DefuncionesRegistradas2020_Pnles.pdf (accessed April 23, 2021).
- 32.CENATRA Centro Nacional de Trasplantes. Datos Abiertos. 2021. Available from: https://www.gob.mx/cenatra (accesed May 15, 2021).
- 33.Fayek S.A., Quintini C., Chavin K.D., Marsh C.L. The current state of liver transplantation in the united states: perspective from american society of transplant surgeons (ASTS) scientific studies committee and endorsed by ASTS council. Am J Transplant. 2016;16(11):3093–3104. doi: 10.1111/ajt.14017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.