Abstract
Objective
Adolescents’ mental health was severely compromised during the COVID-19 pandemic. Longitudinal real-world studies on changes in the mental health of adolescents during the later phase of the pandemic are limited. We aimed to quantify the effect of COVID-19 pandemic on adolescents’ mental health outcomes based on electronic health records.
Method
This was a retrospective cohort study using the computerized database of a 2.5 million members, state-mandated health organization in Israel. Rates of mental health diagnoses and psychiatric drug dispensations were measured among adolescents 12 to 17 years of age with and without pre-existing mental history, for the years 2017 to 2021. Relative risks were computed between the years, and interrupted time series (ITS) analyses evaluated changes in monthly incidence rates of psychiatric outcomes.
Results
The average population size was 218,146 in 2021. During the COVID-19 period, a 36% increase was observed in the incidence of depression (95% CI = 25-47), 31% in anxiety (95% CI = 23-39), 20% in stress (95% CI = 13-27), 50% in eating disorders (95% CI = 35-67), 25% in antidepressant use (95% CI = 25-33), and 28% in antipsychotic use (95% CI = 18-40). A decreased rate of 26% (95% CI = 0.80-0.88) was observed in ADHD diagnoses. The increase of the examined outcomes was most prominent among youth without psychiatric history, female youth, general secular Jewish population, youth with medium−high socioeconomic status, and those 14 to 15 years of age. ITS analysis confirmed a significantly higher growth in the incidence of psychiatric outcomes during the COVID-19 period, compared to those in previous years.
Conclusion
This real-world study highlights the deterioration of adolescents’ mental health during the COVID-19 pandemic and suggests that youth mental health should be considered during health policy decision making.
Diversity & Inclusion Statement
We worked to ensure sex and gender balance in the recruitment of human participants. We worked to ensure race, ethnic, and/or other types of diversity in the recruitment of human participants. We actively worked to promote sex and gender balance in our author group. The author list of this paper includes contributors from the location and/or community where the research was conducted who participated in the data collection, design, analysis, and/or interpretation of the work.
Key words: mental health, COVID-19, cohort study
The COVID-19 pandemic and measures taken to control its spread have transformed the lives of adolescents, raising concern for their mental health. Although children and adolescents mostly present a milder course of the virus compared to adults, their mental health and well-being have been negatively affected during the pandemic.1 , 2 Recent reports have indicated that depression, anxiety, and eating disorders have increased significantly since the outbreak of COVID-19, with greater increases among female individuals3 , 4 and a gradual association with increasing age.5 However, information regarding the increase in adolescent mental health rates during COVID-19 is still limited and mostly not based on longitudinal follow-up of real-world data population studies.5 Most of the present studies are based on survey data collected during the early phase of the COVID-19 outbreak.3 , 5 A large meta-analysis study concluded that quantitative study designs, based on real-world data, are needed to assess changes in mental health of children and adolescents during the COVID-19 pandemic more accurately and to compare these to previous years.5
The disruption caused by the pandemic was further exacerbated by the steps that were taken to mitigate it, such as 3 full lockdowns in Israel (Table S1, available online), social distancing policies, and quarantine instructions for those exposed and infected by the SARS-CoV-2 virus6 (hereafter referred to as COVID-19). The disruption to the education system affected millions of pupils worldwide despite significant efforts to deploy distance learning. Previous studies have shown that whenever children are not in their educational routine, they become physically less active, exposed to prolonged screen time, have irregular sleep schedules, and have less healthy diets.7 , 8 Furthermore, pandemic stressors such as the threat of the disease, decreased peer interactions, lack of personal space at home, and family financial loss may have even more troublesome and enduring impacts on children’s mental health.7
Adolescents with pre-existing mental health disorders might be especially vulnerable to the effects of COVID-19 containment measures including lockdowns, isolations, and social distancing. Those measures may increase loneliness that was found to be correlated with severity of future mental health outcomes, such as depression and anxiety.9 However, few studies showed that young people with pre-existing depression experienced improvement during lockdowns.10 , 11 Nevertheless, adolescents without pre-existing mental health symptoms showed a deterioration in mental health, which might represent a response to fear from uncertainty due to the COVID-19 pandemic.10, 11, 12
In this study, we quantified the effect of the COVID-19 pandemic on the incidence of Israeli youth mental health outcomes based on comprehensive electronic health record (EHR) data. In addition, this study explored the effect of the COVID-19 pandemic on adolescents with pre-existing mental health diagnoses or prescriptions.
Method
Study Design
We performed a retrospective cohort study design of adolescents 12 to 17 years of age (up to their 18th birthday) between November 1, 2016, and October 31, 2021.
Data in this study originated from Maccabi Healthcare Services (MHS), the second largest Health Maintenance Organization (HMO) in Israel, which includes 2.5 million insured citizens with longitudinal EHRs dating back to 1993. Israel has an advanced public health system, with a wide range of services and technologies available to all residents, mostly free of charge, through the National Health Insurance Law from 1994.13 The Israeli national health insurance law guarantees a universal health care services basket to all Israeli citizens through 4 nationwide health funds.13 Enrollment in a health fund is mandatory, and every citizen is free to choose any of the 4 funds, without any limitations of preconditions or age. Each fund is both the provider and insurer of health care services to its members. Moreover, the data source used for this study is nationally representative as all 4 HMOs share a similar sociodemographic distribution. The data of Maccabi includes psychiatric outpatient visits within the HMO and does not include those who receive psychiatric treatment in private outpatient care, outside of the HMO. Furthermore, the data of this study do not include inpatient mental health treatments. This study was approved by Maccabi Health Services’ institutional review board (MH6-0006-21), and informed consent was waived.
Outcomes
We examined incidence rates of several outcomes associated with mental distress. These included 5 categories of mental health diagnoses: depression (ICD10 F32, F34); anxiety and obsessive-compulsive disorders (ICD10 F41, F42); adjustment and emotional problems, stress-related conditions (ICD10 F43, F93; henceforth denoted as “stress”), eating disorders (ICD10 F50), and attention-deficit/hyperactivity disorder (ADHD) (ICD10 F90). Furthermore, we assessed 4 categories of drugs dispensed during those years: namely, antidepressants (ATC code N06A), anxiolytics (ATC code N05B), antipsychotics (ATC code N05A), and psychostimulants, agents used for ADHD, and nootropics (ATC code N06B; henceforth denoted as “ADHD agents”). These diagnoses and prescriptions were provided by physicians of various specializations in outpatient care clinics within the MHS (see Figure S8, available online). The rates of these mental health outcomes were also quantified in adolescents diagnosed or prescribed with the same outcomes during the 2 years before the index year. For brevity, we henceforth refer to this as “psychiatric history.”
Demographic Variables
We examined trends in mental illness stratified by age subgroups (12-13, 14-15, and 16-17 years of age), sex assigned at birth (male, female), sector (general secular Jewish population, Israeli Arab, and ultra-orthodox Jewish) and socioeconomic status (SES) on a scale from 1 to 10 (categorized into 1-3 = low, 4-7 = medium, and 8-10 = high). SES and population sectors were determined by the participants’ geo-statistical area of residence using Points Location Services Ltd (POINTS), which integrates information from the Israeli Central Bureau of Statistics with other socio-economic and demographic data sources.14 The POINTS scale is routinely used by the Israeli Ministry of Health and all 4 health maintenance organizations.
Individuals with missing sector information (less than 0.01%) and unlisted SES were excluded from the SES subanalysis (1.1%) but were included in all other analyses. Sex and age were listed for all members.
Statistical Analysis
Incidence was computed based on all MHS’ members 12 to 17 years of age at the beginning of the year who did not previously receive a diagnosis or a medication of the type being considered (“cohort at risk”). The number of members who received the measured diagnosis or medication during the year was standardized via division by the size of the “cohort at risk.” Relative risks (RRs) per 1,000 members, 95% CIs, and p values were computed to measure the annual changes in mental illness trends between each 2 consecutive years and between 2 time periods: pre−COVID-19 (year 2019 vs 2017) and during COVID-19 (year 2021 vs 2019). As the year 2020 included a pre-pandemic period in the beginning of the year, followed by the COVID-19 outbreak in March, a period when access to mental health services was severely disrupted, we considered 2021 as the COVID-19 period and 2019 as the pre-pandemic period. RRs were presented overall and stratified by age, sex, sector, and SES. Considering the large population size, the balance between the groups was assessed by standardized mean differences (SMD), and smaller than 0.1 was considered well balanced. Because our data extended to October 31, 2021, each analyzed year started on November 1 of the previous year and ended on October 31. To present the results of the RRs and 95% CIs, we used forest plots. In addition, similar analyses were conducted among adolescents with a psychiatric history.
We used an interrupted time series design (ITS)15 to quantify changes in the level and growth in monthly incident rates before and during the COVID-19 pandemic. ITS is a quasi-experimental design in which the effects of an intervention or event are evaluated by comparing outcome measures obtained at several time intervals before and after the intervention/event occurred.15 The interruption was defined on February 27, 2020, the day that the first case of COVID-19 was detected in Israel. We used linear regression models and included Fourier terms to model the seasonal factors, with a p value <.05 considered statistically significant. Fourier analysis resolves the time dimension variable and allows identification, quantification, and removal of the time-based cycles in the data.15 Statistical analyses were conducted using Python version 3.7.1 and the statsmodels package version 0.12.
Results
The average population of adolescents without psychiatric history was N = 200,824 in 2017, N = 207,703 in 2019, and N = 218,146 in 2021 and consisted of 50.4% male adolescents on average (Table 1 , Table S2, available online). The cohorts slightly differed between outcomes because for each outcome we excluded individuals with a history of that specific outcome. The cohort consisted of 79.8% general secular Jewish population, 12.5% ultra-orthodox Jews, and 7.7% Israeli Arabs (Table S2, available online). Among adolescents with psychiatric history, the size of the population ranged from 1,478 for participants with eating disorders to 32,445 for participants with ADHD diagnoses in 2021 (Table 2 ).
Table 1.
Study Population Characteristics and Incidence Rates of Mental Health Diagnoses and Medications by Year, Diagnoses, and Medications
| Characteristics | Year | Depression |
Anxiety |
Eating disorder |
Stress |
ADHD |
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N population | N incidence | Rate per 1,000 | RR year/ year 1 (95% CI) | p | N population | N incidence | Rate per 1,000 | RR year/ year 1 (95% CI) | p | N population | N incidence | Rate per 1,000 | RR year/ year 1 (95% CI) | p | N population | N incidence | Rate per 1,000 | RR year/ year 1 (95% CI) | p | N population | N incidence | Rate per 1,000 | RR year/ year 1 (95% CI) | p | ||
| Total | ||||||||||||||||||||||||||
| 2017 | 216,121 | 945 | 4.4 | 209,208 | 1,534 | 7.3 | 212,104 | 523 | 2.5 | 201,670 | 2,169 | 10.8 | 158,159 | 3,924 | 24.8 | |||||||||||
| 2018 | 220,668 | 1,005 | 4.6 | 1.04 (0.95-1.14) | .376 | 213,330 | 1,638 | 7.7 | 1.05 (0.97-1.12) | .193 | 216,109 | 559 | 2.6 | 1.05 (0.93-1.18) | .447 | 204,166 | 2,206 | 10.8 | 1.00 (0.94-1.07) | .879 | 159,974 | 3,654 | 22.8 | 0.92 (0.88-0.96) | <.001 | |
| 2019 | 224,552 | 978 | 4.4 | 0.96 (0.87-1.04) | .322 | 216,751 | 1,657 | 7.6 | 1.00 (0.93-1.07) | .903 | 219,590 | 567 | 2.6 | 1.00 (0.88-1.12) | 1.000 | 205,791 | 2,132 | 10.4 | 0.96 (0.90-1.02) | .165 | 162,529 | 3,657 | 22.5 | 0.99 (0.94-1.03) | .523 | |
| 2020 | 230,517 | 1,081 | 4.7 | 1.08 (0.98-1.17) | .093 | 222,127 | 1,839 | 8.3 | 1.08 (1.01-1.16) | .018 | 225,047 | 721 | 3.2 | 1.24 (1.11-1.39) | <.001 | 209,333 | 2,284 | 10.9 | 1.05 (0.99-1.12) | .085 | 166,922 | 3,201 | 19.2 | 0.85 (0.81-0.89) | .000 | |
| 2021 | 236,291 | 1,398 | 5.9 | 1.26 (1.17-1.37) | <.001 | 227,311 | 2,275 | 10.0 | 1.21 (1.14-1.29) | <.001 | 230,499 | 894 | 3.9 | 1.21 (1.10-1.34) | <.001 | 212,331 | 2,632 | 12.4 | 1.14 (1.07-1.20) | <.001 | 172,073 | 3,262 | 19.0 | 0.99 (0.94-1.04) | .642 | |
| Sex | ||||||||||||||||||||||||||
| Male | 2017 | 110,989 | 427 | 3.8 | 107,062 | 749 | 7.0 | 109,179 | 126 | 1.2 | 102,598 | 990 | 9.6 | 73,816 | 1,988 | 26.9 | ||||||||||
| 2018 | 113,307 | 443 | 3.9 | 1.02 (0.89-1.16) | .839 | 109,137 | 791 | 7.2 | 1.04 (0.93-1.14) | .490 | 111,185 | 144 | 1.3 | 1.12 (0.88-1.43) | .361 | 103,829 | 1,014 | 9.8 | 1.01 (0.92-1.10) | .788 | 74,664 | 1,846 | 24.7 | 0.92 (0.86-0.97) | .008 | |
| 2019 | 115,245 | 417 | 3.6 | 0.93 (0.81-1.06) | .260 | 110,750 | 723 | 6.5 | 0.90 (0.81-0.99) | .042 | 112,863 | 124 | 1.1 | 0.85 (0.66-1.08) | .179 | 104,505 | 885 | 8.5 | 0.87 (0.79-0.94) | .002 | 75,835 | 1,850 | 24.4 | 0.99 (0.92-1.05) | .689 | |
| 2020 | 118,088 | 429 | 3.6 | 1.00 (0.87-1.15) | .973 | 113,309 | 794 | 7.0 | 1.07 (0.97-1.19) | .172 | 115,454 | 150 | 1.3 | 1.18 (0.93-1.50) | .183 | 106,046 | 971 | 9.2 | 1.08 (0.98-1.18) | .093 | 77,803 | 1,552 | 19.9 | 0.82 (0.76-0.87) | <.001 | |
| 2021 | 120,988 | 447 | 3.7 | 1.02 (0.89-1.16) | .813 | 115,801 | 941 | 8.1 | 1.16 (1.06-1.27) | .002 | 118,174 | 153 | 1.3 | 1.00 (0.79-1.25) | 1.000 | 107,329 | 991 | 9.2 | 1.01 (0.92-1.10) | .856 | 80,338 | 1,504 | 18.7 | 0.94 (0.87-1.01) | .079 | |
| Female | 2017 | 105,132 | 518 | 4.9 | 102,146 | 785 | 7.7 | 102,925 | 397 | 3.9 | 99,072 | 1,179 | 11.9 | 84,343 | 1,936 | 23.0 | ||||||||||
| 2018 | 107,361 | 562 | 5.2 | 1.06 (0.94-1.20) | .329 | 104,193 | 847 | 8.1 | 1.06 (0.96-1.17) | .263 | 104,924 | 415 | 4.0 | 1.03 (0.89-1.18) | .725 | 100,337 | 1,192 | 11.9 | 1.00 (0.92-1.08) | .984 | 85,310 | 1,808 | 21.2 | 0.92 (0.86-0.98) | .014 | |
| 2019 | 109,307 | 561 | 5.1 | 0.98 (0.87-1.10) | .742 | 106,001 | 934 | 8.8 | 1.08 (0.98-1.19) | .091 | 106,727 | 443 | 4.2 | 1.05 (0.91-1.20) | .494 | 101,286 | 1,247 | 12.3 | 1.04 (0.95-1.12) | .381 | 86,694 | 1,807 | 20.8 | 0.98 (0.92-1.05) | .614 | |
| 2020 | 112,429 | 652 | 5.8 | 1.13 (1.01-1.26) | .036 | 108,818 | 1,045 | 9.6 | 1.09 (0.99-1.19) | .055 | 109,593 | 571 | 5.2 | 1.26 (1.11-1.42) | <.001 | 103,287 | 1,313 | 12.7 | 1.03 (0.95-1.12) | .426 | 89,119 | 1,649 | 18.5 | 0.89 (0.83-0.94) | <.001 | |
| 2021 | 115,303 | 951 | 8.2 | 1.42 (1.29-1.57) | <.001 | 111,510 | 1,334 | 12.0 | 1.25 (1.15-1.35) | <.001 | 112,325 | 741 | 6.6 | 1.27 (1.14-1.41) | <.001 | 105,002 | 1,641 | 15.6 | 1.23 (1.14-1.32) | <.001 | 91,735 | 1,758 | 19.2 | 1.04 (0.96-1.11) | .307 | |
| Age groups | ||||||||||||||||||||||||||
| 12-13 years old | 2017 | 74,563 | 219 | 2.9 | 72,386 | 450 | 6.2 | 72,594 | 188 | 2.6 | 69,296 | 833 | 12.0 | 55,799 | 1,603 | 28.7 | ||||||||||
| 2018 | 75,226 | 222 | 3.0 | 1.00 (0.83-1.21) | .962 | 72,962 | 483 | 6.6 | 1.06 (0.93-1.21) | .341 | 73,162 | 181 | 2.5 | 0.96 (0.77-1.17) | .677 | 69,227 | 820 | 11.8 | 0.99 (0.89-1.09) | .767 | 55,881 | 1,481 | 26.5 | 0.92 (0.86-0.99) | .024 | |
| 2019 | 75,907 | 214 | 2.8 | 0.96 (0.79-1.15) | .666 | 73,494 | 502 | 6.8 | 1.03 (0.91-1.17) | .632 | 73,804 | 181 | 2.5 | 0.99 (0.80-1.22) | .958 | 68,944 | 772 | 11.2 | 0.95 (0.85-1.04) | .267 | 56,567 | 1,375 | 24.3 | 0.92 (0.85-0.98) | .020 | |
| 2020 | 78,036 | 230 | 2.9 | 1.05 (0.86-1.26) | .669 | 75,369 | 539 | 7.2 | 1.05 (0.92-1.18) | .474 | 75,935 | 223 | 2.9 | 1.20 (0.98-1.46) | .073 | 70,082 | 777 | 11.1 | 0.99 (0.89-1.09) | .858 | 58,521 | 1,256 | 21.5 | 0.88 (0.81-0.95) | .001 | |
| 2021 | 81,247 | 338 | 4.2 | 1.41 (1.19-1.67) | <.001 | 78,300 | 667 | 8.5 | 1.19 (1.06-1.33) | .002 | 79,002 | 275 | 3.5 | 1.19 (0.99-1.41) | .059 | 72,176 | 936 | 13.0 | 1.17 (1.06-1.29) | .001 | 61,447 | 1,333 | 21.7 | 1.01 (0.93-1.09) | .796 | |
| 14-15 years old | 2017 | 71,692 | 300 | 4.2 | 69,327 | 487 | 7.0 | 70,374 | 206 | 2.9 | 66,829 | 687 | 10.3 | 52,167 | 1,449 | 27.8 | ||||||||||
| 2018 | 73,843 | 341 | 4.6 | 1.10 (0.94-1.29) | .220 | 71,306 | 558 | 7.8 | 1.11 (0.98-1.26) | .082 | 72,117 | 209 | 2.9 | 0.99 (0.81-1.20) | .922 | 68,283 | 700 | 10.3 | 1.00 (0.89-1.11) | .978 | 53,416 | 1,328 | 24.9 | 0.90 (0.83-0.96) | .003 | |
| 2019 | 75,910 | 317 | 4.2 | 0.90 (0.77-1.05) | .197 | 73,264 | 534 | 7.3 | 0.93 (0.82-1.05) | .248 | 74,070 | 216 | 2.9 | 1.01 (0.83-1.22) | .961 | 69,619 | 695 | 10.0 | 0.97 (0.87-1.08) | .628 | 54,742 | 1,440 | 26.3 | 1.06 (0.98-1.14) | .133 | |
| 2020 | 77,165 | 389 | 5.0 | 1.21 (1.04-1.40) | .013 | 74,396 | 600 | 8.1 | 1.11 (0.98-1.24) | .089 | 75,200 | 269 | 3.6 | 1.23 (1.03-1.47) | .026 | 70,163 | 770 | 11.0 | 1.10 (0.99-1.22) | .070 | 55,511 | 1,168 | 21.0 | 0.80 (0.74-0.86) | <.001 | |
| 2021 | 77,825 | 485 | 6.2 | 1.24 (1.08-1.41) | .002 | 74,891 | 751 | 10.0 | 1.24 (1.12-1.38) | <.001 | 75,807 | 354 | 4.7 | 1.31 (1.11-1.53) | .001 | 69,895 | 899 | 12.9 | 1.17 (1.06-1.29) | .001 | 56,428 | 1,217 | 21.6 | 1.03 (0.94-1.11) | .548 | |
| 16-17 years old | 2017 | 69,866 | 426 | 6.1 | 67,495 | 597 | 8.8 | 69,136 | 129 | 1.9 | 65,545 | 649 | 9.9 | 50,193 | 872 | 17.4 | ||||||||||
| 2018 | 71,599 | 442 | 6.2 | 1.01 (0.88-1.16) | .865 | 69,062 | 597 | 8.6 | 0.98 (0.87-1.09) | .706 | 70,830 | 169 | 2.4 | 1.28 (1.02-1.61) | .037 | 66,656 | 686 | 10.3 | 1.04 (0.93-1.16) | .492 | 50,677 | 845 | 16.7 | 0.96 (0.87-1.06) | .394 | |
| 2019 | 72,735 | 447 | 6.1 | 1.00 (0.87-1.14) | .973 | 69,993 | 621 | 8.9 | 1.03 (0.91-1.15) | .666 | 71,716 | 170 | 2.4 | 0.99 (0.80-1.23) | .957 | 67,228 | 665 | 9.9 | 0.96 (0.86-1.07) | .477 | 51,220 | 842 | 16.4 | 0.99 (0.89-1.08) | .787 | |
| 2020 | 75,316 | 462 | 6.1 | 1.00 (0.87-1.14) | 1.000 | 72,362 | 700 | 9.7 | 1.09 (0.97-1.21) | .115 | 73,912 | 229 | 3.1 | 1.31 (1.07-1.59) | .008 | 69,088 | 737 | 10.7 | 1.08 (0.97-1.20) | .163 | 52,890 | 777 | 14.7 | 0.89 (0.81-0.98) | .024 | |
| 2021 | 77,219 | 575 | 7.4 | 1.21 (1.07-1.37) | .002 | 74,120 | 857 | 11.6 | 1.20 (1.08-1.32) | <.001 | 75,690 | 265 | 3.5 | 1.13 (0.94-1.35) | .177 | 70,260 | 797 | 11.3 | 1.06 (0.96-1.18) | .228 | 54,198 | 712 | 13.1 | 0.89 (0.80-0.99) | .030 | |
| Sector | ||||||||||||||||||||||||||
| General Jewish | 2017 | 174,062 | 851 | 4.9 | 167,906 | 1,336 | 8.0 | 170,742 | 470 | 2.8 | 160,951 | 1,895 | 11.8 | 123,540 | 3,424 | 27.7 | ||||||||||
| 2018 | 177,600 | 900 | 5.1 | 1.04 (0.94-1.14) | .458 | 171,070 | 1,456 | 8.5 | 1.07 (0.99-1.15) | .077 | 173,872 | 506 | 2.9 | 1.06 (0.93-1.20) | .387 | 162,749 | 1,952 | 12.0 | 1.02 (0.95-1.09) | .570 | 124,945 | 3,187 | 25.5 | 0.92 (0.87-0.96) | .001 | |
| 2019 | 180,155 | 876 | 4.9 | 0.96 (0.87-1.05) | .392 | 173,174 | 1,500 | 8.7 | 1.02 (0.94-1.09) | .644 | 176,131 | 514 | 2.9 | 1.00 (0.88-1.13) | .975 | 163,327 | 1,860 | 11.4 | 0.95 (0.89-1.01) | .110 | 126,440 | 3,167 | 25.0 | 0.98 (0.93-1.03) | .469 | |
| 2020 | 185,019 | 979 | 5.3 | 1.09 (0.99-1.19) | .069 | 177,481 | 1,655 | 9.3 | 1.08 (1.00-1.15) | .038 | 180,607 | 682 | 3.8 | 1.29 (1.15-1.45) | <.001 | 166,137 | 1,987 | 12.0 | 1.05 (0.98-1.12) | .127 | 130,139 | 2,797 | 21.5 | 0.86 (0.81-0.90) | <.001 | |
| 2021 | 189,689 | 1,305 | 6.9 | 1.30 (1.20-1.41) | <.001 | 181,615 | 2,043 | 11.2 | 1.21 (1.13-1.29) | <.001 | 185,017 | 832 | 4.5 | 1.19 (1.08-1.32) | .001 | 168,472 | 2,312 | 13.7 | 1.15 (1.08-1.22) | <.001 | 134,397 | 2,776 | 20.7 | 0.96 (0.91-1.01) | .136 | |
| Ultra-orthodox Jewish | 2017 | 26,314 | 69 | 2.6 | 25,830 | 149 | 5.8 | 25,705 | 36 | 1.4 | 25,562 | 177 | 6.9 | 20,911 | 386 | 18.5 | ||||||||||
| 2018 | 27,045 | 76 | 2.8 | 1.07 (0.77-1.48) | .740 | 26,502 | 124 | 4.7 | 0.81 (0.63-1.03) | .089 | 26,313 | 43 | 1.6 | 1.17 (0.74-1.82) | .502 | 26,039 | 177 | 6.8 | 0.98 (0.79-1.21) | .873 | 21,163 | 384 | 18.1 | 0.98 (0.85-1.13) | .827 | |
| 2019 | 27,423 | 73 | 2.7 | 0.95 (0.68-1.31) | .744 | 26,852 | 114 | 4.2 | 0.91 (0.70-1.17) | .475 | 26,563 | 43 | 1.6 | 0.99 (0.64-1.51) | 1.000 | 26,162 | 184 | 7.0 | 1.03 (0.84-1.27) | .752 | 21,207 | 387 | 18.2 | 1.01 (0.87-1.16) | .942 | |
| 2020 | 28,405 | 65 | 2.3 | 0.86 (0.61-1.20) | .395 | 27,790 | 141 | 5.1 | 1.20 (0.93-1.53) | .167 | 27,425 | 30 | 1.1 | 0.68 (0.42-1.08) | .102 | 26,824 | 213 | 7.9 | 1.13 (0.92-1.38) | .227 | 21,811 | 287 | 13.2 | 0.72 (0.61-0.84) | <.001 | |
| 2021 | 29,541 | 68 | 2.3 | 1.01 (0.71-1.41) | 1.000 | 28,862 | 161 | 5.6 | 1.10 (0.87-1.38) | .420 | 28,499 | 41 | 1.4 | 1.32 (0.82-2.11) | .285 | 27,588 | 223 | 8.1 | 1.02 (0.84-1.23) | .885 | 22,728 | 383 | 16.9 | 1.28 (1.10-1.49) | .001 | |
| Arab | 2017 | 15,745 | 25 | 1.6 | 15,472 | 49 | 3.2 | 15,657 | 17 | 1.1 | 15,157 | 97 | 6.4 | 13,708 | 114 | 8.3 | ||||||||||
| 2018 | 16,023 | 29 | 1.8 | 1.14 (0.66-1.95) | .684 | 15,758 | 58 | 3.7 | 1.16 (0.79-1.70) | .441 | 15,924 | 10 | 0.6 | 0.58 (0.26-1.26) | .181 | 15,378 | 77 | 5.0 | 0.78 (0.58-1.06) | .111 | 13,866 | 83 | 6.0 | 0.72 (0.54-0.95) | .022 | |
| 2019 | 16,974 | 29 | 1.7 | 0.94 (0.56-1.58) | .896 | 16,725 | 43 | 2.6 | 0.70 (0.47-1.04) | .074 | 16,896 | 10 | 0.6 | 0.94 (0.39-2.26) | 1.000 | 16,302 | 88 | 5.4 | 1.08 (0.79-1.46) | .640 | 14,882 | 103 | 6.9 | 1.16 (0.86-1.54) | .339 | |
| 2020 | 17,093 | 37 | 2.2 | 1.27 (0.77-2.06) | .389 | 16,856 | 43 | 2.6 | 0.99 (0.65-1.51) | 1.000 | 17,015 | 9 | 0.5 | 0.89 (0.36-2.20) | .823 | 16,372 | 84 | 5.1 | 0.95 (0.70-1.28) | .760 | 14,972 | 117 | 7.8 | 1.13 (0.86-1.47) | .380 | |
| 2021 | 17,061 | 25 | 1.5 | 0.68 (0.40-1.12) | .162 | 16,834 | 71 | 4.2 | 1.65 (1.13-2.41) | .009 | 16,983 | 21 | 1.2 | 2.34 (1.07-5.10) | .029 | 16,271 | 97 | 6.0 | 1.16 (0.86-1.56) | .333 | 14,948 | 103 | 6.9 | 0.88 (0.67-1.15) | .379 | |
| Socioeconomic status | ||||||||||||||||||||||||||
| Low (1-3) | 2017 | 26,273 | 70 | 2.7 | 25,706 | 120 | 4.7 | 25,881 | 46 | 1.8 | 25,253 | 174 | 6.9 | 21,351 | 282 | 13.2 | ||||||||||
| 2018 | 27,015 | 72 | 2.7 | 1.00 (0.72-1.39) | 1.000 | 26,448 | 115 | 4.3 | 0.93 (0.72-1.20) | .601 | 26,559 | 39 | 1.5 | 0.83 (0.53-1.27) | .387 | 25,836 | 193 | 7.5 | 1.08 (0.88-1.33) | .463 | 21,737 | 280 | 12.9 | 0.98 (0.82-1.15) | .767 | |
| 2019 | 28,143 | 64 | 2.3 | 0.85 (0.60-1.19) | .391 | 27,569 | 100 | 3.6 | 0.83 (0.63-1.09) | .194 | 27,643 | 29 | 1.0 | 0.71 (0.44-1.16) | .183 | 26,778 | 181 | 6.8 | 0.90 (0.73-1.11) | .350 | 22,745 | 278 | 12.2 | 0.95 (0.80-1.12) | .551 | |
| 2020 | 28,692 | 77 | 2.7 | 1.18 (0.84-1.64) | .354 | 28,099 | 130 | 4.6 | 1.28 (0.98-1.66) | .074 | 28,156 | 23 | 0.8 | 0.78 (0.45-1.35) | .407 | 27,149 | 227 | 8.4 | 1.24 (1.02-1.50) | .033 | 23,122 | 225 | 9.7 | 0.80 (0.66-0.94) | .011 | |
| 2021 | 29,215 | 76 | 2.6 | 0.97 (0.70-1.33) | .872 | 28,599 | 155 | 5.4 | 1.17 (0.92-1.48) | .191 | 28,674 | 37 | 1.3 | 1.58 (0.93-2.66) | .093 | 27,398 | 231 | 8.4 | 1.01 (0.84-1.21) | .963 | 23,584 | 264 | 11.2 | 1.15 (0.96-1.37) | .122 | |
| Medium (4-7) | 2017 | 138,133 | 656 | 4.7 | 133,473 | 1,048 | 7.9 | 135,352 | 342 | 2.5 | 128,074 | 1,516 | 11.8 | 99,492 | 2,520 | 25.3 | ||||||||||
| 2018 | 140,250 | 672 | 4.8 | 1.01 (0.90-1.12) | .891 | 135,291 | 1,111 | 8.2 | 1.05 (0.96-1.14) | .300 | 137,122 | 383 | 2.8 | 1.11 (0.95-1.28) | .181 | 128,781 | 1,549 | 12.0 | 1.02 (0.94-1.09) | .663 | 99,946 | 2,284 | 22.9 | 0.90 (0.85-0.95) | <.001 | |
| 2019 | 141,445 | 641 | 4.5 | 0.95 (0.84-1.05) | .319 | 136,173 | 1,107 | 8.1 | 0.99 (0.91-1.08) | .815 | 138,060 | 378 | 2.7 | 0.98 (0.85-1.13) | .799 | 128,413 | 1,482 | 11.5 | 0.96 (0.89-1.03) | .257 | 100,311 | 2,336 | 23.3 | 1.02 (0.96-1.08) | .522 | |
| 2020 | 144,692 | 750 | 5.2 | 1.14 (1.03-1.27) | .012 | 139,033 | 1,239 | 8.9 | 1.10 (1.01-1.19) | .026 | 140,963 | 487 | 3.5 | 1.26 (1.10-1.44) | .001 | 129,947 | 1,539 | 11.8 | 1.03 (0.95-1.10) | .475 | 102,594 | 1,972 | 19.2 | 0.83 (0.77-0.87) | <.001 | |
| 2021 | 147,839 | 969 | 6.6 | 1.26 (1.15-1.39) | <.001 | 141,809 | 1,522 | 10.7 | 1.20 (1.12-1.30) | <.001 | 143,872 | 585 | 4.1 | 1.18 (1.04-1.33) | .008 | 131,243 | 1,794 | 13.7 | 1.15 (1.08-1.24) | <.001 | 105,323 | 1,952 | 18.5 | 0.96 (0.90-1.03) | .252 | |
| High (8-10) | 2017 | 51,128 | 218 | 4.3 | 49,463 | 363 | 7.3 | 50,300 | 132 | 2.6 | 47,787 | 475 | 9.9 | 36,857 | 1,118 | 30.3 | ||||||||||
| 2018 | 52,743 | 258 | 4.9 | 1.15 (0.95-1.37) | .141 | 50,952 | 407 | 8.0 | 1.09 (0.94-1.25) | .247 | 51,783 | 137 | 2.6 | 1.01 (0.79-1.28) | .951 | 48,927 | 455 | 9.3 | 0.94 (0.82-1.06) | .323 | 37,767 | 1,080 | 28.6 | 0.94 (0.86-1.02) | .166 | |
| 2019 | 54,216 | 272 | 5.0 | 1.03 (0.86-1.22) | .794 | 52,282 | 444 | 8.5 | 1.06 (0.92-1.22) | .371 | 53,149 | 160 | 3.0 | 1.14 (0.90-1.43) | .270 | 49,898 | 463 | 9.3 | 1.00 (0.87-1.14) | 1.000 | 38,859 | 1,033 | 26.6 | 0.93 (0.85-1.01) | .089 | |
| 2020 | 56,274 | 247 | 4.4 | 0.87 (0.73-1.04) | .135 | 54,159 | 463 | 8.5 | 1.01 (0.88-1.15) | .947 | 55,078 | 205 | 3.7 | 1.24 (1.01-1.52) | .046 | 51,433 | 507 | 9.9 | 1.06 (0.93-1.20) | .350 | 40,482 | 991 | 24.5 | 0.92 (0.84-1.00) | .062 | |
| 2021 | 58,247 | 348 | 6.0 | 1.36 (1.16-1.60) | <.001 | 55,934 | 583 | 10.4 | 1.22 (1.08-1.38) | .001 | 56,969 | 268 | 4.7 | 1.26 (1.05-1.52) | .011 | 52,765 | 593 | 11.2 | 1.14 (1.01-1.28) | .031 | 42,312 | 1,034 | 24.4 | 1.00 (0.91-1.09) | .982 | |
| Characteristics | Year | Antidepressant |
Anxiolytic |
Antipsychotic |
ADHD agents |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population N |
Incidence n | Rate per 1,000 | RR year/ year 1 (95% CI) | p Value | Population N |
Incidence n | Rate per 1,000 | RR year/year 1 (95% CI) | p Value | Population N |
Incidence n | Rate per 1,000 | RR year/ year 1 (95% CI) | p Value | Population N |
Incidence n | Rate per 1,000 | RR year/ year 1 (95% CI) | p Value | ||
| Total | |||||||||||||||||||||
| 2017 | 212,163 | 1,787 | 8.4 | 215,824 | 539 | 2.5 | 212,741 | 850 | 4.0 | 169,423 | 4,886 | 28.8 | |||||||||
| 2018 | 216,569 | 1,943 | 9.0 | 1.07 (0.99-1.14) | .054 | 220,652 | 488 | 2.2 | 0.89 (0.78-1.00) | .053 | 216,937 | 877 | 4.0 | 1.01 (0.92-1.11) | .810 | 171,754 | 4,734 | 27.6 | 0.96 (0.91-0.99) | .025 | |
| 2019 | 220,245 | 2,054 | 9.3 | 1.04 (0.97-1.11) | .221 | 224,870 | 509 | 2.3 | 1.02 (0.90-1.16) | .727 | 220,544 | 983 | 4.5 | 1.10 (1.01-1.21) | .036 | 174,454 | 4,677 | 26.8 | 0.97 (0.93-1.01) | .174 | |
| 2020 | 225,826 | 2,198 | 9.7 | 1.04 (0.98-1.11) | .165 | 231,124 | 497 | 2.2 | 0.95 (0.84-1.07) | .430 | 226,158 | 1,069 | 4.7 | 1.06 (0.97-1.16) | .184 | 179,053 | 4,193 | 23.4 | 0.87 (0.83-0.91) | <.001 | |
| 2021 | 231,381 | 2,706 | 11.7 | 1.20 (1.14-1.27) | <.001 | 237,292 | 572 | 2.4 | 1.12 (0.99-1.26) | .066 | 231,593 | 1,326 | 5.7 | 1.21 (1.12-1.31) | <.001 | 184,540 | 4,453 | 24.1 | 1.03 (0.98-1.07) | .160 | |
| Sex | |||||||||||||||||||||
| Male | 2017 | 108,504 | 832 | 7.7 | 110,806 | 241 | 2.2 | 107,907 | 498 | 4.6 | 81,001 | 2,474 | 30.5 | ||||||||
| 2018 | 110,798 | 932 | 8.4 | 1.10 (0.99-1.20) | .053 | 113,272 | 208 | 1.8 | 0.84 (0.70-1.02) | .080 | 109,966 | 511 | 4.6 | 1.01 (0.89-1.14) | .925 | 82,071 | 2,357 | 28.7 | 0.94 (0.88-0.99) | .031 | |
| 2019 | 112,594 | 957 | 8.5 | 1.01 (0.92-1.11) | .835 | 115,366 | 207 | 1.8 | 0.98 (0.80-1.18) | .844 | 111,631 | 578 | 5.2 | 1.11 (0.98-1.26) | .078 | 83,246 | 2,295 | 27.6 | 0.96 (0.90-1.02) | .158 | |
| 2020 | 115,235 | 935 | 8.1 | 0.95 (0.87-1.04) | .321 | 118,310 | 238 | 2.0 | 1.12 (0.93-1.35) | .236 | 114,177 | 565 | 4.9 | 0.96 (0.85-1.07) | .458 | 85,409 | 1,918 | 22.5 | 0.81 (0.76-0.86) | <.001 | |
| 2021 | 118,047 | 1,086 | 9.2 | 1.13 (1.04-1.24) | .005 | 121,341 | 230 | 1.9 | 0.94 (0.78-1.13) | .548 | 116,821 | 618 | 5.3 | 1.07 (0.95-1.20) | .256 | 88,125 | 1,884 | 21.4 | 0.95 (0.89-1.01) | .127 | |
| Female | 2017 | 103,659 | 955 | 9.2 | 105,018 | 298 | 2.8 | 104,834 | 352 | 3.4 | 88,422 | 2,412 | 27.3 | ||||||||
| 2018 | 105,771 | 1,011 | 9.6 | 1.04 (0.95-1.13) | .415 | 107,380 | 280 | 2.6 | 0.92 (0.78-1.08) | .318 | 106,971 | 366 | 3.4 | 1.02 (0.88-1.18) | .823 | 89,683 | 2,377 | 26.5 | 0.97 (0.91-1.03) | .319 | |
| 2019 | 107,651 | 1,097 | 10.2 | 1.07 (0.97-1.16) | .142 | 109,504 | 302 | 2.8 | 1.06 (0.89-1.24) | .507 | 108,913 | 405 | 3.7 | 1.09 (0.94-1.25) | .249 | 91,208 | 2,382 | 26.1 | 0.99 (0.93-1.04) | .607 | |
| 2020 | 110,591 | 1,263 | 11.4 | 1.12 (1.03-1.22) | .006 | 112,814 | 259 | 2.3 | 0.83 (0.70-0.98) | .031 | 111,981 | 504 | 4.5 | 1.21 (1.06-1.38) | .004 | 93,644 | 2,275 | 24.3 | 0.93 (0.87-0.98) | .013 | |
| 2021 | 113,334 | 1,620 | 14.3 | 1.25 (1.16-1.35) | <.001 | 115,951 | 342 | 2.9 | 1.28 (1.09-1.51) | .002 | 114,772 | 708 | 6.2 | 1.37 (1.22-1.54) | <.001 | 96,415 | 2,569 | 26.6 | 1.10 (1.04-1.16) | .001 | |
| Age groups | |||||||||||||||||||||
| 12-13 years old | 2017 | 73609 | 436 | 5.9 | 74,351 | 71 | 1.0 | 73,193 | 268 | 3.7 | 60,395 | 1,789 | 29.6 | ||||||||
| 2018 | 74281 | 467 | 6.3 | 1.06 (0.93-1.21) | .385 | 75,109 | 74 | 1.0 | 1.03 (0.74-1.43) | .868 | 73,774 | 255 | 3.5 | 0.94 (0.79-1.12) | .512 | 60,738 | 1,698 | 28.0 | 0.94 (0.88-1.01) | .086 | |
| 2019 | 74974 | 537 | 7.2 | 1.14 (1.01-1.29) | .040 | 75,875 | 70 | 0.9 | 0.94 (0.67-1.30) | .739 | 74,360 | 294 | 4.0 | 1.14 (0.96-1.35) | .124 | 61,305 | 1,643 | 26.8 | 0.96 (0.89-1.03) | .219 | |
| 2020 | 76998 | 557 | 7.2 | 1.01 (0.89-1.14) | .879 | 78,081 | 63 | 0.8 | 0.87 (0.62-1.23) | .488 | 76,479 | 307 | 4.0 | 1.02 (0.86-1.19) | .870 | 63,206 | 1,416 | 22.4 | 0.84 (0.77-0.89) | <.001 | |
| 2021 | 80126 | 676 | 8.4 | 1.17 (1.04-1.30) | .007 | 81,363 | 83 | 1.0 | 1.26 (0.91-1.75) | .185 | 79,590 | 352 | 4.4 | 1.1 (0.94-1.28) | .226 | 66,260 | 1,496 | 22.6 | 1.01 (0.93-1.08) | .837 | |
| 14-15 years old | 2017 | 70412 | 576 | 8.2 | 71,562 | 158 | 2.2 | 70,550 | 289 | 4.1 | 56,031 | 1,718 | 30.7 | ||||||||
| 2018 | 72479 | 700 | 9.7 | 1.18 (1.06-1.32) | .003 | 73,766 | 127 | 1.7 | 0.78 (0.61-0.98) | .038 | 72,521 | 313 | 4.3 | 1.05 (0.89-1.24) | .540 | 57,316 | 1,701 | 29.7 | 0.97 (0.90-1.04) | .339 | |
| 2019 | 74450 | 684 | 9.2 | 0.95 (0.85-1.06) | .358 | 76,027 | 128 | 1.7 | 0.98 (0.76-1.25) | .900 | 74,508 | 326 | 4.4 | 1.01 (0.86-1.18) | .874 | 58,836 | 1,723 | 29.3 | 0.99 (0.92-1.06) | .703 | |
| 2020 | 75628 | 696 | 9.2 | 1.00 (0.90-1.11) | .978 | 77,375 | 143 | 1.8 | 1.10 (0.86-1.39) | .466 | 75,631 | 347 | 4.6 | 1.05 (0.90-1.22) | .562 | 59,850 | 1,448 | 24.2 | 0.83 (0.77-0.88) | <.001 | |
| 2021 | 76253 | 928 | 12.2 | 1.32 (1.2-1.46) | <.001 | 78,170 | 141 | 1.8 | 0.98 (0.77-1.23) | .859 | 76,189 | 459 | 6.0 | 1.31 (1.14-1.51) | <.001 | 60,644 | 1,605 | 26.5 | 1.09 (1.02-1.17) | .013 | |
| 16-17 years old | 2017 | 68142 | 775 | 11.4 | 69,911 | 310 | 4.4 | 68,998 | 293 | 4.2 | 52,997 | 1,379 | 26.0 | ||||||||
| 2018 | 69809 | 776 | 11.1 | 0.98 (0.88-1.08) | .664 | 71,777 | 287 | 4.0 | 0.90 (0.76-1.06) | .218 | 70,642 | 309 | 4.4 | 1.03 (0.87-1.21) | .744 | 53,700 | 1,335 | 24.9 | 0.96 (0.88-1.03) | .236 | |
| 2019 | 70821 | 833 | 11.8 | 1.06 (0.96-1.17) | .259 | 72,968 | 311 | 4.3 | 1.07 (0.90-1.25) | .437 | 71,676 | 363 | 5.1 | 1.16 (0.99-1.35) | .058 | 54,313 | 1,311 | 24.1 | 0.97 (0.90-1.05) | .443 | |
| 2020 | 73200 | 945 | 12.9 | 1.10 (1.00-1.20) | .050 | 75,668 | 291 | 3.8 | 0.90 (0.76-1.06) | .220 | 74,048 | 415 | 5.6 | 1.11 (0.96-1.27) | .161 | 55,997 | 1,329 | 23.7 | 0.98 (0.91-1.06) | .665 | |
| 2021 | 75002 | 1102 | 14.7 | 1.14 (1.04-1.24) | .003 | 77,759 | 348 | 4.5 | 1.16 (0.99-1.36) | .057 | 75,814 | 515 | 6.8 | 1.21 (1.07-1.38) | .003 | 57,636 | 1,352 | 23.5 | 0.99 (0.91-1.07) | .769 | |
| Sector | |||||||||||||||||||||
| General Jewish | 2017 | 170,748 | 1,582 | 9.3 | 173,941 | 461 | 2.7 | 171,296 | 659 | 3.8 | 133,344 | 4,168 | 30.9 | 0.96 (0.91-0.99) | .036 | ||||||
| 2018 | 174,114 | 1,707 | 9.8 | 1.06 (0.98-1.13) | .107 | 177,737 | 409 | 2.3 | 0.87 (0.76-0.99) | .038 | 174,559 | 670 | 3.8 | 1.00 (0.89-1.11) | .978 | 135,086 | 4,064 | 29.7 | 0.96 (0.92-1.01) | .089 | |
| 2019 | 176,479 | 1,794 | 10.2 | 1.04 (0.97-1.11) | .285 | 180,585 | 431 | 2.4 | 1.04 (0.90-1.19) | .604 | 176,880 | 748 | 4.2 | 1.10 (0.99-1.22) | .070 | 136,686 | 3,692 | 26.3 | 0.88 (0.84-0.92) | <.001 | |
| 2020 | 181,047 | 1,951 | 10.8 | 1.06 (0.99-1.13) | .073 | 185,714 | 413 | 2.2 | 0.93 (0.81-1.07) | .318 | 181,497 | 851 | 4.7 | 1.11 (1.01-1.22) | .040 | 140,548 | 3,870 | 26.7 | 1.02 (0.97-1.06) | .499 | |
| 2021 | 185,511 | 2,432 | 13.1 | 1.22 (1.15-1.29) | <.001 | 190,761 | 499 | 2.6 | 1.18 (1.03-1.34) | .015 | 185,885 | 1,056 | 5.7 | 1.21 (1.11-1.33) | <.001 | 145,076 | |||||
| Ultra-orthodox Jewish | 2017 | 25,818 | 171 | 6.6 | 26,204 | 56 | 2.1 | 25,792 | 170 | 6.6 | 21,719 | 460 | 21.2 | ||||||||
| 2018 | 26,549 | 206 | 7.8 | 1.17 (0.95-1.43) | .134 | 26,944 | 47 | 1.7 | 0.82 (0.55-1.20) | .325 | 26,456 | 185 | 7.0 | 1.06 (0.86-1.31) | .595 | 22,051 | 477 | 21.6 | 1.02 (0.89-1.16) | .766 | |
| 2019 | 26,884 | 221 | 8.2 | 1.06 (0.87-1.28) | .560 | 27,339 | 50 | 1.8 | 1.05 (0.70-1.56) | .839 | 26,771 | 214 | 8.0 | 1.14 (0.93-1.39) | .191 | 22,142 | 497 | 22.4 | 1.04 (0.91-1.18) | .582 | |
| 2020 | 27,769 | 192 | 6.9 | 0.84 (0.69-1.02) | .084 | 28,322 | 68 | 2.4 | 1.31 (0.91-1.89) | .167 | 27,654 | 189 | 6.8 | 0.85 (0.70-1.04) | .121 | 22,750 | 382 | 16.8 | 0.75 (0.65-0.85) | <.001 | |
| 2021 | 28,891 | 226 | 7.8 | 1.13 (0.93-1.37) | .220 | 29,464 | 52 | 1.8 | 0.74 (0.51-1.05) | .100 | 28,727 | 237 | 8.3 | 1.21 (0.99-1.46) | .058 | 23,697 | 463 | 19.5 | 1.16 (1.02-1.33) | .029 | |
| Arab | 2017 | 15,597 | 34 | 2.2 | 15,679 | 22 | 1.4 | 15,653 | 21 | 1.3 | 14,360 | 122 | 8.5 | ||||||||
| 2018 | 15,906 | 30 | 1.9 | 0.87 (0.53-1.41) | .617 | 15,971 | 32 | 2.0 | 1.43 (0.83-2.46) | .221 | 15,922 | 22 | 1.4 | 1.03 (0.56-1.87) | 1.000 | 14,617 | 89 | 6.1 | 0.72 (0.54-0.94) | .019 | |
| 2019 | 16,882 | 39 | 2.3 | 1.22 (0.76-1.97) | .470 | 16,946 | 28 | 1.7 | 0.82 (0.49-1.37) | .519 | 16,893 | 21 | 1.2 | 0.90 (0.49-1.64) | .762 | 15,626 | 116 | 7.4 | 1.22 (0.92-1.61) | .161 | |
| 2020 | 17,010 | 55 | 3.2 | 1.40 (0.92-2.11) | .121 | 17,088 | 16 | 0.9 | 0.57 (0.30-1.05) | .071 | 17,007 | 29 | 1.7 | 1.37 (0.78-2.41) | .322 | 15,755 | 119 | 7.6 | 1.02 (0.78-1.31) | .896 | |
| 2021 | 16,979 | 48 | 2.8 | 0.87 (0.59-1.29) | .554 | 17,067 | 21 | 1.2 | 1.31 (0.68-2.52) | .417 | 16,981 | 33 | 1.9 | 1.14 (0.69-1.88) | .614 | 15,767 | 120 | 7.6 | 1.01 (0.78-1.30) | 1.000 | |
| Socioeconomic status | |||||||||||||||||||||
| Low (1-3) | 2017 | 25,890 | 123 | 4.8 | 26,150 | 50 | 1.9 | 25,864 | 104 | 4.0 | 22,614 | 327 | 14.5 | ||||||||
| 2018 | 26,669 | 149 | 5.6 | 1.18 (0.92-1.49) | .202 | 26,925 | 55 | 2.0 | 1.07 (0.72-1.57) | .770 | 26,563 | 114 | 4.3 | 1.07 (0.81-1.39) | .635 | 23,137 | 357 | 15.4 | 1.07 (0.91-1.24) | .397 | |
| 2019 | 27,785 | 155 | 5.6 | 1.00 (0.79-1.25) | 1.000 | 28,085 | 51 | 1.8 | 0.89 (0.60-1.30) | .561 | 27,651 | 122 | 4.4 | 1.03 (0.79-1.33) | .845 | 24,141 | 377 | 15.6 | 1.01 (0.87-1.17) | .882 | |
| 2020 | 28,307 | 138 | 4.9 | 0.87 (0.69-1.10) | .266 | 28,662 | 59 | 2.1 | 1.13 (0.77-1.65) | .567 | 28,156 | 131 | 4.7 | 1.05 (0.82-1.35) | .705 | 24,568 | 283 | 11.5 | 0.74 (0.63-0.86) | <.001 | |
| 2021 | 28,860 | 159 | 5.5 | 1.13 (0.90-1.42) | .296 | 29,208 | 56 | 1.9 | 0.93 (0.64-1.34) | .710 | 28,659 | 140 | 4.9 | 1.05 (0.82-1.33) | .715 | 25,088 | 315 | 12.6 | 1.09 (0.92-1.28) | .304 | |
| Medium (4-7) | 2017 | 135,607 | 1,200 | 8.8 | 137,997 | 365 | 2.6 | 135,797 | 548 | 4.0 | 107,325 | 3,108 | 29.0 | ||||||||
| 2018 | 137,642 | 1,259 | 9.1 | 1.03 (0.95-1.12) | .418 | 140,272 | 294 | 2.1 | 0.79 (0.68-0.92) | .003 | 137,711 | 592 | 4.3 | 1.07 (0.94-1.20) | .286 | 108,151 | 2,988 | 27.6 | 0.95 (0.90-1.00) | .063 | |
| 2019 | 138,738 | 1,328 | 9.6 | 1.05 (0.96-1.13) | .252 | 141,723 | 328 | 2.3 | 1.10 (0.94-1.29) | .228 | 138,775 | 648 | 4.7 | 1.09 (0.97-1.21) | .147 | 108,595 | 2,917 | 26.9 | 0.97 (0.92-1.02) | .273 | |
| 2020 | 141,717 | 1,441 | 10.2 | 1.06 (0.98-1.14) | .113 | 145,151 | 330 | 2.3 | 0.98 (0.84-1.14) | .845 | 141,754 | 699 | 4.9 | 1.06 (0.94-1.18) | .325 | 110,998 | 2,617 | 23.6 | 0.88 (0.83-0.92) | <.001 | |
| 2021 | 144,750 | 1,778 | 12.3 | 1.21 (1.13-1.29) | <.001 | 148,576 | 369 | 2.5 | 1.09 (0.94-1.27) | .256 | 144,661 | 874 | 6.0 | 1.23 (1.11-1.35) | <.001 | 113,948 | 2,782 | 24.4 | 1.04 (0.98-1.09) | .195 | |
| High (8-10) | 2017 | 50,092 | 461 | 9.2 | 51,089 | 123 | 2.4 | 50,499 | 195 | 3.9 | 39,003 | 1,443 | 37.0 | ||||||||
| 2018 | 51,611 | 527 | 10.2 | 1.11 (0.97-1.26) | .103 | 52,794 | 138 | 2.6 | 1.09 (0.85-1.38) | .536 | 52,013 | 169 | 3.2 | 0.84 (0.68-1.03) | .104 | 39,922 | 1,373 | 34.4 | 0.93 (0.86-1.00) | .050 | |
| 2019 | 52,989 | 568 | 10.7 | 1.05 (0.93-1.18) | .430 | 54,309 | 128 | 2.4 | 0.90 (0.70-1.15) | .425 | 53,379 | 208 | 3.9 | 1.20 (0.97-1.47) | .080 | 41,085 | 1,375 | 33.5 | 0.97 (0.90-1.05) | .473 | |
| 2020 | 54,956 | 607 | 11.0 | 1.03 (0.91-1.16) | .618 | 56,447 | 107 | 1.9 | 0.80 (0.62-1.04) | .102 | 55,400 | 234 | 4.2 | 1.08 (0.89-1.31) | .418 | 42,745 | 1,272 | 29.8 | 0.89 (0.82-0.96) | .002 | |
| 2021 | 56,794 | 758 | 13.3 | 1.21 (1.09-1.34) | <.001 | 58,510 | 147 | 2.5 | 1.33 (1.03-1.70) | .028 | 57,294 | 308 | 5.4 | 1.27 (1.07-1.51) | .006 | 44,634 | 1,339 | 30.0 | 1.01 (0.93-1.09) | .842 | |
ADHD = attention-deficit/hyperactivity disorder; RR = relative risk.
Table 2.
Study Population Characteristics of Adolescents With a Psychiatric History and Rates of Mental Health Diagnoses and Medications by Years, Diagnoses, and Medications
| Characteristics | Depression |
Anxiety |
Eating disorder |
Stress |
ADHD |
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population, n | Event, n | Rate per 1,000 | RR year/ year 1 (95% CI) | p | Population, n | Event, n | Rate per 1,000 | RR year/year 1 (95% CI) | p | Population, n | Event, n | Rate per 1,000 | RR year/year 1 (95% CI) | p | Population, n | Event, n | Rate per 1,000 | RR year/year 1 (95% CI) | p | Population, n | Event, n | Rate per 1,000 | RR year/ year 1 (95% CI) | p | ||
| Total | Year | |||||||||||||||||||||||||
| 2017 | 1,194 | 295 | 247.1 | 3,554 | 940 | 264.5 | 1,203 | 266 | 221.1 | 6,624 | 1,306 | 197.2 | 33,940 | 15,230 | 448.7 | |||||||||||
| 2018 | 1,260 | 328 | 260.3 | 1.05 (0.92-1.21) | .458 | 3,946 | 1,065 | 269.9 | 1.02 (0.95-1.10) | .601 | 1,311 | 272 | 207.5 | 0.94 (0.81-1.09) | .408 | 7,675 | 1,428 | 186.1 | 0.94 (0.88-1.01) | .096 | 35,219 | 14,962 | 424.8 | 0.95 (0.93-0.96) | <.001 | |
| 2019 | 1,418 | 372 | 262.3 | 1.01 (0.89-1.14) | .930 | 4,438 | 1,193 | 268.8 | 1.00 (0.93-1.07) | .921 | 1,387 | 295 | 212.7 | 1.03 (0.89-1.19) | .741 | 8,471 | 1,553 | 183.3 | 0.99 (0.92-1.05) | .670 | 35,787 | 14,316 | 400.0 | 0.94 (0.93-0.96) | <.001 | |
| 2020 | 1,486 | 407 | 273.9 | 1.04 (0.93-1.18) | .503 | 4,699 | 1,339 | 285.0 | 1.06 (0.99-1.13) | .088 | 1,374 | 343 | 249.6 | 1.17 (1.02-1.35) | .021 | 8,792 | 1,587 | 180.5 | 0.98 (0.92-1.05) | .636 | 35,099 | 12,928 | 368.3 | 0.92 (0.90-0.94) | <.001 | |
| 2021 | 1,607 | 449 | 279.4 | 1.02 (0.91-1.14) | .748 | 4,992 | 1,444 | 289.3 | 1.02 (0.95-1.08) | .653 | 1,478 | 420 | 284.2 | 1.14 (1.01-1.29) | .038 | 8,959 | 1,726 | 192.7 | 1.07 (1.00-1.13) | .039 | 32,445 | 11,739 | 361.8 | 0.98 (0.96-1.00) | .080 | |
| Sex | ||||||||||||||||||||||||||
| Female | 2017 | 642 | 181 | 281.9 | 1,607 | 415 | 258.2 | 779 | 211 | 270.9 | 3,057 | 621 | 203.1 | 11,918 | 5012 | 420.5 | ||||||||||
| 2018 | 676 | 189 | 279.6 | 0.99 (0.83-1.18) | .951 | 1,776 | 450 | 253.4 | 0.98 (0.87-1.10) | .752 | 845 | 213 | 252.1 | 0.93 (0.79-1.10) | .397 | 3,549 | 702 | 197.8 | 0.97 (0.88-1.07) | .600 | 12,343 | 4973 | 402.9 | 0.96 (0.93-0.99) | .005 | |
| 2019 | 779 | 238 | 305.5 | 1.09 (0.93-1.28) | .299 | 1,985 | 512 | 257.9 | 1.02 (0.91-1.14) | .765 | 913 | 244 | 267.3 | 1.06 (0.91-1.24) | .480 | 3,998 | 773 | 193.3 | 0.98 (0.89-1.07) | .642 | 12,703 | 4,852 | 382.0 | 0.95 (0.92-0.98) | .001 | |
| 2020 | 823 | 239 | 290.4 | 0.95 (0.82-1.10) | .512 | 2,100 | 588 | 280.0 | 1.09 (0.98-1.20) | .113 | 906 | 280 | 309.1 | 1.16 (1.00-1.34) | .049 | 4,219 | 776 | 183.9 | 0.95 (0.87-1.04) | .284 | 12,637 | 4,548 | 359.9 | 0.94 (0.91-0.97) | <.001 | |
| 2021 | 908 | 282 | 310.6 | 1.07 (0.93-1.24) | .373 | 2,314 | 662 | 286.1 | 1.02 (0.93-1.12) | .664 | 1,036 | 364 | 351.4 | 1.14 (1.00-1.29) | .053 | 4,389 | 898 | 204.6 | 1.11 (1.02-1.21) | .017 | 11,942 | 4,149 | 347.4 | 0.97 (0.93-1.00) | .041 | |
| Male | 2017 | 552 | 114 | 206.5 | 1,947 | 525 | 269.6 | 424 | 55 | 129.7 | 3,567 | 685 | 192.0 | 22,022 | 10,218 | 464.0 | ||||||||||
| 2018 | 584 | 139 | 238.0 | 1.15 (0.93-1.43) | .225 | 2,170 | 615 | 283.4 | 1.05 (0.95-1.16) | .329 | 466 | 59 | 126.6 | 0.98 (0.69-1.38) | .920 | 4,126 | 726 | 176.0 | 0.92 (0.83-1.01) | .072 | 22,876 | 9,989 | 436.7 | 0.94 (0.92-0.96) | <.001 | |
| 2019 | 639 | 134 | 209.7 | 0.88 (0.71-1.09) | .243 | 2,453 | 681 | 277.6 | 0.98 (0.89-1.07) | .670 | 474 | 51 | 107.6 | 0.85 (0.60-1.21) | .417 | 4,473 | 780 | 174.4 | 0.99 (0.90-1.09) | .865 | 23,084 | 9,464 | 410.0 | 0.94 (0.92-0.96) | <.001 | |
| 2020 | 663 | 168 | 253.4 | 1.21 (0.99-1.47) | .066 | 2,599 | 751 | 289.0 | 1.04 (0.95-1.14) | .382 | 468 | 63 | 134.6 | 1.25 (0.88-1.77) | .231 | 4,573 | 811 | 177.3 | 1.02 (0.93-1.11) | .720 | 22,462 | 8,380 | 373.1 | 0.91 (0.89-0.93) | <.001 | |
| 2021 | 699 | 167 | 238.9 | 0.94 (0.78-1.14) | .571 | 2,678 | 782 | 292.0 | 1.01 (0.93-1.10) | .808 | 442 | 56 | 126.7 | 0.94 (0.67-1.32) | .768 | 4,570 | 828 | 181.2 | 1.02 (0.94-1.12) | .643 | 20,503 | 7,590 | 370.2 | 0.99 (0.97-1.02) | .542 | |
| Age, y | ||||||||||||||||||||||||||
| 12-13 | 2017 | 185 | 36 | 194.6 | 1072 | 268 | 250.0 | 323 | 53 | 164.1 | 2582 | 522 | 202.2 | 11659 | 5670 | 486.3 | ||||||||||
| 2018 | 194 | 31 | 159.8 | 0.82 (0.53-1.27) | .420 | 1318 | 351 | 266.3 | 1.07 (0.93-1.22) | .373 | 354 | 63 | 178.0 | 1.08 (0.78-1.51) | .683 | 3147 | 575 | 182.7 | 0.90 (0.81-1.01) | .064 | 12016 | 5471 | 455.3 | 0.94 (0.91-0.96) | <.001 | |
| 2019 | 236 | 54 | 228.8 | 1.43 (0.96-2.13) | .088 | 1452 | 350 | 241.0 | 0.91 (0.80-1.03) | .137 | 347 | 35 | 100.9 | 0.57 (0.39-0.83) | .003 | 3514 | 622 | 177.0 | 0.97 (0.87-1.07) | .565 | 12283 | 5187 | 422.3 | 0.93 (0.90-0.95) | <.001 | |
| 2020 | 248 | 63 | 254.0 | 1.11 (0.81-1.52) | .526 | 1570 | 406 | 258.6 | 1.07 (0.95-1.21) | .275 | 333 | 42 | 126.1 | 1.25 (0.82-1.91) | .333 | 3699 | 649 | 175.5 | 0.99 (0.90-1.10) | .877 | 12158 | 4716 | 387.9 | 0.92 (0.89-0.95) | <.001 | |
| 2021 | 287 | 61 | 212.5 | 0.84 (0.61-1.14) | .261 | 1,642 | 441 | 268.6 | 1.04 (0.93-1.17) | .522 | 334 | 58 | 173.7 | 1.38 (0.95-1.99) | .103 | 3,768 | 706 | 187.4 | 1.07 (0.97-1.18) | .186 | 11,259 | 4272 | 379.4 | 0.98 (0.95-1.01) | .188 | |
| 14-15 | 2017 | 335 | 81 | 241.8 | 1,219 | 323 | 265.0 | 371 | 87 | 234.5 | 2,168 | 405 | 186.8 | 11,452 | 5059 | 441.8 | ||||||||||
| 2018 | 432 | 108 | 250.0 | 1.03 (0.81-1.33) | .801 | 1,281 | 347 | 270.9 | 1.02 (0.90-1.16) | .752 | 442 | 89 | 201.4 | 0.86 (0.66-1.12) | .267 | 2,523 | 467 | 185.1 | 0.99 (0.88-1.12) | .880 | 12,145 | 5113 | 421.0 | 0.95 (0.93-0.98) | .001 | |
| 2019 | 445 | 97 | 218.0 | 0.87 (0.69-1.11) | .265 | 1,426 | 372 | 260.9 | 0.96 (0.85-1.09) | .571 | 475 | 116 | 244.2 | 1.21 (0.95-1.55) | .132 | 2,701 | 488 | 180.7 | 0.98 (0.87-1.09) | .694 | 12,060 | 4703 | 390.0 | 0.93 (0.90-0.96) | <.001 | |
| 2020 | 444 | 115 | 259.0 | 1.19 (0.94-1.50) | .157 | 1,474 | 420 | 284.9 | 1.09 (0.97-1.23) | .156 | 461 | 122 | 264.6 | 1.08 (0.87-1.35) | .500 | 2,756 | 480 | 174.2 | 0.96 (0.86-1.08) | .547 | 11,543 | 4101 | 355.3 | 0.91 (0.88-0.94) | <.001 | |
| 2021 | 484 | 137 | 283.1 | 1.09 (0.88-1.35) | .417 | 1,595 | 473 | 296.6 | 1.04 (0.93-1.16) | .499 | 459 | 143 | 311.5 | 1.18 (0.96-1.44) | .126 | 2,758 | 529 | 191.8 | 1.10 (0.98-1.23) | .095 | 10,743 | 3750 | 349.1 | 0.98 (0.95-1.02) | .333 | |
| 16-17 | 2017 | 674 | 178 | 264.1 | 1,263 | 349 | 276.3 | 509 | 126 | 247.5 | 1,874 | 379 | 202.2 | 10,829 | 4501 | 415.6 | ||||||||||
| 2018 | 634 | 189 | 298.1 | 1.13 (0.95-1.34) | .176 | 1,347 | 367 | 272.5 | 0.99 (0.87-1.12) | .826 | 515 | 120 | 233.0 | 0.94 (0.76-1.17) | .609 | 2,005 | 386 | 192.5 | 0.95 (0.84-1.08) | .467 | 11,058 | 4378 | 395.9 | 0.95 (0.92-0.98) | .003 | |
| 2019 | 737 | 221 | 299.9 | 1.01 (0.85-1.18) | .953 | 1,560 | 471 | 301.9 | 1.11 (0.99-1.24) | .085 | 565 | 144 | 254.9 | 1.09 (0.89-1.35) | .436 | 2,256 | 443 | 196.4 | 1.02 (0.90-1.15) | .757 | 11,444 | 4,426 | 386.8 | 0.98 (0.95-1.01) | .159 | |
| 2020 | 794 | 229 | 288.4 | 0.96 (0.82-1.12) | .653 | 1,655 | 513 | 310.0 | 1.03 (0.93-1.14) | .646 | 580 | 179 | 308.6 | 1.21 (1.01-1.46) | .049 | 2,337 | 458 | 196.0 | 1.00 (0.89-1.12) | 1.000 | 11,398 | 4,111 | 360.7 | 0.93 (0.90-0.96) | <.001 | |
| 2021 | 836 | 251 | 300.2 | 1.04 (0.90-1.21) | .625 | 1,755 | 530 | 302.0 | 0.97 (0.88-1.08) | .629 | 685 | 219 | 319.7 | 1.04 (0.88-1.22) | .715 | 2,433 | 491 | 201.8 | 1.03 (0.92-1.15) | .637 | 10,443 | 3,717 | 355.9 | 0.99 (0.95-1.02) | .471 | |
| Sector | ||||||||||||||||||||||||||
| General Jewish | 2017 | 1,086 | 272 | 250.5 | 3,187 | 860 | 269.8 | 1,076 | 250 | 232.3 | 5,909 | 1,197 | 202.6 | 29,396 | 13,476 | 458.4 | ||||||||||
| 2018 | 1,137 | 304 | 267.4 | 1.07 (0.93-1.23) | .383 | 3,532 | 989 | 280.0 | 1.04 (0.96-1.12) | .353 | 1,155 | 255 | 220.8 | 0.95 (0.82-1.11) | .544 | 6,737 | 1,305 | 193.7 | 0.96 (0.89-1.03) | .219 | 30,588 | 13,270 | 433.8 | 0.95 (0.93-0.96) | <.001 | |
| 2019 | 1,290 | 340 | 263.6 | 0.99 (0.86-1.13) | .854 | 3,987 | 1,101 | 276.1 | 0.99 (0.92-1.06) | .718 | 1,241 | 279 | 224.8 | 1.02 (0.88-1.18) | .844 | 7,462 | 1,424 | 190.8 | 0.99 (0.92-1.05) | .670 | 31,049 | 12,628 | 406.7 | 0.94 (0.92-0.96) | <.001 | |
| 2020 | 1,360 | 385 | 283.1 | 1.07 (0.95-1.22) | .276 | 4,257 | 1,231 | 289.2 | 1.05 (0.98-1.12) | .195 | 1,250 | 321 | 256.8 | 1.14 (0.99-1.31) | .068 | 7,789 | 1,435 | 184.2 | 0.97 (0.90-1.03) | .299 | 30,429 | 11,348 | 372.9 | 0.92 (0.90-0.94) | <0.001 | |
| 2021 | 1,479 | 421 | 284.7 | 1.01 (0.89-1.13) | .934 | 4,531 | 1,349 | 297.7 | 1.03 (0.96-1.10) | .386 | 1,360 | 402 | 295.6 | 1.15 (1.02-1.30) | .029 | 7,897 | 1,578 | 199.8 | 1.08 (1.02-1.16) | .013 | 28,029 | 10,127 | 361.3 | 0.97 (0.95-0.99) | 0.004 | |
| Ultra-orthodox Jewish | 2017 | 77 | 17 | 220.8 | 280 | 71 | 253.6 | 103 | 13 | 126.2 | 482 | 66 | 136.9 | 3635 | 1512 | 416.0 | ||||||||||
| 2018 | 80 | 14 | 175.0 | 0.79 (0.42-1.49) | .549 | 306 | 60 | 196.1 | 0.77 (0.57-1.05) | .112 | 124 | 14 | 112.9 | 0.89 (0.44-1.82) | .838 | 657 | 75 | 114.2 | 0.83 (0.61-1.14) | .275 | 3777 | 1466 | 388.1 | 0.93 (0.88-0.99) | .015 | |
| 2019 | 77 | 21 | 272.7 | 1.56 (0.86-2.84) | .180 | 341 | 79 | 231.7 | 1.18 (0.88-1.59) | .292 | 121 | 13 | 107.4 | 0.95 (0.47-1.94) | 1.000 | 734 | 86 | 117.2 | 1.03 (0.77-1.37) | .867 | 3920 | 1457 | 371.7 | 0.96 (0.90-1.01) | .139 | |
| 2020 | 92 | 18 | 195.7 | 0.72 (0.41-1.25) | .273 | 348 | 91 | 261.5 | 1.13 (0.87-1.47) | .378 | 104 | 20 | 192.3 | 1.79 (0.94-3.42) | .089 | 747 | 113 | 151.3 | 1.29 (0.99-1.68) | .057 | 3912 | 1369 | 349.9 | 0.94 (0.89-1.00) | .046 | |
| 2021 | 93 | 18 | 193.5 | 0.99 (0.55-1.78) | 1.000 | 377 | 80 | 212.2 | 0.81 (0.62-1.06) | .137 | 92 | 15 | 163.0 | 0.85 (0.46-1.56) | .709 | 831 | 105 | 126.4 | 0.84 (0.65-1.07) | .165 | 3710 | 1391 | 374.9 | 1.07 (1.01-1.14) | .024 | |
| Arab | 2017 | 31 | 6 | 193.5 | 87 | 9 | 103.4 | 24 | 3 | 125.0 | 233 | 43 | 184.5 | 908 | 242 | 266.5 | ||||||||||
| 2018 | 43 | 10 | 232.6 | 1.20 (0.49-2.96) | .780 | 108 | 16 | 148.1 | 1.43 (0.67-3.08) | .395 | 32 | 3 | 93.8 | 0.75 (0.17-3.40) | 1.000 | 281 | 48 | 170.8 | 0.93 (0.64-1.34) | .728 | 853 | 226 | 264.9 | 0.99 (0.85-1.16) | .957 | |
| 2019 | 51 | 11 | 215.7 | 0.93 (0.44-1.97) | 1.000 | 110 | 13 | 118.2 | 0.80 (0.40-1.58) | .554 | 25 | 3 | 120.0 | 1.28 (0.28-5.81) | 1.000 | 275 | 43 | 156.4 | 0.92 (0.63-1.33) | .649 | 817 | 231 | 282.7 | 1.07 (0.91-1.25) | .442 | |
| 2020 | 34 | 4 | 117.6 | 0.55 (0.19-1.57) | .384 | 94 | 17 | 180.9 | 1.53 (0.78-2.98) | .237 | 20 | 2 | 100.0 | 0.83 (0.15-4.52) | 1.000 | 256 | 39 | 152.3 | 0.97 (0.65-1.45) | .905 | 758 | 211 | 278.4 | 0.98 (0.84-1.15) | .866 | |
| 2021 | 35 | 10 | 285.7 | 2.43 (0.84-7.00) | .133 | 84 | 15 | 178.6 | 0.99 (0.53-1.85) | 1.000 | 26 | 3 | 115.4 | 1.15 (0.21-6.26) | 1.000 | 231 | 43 | 186.1 | 1.22 (0.82-1.81) | .334 | 706 | 221 | 313.0 | 1.12 (0.96-1.32) | .152 | |
| Socio-economic status | ||||||||||||||||||||||||||
| Low | 2017 | 65 | 15 | 230.8 | 243 | 44 | 181.1 | 81 | 8 | 98.8 | 491 | 91 | 185.3 | 2818 | 1117 | 396.4 | ||||||||||
| 2018 | 87 | 18 | 206.9 | 0.90 (0.49-1.64) | .843 | 287 | 56 | 195.1 | 1.08 (0.75-1.54) | .739 | 105 | 12 | 114.3 | 1.16 (0.50-2.70) | .814 | 606 | 83 | 137.0 | 0.74 (0.56-0.97) | .031 | 2908 | 1080 | 371.4 | 0.94 (0.88-1.00) | .054 | |
| 2019 | 97 | 20 | 206.2 | 1.00 (0.57-1.76) | 1.000 | 306 | 68 | 222.2 | 1.14 (0.83-1.56) | .421 | 101 | 12 | 118.8 | 1.04 (0.49-2.21) | 1.000 | 689 | 108 | 156.7 | 1.14 (0.88-1.49) | .346 | 2863 | 1009 | 352.4 | 0.95 (0.89-1.02) | .139 | |
| 2020 | 86 | 18 | 209.3 | 1.02 (0.58-1.79) | 1.000 | 295 | 78 | 264.4 | 1.19 (0.90-1.58) | .254 | 77 | 14 | 181.8 | 1.53 (0.75-3.12) | .286 | 696 | 104 | 149.4 | 0.95 (0.74-1.22) | .710 | 2861 | 964 | 336.9 | 0.96 (0.89-1.03) | .221 | |
| 2021 | 92 | 16 | 173.9 | 0.83 (0.45-1.52) | .572 | 338 | 73 | 216.0 | 0.82 (0.62-1.08) | .162 | 70 | 12 | 171.4 | 0.94 (0.47-1.90) | 1.000 | 747 | 122 | 163.3 | 1.09 (0.86-1.39) | .514 | 2716 | 987 | 363.4 | 1.08 (1.00-1.16) | .040 | |
| Medium | 2017 | 834 | 201 | 241.0 | 2,407 | 647 | 268.8 | 795 | 165 | 207.5 | 4,608 | 883 | 191.6 | 22,419 | 10,026 | 447.2 | ||||||||||
| 2018 | 875 | 231 | 264.0 | 1.10 (0.93-1.29) | .290 | 2,665 | 739 | 277.3 | 1.03 (0.94-1.13) | .508 | 873 | 178 | 203.9 | 0.98 (0.81-1.19) | .856 | 5,352 | 994 | 185.7 | 0.97 (0.89-1.05) | .456 | 23,214 | 9,861 | 424.8 | 0.95 (0.93-0.97) | <.001 | |
| 2019 | 969 | 264 | 272.4 | 1.03 (0.89-1.2) | .713 | 3,003 | 836 | 278.4 | 1.00 (0.92-1.09) | .929 | 942 | 199 | 211.3 | 1.04 (0.87-1.24) | .728 | 5,898 | 1,059 | 179.6 | 0.97 (0.89-1.05) | .406 | 23,662 | 9,503 | 401.6 | 0.95 (0.93-0.97) | <.001 | |
| 2020 | 1,027 | 300 | 292.1 | 1.07 (0.93-1.23) | .345 | 3,197 | 949 | 296.8 | 1.07 (0.99-1.15) | .110 | 936 | 227 | 242.5 | 1.15 (0.97-1.36) | .110 | 6,167 | 1,115 | 180.8 | 1.01 (0.93-1.09) | .868 | 23,226 | 8,473 | 364.8 | 0.91 (0.89-0.93) | <.001 | |
| 2021 | 1,107 | 326 | 294.5 | 1.01 (0.88-1.15) | .924 | 3,322 | 979 | 294.7 | 0.99 (0.92-1.07) | .871 | 1,013 | 275 | 271.5 | 1.12 (0.96-1.30) | .147 | 6,253 | 1,219 | 194.9 | 1.08 (1.00-1.16) | .046 | 21,383 | 7,660 | 358.2 | 0.98 (0.96-1.01) | .150 | |
| High | 2017 | 293 | 78 | 266.2 | 897 | 246 | 274.2 | 323 | 92 | 284.8 | 1,508 | 326 | 216.2 | 8,627 | 4047 | 469.1 | ||||||||||
| 2018 | 294 | 78 | 265.3 | 1.00 (0.76-1.30) | 1.000 | 983 | 265 | 269.6 | 0.98 (0.85-1.14) | .836 | 326 | 82 | 251.5 | 0.88 (0.68-1.14) | .376 | 1,694 | 347 | 204.8 | 0.95 (0.83-1.08) | .435 | 9,014 | 3983 | 441.9 | 0.94 (0.91-0.97) | <.001 | |
| 2019 | 347 | 87 | 250.7 | 0.95 (0.73-1.23) | .717 | 1,116 | 284 | 254.5 | 0.94 (0.82-1.09) | .455 | 339 | 83 | 244.8 | 0.97 (0.75-1.27) | .858 | 1,854 | 384 | 207.1 | 1.01 (0.89-1.15) | .868 | 9,174 | 3773 | 411.3 | 0.93 (0.90-0.96) | <.001 | |
| 2020 | 370 | 89 | 240.5 | 0.96 (0.74-1.24) | .795 | 1,191 | 309 | 259.4 | 1.02 (0.89-1.17) | .812 | 360 | 102 | 283.3 | 1.16 (0.90-1.48) | .265 | 1,903 | 366 | 192.3 | 0.93 (0.82-1.06) | .270 | 8,921 | 3453 | 387.1 | 0.94 (0.91-0.98) | .001 | |
| 2021 | 403 | 107 | 265.5 | 1.10 (0.87-1.41) | .457 | 1,314 | 385 | 293.0 | 1.13 (0.99-1.28) | .067 | 391 | 131 | 335.0 | 1.18 (0.95-1.47) | .134 | 1,927 | 379 | 196.7 | 1.02 (0.90-1.16) | .744 | 8,253 | 3057 | 370.4 | 0.96 (0.92-0.99) | .025 | |
| Characteristics | Antidepressant |
Anxiolytic |
Antipsychotics |
ADHD agents |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population, N | Event, n | Rate per 1,000 | RR year/ year 1 (95% CI) | p | Population, N | Event, n | Rate per 1,000 | RR year/ year 1 (95% CI) | p | Population, N | Event, n | Rate per 1,000 | RR year/ year 1 (95% CI) | p | Population, N | Event, n | Rate per 1,000 | RR year/Year 1 (95% CI) | p | ||
| Total | Year | ||||||||||||||||||||
| 2017 | 3,684 | 2,010 | 545.6 | 726 | 167 | 230.0 | 3,815 | 2,221 | 582.2 | 34,033 | 21,557 | 633.4 | |||||||||
| 2018 | 3,826 | 2,154 | 563.0 | 1.03 (0.99-1.07) | .131 | 702 | 160 | 227.9 | 0.99 (0.82-1.20) | .950 | 4,050 | 2,467 | 609.1 | 1.05 (1.01-1.09) | .016 | 34,581 | 20,686 | 598.2 | 0.94 (0.93-0.96) | <.001 | |
| 2019 | 4,247 | 2,403 | 565.8 | 1.01 (0.97-1.04) | .805 | 659 | 167 | 253.4 | 1.11 (0.92-1.34) | .281 | 4,275 | 2,611 | 610.8 | 1.00 (0.97-1.04) | .893 | 34,223 | 19,922 | 582.1 | 0.97 (0.96-0.99) | <.001 | |
| 2020 | 4,624 | 2,724 | 589.1 | 1.04 (1.00-1.08) | .027 | 598 | 166 | 277.6 | 1.10 (0.91-1.32) | .338 | 4,617 | 2,785 | 603.2 | 0.99 (0.96-1.02) | .473 | 33,427 | 18,131 | 542.4 | 0.93 (0.92-0.94) | <.001 | |
| 2021 | 4,823 | 2,984 | 618.7 | 1.05 (1.02-1.09) | .003 | 601 | 179 | 297.8 | 1.07 (0.90-1.28) | .445 | 4,744 | 2,866 | 604.1 | 1.00 (0.97-1.03) | .933 | 30,782 | 15,669 | 509.0 | 0.94 (0.92-0.95) | <.001 | |
| Sex | |||||||||||||||||||||
| Female | 2017 | 1,591 | 871 | 547.5 | 374 | 92 | 246.0 | 1,050 | 593 | 564.8 | 11,586 | 7,169 | 618.8 | ||||||||
| 2018 | 1,658 | 947 | 571.2 | 1.04 (0.98-1.11) | .179 | 357 | 79 | 221.3 | 0.90 (0.69-1.17) | .433 | 1,079 | 662 | 613.5 | 1.09 (1.01-1.17) | .025 | 11,748 | 6,785 | 577.5 | 0.93 (0.91-0.95) | <.001 | |
| 2019 | 1,862 | 1,099 | 590.2 | 1.03 (0.98-1.09) | .259 | 331 | 87 | 262.8 | 1.19 (0.91-1.55) | .213 | 1,164 | 711 | 610.8 | 1.00 (0.93-1.06) | .897 | 11,721 | 6,658 | 568.0 | 0.98 (0.96-1.01) | .143 | |
| 2020 | 2,061 | 1,245 | 604.1 | 1.02 (0.97-1.08) | .379 | 300 | 78 | 260.0 | 0.99 (0.76-1.29) | 1.000 | 1,256 | 783 | 623.4 | 1.02 (0.96-1.09) | .530 | 11,573 | 6,116 | 528.5 | 0.93 (0.91-0.95) | <.001 | |
| 2021 | 2,269 | 1,471 | 648.3 | 1.07 (1.02-1.12) | .003 | 307 | 89 | 289.9 | 1.12 (0.86-1.44) | .415 | 1,388 | 858 | 618.2 | 0.99 (0.93-1.05) | .810 | 10,809 | 5,381 | 497.8 | 0.94 (0.92-0.97) | <.001 | |
| Male | 2017 | 2,093 | 1,139 | 544.2 | 352 | 75 | 213.1 | 2,765 | 1,628 | 588.8 | 22,447 | 14,388 | 641.0 | ||||||||
| 2018 | 2,168 | 1,207 | 556.7 | 1.02 (0.97-1.08) | .423 | 345 | 81 | 234.8 | 1.1 (0.84-1.45) | .525 | 2,971 | 1,805 | 607.5 | 1.03 (0.99-1.08) | .153 | 22,833 | 13,901 | 608.8 | 0.95 (0.94-0.96) | <.001 | |
| 2019 | 2,385 | 1,304 | 546.8 | 0.98 (0.93-1.03) | .512 | 328 | 80 | 243.9 | 1.04 (0.79-1.36) | .787 | 3,111 | 1,900 | 610.7 | 1.01 (0.97-1.05) | .813 | 22,502 | 13,264 | 589.5 | 0.97 (0.95-0.98) | <.001 | |
| 2020 | 2,563 | 1,479 | 577.1 | 1.06 (1.00-1.11) | .034 | 298 | 88 | 295.3 | 1.21 (0.93-1.57) | .150 | 3,361 | 2,002 | 595.7 | 0.98 (0.94-1.01) | .222 | 21,854 | 12,015 | 549.8 | 0.93 (0.92-0.95) | <.001 | |
| 2021 | 2,554 | 1,513 | 592.4 | 1.03 (0.98-1.08) | .269 | 294 | 90 | 306.1 | 1.04 (0.81-1.33) | .789 | 3,356 | 2,008 | 598.3 | 1.00 (0.97-1.04) | .842 | 19,973 | 10,288 | 515.1 | 0.94 (0.92-0.95) | <.001 | |
| Age, y | |||||||||||||||||||||
| 12-13 | 2017 | 764 | 408 | 534.0 | 154 | 37 | 240.3 | 1227 | 732 | 596.6 | 10,829 | 7,250 | 669.5 | ||||||||
| 2018 | 796 | 433 | 544.0 | 1.02 (0.93-1.12) | .722 | 134 | 38 | 283.6 | 1.18 (0.8-1.74) | .422 | 1323 | 828 | 625.9 | 1.05 (0.99-1.12) | .133 | 10,843 | 6,873 | 633.9 | 0.95 (0.93-0.97) | <.001 | |
| 2019 | 862 | 474 | 549.9 | 1.01 (0.93-1.10) | .843 | 134 | 30 | 223.9 | 0.79 (0.52-1.19) | .326 | 1369 | 874 | 638.4 | 1.02 (0.96-1.08) | .522 | 10,872 | 6,628 | 609.6 | 0.96 (0.94-0.98) | <.001 | |
| 2020 | 956 | 562 | 587.9 | 1.07 (0.99-1.16) | .107 | 109 | 41 | 376.1 | 1.68 (1.13-2.50) | .011 | 1454 | 901 | 619.7 | 0.97 (0.92-1.03) | .311 | 10,831 | 6,126 | 565.6 | 0.93 (0.91-0.95) | <.001 | |
| 2021 | 1,017 | 581 | 571.3 | 0.97 (0.90-1.05) | .466 | 122 | 48 | 393.4 | 1.05 (0.75-1.45) | .892 | 1,529 | 931 | 608.9 | 0.98 (0.93-1.04) | .547 | 9,961 | 5,259 | 528.0 | 0.93 (0.91-0.96) | <.001 | |
| 14-15 | 2017 | 1,185 | 660 | 557.0 | 237 | 61 | 257.4 | 1,286 | 776 | 603.4 | 11,501 | 7,357 | 639.7 | ||||||||
| 2018 | 1,303 | 753 | 577.9 | 1.04 (0.97-1.11) | .311 | 217 | 52 | 239.6 | 0.93 (0.68-1.28) | .666 | 1,387 | 843 | 607.8 | 1.01 (0.95-1.07) | .843 | 12,005 | 7,175 | 597.7 | 0.93 (0.92-0.95) | <.001 | |
| 2019 | 1,357 | 736 | 542.4 | 0.94 (0.88-1.00) | .066 | 185 | 62 | 335.1 | 1.4 (1.02-1.91) | .036 | 1,363 | 806 | 591.3 | 0.97 (0.92-1.03) | .392 | 11,558 | 6,715 | 581.0 | 0.97 (0.95-0.99) | .009 | |
| 2020 | 1,447 | 862 | 595.7 | 1.10 (1.03-1.17) | .005 | 176 | 50 | 284.1 | 0.85 (0.62-1.16) | .308 | 1,529 | 927 | 606.3 | 1.03 (0.97-1.09) | .425 | 11,051 | 5,946 | 538.1 | 0.93 (0.9-0.95) | <.001 | |
| 2021 | 1,586 | 996 | 628.0 | 1.05 (1.00-1.12) | .073 | 155 | 43 | 277.4 | 0.98 (0.69-1.38) | .903 | 1,578 | 974 | 617.2 | 1.02 (0.96-1.08) | .532 | 10,312 | 5,133 | 497.8 | 0.93 (0.9-0.95) | <.001 | |
| 16-17 | 2017 | 1,735 | 942 | 542.9 | 335 | 69 | 206.0 | 1,302 | 713 | 547.6 | 11,703 | 6,950 | 593.9 | ||||||||
| 2018 | 1,727 | 968 | 560.5 | 1.03 (0.97-1.10) | .305 | 351 | 70 | 199.4 | 0.97 (0.72-1.3) | .850 | 1,340 | 796 | 594.0 | 1.08 (1.02-1.16) | .017 | 11,733 | 6,638 | 565.8 | 0.95 (0.93-0.97) | <.001 | |
| 2019 | 2,028 | 1,193 | 588.3 | 1.05 (0.99-1.11) | .091 | 340 | 75 | 220.6 | 1.11 (0.83-1.48) | .514 | 1,543 | 931 | 603.4 | 1.02 (0.96-1.08) | .621 | 11,793 | 6,579 | 557.9 | 0.99 (0.96-1.01) | .227 | |
| 2020 | 2,221 | 1,300 | 585.3 | 0.99 (0.95-1.05) | .852 | 313 | 75 | 239.6 | 1.09 (0.82-1.44) | .577 | 1,634 | 957 | 585.7 | 0.97 (0.92-1.03) | .312 | 11,545 | 6,059 | 524.8 | 0.94 (0.92-0.96) | <.001 | |
| 2021 | 2,220 | 1,407 | 633.8 | 1.08 (1.03-1.14) | .001 | 324 | 88 | 271.6 | 1.13 (0.87-1.48) | .365 | 1,637 | 961 | 587.0 | 1.00 (0.95-1.06) | .943 | 10,509 | 5,277 | 502.1 | 0.96 (0.93-0.98) | .001 | |
| Sector | |||||||||||||||||||||
| General Jewish | 2017 | 3,217 | 1,788 | 555.8 | 585 | 125 | 213.7 | 3,216 | 1,865 | 579.9 | 29,393 | 18,661 | 634.9 | ||||||||
| 2018 | 3,356 | 1,934 | 576.3 | 1.04 (0.99-1.08) | .095 | 577 | 116 | 201.0 | 0.94 (0.75-1.18) | .613 | 3,434 | 2,094 | 609.8 | 1.05 (1.01-1.09) | .013 | 29,825 | 17,895 | 600.0 | 0.95 (0.93-0.96) | <.001 | |
| 2019 | 3,717 | 2,157 | 580.3 | 1.01 (0.97-1.05) | .736 | 539 | 126 | 233.8 | 1.16 (0.93-1.45) | .191 | 3,597 | 2,205 | 613.0 | 1.01 (0.97-1.04) | .788 | 29,474 | 17,208 | 583.8 | 0.97 (0.96-0.99) | <.001 | |
| 2020 | 4,040 | 2,429 | 601.2 | 1.04 (1.00-1.08) | .061 | 484 | 123 | 254.1 | 1.09 (0.88-1.35) | .466 | 3,897 | 2,330 | 597.9 | 0.98 (0.94-1.01) | .185 | 28,756 | 15,587 | 542.0 | 0.93 (0.92-0.94) | <.001 | |
| 2021 | 4,246 | 2,687 | 632.8 | 1.05 (1.02-1.09) | .003 | 484 | 141 | 291.3 | 1.15 (0.93-1.41) | .220 | 3,997 | 2,404 | 601.5 | 1.01 (0.97-1.04) | .748 | 26,393 | 13,332 | 505.1 | 0.93 (0.92-0.95) | <.001 | |
| Ultra-orthodox Jewish | 2017 | 401 | 195 | 486.3 | 98 | 28 | 285.7 | 489 | 291 | 595.1 | 3,855 | 2,552 | 662.0 | ||||||||
| 2018 | 403 | 194 | 481.4 | 0.99 (0.86-1.14) | .944 | 84 | 30 | 357.1 | 1.25 (0.82-1.91) | .340 | 515 | 310 | 601.9 | 1.01 (0.91-1.12) | .847 | 4,013 | 2,470 | 615.5 | 0.93 (0.90-0.96) | <.001 | |
| 2019 | 464 | 221 | 476.3 | 0.99 (0.86-1.14) | .892 | 85 | 26 | 305.9 | 0.86 (0.56-1.32) | .516 | 570 | 338 | 593.0 | 0.99 (0.89-1.09) | .804 | 4,083 | 2,409 | 590.0 | 0.96 (0.93-0.99) | .019 | |
| 2020 | 519 | 266 | 512.5 | 1.08 (0.95-1.22) | .277 | 82 | 30 | 365.9 | 1.20 (0.78-1.84) | .419 | 624 | 395 | 633.0 | 1.07 (0.98-1.17) | .171 | 4,063 | 2,292 | 564.1 | 0.96 (0.92-0.99) | .019 | |
| 2021 | 510 | 272 | 533.3 | 1.04 (0.93-1.17) | .533 | 89 | 24 | 269.7 | 0.74 (0.47-1.15) | .191 | 652 | 407 | 624.2 | 0.99 (0.91-1.07) | .772 | 3,880 | 2,141 | 551.8 | 0.98 (0.94-1.02) | .278 | |
| Arab | 2017 | 66 | 27 | 409.1 | 43 | 14 | 325.6 | 110 | 65 | 590.9 | 784 | 344 | 438.8 | ||||||||
| 2018 | 67 | 26 | 388.1 | 0.95 (0.62-1.44) | .860 | 41 | 14 | 341.5 | 1.05 (0.57-1.92) | 1.000 | 101 | 63 | 623.8 | 1.06 (0.85-1.31) | .673 | 742 | 321 | 432.6 | 0.99 (0.88-1.11) | .836 | |
| 2019 | 66 | 25 | 378.8 | 0.98 (0.63-1.50) | 1.000 | 35 | 15 | 428.6 | 1.26 (0.71-2.22) | .484 | 108 | 68 | 629.6 | 1.01 (0.82-1.24) | 1.000 | 666 | 305 | 458.0 | 1.06 (0.94-1.19) | .361 | |
| 2020 | 65 | 29 | 446.2 | 1.18 (0.78-1.78) | .480 | 32 | 13 | 406.3 | 0.95 (0.54-1.67) | 1.000 | 96 | 60 | 625.0 | 0.99 (0.80-1.23) | 1.000 | 608 | 252 | 414.5 | 0.91 (0.80-1.03) | .127 | |
| 2021 | 67 | 25 | 373.1 | 0.84 (0.55-1.26) | .479 | 28 | 14 | 500.0 | 1.23 (0.70-2.15) | .604 | 95 | 55 | 578.9 | 0.93 (0.74-1.17) | .556 | 509 | 196 | 385.1 | 0.93 (0.80-1.07) | .327 | |
| Socio-economic status | |||||||||||||||||||||
| Low | 2017 | 276 | 125 | 452.9 | 78 | 26 | 333.3 | 416 | 233 | 560.1 | 2,701 | 1,586 | 587.2 | ||||||||
| 2018 | 271 | 146 | 538.7 | 1.19 (1.00-1.41) | .049 | 84 | 25 | 297.6 | 0.89 (0.57-1.41) | .735 | 439 | 249 | 567.2 | 1.01 (0.9-1.14) | .836 | 2,767 | 1,511 | 546.1 | 0.93 (0.89-0.97) | .002 | |
| 2019 | 303 | 153 | 505.0 | 0.94 (0.80-1.10) | .452 | 74 | 24 | 324.3 | 1.09 (0.68-1.73) | .733 | 460 | 287 | 623.9 | 1.10 (0.99-1.23) | .089 | 2,663 | 1,404 | 527.2 | 0.97 (0.92-1.01) | .165 | |
| 2020 | 336 | 168 | 500.0 | 0.99 (0.85-1.16) | .937 | 64 | 32 | 500.0 | 1.54 (1.02-2.32) | .039 | 473 | 296 | 625.8 | 1.00 (0.91-1.11) | 1.000 | 2,602 | 1,292 | 496.5 | 0.94 (0.89-0.99) | .027 | |
| 2021 | 316 | 165 | 522.2 | 1.04 (0.90-1.21) | .584 | 75 | 26 | 346.7 | 0.69 (0.47-1.03) | .085 | 479 | 296 | 618.0 | 0.99 (0.89-1.09) | .841 | 2,389 | 1,180 | 493.9 | 0.99 (0.94-1.05) | .865 | |
| Medium | 2017 | 2,378 | 1,265 | 532.0 | 482 | 100 | 207.5 | 2,587 | 1,516 | 586.0 | 22,481 | 14,206 | 631.9 | ||||||||
| 2018 | 2,471 | 1,347 | 545.1 | 1.02 (0.97-1.08) | .372 | 457 | 100 | 218.8 | 1.05 (0.82-1.35) | .691 | 2,694 | 1,638 | 608.0 | 1.04 (0.99-1.08) | .104 | 22,702 | 13,457 | 592.8 | 0.94 (0.92-0.95) | <.001 | |
| 2019 | 2,725 | 1,503 | 551.6 | 1.01 (0.96-1.06) | .655 | 409 | 103 | 251.8 | 1.15 (0.90-1.46) | .261 | 2,877 | 1,740 | 604.8 | 0.99 (0.95-1.04) | .826 | 22,465 | 12,953 | 576.6 | 0.97 (0.96-0.99) | <.001 | |
| 2020 | 2,962 | 1,721 | 581.0 | 1.05 (1.01-1.10) | .026 | 379 | 100 | 263.9 | 1.05 (0.83-1.33) | .744 | 3,149 | 1,884 | 598.3 | 0.99 (0.95-1.03) | .617 | 21,839 | 11,774 | 539.1 | 0.94 (0.92-0.95) | <.001 | |
| 2021 | 3,106 | 1,876 | 604.0 | 1.04 (1.00-1.08) | .071 | 391 | 117 | 299.2 | 1.13 (0.90-1.42) | .298 | 3,200 | 1,953 | 610.3 | 1.02 (0.98-1.06) | .330 | 20,036 | 10,022 | 500.2 | 0.93 (0.91-0.95) | <.001 | |
| High | 2017 | 1,017 | 614 | 603.7 | 164 | 41 | 250.0 | 798 | 463 | 580.2 | 8,765 | 5,706 | 651.0 | ||||||||
| 2018 | 1,071 | 653 | 609.7 | 1.01 (0.94-1.08) | .788 | 160 | 35 | 218.8 | 0.88 (0.59-1.30) | .515 | 902 | 570 | 631.9 | 1.09 (1.01-1.18) | .032 | 9,029 | 5,670 | 628.0 | 0.96 (0.94-0.99) | .001 | |
| 2019 | 1,203 | 738 | 613.5 | 1.01 (0.94-1.07) | .863 | 174 | 40 | 229.9 | 1.05 (0.70-1.57) | .896 | 926 | 576 | 622.0 | 0.98 (0.92-1.06) | .664 | 9,008 | 5,513 | 612.0 | 0.97 (0.95-1.00) | .028 | |
| 2020 | 1,315 | 831 | 631.9 | 1.03 (0.97-1.09) | .344 | 153 | 34 | 222.2 | 0.97 (0.65-1.45) | .895 | 983 | 597 | 607.3 | 0.98 (0.91-1.05) | .511 | 8,909 | 5,023 | 563.8 | 0.92 (0.90-0.94) | <.001 | |
| 2021 | 1,385 | 932 | 672.9 | 1.06 (1.01-1.13) | .026 | 133 | 36 | 270.7 | 1.22 (0.81-1.83) | .408 | 1,046 | 607 | 580.3 | 0.96 (0.89-1.03) | .222 | 8,268 | 4,419 | 534.5 | 0.95 (0.92-0.97) | <.001 | |
ADHD = attention-deficit/hyperactivity disorder; RR = relative risk.
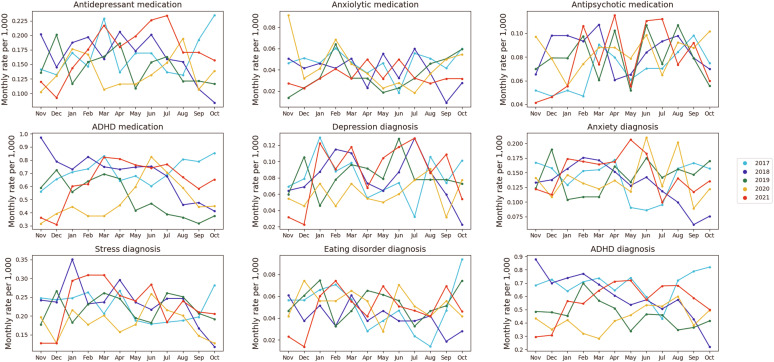
First, we explored the yearly outlook of all the outcomes tested by plotting the monthly incidence rates of an outcome per 1,000 members for each year from 2017 to 2021. In the beginning of the COVID-19 pandemic (March-April 2020), we observed a drastic decrease in the rates of all diagnoses and medications, corresponding to the first, and strictest, lockdown. However, from May 2020, rates of most diagnoses and medications increased and were high throughout 2021 compared to the years before the pandemic (Figure 1 ). To quantify the pandemic’s effect on adolescents’ mental health, we compared the relative risk in the pre-COVID-19 period (2019 vs 2017) and during the COVID-19 period (2021 vs 2019) (Table S3, available online; Figure 2 ). Among adolescents without psychiatric history, the analysis of the COVID-19 period presented sharp rises in mental health outcomes such as a 36% increase in depression (RR = 1.36; 95% CI = 1.25-147), 31% in anxiety (RR = 1.31; 95% CI = 1.23-1.39), 20% in stress (RR = 1.20; 95% CI = 1.13-1.27), 50% in eating disorders (RR = 1.50; 95% CI = 1.35-1.67), 25% in antidepressants (RR = 1.25; 95% CI = 1.25-1.33), and 28% in antipsychotics (RR = 1.28; 95% CI = 1.18-1.40). We found a decrease in ADHD diagnoses (RR = 0.84; 95% CI = 0.80-0.88) and corresponding prescriptions of ADHD agents (RR = 0.90; 95% CI = 0.86-0.93). Among adolescents with psychiatric history (Table S4, available online) a significant increase during COVID-19 period was measured in anxiety (RR = 1.08; 95% CI = 1.01-1.15), eating disorders (RR = 1.34; 95% CI = 1.17-1.52) and antidepressants (RR = 1.09; 95% CI = 1.06-1.13). Significant decrease was measured in ADHD diagnoses (RR = 0.90; 95% CI = 0.89-0.92) and prescriptions of ADHD agents (RR = 0.87; 95% CI = 0.86-0.86).
Figure 1.
Monthly Incidence Rates of Mental Health Diagnoses and Drug Dispensation, Comparison by Years
Note: ADHD = attention-deficit/hyperactivity disorder.
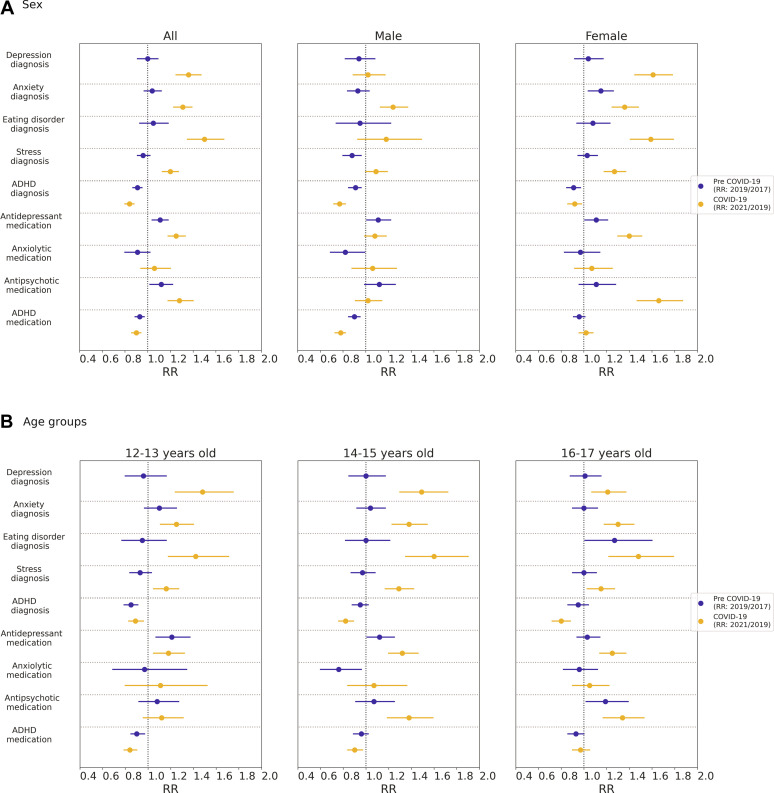
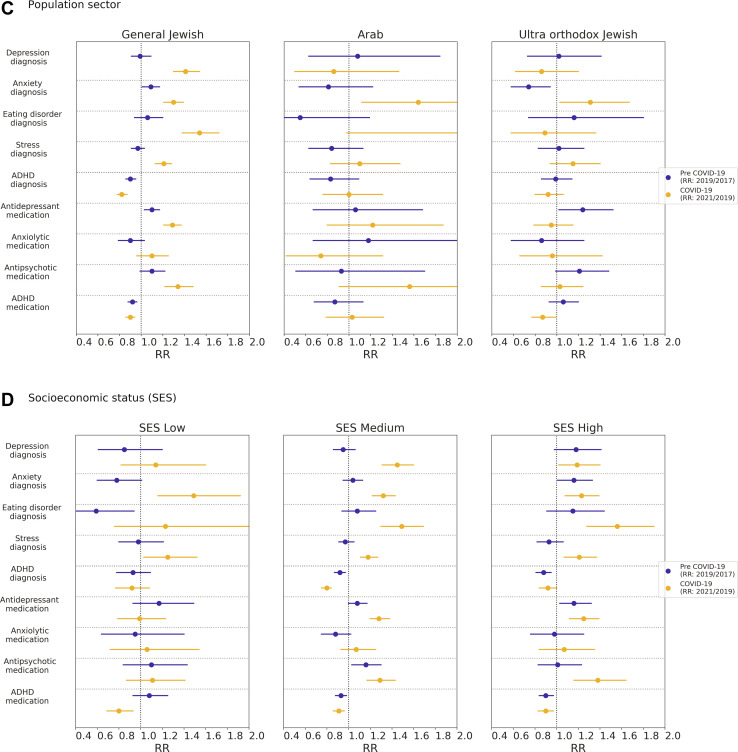
Figure 2.
Relative risks (RRs) and 95% CIs of Incidence Rates During Pre−COVID-19 and COVID-19 Periods
Note:(A) Sex; (B) age group; (C) population sector; (D) socioeconomic status.Blue lines indicate pre−COVID-19 period (RR: 2019 year rate/2017 year rate); orange lines indicate COVID-19 period (RR: 2021 year rate/2019 year rate). ADHD = attention-deficit/hyperactivity disorder.
In the sex-stratified analyses, most of the increase in incidence rates was associated with female participants, whereas male participants generally presented with risk rates that were not significantly different from previous years (see Table S3, available online; Figure 2A). Although in the pre−COVID-19 period a significant increase among female individuals was measured only in anxiety diagnoses (RR = 1.15; 95% CI = 1.04-1.26) and antidepressant dispensation (RR = 1.11; 95% CI = 1.01-1.21), during the COVID-19 period we observed significant increases in incidence rates of depression (RR = 1.61; 95% CI = 1.45-1.88), anxiety (RR = 1.36; 95% CI = 1.25-1.48), stress (RR = 1.27; 95% CI = 1.18-1.37), eating disorders (RR = 1.59; 95% CI = 1.41-1.79), antidepressant use (RR = 1.40; 95% CI = 1.3-1.51), and antipsychotic use (RR = 1.66; 95% CI = 1.47-1.80). The only significant increase diagnosis measured in male individuals during the COVID-19 period was 24% in anxiety (RR = 1.24; 95% CI = 1.13-1.37). Among adolescents with a psychiatric history, significant increases in rates of anxiety (RR = 1.11; 95% CI = 1.01-1.22) and eating disorders (RR = 1.31; 95% CI = 1.15-1.51) were observed only in female individuals (see Table S4, available online). Antidepressant dispensation was increased in both female (RR = 1.10; 95% CI = 1.05-1.15) and male (RR = 1.08; 95% CI = 1.03-1.14) individuals. ADHD diagnosis and medications dispensation were significantly decreased in both sexes.
Age-stratified incidence analyses have shown a significant increase during the COVID-19 period in diagnoses of depression, anxiety, stress, and eating disorders among all the groups, with the highest increase observed in 14- to 15-year-olds (see Table S3, available online; Figure 2B). This group presented significant increases in diagnoses of depression (RR = 1.49; 95% CI = 1. 1.30-1.72), anxiety (RR = 1.38; 95% CI = 1.23-1.54), stress (RR = 1.29; 95% CI = 1.17-1.42), and eating disorders (RR = 1.60; 95% CI = 1.35-1.90). Furthermore, the incidence rates of antidepressants and antipsychotics dispensation had the most pronounced increase among the same age group (RR = 1.32; 95% CI = 1.20-1.46 and RR = 1.38; 95% CI = 1.19-1.59, respectively). Among adolescents with a psychiatric history, significant increases in rates of depression (RR = 1.30; 95% CI = 1.04-1.63) and anxiety (RR = 1.14; 95% CI = 1.01-1.28) were found only in the 14- to 15-year-old age group (see Table S4, available online). Increased rates of eating disorders were found across all age groups, with the largest increase among 12- to 13-year-olds (RR = 1.72; 95% CI = 1.16-2.55).
The Israeli society is composed of different sectors that usually present with considerable disparities between them; therefore, we stratified the pandemic effect on mental health outcomes of adolescents by sector. The sector-stratified analyses showed that most of the increase in the incidence rates of psychiatric diagnoses and medications dispensation was associated with the general Israeli population. A single significant increase was observed in the Israeli Arab and ultra-orthodox communities in anxiety diagnosis (see Table S3, available online; Figure 2C). The incidence rates of anxiety in the ultra-orthodox community increased by 31% during the pandemic period (RR = 1.31; 95% CI = 1.03-1.67) and among Israeli Arabs by 64% (RR = 1.64; 95% CI = 1.12-2.40). Among adolescents with a psychiatric history, a significant increase in rates of anxiety (RR = 1.08; 95% CI = 1.01-1.15), eating disorders (RR = 1.31; 95% CI = 1.15-1.50), and antidepressant (RR = 1.09; 95% CI = 1.05-1.13) and anxiolytic (RR = 1.25; 95% CI = 1.01-1.53) dispensations were observed only in the general Israeli population (see Table S4, available online).
Subgroup analysis by SES (Figure 2D) was done by stratifying the cohorts into 3 groups: low (12%), medium (60%), and high (25%) SES. The medium and high SES groups presented a more distinct change, showing significant incident increases in 6 outcomes: depression (RR = 1.45; 95% CI = 1.31-1.60; RR = 1.19; 95% CI = 1.02-1.40, respectively), anxiety (RR = 1.32; 95% CI = 1.22-1.43; RR = 1.23; 95% CI = 1.08-1.39), eating disorders (RR = 1.49; 95% CI = 1.30-1.69; RR = 1.56; 95% CI = 1.28-1.90), stress (RR = 1.18; 95% CI = 1.11-1.27; RR = 1.21; 95% CI = 1.07-1.37), antidepressants dispensation (RR = 1.28; 95% CI = 1.20-1.38; RR = 1.25; 95% CI = 1.12-1.39), and antipsychotics dispensation (RR = 1.29; 95% CI = 1.17-1.43; RR = 1.38; 95% CI = 1.16-1.64). In the low SES group, the increase was less visible, with only 2 significantly increased outcomes: anxiety (RR = 1.49; 95% CI = 1.16-1.92) and stress (RR = 1.25; 95% CI = 1.03-1.52). The decrease in ADHD agents was observed across all SES groups. Notably, we observed among the high SES group a significant increase in prescription of antidepressants (RR = 1.16; 95% CI = 1.03-1.32), and among the medium SES group a significant increase in prescription of antipsychotics (RR = 1.16; 95% CI = 1.03-1.30) for the pre-pandemic period. Adolescents with a psychiatric history had a significantly increased rate of anxiety in the high SES group (RR = 1.15; 95% CI = 1.01-1.31), increased rate of stress in the medium SES group (RR = 1.09; 95% CI = 1.01-1.17), and increased rates of eating disorders and antidepressants in the medium and high SES groups (Table S4, available online).
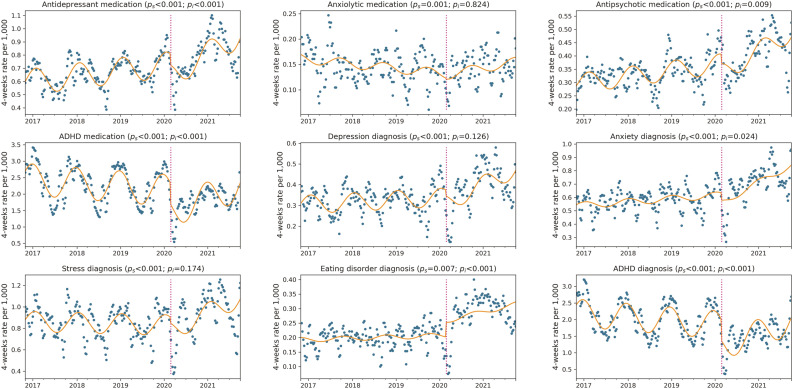
To enable a more refined analysis examining to what extent the trends during the COVID-19 era are continuations of past trends and to what extent they break away from them, we performed Interrupted Time Series (ITS) analysis. We evaluated 7 different models for this analysis that differed in the time periods used to fit the data and the number of interruption points (Figures S1-S7, available online). We observed that following a decline in incidence rates during the first lockdown (from mid-March to the end of April 2020), there was an increase in incidence rates of all diagnoses and medications dispensation, which was significantly higher than the trend in previous years (Figure 3 ). Varying the analysis by introducing a “gap” period during this first lockdown period, and optionally also during the following month, so as not to be biased by the initial sharp decline, led to qualitatively comparable results (Figures S2-S5, available online). Introducing a second interruption point on March 7, 2021, the day that all schools were opened following an extensive vaccination campaign, resulted in a significant decline following that point in the incidence of antidepressant and anxiolytic dispensation as well as of diagnoses of anxiety, stress, and eating disorders (Figure S6 and Table S5, available online). During May 2021, an additional geo-political stressor unrelated to the COVID-19 pandemic appeared in Israel, where the Israeli−Palestinian conflict escalated into violent outbreaks throughout the country. Because this crisis may have further exacerbated the mental health situation is Israel, we analyzed data with the gap between May 6 and June 21. The results were nearly identical to those in the previous models, suggesting that the crisis did not have a direct effect on the underlying trend (Figure S7, available online).
Figure 3.
Interrupted Times Series Analysis (ITS) for Mental Health Incidence for 5 Years
Note:Magenta line delineates February 27, the date of the first COVID-19 case in Israel. Orange lines depict ITS models with an interruption on this date. Blue dots represent incidence rates for a 4-week period. ADHD = attention-deficit/hyperactivity disorder.
Discussion
The COVID-19 pandemic has taken a toll on the mental health and well-being of children and adolescents. Whereas most recent studies used surveys to assess the status of mental health in adolescents,5 we approached the issue from a quantitative perspective and compared new psychiatric diagnoses and drug dispensation in adolescents with and without psychiatric history, before and during the COVID-19 pandemic, based on comprehensive EHR data. Consistent with published surveys showing a sharp increase in mental health disorders,5 , 16 we observed from EHR data a significant increase in diagnoses of depression, anxiety, stress, and eating disorders during the pandemic compared to previous years. Importantly, this study found a sharper increase in the incidence of psychiatric outcomes among youth without a psychiatric history compared to youth with a psychiatric history. Our study supports previous findings and shows that adolescents without a psychiatric history had a higher risk of developing mental health outcomes from the pre-pandemic to the pandemic period, whereas among adolescents with a psychiatric history this risk was moderate and mostly related to diagnoses of anxiety and eating disorders.
These observations of a rise in psychiatric diagnoses and dispensed medications can be attributed to a wide range of stressors that appeared during the pandemic. The increase in depression, anxiety, and stress might have been a result of the following: fear of morbidity and mortality (to self or loved ones) from the new unknown illness; excessive media exposure with alarming content; continuous changes in guidelines and restrictions that led to prolonged social isolation, loss of peer interactions, and support during school closures; reduced extracurricular and physical activity; disruption of daily routines; decreased hope for the future; and loss of pleasure in activities.17 , 18 The introduction of new distance learning technologies imposed new challenges involving constant self-observation through cameras and different academic success evaluation, compromising adolescents’ self-esteem.19, 20, 21 Eating disorders are associated with body dissatisfaction, poor self-esteem, and depression.22 In addition, eating disorders behaviors may arise as ways to gain control and compensate for the uncertainty of the new reality that was imposed by the pandemic.23 Although the increase in psychiatric drug dispensation was mostly aligned with the corresponding diagnoses, the increase in antipsychotic drug dispensation was not associated with any specific diagnosis measured in this study. The latter, which was particularly pronounced in female individuals, might indicate incidences of self-harm and personality disorders.24 However, there are limited data from which to draw conclusions about specific reasons for the increase in antipsychotic use, and further research is needed. Among the reasons for increased incidence of psychiatric outcomes, we should also consider the extended time periods that adolescents spent at home with their immediate family, which may have promoted enhanced parental awareness and increased legitimacy to discuss mental distress during these times.25 Notably, the interrupted time series analysis, which included interruption points for the first closure and then the full reopening of schools, indicates that, at least for some mental health outcomes (antidepressant and anxiolytic treatment, as well as anxiety, stress, and eating disorder diagnoses), the “return to normality” was associated with a decrease in the incidence of these outcomes. Although, in this study, the rates of depression and anxiety increased during the COVID-19 period, we observed a reduction in the incidence rates of ADHD diagnoses and prescription medications. As reports in recent years have shown an overall rise in ADHD diagnoses and medications,26 one explanation of our findings might be the tight association between ADHD incidence and school activity.27 , 28 Because the COVID-19 period was characterized by intermittent closure of schools, this observed reduction in diagnoses and drug use is in line with the decrease during a normal school year’s summer break. Another reason for the decrease in ADHD diagnoses and prescription medications could be that psychiatric cases such as depression and anxiety seemed more urgent and were given priority in limited slots for patient care. These findings may suggest under-diagnosed and untreated ADHD in adolescents during school closures, putting them at risk for more serious outcomes, such as increased rates of criminal activity, accidents, as well as anxiety and depression.28 However, a decrease in ADHD rates might be a temporary event and indicate a delay in evaluation or diagnosis, due to limited resources during the pandemic.
The most significant finding in this study is the greater risk among adolescent female compared with male individuals to be diagnosed with a variety of mental disorders for the first time during the pandemic. In this EHR analysis, risk for anxiety was the only significant mental outcome that was increased among male participants. These findings are consistent with previous studies that suggested that loneliness was associated with elevated depression symptoms in female individuals and with elevated social anxiety in male individuals.29 , 30 Other studies found both increased depressive and anxiety symptoms among female participants.3, 4, 5 Previous studies of pandemics have shown that such events often widen health inequalities in society and have a greater impact on socially disadvantaged groups.31 A recent systematic review has shown that inequality factors such as female sex and young age were likely to increase risk for adverse mental health outcomes during the COVID-19 outbreak.32 The World Health Organization (WHO) reported lower levels of mental health and life satisfaction among female compared to male individuals.33 Gender differences in mental disorders are known and consistent in the field of psychiatry, but the reasons for these differences are still not clear enough.34 The potential risk factors could be the influence of sex hormones, higher rates of interpersonal stressors, female individuals’ lower baseline self-esteem and higher tendency toward a negative body image, exposure to stress associated with lack of gender equality and discrimination, and greater chance of experiencing interpersonal violence.35 Importantly, mental distress among male adolescents may manifest in ways that are not directly reported in the EHR, such as violence, dropout, and substance abuse.
Stratifying by age, our findings show that there was an increase in mental illness in all age groups that was more pronounced among 14- to 15-year-olds. Yet, as described in previous studies,5 we found that the absolute incidence rates of depression, anxiety, and the associated medication were highest among 16- to 17-year-olds. High rates among older adolescents may be due to changes associated with puberty, a response to the stress of lockdowns and the global pandemic, and lack of socialization with peers, which is particularly important at this age. In younger children, increased anxiety and depression may be more readily attributed to changes in routine.35
Comparing the sectors in the Israeli population showed that different circumstances and lifestyle during the COVID-19 period are associated with different mental health outcomes in adolescents. In the ultra-orthodox community, we observed a significant increase only in the diagnosis of anxiety (31%). Ultra-orthodox Jews, accounting for 12% of the Israeli population, form closely-knit religious communities, living by strict Jewish laws and tradition.36 In this sector, the pandemic caused tension between governmental instructions and instructions from prominent community leaders who advocated keeping schools open for holy studies.37 Many media venues such as television, the Internet, and secular newspapers are not used in this sector, potentially buffering them from the exacerbating impact of reports and discussions in these venues. Moreover, although in recent years there is a growing openness and legitimacy for discussing mental health in this community, use of mental health services is still much lower than in the general Israeli population.37 Similar to the ultra-orthodox sector, in the Israeli Arab sector we observed a significant increase only in the diagnosis of anxiety (64%). This sector, which accounts for 20% of the total Israeli population, uses mental health services at a much lower rate than the rest of the population, possibly due to lower access to health care services, as many persons reside in peripheral areas, as well as negative cultural perception and stigma associated with mental health problems.38
A significant increase in mental health diagnoses during the COVID-19 pandemic period was observed across different SES. In contrast to previous studies reporting that children and adolescents who grow up in families with lower SES have more symptoms of anxiety and depression,39 the incidence rates of most diagnoses in this study increased with higher SES. Distinctly in Israel, the Israeli Arab and ultra-orthodox communities are associated with lower SES37 and, as mentioned earlier, in these sectors the rates of mental health diagnoses are lower than in the rest of the population for cultural, religious, and other reasons. Although lower SES is often associated with poor mental health, other mediators might affect this association. Social engagement with friends and family is linked to better mental health and affects the link between SES and mental health.40 Ultra-orthodox communities in Israel are usually of lower SES; nevertheless, they are socially active environments that provide members with social and spiritual support.41 The community settings offer psychosocial engagement and continuous assistance, which results in better health and mental health than would be expected based on their SES.41
Our study has several limitations. First, although the findings in this study are clear and consistent with those of other studies, the reported rates are probably an underestimation of the actual numbers. Some adolescents are diagnosed and treated by mental health professionals in private clinics outside their HMO, and such diagnoses and psychiatric drugs are not recorded in their EHR. However, most of those who receive private psychiatric treatment still contact a physician from the HMO to get a prescription for drugs and thus to receive a subsidy for the purchase. Data on the proportion of private treatments are not available, but purchases of prescription drugs were fully captured in this database. Furthermore, there is a long standby time for mental health services, starting at an average of 3 months before an initial assessment, and several additional months before receiving treatment42; therefore, not all those who seek and need help are included in this study. This information bias is likely non-differential. Our analysis addressed this limitation by comparing the risk ratios of the outcomes, measuring the difference in rates of mental health diagnoses and dispensations within the HMO in different time periods. Second, some under-reporting is expected during the pandemic for non-fatal mental health events, which would bias our results towards the null. Nevertheless, a significant association was observed, although its magnitude may have been a conservative estimate.
In conclusion, this observational cohort study is the first data-driven quantitative estimation of the mental health burden on adolescents during the COVID-19 pandemic that showed a significant increase in mental health diagnoses and psychiatric drugs dispensation compared to the corresponding pre-COVID period. Our findings highlight the specific subpopulations that need to be considered when deciding on policies and promotion of adolescent resilience. These findings should warrant similar studies in other geographical areas and in other age groups. Policy makers should prioritize strategies to address the deteriorating mental health of adolescents during the COVID-19 pandemic and to prevent further escalation.
Acknowledgments
The authors wish to thank Joseph Levi, PhD, of the Clalit Innovation and Yair Goldberg, PhD, of the Technion for helpful comments and discussion on the Interrupted Time Series methodology. Chen Yanover, PhD, and Tal El-Hay, PhD, of the KI Institute, are acknowledged for their insightful methodological suggestions and illuminating discussions. The authors thank Inbal Goldshtein, PhD, of the KI Institute, for her valuable comments and assistance in manuscript revision preparation.
Footnotes
The authors have reported no funding for this work.
The research was performed with permission from Maccabi Health Services’ Institutional Review Board (MH6-0006-21).
This work has been previously posted on a preprint server: https://www.medrxiv.org/content/10.1101/2022.01.06.22268809v2.
Inbal Goldshtein, PhD, of the KI Institute, served as the statistical expert for this research.
Author Contributions
Conceptualization: Bilu, Flaks-Manov, Kalkstein, Yehezkelli, Greenfeld
Data curation: Bilu
Formal analysis: Bilu
Investigation: Bilu, Bodenheimer
Methodology: Bilu, Flaks-Manov
Project administration: Akiva, Greenfeld
Supervision: Bivas-Benita, Yehezkelli, Mizrahi-Reuveni, Ekka-Zohar, Shapiro Ben David, Lerner, Bodenheimer, Greenfeld
Writing – original draft: Flaks-Manov, Bivas-Benita
Writing – review and editing: Bilu, Akiva, Shapiro Ben David, Lerner, Bodenheimer, Greenfeld
Disclosure: Drs. Bilu, Flaks-Manov, Bivas-Benita, Akiva, Yehezkelli, Mizrahi-Reuveni, Ekka-Zohar, Shapiro Ben David, Lerner, Bodenheimer, and Greenfeld and Mr. Kalkstein have reported no biomedical financial interests or potential conflicts of interest.
Supplemental Material
References
- 1.Götzinger F., Santiago-García B., Noguera-Julián A., et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4(9):653–661. doi: 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zimmermann P., Curtis N. Why is COVID-19 less severe in children? A review of the proposed mechanisms underlying the age-related difference in severity of SARS-CoV-2 infections. Arch Dis Child. 2021;106(5):429–439. doi: 10.1136/archdischild-2020-320338. [DOI] [PubMed] [Google Scholar]
- 3.Meherali S., Punjani N., Louie-Poon S., et al. Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health. 2021;18(7):3432. doi: 10.3390/ijerph18073432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thorisdottir I.E., Asgeirsdottir B.B., Kristjansson A.L., et al. Depressive symptoms, mental wellbeing, and substance use among adolescents before and during the COVID-19 pandemic in Iceland: a longitudinal, population-based study. Lancet Psychiatry. 2021;8(8):663–672. doi: 10.1016/S2215-0366(21)00156-5. [DOI] [PubMed] [Google Scholar]
- 5.Racine N., McArthur B.A., Cooke J.E., Eirich R., Zhu J., Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatrics. 2021;175:1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.https://datadashboard.health.gov.il/COVID-19/general Health.Gov.Il.
- 7.Brooks S.K., Webster R.K., Smith L.E., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pandya A., Lodha P. Social connectedness, excessive screen time during COVID-19 and mental health: a review of current evidence. Front Hum Dynam. 2021;3 https://www.frontiersin.org/articles/10.3389/fhumd.2021.684137 [Google Scholar]
- 9.Bu F., Steptoe A., Fancourt D. Loneliness during a strict lockdown: trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc Sci Med. 2020;265 doi: 10.1016/j.socscimed.2020.113521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joensen A., Danielsen S., Andersen P.K., Groot J., Strandberg-Larsen K. The impact of the initial and second national COVID-19 lockdowns on mental health in young people with and without pre-existing depressive symptoms. J Psychiatr Res. 2022;149:233–242. doi: 10.1016/j.jpsychires.2022.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hards E., Loades M.E., Higson-Sweeney N., et al. Loneliness and mental health in children and adolescents with pre-existing mental health problems: a rapid systematic review. Br J Clin Psychol. 2022;61(2):313–334. doi: 10.1111/bjc.12331. [DOI] [PubMed] [Google Scholar]
- 12.McKinlay A.R., May T., Dawes J., Fancourt D., Burton A. ‘You’re just there, alone in your room with your thoughts’: a qualitative study about the psychosocial impact of the COVID-19 pandemic among young people living in the UK. BMJ Open. 2022;12(2) doi: 10.1136/bmjopen-2021-053676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clarfield A.M., Manor O., Nun G.B., et al. Health and health care in Israel: an introduction. Lancet. 2017;389(10088):2503–2513. doi: 10.1016/S0140-6736(17)30636-0. [DOI] [PubMed] [Google Scholar]
- 14.Hananel R., Fishman R., Malovicki-Yaffe N. Urban diversity and epidemic resilience: the case of the COVID-19. Cities. 2022;122 doi: 10.1016/j.cities.2021.103526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernal J.L., Cummins S., Gasparrini A. Corrigendum to: Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2020;50(3):1045. doi: 10.1093/ije/dyaa118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cost K.T., Crosbie J., Anagnostou E., et al. Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatry. 2021:1–14. doi: 10.1007/s00787-021-01744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Figueiredo, Sandre P.C., Portugal L.C.L., et al. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Progress Neuro-Psychopharmacol Biol Psychiatr. 2021;106:110171. doi: 10.1016/j.pnpbp.2020.110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;4(6):421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bányai F., Zsila Á., Király O., et al. Problematic social media use: results from a large-scale nationally representative adolescent sample. PLoS One. 2017;12(1) doi: 10.1371/journal.pone.0169839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodgers R.F. The relationship between body image concerns, eating disorders and Internet use, part II: an integrated theoretical model. Adolesc Res Rev. 2016;1(2):121–137. doi: 10.1007/s40894-015-0017-5. [DOI] [Google Scholar]
- 21.McLean S.A., Jarman H.K., Rodgers R.F. How do “selfies” impact adolescents’ well-being and body confidence? A narrative review. Psychol Res Behav Manag. 2019;12:513–521. doi: 10.2147/PRBM.S177834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jebeile H., Lister N.B., Baur L.A., Garnett S.P., Paxton S.J. Eating disorder risk in adolescents with obesity. Obesity Rev. 2021;22(5) doi: 10.1111/obr.13173. [DOI] [PubMed] [Google Scholar]
- 23.Kilteni K., Maselli A., Kording K.P., Slater M. Over my fake body: body ownership illusions for studying the multisensory basis of own-body perception. Front Hum Neurosci. 2015;9 doi: 10.3389/fnhum.2015.00141. https://www.frontiersin.org/articles/10.3389/fnhum.2015.00141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hawton K., Witt K.G., Salisbury T.L.T., et al. Interventions for self-harm in children and adolescents. Cochrane Database Syst Rev. 2015;12 doi: 10.1002/14651858.CD012013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rider E.A., Ansari E., Varrin P.H., Sparrow J. Mental health and wellbeing of children and adolescents during the covid-19 pandemic. BMJ. 2021:374. doi: 10.1136/bmj.n1730. [DOI] [PubMed] [Google Scholar]
- 26.Ponizovsky A.M., Marom E., Fitoussi I. Trends in attention deficit hyperactivity disorder drugs consumption, Israel, 2005–2012. Pharmacoepidemiol Drug Saf. 2014;23(5):534–538. doi: 10.1002/pds.3604. [DOI] [PubMed] [Google Scholar]
- 27.Shyu Y.C., Lee S.Y., Yuan S.S., et al. Seasonal patterns of medications for treating attention-deficit/hyperactivity disorder: comparison of methylphenidate and atomoxetine. Clin Ther. 2016;38(3):595–602. doi: 10.1016/j.clinthera.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 28.Cohen H.A., Savitsky B., Ashkenasi A., Hoshen M. Seasonality of methylphenidate administration among children in Israel. Isr Med Assoc J. 2016;18(11):655–660. [PubMed] [Google Scholar]
- 29.Liu H., Zhang M., Yang Q., Yu B. Gender differences in the influence of social isolation and loneliness on depressive symptoms in college students: a longitudinal study. Soc Psychiatry Psychiatr Epidemiol. 2020;55(2):251–257. doi: 10.1007/s00127-019-01726-6. [DOI] [PubMed] [Google Scholar]
- 30.Loades M.E., Chatburn E., Higson-Sweeney N., et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218–1239. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bambra C., Riordan R., Ford J., Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020;74(11):964–968. doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gibson B., Schneider J., Talamonti D., Forshaw M. The impact of inequality on mental health outcomes during the COVID-19 pandemic: a systematic review. Can Psychol. 2021;62:101. doi: 10.1037/cap0000272. [DOI] [Google Scholar]
- 33.World Health Organization . Health behaviour in school-aged children (HBSC) study: international report from the 2013/2014 survey. WHO Regional Office for Europe; Copenhagen: 2016. [Google Scholar]
- 34.Riecher-Rössler A Sex and gender differences in mental disorders. Lancet Psychiatry. 2017;4(1):8–9. doi: 10.1016/S2215-0366(16)30348-0. [DOI] [PubMed] [Google Scholar]
- 35.Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4(2):146–158. doi: 10.1016/S2215-0366(16)30263-2. [DOI] [PubMed] [Google Scholar]
- 36.Coleman-Brueckheimer K., Dein S. Health care behaviours and beliefs in hasidic jewish populations: a systematic review of the literature. J Relig Health. 2011;50(2):422–436. doi: 10.1007/s10943-010-9448-2. [DOI] [PubMed] [Google Scholar]
- 37.Saban M., Myers V., Shachar T., Miron O., Wilf-Miron R.R. Effect of socioeconomic and ethnic characteristics on COVID-19 infection: the case of the ultra-orthodox and the Arab communities in Israel. J Racial Ethnic Health Disparities. 2021:1–8. doi: 10.1007/s40615-021-00991-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chernichovsky D., Bisharat B., Bowers L., Brill A., Sharony C. The health of the Arab Israeli population. State of the Nation Report. 2017;325:8–20. [Google Scholar]
- 39.Verhulst F., Tiemeier H. In: Mental Health and Illness of Children and Adolescents. Mental Health and Illness Worldwide. Taylor E.A., Verhulst F.C., Wong J., Yoshida K., Nikapota A., editors. Springer; 2020. Socioeconomic inequalities and mental health problems in children and adolescents; pp. 257–274. [DOI] [Google Scholar]
- 40.Achdut N., Sarid O. Socio-economic status, self-rated health and mental health: the mediation effect of social participation on early-late midlife and older adults. Isr J Health Policy Res. 2020;9(1):4. doi: 10.1186/s13584-019-0359-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tchernichovsky D., Sharoni C. The connection between social capital and health among the ultra-orthodox. State of the Nation Report. 2015:383–409. [Google Scholar]
- 42.Sterne A., Porter B. Overview of child and adolescent mental health services in Israel. Myers-JDC-Brookdale Institute, Smokler Center for Health Policy Research. 2013. https://brookdale.jdc.org.il/en/publication/overview-child-adolescent-mental-health-services-israel/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.