Abstract
Physician wellness is critical for patient safety and quality of care. Coaching has been successfully and widely applied across many industries to enhance well-being but has only recently been considered for physicians. This review aimed to summarize the existing evidence on the effect of coaching by trained coaches on physician well-being, distress and burnout. MEDLINE, Embase, ERIC, PsycINFO and Web of Science were searched without language restrictions to December 21, 2022. Studies of any design were included if they involved physicians of any specialty undergoing coaching by trained coaches and assessed at least one measure along the wellness continuum. Pairs of independent reviewers determined reference eligibility. Risk of bias was assessed using the Cochrane Risk of Bias Tools for Randomized Controlled Trials (RCTs) and for Non-randomized Studies of Interventions (ROBINS-I). Meta-analysis was not possible due to heterogeneity in study design and outcome measures as well as inconsistent reporting. The search retrieved 2531 references, of which 14 were included (5 RCTs, 2 non-randomized controlled studies, 4 before-and-after studies, 2 mixed-methods studies, 1 qualitative study). There were 1099 participants across all included studies. Risk of bias was moderate or serious for non-RCTs, while the 5 RCTs were of lower risk. All quantitative studies reported effectiveness of coaching for at least one outcome assessed. The included qualitative study reported a perceived positive impact of coaching by participants. Evidence from available RCTs suggests coaching for physicians can improve well-being and reduce distress/burnout. Non-randomized interventional studies have similar findings but face many limitations. Consistent reporting and standardized outcome measures are needed.
Introduction
Physician burnout represents a profound and longstanding epidemic in healthcare, with rates reported to be 1.5 times higher than the general US working population (37.9% vs. 27.8%) [1]. The prevalence of physician burnout has only been exacerbated by the COVID-19 pandemic. According to a national study conducted in 2021 in Canada, 53% of physicians and medical learners experienced symptoms of burnout, nearly double what was reported in a 2017 study (30%) [2].
The rise in physician burnout has serious consequences for both patient safety and quality of care. According to a recent systematic review and meta-analysis, physicians with burnout are twice as likely to be involved in patient safety incidents, to exhibit low professionalism and to receive low satisfaction ratings from patients [3]. Burnout is also costly to the healthcare system, with the cost to replace one physician estimated at $500 000, taking into account hiring and training costs as well as productivity losses [4].
Although many different interventions have been implemented to address physician burnout, several systematic reviews have found a wide range in effectiveness, from modest improvement in, to worsening of, burnout [5–12]. Existing interventions have largely focused on a specific stressor (e.g., modifications to electronic health record documentation to reduce associated burnout [6, 7]) and are short in duration (e.g., self-care workshops, stress management skills training [9]), or unsustainable given the resource limitations of the healthcare system (e.g., reducing physician workload [9]). Interventions involving single or short-term training sessions do not show consistent evidence of effectiveness, and in several instances, have even worsened resilience upon completion [5]. Other interventions have limited capacity to generalize to all aspects of physicians’ lives. For example, wellness interventions for neurosurgical faculty and residents involved free gym memberships, group gym visits, and team-based exercise sessions [8]. Evidence also suggests that interventions perceived as adding “burden” to physicians’ lives (i.e., requiring a substantial time commitment outside of working hours) are unlikely to be effective [13]. These limitations highlight the need for interventions that are tailored to the complex and unique lived experiences of individual physicians, rather than imposing a top-down, one-size-fits-all approach. The most effective interventions are those designed to meet the needs of the individuals they serve [14, 15]. Furthermore, evidence suggests that physicians are typically reluctant or ashamed to access mental health services or perceive that their problems are “not severe enough” [16]. Thus, initiatives framed as proactive professional development (rather than reactive) may ultimately be more accessible and effective in preventing distress and burnout, rather than offering resources too late in the game.
Coaching has been found to improve well-being and reduce burnout across many industries (e.g., finance, nuclear power, education), and more recently, healthcare [17–19]. The International Coaching Federation (ICF) defines coaching as “a thought-provoking and creative process that inspires [participants] to maximize their personal and professional potential.” [20] Delivered by trained coaches, coaching is a proactive and action-oriented intervention intended to empower individuals to with self-discovery, strength-building and self-efficacy [20, 21]. Through powerful questions and other techniques such as embodiment, active listening, curiosity, or emotional literacy, trained coaches help individuals to act according to their core values, regain control over their lives and achieve fulfillment [20, 21]. Although coaching is emerging as a promising intervention for physician wellness, a comprehensive summary and appraisal of the available evidence has yet to be completed. This is necessary to guide healthcare organizations considering implementation of coaching to support physician wellness.
Objectives
We aimed to conduct a systematic review of the existing evidence on the effect of coaching by trained coaches on physician wellness.
Methods
Protocol
This systematic review was planned and conducted according to A Measurement Tool to Assess Systematic Reviews (AMSTAR-2) standards [22] and reported in adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [23]. The review protocol was developed a priori and published on Open Science Framework [24].
Eligibility criteria
Studies of any interventional design were included if they involved licensed physicians or post-graduate trainees of any specialty undergoing coaching by trained coaches, delivered individually or to groups. Studies had to assess at least one outcome related to wellness (e.g., quality of life, resilience, psychological well-being), distress, and burnout [25] to be included. To be included, the coaching intervention had to meet the internationally recognized definition and core competencies described by the ICF (Table 1) [20, 21]. The ICF defines coaching as “a though-provoking and creative process that inspires [participants] to maximize their personal and professional potential” [20]. This was important to distinguish coaching from other interventions with which it is often confused (e.g., feedback, teaching, mentoring, peer support) [26], and was verified with specific screening questions during the reference selection process. We specifically excluded coaching interventions that did not meet the ICF standard definition or that were implemented as part of a multifaceted intervention. Studies involving medical students were also excluded. Conference abstracts, letters, editorials, and commentaries were not eligible for inclusion.
Table 1. International coaching federation coaching competencies [20, 21].
| Competency | Definition |
|---|---|
| A. Building the foundation | |
| 1. Demonstrating ethical practice | Understanding and consistently applying coaching ethics and standards. |
| 2. Embodying a coaching mindset | Developing and maintaining a mindset that is open, curious, flexible and client centered. |
| B. Co-creating the relationship | |
| 3. Establishing and maintaining agreements | Partnering with the client to create clear agreements about the coaching relationship, process, plans and goals. Establishing agreements for the overall coaching engagement as well as those for each coaching session. |
| 4. Cultivating trust and safety | Partnering with the client to create a safe, supportive environment that allows the client to share freely. Maintaining a relationship of mutual respect and trust. |
| 5. Maintaining presence | Being fully conscious and present with the client, employing a style that is open, flexible, grounded and confident. |
| C. Communicating effectively | |
| 6. Listening actively | Focusing on what the client is and is not saying to fully understand what is being communicated in the context of the client systems and to support client self-expression. |
| 7. Evoking awareness | Facilitating client insight and learning by using tools and techniques such as powerful questioning, silence, metaphor or analogy. |
| D. Cultivating learning and growth | |
| 8. Facilitating client growth | Partnering with the client to transform learning and insight into action. Promoting client autonomy in the coaching process. |
Search strategy and information sources
The search strategy was developed by an experienced information specialist (VL) in close collaboration with the research team (S1 Appendix) and reviewed by a second information specialist as per Peer Review of Electronic Search Strategies (PRESS) guidelines [27]. The databases MEDLINE, Embase, ERIC, and PsycINFO via Ovid and Web of Science were searched without date or language restrictions; however, only studies published in English or French were included in the final review. We planned to include an appendix of potentially relevant studies published in other languages; however, none were identified. The reference lists of included studies were also searched for potentially relevant studies that may not have been identified in the initial search. The final list of included studies was reviewed by coaching experts (SB, MDL, CA, AS) to confirm its relevance and completeness.
Study selection
Identified studies were uploaded to Covidence, a web-based systematic review software (Melbourne, Australia). Duplicates were detected and removed automatically by Covidence. A screening tool was developed by the research team, piloted, and iteratively refined until acceptable inter-rater reliability was established (minimum Cohen’s kappa = 0.7). The tool was designed to facilitate a judgement of “include” or “exclude” based on the pre-specified inclusion criteria described above. Pairs of independent reviewers (CD, PMD, CE, MK) first assessed titles and abstracts for eligibility, followed by the full texts of articles of included studies and those deemed “unclear”. Screening for inclusion at each level was always conducted in duplicate, with disagreements resolved by consensus or involvement of a third reviewer as needed (SB).
Data extraction
A data extraction form was developed and piloted, then used by the reviewers in duplicate to extract relevant information with Covidence. Extracted data included publication details (e.g., first author name, year of publication, country of data collection), study characteristics (e.g., study design, sample size, inclusion criteria), physician demographics, healthcare setting (e.g., community or academic hospital, specialty), intervention and comparator details, and the effect of intervention on reported outcomes of interest.
Risk of bias
Pairs of independent reviewers (CD, PMD, CE, MK) assessed included studies for risk of bias using the Cochrane Risk of Bias Tool 2 (RoB2) [28], and for Non-randomized Studies of Interventions (ROBINS-I) [29], as appropriate. The RoB2 tool assesses the potential for bias in terms of trial design, conduct, and reporting. Within each domain, there is a series of questions which facilitate a judgement about the risk of bias. The judgement can be “low”, “high”, or can express “some concerns.” [28], The ROBINS-I tool includes seven domains of bias: bias due to confounding, bias in selection of participants into the study, bias in classification interventions, bias due to deviations from intended interventions, bias due to missing data, bias in measurement of outcomes, and bias in selection of the reported result [29]. Within and across each domain, a judgement is made based on specified criteria as to whether there is a “low”, “moderate”, “serious”, or “critical” risk of bias [29].
Data synthesis
A narrative synthesis of results was conducted. We planned to conduct a meta-analysis if appropriate; however, this was not possible based on the heterogeneity in study design and outcome measures as well as inconsistent reporting.
Results
Study selection
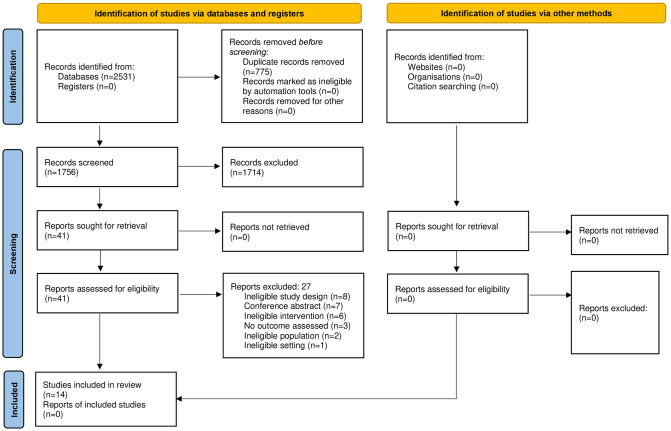
The literature search yielded 2531 studies. After removal of duplicates, 1756 studies were assessed for eligibility (Fig 1). Subsequently, 14 studies met the inclusion criteria and were included in this systematic review.
Fig 1. PRISMA flow diagram.
Study and participant characteristics
Details on included study and participant characteristics are provided in Table 2. Of the 14 included studies, 5 (36%) were RCTs, 2 were non-randomized controlled studies, 4 (29%) were before- and after-studies, 2 (14%) were mixed-methods studies, and 1 (7%) was a qualitative study. There were 1099 participants across all included studies. Over half of the included studies (n = 8 [57%]) involved post-graduate trainees (n = 707 [64%]) as the recipients of the coaching intervention. Approximately half of participants were general practitioners or internal medicine specialists (n = 572 [52%]). Three studies did not report participant specialty (n = 158 [14%]). Of the 6 studies that reported participant age, the majority of participants were between 41 and 50. Across the 11 studies reporting participant sex, nearly two thirds of participants were male (n = 491 [57%]).
Table 2. Characteristics of included studies and participants.
| First author, year, (country) | Study design | Sample size | Participants | Definition/description of coaching | Certification/training of coaches | Participant age (mean/median years) or Age groups (n/%) | Participant sex, No. (%) |
|---|---|---|---|---|---|---|---|
| de Lasson, [30] 2016, (Denmark) | Qualitative study | 45 | Staff physicians (speciality NR) | Coaching as a means to unfold a person’s potential in order to maximize performance. | “The medical consultant had a Master’s degree in Organizational Coaching. The nurses had academic degrees. One held a PhD in learning processes; the other a diploma in coaching from Cambridge University.” | NR | F: 38 (84.4) M: 7(15.6) |
| Dyrbye, [19] 2019 (United States) | Randomized controlled trial | 88 | Family medicine, general pediatrics, general internal medicine physicians | “Coaching is distinct from mentorship and peer support and involves inquiry, encouragement, and accountability to increase self-awareness, motivation, and the capacity to take effective action… Professional coaching can be tailored to focus on the aspects desired by recipients and can assist individuals in their effort to navigate their professional life, their choices, and the direction of their career.” | “Credentialed professional coaches were provided by Bluepoint Leadership Development Inc, an established international professional coaching company with experience coaching physicians.” | Intervention group: 31–40: 7 (15.9%) 41–50: 25 (56.8%) 51–60: 12 (27.3%) >60: 0 Control group: 31–40: 7 (16.7%) 41–50: 20 (47.6%) 51–60: 12 (28.6%) >60: 3 (7.1%) |
F: 48 (54.5) M: 40 (45.4) |
| Dyrbye, [31] 2022 (United States) | Randomized controlled trial | 80 | Surgical specialties: cardiology, gastrointestinal, general, gynecologic, neurological, oncology, ophthalmologic, orthopedic, otorhinolaryngologic, pediatrics, plastic, trauma, urologic, vascular, thoracic, transplant, other (e.g. oral) | Professional coaching is "tailored to the individual’s needs and assists individuals in navigating professional choices and behaviors… Professional coaching allows individuals to identify opportunities, generate goals, and take action related to professional needs, such as influencing change, dealing with conflict, addressing detrimental aspects of work, improving career fit, and improving work-life integration." | “The coaches had received training from various organizations with robust offerings including Right Management Global Coaching Program, Columbia University Executive Coaching Program, the Association for Professional Executive Coaches and Supervisors, and the Institute of Leadership and Management Coaching Program resulting in a coaching certification by the training organization and/or the International Coach Federation. The coaches had 15 years to over 25 years of coaching experience and 7 to 15 years of experience specifically coaching physicians and surgeons.” | Intervention group: 31–40: 12 (30%) 41–50: 21 (52.5%) 51–60: 7 (17.5%) 61+: 0 Control group: 31–40: 18 (45%) 41–50: 12 (30.0%) 51–60: 9 (22.5%) 61+: 1 (2.5%) |
F: 32 (40%) M: 48 (60%) |
| Fainstad, [32] 2022 (United States) | Randomized controlled trial | 101 | Residents across 12 programs (specialties NR) | “Professional coaching uses inquiry around perceptions, beliefs, and habits to define, reframe, and align work with personal values.” | “Coaches were certified by The Life Coach School, a thought-based coaching institution with training in both group and individual coaching.” | Intervention group: Mean (SD): 29.1 (2.3) Median (Range): 29 (25–35) Control group: Mean (SD): 29.6 (2.2) Median (Range): 29 (26–35) |
F: 101 (100%) |
| Gardiner, [33] 2013, (Australia) | Non-randomized experimental study | 69 | General practitioners | “A cognitive behavioural coaching program advertised as a work-life balance retreat by the Rural Doctors Work-force Agency (RDWA).” | Two qualified coaching psychologists | NR | NR |
| Kakarala, [34] 2018 (United States) | Pre-post study design | 12 | Post-graduate trainees (specialty NR) | “The Massachusetts General Hospital (MGH) Professional Development Coaching Program (PDCP) was designed to optimize resident performance through principles of positive psychology, using a strength-based model.” | Certified Health and Wellness Coaches trained by Coaching Program Director. The training was 2 hours, and “combined theory and real-life practice utilizing positive psychology, mindful listening, self-reflection, exploration of possible solutions, and validation of the coachee’s self-identified strategies to reach goals.” | NR | F: 4 (33.3) M: 8 (66.7) |
| McGonagle, [35] 2020, (United States) | Randomized controlled trial | 58 | General practitioners | “Coaching is a one-on-one intervention between a coach and individual coachee that is systematic, collaborative, future-focused, and goal-focused, and is meant to help coachees attain valued professional or personal development outcome.” | Credentialing organizations included the Center for Credentialing and Education, the Center for Creative Leadership, International Coach Federation, Coaches Training Institute, and Wellcoaches. | Mean +/- Standard deviation: Intervention group: 43.31 +/- 8.76 Control group: 41.83+/-7.42 |
Intervention group: F: 21 (72.4) M: 8 (27.6) Control group: F: 25 (86.2) M: 5 (13.8) |
| McKimm, [36] 2018, United Kingdom | Mixed-methods study (pre/post design + qualitative interviews) | 52 | General practitioners | “The purpose of the coaching was to support [participants] in their decision-making processes and prepare them for any transition… Coaches worth with their clients to meet their need to reflect, practice, step back or forge ahead with changes they wanted to make.” | “Coaches belonged to a national network of experienced, executive, professional coaches who work within professional codes of ethics. The coaches were all trained professionals (2 with mental health backgrounds) well versed in managing the boundaries between coaching and therapy and could therefore direct [participants] towards counselling/therapy where relevant.” | Range: 30–50 | F: 36 (69.2) M: 16 (30.8) |
| Palamara, [37] 2015 (United States) | Pre-post study design | 72 | Post-graduate trainees, internal medicine | “Coaching was based on the principles of positive psychology…Positive psychology coaching uses a strengths approach that emphasizes engagement, meaning, and accomplishment.” | “All coaches participated in 2 hours of training. Coaches were introduced to core concepts of developmental coaching and positive psychology, using hands on experience of coaching exercises. Strategies for managing particular situations such as poor intern performance and unrealistic self-assessment were reviewed.” |
NR | NR |
| Palamara, [38] 2018 (United States) | Pre-post study design | 104 | Post-graduate trainees, internal medicine | “Positive psychology coaching, using a strengths-based approach, provides participants with additional tools required to cope with… personal and professional stressors.” | Coaches trained in the Professional Development Coaching Program using positive psychology and coaching principles. | NR | NR |
| Palamara, [39] 2021 (United States) | Pre-post study design | 129 | Post-graduate trainees, internal medicine | “Coaching focused on strengths evaluation, resiliency, and constructing a framework of positive well-being.” | “Coaches were provided a 3-hour skills-based training in positive psychology and coaching principles and given curricular guides for 1:1 meetings with their coachees.” | NR | F: 56 (43.8) M: 72 (56.2) |
| Palamara, [40] 2022 (United States) | Randomized controlled trial | 150 | Surgical residents (specialties NR) | Coaching uses “principles of positive psychology [and focuses on] creating an effect coaching presence, core coaching skills of listening, goal-setting, [and] asking future-oriented questions rather than giving advice.” | Coaches participated in a 3-hour training program from the Institute of Coaching and had the option to participate in two additional 90-minute refresher training sessions | Mean (SD): Intervention group: 30.3 (3) Control group: 30.7 (2.9) |
F: 150 (100%) |
| Solms, [41] 2021 (Netherlands) | Non-randomized experimental study | 114 | Post-graduate trainees, pediatrics | “A result-oriented, systematic process in which the coach facilitates the enhancement of life experience and goal attainment in the personal and/or professional life of clients.” | Senior level of coaching experience, their experience with physician-clients, positive references from previous physician clients, and accredited coaching training. | Median (interquartile range): Intervention group: 33 (9.5) Control group: 35 (12) |
Intervention group: F: 47 (82.5) M: 10 (17.5) Control group: F: 42 (73.7) M: 15 (26.3) |
| Song, [42] 2020 (United States) | Mixed-methods study (pre/post design + qualitative interviews) | 25 | Post-graduate trainees; General Surgery, Vascular Surgery, Cardiac Surgery, Plastic Surgery, Urology | Coaching focuses “on continued and evolving collaboration between coach and [participant]… The individual coaching sessions adapted to each [participant’s] needs at the time of the session.” | “The program was administered by a certified, professional coach.” | NR | F: 8 (32) M: 17 (68) |
Risk of bias
All five of the RCTs were found to be at low risk of bias across almost all domains (Table 3). The measurement of outcome domain and the missing outcome domain were found to be at some risk of bias for the Dyrbye et al. [19] and McGonagle et al. [35] RCTs, respectively. The Palamara et al. study [40] was found to have some concerns of bias for the deviations from intended interventions domain and the missing outcome domain. The included non-randomized interventional studies and quantitative portions of the mixed-methods studies were mostly at moderate or serious risk of bias across all domains (Table 4). The included qualitative study was not assessed for risk of bias.
Table 3. Risk of bias of included randomized controlled trials.
| Author, year | Cochrane Risk of Bias 2 Assessment Domains | |||||
|---|---|---|---|---|---|---|
| Randomization process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported result | Overall bias | |
| Dyrbye, [19] 2019 | Low risk | Low risk | Low risk | Some concerns | Low risk | Some concerns |
| Dyrbye, [31] 2022 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Fainstad, [32] 2022 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| McGonagle, [35] 2020 | Low risk | Low risk | Some concerns | Low risk | Low risk | Some concerns |
| Palamara, [40] 2022 | Low risk | Some concerns | Some concerns | Low risk | Low risk | Some concerns |
Table 4. Risk of bias of included non-randomized interventional studies.
| Author, year | ROBINS-I Assessment Domains | |||||||
|---|---|---|---|---|---|---|---|---|
| Confounding | Selection of patients into the study | Classification of interventions | Deviations form intended interventions | Missing data | Measurement of outcomes | Selection of the reported result | Total risk of bias | |
| Gardiner, [33] 2013 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kakarala, [34] 2018 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| McKimm, [36] 2018 | No information | Serious risk | Low risk | Low risk | No information | Moderate risk | Moderate risk | Serious risk |
| Palamara, [37] 2015 | Serious risk | Moderate risk | Low risk | Low risk | No information | Moderate risk | Moderate risk | Serious risk |
| Palamara, [38] 2018 | Moderate risk | Moderate risk | Moderate risk | Moderate risk | No information | Moderate risk | Moderate risk | Serious risk |
| Palamara, [39] 2021 | Moderate risk | Moderate risk | Moderate risk | Moderate risk | No information | Low risk | Low risk | Moderate risk |
| Solms, [41] 2021 | Moderate risk | Moderate risk | Low risk | Low risk | No information | Low risk | Low risk | Moderate risk |
| Song, [42] 2020 | Moderate risk | Moderate risk | Moderate risk | Moderate risk | Moderate risk | Moderate risk | Moderate risk | Serious risk |
Definition of coaching and qualifications of coaches
Each of the included studies fell within the ICF definition of coaching, focusing on participant-centered goals, a collaborative coach-participant relationship, strengths-development, and maximizing participants’ potential or performance (Table 2). Ten studies specifically indicated that the coaches involved were accredited by a coaching organization or had professional coaching certifications. The other 4 studies indicated that coaches were trained but provided limited certification details. Details about coaches’ certification for individual studies are included in Table 1.
Coaching intervention and control description
The median number of coaching sessions involved was 5.5 (IQR = 2.75) (Table 5). Two studies did not report the number of sessions and were excluded from this calculation. Coaching sessions ranged in duration from 30 minutes to a full day. Six studies included a control group, where participants received no intervention at all or were offered coaching at the end of the study (Table 5). One study included a control group that received wellness resources via email during the study period. The other 7 studies did not include a control group (Table 5). Coaching was delivered at the group level in four studies [30, 32, 33, 42], and at the individual level by the remaining 10 studies.
Table 5. Effectiveness of coaching on physician well-being, distress and burnout.
| First author, year | Study design, sample size | Coaching intervention (number, duration, frequency of sessions) vs. control | Outcome(s), measure, timing | Results |
|---|---|---|---|---|
| de Lasson, [30] 2016 | Qualitative study, 45 | 8, three whole-day sessions and five 2 h sessions, NR Control: NA |
Adoption to medical culture, career planning, work/life balance; thematic analysis; halfway point (2 months) and end of intervention (4 months) | “Participants typically stated that they had gained a new awareness of their patterns of thinking, feelings and reactions and found new ways of taking control of their professional lives. Participants were more at ease with themselves.” |
| Dyrbye, [19] 2019 | Randomized controlled trial, 88 | 5, initial: 1 hour; remainder: 30 minutes, every 2–3 weeks over 5 months Control: No coaching intervention (but given access to coaches after 5 months). |
Burnout: Maslach Burnout Inventory; Baseline and end of study (5 months) | Prevalence of symptoms decreased by 17.1% in the intervention and increased by 4.9% in the control group; absolute change -22.0 (95% CI, -25.2 to -18.7), p<0.001 |
| Quality of life; Single-item linear analog scale; Baseline and end of study (5 months) | Improved in intervention group: absolute change mean score (SD) = 1.2 (2.5) vs control group = 0.1 (1.7); absolute change, intervention vs. control = 1.1 (95% CI, 0.04 to 1.21), p = 0.005 | |||
| Resilience; Connor-Davidson Resilience Scale; Baseline and end of study (5 months) | Improved in intervention group: absolute change mean score (SD) = 1.3 (5.2) vs. control group = 0.6(4.0); absolute change intervention vs. control group = 0.7 (95% CI, 0.0 to 3.0), p = 0.04 | |||
| Job satisfaction; Global job satisfaction subscale of the Physician Job Satisfaction Scale; Baseline and end of study (5 months) | No difference (p = 0.79) | |||
| Work engagement; Utrecht Work Engagement Scale; Baseline and end of study (5 months) | No difference (Vigor: p = 0.16; Dedication: p = 0.73; Absorption: p = 0.77) | |||
| Empowerment at work; Empowerment at Work Scale; Baseline and end of study (5 months) | No difference (p = 0.95) | |||
| Dyrbye, 2022 [31] | Randomized controlled trial, 80 | 6, initial: 1 hour; remainder: 30 minutes, every 2–3 weeks over 5 months Control: No coaching intervention (but given access to coaches after 6 months). |
Burnout: Maslach Burnout Inventory (MBI); Baseline and end of study (6 months) | Decreased by 2.5% in intervention group; increased by 2.5% control group (delta -5.0%, 95% CI -8.6%, -1.4%, p = 0.007). |
| Quality of life; Single-item linear analog scale; Baseline and end of study (6 months) | No statistically significant difference. | |||
| Resilience; Connor-Davidson Resilience Scale; Baseline and end of study (6 months) | Increased by 1.9 points in intervention group; decreased by 0.2 points in control group (delta 2.2 points, 95% CI0.1, 4.3, p = 0.04). | |||
| Depersonalization; Subscale of MBI (6 months) | Greater reduction in intervention group vs. control group: mean (SD) = -1.3 (3.1) points vs. 0.4 (3.6) points, delta -1.7 points, 95% CI -3.2, -0.2; p = 0.03). Rates of high depersonalization decreased by 3.8% in intervention group; increased by 2.5% in control group (delta -6.3%, 95% CI -9.5%, -3.1%; p <0.001). |
|||
| Emotional exhaustion; Subscale of MBI (6 months) | Rates of high emotional exhaustion decreased by 5.4% in intervention group and by 2.5% in control group (delta -2.9%, 95% CI -6.4%, 0.7%; p = 0.11). | |||
| Fainstad, 2022 [32] | Randomized controlled trial, 101 | Intervention: Participants could participate in any or all of the following over a 6-month period: (1) two 1-hour group coaching calls per week; unlimited anonymous written coaching via online forum; unlimited access to weekly self-study modules Control: No coaching intervention (but offered coaching program after 6 months). |
Burnout: Maslach Burnout Inventory subscales of Emotional Exhaustion (EE), Depersonalization (DP), Professional Accomplishment (PA); Baseline and end of study (6 months) | EE lower in intervention group, increased in control group: mean (SE) score = -3.26 (1.25) vs. 1.07 (1.12), p = 0.01 DP: No statistically significant effect for intervention or control group (−1.06 [0.64] vs −0.03 [0.58]; P = .23) PA: No statistically significant effect for intervention or control group (1.16[0.83] vs 0.25 [0.75]; P = .41) |
| Imposter syndrome: Young Imposter Syndrome Scale; Baseline and end of study (6 months) | Reduced in intervention group; increased in control group: mean (SE) score = −1.16(0.31) vs 0.11 (0.27), p = 0.003 | |||
| Self-compassion: Neff’s Self-Compassion Scale—Short Form; Baseline and end of study (6 months) | Improved in intervention group: mean (SE) score = 5.5(0.89) vs. -1.32 (0.80), p<0.001 | |||
| Moral Injury: Moral Injury Symptom Scale—Healthcare professionals; Baseline and end of study (6 months) | No statistically significant effect for intervention or control group: mean(SE) score = -5.39 (1.62) vs. -183 (1.47), p = 0.10 | |||
| Gardiner, [33] 2013 | Non-randomized experimental study, 69 | 8 coaching workshops and 6 weeks of email coaching, 9-hours total, Over 3 year period Control: No coaching intervention |
Distress; 10-item unnamed scale; before and 3 to 42 months after the intervention | Lower in intervention group: Mean score = 24.50 (95% CI, 21.71–27.29) vs. control group: mean score = 28.63 (95% CI, 27.08–30.17) |
| Intention to leave practice; 7-item unnamed scale; before and 3 to 42 months after the intervention | Before coaching, 81% of participants in the intervention group had considered leaving general practice; decreased to 40% after coaching (c2(2) = 16.31, P < .001). | |||
| Retention rate; calculated by comparing coaching participants with the total remaining population of rural physicians (n = 312); 2 time points, 3 years apart. | “Over a 3-year period, 94% of the coaching group remained in general practice compared with 80% of the control group (c2(1) = 4.89, P = 0.027).” | |||
| Kakarala, [34] 2018 | Pre-post study design, 12 | NR, 1 year program, NR Control: NA |
Emotional exhaustion; subscale of Maslach Burnout Inventory; Baseline and 1-year. | Emotional exhaustion was high or medium for 60% of participants at baseline, and 56% at 1-year. |
| McGonagle, [35] 2020 | Randomized controlled trial, 58 | 6, First session: 60min; remainder: 30 min, approximately every 2 weeks Control: No coaching intervention |
Burnout; Maslach Burnout Inventory; Pre- and post-intervention and 3- and 6-months post-intervention. | Intervention group vs. control group (p = 0.003): F = 9.82** Pre: M(SD) = 2.32 (0.68) vs. 2.37 (0.71) Post: M(SD) = 1.97 (0.72) vs. 2.45 (0.72) |
| Work stress; 15-item Stress in General Scale; Pre- and post-intervention and 3- and 6-months post-intervention. | Intervention group vs. control group (p = 0.077): Pre: M(SD) = 2.04 (0.77) vs. 2.13 (0.45) Post: M(SD) = 1.72 (0.76) vs. 2.09 (0.57) |
|||
| Turnover intentions; 3-item Turnover Intentions scale; Pre- and post-intervention and 3- and 6-months post-intervention. | Intervention group vs. control group (p = 0.062): Pre: M(SD) = 2.05 (0.91) vs. 1.75 (0.67) Post: M(SD) = 1.82 (0.85) vs. 1.76 (0.76) |
|||
| Engagement; 17-item Engagement Scale; Pre- and post-intervention and 3- and 6-months post-intervention. Psychological capital; 24-item Psychological Capital Questionnaire; Pre- and post-intervention and 3- and 6-months post-intervention. |
Intervention group vs. control group (p = 0.023): F = 5.49** Pre: M(SD) = 5.73 (0.78) vs. 5.87 (0.88) Post: M(SD) = 6.06 (0.68) vs. 5.92 (0.68) Intervention group vs. control group (p = 0.002): f = 10.39** Pre: M(SD) = 4.08 (0.69) vs. 4.23 (0.68) Post: M(SD) = 4.63 (0.68) vs. 4.39 (0.74) |
|||
| Compassion; 5-item Santa Clara | Intervention group vs. control group (p = 0.784): | |||
| Brief Compassion Scale; Pre- and post-intervention and 3- and 6-months post-intervention. | Pre: M(SD) = 5.47 (0.93) vs. 5.48 (0.99) Post: M(SD) = 5.63 (0.83) vs. 5.58(1.01) |
|||
| Job self-efficacy; 7-item Job Self-Efficacy Scale; Pre- and post-intervention and 3- and 6-months post-intervention. | Intervention group vs. control group (p = 0.62): Pre: M(SD) = 3.78 (0.66) vs. 3.46 (0.72) Post: M(SD) = 4.01 (0.60) vs. 3.61 (0.70) |
|||
| Job satisfaction; three items from Cammann, Fichman, Jenkins, and Klesh Scale; Pre- and post-intervention and 3- and 6-months post-intervention. | Intervention group vs. control group (p = 0.021): F = 5.74** Pre: M(SD) = 3.59 (0.95) vs. 4.11 (0.54) Post: M(SD) = 3.91 (0.80) vs. 4.04 (0.53) |
|||
| McKimm, [36] 2018 | Mixed-methods study (pre/post design + qualitative interviews), 52 | 4, NR, a period of up to 18 months. Control: NA |
Likelihood of leaving profession; unnamed 10-point scale; baseline and immediately after intervention | “Pre-coaching, 75% of respondents said they were likely (score of 7+) to leave general practice; this fell to 21% (nine GPs) of post-coaching questionnaire respondents. Of the latter group, half of them were aged between 50 and –60 and 4 planned to continue working as a doctor in different roles.” |
| Performance under pressure; Human Function Curve; first and last coaching sessions. | “At the start of coaching, 4 GPs rated themselves at breakdown point, 27 at the point of exhaustion and a further 4 considered themselves fatigued. GPs’ self-rated performance was considerably improved at the end of coaching. The final ratings of all except 4 GPs moved from ‘distress’, ‘boredom’ and excess pressure nearer to the ‘safe zone’, with 27 moving to the ‘safe zone’. Only one GP moved further up the ‘pressure scale’; however, they explained that coaching had revealed they were in denial about the pressure they were working under at the start of coaching.” |
|||
| Palamara, [37] 2015 | Pre-post study design, 72 | Up to 4, 40 minutes, every 3 months Control: NA |
Personal accomplishment; subscale of Maslach Burnout Inventory; Baseline, 3-months, 12-months (post) | High personal accomplishment: pre-coaching 49/59 participants; post-coaching: 48/59 participants |
| Emotional exhaustion; subscale of Maslach Burnout Inventory; Baseline, 3-months, 12-months (post) | High emotional exhaustion: pre-coaching: 44/59 participants; post-coaching: 33/59 participants | |||
| Palamara, [38] 2018 | Pre-post study design, 104 | 3 or more per year, NR, every 3 months Control: NA |
Coping skills; unnamed survey; 3 years | 70% of those who participated fully in the coaching program indicated improved coping skills |
| Perception of professional relationships; unnamed survey; 3 years | 70% of those who participated fully in the coaching program indicated improved relationships | |||
| Emotional exhaustion; subscale of Maslach Burnout Inventory; 3 years | 62.8% of participants who reported excellent opportunities for reflection with their coach also reported lower levels of emotional exhaustion | |||
| Palamara, [37] 2021 | Pre-post study design, 129 | 2–3 per year, 45–60 minutes, every 3 months Control: NA |
Burnout; Depersonalization and Emotional exhaustion subscales of Maslach Burnout Inventory; baseline and 8 months | Participants with higher burnout (measured by depersonalization and emotional exhaustion scores) at baseline more likely to improve and experience lower burnout at 8 months (-0.393, p<0.001; -0.476, p<0.001). |
| Emotional exhaustion; subscale of Maslach Burnout Inventory; baseline and 8 months | Black/Asian/Hispanic participants more likely to experience increase compared to non-Hispanic white participants (2.608, 0.46). Decrease for non-Hispanic white participants (mean difference = -1.86, p = 0.02) |
|||
| Well-being; PERMA Well-being Scale; baseline and 8 months | Well-being changed from baseline to follow-up in all participants; females showed a decline while males showed an increase (−1.41 vs. 0.83, p = 0.04). Less improvement observed if participant had higher well-being at baseline (-0.407, p<0.001). |
|||
| Palamara, [40] 2022 | Randomized controlled trial, 150 | Intervention: Minimum 3 coaching sessions, 45–60 minutes, 9-month period Control: three emails over study period containing well-being resources |
Professional fulfillment; Professional fulfillment index (PFI) subscale; baseline and post-intervention (9 months) | Increase: mean (SD) pre 2.33(0.67) vs post 2.52(0.77) p = 0.021; Cohen’s d = 0.26 |
| Burnout (work exhaustion + interpersonal disengagement); PFI subscale; baseline and post-intervention (9 months) | Decrease in burnout: mean (SD) pre 1.39(0.68) vs post 1.19(0.58) p = 0.026; Cohen’s d = -0.26], Decrease in work exhaustion: mean (SD) pre 1.72(0.78) vs post 1.48(0.67) p = 0.017; Cohen’s d = -0.27 Decrease in interpersonal disengagement: mean (SD) pre 1.17(0.71) vs post 1.00(0.62) p = 0.071; Cohen’s d = -0.21 |
|||
| Self-evaluation; unnamed 5-point Likert scale; baseline and post-intervention (9 months) | Increase: mean (SD) pre 1.42(0.71) vs post 1.75(0.82) p = 0.0003; Cohen’s d = 0.35 | |||
| Positive emotions, engagement, relationship, meaning and accomplishment (PERMA); PERMA scale; baseline and post-intervention (9 months) | Increase: mean (SD) pre 55.47(7.60) vs post 58.05(7.90) p = 0.002; Cohen’s d = 0.37 | |||
| Intolerance of Uncertainty (IUS); IUS scale; baseline and post-intervention (9 months) | Improvement (reduction in IUS score) in intervention group (53.0% to 40.8%), but not statistically significant (p = 0.07) | |||
| Resilience: Hardiness Resilience Score scale; baseline and post-intervention (9 months) | No significant change | |||
| Solms, [41] 2021 | Non-randomized experimental study, 114 | 6, 60–90 minutes, varied (time in between sessions determined by participants) Control: No coaching intervention |
Emotional exhaustion; subscale of Maslach Burnout Inventory; baseline and 10 months | Pre: mean(SD) = 2.75 (1.08) Post: mean(SD) = 2.25 (0.79), p = 0.000 |
| Cynicism; subscale of Maslach Burnout Inventory; baseline and 10 months | Pre: mean(SD) = 2.11(1.08) Post: mean(SD) = 1.90 (SD 0.75), p = 0.151 |
|||
| Work engagement; Utrecht Work Engagement Scale; baseline and 10 months | Pre: mean(SD) = 5.08(0.78) Post: mean(SD) = 5.28 (0.59), p = 0.033 |
|||
| Psychological capital; PsyCap questionnaire; baseline and 10 months | Pre: mean (SD) = 4.83(0.69) Post: mean (SD) = 5.16(0.65), p = 0.000 |
|||
| Self-compassion; Self-Compassion Scale; baseline and 10 months | Pre: mean (SD) = 3.07(0.60) Post: mean (SD) = 3.27(0.52), p = 0.009 |
|||
| Psychological flexibility; Work Acceptance and Action Questionnaire; baseline and 10 months | Pre: mean (SD) = 3.43(0.63) Post: mean (SD) = 3.47(0.65), p = 0.6 |
|||
| Song, [42] 2020 | Mixed-methods study (pre/post design + qualitative interviews), 25 | 1 group workshop (2 hours) + 8 individual sessions (1 hour), spaced throughout academic year Control: NA |
Burnout; Abbreviated Maslach Burnout Inventory; first and last coaching sessions | No statistically significant changes in burnout scores or the proportion of participants at risk of burnout before (60%) and after (52%) coaching (p = 0.78). |
| Resilience; Brief Resilience Scale; first and last coaching sessions | Mean resilience score improved: mean (SD) = 3.8 (0.8) to 4.2 (0.7) (p = 0.002). Improvement was observed primarily among men (mean [SD], 4.1 [0.7] vs. 4.5 [0.5], p = 0.007) rather than women (mean [SD], 3.4 [1.0] vs 3.6 [0.8], p = 0.16). |
|||
| Positive and negative feelings; Scale of Positive and Negative Experience; first and last coaching sessions | No statistically significant improvement (mean [SD] = 6.7 [8.2] vs 8.4 [8.3], p = 0.14) | |||
| Perceptions of coaching experience, burnout and wellness; grounded theory analysis; end of intervention | Most participants reported that coaching provided useful skills and was helpful for improve well-being, but felt it should be offered for a longer duration. |
Effectiveness of coaching for improving well-being, distress and burnout
Of the 13 included studies with a quantitative component, 7 reported a decrease in emotional exhaustion (n participants = 612 [58%]) and 5 reported a decrease in overall burnout (n participants = 505 [48%]) (Table 5). Four of the 5 studies that found a decrease in burnout were RCTs (Table 5). McGonagle et al. [35] reported a mean burnout score of 1.97 (baseline: 2.32) for the intervention group compared to 2.45 (baseline: 2.37) for the control group (p = 0.003). Dyrbye et al. [19] reported that the prevalence of symptoms decreased by 17.1% in the intervention group and increased by 4.9% in the control group (absolute change = -22.0 [95% CI, -25.2 to -18.7], p<0.001). In their 2022 study, Dyrbye et al. [31] reported a 2.5% decrease in burnout in the intervention group, whereas burnout increased in the control group (p = 0.007). Palamara et al. [40] reported a decrease in burnout score from 1.39 to 1.19 for participants who received coaching (p = 0.026). The remaining studies either did not assess these outcomes or reported no difference (Table 5).
Increased resilience of coaching participants was observed by three studies (n participants = 193 [18%]). Each of the outcomes—psychological capital (n participants = 172 [16%]), work engagement (n participants = 172 [16%]), emotional well-being (n participants = 279 [26%]) and job retention (n participants = 190 [18%])—were reported to improve after participation in the coaching intervention by 2 studies (Table 5). Improvements in compassion (n participants = 114 [11%]), coping skills (n participants = 104 [10%]), job satisfaction (n participants = 58 [6%]), perception of professional relationships (n participants = 104 [10%]), performance under pressure (n participants = 52 [5%]), quality of life (n participants = 88 [8%]), self-compassion (n participants = 101 [10%]), professional fulfillment (n participants = 150 [14%]), self-evaluation (n = 150 [14%]) were each observed by 1 study (Table 5). Reduction in imposter syndrome (n participants = 101 [10%]), work exhaustion (n participants = 150 [14%]), interpersonal disengagement (n participants = 150 [14%]), depersonalization (n participants = 80 [8%]), intolerance of uncertainty (n participants = 150 [14%]) were each observed by one study. One study also reported that positive changes in well-being after coaching were experienced only by Caucasian and male participants [39].
In the sole included qualitative study by de Lasson et al., [30] participants reported gaining “a new awareness of their patterns of thinking, feelings and reactions” and being “more at ease with themselves”. Participants also reported finding new ways to take control of their professional lives (Table 5).
Discussion
Summary of main findings
This systematic review identified 14 studies assessing the effect of coaching on physician wellness and burnout. Five of these studies were RCTs at relatively low risk of bias, while the included non-randomized interventional studies were mostly at moderate or serious risk of bias. Across all studies, coaching was observed to improve several outcomes related to wellness, including work/life balance, quality of life, resilience, job satisfaction, work engagement, empowerment at work, and psychological capital. Coaching was also generally observed to decrease emotional exhaustion, distress, and burnout.
The definition of coaching used in included studies was relatively homogeneous, as could be expected based on our inclusion criteria which rigorously adhered to the International Coaching Federation definition of coaching [20]. Although studies viewed coaching similarly, their implementation of coaching varied. For example, some studies involved only 3 to 4 sessions while others involved 6 or more. The duration of the sessions also differed between studies as well as the time period over which coaching was offered and whether coaching was delivered at the group or individual level. Despite this variation, coaching still appeared to positively impact participant wellness regardless of its mode of delivery. It may be worthwhile to explore the minimally effective “dose” of coaching in future research to maximize benefits for physician wellness while working within resource constraints and scheduling challenges. In addition, the optimal level of coach certification for maximizing physician wellness should be explored as it also varied between the studies included here. Currently, coaching is an unregulated profession, albeit there are national and international certification bodies. Minimum standards of coach competency and conduct may be in participants’ best interest moving forward if there is a relationship between coach certification and participant outcomes.
In order to effectively make comparisons, standardized reporting and outcome measures are also needed. The included studies assessed a wide range of outcome measures and designs. Baseline and post-intervention proportions of the outcome measures were also not regularly reported. The heterogeneity in outcome measures among the included studies may reflect the lack of consensus in the broader literature regarding the best way to conceptualize and assess physician wellness [43]. Given the multifaceted nature of physician wellness, there is a need for “a shared, holistic definition… that explicitly includes integrated well-being constructs (e.g., purpose, thriving, vigor, work-life balance) along with mental, social and physical constructs.” [43] A comprehensive and shared definition will improve the quality of research on physician wellness, including studies of intervention effectiveness, and increase comparability of findings.
Another consideration for reporting is to disaggregate results by relevant participant characteristics, such as sex, gender, and ethnicity. One of the included studies observed differential effectiveness of coaching by sex and ethnicity of participants, while other studies did not report results across these variables. Recent studies document that the prevalence, presentation, and factors contributing to burnout can vary by race/ethnicity, gender, and sexual orientation [44–48]. Consequently, these and other equity-related characteristics may be important to consider when evaluating the outcomes of coaching. Interestingly, two of the included RCTs evaluated the effectiveness of coaching for female participants only, and found significant benefits [44, 45]. Qualitative research may be useful to explore the mechanisms of change among coaching participants and generate hypotheses regarding its relative effectiveness within and across groups of physicians.
Strengths and limitations
This review identifies five RCTs at relatively low risk of bias that show evidence supporting the effectiveness of coaching for physicians. There are some limitations based on inconsistent and incomplete reporting were common across the included studies. In addition, most studies were not RCTs, and these were all at moderate to serious risk of bias. Nevertheless, this review addresses an emerging and promising intervention for physician wellness at a time when levels of distress and burnout are on the rise. It also identifies key gaps for future research on coaching to address.
Implications for researchers, clinicians and policymakers
Based on the available evidence, coaching may be a promising intervention for improving physician wellness but requires further study to precisely determine its optimal delivery and effectiveness. Additional RCTs with standardized reporting and outcome measures, sub-group analyses, and qualitative exploratory work are needed. At the same time, coaching may be an appealing intervention to clinicians given its flexibility and strengths-based approach. Should future research conclusively support its effectiveness for improving physician wellness, healthcare organizations may wish to facilitate coaching as part of their wellness programs for physicians.
Conclusions
Evidence from available RCTs suggests coaching for physicians can improve well-being and reduce distress/burnout. Non-randomized interventional studies have similar findings but face many limitations. Consistent reporting and standardized outcome measures are needed.
Supporting information
(DOCX)
(DOCX)
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
Dr. Sylvain Boet was supported by The Ottawa Hospital Anesthesia Alternate Funds Association, the Faculty of Medicine, University of Ottawa with a Tier 2 Clinical Research Chair, and the Faculty of Medicine.
References
- 1.Vogel L. Even resilient doctors report high levels of burnout, finds CMA survey. CMAJ Can Med Assoc J. 2018. Oct 29;190(43):E1293. doi: 10.1503/cmaj.109-5674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canadian Medical Association. National Physician Health Survey [Internet]. 2022 Aug [cited 2022 Dec 19]. https://www.cma.ca/sites/default/files/2022-08/NPHS_final_report_EN.pdf
- 3.Hodkinson A, Zhou A, Johnson J, Geraghty K, Riley R, Zhou A, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. 2022. Sep 14;e070442. doi: 10.1136/bmj-2022-070442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017. Dec 1;177(12):1826–32. doi: 10.1001/jamainternmed.2017.4340 [DOI] [PubMed] [Google Scholar]
- 5.Seo C, Corrado M, Fournier K, Bailey T, Haykal KA. Addressing the physician burnout epidemic with resilience curricula in medical education: a systematic review. BMC Med Educ. 2021;21(1). doi: 10.1186/s12909-021-02495-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeChant PF, Acs A, Rhee KB, Boulanger TS, Snowdon JL, Tutty MA, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019. Dec;3(4):384–408. doi: 10.1016/j.mayocpiqo.2019.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas Craig KJ, Willis VC, Gruen D, Rhee K, Jackson GP. The burden of the digital environment: a systematic review on organization-directed workplace interventions to mitigate physician burnout. J Am Med Inform Assoc JAMIA. 2021. Apr 23;28(5):985–97. doi: 10.1093/jamia/ocaa301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berardo L, Gerges C, Wright J, Stout A, Shah H, Papanastassiou A, et al. Assessment of burnout prevention and wellness programs for US-based neurosurgical faculty and residents: a systematic review of the literature. J Neurosurg. 2020;1–9. doi: 10.3171/2020.6.JNS201531 [DOI] [PubMed] [Google Scholar]
- 9.De Simone S, Vargas M, Servillo G. Organizational strategies to reduce physician burnout: a systematic review and meta-analysis. Aging Clin Exp Res. 2021. Apr;33(4):883–94. doi: 10.1007/s40520-019-01368-3 [DOI] [PubMed] [Google Scholar]
- 10.Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ. 2017. Jun;9(3):294–301. doi: 10.4300/JGME-D-16-00372.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalani SD, Azadfallah P, Oreyzi H, Adibi P. Interventions for physician burnout: a systematic review of systematic reviews. Int J Prev Med. 2018;9:81. doi: 10.4103/ijpvm.IJPVM_255_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet Lond Engl. 2016. Nov 5;388(10057):2272–81. doi: 10.1016/S0140-6736(16)31279-X [DOI] [PubMed] [Google Scholar]
- 13.Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M. Efficacy of Interventions to Reduce Resident Physician Burnout: A Systematic Review. J Grad Med Educ. 2017;9(3):294–301. doi: 10.4300/JGME-D-16-00372.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brooks E, Early SR, Gendel MH, Miller L, Gundersen DC. Helping the healer: Population-informed workplace wellness recommendations for physician well-being. Occup Med. 2018;68(4):279–81. doi: 10.1093/occmed/kqy018 [DOI] [PubMed] [Google Scholar]
- 15.Ontario Medical Association. Healing the Healers: System-Level Solutions to Physician Burnout. Toronto; 2021.
- 16.Bynum WE, Sukhera J. Perfectionism, Power, and Process: What We Must Address to Dismantle Mental Health Stigma in Medical Education. Acad Med. 2021;96(5):621–3. doi: 10.1097/ACM.0000000000004008 [DOI] [PubMed] [Google Scholar]
- 17.Grant A, Cavanagh M, Passmore J, Parker H. The state of play in coaching today: a comprehensive review of the field. Int Rev Ind Organ Psychol. 2010;25(March):125–67. doi: 10.1002/9780470661628.ch4 [DOI] [Google Scholar]
- 18.Schneider S, Kingsolver K, Rosdahl J. Physician coaching to enhance well-being: A qualitative analysis of a pilot intervention. Explore J Sci Heal. 2014. Nov 1;10(6):372–9. doi: 10.1016/j.explore.2014.08.007 [DOI] [PubMed] [Google Scholar]
- 19.Dyrbye LN, Shanafelt TD, Gill PR, Satele VD, West CP. Effect of a professional coaching intervention on the well-being and distress of physicians: a pilot randomized clinical trial. JAMA Intern Med. 2019;179(10):1406–14. doi: 10.1001/jamainternmed.2019.2425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.International Coaching Federation. What is Coaching? [Internet]. ALL THINGS COACHING. 2021 [cited 2021 Jun 14]. https://coachingfederation.org/about
- 21.International Coaching Federation. Updated ICF Core Competencies [Internet]. 2019 [cited 2021 Jul 26]. https://coachingfederation.org/credentials-and-standards/core-competencies
- 22.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017. Sep 21;358:j4008. doi: 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Etherington C. The effect of coaching on physician well-being, distress and burnout: A systematic review of interventional studies. OSF [Internet]. 2022 Aug 25 [cited 2022 Aug 29]; https://osf.io/akbxf https://osf.io/th3nx/
- 25.Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians a systematic review. JAMA—J Am Med Assoc. 2018;320(11):1131–50. doi: 10.1001/jama.2018.12777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boet S, Etherington C, Andreas C, Denis-LeBlanc M. Professional coaching as a continuing professional development intervention to address the physician distress epidemic. J Contin Educ Health Prof. doi: 10.1097/CEH.0000000000000450 [DOI] [PubMed] [Google Scholar]
- 27.McGowan J, Sampson M, Salzwedel D, Cogo E, Foerster V, Lefebvre C. PRESS—Peer Review of Electronic Search Strategies Guideline: Explanation & Elaboration. 2016;(January). [DOI] [PubMed] [Google Scholar]
- 28.RoB 2: A revised Cochrane risk-of-bias tool for randomized trials [Internet]. Cochrane Methods Bias. [cited 2022 Aug 31]. https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials
- 29.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016. Oct 12;355:i4919. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Lasson L, Just E, Stegeager N, Malling B. Professional identity formation in the transition from medical school to working life: a qualitative study of group-coaching courses for junior doctors. BMC Med Educ. 2016. Jun 24;16:165. doi: 10.1186/s12909-016-0684-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dyrbye LN, Gill PR, Satele DV, West CP. Professional coaching and surgeon well-being. a randomized controlled trial. Ann Surg. 2022; doi: 10.1097/SLA.0000000000005678 [DOI] [PubMed] [Google Scholar]
- 32.Fainstad T, Mann A, Suresh K, Shah P, Dieujuste N, Thurmon K, et al. Effect of a novel online group-coaching program to reduce burnout in female resident physicians: A randomized clinical trial. JAMA Netw Open. 2022. May 2;5(5):e2210752. doi: 10.1001/jamanetworkopen.2022.10752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gardiner M, Kearns H, Tiggemann M. Effectiveness of cognitive behavioural coaching in improving the well-being and retention of rural general practitioners. Aust J Rural Health. 2013. Jun;21(3):183–9. doi: 10.1111/ajr.12033 [DOI] [PubMed] [Google Scholar]
- 34.Kakarala R, Smith SJ, Barreto E, Donelan K, Palamara K. When coaching meets mentoring: impact of incorporating coaching into an existing mentoring program at a community hospital. Cureus. 2018. Aug;10(8):e3138. doi: 10.7759/cureus.3138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McGonagle AK, Schwab L, Yahanda N, Duskey H, Gertz N, Prior L, et al. Coaching for primary care physician well-being: A randomized trial and follow-up analysis. J Occup Health Psychol. 2020. Oct;25(5):297–314. doi: 10.1037/ocp0000180 [DOI] [PubMed] [Google Scholar]
- 36.McKimm J, Povey J. Evaluating the impact of a coaching pilot on the resilience and retention of UK general practitioners. BMJ Lead. 2018. Dec 1;2(4):144–8. https://bmjleader.bmj.com/content/2/4/144 [Google Scholar]
- 37.Palamara K, Kauffman C, Stone VE, Bazari H, Donelan K. Promoting success: A professional development coaching program for interns in medicine. J Grad Med Educ. 2015. Dec;7(4):630–7. doi: 10.4300/JGME-D-14-00791.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Palamara K, Kauffman C, Chang Y, Barreto EA, Yu L, Bazari H, et al. Professional development coaching for residents: results of a 3-year positive psychology coaching intervention. J Gen Intern Med [Internet]. 2018. Nov; 33(11):1842–4. doi: 10.1007/s11606-018-4589-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Palamara K, Chu JT, Chang Y, Yu L, Cosco D, Higgins S, et al. Who benefits most? A multisite study of coaching and resident well-being. J Gen Intern Med. 2021;37(3):539–47. doi: 10.1007/s11606-021-06903-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Palamara K, McKinley SK, Chu JT, Merrill A, Yu L, Parangi S, et al. Impact of a virtual professional development coaching program on the professional fulfillment and well-being of women surgery residents: A randomized controlled trial. Ann Surg. 2022;277(2):188–95. doi: 10.1097/SLA.0000000000005562 [DOI] [PubMed] [Google Scholar]
- 41.Solms L, van Vianen A, Koen J, Theeboom T, de Pagter APJ, De Hoog M, et al. Turning the tide: a quasi-experimental study on a coaching intervention to reduce burn-out symptoms and foster personal resources among medical residents and specialists in the Netherlands. BMJ Open. 2021. Jan 25;11(1):e041708. doi: 10.1136/bmjopen-2020-041708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Song Y, Swendiman RA, Shannon AB, Torres-Landa S, Khan FN, Williams NN, et al. Can we coach resilience? An evaluation of professional resilience coaching as a well-being initiative for surgical interns. J Surg Educ. 2020. Dec;77(6):1481–9. doi: 10.1016/j.jsurg.2020.04.014 [DOI] [PubMed] [Google Scholar]
- 43.Brady KJS, Trockel MT, Khan CT, Raj KS, Murphy ML, Bohman B, et al. What Do we mean by physician wellness? A systematic review of its definition and measurement. Acad Psychiatry. 2018. Feb;42(1):94–108. doi: 10.1007/s40596-017-0781-6 [DOI] [PubMed] [Google Scholar]
- 44.Sudol NT, Guaderrama NM, Honsberger P, Weiss J, Li Q, Whitcomb EL. Prevalence and nature of sexist and racial/ethnic microaggressions against surgeons and anesthesiologists. JAMA Surg. 2021;92618:e210265. doi: 10.1001/jamasurg.2021.0265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Samuels EA, Boatright DH, Wong AH, Cramer LD, Desai MM, Solotke MT, et al. Association between sexual orientation, mistreatment, and burnout among US medical students. JAMA Netw Open [Internet]. 2021. Feb 2 [cited 2022 Dec 19];4(2):e2036136. doi: 10.1001/jamanetworkopen.2020.36136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lu PW, Columbus AB, Fields AC, Melnitchouk N, Cho NL. Gender differences in surgeon burnout and barriers to career satisfaction: A qualitative exploration. J Surg Res. 2019;9:1–6. doi: 10.1016/j.jss.2019.10.045 [DOI] [PubMed] [Google Scholar]
- 47.Rotenstein L, Harry E, Wickner P, Gupte A, Neville BA, Lipsitz S, et al. Contributors to gender differences in burnout and professional fulfillment: A Survey of Physician Faculty. Jt Comm J Qual Patient Saf. 2021. Nov;47(11):723–30. doi: 10.1016/j.jcjq.2021.08.002 [DOI] [PubMed] [Google Scholar]
- 48.Lawrence JA, Davis BA, Corbette T, Hill EV, Williams DR, Reede JY. Racial/Ethnic differences in burnout: A systematic review. J Racial Ethn Health Disparities. 2022. Feb;9(1):257–69. doi: 10.1007/s40615-020-00950-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting information files.