Abstract
The distal radioulnar joint (DRUJ), the articulation between the sigmoid notch of the radius and the distal ulna, plays a pivotal role in stability and load bearing and allows for pronation and supination of the forearm. Osteoarthritis (OA) of the DRUJ commonly occurs due to distal radius trauma but may also be the result of conditions such as joint instability, septic arthritis, or primary OA. It is initially managed with conservative therapy, but surgery is often considered when nonoperative methods fail. The surgical approaches available to treat this pathology have grown over the years. The procedures have generally favorable outcomes, each with their own unique complications and considerations. This paper comprises a review of the outcomes and complications for the different procedures commonly used to surgically treat DRUJ OA.
Keywords: distal radioulnar joint, osteoarthritis, Darrach, Sauve-Kapandji, hemi-resection
Introduction
The distal radioulnar joint (DRUJ) is the articulation between the sigmoid notch of the radius and the distal ulna. Its plays a pivotal role in stability and load bearing and allows for pronation and supination of the forearm. However, the bony components of the joint provide minimal stability and rely on the soft tissue support which is primarily provided by the triangular fibrocartilage complex (TFCC) including the distal radioulnar ligaments to maintain stability. Disruption of this support allows for excessive translation and shearing of the joint, leading to the development of osteoarthritis (OA). This commonly occurs following trauma to the distal radius, occurring in 11 to 19% of cases, but may also be the result of joint instability, septic arthritis, or primary OA. 1
Degeneration of the articular surface of the DRUJ is a common cause of wrist pain and functional impairment. Initially, this pathology can be managed conservatively with physiotherapy, anti-inflammatory medication, splinting, or even a corticosteroid injection. When conservative management such as activity modification, medication, bracing, or corticosteroid injections are not effective, surgery is considered. Since the early 20th century, several surgical approaches have been developed to treat this pathology. Surgical options include resection of the ulnar head (Darrach procedure), which was first described in 1855 and then later popularized in 1913 by the eponymous William Darrach. 2 3 Another popular technique is the Sauvé-Kapandji procedure, which combines arthrodesis of the DRUJ with ulna resection proximal to the sigmoid notch, creating a distal ulnar pseudoarthrosis. 4 Bowers described a procedure which involves distal ulnar hemi-resection and tendon interposition. 5 Over the years, several modifications to these surgical choices have been developed for specific pathologic circumstances. 6 7 8 Furthermore, recent studies have supported the use of ulnar head implant arthroplasty as a primary or salvage procedure for DRUJ arthrosis. 9
Despite multiple studies comparing these various surgical approaches, it has been difficult to derive evidence-based criteria for procedure choice due to varying results, follow-up time, limited number of cases, and differing outcome measures. In practice, surgical choice is based on multiple factors, including patient age, functional demands, degree of pathology, and associated complications. Physicians often choose the surgical procedure based on fellowship training, personal experience, and surgical level of comfort. In lieu of validated guidelines, we present an up-to-date review of the literature on the outcomes and complications of these techniques for OA of the DRUJ.
Darrach Procedure
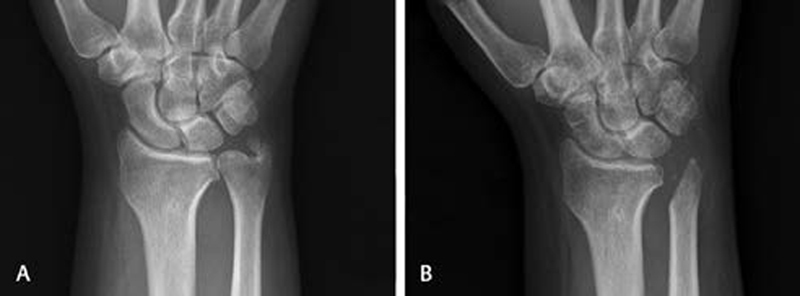
The Darrach procedure involves a subperiosteal resection of the distal ulna just proximal to the sigmoid notch of the radius ( Fig. 1 ). This procedure has traditionally been utilized for DRUJ OA pain relief and improvement in range of motion, with approximately 80% of patients reporting pain relief following the procedure. 10 However, minimal improvement of functional outcomes and occurrence of complications including grip strength weakness, stump instability, and ulnar translation, leading to painful radioulnar convergence have been reported. 11 12 13 This has led to the belief that the technique should be reserved for older patients who have lower functional demands.
Fig. 1.

A 55-year old-male with distal radioulnar joint arthritis secondary to Colles' fracture scheduled for Darrach. ( A ) Preoperative posteroanterior radiograph. ( B ) A 1-month postoperative posteroanterior radiograph. ( C ) Preoperative lateral radiograph. ( D ) A 1-month postoperative lateral radiograph.
Attempts have been made to alleviate these common complications through multiple modifications of the traditional technique. Now many incorporate soft tissue supports to reduce the likelihood of proximal ulnar stump instability and convergence. Tulipan et al described a surgical modification by creating a dorsal-based flap of the extensor retinaculum passed beneath the extensor carpi ulnaris (ECU) tendon and then sutured to itself and the dorsal retinaculum. This structure serves as a sling loop bringing the ECU tendon more dorsally and eliminating the tendon's ulnar pull. 6 They reported good to excellent results in 91% of patients, as well as significant improvements in extension (58%), flexion (40%), pronation (40%), and supination (60%) compared with preoperative range of motion over an average follow-up of 54.4 months. Breen et al and more recently Chu et al described a modification that involves passing a distally based, bisected strip of the ECU tendon through the ulnar collateral ligament, a drill hole through the ulnar stump, and the interosseous membrane. 8 14 The remaining tendon is placed dorsally over the ulnar stump and is stabilized by the extensor retinaculum. 8 14 Both authors reported no patient complications related to stump instability at last follow-up.
More recent studies are concordant with these findings. De Witte et al evaluated 26 patients with post-traumatic DRUJ arthritis treated with the Darrach procedure, where the primary surgical indication was to increase mobility more than pain relief. 15 Their study population had a mean follow-up of 21 months and a patient average age of 53 years. They found that there was a significant improvement in the arc of forearm rotation, from 49 degrees preoperatively to 136 degrees postoperatively ( p < 0.001), and that 19 of 26 (73%) of patients reported pain relief. Two patients required a reoperation, one for malunion of the radius and the other to remove bony protuberances from the ulnar stump that were associated with pain. Five patients had dynamic radioulnar convergence on radiography, but none were associated with pain or functional impairment.
In 2012, Grawe et al published their long-term outcomes with a retrospective review of 27 patients treated with Darrach procedure for post-traumatic DRUJ arthritis. 16 Their study population had an average age of 51 years with an average follow-up time of 13 years. Grawe et al reported an average pronation of 85 degrees, supination of 78 degrees, flexion of 41 degrees, and extension of 45 degrees post procedure. There were no reports of distal ulna instability, clicking, or pain. Thirteen patients had dynamic radioulnar convergence by radiography, but it was not associated with pain or reoperation in any patients.
Most recently, Jochen-Frederick et al retrospectively evaluated 37 patients with post-traumatic and chronic DRUJ OA. 17 Their patient population had a mean age of 52 years with an average follow-up time of 53 months. They reported a postoperative active motion arc (pronation and supination) of 89.7% compared with the contralateral side and a grip strength of 57.1% of the contralateral side. Their mean DASH score postoperatively was 25.5 and a decrease in VAS pain scale from 6.5 to 2.2 was noted. Two patients had persistent pain in the ulnar stump, with one requiring revision surgery.
These recent studies put into question historical concerns of the Darrach procedure. Innovations in the surgical technique have led to improvements in both objective and subjective outcomes. Grip strength improvements continue to be limited. Radioulnar convergence, a frequently reported complication of the Darrach procedure, is diagnosed based on radiography and often does not influence patient outcomes or pain. Ulnar translation of the carpus postoperatively is rarely reported when performing this procedure for individuals with painful DRUJ OA. These recent results suggest the Darrach procedure remains a good option for many patients with DRUJ OA.
Sauve-Kapandji Procedure
The Sauve-Kapandji (SK) procedure is an arthrodesis of the head of the ulna to the radius at the DRUJ ( Fig. 2 ). It also involves creation of pseudoarthrosis with resection of a portion of the ulna shaft proximal to the sigmoid notch to allow forearm rotation. For OA of the DRUJ, the SK procedure can be especially useful when there is associated destruction of the TFCC or a positive ulnar variance with ulnar carpal abutment. The benefit of maintaining the ulnar head is preserving soft tissue attachments distally, which stabilize the carpus, preventing possible ulnar carpal translation and theoretically allowing for maintenance of wrist function. For these reasons, the procedure is often considered to be the first choice for young, active patients looking to maintain wrist function.
Fig. 2.

A 64-year-old female with primary distal radioulnar joint osteoarthritis scheduled for Sauve-Kapandji. ( A ) Preoperative posteroanterior radiograph. ( B ) A 7-month posteroanterior radiograph. ( C ) Preoperative lateral radiograph. ( D ) A 7-month postoperative lateral radiograph.
Several studies related to the SK procedure support the claims of good functional outcomes. 18 19 20 Zimmerman et al evaluated 117 patients treated with the SK procedure for DRUJ OA over an average follow-up of 8 years. 18 They noted pain reduction in 97% of patients down to a mean of 1.6 points on VAS, with 91% having no pain at the proximal ulnar stump. They further noted significant improvement in forearm rotation increasing 53% from baseline and achieving approximately 80% of the rotation of the contralateral side. Grip strength improvement went from 38% to 55% of the contralateral arm. In a retrospective review of 15 patients treated with the SK procedure for DRUJ OA, Czermak et al found an improvement in forearm rotation from 89.3 to 142.7 degrees as well as an improvement in grip strength by 63.6% over baseline after an average follow-up of 55 months. 19 Most recently, Giberson-Chen et al performed a retrospective study including 42 patients with DRUJ OA with a mean follow-up of 24.5 months. 20 They found that qDASH decreased from 52 preoperatively to 28 postoperatively and that supination significantly increased from 48 to 74 degrees in 12 months.
The residual proximal ulnar stump created by the procedure leads to similar complications found with the Darrach procedure, primarily proximal stump instability and radioulnar convergence. Radioulnar convergence can be easily demonstrated on a horizontal posteroanterior X-ray while the patient holds a 5-pound weight in their hand. 21 Earlier reports on the procedure showed painful instability as a common complication in treated patients. 22 23 Similar modifications have been developed for the SK procedure to avoid these complications. In 2000, Minami et al described a modification that involved dividing the ECU tendon while maintaining its musculotendinous junction. 24 This strip is then passed through a drill hole created within the proximal ulna stump and sutured back on itself, providing stability to the ulnar stump. Recently, Tomori et al performed a retrospective analysis with short-term follow-up of 17.5 months comparing clinical and radiographic results for the SK procedure with and without ECU tendon stabilization. 25 They found stump pain in 6 wrists of 13 (46%) in the group without stabilization compared with 0 wrists of 11 in the ECU tendon stabilization modification group, but noted no differences in functional or radiographic outcomes. Stabilizing the proximal ulnar stump with the ECU tendon proves to be an effective method for treating a common complication of this procedure.
The arthrodesis created in the procedure lends itself to unique complications, primarily nonunion. Re-ossification can be seen at the site of the created pseudoarthrosis, resulting in limited forearm rotation. Overall, the occurrence of these complications is relatively rare; Zimmerman et al only reported two instances of re-ossification and no instances of nonunion in their cohort of 117 patients. 18 Similarly, out of their 43 OA patients, Giberson-Chen et al noted four incidences of re-ossification and no instances of nonunion. 20 Nonunion seems to be a complication more frequently referenced for DRUJ rheumatoid arthritis rather than DRUJ OA. 26 Painful re-ossification is typically managed with a revision osteotomy; however, Lluch et al reported good results in three patients treated with steroids and rest alone. 27
While the literature on the SK procedure has been heterogeneous in terms of patient population, follow-up, and outcome measures, a few conclusions can be made. The SK procedure generally improves functional outcome measures and reduces pain when used for the treatment of DRUJ OA. The two most common complications include proximal stump instability and painful radioulnar convergence which can be reduced with soft tissue stabilization techniques. Nonunion and re-ossification represent rare complications of the procedure that can be reliably managed with revision procedures.
Distal Ulnar Hemi-Resection Arthroplasty
The DRUJ and TFCC are critical in providing rotational mobility and stability of the radioulnar connection. 28 In 1985, Bowers reported the importance of maintaining ulnocarpal stability by conservation or reconstruction of the TFCC, which led to the development of the distal ulnar hemi-resection arthroplasty. 5 Other authors refer to this procedure as a hemi-resection interposition arthroplasty (HIA). This technique is described as removal of the ulnar articular cylinder and subchondral bone while maintaining a bony connection of the ulnar shaft and styloid ( Fig. 3 ). HIA allows for the preservation of soft tissues that stabilize the DRUJ, while interposition of a tendon into the defect maintains radioulnar separation. 5 28 Studies that specifically discuss outcomes of HIA for the treatment of OA are lacking. Many studies are retrospective in nature with small patient populations and heterogeneous pathology.
Fig. 3.
A 37-year-old male with post-traumatic distal radioulnar joint arthritis scheduled for hemi-resection interposition arthroplasty. ( A ) Preoperative posteroanterior radiograph. ( B ) A 2-week postoperative posteroanterior radiograph.
In his 1985 study, Bowers investigated 38 patients with an average of 2.5 years of follow-up. The patient population included 71% ( n = 27) of patients with rheumatoid arthritis, 13% ( n = 5) had ulnocarpal abutment syndrome, and 16% ( n = 6) had DRUJ OA. Bowers found that HIA resulted in 85% of patients with rheumatoid arthritis, and 100% of those with degenerative arthritis having painless movement. 5 A year later, Watson et al reported on matched ulna resection that leaves the TFCC and ligamentous attachments of the distal ulna intact. 29 This study explored 54 wrists of varied pathology and demonstrated significant pain relief, as well as increased painless pronation and supination. However, both Bower's and Watson's first study had a significant number of patients with rheumatoid arthritis, 71 and 62% of total patients, respectively. In 1992, Watson et al reported a retrospective review of 44 patients who underwent matched ulnar resection in patients with post-traumatic and a mechanical disorder of the DRUJ from 1984 to 1988. 30 Of the 44 patients, 32 patients were available for follow-up with a mean follow-up of 51 months. This study reported 75% ( n = 24) of patients with mild or no pain, and all but two patients reporting subjective improvement. They found patients who had preexisting conditions or had undergone prior DRUJ surgery had worse pain outcomes at final follow-up.
Bain et al retrospectively reviewed 55 wrists that underwent HIA and explored subjective and functional outcome measures. 31 The study's patient population largely included 71% ( n = 39) post-traumatic DRUJ OA patients; however, it also included 22% ( n = 12) with rheumatoid arthritis. Of the 55 patients who underwent HIA, 84% ( n = 41) of patients were satisfied with their surgery, and 72% ( n = 35) reported improvements in pain. Supination and pronation also demonstrated some improvement from 54/67 degrees preoperatively to 72/72 degrees postoperatively, respectively. Additionally, Bain et al reported that patient satisfaction is closely correlated with pain improvement, suggesting pain relief should be the primary indication for surgery.
An early study by Minami et al reported on 12 male patients treated with HIA for DRUJ OA. 32 In this patient population, the primary diagnosis was primary OA ( n = 10) or post-traumatic OA ( n = 2). Pain was present preoperatively in all 12 patients with six severe and six moderate pain. Postoperative pain was reported to be resolved in six patients and only minimally present in six patients. The study also reported significant improvements in grip strength, extension, supination, and pronation.
A 2019 retrospective study by Nawijn et al investigated long-term follow-up of 66 patients who underwent HIA arthroplasty. 33 The study was only able to obtain long-term follow-up of 31 patients of which 80% had inflammatory arthritis, 16% had post-traumatic arthritis, and two had other conditions effecting the DRUJ. Mean interval between surgery and survey was 8.6 ± 2.4 years. Primary outcomes included qDASH, pain and patient satisfaction, and a nonvalidated arthroplasty questionnaire. Mean qDASH was 31.0 ± 20.2 with DRUJ subluxation on radiograph associated with a higher qDASH. Pain scores were associated with older age, male sex, presence of osteoporosis, as well as nonunion or malunion diagnosis at time of surgery. Average satisfaction score was 9 out of 10. Patients with prior surgery, fracture, subluxation on radiograph, tendon rupture at time of surgery, and tendon repair as follow-up procedure reported less satisfaction with their procedure.
Complications that evolve from HIA are often related to instability, impingement of the DRUJ, or persistent pain. 28 Bowers et al found 15.7% ( n = 6) of patients reported persistent pain, with five patients having pain attributed to stylocarpal impingement. 5 Overall, unresolved postoperative pain was mild and reported in 10.5% ( n = 4) of patients. Bowers believed that stylocarpal impingement could be reduced with increased tendon interposition bulking or ulnar shortening during the original procedure in patients with a positive ulnar variance of more than 2 mm. 29 Bain et al reported 7.2% ( n = 4) patients with stylocarpal impaction based on clinical examination and radiographic findings. All four patients in this study underwent revision surgery with shortening of the distal ulna and successful de-impaction. 31 Watson et al reported revision procedures performed on 9.3% ( n = 3) patients for radioulnar impingement symptoms. These patients were found to have new onset ulnar periosteal bone spurs at the site of previous resection and responded to excision of spurs with all patients having no or mild pain post resection. 30
Minami et al reported one case of persistent moderate pain, and three cases of ECU tendonitis. 32 The study attributes the ECU tendonitis to the retinacular reconstruction described in Bowers, and they no longer perform this portion of the procedure. 32 The tendonitis was resolved with splinting and steroid injections within 6 months postoperatively. The study also reported one episode of ulnar stump fracture 3 months postoperatively, and one incidence of bony union between the radius and ulna. 32
Complications postoperatively from distal ulnar hemi-resection are largely reported to be related to instability, stylocarpal impaction, or persistent pain. 28 Another potential disadvantage of HIA is the narrowing of the wrist, which is felt as a cosmetic impairment to some patients. In all studies, patients consistently reported high levels of satisfaction, substantial relief of pain, and limited postoperative complications. The distal ulnar hemi-resection remains an important tool in the management of DRUJ OA with an intact or reconstructed TFCC.
Implant Arthroplasty
In recent years, ulnar head arthroplasty and total DRUJ arthroplasty have been proposed to serve as an adjunct to failed painful ulnar head resection. These procedures can stabilize the ulna, increase strength, and improve postoperative range of motion. Partial head arthroplasty has also been used but requires the presence of a stable joint and intact ligamentous structures.
Ulnar head replacement without resection of the sigmoid radial notch may be considered in a joint with failed prior distal ulnar resection and/or degeneration of the soft tissue surrounding the joint. In the paper describing the procedure in detail, Herbert concludes that “excision arthroplasty (i.e., Darrach procedure) should be reserved for patients with low functional demands in whom instability is unlikely to be a major problem.” 9 He further concludes that ulnar head replacement should be considered the “procedure of choice for most patients with symptomatic arthritis at the DRUJ.” Stable native soft-tissue support is considered to be essential for good outcomes in total ulnar head arthroplasty. Rheumatoid arthritis and/or injuries to the interosseous membrane would be contraindications to this procedure. 34 Herbert notes several potential major complications of implant arthroplasty, including recurrent instability, ulnar impaction, stem loosening, ulnar fracture, recurrent pain, and loss of movement. 9
Using the Herbert ulnar head prosthesis (UHP) for total ulnar head arthroplasty, van Schoonhoven completed a retrospective review of 23 patients at both short-term (28 months) and long-term (11 years, 2 months) follow-up. 35 36 These studies demonstrated significant improvement in pain, range of motion, and grip strength. Two patients required reoperation to address recurrent instability at the short-term time point, and one required removal of the prosthesis due to a low-grade infection. At long-term follow-up, all 23 patients, including the two who required reoperation, maintained stability of the joint and did not require any further surgery.
Aita et al evaluated a case series of 10 patients in which one patient was treated with partial ulnar head arthroplasty and 9 with total ulnar head arthroplasty. 37 Overall, the 10 patients in this study showed range of motion in pronosupination 174.5 ± 7.15 degrees. VAS of 2.13, and palmar grip strength at 90.7% of unaffected side after 1-year follow-up. One patient presented with postoperative instability and pain secondary to dorsal subluxation of the prosthesis at 12 months. This patient's chronic ligament damage was the original indication for arthroplasty.
In 2009, Shipley et al reported their experience with ulnar head arthroplasty using both the Herbert UHP (14 patients) and uHead (8 patients) to treat painful DRUJ arthroses. 38 Six patients in this cohort had no prior DRUJ surgery while 16 had undergone previous wrist surgery. No difference in functional outcome was noted between primary treatment and salvage groups. Three of 22 wrists required reoperation, two of which were for symptomatic dorsal instability. This dorsal instability was treated with soft tissue reconstruction of the dorsal capsule with either the ECU tendon or the extensor digiti minimi tendon as a graft. One case required reoperation due to sensitivity at the head of the implant, which may have been associated with the synovitis found on exploration of the ulnocarpal joint. This was successfully treated with a synovial debridement.
Sauerbier et al described an evaluation of 25 wrists treated with total ulnar head arthroplasty (uHead [5] and Herbert UHP [20]) and reported that results of primary implantation had better functional outcomes when compared with secondary or salvage procedures of the DRUJ. 34 At a mean clinical follow-up of 30 months, no revision procedures were necessary, and all wrists were radiographically stable with no signs of loosening. An asymptomatic positive ulnar grind test was noted in 8/25 patients.
Total DRUJ arthroplasty involves reconstruction of the ulnar head as well as the articulating sigmoid notch of the distal radius. This is often a second-line treatment in the management algorithm of DRUJ OA. The procedure involves removal of the soft-tissue stabilizers of the joint. Placing the radial component of the implant as near as possible to the original sigmoid notch is designed to optimize its overall function and limit stresses on both components of the implant. However, this is surgically complex in the face of prior wrist surgeries or distorted anatomy. 39 Indications for the procedure have included chronic instability, post-traumatic arthrosis, and Madelung deformity. The implant, as designed by Aptis Medical, is a semi-constrained DRUJ prosthesis composed of an ulnar stem, a radius plate, a polyethylene ball, and a socket covering which connects the ulnar stem and the radial plate 39 ( Fig. 4 ).
Fig. 4.

Distal radioulnar joint arthroplasty with a Scheker prosthesis. ( A ) postoperative posteroanterior view. ( B ) Postoperative lateral view. ( C ) Postoperative oblique view.
It should be noted that salvage with an ulnar head prosthesis is much simpler following HIA than after SK procedure. The conversion to a prosthesis from a SK is a technically demanding endeavor, especially when multiple prior surgeries have been performed and soft tissue support is lacking. Fok et al reported their results with this conversion and inserted the ulnar implant into the DRUJ fusion mass. 40 They noted the need for an incomplete opening wedge radial osteotomy, hinging on the radial cortex, proximal to the arthrodesis is indicated when easy reduction of the spherical head into the reamed socket cannot be achieved with simple longitudinal traction on the hand. They found in the medium term, their technique provided a satisfactory clinical, functional, and radiological result. Their reconstruction methods allowed the avoidance of more radical salvage procedures, such as 1-bone forearm and wide ulnar excision.
Kachooei et al evaluated the total DRUJ prosthesis in 14 wrists over a 10-year period with follow-up averaging 60 months. 41 Two wrists required reoperation, both to debride the screw tip over the radius, a complication due to possible inaccurate screw length in the radial plate. No other complications were reported. Supination/pronation on follow-up was 51/64 degrees, respectively. Indications of this cohort included eight for chronic instability, two for post-traumatic arthrosis, one for stiff DRUJ, one for DRUJ deformity, and two for chronic instability in the context of Ehlers–Danlos syndrome. As this is not a first line treatment, all patients had history of prior wrist surgery, with a range of one to six prior surgeries.
Lans et al prospectively evaluated 14 patients who received a total DRUJ prosthesis for a painful DRUJ and/or instability after prior wrist surgery. 39 The inclusion criteria for their evaluation was multiple prior wrist surgeries with the goal of describing complications in technically difficult DRUJ arthroplasties. In total, 7 of their 14 patients required reoperation. One patient developed a deep infection, for which the implant was removed, infection cleared, then implant reinserted. One patient developed heterotopic ossification around the ulna, requiring excision. Five patients had residual ulnar sided pain severe enough to require reoperation, treated with excision of the pisiform, triquetrum, or both. Two patients developed superficial infections treated successfully with antibiotics, but surgery was not required. Overall, supination/pronation improved from 45.6/42.3 degrees preoperatively to 76.1/76.1 degrees postoperatively. Lifting strength also significantly improved postoperatively. The authors conclude that despite complications, this procedure is a valid option for those with DRUJ arthroses who have failed prior wrist procedures.
Comparison Studies
True comparison between procedures for OA of the DRUJ is difficult. There are no prospective randomized controlled trials published in the literature. To date, there are no prospective trials for the management of this condition. Retrospective reviews with heterogeneous diagnoses constitute the available literature. The functional demands on the wrist and patient expectations can be very different between patients with arthritis due to rheumatoid disease compared with those with degenerative osteoarthrosis and post-traumatic disease.
Traditionally, the Darrach resection was reserved for an older less active individual. In the report by Giberson-Chen, they stated, “in our practices, SK arthrodesis is preferred over Darrach resection or hemi-resection arthroplasty for patients with DRUJ arthritis or instability. Darrach resection is reserved for elderly patients with low functional demands.” 20
Verhiel et al completed a retrospective study of 85 patients with only post-traumatic DRUJ dysfunction. 42 The purpose of their study was to assess differences in long-term patient reported outcomes for Darrach versus SK. Nine patients underwent a hemi-resection arthroplasty but were not included in the study. They found no significant difference between the groups with regard to PROMIS UE Physical Function score (39, p = 0.91), numerical rating scale pain score (2.5, p = 0.76), or satisfaction score (9.5, p = 0.89). These scores were obtained after a median of 8.4 years after the index procedure. The mean ulnar distance (the distance from the articular surface of the radius to the proximal stump of the ulna) was 18 ± 7.3 mm after Darrach versus 33 ± 6.3 mm after SK. The median radioulnar distance was 5.5 mm in Darrach group versus 8 mm in SK group. This distance is the width of the interosseous space between the radius and ulna at the proximal stump of the ulna and is a measure of radio-ulnar convergence.
The most common complication reported for both procedures was ulnar stump instability, 14% in Darrach versus 7.1% in SK. In total, 19% of patients in the Darrach group underwent a stabilization of the ulnar distal stump whereas 46% in the SK group had a stabilization performed concomitantly. Heterotopic ossification was more common after SK with five patients versus one patient in Darrach group ( p = 0.014). Reoperation rate was noticeable but not significantly different between the two groups, 18% in Darrach versus 36% in SK ( p = 0.10). The authors report comparable long-term outcomes and complication rates for surgical treatment of post-traumatic DRUJ dysfunction with either the Darrach or the SK procedures.
In 2005, Minami et al published a retrospective study evaluating long-term clinical and radiographic results in 61 patients with OA of the DRUJ. 43 They had three surgical cohorts including patients having either a Darrach ( n = 20), SK ( n = 25), or HIA ( n = 16) procedure. A lower percentage of patients treated with a Darrach resection rated postoperative pain levels as “none” or “slight” compared with SK and HIA. Flexion and extension significantly improved for those patients undergoing either SK or HIA, but not for Darrach. Pronation and supination significantly improved after all three procedures. Grip strength significantly increased after SK and HIA but decreased after Darrach.
Minami et al found significantly fewer patients returned to their original work and more complications followed after a Darrach procedure. A Darrach resection was associated with poorer outcomes and more complications than SK and HIA, but this may be in part due to the older patient population that received this procedure. The authors do not mention if any patients who underwent a Darrach procedure had stabilization of the ulnar stump. The results for the SK group improved dramatically after an ECU stabilization procedure was added. This additional step appeared to prevent subluxation of the proximal ulnar stump. Due to the different demographics undergoing each of these procedures, their conclusions must be guarded. They did however provide their framework for deciding preoperatively who should undergo a SK verses a HIA. They suggest that HIA was indicated when the TFCC was intact or could be reconstructed while the SK is optimal when the TFCC could not be reconstructed or there was positive ulnar variance of more than 5 mm even though the TFCC was functional. This framework may prove useful as a preoperative treatment algorithm. Surgeons should be advised to have all equipment necessary to complete either procedure should the TFCC be torn and not reparable.
George et al completed a retrospective study of 18 patients younger than 50 years old with DRUJ dysfunction following a Colles' fracture. 44 They compared the results of both the Darrach resection and the SK arthrodesis. No significant difference between the two groups with respect to forearm and wrist range of motion was identified. Grip strength was not significantly lower in Darrach (82%) versus SK (103%) compared with the opposite wrist. No significant difference in Mayo Wrist, DASH scores, or complication rates were perceived. The authors stated that the Darrach and SK are comparable in terms of outcomes and complications following Colles' fractures for patients under the age of 50 years.
In a recent retrospective review, Yayac et al reviewed 121 patients (44 with degenerative OA and 51 with posttraumatic) undergoing Darrach, SK, and HIA procedures for the DRUJ. 45 Although they did not look at patient reported outcome scores, no significant differences were found in motion, persistent pain, or swelling. There was no statistical difference in the complications among the three procedures although adverse outcomes were commonly experienced in all three procedures. Of note, the age at operation was significantly lower in patients undergoing SK (42 years) versus Darrach (59 years) and HIA (62 years) ( p < 0.001). There was a preference for the surgeons to suggest the SK to younger patients.
Summary
OA of the DRUJ is a common condition that typically occurs following trauma to the distal radius. While conservative therapy should be tried initially, often surgical intervention is implemented to recover function of the wrist and improve patient quality of life. The literature is not clear as to the optimal treatment for symptomatic OA of the DRUJ. Taken individually, each procedure has shown benefit in helping those suffering from pain and/or functional limitation to improve their situation. In a letter in 2011, Nikkah et al asked “do patients really do better after the SK procedure when compared to the Darrach procedure?” 46 A decade later, this question has not yet been sufficiently answered. Along with the hemi-resection arthroplasty, all these procedures have a role in the management of patients with symptomatic OA of the DRUJ.
Funding Statement
Funding None.
Footnotes
Conflict of Interest None declared.
References
- 1.Geissler W B, Fernandez D L, Lamey D M. Distal radioulnar joint injuries associated with fractures of the distal radius. Clin Orthop Relat Res. 1996;(327):135–146. doi: 10.1097/00003086-199606000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Malgaine J F. Paris JB Brailliére; 1855. Traité Des Fractures Et Des Luxations, Vol. 2. [Google Scholar]
- 3.Darrach W. Partial excision of lower shaft of ulna for deformity following Colles's fracture. 1913. Clin Orthop Relat Res. 1992;(275):3–4. [PubMed] [Google Scholar]
- 4.Sauvé L. Nouvelle technique de traitement chirurgical des luxations recidivantes isolees de I'extremite inferieure du cubitus. J Chir (Paris) 1936;47:589–594. [Google Scholar]
- 5.Bowers W H. Distal radioulnar joint arthroplasty: the hemiresection-interposition technique. J Hand Surg Am. 1985;10(02):169–178. doi: 10.1016/s0363-5023(85)80100-3. [DOI] [PubMed] [Google Scholar]
- 6.Tulipan D J, Eaton R G, Eberhart R E. The Darrach procedure defended: technique redefined and long-term follow-up. J Hand Surg Am. 1991;16(03):438–444. doi: 10.1016/0363-5023(91)90010-9. [DOI] [PubMed] [Google Scholar]
- 7.Minami A, Iwasaki N, Ishikawa J, Suenaga N, Kato H. Stabilization of the proximal ulnar stump in the Sauvé-Kapandji procedure by using the extensor carpi ulnaris tendon: long-term follow-up studies. J Hand Surg Am. 2006;31(03):440–444. doi: 10.1016/j.jhsa.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 8.Chu P-J, Lee H-M, Hung S-T, Shih J-T. Stabilization of the proximal ulnar stump after the Darrach or Sauvé-Kapandji procedure by using the extensor carpi ulnaris tendon. Hand (N Y) 2008;3(04):346–351. doi: 10.1007/s11552-008-9113-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herbert T J, van Schoonhoven J. Ulnar head replacement. Tech Hand Up Extrem Surg. 2007;11(01):98–108. doi: 10.1097/bth.0b013e318033738a. [DOI] [PubMed] [Google Scholar]
- 10.Hartz C R, Beckenbaugh R D. Long-term results of resection of the distal ulna for post-traumatic conditions. J Trauma. 1979;19(04):219–226. doi: 10.1097/00005373-197904000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Bell M J, Hill R J, McMurtry R Y. Ulnar impingement syndrome. J Bone Joint Surg Br. 1985;67(01):126–129. doi: 10.1302/0301-620X.67B1.3968131. [DOI] [PubMed] [Google Scholar]
- 12.Bieber E J, Linscheid R L, Dobyns J H, Beckenbaugh R D. Failed distal ulna resections. J Hand Surg Am. 1988;13(02):193–200. doi: 10.1016/s0363-5023(88)80047-9. [DOI] [PubMed] [Google Scholar]
- 13.Field J, Majkowski R J, Leslie I J. Poor results of Darrach's procedure after wrist injuries. J Bone Joint Surg Br. 1993;75(01):53–57. doi: 10.1302/0301-620X.75B1.8421034. [DOI] [PubMed] [Google Scholar]
- 14.Breen T F, Jupiter J B. Extensor carpi ulnaris and flexor carpi ulnaris tenodesis of the unstable distal ulna. J Hand Surg Am. 1989;14(04):612–617. doi: 10.1016/0363-5023(89)90176-7. [DOI] [PubMed] [Google Scholar]
- 15.De W itte, PB, Wijffels M, Jupiter J B, Ring D. The Darrach procedure for post-traumatic reconstruction. Acta Orthop Belg. 2009;75(03):316–322. [PubMed] [Google Scholar]
- 16.Grawe B, Heincelman C, Stern P. Functional results of the Darrach procedure: a long-term outcome study. J Hand Surg Am. 2012;37(12):2475–80.e1, 2. doi: 10.1016/j.jhsa.2012.08.044. [DOI] [PubMed] [Google Scholar]
- 17.Jochen-Frederick H, Pouyan Y, Khosrow B A. Long-term functional outcome and patient satisfaction after ulnar head resection. J Plast Reconstr Aesthet Surg. 2016;69(10):1417–1423. doi: 10.1016/j.bjps.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Zimmermann R, Gschwentner M, Arora R, Harpf C, Gabl M, Pechlaner S. Treatment of distal radioulnar joint disorders with a modified Sauvé-Kapandji procedure: long-term outcome with special attention to the DASH Questionnaire. Arch Orthop Trauma Surg. 2003;123(06):293–298. doi: 10.1007/s00402-003-0529-5. [DOI] [PubMed] [Google Scholar]
- 19.Czermak C, Wittemann M, Germann G, Sauerbier M. Funktionelle ergebnisse der kapandji-sauvé-operation als Rettungseingriff am distalen Radioulnargelenk. Handchir Mikrochir Plast Chir. 2007;39(06):403–408. doi: 10.1055/s-2007-965025. [DOI] [PubMed] [Google Scholar]
- 20.Giberson-Chen C C, Leland H A, Benavent K A, Harper C M, Earp B E, Rozental T D. Functional outcomes after sauve-kapandji arthrodesis. J Hand Surg Am. 2020;45(05):408–416. doi: 10.1016/j.jhsa.2019.11.014. [DOI] [PubMed] [Google Scholar]
- 21.Lees V C, Scheker L R. The radiological demonstration of dynamic ulnar impingement. J Hand Surg Br Eur Vol. 1997;22(04):448–450. [Google Scholar]
- 22.Nakamura R, Tsunoda K, Watanabe K, Horii E, Miura T. The Sauvé-Kapandji procedure for chronic dislocation of the distal radio-ulnar joint with destruction of the articular surface. J Hand Surg [Br] 1992;17(02):127–132. doi: 10.1016/0266-7681(92)90071-9. [DOI] [PubMed] [Google Scholar]
- 23.Minami A, Suzuki K, Suenaga N, Ishikawa J. The Sauvé-Kapandji procedure for osteoarthritis of the distal radioulnar joint. J Hand Surg Am. 1995;20(04):602–608. doi: 10.1016/s0363-5023(05)80276-x. [DOI] [PubMed] [Google Scholar]
- 24.Minami A, Kato H, Iwasaki N. Modification of the Sauvé-Kapandji procedure with extensor carpi ulnaris tenodesis. J Hand Surg Am. 2000;25(06):1080–1084. doi: 10.1053/jhsu.2000.20158. [DOI] [PubMed] [Google Scholar]
- 25.Tomori Y, Sawaizumi T, Nanno M, Takai S. Functional outcomes after the Sauvé-Kapandji procedure for distal radio-ulnar post-traumatic instability: a case-control comparison of three different operative methods of stabilization of the ulnar stump. Int Orthop. 2018;42(09):2173–2179. doi: 10.1007/s00264-018-4042-4. [DOI] [PubMed] [Google Scholar]
- 26.Rothwell A G, O'Neill L, Cragg K. Sauvé-Kapandji procedure for disorders of the distal radioulnar joint: a simplified technique. J Hand Surg Am. 1996;21(05):771–777. doi: 10.1016/S0363-5023(96)80190-0. [DOI] [PubMed] [Google Scholar]
- 27.Lluch A. The sauvé-kapandji procedure. J Wrist Surg. 2013;2(01):33–40. doi: 10.1055/s-0032-1333465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glowacki K A. Hemiresection arthroplasty of the distal radioulnar joint. Hand Clin. 2005;21(04):591–601. doi: 10.1016/j.hcl.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 29.Watson H K, Ryu J Y, Burgess R C. Matched distal ulnar resection. J Hand Surg Am. 1986;11(06):812–817. doi: 10.1016/s0363-5023(86)80228-3. [DOI] [PubMed] [Google Scholar]
- 30.Watson H K, Gabuzda G M. Matched distal ulna resection for posttraumatic disorders of the distal radioulnar joint. J Hand Surg Am. 1992;17(04):724–730. doi: 10.1016/0363-5023(92)90324-i. [DOI] [PubMed] [Google Scholar]
- 31.Bain G I, Pugh D M, MacDermid J C, Roth J H. Matched hemiresection interposition arthroplasty of the distal radioulnar joint. J Hand Surg Am. 1995;20(06):944–950. doi: 10.1016/S0363-5023(05)80141-8. [DOI] [PubMed] [Google Scholar]
- 32.Minami A, Suzuki K, Suenaga N, Ishikawa J. Hemiresection-interposition arthroplasty for osteoarthritis of the distal radioulnar joint. Int Orthop. 1995;19(01):35–39. doi: 10.1007/BF00184912. [DOI] [PubMed] [Google Scholar]
- 33.Nawijn F, Verhiel S HWL, Jupiter J B, Chen N C.Hemiresection interposition arthroplasty of the distal radioulnar joint: a long-term outcome studyHand (N Y) 2019 [DOI] [PMC free article] [PubMed]
- 34.Sauerbier M, Arsalan-Werner A, Enderle E, Vetter M, Vonier D. Ulnar head replacement and related biomechanics. J Wrist Surg. 2013;2(01):27–32. doi: 10.1055/s-0032-1333464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van S choonhoven, J, Fernandez D L, Bowers W H, Herbert T J. Salvage of failed resection arthroplasties of the distal radioulnar joint using a new ulnar head prosthesis. J Hand Surg Am. 2000;25(03):438–446. doi: 10.1053/jhsu.2000.6006. [DOI] [PubMed] [Google Scholar]
- 36.van Schoonhoven J, Mühldorfer-Fodor M, Fernandez D L, Herbert T J. Salvage of failed resection arthroplasties of the distal radioulnar joint using an ulnar head prosthesis: long-term results. J Hand Surg Am. 2012;37(07):1372–1380. doi: 10.1016/j.jhsa.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 37.Aita M A, Ibanez D S, Saheb G CB, Alves R S. Arthroplasty of the distal ulna distal in managing patients with post-traumatic disorders of the distal radioulnar joint: measurement of quality of life. Rev Bras Ortop. 2015;50(06):666–672. doi: 10.1016/j.rboe.2015.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yen S hipley, N, Dion G R, Bowers W H. Ulnar head implant arthroplasty: an intermediate term review of 1 surgeon's experience. Tech Hand Up Extrem Surg. 2009;13(03):160–164. doi: 10.1097/BTH.0b013e3181b4c52d. [DOI] [PubMed] [Google Scholar]
- 39.Lans J, Chen S-H, Jupiter J B, Scheker L R. Distal radioulnar joint replacement in the scarred wrist. J Wrist Surg. 2019;8(01):55–60. doi: 10.1055/s-0038-1670681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fok M W, Fernandez D L, van Schoonhoven J. Midterm outcomes of the use of a spherical ulnar head prosthesis for failed Sauvé-Kapandji Procedures. J Hand Surg Am. 2019;44(01):660–6.6E10. doi: 10.1016/j.jhsa.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 41.Kachooei A R, Chase S M, Jupiter J B. Outcome assessment after aptis distal radioulnar joint (DRUJ) implant arthroplasty. Arch Bone Jt Surg. 2014;2(03):180–184. [PMC free article] [PubMed] [Google Scholar]
- 42.Verhiel S HWL, Özkan S, Ritt M JPF, Chen N C, Eberlin K R. A comparative study between Darrach and Sauvé-Kapandji procedures for post-traumatic distal radioulnar joint dysfunction. Hand (N Y) 2019 doi: 10.1177/1558944719855447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Minami A, Iwasaki N, Ishikawa J, Suenaga N, Yasuda K, Kato H.Treatments of osteoarthritis of the distal radioulnar joint: long-term results of three procedures Hand Surg 200510(2-3)243–248. [DOI] [PubMed] [Google Scholar]
- 44.George M S, Kiefhaber T R, Stern P J. The Sauve-Kapandji procedure and the Darrach procedure for distal radio-ulnar joint dysfunction after Colles' fracture. J Hand Surg [Br] 2004;29(06):608–613. doi: 10.1016/j.jhsb.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 45.Yayac M, Padua F G, Banner L. Treatment outcomes in patients undergoing surgical treatment for arthritis of the distal radioulnar joint. J Wrist Surg. 2020;9(03):230–234. doi: 10.1055/s-0040-1702200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nikkhah D, Rodrigues J, Dejager L. Do patients really do better after the Sauve-Kapandji procedure when compared to the Darrach procedure? A systematic review. J Hand Surg Eur Vol. 2011;36(07):615. doi: 10.1177/1753193411414630. [DOI] [PubMed] [Google Scholar]


