Abstract
Endometrial cancer (EC) incidence is on the rise. Although early-onset endometrial cancer (EOEC; age at diagnosis <50 years) is relatively uncommon, the incidence of EOEC has been reportedly increasing in recent decades. However, the rising EOEC has not been thoroughly described with regard to the racial and ethnic disparities and compared with late-onset EC (age at diagnosis ≥50 years). We used the Cancer in North America (CiNA) Analytic File, 1995-2018, from the North American Association of Central Cancer Registries, which allowed us to examine trends in invasive EC incidence by racial and ethnic groups and by age at diagnosis. We found striking differences for demographic and tumor characteristics as well as racial and ethnic patterns and time trends in EC incidence between EOEC and late-onset EC. The faster increases in EOEC incidence rates, especially among non-White women, mirror similar observations in other cancers, pointing to a possible link with rising obesity epidemic in younger generations.
Endometrial cancer (EC) is the most common gynecologic cancer and the fourth-most common cancer among women in the United States (1). EC incidence is on the rise disproportionately among minority racial and ethnic groups (2,3). EC primarily affects postmenopausal women, and early-onset endometrial cancer (EOEC), diagnosed before age 50 years, is relatively uncommon (2018 incidence rates: 6.9/100 000) (4). Several studies have reported an increasing incidence of EC cases across all age groups in recent decades, including EOEC (5-7). However, no prior studies, to our knowledge, have compared characteristics and trends between EOEC and late-onset EC (LOEC; diagnosed at age ≥50 years) by race and ethnicity (8-10). Therefore, we conducted an analysis using a large representative dataset of the United States to provide a more detailed assessment of EOEC vs LOEC incidence trends by race and ethnicity across 2 decades.
We used the population-based Cancer in North America (CiNA) Public Use incidence dataset from the North American Association of Central Cancer Registries, which provides nearly complete coverage of all US states, to compare incidence rates and trends of EOEC and LOEC across multiple racial and ethnic populations among women during 1995-2018 (11,12). We identified 930 176 invasive EC cases based on the International Classification of Diseases for Oncology, Third Edition code C54.1 (endometrium), including all histology codes except 9050-9055, 9140, and 9590-9992, as defined by Surveillance, Epidemiology, and End Results (SEER) Site Recode (13) (Supplementary Figure 1, available online).
We examined the distribution of race and ethnicity (Hispanic, Non-Hispanic Asian/Pacific Islander, Non-Hispanic Black, Non-Hispanic White, and Other/Unknown [including Alaska Native, American Indian, other race, and unknown or missing race]) and tumor characteristics (stage at diagnosis, tumor grade, and histologic subtype [Supplementary Table 1, available online]) by EOEC or LOEC status. Race and ethnicity information was provided in the CiNA dataset based on information abstracted from patients’ medical charts, that may or may not be self-reported, as well as through application of the respective Asian/Pacific Islander and Hispanic identification algorithms developed by North American Association of Central Cancer Registries (14,15). There is no information on multiple races in the CiNA dataset we used.
We used SEER*Stat 8.3.9 software to calculate annual overall and race- and ethnicity-specific age-adjusted (2000 US standard population) incidence rates (AAIRs) per 100 000 population. The denominators used in calculating the AAIRs are provided in the CiNA dataset and are known as “SEER modified populations” (12,16). We used the Joinpoint Regression Program version 4.9.0.0 to calculate the average annual percent change (AAPC) of AAIRs for EOEC and LOEC for 1995-2018 to analyze the incidence trends. All statistical tests were 2-sided, and statistical significance was set at P < .05.
From 1995 to 2018, 930 176 invasive EC cases were diagnosed among US women, including 116 750 (12.6%) EOEC and 813 426 (87.4%) LOEC (Table 1). The overwhelming majority of EC were Non-Hispanic White patients (78.9%), diagnosed at localized stage (70.1%), and of endometrioid histology (80.0%). Compared with LOEC cases, women with EOEC were less likely to be Non-Hispanic White (68.4% vs 80.5%), more likely to be Hispanic (15.2% vs 6.4%) or Non-Hispanic Asian/Pacific Islander (6.1% vs 2.7%), and less likely to have advanced-stage (regional stage: 15.4% vs 18.8%; distant stage: 4.8% vs 7.2%) or poorly differentiated tumors (grade III: 9.0% vs 17.5%; grade IV: 1.9% vs 4.2%), respectively. EOEC also had higher percentages of endometrioid tumors (87.0% vs 79.0%) but a lower share of non-endometrioid tumor (5.7% vs 17.2%) than LOEC.
Table 1.
Case count (and percentage) distributions by race and ethnicity and tumor characteristics for EOEC and LOEC, 1995-2018, United Statesa
| Patient and tumor characteristics | EOEC (age 0-49 years) | LOEC (age ≥50 years) | Total |
|---|---|---|---|
| (n = 116 750) | (n = 813 426) | (N = 930 176) | |
| Race and ethnicity | |||
| Hispanic | 17 734 (15.2) | 52 170 (6.4) | 69 904 (7.5) |
| Non-Hispanic Asian/Pacific Islander | 7112 (6.1) | 21 836 (2.7) | 28 948 (3.1) |
| Non-Hispanic Black | 9530 (8.2) | 76 071 (9.4) | 85 601 (9.2) |
| Non-Hispanic White | 79 844 (68.4) | 654 407 (80.5) | 734 251 (78.9) |
| Other/unknown | 2530 (2.2) | 8942 (1.1) | 11 472 (1.2) |
| Summary stage | |||
| Localized | 87 753 (75.2) | 564 014 (69.3) | 651 767 (70.1) |
| Regional | 17 927 (15.4) | 153 157 (18.8) | 171 084 (18.4) |
| Distant | 5565 (4.8) | 58 534 (7.2) | 64 099 (6.9) |
| Unknown | 5505 (4.7) | 37 721 (4.6) | 43 226 (4.6) |
| Grade | |||
| I (low) | 54 591 (46.8) | 265 568 (32.6) | 320 159 (34.4) |
| II | 26 287 (22.5) | 194 498 (23.9) | 220 785 (23.7) |
| III | 10 554 (9.0) | 142 385 (17.5) | 152 939 (16.4) |
| IV (high) | 2178 (1.9) | 33 926 (4.2) | 36 104 (3.9) |
| Unknown | 23 140 (19.8) | 177 049 (21.8) | 200 189 (21.5) |
| Histologic subtype | |||
| Endometrioid | 101 541 (87.0) | 642 678 (79.0) | 744 219 (80.0) |
| Non-endometrioid | 6683 (5.7) | 139 627 (17.2) | 146 310 (15.7) |
| Sarcoma | 5874 (5.0) | 11 818 (1.5) | 17 692 (1.9) |
| Other | 2621 (2.3) | 19 132 (2.4) | 21 753 (2.3) |
| Unknown | 31 (0.0) | 171 (0.0) | 202 (0.0) |
Mantel-Haenszel χ2 test was used to obtain the P values comparing EOEC with LOEC by race and ethnicity and tumor characteristics. All P values were less than .001. EOEC = early-onset endometrial cancer; LOEC = late-onset endometrial cancer.
Other/Unknown race and ethnicity includes Alaska Native, American Indian, other race, and unknown or missing race.
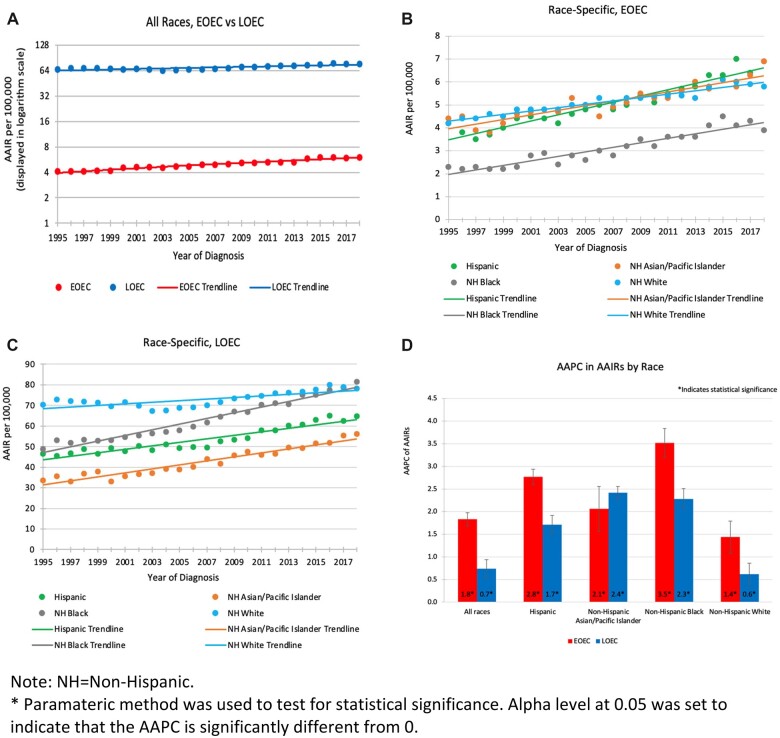
During 1995-2018, AAIRs for both EOEC and LOEC increased overall (Figure 1, A) and in each racial and ethnic population (Figure 1, B and C). For all races combined, the AAIR for EOEC increased from 4.1/100 000 in 1995 to 6.0/100 000 in 2018 and for LOEC from 65.8/100 000 to 76.7/100 000 (Supplementary Table 2, available online). These rising AAIR trends were statistically significant across the racial and ethnic groups, with the overall AAPC for EOEC being over 2 times greater than the overall AAPC for LOEC (1.8 vs 0.7) (Figure 1, D; Supplementary Table 3, available online). For EOEC, the AAPC was highest in Non-Hispanic Black women (3.5), followed by Hispanic women (2.8), Non-Hispanic Asian/Pacific Islander women (2.1), and lowest in Non-Hispanic White women (1.4). For LOEC, the AAPC was highest in Non-Hispanic Asian/Pacific Islander women (2.4), followed by Non-Hispanic Black women (2.3), Hispanic women (1.7), and lowest in Non-Hispanic White women (0.6). At the end of the study period, the highest AAIR for EOEC was observed in both Hispanic and Non-Hispanic Asian/Pacific Islander patient groups (6.9/100 000), and the highest AAIR for LOEC was observed among Non-Hispanic Black patients (81.4/100 000) (Figure 1, B and C; Supplementary Table 2, available online).
Figure 1.
Annual age-adjusted incidence rates (AAIRs) with trendlines with 95% confidence intervals (A) for all races, (B) by race and ethnicity for early-onset endometrial cancer (EOEC), and (C) by race-ethnicity for late-onset endometrial cancer (LOEC). (D) Average annual percent change (AAPC) in AAIRs with 95% confidence intervals by race and ethnicity for EOEC and LOEC, 1995-2018, United States. API = Asian/Pacific Islander; NH = Non-Hispanic.
The increase in EC incidence observed in our study is consistent with results from prior SEER-based analyses (6-8). Our unique contribution lies in using a larger database that enabled more granular evaluation of EC incidence trends not only by age but also by race and ethnicity, which revealed the faster and more substantial increasing incidence trends for EOEC than for LOEC, and in Hispanic, Non-Hispanic Asian/Pacific Islander, and Non-Hispanic Black women than in Non-Hispanic White women.
The accelerating EC incidence could be due to shifts in reproductive trends and rising obesity rates (6-8,17). Obesity, an established EC risk factor, has significantly increased in the US in the younger women (18,19). This rising obesity prevalence is more pronounced in Non-Hispanic Black (56.9%) and Hispanic (43.7%) compared with Non-Hispanic White (39.8%) and Non-Hispanic Asian/Pacific Islander (17.2%) women (19). Data suggest the incidence of obesity-related cancers is increasing in successively younger birth cohorts in the United States (20). Our findings of more substantial increase in EC incidence by race and ethnicity likely reflect the higher obesity rates in Hispanic and Non-Hispanic Black individuals. Socioeconomic and structural factors such as neighborhood safety and walkability, food insecurity, and lack of affordable and accessible healthy food options may also play a role in these obesity-related disparities. Non-Hispanic Asian/Pacific Islander women differ from all the other groups because they have a faster increase for LOEC than EOEC, which deserves further investigation. The faster increase in both EOEC and LOEC incidence among Hispanic, Non-Hispanic Asian/Pacific Islander, and Non-Hispanic Black individuals is concerning because prior studies have shown worse EC outcomes among Hispanic and Non-Hispanic Black women compared with Non-Hispanic White women (10). The faster increase in EOEC incidence also coincides with observations of broader increases in cancer among younger adults (21,22).
In conclusion, our study provides novel information to guide future directions in EC research. The recent increase in EC incidence among younger and non-White populations underscores the modifiable risk factors that likely exist at both individual and systemic levels that would require a comprehensive approach to intervention.
Supplementary Material
Contributor Information
Lihua Liu, Department of Population and Public Health Sciences, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA; Norris Comprehensive Cancer Center, University of Southern California, Los Angeles, CA, USA; Los Angeles Cancer Surveillance Program, Los Angeles, CA, USA.
Talar S Habeshian, Department of Population and Public Health Sciences, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA; Kaiser Permanente Southern California Department of Research and Evaluation, Pasadena, CA, USA.
Juanjuan Zhang, Department of Population and Public Health Sciences, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA.
Noah C Peeri, Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center, New York, NY, USA.
Mengmeng Du, Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center, New York, NY, USA.
Immaculata De Vivo, Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA, USA.
Veronica Wendy Setiawan, Department of Population and Public Health Sciences, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA; Norris Comprehensive Cancer Center, University of Southern California, Los Angeles, CA, USA.
Funding
This study was supported by the National Cancer Institute at the National Institutes of Health (U01CA250476 to IDV, MD and VWS).
Notes
Role of the funder: The funder did not play a role in the design of the study; the collection, analysis, and interpretation of the data; the writing of the manuscript; and the decision to submit the manuscript for publication.
Author disclosures: The authors have no disclosures.
Author contributions: LL (Conceptualization; Visualization; Writing—original draft; Writing—review & editing); TSH (Conceptualization; Project administration; Visualization; Writing—original draft; Writing—review & editing); JZ (Data curation; Formal analysis); NCP (Writing—review & editing); MD (Writing—review & editing); IDV (Writing—review & editing); VWS (Conceptualization; Funding acquisition; Project administration; Supervision; Writing—original draft, Writing—review & editing).
Prior presentations: The main results in this manuscript were presented as a poster at the American Association for Cancer Research Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved on September 18, 2022, in Philadelphia, PA.
Data availability
Data used in this study are publicly available through the North American Association of Central Cancer Registries (NAACCR) at https://www.naaccr.org/cina-data-products-overview/.
References
- 1. American Cancer Society. Cancer Facts and Figures 2022. American Cancer Society; 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf. Accessed December 9, 2022. [Google Scholar]
- 2. Siegel RL, Miller KD, Fuchs HE, Jemal A.. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 3. Cronin KA, Scott S, Firth AU, et al. Annual report to the nation on the status of cancer, part 1: national cancer statistics. Cancer. 2022;128(24):4251-4284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. SEERExplorer. Corpus and Uterus, NOS Recent Trends in SEER Age-Adjusted Incidence Rates, 2000-2019. https://seer.cancer.gov/statistics-network/explorer/. Accessed December 9, 2022.
- 5. Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA.. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. 2009;27(17):2758-2765. [DOI] [PubMed] [Google Scholar]
- 6. Constantine GD, Kessler G, Graham S, Goldstein SR.. Increased incidence of endometrial cancer following the Women's Health Initiative: an assessment of risk factors. J Womens Health (Larchmt). 2019;28(2):237-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Duong LM, Wilson RJ, Ajani UA, Singh SD, Eheman CR.. Trends in endometrial cancer incidence rates in the United States, 1999-2006. J Womens Health (Larchmt). 2011;20(8):1157-1163. [DOI] [PubMed] [Google Scholar]
- 8. Gaber C, Meza R, Ruterbusch JJ, Cote ML.. Endometrial cancer trends by race and histology in the USA: projecting the number of new cases from 2015 to 2040. J Racial Ethn Health Disparities. 2019. doi: 10.1007/s40615-016-0292-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rodriguez VE, LeBrón AMW, Chang J, Bristow RE.. Racial-ethnic and socioeconomic disparities in guideline-adherent treatment for endometrial cancer. Obstet Gynecol. 2021;138(1):21-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Baskovic M, Lichtensztajn DY, Nguyen T, Karam A, English DP.. Racial disparities in outcomes for high-grade uterine cancer: a California Cancer Registry Study. Cancer Med. 2018;7(9):4485-4495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cancer in North America (CiNA) Public Use Data Set, 2015-2019. Springfield, IL: North American Association of Central Cancer Registries, Inc. https://www.naaccr.org/cina-public-use-data-set/. Accessed December 9, 2022. [Google Scholar]
- 12. Sherman R, Firth R, De P, et al. Cancer in North America, 2014-2018. Volume Two: Registry-specific Cancer Incidence in the United States and Canada. North American Association of Central Cancer Registries, Inc.; 2021. [Google Scholar]
- 13. SEER Site Recode ICD-O-3/WHO 2008 Definition. https://seer.cancer.gov/siterecode/icdo3_dwhoheme/index.html. Accessed December 9, 2022.
- 14. NAACCR Race and Ethnicity Work Group. NAACCR Guideline for Enhancing Hispanic/Latino Identification: Revised NAACCR Hispanic/Latino Identification Algorithm [NHIA v2.2.1]. Springfield, IL: North American Association of Central Cancer Registries; 2011. https://www.naaccr.org/wp-content/uploads/2016/11/NAACCR-Method-to-Estimate-Completeness-Workbook-1995-2013.pdf. Accessed December 9, 2022. [Google Scholar]
- 15. NAACCR Race and Ethnicity Work Group. NAACCR Asian Pacific Islander Identification Algorithm [NAPIIA v1.2.1]. Springfield, IL: North American Association of Central Cancer Registries; 2011. https://www.naaccr.org/?s=napiia. Accessed December 9, 2022. [Google Scholar]
- 16. NCI-SEER. Modifications to Census Bureau’s County Population Data. https://seer.cancer.gov/popdata/modifications.html. Accessed December 9, 2022.
- 17. Birmann BM, Barnard ME, Bertrand KA, et al. Nurses' Health Study contributions on the epidemiology of less common cancers: endometrial, ovarian, pancreatic, and hematologic. Am J Public Health. 2016;106(9):1608-1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Onstad MA, Schmandt RE, Lu KH.. Addressing the role of obesity in endometrial cancer risk, prevention, and treatment. J Clin Oncol. 2016;34(35):4225-4230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity and Severe Obesity among Adults: United States, 2017–2018. NCHS Data Brief, no 360. Hyattsville, MD: National Center for Health Statistics; 2020. https://www.cdc.gov/nchs/data/databriefs/db360-h.pdf. Accessed December 9, 2022. [PubMed] [Google Scholar]
- 20. Scott AR, Stoltzfus KC, Tchelebi LT, et al. Trends in cancer incidence in US adolescents and young adults, 1973-2015. JAMA Netw Open. 2020;3(12):e2027738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sung H, Siegel RL, Rosenberg PS, Jemal A.. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health. 2019;4(3):e137-e147. [DOI] [PubMed] [Google Scholar]
- 22. Huang BZ, Liu L, Zhang J, et al. Rising incidence and racial disparities of early-onset pancreatic cancer in the United States, 1995-2018. Gastroenterology. 2022;163(1):310-312.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Clarke MA, Devesa SS, Hammer A, Wentzensen N.. Racial and ethnic differences in hysterectomy-corrected uterine corpus cancer mortality by stage and histologic subtype. JAMA Oncol. 2022;8(6):895-903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Clarke MA, Devesa SS, Harvey SV, Wentzensen N.. Hysterectomy-corrected uterine corpus cancer incidence trends and differences in relative survival reveal racial disparities and rising rates of nonendometrioid cancers. J Clin Oncol. 2019;37(22):1895-1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used in this study are publicly available through the North American Association of Central Cancer Registries (NAACCR) at https://www.naaccr.org/cina-data-products-overview/.