Abstract
Background
There are multiple reviews on cardiovascular aspects of COVID-19 disease on cardiovascular system in different population but there is lack of evidence about cardiovascular adverse effects of COVID vaccines.
Objectives
The purpose of this study was to compare the cardiac complications of COVID19 vaccines, based on vaccine type (mRNA, vector-based, and inactivated vaccines).
Methods
A systematic search was performed covering PubMed for English case-reports and case-series studies, and finally 100 studies were included.
Results
Myocarditis (with overall rate around 1.62%) was shown to be the most common post-COVID19 immunization cardiac event. More than 90% of post-COVID19 vaccination myocarditis occurred after receiving mRNA vaccines (Moderna & Pfizer-BioNTech), but the report of this event was less in the case of vector-based vaccinations and/or inactivated vaccines. Myocarditis was reported more commonly in men and following the second dose of the immunization. Takotsubo cardiomyopathy (TTC) was reported after mRNA (more commonly) and vector-based vaccinations, with no case report after inactivated vaccines. When mRNA and vector-based vaccinations were used instead of inactivated vaccines, a greater frequency of vaccine-induced thrombotic thrombocytopenia (VITT) and pulmonary emboli (PE) was reported. Myocardial infarction/cardiac arrest was recorded in those beyond the age of 75 years.
Conclusion
The personal and public health benefits of COVID-19 vaccination much outweigh the minor cardiac risks. Reporting bias, regarding more available mRNA vaccines in developed countries, may conflict these results.
Keywords: COVID-19, mRNA vaccine, Adenoviral vector vaccine, Inactivated vaccine, Cardiovascular complications, Review
Introduction
The new coronavirus is known as “Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV2)”, responsible for COVID-19 disease originated in China in 2019 and rapidly became a pandemic. Soon after vaccination was started and till now, 38 types of vaccines are approved in different countries.1, 2, 3 The development of an effective vaccine against the SARS-CoV-2 virus that causes COVID-19 disease has been proven to be a vital tool in controlling the high pandemic's spread and its enormous effects.4 Multiple coronavirus vaccines are currently being developed, including the mRNA-1273 (Moderna), mRNA vaccines BNT162b2 (Pfizer-BioNTech/Comirnaty), adenoviral vector vaccine: Ad26.COV2.S (Johnson & Johnson/Janssen), AZD1222 (Oxford-AstraZeneca/Covidshield) and the inactivated vaccines: CoronaVac (Sinovac Bio (Sputnik V) and WIBP / BBIBP-CorV COVID-19 vaccine (Sinopharm).5
Safety monitoring is an important part of ensuring comprehensive and effective vaccination.6 Safe and effective vaccination is vital to eliminating the SARS-CoV-2 pandemic; however, a substantial number of patients have underlying cardiovascular disease and/or risk factors for heart disease. There are multiple reviews on the effects of COVID-19 disease on the cardiovascular system in different populations but there is a lack of evidence about the cardiovascular adverse effects of COVID vaccines.1 , 2 Some significant cardiovascular adverse effects are linked to COVID-19 immunization, such as the development of myocarditis, pericarditis, or peri myocarditis.5 , 7, 8, 9, 10, 11, 12 Because of the small sample size, tight inclusion criteria, short follow-up periods, and trial participants who may not be the same as the general population who will receive the vaccination, rare or serious vaccine effects may be undetected in phase 3 trials.13 Although pericarditis and myocarditis were not reported as side effects in COVID-19 vaccine in clinical trials, there have been multiple reports of probable cases in the general population following immunization.14 Systematic reviews of case reports are used to summarize current scientific knowledge about rare events.15 It has been believed that in the case of relatively rare events such as cardiovascular-related side effects of COVID-19 vaccines, case reports and case series studies may provide important evidence for systematic reviews. Hence in the present systematic review, we aimed to collect and analyze the case-report and case-series studies on all types of commonly used mRNA, vector-based and inactivated COVID-19 vaccines to compare cardiovascular adverse effects between different types of these vaccines.
Methods
PRISMA 2020 standards for reporting systematic reviews and meta-analyses were followed in this study.16 All three writers conducted and assessed the initial search, screening, and eligibility of the publications, and any disputes were handled by consensus.
Literature search
We performed a search on PubMed for articles reported cardiac complications of mRNA vaccine: BNT162b2 (Pfizer-BioNTech/Comirnaty) and mRNA-1273 (Moderna), and Vector vaccine: AZD1222 (Oxford-AstraZeneca/Covidshield), Ad26.COV2.S (Johnson & Johnson/Janssen), Gam-COVID-Vac (Sputnik V), and JNJ-78,436,735 (Johnson & Johnson). The search strategy in PubMed was as follows:
((“vaccine*”[Title/Abstract]))) OR (Vaccines[MeSH Terms])) OR (jab[Title/Abstract])) OR (Immunization[Title/Abstract])) OR (Immunization[MeSH Terms])) OR (Vaccination[MeSH Terms])) OR (Vaccination[Title/Abstract])) OR (injection[Title/Abstract])) OR (injections[MeSH Terms])) OR (BioNTech[Title/Abstract])) OR (Pfizer[Title/Abstract])) OR (Comirnaty[Title/Abstract])) OR (BNT162b2[Title/Abstract])) OR (“BNT162 Vaccine”[Title/Abstract])) OR (“BNT162 Vaccine”[MeSH Terms])) OR (Moderna[Title/Abstract])) OR (“mRNA-1273″[Title/Abstract])) OR (“2019-nCoV Vaccine mRNA-1273″[MeSH Terms])) OR (“2019-nCoV Vaccine mRNA-1273″[Title/Abstract])) OR (“mRNA Vaccines”[Title/Abstract])) OR (“Johnson & Johnson”[Title/Abstract])) OR (Janssen[Title/Abstract])) OR (AstraZeneca[Title/Abstract])) OR (“ChAdOx1 nCoV-19″[Title/Abstract])) OR (“ChAdOx1 nCoV-19″[MeSH Terms])) OR (AZD1222[Title/Abstract])) OR (Vaxzevria[Title/Abstract])) OR (Covishield[Title/Abstract])) OR (“Sputnik V”[Title/Abstract])) OR (“Gam-COVID-Vac”[Title/Abstract])) OR (“Gam-COVID-Vac vaccine”[Title/Abstract])) OR (“Gam-COVID-Vac vaccine”[MeSH Terms])) OR (“JNJ-78,436,735″[Title/Abstract])) OR (Ad26COVS1[Title/Abstract])) OR (Ad26COVS1[MeSH Terms])) OR (“Ad26.COV2.S”[Title/Abstract])) OR (Janssen[Title/Abstract])) OR (“Adenoviral vector”[Title/Abstract])) AND (heart[Title/Abstract]))) OR (myocardial*[Title/Abstract])) OR (cardio*[Title/Abstract])) OR (coronary*[Title/Abstract])) OR (vascu*[Title/Abstract])) OR (“myocardial infarction”[Title/Abstract])) OR (“myocardial infarction”[MeSH Terms])) OR (heart[MeSH Terms])) OR (Cardiovascular[Title/Abstract])) OR ("Cardiovascular System"[MeSH Terms])) AND (“adverse events”[MeSH Terms]))) OR (“adverse events”[Title/Abstract])) OR (“adverse effects”[Title/Abstract])) OR (“adverse effects”[MeSH Terms])) OR (“side effects”[MeSH Terms])) OR (“side effects”[Title/Abstract])) OR (“Complications”[Title/Abstract])) OR (“Complications”[MeSH Terms]) AND LitCCASEREPORT[filter])). We used a predefined filter of PubMed for identifying case report studies on COVID-19 regarding our search term.
Eligibility criteria and study selection
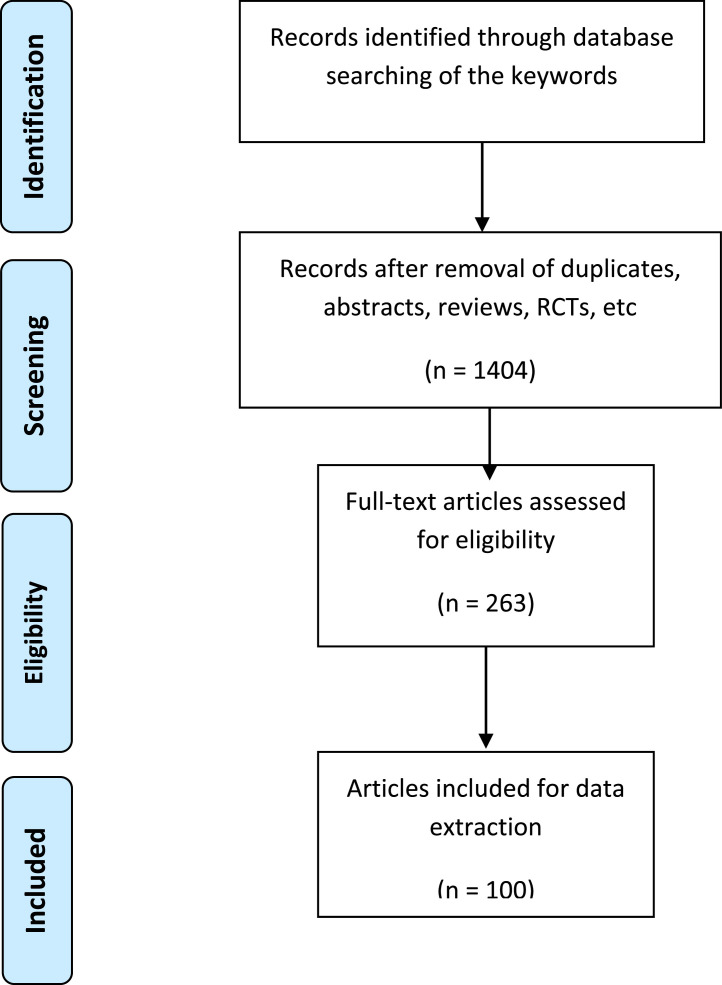
After the initial search, duplicate entries, reviews, clinical studies, clinical trials, and full-text articles that were unavailable were eliminated. We considered English case reports and case-series studies. Then, based on the title and abstract, the article records were evaluated and excluded if they had an unsuitable correlation with the current study keywords. The full-text papers were then evaluated for qualifying criteria (Table 1 ). Fig. 1 shows the study selection process.
Table 1.
Eligibility criteria.
| No. | Criteria | Description |
|---|---|---|
| 1. | Study Design | Inclusion: Case-reports-case-seriesExclusion: A review article, clinical study, clinical trials, cohort studies |
| 2. | Population | Inclusion: People who received COVID-19 vaccinationExclusion: N/A* |
| 3. | Intervention | Inclusion: COVID-19 vaccinationExclusion: N/A* |
| 4. | Outcome | Inclusion: Cardiovascular eventsExclusion: N/A* |
| 5. | Language | Inclusion: EnglishExclusion: N/A* |
| 6. | Time of Publication | Inclusion: No beginning date- January 2022Exclusion: N/A* |
*N/A; Not Applicable.
Fig. 1.
Flowchart of study selection.
Results and discussion
A total of 100 case reports or case series which reported cardiac complications after COVID-19 vaccination were included.17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117 The manifestations, treatment, and outcomes of cardiac complications of COVID-19 vaccination, are summarized in Table 2 .
Table 2.
Reviewing the severity of post-COVID-19 vaccination cardiac manifestations, treatments, and outcomes.
| Cardiac event | Manifestations/diagnosis criteria | Treatment | Outcome | Incidence in vaccine groups |
|---|---|---|---|---|
| Myocarditis/ Pericarditis | Chest pain, pulmonary edema, inappropriate exertional tachycardia, exertional dyspneaThe diagnosis of myocarditis was established after a cardiac MRI | Medication and rest(admission based on patient risk) | Patients felt better quickly and following an improvement in their symptoms, patients can typically resume their regular daily activities | 70- 80% of the patients received the mRNA COVID-19 vaccine, while 20- 25% received other types.29,124,125 |
| Takotsubo cardiomyopathy (TTC) | Chest pain, transitory left ventricular failure, electrocardiographic abnormalities, an increased troponin level, the lack of occlusive coronary artery disease | Admission to the hospital and supportive care | All patients recovered from their symptoms, patients can typically resume their regular daily activities | 80% of the patients received the mRNA COVID-19 vaccine, while 20% received other types.134 |
| Myocardial infarction (MI) | Chest pain/discomfort | Admission to the hospital and management based on guidelines | Some patients developed heart failure, some cardiogenic shock, some were intubated, and some had cardiovascular-related mortality | No exact statistics were found |
| vaccine-induced thrombotic thrombocytopenia (VITT)/ pulmonary embolism (PE) | Breathlessness, Pain in the chest or stomach, swelling or coldness in a leg, severe or worsening headache or blurred vision after vaccination, persistent bleeding, reddish or purplish spots, or blood blisters under the skin | Admission to the hospital, treatment with nonheparin anticoagulation, followed by a rapid increase in platelet count102,106 | Thrombocytopenia associated, pulmonary embolism and portal vein thrombosis is more frequently in women under 55 | Most frequently reported after the use of the Vaxzevria (AstraZeneca) vaccine(106), next after the use of Janssen, and rarely by the use of mRNA vaccines |
Myocarditis/ pericarditis/ myopericarditis
Myocarditis is defined as inflammation of the heart muscle (myocardium). Inflammation happens when the immune system responds to internal or external stimuli for example viral infections as well as more systemic inflammatory illnesses including autoimmune disorders.118 In myopericarditis, chest pain, increased levels of cardiac enzymes and electrocardiographic changes occur. Pericarditis is a somewhat prevalent cause of chest pain, and around 5% of all hospitalizations for chest pain are due to pericarditis.119 Myocarditis has been reported as a major side effect of these vaccines; however, the overall rate of post-COVID19 vaccination-myocarditis is around 1.62% which is very small.120, 121, 122
mRNA vaccines
A study by Abu Mouch et al. reported 6 cases of myocarditis (5 cases after the second dose and 1 case after the first dose) with no evidence of COVID-19 infection, which occurred shortly after the mRNA vaccine Pfizer/BioNTech BNT162b2 injection. In their study, the diagnosis of myocarditis was established after cardiac MRI and all 6 cases were male.29 Another study by Al-Rasbi et al. in Oman also reported a case of a 37-year-old male subject with myocarditis, who presented with pulmonary edema. He demonstrated severe multisystem involvement including thrombocytopenia, rhabdomyolysis, pulmonary hemorrhage, and non-oliguric acute kidney injury after the BNT162b2 mRNA vaccine.34 Alania-Torres et al. reported another case of myocarditis in patients with arrhythmogenic left ventricular cardiomyopathy (ALVC) after mRNA vaccination against COVID-19.35 A case of fatal fulminant necrotizing myocarditis also has been reported in New Zealand for a 57-year-old female, after receiving the first dose of the Pfizer-BioNTech vaccine.36 A study from Korea reported a 22-year-old man who developed myocarditis 5 days after the first dose of the BNT162b2 mRNA vaccine and died 7 h later.44 Myocarditis also occurred after mRNA COVID vaccines in paediatrics as reported for a 17 years old boy,89 and a 14-year-old male subject.108 Istampoulouoglou et al. reported a series of 9 cases with perimyocarditis, 5 myocarditis cases, and 3 pericarditis cases.95 Another case series study reported 9 cases of acute pericarditis of them seven received mRNA vaccines BNT162b2 and mRNA-1273, and 2 cases received AZD1222.99 Several more case-report studies documented myocarditis or recurrence of acute myocarditis after receiving mRNA vaccination against COVID-19 infection.5 , 7, 8, 9, 10, 11 , 17 , 18 , 20 , 22 , 24 , 37, 38, 39 , 41, 42, 43 , 47, 48, 49, 50, 51, 52, 53, 54, 55 , 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68 , 71 , 72 , 75 , 77 , 80 , 81 , 83 , 88 , 90 , 91 , 98 , 109 , 110 , 123 Myocarditis was reported to be more common in patients who received the COVID-19 mRNA vaccine versus the non-mRNA vaccine, and it was also more common in patients who received the vaccine for the second time. It was also found to be more common in men and patients aged 16 to 39 years.124 , 125
Non-mRNA vaccines (vector-based vaccines/ inactivated vaccines)
A recent systematic review on myocarditis after COVID-19 vaccination reported only one case after Astra Zeneca, one case after Sputnik V injection, and one case after vector Johnson & Johnson, out of a total of 277 cases.120 A 32-year-old female case developed myocarditis on the third day after receiving the first dose of the AstraZeneca. The patient started experiencing inappropriate exertional tachycardia and exertional dyspnea.111 A case report of myocarditis following the administration of the Janssen vaccine in a healthy, young male also has been reported.112 A study in Brazil reported a 47-year-old African-American male patient with type 2 diabetes and a previous history of COVID-19 infection. He had heart failure as a result of myocarditis after the second dose of an inactivated COVID-19 vaccine.45 Other studies reported no myocarditis incidence in a subject receiving inactivated COVID-19 vaccine.126 , 127 A population-based study also showed that mainly, two mRNA vaccines mRNA-1273 (Moderna) & BNT162b2 (Pfizer-BioNTech) were more associated with increased risks for myocarditis/pericarditis compared to all other vaccines forms including viral vector vaccines of Ad26.COV2.S (Janssen) and AstraZeneca.128
Proposed mechanisms for COVID-19 vaccines induced- Myocarditis
The existence of modest residual quantities of double-strand RNA (dsRNA) in mRNA COVID-19 vaccine preparations has been documented.129 , 130 Double-strand RNA (dsRNA) is well-known for inducing immune-inflammatory responses. The presence of dsRNA in vaccine nanoparticles might be the source of the unsolved instances of myocarditis.129 , 130 Patients who have experienced a past or recent experience of myocarditis constitute a prospective "susceptible" population that poses a treatment problem. In this population, patients are discouraged from obtaining COVID-19 immunization in the first 6 months after the onset of illness or in the context of chronic or relapsing troponin release.131 Most patients who received care for myocarditis or pericarditis responded well to medication and rest, with benign clinical course. It is worth noting that individual and public health advantages of COVID-19 immunization outweigh the modest risk of myocarditis following vaccination which could be resolved usually within days or weeks.8 , 132
Takotsubo cardiomyopathy (TTC)
Takotsubo cardiomyopathy (TTC) is an acute transient left ventricular systolic dysfunction, after physical or emotional stress that is in differential diagnosis with myocardial infarction. Adrenergic stimuli, coronary vasospasm, microvascular dysfunction, inflammation, and alteration in cellular metabolism have been proposed to be responsible for this entity.133
mRNA vaccines
A systematic review study on the prevalence of TTC after receiving COVID-19 vaccines included 10 case reports and their results showed that 80% of the patients received the mRNA vaccines, while 20% received other non-mRNA vaccines.134 According to their results, TTC happened more frequently in female subjects compared to male subjects (90% vs. 10%), and in half of the subjects, TTC occurred after receiving the first dose.134 Boscolo et al. reported a TTC case related to a healthy 30-year-old Asian female subject following mRNA COVID-19 vaccination (Pfizer).40 A case of an 80-year-old woman on maintenance hemodialysis who developed TTC 4 days after administration of the first dose of the Pfizer-BioNTech COVID-19 vaccine also has been reported,85 and a 73-year-old woman with recently diagnosed myocardial infarction (MI) found to have TTC immediately a day after administration of mRNA Moderna vaccine.86
Non-mRNA vaccines (vector-based vaccines/ inactivated vaccines)
There are reports of TTC after COVID-19.76 , 113 Three cases of TTC have been reported for vector-based vaccines; a case of TTC for chadox1 Nov-19 adenoviral vector vaccine (AstraZeneca) was reported in a 72-year-old male subject.46 Another case of TTC was also reported short term following AstraZeneca injection.56 The third case reported by Stewart et al. was an unusual female case of TTC who was the first case of a patient on hemodialysis and showed TTC symptoms 8 days after receiving the second dose of the DNA ChadOX1 nCOV-19 (AZD122) vaccination.76 TTC was verified based on the results, which included transitory left ventricular failure, electrocardiographic abnormalities, an increased troponin level, and the lack of occlusive coronary artery disease. We found no reports of TTC caused by inactivated COVID-19 vaccines. An exclusive systematic review of the TCC cases following COVID-19 vaccination also reported no cases after inactive COVID-19 vaccination.134
Recommended mechanisms for COVID-19 vaccines induced-TTC
Most of the participants who experienced TTC were female, and their age range for DNA vaccine /vector-based vaccines was around 50 years old, but for mRNA vaccines, it was around 60 years old. Acute emotional or physical stress increases cortisol hormone and catecholamine levels and their bioavailability in the blood, which mediates many routes such as direct damage of muscle cells, microvascular malfunction, and pericardial coronary artery spasm that all of these pathways are associated with TTC.135 TTC patients have impaired neural networks in limbic brain regions such as the amygdala, prefrontal cortex, and hippocampus during stress.134 Risk factors for COVID-19 vaccine-TTC reported as sex, age, and anxiety about the vaccine.86 The overall rate of TTC incidence after COVID-19 vaccination is rare, but can be life-threatening. Chest pain should be taken seriously as an alarming symptom.134
Myocardial infarction (MI)
mRNA vaccines
A case-series study in the UK reported an increased risk of MI after BNT162b2 (Pfizer-BioNTech) mRNA vaccination.93 Sung et al.97 and Kunis et al.96 reported 2 cases and 1 case of MI, occurred 24 h post-vaccination with mRNA vaccines respectively. A population-based study reported the short-term risk of severe cardiovascular events including MI in people aged 75 years or older following the administration of BNT162b2 mRNA COVID-19 vaccination.11 A WHO report also confirmed that vaccines related to MI, cardiac arrest, and circulatory collapse were observed in the age group >75 years.136
Non-mRNA vaccines (vector-based vaccines/ inactivated vaccines)
A 40-year-old man with no history of cardiovascular disease manifested with retrosternal chest discomfort 8 days after receiving the ChAdOx1 nCov-19 vaccination against COVID-19, ST elevation in the electrocardiogram and regional wall motion abnormality in echocardiography. His-blood testing revealed a high level of d-dimer, a troponin of 3185 ng/L with a strongly positive platelet factor-4 (PF-4) antibody test. On coronary angiography, an obstruction of the left anterior descending coronary artery was discovered. His-platelet counts increased after 6 days, and his PF-4 antibody, d-dimer, and troponin levels decreased. After 14 days, he was successfully discharged.92 Hsu et al. also reported a case of 33 years old male subject who presented acute ST-Segment elevation MI following ChAdOx1 nCoV-19 vaccination in Taiwan.94
Recommended mechanisms for COVID-19 vaccines induced-MI
Some hypotheses can be made since there is currently no experiment being conducted to specifically examine the incidence of MI among recipients of the COVID-19 vaccine. First, it has been proposed that the thrombotic phenomenon following vaccination was caused by vaccine-induced thrombotic thrombocytopenia (VITT) as a possible mechanism, a condition related to heparin-induced thrombocytopenia.115 , 116 The second hypothesis is that after vaccination, a supply and demand mismatch occurs in a diseased cardiovascular system.137 It is also possible that a vasospastic allergic MI known as Kounis syndrome occurred in response to COVID-19 vaccines.138 , 139 However, the pathogenic mechanism underlying most cases remains undetermined.117
Pulmonary hemorrhage/ pulmonary embolism/ thrombotic thrombocytopenia (VITT)
mRNA vaccines
Al-Rasbi et al. presented a 37-year-old man with myocarditis, pulmonary edema, and pulmonary hemorrhage 12 days after receiving the first dose of Pfizer mRNA COVID-19 vaccination. He responded favorably to a 5-day course of intravenous methylprednisolone and immunoglobulin.34 A case-series study also reported a short-term risk of pulmonary embolism (PE) among French residents aged 75 years or older after receipt of the BNT162b2 mRNA injection.11 A study in Italy also reported a combination of acute exacerbation of interstitial lung diseases and PE in an elderly patient after booster mRNA vaccination against COVID-19.100 A study in Saudi Arabia also reported a 78-year-old case with PE one day after receiving the second dosage of the Pfizer vaccine.103 Another case of a healthy 24-year-old young man with PE due to the Pfizer vaccine also reported that his symptoms started 6 h after administration of the second dose of vaccine.104 Idiopathic pulmonary fibrosis also was found after the Pfizer vaccine which was successfully treated with a short course of glucocorticoids.105
Non-mRNA vaccines (vector-based vaccines /inactivated vaccines)
VITT has emerged as a rare side effect of adenoviral vector-based vaccines against coronavirus disease 2019 (COVID-19) and is most frequently reported after the use of the Vaxzevria (AstraZeneca) vaccine.106 A 73-year-old case with PE was reported two weeks after receiving inactivated COVID-19 vaccine.102 A study in Germany reported a case with life-threatening bilateral PE as a complication of vaccine-induced thrombotic thrombocytopenia (VITT) after the first dose of the Oxford-AstraZeneca vaccine.101 A rare case of small segmental PE and VITT was reported for a 47-year-old woman 0 days after receiving the AstraZeneca vaccination.107 A case with VITT and PE was reported13 days after receiving the single dose of Janssen vaccines.106 Based on early clinical suspicion, the patient was treated with corticosteroids and intravenous immunoglobulin, which resulted in a rapid increase in platelet count, allowing full-dose anticoagulation to be administered on time. However, intravenous immunoglobulin treatment may mask the ability of anti-platelet factor 4-heparin antibodies to bind and activate platelets in the presence of heparin, resulting in false-negative immunoassay functional test results.
Recommended mechanisms for COVID-19 vaccines induced-VITT
Antibodies that target platelet factor 4 (PF4, also known as CXCL4) are responsible for VITT. The low affinities of platelet Fc-IIa receptors to these antibodies, which are immunoglobulin G (IgG) molecules, activate platelets.140 , 141 Investigations are being conducted to determine the mechanism(s) by which the implicated vaccines cause the production of new antibodies (and/or immune stimulation of already-existing antibodies). According to an evolving model, the vaccine stimulates the formation of neoantigens (the first struck) and a systemic inflammatory response (the second struck), which together cause the production of anti-PF4 antibodies. Virus proteins from the HEK3 cell line and free DNA are examples of vaccine components that could bind to PF4 and change its conformation, creating a neoantigen. According to preliminary research, adenoviral hexon proteins bound to PF4 may be to blame.114 , 141 , 142
Conclusion
Our study showed that myocarditis was the most reported post-COVID19 vaccination cardiac event. All reported cardiac events including myocarditis, TTC, MI, and VITT occurred most frequently after receiving mRNA vaccines (Moderna & Pfizer-BioNTech). In the case of vector-based vaccines and/or inactivated vaccines, the prevalence of myocarditis and TTC were lower. Myocarditis was also more common in men between the ages of 16 and 39. MI/cardiac arrest was observed in the age group >75 years and was very rare. There have been no reports of TTC occurring after the injection of inactivated COVID-19 vaccines. Finally, the personal and public health advantages of COVID-19 immunization much outweigh the modest cardiac risk of that, which usually disappears in a matter of days or weeks. Reporting bias, regarding more available mRNA vaccines in developed countries, may conflict these results.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
References
- 1.Soleimani A., Soleimani Z. Presentation and outcome of congenital heart disease during COVID-19 pandemic: a review. Curr Probl Cardiol. 2022;47(1) doi: 10.1016/j.cpcardiol.2021.100905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hantoushzadeh S., Nabavian S.M., Soleimani Z., Soleimani A. COVID-19 disease during pregnancy and peripartum period: a cardiovascular review. Curr Probl Cardiol. 2022;47(1) doi: 10.1016/j.cpcardiol.2021.100888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chandra A., Gurjar V., Qamar I., Singh N. Exploring potential inhibitor of SARS-CoV2 replicase from FDA approved drugs using insilico drug discovery methods. J Biomol Struct Dyn. 2021 doi: 10.1080/07391102.2020.1871416. [DOI] [PubMed] [Google Scholar]
- 4.Xia S., Duan K., Zhang Y., Zhao D., Zhang H., Xie Z., et al. Effect of an inactivated vaccine against SARS-CoV-2 on safety and immunogenicity outcomes: interim analysis of 2 randomized clinical trials. JAMA. 2020;324(10):951–960. doi: 10.1001/jama.2020.15543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho J.S., Sia C.H., Ngiam J.N., Loh P.H., Chew N.W., Kong W.K., et al. A review of COVID-19 vaccination and the reported cardiac manifestations. Singapore Med J. 2021 doi: 10.11622/smedj.2021210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Griffin M.R., Braun M.M., Bart K.J. What should an ideal vaccine postlicensure safety system be? Am J Public Health. 2009;99 doi: 10.2105/AJPH.2008.143081. Suppl 2(Suppl 2):S345-S50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hendren N.S., Carter S., Grodin J.L. Severe COVID-19 vaccine associated myocarditis: zebra or unicorn? Int J Cardiol. 2021;343:197–198. doi: 10.1016/j.ijcard.2021.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heymans S., Cooper L.T. Myocarditis after COVID-19 mRNA vaccination: clinical observations and potential mechanisms. Nat Rev Cardiol. 2022;19(2):75–77. doi: 10.1038/s41569-021-00662-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Husby A., Hansen J.V., Fosbøl E., Thiesson E.M., Madsen M., Thomsen R.W., et al. SARS-CoV-2 vaccination and myocarditis or myopericarditis: population based cohort study. BMJ. 2021;375 doi: 10.1136/bmj-2021-068665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Isaak A., Feisst A., Luetkens J.A. Myocarditis following COVID-19 vaccination. Radiology. 2021;301(1):E378. doi: 10.1148/radiol.2021211766. -e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jabagi M.J., Botton J., Bertrand M., Weill A., Farrington P., Zureik M., et al. Myocardial infarction, stroke, and pulmonary embolism after BNT162b2 mRNA COVID-19 vaccine in people aged 75 years or older. JAMA. 2022;327(1):80–82. doi: 10.1001/jama.2021.21699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pepe S., Gregory A.T., Myocarditis DennissAR. Pericarditis and cardiomyopathy after COVID-19 vaccination. Heart Lung Circ. 2021;30(10):1425–1429. doi: 10.1016/j.hlc.2021.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Callaghan K.P., Blatz A.M., Offit P.A. Developing a SARS-CoV-2 vaccine at warp speed. JAMA. 2020;324(5):437–438. doi: 10.1001/jama.2020.12190. [DOI] [PubMed] [Google Scholar]
- 14.Patone M., Mei X.W., Handunnetthi L., Dixon S., Zaccardi F., Shankar-Hari M., et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2022;28(2):410–422. doi: 10.1038/s41591-021-01630-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nambiema A., Sembajwe G., Lam J., Woodruff T., Mandrioli D., Chartres N., et al. A protocol for the use of case reports/studies and case series in systematic reviews for clinical toxicology. Front Med. 2021;8 doi: 10.3389/fmed.2021.708380. (Lausanne) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marshall M., Ferguson I.D., Lewis P., Jaggi P., Gagliardo C., Collins J.S., et al. Symptomatic acute myocarditis in 7 adolescents after Pfizer-BioNTech COVID-19 vaccination. Pediatrics. 2021;148(3) doi: 10.1542/peds.2021-052478. [DOI] [PubMed] [Google Scholar]
- 18.Deb A., Abdelmalek J., Iwuji K., Nugent K. Acute myocardial injury following COVID-19 vaccination: a case report and review of current evidence from vaccine adverse events reporting system database. J Prim Care Community Health. 2021;12 doi: 10.1177/21501327211029230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Welsh K.J., Baumblatt J., Chege W., Goud R., Nair N. Thrombocytopenia including immune thrombocytopenia after receipt of mRNA COVID-19 vaccines reported to the vaccine adverse event reporting system (VAERS) Vaccine. 2021;39(25):3329–3332. doi: 10.1016/j.vaccine.2021.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park J., Brekke D.R., Bratincsak A. Self-limited myocarditis presenting with chest pain and ST segment elevation in adolescents after vaccination with the BNT162b2 mRNA vaccine. Cardiol Young. 2022;32(1):146–149. doi: 10.1017/S1047951121002547. [DOI] [PubMed] [Google Scholar]
- 21.Nassar M., Nso N., Gonzalez C., Lakhdar S., Alshamam M., Elshafey M., et al. COVID-19 vaccine-induced myocarditis: case report with literature review. Diabetes Metab Syndr. 2021;15(5) doi: 10.1016/j.dsx.2021.102205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oster M.E., Shay D.K., Su J.R., Gee J., Creech C.B., Broder K.R., et al. Myocarditis cases reported after mRNA-based COVID-19 vaccination in the US from. JAMA. 2022;327(4):331–340. doi: 10.1001/jama.2021.24110. December 2020 to August 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shams P., Ali J., Saadia S., Khan A.H., Sultan F.A.T., Tai J. COVID-19 BBIBP-CorV vaccine and transient heart block - A phenomenon by chance or a possible correlation - A case report. Ann Med Surg (Lond) 2021;71 doi: 10.1016/j.amsu.2021.102956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mansour J., Short R.G., Bhalla S., Woodard P.K., Verma A., Robinson X., et al. Acute myocarditis after a second dose of the mRNA COVID-19 vaccine: a report of two cases. Clin Imaging. 2021;78:247–249. doi: 10.1016/j.clinimag.2021.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muthukumar A., Narasimhan M., Li Q.-.Z., Mahimainathan L., Hitto I., Fuda F., et al. In-depth evaluation of a case of presumed myocarditis after the second dose of COVID-19 mRNA vaccine. Circulation. 2021;144(6):487–498. doi: 10.1161/CIRCULATIONAHA.121.056038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McLean K., Johnson T.J. Myopericarditis in a previously healthy adolescent male following COVID-19 vaccination: a case report. Acad Emerg Med. 2021;28(8):918–921. doi: 10.1111/acem.14322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ammirati E., Cavalotti C., Milazzo A., Pedrotti P., Soriano F., Schroeder J.W., et al. Temporal relation between second dose BNT162b2 mRNA COVID-19 vaccine and cardiac involvement in a patient with previous SARS-COV-2 infection. Int J Cardiol Heart Vasc. 2021;34 doi: 10.1016/j.ijcha.2021.100774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cereda A., Conca C., Barbieri L., Ferrante G., Tumminello G., Lucreziotti S., et al. Acute myocarditis after the second dose of SARS-CoV-2 vaccine: serendipity or atypical causal relationship? Anatol J Cardiol. 2021;25(7):522–523. doi: 10.5152/AnatolJCardiol.2021.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abu Mouch S., Roguin A., Hellou E., Ishai A., Shoshan U., Mahamid L., et al. Myocarditis following COVID-19 mRNA vaccination. Vaccine. 2021;39(29):3790–3793. doi: 10.1016/j.vaccine.2021.05.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aiba T., Ishibashi K., Hattori K., Wada M., Ueda N., Miyazaki Y., et al. Frequent premature ventricular contraction and non-sustained ventricular tachycardia after the SARS-CoV-2 vaccination in patient with implantable cardioverter defibrillator due to acquired long-QT syndrome. Circ J. 2021;85(11):2117. doi: 10.1253/circj.CJ-21-0515. [DOI] [PubMed] [Google Scholar]
- 31.Kim D., Choi J.H., Jang J.Y., So O., Cho E., Choi H., et al. A case report for myopericarditis after BNT162b2 COVID-19 mRNA vaccination in a Korean young male. J Korean Med Sci. 2021;36(39):e277. doi: 10.3346/jkms.2021.36.e277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim H.W., Jenista E.R., Wendell D.C., Azevedo C.F., Campbell M.J., Darty S.N., et al. Patients with acute myocarditis following mRNA COVID-19 vaccination. JAMA Cardiol. 2021;6(10):1196–1201. doi: 10.1001/jamacardio.2021.2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim Y., Zhu Z., Kochar P., Gavigan P., Kaur D., Kumar A. A pediatric case of sensory predominant guillain-barré syndrome following COVID-19 vaccination. Child Neurol Open. 2022;9 doi: 10.1177/2329048X221074549. 2329048x221074549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al-Rasbi S., Al-Maqbali J.S., Al-Farsi R., MA AlShukaili, Al-Riyami M.H., Z AlFalahi, et al. Myocarditis, pulmonary hemorrhage, and extensive myositis with rhabdomyolysis 12 days after first dose of Pfizer-BioNTech BNT162b2 mRNA COVID-19 vaccine: a case report. Am J Case Rep. 2022;23 doi: 10.12659/AJCR.934399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alania-Torres E., Morillas-Climent H., García-Escrivá A., Vinueza-Buitrón P., Poquet-Catalá I., Zorio E., et al. Case report: probable myocarditis after COVID-19 mRNA vaccine in a patient with arrhythmogenic left ventricular cardiomyopathy. Front Cardiovasc Med. 2021;8 doi: 10.3389/fcvm.2021.759119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ameratunga R., Woon S.T., Sheppard M.N., Garland J., Ondruschka B., Wong C.X., et al. First identified case of fatal fulminant necrotizing eosinophilic myocarditis following the initial dose of the Pfizer-BioNTech mRNA COVID-19 vaccine (BNT162b2, Comirnaty): an extremely rare idiosyncratic hypersensitivity reaction. J Clin Immunol. 2022:1–7. doi: 10.1007/s10875-021-01187-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aviram G., Viskin D., Topilsky Y., Sadon S., Shalmon T., Taieb P., et al. Myocarditis associated with COVID-19 booster vaccination. Circ Cardiovasc Imaging. 2022;15(2) doi: 10.1161/CIRCIMAGING.121.013771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bautista García J., Peña Ortega P., Bonilla Fernández J.A., Cárdenes León A., Ramírez Burgos L., Caballero Dorta E. Acute myocarditis after administration of the BNT162b2 vaccine against COVID-19. Rev Esp Cardiol (Engl Ed) 2021;74(9):812–814. doi: 10.1016/j.rec.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bengel C.P., Kacapor R. A report of two cases of myocarditis following mRNA coronavirus disease 2019 vaccination. Eur Heart J Case Rep. 2022;6(1) doi: 10.1093/ehjcr/ytac004. ytac004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boscolo Berto M., Spano G., Wagner B., Bernhard B., Häner J., Huber A.T., et al. Takotsubo cardiomyopathy after mRNA COVID-19 vaccination. Heart Lung Circ. 2021;30(12):e119. doi: 10.1016/j.hlc.2021.06.521. -e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bozkurt B., Kamat I., Hotez P.J. Myocarditis with COVID-19 mRNA vaccines. Circulation. 2021;144(6):471–484. doi: 10.1161/CIRCULATIONAHA.121.056135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Caforio A.L.P. Receipt of mRNA vaccine against COVID-19 and myocarditis. N Engl J Med. 2021;385(23):2189–2190. doi: 10.1056/NEJMe2116493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chamling B., Vehof V., Drakos S., Weil M., Stalling P., Vahlhaus C., et al. Occurrence of acute infarct-like myocarditis following COVID-19 vaccination: just an accidental co-incidence or rather vaccination-associated autoimmune myocarditis? Clin Res Cardiol. 2021;110(11):1850–1854. doi: 10.1007/s00392-021-01916-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Choi S., Lee S., Seo J.W., Kim M.J., Jeon Y.H., Park J.H., et al. Myocarditis-induced Sudden Death after BNT162b2 mRNA COVID-19 Vaccination in Korea: case report focusing on histopathological findings. J Korean Med Sci. 2021;36(40):e286. doi: 10.3346/jkms.2021.36.e286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Riedel P.G., Sakai V.F., Toniasso S.C.C., Brum M.C.B., Fernandes F.S., Pereira R.M., et al. Heart failure secondary to myocarditis after SARS-CoV-2 reinfection: a case report. Int J Infect Dis. 2021;113:175–177. doi: 10.1016/j.ijid.2021.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Crane P., Wong C., Mehta N., Barlis P. Takotsubo (stress) cardiomyopathy after ChAdOx1 nCoV-19 vaccination. BMJ Case Rep. 2021;14(10) doi: 10.1136/bcr-2021-246580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.D'Angelo T., Cattafi A., Carerj M.L., Booz C., Ascenti G., Cicero G., et al. Myocarditis after SARS-CoV-2 vaccination: a vaccine-induced reaction? Can J Cardiol. 2021;37(10):1665–1667. doi: 10.1016/j.cjca.2021.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.De Jesus M.L., Yabut J., Kumar M., Meng J. Cardiac adverse reactions with COVID-19 vaccinations. Cureus. 2022;14(1):e21372. doi: 10.7759/cureus.21372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ehrlich P., Klingel K., Ohlmann-Knafo S., Hüttinger S., Sood N., Pickuth D., et al. Biopsy-proven lymphocytic myocarditis following first mRNA COVID-19 vaccination in a 40-year-old male: case report. Clin Res Cardiol. 2021;110(11):1855–1859. doi: 10.1007/s00392-021-01936-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Facetti S., Giraldi M., Vecchi A.L., Rogiani S., Nassiacos D. [Acute myocarditis in a young adult two days after Pfizer vaccination] G Ital Cardiol (Rome) 2021;22(11):891–893. doi: 10.1714/3689.36746. [DOI] [PubMed] [Google Scholar]
- 51.Foltran D., Delmas C., Flumian C., De Paoli P., Salvo F., Gautier S., et al. Myocarditis and pericarditis in adolescents after first and second doses of mRNA COVID-19 vaccines. Eur Heart J Qual Care Clin Outcomes. 2022;8(2):99–103. doi: 10.1093/ehjqcco/qcab090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gellad W.F. Myocarditis after vaccination against COVID-19. BMJ. 2021;375:n3090. doi: 10.1136/bmj.n3090. [DOI] [PubMed] [Google Scholar]
- 53.Giray D., Epçaçan S. Acute myocarditis following COVID-19 mRNA vaccination: a paediatric case. Cardiol Young. 2022:1–3. doi: 10.1017/S1047951121004698. [DOI] [PubMed] [Google Scholar]
- 54.Goldman R.D. Myocarditis and pericarditis after COVID-19 messenger RNA vaccines. Can Fam Physician. 2022;68(1):17–18. doi: 10.46747/cfp.680117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hasnie A.A., Hasnie U.A., Patel N., Aziz M.U., Xie M., Lloyd S.G., et al. Perimyocarditis following first dose of the mRNA-1273 SARS-CoV-2 (Moderna) vaccine in a healthy young male: a case report. BMC Cardiovasc Disord. 2021;21(1):375. doi: 10.1186/s12872-021-02183-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jani C., Leavitt J., Al Omari O., Dimaso A., Pond K., Gannon S., et al. COVID-19 vaccine-associated takotsubo cardiomyopathy. Am J Ther. 2021;28(3):361–364. doi: 10.1097/MJT.0000000000001379. [DOI] [PubMed] [Google Scholar]
- 57.Khogali F., Abdelrahman R. Unusual presentation of acute perimyocarditis following SARS-COV-2 mRNA-1237 moderna vaccination. Cureus. 2021;13(7):e16590. doi: 10.7759/cureus.16590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.King W.W., Petersen M.R., Matar R.M., Budweg J.B., Cuervo Pardo L., Petersen J.W. Myocarditis following mRNA vaccination against SARS-CoV-2, a case series. Am Heart J Plus. 2021;8 doi: 10.1016/j.ahjo.2021.100042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Levin D., Shimon G., Fadlon-Derai M., Gershovitz L., Shovali A., Sebbag A., et al. Myocarditis following COVID-19 vaccination - a case series. Vaccine. 2021;39(42):6195–6200. doi: 10.1016/j.vaccine.2021.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maki H., Aikawa T., Ibe T., Oyama-Manabe N., Fujita H. Biventricular systolic dysfunction in acute myocarditis after SARS-CoV-2 mRNA-1273 vaccination. Eur Heart J Cardiovasc Imaging. 2022;23(2):e87. doi: 10.1093/ehjci/jeab206. [DOI] [PubMed] [Google Scholar]
- 61.Mevorach D., Anis E., Cedar N., Bromberg M., Haas E.J., Nadir E., et al. Myocarditis after BNT162b2 mRNA Vaccine against COVID-19 in Israel. N Engl J Med. 2021;385(23):2140–2149. doi: 10.1056/NEJMoa2109730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Minocha P.K., Better D., Singh R.K., Hoque T. Recurrence of acute myocarditis temporally associated with receipt of the mRNA coronavirus disease 2019 (COVID-19) vaccine in a male adolescent. J Pediatr. 2021;238:321–323. doi: 10.1016/j.jpeds.2021.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Montgomery J., Ryan M., Engler R., Hoffman D., McClenathan B., Collins L., et al. Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US military. JAMA Cardiol. 2021;6(10):1202–1206. doi: 10.1001/jamacardio.2021.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mungmunpuntipantip R., Wiwanitkit V. Myocarditis following mRNA-based COVID-19 vaccines: correspondence. Cardiology. 2022 doi: 10.1159/000522588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Murakami Y., Shinohara M., Oka Y., Wada R., Noike R., Ohara H., et al. Myocarditis following a COVID-19 messenger RNA vaccination: a Japanese case series. Intern Med. 2022;61(4):501–505. doi: 10.2169/internalmedicine.8731-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nguyen T.D., Mall G., Westphal J.G., Weingärtner O., Möbius-Winkler S., Schulze P.C. Acute myocarditis after COVID-19 vaccination with mRNA-1273 in a patient with former SARS-CoV-2 infection. ESC Heart Fail. 2021;8(6):4710–4714. doi: 10.1002/ehf2.13613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nunn S., Kersten J., Tadic M., Wolf A., Gonska B., Hüll E., et al. Case report: myocarditis after COVID-19 vaccination - case series and literature review. Front Med. 2022;9 doi: 10.3389/fmed.2022.836620. (Lausanne) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Perez Y., Levy E.R., Joshi A.Y., Virk A., Rodriguez-Porcel M., Johnson M., et al. Myocarditis following COVID-19 mRNA vaccine: a case series and incidence rate determination. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rosner C.M., Genovese L., Tehrani B.N., Atkins M., Bakhshi H., Chaudhri S., et al. Myocarditis temporally associated with COVID-19 vaccination. Circulation. 2021;144(6):502–505. doi: 10.1161/CIRCULATIONAHA.121.055891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sadiq W., Waleed M.S., Suen P., Chalhoub M.N. Cardiopulmonary arrest after COVID-19 vaccination: a case report. Cureus. 2022;14(1):e21141. doi: 10.7759/cureus.21141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schauer J., Buddhe S., Colyer J., Sagiv E., Law Y., Mallenahalli Chikkabyrappa S., et al. Myopericarditis after the pfizer messenger ribonucleic acid coronavirus disease vaccine in adolescents. J Pediatr. 2021;238:317–320. doi: 10.1016/j.jpeds.2021.06.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schmitt P., Demoulin R., Poyet R., Capilla E., Rohel G., Pons F., et al. Acute myocarditis after COVID-19 vaccination: a case report. Rev Med Interne. 2021;42(11):797–800. doi: 10.1016/j.revmed.2021.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.See I., Lale A., Marquez P., Streiff M.B., Wheeler A.P., Tepper N.K., et al. Case series of thrombosis with thrombocytopenia syndrome after COVID-19 vaccination-United States. Ann Intern Med. 2021:2022. doi: 10.7326/M21-4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sánchez van Kammen M., Heldner M.R., Brodard J., Scutelnic A., Silvis S., Schroeder V., et al. Frequency of thrombocytopenia and platelet factor 4/heparin antibodies in patients with cerebral venous sinus thrombosis prior to the COVID-19 pandemic. JAMA. 2021;326(4):332–338. doi: 10.1001/jama.2021.9889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Simone A., Herald J., Chen A., Gulati N., Shen A.Y., Lewin B., et al. Acute myocarditis following COVID-19 mRNA vaccination in adults aged 18 years or older. JAMA Intern Med. 2021;181(12):1668–1670. doi: 10.1001/jamainternmed.2021.5511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stewart C., Gamble D.T., Dawson D. Novel case of takotsubo cardiomyopathy following COVID-19 vaccination. BMJ Case Rep. 2022;15(1) doi: 10.1136/bcr-2021-247291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tailor P.D., Feighery A.M., El-Sabawi B., Prasad A. Case report: acute myocarditis following the second dose of mRNA-1273 SARS-CoV-2 vaccine. Eur Heart J Case Rep. 2021;5(8):ytab319. doi: 10.1093/ehjcr/ytab319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Toida R., Uezono S., Komatsu H., Toida T., Imamura A., Fujimoto S., et al. Takotsubo cardiomyopathy after vaccination for coronavirus disease 2019 in a patient on maintenance hemodialysis. CEN Case Rep. 2021:1–5. doi: 10.1007/s13730-021-00657-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Vidula M.K., Ambrose M., Glassberg H., Chokshi N., Chen T., Ferrari V.A., et al. Myocarditis and other cardiovascular complications of the mRNA-based COVID-19 vaccines. Cureus. 2021;13(6):e15576. doi: 10.7759/cureus.15576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Verma A.K., Lavine K.J., Lin C.Y. Myocarditis after COVID-19 mRNA vaccination. N Engl J Med. 2021;385(14):1332–1334. doi: 10.1056/NEJMc2109975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Visclosky T., Theyyunni N., Klekowski N., Bradin S. Myocarditis following mRNA COVID-19 vaccine. Pediatr Emerg Care. 2021;37(11):583–584. doi: 10.1097/PEC.0000000000002557. [DOI] [PubMed] [Google Scholar]
- 82.Viskin D., Topilsky Y., Aviram G., Mann T., Sadon S., Hadad Y., et al. Myocarditis associated with COVID-19 Vaccination: echocardiography, cardiac tomography, and magnetic resonance imaging findings. Circ Cardiovasc Imaging. 2021;14(9) doi: 10.1161/CIRCIMAGING.121.013236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Watkins K., Griffin G., Septaric K., Simon E.L. Myocarditis after BNT162b2 vaccination in a healthy male. Am J Emerg Med. 2021;50:815. doi: 10.1016/j.ajem.2021.06.051. e1-.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yap J., Tham M.Y., Poh J., Toh D., Chan C.L., Lim T.W., et al. Pericarditis and myocarditis after COVID-19 mRNA vaccination in a nationwide setting. Ann Acad Med Singap. 2022;51(2):96–100. [PubMed] [Google Scholar]
- 85.Toida R., Uezono S., Komatsu H., Toida T., Imamura A., Fujimoto S., et al. Takotsubo cardiomyopathy after vaccination for coronavirus disease 2019 in a patient on maintenance hemodialysis. CEN Case Rep. 2022;11(2):220–224. doi: 10.1007/s13730-021-00657-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fearon C., Parwani P., Gow-Lee B., Abramov D. Takotsubo syndrome after receiving the COVID-19 vaccine. J Cardiol Cases. 2021;24(5):223–226. doi: 10.1016/j.jccase.2021.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Abbate A., Gavin J., Madanchi N., Kim C., Shah P.R., Klein K., et al. Fulminant myocarditis and systemic hyperinflammation temporally associated with BNT162b2 mRNA COVID-19 vaccination in two patients. Int J Cardiol. 2021;340:119–121. doi: 10.1016/j.ijcard.2021.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Azdaki N., Farzad M. Long QT interval and syncope after a single dose of COVID-19 vaccination: a case report. Pan Afr Med J. 2021;40:67. doi: 10.11604/pamj.2021.40.67.31546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Azir M., Inman B., Webb J., Mimic T.L. STEMI: focal myocarditis in an adolescent patient after mRNA COVID-19 vaccine. J Emerg Med. 2021;61(6):e129. doi: 10.1016/j.jemermed.2021.09.017. -e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dickey J.B., Albert E., Badr M., Laraja K.M., Sena L.M., Gerson D.S., et al. A series of patients with myocarditis following SARS-CoV-2 vaccination with mRNA-1279 and BNT162b2. JACC Cardiovasc Imaging. 2021;14(9):1862–1863. doi: 10.1016/j.jcmg.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dionne A., Sperotto F., Chamberlain S., Baker A.L., Powell A.J., Prakash A., et al. Association of myocarditis with BNT162b2 messenger RNA COVID-19 vaccine in a case series of children. JAMA Cardiol. 2021;6(12):1446–1450. doi: 10.1001/jamacardio.2021.3471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Flower L., Bares Z., Santiapillai G., Harris S. Acute ST-segment elevation myocardial infarction secondary to vaccine-induced immune thrombosis with thrombocytopaenia (VITT) BMJ Case Rep. 2021;14(9) doi: 10.1136/bcr-2021-245218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hippisley-Cox J., Patone M., Mei X.W., Saatci D., Dixon S., Khunti K., et al. Risk of thrombocytopenia and thromboembolism after COVID-19 vaccination and SARS-CoV-2 positive testing: self-controlled case series study. BMJ. 2021;374:n1931. doi: 10.1136/bmj.n1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hsu M.H., Lee C.P., Huang Y.C. Acute ST-segment elevation myocardial infarction after ChAdOx1 nCoV-19 vaccination in a 33-year-old man. Ann Emerg Med. 2022;79(2):220–221. doi: 10.1016/j.annemergmed.2021.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Istampoulouoglou I., Dimitriou G., Späni S., Christ A., Zimmermanns B., Koechlin S., et al. Myocarditis and pericarditis in association with COVID-19 mRNA-vaccination: cases from a regional pharmacovigilance centre. Glob Cardiol Sci Pract. 2021;2021(3) doi: 10.21542/gcsp.2021.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kounis N.G., Koniari I., Mplani V., Kouni S.N., Plotas P., Tsigkas G. Acute myocardial infarction within 24 H After COVID-19 vaccination: is Kounis syndrome the culprit? Am J Cardiol. 2022;162:207. doi: 10.1016/j.amjcard.2021.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sung J.G., Sobieszczyk P.S., Bhatt D.L. Acute Myocardial infarction within 24 H After COVID-19 vaccination. Am J Cardiol. 2021;156:129–131. doi: 10.1016/j.amjcard.2021.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Larson K.F., Ammirati E., Adler E.D., Cooper L.T., Jr., Hong K.N., Saponara G., et al. Myocarditis after BNT162b2 and mRNA-1273 vaccination. Circulation. 2021;144(6):506–508. doi: 10.1161/CIRCULATIONAHA.121.055913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lazaros G., Anastassopoulou C., Hatziantoniou S., Kalos T., Soulaidopoulos S., Lazarou E., et al. A case series of acute pericarditis following COVID-19 vaccination in the context of recent reports from Europe and the United States. Vaccine. 2021;39(45):6585–6590. doi: 10.1016/j.vaccine.2021.09.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bocchino M., Rea G., Buonocore A., Lieto R., Mazzocca A., Di Domenico A., et al. Combination of acute exacerbation of idiopathic nonspecific interstitial pneumonia and pulmonary embolism after booster anti-COVID-19 vaccination. Respir Med Case Rep. 2022;38 doi: 10.1016/j.rmcr.2022.101674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Elkoumy M., Schoen J., Loew A. Management of a severe bilateral pulmonary embolism as a complication of VITT following vaccination with AstraZeneca COVID-19 vaccine. BMJ Case Rep. 2022;15(5) doi: 10.1136/bcr-2021-246770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Devi K., Ali N., Nasir N., Mahmood S.F. VITT with inactivated SARS-CoV-2 vaccine - index case. Hum Vaccin Immunother. 2022;18(1) doi: 10.1080/21645515.2022.2036556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Alshammari F., Abuzied Y., Korairi A., Alajlan M., Alzomia M., AlSheef M. Bullous pemphigoid after second dose of mRNA- (Pfizer-BioNTech) COVID-19 vaccine: a case report. Ann Med Surg (Lond) 2022;75 doi: 10.1016/j.amsu.2022.103420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kyaw H., Shajahan S., Gulati A., Synn S., Khurana S., Nazar N., et al. COVID-19 mRNA vaccine-associated myocarditis. Cureus. 2022;14(1):e21009. doi: 10.7759/cureus.21009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ghincea A., Ryu C., Herzog E.L. An acute exacerbation of idiopathic pulmonary fibrosis after BNT162b2 mRNA COVID-19 vaccination: a case report. Chest. 2022;161(2):e71. doi: 10.1016/j.chest.2021.07.2160. -e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Curcio R., Gandolfo V., Alcidi R., Giacomino L., Campanella T., Casarola G., et al. Vaccine-induced massive pulmonary embolism and thrombocytopenia following a single dose of Janssen Ad26.COV2.S vaccination. Int J Infect Dis. 2022;116:154–156. doi: 10.1016/j.ijid.2021.12.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Asmat H., Fayeye F., Alshakaty H., Patel J. A rare case of COVID-19 vaccine-induced thrombotic thrombocytopaenia (VITT) involving the veno-splanchnic and pulmonary arterial circulation, from a UK district general hospital. BMJ Case Rep. 2021;14(9) doi: 10.1136/bcr-2021-244223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Türe M., Akın A., Demir M., Akay C. A paediatric case of myopericarditis post-COVID-19 mRNA vaccine. Cardiol Young. 2022:1–4. doi: 10.1017/S1047951122000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Das B.B., Kohli U., Ramachandran P., Nguyen H.H., Greil G., Hussain T., et al. Myopericarditis after messenger RNA Coronavirus Disease 2019 Vaccination in Adolescents 12 to 18 Years of Age. J Pediatr. 2021;238:26–32. doi: 10.1016/j.jpeds.2021.07.044. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Koizumi T., Awaya T., Yoshioka K., Kitano S., Hayama H., Amemiya K., et al. Myocarditis after COVID-19 mRNA vaccines. QJM. 2021;114(10):741–743. doi: 10.1093/qjmed/hcab244. [DOI] [PubMed] [Google Scholar]
- 111.Hassanzadeh S., Sadeghi S., Mirdamadi A., Nematollahi A. Myocarditis following AstraZeneca (an adenovirus vector vaccine) COVID-19 vaccination: a case report. Clin Case Rep. 2022;10(4):e05744. doi: 10.1002/ccr3.5744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sulemankhil I., Abdelrahman M., Negi S.I. Temporal association between the COVID-19 Ad26.COV2.S vaccine and acute myocarditis: a case report and literature review. Cardiovasc Revasc Med. 2022;38:117–123. doi: 10.1016/j.carrev.2021.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Alizadehasl A., Soleimani A., Peighambari M., Mostafavi A. Biventricular apical ballooning in patient with COVID-19. J Echocardiogr. 2021 doi: 10.1007/s12574-021-00530-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Greinacher A., Selleng K., Palankar R., Wesche J., Handtke S., Wolff M., et al. Insights in ChAdOx1 nCoV-19 vaccine-induced immune thrombotic thrombocytopenia. Blood. 2021;138(22):2256–2268. doi: 10.1182/blood.2021013231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Greinacher A., Thiele T., Warkentin T.E., Weisser K., Kyrle P., Eichinger S. A prothrombotic thrombocytopenic disorder resembling heparin-induced thrombocytopenia following coronavirus-19 vaccination. 2021.
- 116.Baronti A., Gentile F., Manetti A.C., Scatena A., Pellegrini S., Pucci A., et al. Myocardial infarction following COVID-19 vaccine administration: post hoc, ergo propter hoc? Viruses. 2022;14(8) doi: 10.3390/v14081644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Aye Y.N., Mai A.S., Zhang A., Lim O.Z.H., Lin N., Ng C.H., et al. Acute myocardial infarction and myocarditis following COVID-19 vaccination. QJM. 2021 doi: 10.1093/qjmed/hcab252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Grady K.L., Costanzo-Nordin M.R. Myocarditis: review of a clinical enigma. Heart Lung. 1989;18(4):347–353. [PubMed] [Google Scholar]
- 119.LeWinter M.M. Clinical practice. Acute pericarditis. N Engl J Med. 2014;371(25):2410–2416. doi: 10.1056/NEJMcp1404070. [DOI] [PubMed] [Google Scholar]
- 120.Khan Z., Pabani U.K., Gul A., Muhammad S.A., Yousif Y., Abumedian M., et al. COVID-19 vaccine-induced myocarditis: a systemic review and literature search. Cureus. 2022;14(7):e27408. doi: 10.7759/cureus.27408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lota A.S., Halliday B., Tayal U., Salmi S., Shakur R., Hammersley D., et al. Epidemiological trends and outcomes of acute myocarditis in the national health service of England. Circulation. 2019;140(Suppl_1):A11463. -A. [Google Scholar]
- 122.In brief Myocarditis with the Pfizer/BioNTech and moderna COVID-19 vaccines. Med Lett Drugs Ther. 2021;63(1629):e9. [PubMed] [Google Scholar]
- 123.Diaz G.A., Parsons G.T., Gering S.K., Meier A.R., Hutchinson I.V., Robicsek A. Myocarditis and pericarditis after vaccination for COVID-19. JAMA. 2021;326(12):1210–1212. doi: 10.1001/jama.2021.13443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fazlollahi A., Zahmatyar M., Noori M., Nejadghaderi S.A., Sullman M.J.M., Shekarriz-Foumani R., et al. Cardiac complications following mRNA COVID-19 vaccines: a systematic review of case reports and case series. Rev Med Virol. 2022;32(4):e2318. doi: 10.1002/rmv.2318. [DOI] [PubMed] [Google Scholar]
- 125.Ling R.R., Ramanathan K., Tan F.L., Tai B.C., Somani J., Fisher D., et al. Myopericarditis following COVID-19 vaccination and non-COVID-19 vaccination: a systematic review and meta-analysis. Lancet Respir Med. 2022;10(7):679–688. doi: 10.1016/S2213-2600(22)00059-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Saeed B.Q., Al-Shahrabi R., Alhaj S.S., Alkokhardi Z.M., Adrees A.O. Side effects and perceptions following Sinopharm COVID-19 vaccination. Int J Infect Dis. 2021;111:219–226. doi: 10.1016/j.ijid.2021.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Xia S., Zhang Y., Wang Y., Wang H., Yang Y., Gao G.F., et al. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBIBP-CorV: a randomised, double-blind, placebo-controlled, phase 1/2 trial. Lancet Infect Dis. 2021;21(1):39–51. doi: 10.1016/S1473-3099(20)30831-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Li M., Yuan J., Lv G., Brown J., Jiang X., Lu Z.K. Myocarditis and pericarditis following COVID-19 vaccination: inequalities in age and vaccine types. J Pers Med. 2021;11(11) doi: 10.3390/jpm11111106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Milano G., Gal J., Creisson A., Chamorey E. Myocarditis and COVID-19 mRNA vaccines: a mechanistic hypothesis involving dsRNA. Future Virol. 2021 doi: 10.2217/fvl-2021-0280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Pardi N., Hogan M.J. Weissman D. Recent advances in mRNA vaccine technology. Curr Opin Immunol. 2020;65:14–20. doi: 10.1016/j.coi.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 131.Sinagra G., Merlo M., Porcari A. Exploring the possible link between myocarditis and mRNA COVID-19 vaccines. Eur J Intern Med. 2021;92:28–30. doi: 10.1016/j.ejim.2021.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Haaf P., Kuster G.M., Mueller C., Berger C.T., Monney P., Burger P., et al. The very low risk of myocarditis and pericarditis after mRNA COVID-19 vaccination should not discourage vaccination. Swiss Med Wkly. 2021;151:w30087. doi: 10.4414/smw.2021.w30087. [DOI] [PubMed] [Google Scholar]
- 133.Singh T., Khan H., Gamble D.T., Scally C., Newby D.E., Dawson D. Takotsubo syndrome: pathophysiology, emerging concepts, and clinical implications. Circulation. 2022;145(13):1002–1019. doi: 10.1161/CIRCULATIONAHA.121.055854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ahmed S., Mohamed M., Essa R., Dabou E., Abdulqadir S., Muhammad Omar R. Global reports of takotsubo (stress) cardiomyopathy following COVID-19 vaccination: a systematic review and meta-analysis. IJC Heart Vasc. 2022;43 doi: 10.1016/j.ijcha.2022.101108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wittstein I.S. The sympathetic nervous system in the pathogenesis of takotsubo syndrome. Heart Fail Clin. 2016;12(4):485–498. doi: 10.1016/j.hfc.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 136.Jeet Kaur R., Dutta S., Charan J., Bhardwaj P., Tandon A., Yadav D., et al. Cardiovascular adverse events reported from COVID-19 Vaccines: a study based on WHO database. Int J Gen Med. 2021;14:3909–3927. doi: 10.2147/IJGM.S324349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Boivin Z., Martin J. Untimely myocardial infarction or COVID-19 vaccine side effect. Cureus. 2021;13(3) doi: 10.7759/cureus.13651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kounis N.G., Mazarakis A., Tsigkas G., Giannopoulos S., Goudevenos J. Kounis syndrome: a new twist on an old disease. Future Cardiol. 2011;7(6):805–824. doi: 10.2217/fca.11.63. [DOI] [PubMed] [Google Scholar]
- 139.Kounis N.G., Koniari I., de Gregorio C., Velissaris D., Petalas K., Brinia A., et al. Allergic reactions to current available COVID-19 vaccinations: pathophysiology, causality, and therapeutic considerations. Vaccines. 2021;9(3):221. doi: 10.3390/vaccines9030221. (Basel) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Greinacher A., Thiele T., Warkentin T.E., Weisser K., Kyrle P.A., Eichinger S. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med. 2021;384(22):2092–2101. doi: 10.1056/NEJMoa2104840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Huynh A., Kelton J.G., Arnold D.M., Daka M., Nazy I. Antibody epitopes in vaccine-induced immune thrombotic thrombocytopaenia. Nature. 2021;596(7873):565–569. doi: 10.1038/s41586-021-03744-4. [DOI] [PubMed] [Google Scholar]
- 142.Baker A.T., Boyd R.J., Sarkar D., Teijeira-Crespo A., Chan C.K., Bates E., et al. ChAdOx1 interacts with CAR and PF4 with implications for thrombosis with thrombocytopenia syndrome. Sci Adv. 2021;7(49):eabl8213. doi: 10.1126/sciadv.abl8213. [DOI] [PMC free article] [PubMed] [Google Scholar]