Abstract
Background: Since the COVID-19 pandemic has been affected our daily lives, the global population has been exposed to permanent concerns and thus might suffer from the psychological burden. It is well known that psychological burdens can affect dietary behavior. Aim: The impact of a psychological burden on people, and in particular on their dietary patterns was investigated in this nationawide cross-sectional study. Methods: 7525 participants responded to the questionnaire regarding the psychological burden concerning the COVID-19 pandemic and their current dietary structure with changes in the pattern and food amount (between November 2020 and March 2021). Results: A pandemic-related dysfunction of dietary behavior was found. Some participants reported restrictive (conscious) food intake and as well impulsive food intake, which can be described as dysfunctional eating behaviors. In particular, younger persons and individuals who claimed an increased psychological burden reported dysfunctional dietary behavior. Data clearly show that psychological burdens affect an individual's dietary behavior. Conclusion: Public health strategies have to be developed to support individuals at risk to improve coping strategies. The long-term aim should be avoiding the maintenance of dysfunctional dietary behavior.
Keywords: COVID-19, dietary behavior, food consuming, psychological burden, mental health
Introduction
On 11 March 2020, the WHO declared the outbreak of SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) as a global pandemic (Cucinotta and Vanelli, 2020). Currently, worldwide 623,893,894 people were infected with COVID-19 and 6,553,936 patients died (until 19 October 2022) (Organization, 2021b). Through governmental restrictions on travel, people gathering, curfews, and opening of stores, but also through the concerns and fears of the population worldwide, the pandemic has an enormous impact on our everyday living (Pedrosa et al., 2020). Previous studies demonstrated that people around the world are psychologically burdened by the pandemic (Bäuerle et al., 2020; Musche et al., 2021; Kohler et al., 2021). For anxiety disorder symptoms the described prevalence was 20.7%, for depression 18.1%, and for distress 13% (Leung et al., 2022). Overall, it could be shown, that one in five had a suspected mental disorder during the COVID-19 pandemic (Leung et al., 2022). The psychological burden was not only a phenomenon of the beginning—in the first wave of the COVID-19 pandemic, but it persists continuously (Moradian et al., 2021). Studies, conducted in the second phase of restrictions, showed a high psychological burden, an increased level of depressive symptoms, and less implementation of safety behaviors (Moradian et al., 2021). The COVID-19 pandemic appears to be an enormous stress factor; uncertainties and concerns are a constant companion.
People often react to psychological strain by changing their dietary patterns. Psychological burden is associated with both increased and decreased consumption in amount and type of food (Hill et al., 2018). Chronic life stress has a causal link to weight gaining (Torres and Nowson, 2007). Moreover, consuming a small amount of sweets such as chocolate can lead to an elevation of mood and thus indirectly contributes to stress management (Macht and Mueller, 2007).
In a society where obesity is a major medical problem, the link between psychological distress, which is currently pervasive, and changes in diet that can lead to weight gain is of great importance. Obesity is characterized by an excess of calories with a deficit of options for calorie reduction. One of the numerous factors influencing the development of being overweight is the way how emotions and stressful situations are handled and processed (Ganley, 1989; Organization, 2021a). During the COVID-19 pandemic, increased emotional eating attacks and uncontrolled dietary behaviors were reported (Elmacioglu et al., 2021).
Previous research showed that patients with a history of binge eating disorder or bulimia nervosa had a higher risk for symptom deterioration and relapse during the COVID-19 pandemic (Giel et al., 2021; Schlegl et al., 2020b). Furthermore, both increased restricted eating behavior and binge eating patterns were reported in the general population during the COVID-19 pandemic (Phillipou et al., 2020). Patients with anorexia nervosa in majority described an increase in concerns dealing with eating, shape, and with a growth of drive for physical activity, loneliness, sadness, and inner restlessness (Schlegl et al., 2020a).
To our knowledge, this is the first study to date to phenotype different dietary behavior and assess their associative and contextual embeddedness in the current COVID-19 pandemic. Of the well-known direct link between changes in dietary behavior and psychological burden, and with regard to the general issue of increasing obesity worldwide, the study is of high relevance. It is assumed that the current pandemic has a high influence on an individual's dietary behavior. Connections between psychological burden and changes in dietary habits are presumed. In this context, the respondents may indicate an increased or decreased amount of food intake. In addition, a completely dysfunctional dietary behavior with parts of restrictive as well as impulsive, increased food intake is conceivable. This study has the long-term aim of enabling a more precise assessment of the burden on vulnerable groups in order to be able to offer preventive supportive training.
Method
Procedure and inclusion criteria
Throughout Germany, during the second infection wave, persons were surveyed (online) between November 2020 and March 2021. The eligibility requirements included adult age (≥ 18 years), a good command of the German language, and internet access. Recruitment was performed via online channels and social and print media. All participants gave electronic informed consent to take part in the anonymous survey. The study was approved by the Ethics Committees of the Medical Faculty of the University Duisburg-Essen (20-9307-BO).
Measures
The questionnaire includes validated assessment instruments (COVID-19-anxiety, generalized anxiety, depressive symptoms, and distress) as well as items on social-demographic and medical details. Here, age, gender, education, city size, and mental illnesses were asked. To analyze the symptoms or levels of generalized anxiety and depression established questionnaires such as the Generalized Anxiety Disorder Scale-2 (GAD-7) and the Patient Health Questionaire-2 (PHQ-2) were used. GAD-7 measures self-reported anxiety and its severity in the last past two weeks (Löwe et al., 2008). The PHQ-2 screens for depressive symptoms in the past 2 weeks. The response options were a 4-point Likert scale ranging from not at all = 0 to nearly every day = 3. The cut-off value of 3 indicates major depressive symptoms (Löwe et al., 2005). For measuring the experienced distress the Distress Thermometer (DT) was used. Participants could range their distress from “0” (no distress) to “10” (extreme distress) on a visual analog scale. More than five points indicate an elevated distress (Mehnert et al., 2006).
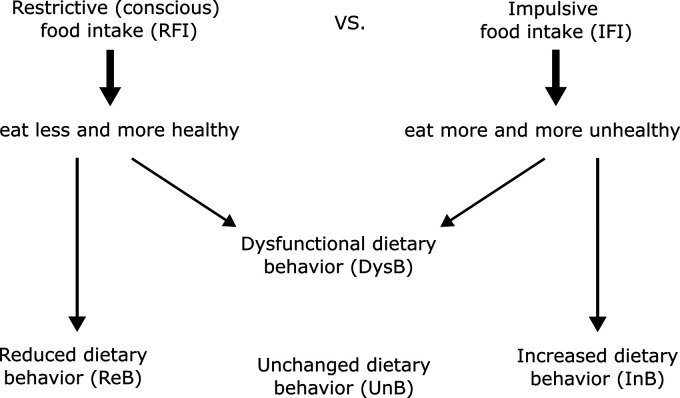
COVID-19-anxiety was assessed by the COVID-19-Anxiety Questionnaire (Petzold et al., 2020). Participants’ changes in dietary behavior due to the COVID-19 pandemic were explored using a self-generated questionnaire on how life during the pandemic has led to aberrations in participants’ normal dietary behavior. The items asked about the amount of food (more or less), types of food (fast food, unhealthy, use of basic ingredients), changes in food purchasing behavior due to hygiene regulations (face mask, distance), the importance of food intake, and loss of control over eating. From an initial set of nine items, eight items were selected due to high internal validity. Eight items were selected based on a factorial analysis. Here, all nine items were assessed using Velicer's minimum average partial test was used to define the optimal number of factors. Based on these results, a factorial analysis with oblimin rotation was applied to extract two factors. One item had a factor loading below 0.4, which is why it was dropped. This left us with two factors including four items each, which are most interpretable as the propensity to eat more and unhealthier as a result of the pandemic (Cronbach's α = .86, MacDonald's ω = .86), and to eat less and healthier during the pandemic (Cronbach's α = .7, MacDonald's ω = .71), each consisting of four items. The scales were named as “restrictive (conscious) food intake = RFI” and “impulsive food intake = IFI.” Using these scales two linear regression models were computed. Hereby, the two dimensions of dietary behavior (RFI, IFI) were assessed to each of the conditional contributions of sociodemographic, psychopathological, and COVID-19-related variables. For clarification see Figure 1.
Figure 1.
Participants’ grouping. The participants were divided into those who reported a restrictive (conscious) and an impulsive food intake (RFI and IFI). Persons’ dietary behavior that showed both RFI and IFI during the pandemic were categorized as dysfunctional (DysB).
Statistical analysis
Goldfeld-Quandt tests were used to assess heteroscedasticity. In case of violation, an additional regression model with Huber-White corrected standard errors was reported to assess whether such deviations jeopardize an appropriate interpretation of the respective model. The linearity assumption was assessed using rainbow tests. The normality of residuals was tested but disregarded due to its negligible effect in large sample sizes (Schmidt and Finan, 2018). In fact, the scales RFI and IFI during the pandemic were positively correlated (rs = .258, p < 0.001). Combined RFI and IFI were defined as dysfunctional.
In order to better illustrate predictors of dysfunctional dietary behavior, and hence, illustrate its closeness to other pathological or burden-related features, four categories were generated via median-split of the dietary-related scales. The categories were named: “unchanged dietary behavior = UnB,” mainly “reduced dietary behavior = ReB,” mainly “increased dietary behavior = InB” and “dysfunctional dietary behavior = DysB” (Figure 1). These categories were then entered as a response variable into a multinomial regression, with all other socio-economic, psychopathological, and COVID-19-related features as regressors.
Large sample sizes go along with a high statistical power, which is why even very small differences and associations can be detected. However, in this case, statistical significance does not equal conceptual, practical, or theoretical significance (Wasserstein et al., 2019). This is why also the magnitude of difference, as well as the 95% CIs, will be considered while interpreting the results. Statistical analyses were performed using R 3.6.3.
Results
Sample
A total of 7525 participants completed the online survey. Table 1 displays all relevant participant characteristics. Power analyses suggest that with such sample sizes, overall regression can easily be spotted f²s of 0.01 with a power of 1 – β > .95.
Table 1.
Participant characteristics: social-demographic and medical details.
| n (% or SD) | |||
|---|---|---|---|
| Total n | 7525 | ||
| Age | |||
| 18–34 years | 3188 (42.5) | ||
| 35–54 years | 3056 (40.6) | ||
| 55–74 years | 1242 (16.5) | ||
| older than 75 years | 39 (0.5) | ||
| Gender | |||
| Female | 5125 (68.1) | ||
| Male | 2357 (31.3) | ||
| Other | 43 (0.6) | ||
| Education | |||
| University degree | 2955 (39.3) | ||
| High school degree | 2399 (31.9) | ||
| Secondary school degree (Realschule) | 1708 (22.7) | ||
| Secondary school degree (Hauptschule) | 359 (4.8) | ||
| No degree | 28 (0.4) | ||
| Other | 76 (1.0) | ||
| City size | |||
| Metropolis | 3624 (48.2) | ||
| Medium-sized city | 1739 (23.1) | ||
| Small city | 1055 (14.0) | ||
| Rural area | 1107 (14.7) | ||
| M (SD) | |||
| Mental illness (“Yes”) | 1173 (15.6) | ||
| Depression (PHQ-2) | 2.08 (1.94) | ||
| Generalized anxiety (GAD-7) | 6.76 (5.66) | ||
| COVID-19-anxiety (COVID-19-Anxiety Questionnaire) | 18.34 (7.10) | ||
| Distress (distress thermometer) | 5.68 (3.00) | ||
Differential associative contexts of pandemic-related changes in dietary behavior
To accomplish the phenotyping of dietary behavior during the COVID-19 pandemic, a multiple regression model was computed for each of the two dimensions (RFI and IFI) as an outcome variable. All sociodemographic variables and medical details as well as the presence of a mental disorder were included as regressors. Furthermore, depressive symptoms, generalized anxiety, distress, and COVID-19-anxiety were added, in order to obtain a comprehensive picture of the occurring psychological burden. Homoscedasticity was assessed using a Goldfeld-Quandt test, resulting in no significant changes in residual variance at different levels of the predicted value. Rainbow tests support the assumption of linearity in both models. Regression coefficients are reported in the Supplemental Material.
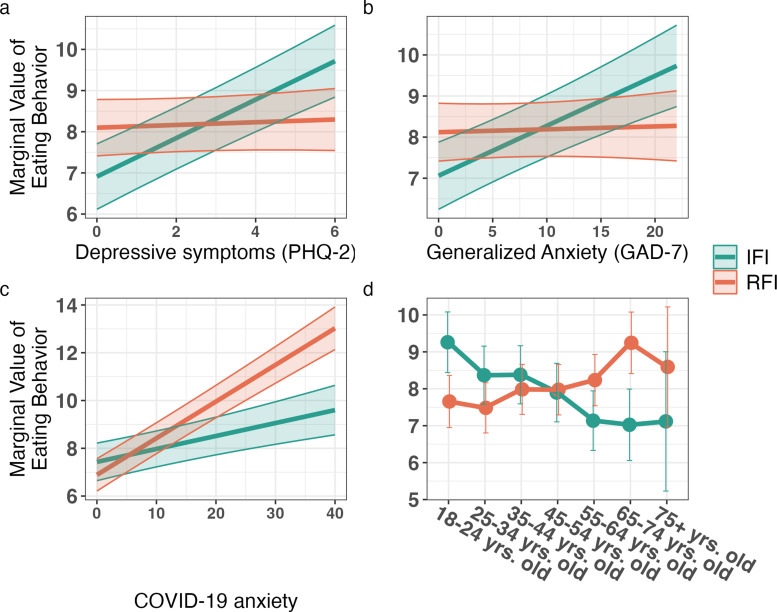
Predicted values of impulsive food intake (IFI) are higher scores of depressive symptoms and symptoms of generalized anxiety, and younger age. In contrast, less depressive symptoms and symptoms of generalized anxiety, higher age, and more COVID-19-related anxiety could be shown as predictors for restrictive (conscious) food intake (RFI).
The associative context of showing increased and unhealthy (=impulsive) and showing decreased and healthy (=restrictive and conscious) food intake differs. The most prominent differences in predictive strength and direction are observed for the variables age, depressive symptoms, and generalized anxiety.
Younger participants react to having an IFI, while RFI is observable for older respondents. Symptoms of depression and generalized anxiety positively covary with pandemic-related shifts toward IFI, in contrast to RFI. A relationship between COVID-19 anxiety and eating more versus eating less was observed. Differences in marginal effects are displayed in Figure 2. Notice that bivariate correlations between the groups reveal similar patterns. A complete report of variable-wise F-tests for global differences, as well as marginal effects for each of the significant variables, is shown in the Supplemental Materials.
Figure 2.
Predicted values of increased and decreased food intake.
Multinomial regression models on subtypes of dietary behaviors
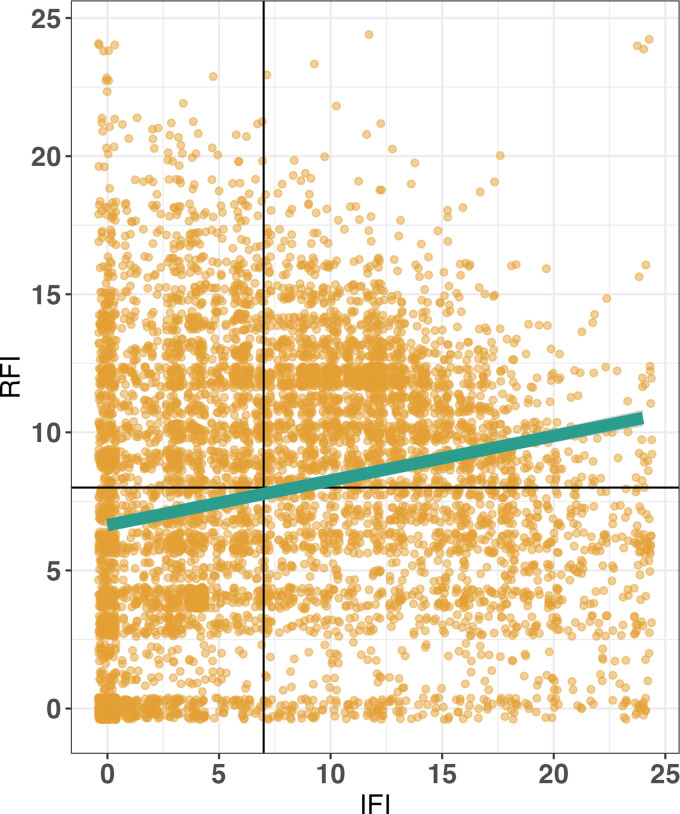
Both scales—RFI and IFI as a result of the pandemic—are far from being orthogonal to each other (see Figure 3). Instead, we find a linear correlation of rs = .258 (or rp = 0.2). This suggests dysfunctional dietary behavior in a significant proportion of participants. This indicates a higher, pandemic-related dysfunctional dietary behavior. In order to characterize this dysfunction, initially median-splits on both scales were used to define four categories (Figures 1 and 4).
Figure 3.
Relationship between impulsive and restrictive food intake. The scales of the impulsive and restrictive food intake (RFI and IFI) show a linear correlation (rs = .258 or rp = 0.2). This indicates the dysfunctional dietary behavior.
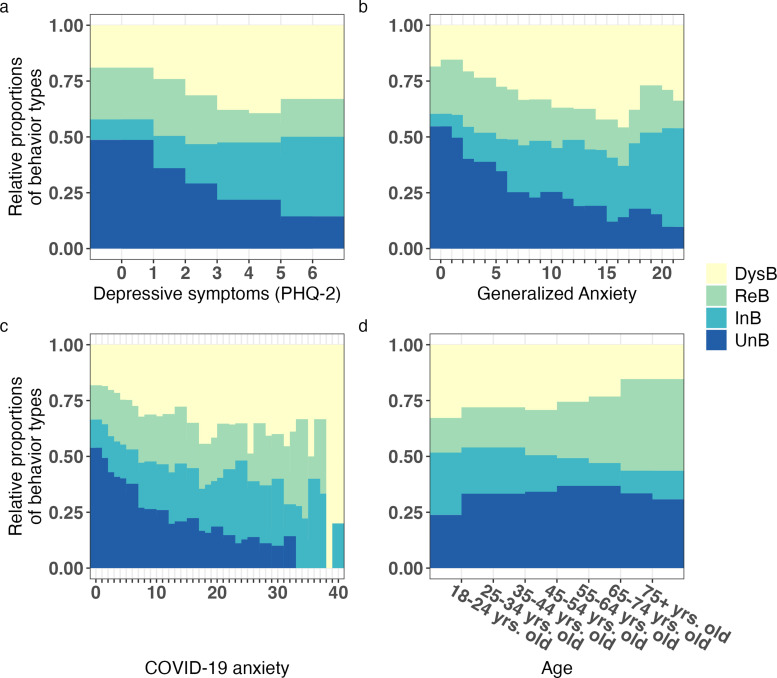
Figure 4.
Associations between the dietary behavior categories and the most relevant dependent variables. Individuals with more depressive symptoms and symptoms of generalized anxiety are more likely to be found in the group of increased and dysfunctional dietary behavior (InB and DysB). Higher scores of COVID-19 anxiety are shown in the proportion of dysfunctional and reduced dietary behavior (DysB and ReB). The categories of increased and dysfunctional dietary behavior seem to be younger (InB and DysB). Categories: “unchanged dietary behavior = UnB,” “reduced dietary behavior = ReB,” “increased dietary behavior = InB,” and “dysfunctional dietary behavior = DysB”.
Then a multinomial regression was applied with these categories as the criteria, and the sociodemographic and medical details as regressors (gender, age, education level, city size, the presence of a mental disorder, depressive symptoms, generalized anxiety, COVID-19 anxiety, and distress). Overall, Nagelkerke's R² amounted to .232. Global F-tests suggested differences in the distribution of the four categories across genders (χ(6) = 15.929, p = 0.014) and age (χ(18) = 88.407, p < 0.001), as well as relationships between the proportions of the four categories and depressive symptoms (χ²(3) = 18.677, p < 0.001), generalized anxiety (χ(3) = 24.326, p < 0.001), distress (χ(3) = 11.30, p = 0.012), and COVID-19 anxiety (χ²(3) = 157.040, p < 0.001; see Supplemental Materials for a full report, including the regression weights, the standard errors, and p-values). Figure 4 shows the associations between the proportions of the four categories and the most relevant dependent variables.
The model suggests that the observed gender differences were negligible. Here, marginal proportion analyses revealed that male participants were slightly more prevalent in DysB (3%) and InB (1%) in comparison to female participants. Participants who indicated to be of “other” gender will not be accounted for due to the small number of cases in this group (n = 43). People having higher scores of depressive symptoms are also more often prevalent in terms of InB and DysB (Figure 4). To put this into perspective, 60.91% of people who are above the critical PHQ-2 score of 3 can be categorized into the DisB-group. On the other hand, only 32.12% of people who score 0, 1, or 2 points in the PHQ-2 fall into this category. Also, while 40.82% of people who are above the PHQ-2 criterion fall into the InB-category, only 15.33% of participants who fall below this criterion report merely increased food intake. A similar pattern also occurs for generalized anxiety (see Figure 4). Here again, individuals who report critically high levels of generalized anxiety (GAD-7 above 10) are twice as often in the DysB-group as people who do not show critically increased generalized anxiety scores (63.35% vs. 33.18%). Similarly, highly anxious participants more often fall into the InB-category (27.56% vs. 17.58%) On the other hand, COVID-19 anxiety is associated with an increased proportion of DysB (Figure 4), as well with people who indicate to have a ReB (Figure 4). Consistent with the linear regression analyses, younger people belong to the InB and DysB categories, while older people tend to more often indicate a ReB (Figure 4).
Discussion
The COVID-19 pandemic has dominated a substantial part of our lives since the beginning of 2020. It has affected a wide variety of life domains, including our mental health and everyday behavior. In particular dietary behavior is tightly linked to emotions and psychological burdens. The aim of the study was to define which variables predict pandemic-related changes in different types of dietary behaviors.
Differential associative features were observed. A high level of psychological burden, indicated by higher depressive symptoms, generalized anxiety, and distress was positively related to IFI. However, COVID-19 anxiety and a higher age acted contradictive: here, increased levels of anxiety and higher age were linked to RFI. Hence, RFI and IFI seemed to emerge and persist under different circumstances with an increased food intake related to a higher psychological burden. However, having an RFI and IFI during the COVID-19 pandemic is not independent. There was a non-negligible number of participants indicating that both behaviors increased in its frequency, respectively. This was followed by an examination of how the dysfunction of the different categories of altered dietary behavior varied across the associative context.
It could be observed that there is an agreement between the two subscales RFI and IF with the results from the linear regression models. The analysis showed that individuals who reported an IFI and a DysB are found often in the critical ranges of an increased psychological burden (higher depressive symptoms, distress, and more generalized anxiety) and had a younger age. In addition, this time participants with a DysB were associated with higher levels of COVID-19 anxiety.
Ouwens et al. (2009) propose that depression increases the likelihood of external, reactive eating, and emotional eating via increased impulsivity and a lack of emotional recognition (Ouwens et al., 2009). Anxiety and obesity are also associated, although a clear mechanistic account is still lacking (Gariepy et al., 2010). Hence, emotional eating seems to be linked to the aberrant pattern of interoception, which is in conformance with recent etiological accounts on depression and anxiety (Paulus and Stein, 2010; Seth and Friston, 2016; Young et al., 2017). Paans et al. (2018), furthermore, suggest that it is mainly the vegetative-depressive symptom cluster that tends to increase the likelihood of emotional eating (Paans et al., 2018). Consequently, depression, anxiety, and increased food intake appear to be tightly linked to each other. In fact, in the presented data, only includes depression, generalized anxiety, distress, and the presence of a diagnosed mental disease in a regression model with eating more as the dependent variable already reaches an R² of .18.
Such type of eating behavior can be—in its extreme form—found in bulimic disorders, where it is assumed to comprise a form of dysfunctional coping mechanism (Meule et al., 2019). In particular, patients appear to respond to negative mood with overeating, but take advantage of periods of positive mood while practicing restricted behavior (Meule et al., 2019). Of course, this behavior appears more cemented in a fully developed eating disorder, which is why the same interpretation cannot easily transferred to our sample from the general population without further assessing mediating mechanisms. Still, an obvious possibility could, however, be a stress-related erosion of the usually functional coping mechanisms, so that people compensate more via adjusting their eating behavior—voluntarily or involuntarily.
Dysfunctional dietary behavior goes along with elevated depressive symptoms and symptoms of generalized anxiety. This result of higher psychological burden in people with dysfunctional dietary behavior is in conformance with an increased comorbidity between depression and anxiety and eating disorders (Walters et al., 1992; Godart et al., 2000; Swinbourne and Touyz, 2007; Hoerster et al., 2015).
The current COVID-19 pandemic affects dietary behavior on the one hand due to the related psychological burden, and on the other hand due to changes in daily life (e.g. loss of job, home office work, hobbies cannot be practiced). European research showed that people feeling bored eats more often than in other emotional states (like anger, anxiety, and depression). Furthermore, a significant increase in emotional eating and uncontrolled eating behavior was reported (Elmacioglu et al., 2021; Koball et al., 2012). Emotional eating (such as food intake because of negative emotions and boredom), and uncontrolled eating behavior, or in the case of this study, dysfunctional dietary behavior is clearly linked to the restricted life during the pandemic (Elmacioglu et al., 2021; Koball et al., 2012). It could be shown, that the reason for an increased food intake is due to the wish of feeling better (Di Renzo et al., 2020).
The desire to feel positive under psychological burden could also explain the dietary behavior of people who report eating both more and less during the pandemic. The dysfunctional dietary behavior reflects their insecurity and anxiety in coping with the current situation. The increased psychological burden may not solely explain changes in dietary behavior. Also, modifications in the daily structure due to increased sitting times in home offices (increased from 5 to 8 h per day) have to be considered (Ammar et al., 2020).
Thus, Ammar et al. (2020) point out that, the important and relevant restrictions to protect public health lead to a change in eating patterns which may course in health problems like being overweight (Ammar et al., 2020). During the pandemic patients with eating disorders reported changes in dietary behavior and enhancement of symptoms of eating disorders like increased restricting, binge eating, purging, and exercise behaviors (Rodgers et al., 2020). However, not only people with eating disorders reported the dysfunctional dietary behavior in previous studies. This could also be shown in the general population (Rodgers et al., 2020). This confirms the results also found in this study.
Nevertheless, it is important to prevent the dysfunctional dietary behavior of actually healthy people lead to a pathological association with food. Due to the increased psychological burden and simultaneously existing dysfunctional dietary behavior, this group of the population is to be considered as more vulnerable to the occurrence of newly diagnosed eating disorders. There should be specific supportive, low-threshold offers for them (Bäuerle et al., 2022). Some of these are already established as online interventions (Bäuerle et al., 2021).
To our knowledge, this present study is currently the largest survey providing relevant evidence for the very first phenotyping of the dietary behavior of populations during the COVID-19 pandemic. However, the limitations of the study must also be considered in its evaluation and interpretation. Indeed, our second analysis containing that applied a categorization based on low versus high levels of IFI and RFI was solely based on median splits. This was a purely exploratory analysis to elucidate the potential benefit of also considering the group of people who reported what we call disorganized or dysfunctional eating behavior. The difficulty here lies in that our questionnaires were not validated before and that, there are no official cut-offs that can—up to a certain extent—discriminate between pathological and non-pathological eating behaviors. At the time of the study, though, there was no validated assessment for this particular topic available. A possibility would be to use the General Dietary Behavior Inventory (GDBI) in follow-up studies (Bäuerle et al., 2022; Marsall et al., 2022). Furthermore, the results of the study are based on self-reporting. Objective verification of the data and diagnoses provided is therefore not possible. There is the possibility of selection bias. Hence, the “high IFI and high RFI”-group is just the upper part of the distribution and does not carry any information about pathology. Still, our analyses could show that sometimes, disorganized eating behavior can exhibit other associative patterns than just reduced or increased food intake. Results from the multinomial regression show that, for instance, the presence of a mental disease increases disorganized eating behavior, but not increased food intake. Similarly, increased COVID-19-related anxiety appears to go along with a pronounced increase in disorganized eating behavior, but less so with increased food intake. Hence, despite not being able to define these eating behaviors as pathological (vs. non-pathological), our data could potentially illustrate that disorganized eating behavior might have different underlying processes.
Conclusion
Dietary behavior during times of the COVID-19 pandemic was phenotyped. The present study clearly showed that the COVID-19 pandemic not only affects psychological health but can lead to the dysfunctional dietary behavior resulting from both restrictive and impulsive food intake. Predictors of dysfunctional dietary behavior seem to be psychologically burdened and young. To prevent dysfunctional dietary behavior and consecutive eating disorders, low-threshold support programs should be established, for example, through online interventions.
Supplemental Material
Supplemental material, sj-docx-1-nah-10.1177_02601060221147768 for The SARS-CoV-2 pandemic causes a dysfunctional dietary behavior: A German cross-sectional study by Hannah Dinse, Adam Schweda, Alexander Bäuerle, Venja Musche, Madeleine Fink, Sheila Geiger, Eva-Maria Skoda and Martin Teufel in Nutrition and Health
Acknowledgements
This study was supported by Essen University Medicine Foundation. We are thankful to our colleagues who provided expertise that greatly assisted the research.
Footnotes
Authors’ contributions: Conceptualization, HD; Methodology, AS; Writing—Original Draft Preparation, HD, AS; Writing—Review & Editing, MF; VM; MT; AB; E-MS, SG, MD; Visualization, HD; AS; Supervision, AB, MT; Project Administration, MT; Funding Acquisition, AB, MT.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committees of the Medical Faculty of the University Duisburg-Essen (20-9307-BO).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent statement: Electronic informed consent was given by all participants. The participation was anonym and voluntary.
ORCID iD: Hannah Dinse https://orcid.org/0000-0002-8855-2699
Supplemental material: Supplemental material for this article is available online.
References
- Ammar A, Brach M, Trabelsi K, et al. (2020) Consortium, OB of the E.-C. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. [DOI] [PMC free article] [PubMed]
- Bäuerle A, Frewer AL, Rentrop V, et al. (2022) Determinants of acceptance of weight management applications in overweight and obese individuals: Using an extended unified theory of acceptance and use of technology model. Nutrients 14(9): 1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bäuerle A, Jahre L, Teufel M, et al. (2021) Evaluation of the E-mental health mindfulness-based and skills-based “CoPE it” intervention to reduce psychological distress in times of COVID-19: Results of a bicentre longitudinal study. Frontiers in Psychiatry 12: 768132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bäuerle A, Teufel M, Musche V, et al. (2020) Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J Public Health (Oxf) 42(4): 672–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta D, Vanelli M. (2020) WHO declares COVID-19 a pandemic. Acta Bio-Medica: Atenei PARmensis 91(1): 157–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Renzo L, Gualtieri P, Cinelli G, et al. (2020) Psychological aspects and eating habits during COVID-19 home confinement: Results of EHLC-COVID-19 Italian online survey. Nutrients 12(7): 2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmacioglu F, Emiroglu E, Ulker MT, et al. (2021) Evaluation of nutritional behavior related to COVID-19.
- Ganley RM. (1989) Emotion and eating in obesity: A review of the literature. International Journal of Eating Disorders 8(3): 343–361. [Google Scholar]
- Gariepy G, Nitka D, Schmitz N. (2010) The association between obesity and anxiety disorders in the population: A systematic review and meta-analysis. International Journal of Obesity (Lond) 34(3): 407–419. [DOI] [PubMed] [Google Scholar]
- Giel KE, Schurr M, Zipfel S, et al. (2021) Eating behaviour and symptom trajectories in patients with a history of binge eating disorder during COVID-19 pandemic. European Eating Disorders Review 29(4): 657–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godart NT, Flament MF, Lecrubier Y, et al. (2000) Anxiety disorders in anorexia nervosa and bulimia nervosa: Co-morbidity and chronology of appearance. European Psychiatry 15(1): 38–45. [DOI] [PubMed] [Google Scholar]
- Hill DC, Moss RH, Sykes-Muskett B, et al. (2018) Stress and eating behaviors in children and adolescents: Systematic review and meta-analysis. Appetite 123: 14–22. [DOI] [PubMed] [Google Scholar]
- Hoerster KD, Jakupcak M, Hanson R, et al. (2015) PTSD and depression symptoms are associated with binge eating among US Iraq and Afghanistan veterans. Eating Behaviors 17: 115–118. [DOI] [PubMed] [Google Scholar]
- Koball AM, Meers MR, Storfer-Isser A, et al. (2012) Eating when bored: Revision of the emotional eating scale with a focus on boredom. Health Psychology 31(4): 521–524. [DOI] [PubMed] [Google Scholar]
- Kohler H, Bauerle A, Schweda A, et al. (2021) Increased COVID-19-related fear and subjective risk perception regarding COVID-19 affects behavior in individuals with internal high-risk diseases. Journal of Primary Care & Community Health 12: 215013272199689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung CMC, Ho MK, Bharwani AA, et al. (2022) Mental disorders following COVID-19 and other epidemics: A systematic review and meta-analysis. Translational Psychiatry 12(1): 05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B, Decker O, Müller S, et al. (2008) Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Medical Care 46(3): 266–274. [DOI] [PubMed] [Google Scholar]
- Löwe B, Kroenke K, Gräfe K. (2005) Detecting and monitoring depression with a two-item questionnaire (PHQ-2). Journal of Psychosomatic Research 58(2): 163–171. [DOI] [PubMed] [Google Scholar]
- Macht M, Mueller J. (2007) Immediate effects of chocolate on experimentally induced mood states. Appetite 49(3): 667–674. [DOI] [PubMed] [Google Scholar]
- Marsall M, Engelmann G, Skoda EM, et al. (2022) Validation of the English version of the general dietary behavior inventory (GDBI-E). International Journal of Environmental Research and Public Health 19(5): 2883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehnert A, Mueller D, Lehmann C, et al. (2006) The German version of the NCCN distress thermometer: Validation of a screening instrument for assessment of psychosocial distress in cancer patients. Zeitschrift fur Psychiatrie Psychologie Und Psychotherapie 54(3): 213–223. [Google Scholar]
- Meule A, Richard A, Schnepper R, et al. (2019) Emotion regulation and emotional eating in anorexia nervosa and bulimia nervosa. Eating Disorders 29(2): 175–191. [DOI] [PubMed] [Google Scholar]
- Moradian S, Bäuerle A, Schweda A, et al. (2021) Differences and similarities between the impact of the first and the second COVID-19-lockdown on mental health and safety behaviour in Germany. J Public Health (Oxf) 43(4): 710–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musche V, Kohler H, Bauerle A, et al. (2021) COVID-19-related fear, risk perception, and safety behavior in individuals with diabetes. Healthcare (Basel) 9(4): 480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization WH (2021a) Obesity and overweight.
- Organization WH (2021b) WHO Coronavirus (COVID-19) Dashboard. Available at:https://covid19.who.int/(accessed 19 October 2022).
- Ouwens MA, van Strien T, van Leeuwe JF. (2009) Possible pathways between depression, emotional and external eating. A structural equation model. Appetite 53(2): 245–248. [DOI] [PubMed] [Google Scholar]
- Paans NPG, Bot M, Brouwer IA, et al. (2018) Contributions of depression and body mass index to body image. Journal of Psychiatric Research 103: 18–25. [DOI] [PubMed] [Google Scholar]
- Paulus MP, Stein MB. (2010) Interoception in anxiety and depression. Brain Structure and Function 214(5-6): 451–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrosa AL, Bitencourt L, Froes ACF, et al. (2020) Emotional, behavioral, and psychological impact of the COVID-19 pandemic. Frontiers in Psychology 11: 566212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petzold MB, Bendau A, Plag J, et al. (2020) Development of the COVID-19-anxiety questionnaire and first psychometric testing. BJPsych Open 6(5): e91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillipou A, Meyer D, Neill E, et al. (2020) Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. International Journal of Eating Disorders 53(7): 1158–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers RF, Lombardo C, Cerolini S, et al. (2020) The impact of the COVID-19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders 53(7): 1166–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlegl S, Maier J, Meule A, et al. (2020a) Eating disorders in times of the COVID-19 pandemic—results from an online survey of patients with anorexia nervosa. International Journal of Eating Disorders 53(11): 1791–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlegl S, Meule A, Favreau M, et al. (2020b) Bulimia nervosa in times of the COVID-19 pandemic-results from an online survey of former inpatients. European Eating Disorders Review 28(6): 847–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt AF, Finan C. (2018) Linear regression and the normality assumption. Journal of Clinical Epidemiology 98: 146–151. [DOI] [PubMed] [Google Scholar]
- Seth AK, Friston KJ. (2016) Active interoceptive inference and the emotional brain. Philosophical Transactions of the Royal Society of London B Biological Sciences 371: 1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinbourne JM, Touyz SW. (2007) The co-morbidity of eating disorders and anxiety disorders: A review. European Eating Disorders Review 15(4): 253–274. [DOI] [PubMed] [Google Scholar]
- Torres SJ, Nowson CA. (2007) Relationship between stress, eating behavior, and obesity. Nutrition (Burbank, Los Angeles County, Calif.) 23(11-12): 887–894. [DOI] [PubMed] [Google Scholar]
- Walters EE, Neale MC, Eaves LJ, et al. (1992) Bulimia nervosa and major depression: A study of common genetic and environmental factors. Psychological Medicine 22(3): 617–622. [DOI] [PubMed] [Google Scholar]
- Wasserstein RL, Schirm AL, Lazar NA. (2019) Moving to a world beyond “p < 0.05”. The American Statistician 73(sup1): 1–19. [Google Scholar]
- Young HA, Williams C, Pink AE, et al. (2017) Getting to the heart of the matter: Does aberrant interoceptive processing contribute towards emotional eating? PLoS One 12(10): e0186312. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-nah-10.1177_02601060221147768 for The SARS-CoV-2 pandemic causes a dysfunctional dietary behavior: A German cross-sectional study by Hannah Dinse, Adam Schweda, Alexander Bäuerle, Venja Musche, Madeleine Fink, Sheila Geiger, Eva-Maria Skoda and Martin Teufel in Nutrition and Health