Abstract
Developmental theories suggest affect-biased attention, preferential attention to emotionally salient stimuli, emerges during infancy through coordinating individual differences. Here we examined bidirectional relations between infant affect-biased attention, temperamental negative affect, and maternal anxiety symptoms using a Random Intercepts Cross-Lagged Panel Model (RI-CLPM). Infant-mother pairs from Central Pennsylvania and Northern New Jersey (N = 342; 52% White; 50% reported as assigned female at birth) participated when infants were 4, 8, 12, 18 and 24 months of age. Infants completed the overlap task while eye-tracking data were collected. Mothers reported their infant’s negative affect and their own anxiety symptoms. In an RI-CLPM, after accounting for between-person variance (random intercepts representing the latent average of a construct), it is possible to assess within-person variance (individual deviations from the latent average of a construct). Positive relations represent stability in constructs (smaller within-person deviations). Negative relations represent fluctuation in constructs (larger within-person deviations). At the between-person level (random intercepts), mothers with greater anxiety symptoms had infants with greater affect-biased attention. However, at the within-person level (deviations), greater fluctuation in maternal anxiety symptoms at 12- and 18-months prospectively related to greater stability in attention to angry facial configurations. Additionally, greater fluctuation in maternal anxiety symptoms at 18-months prospectively related to greater stability in attention to happy facial configurations. Finally, greater fluctuation in maternal anxiety symptoms at 4- and 12-months prospectively related to greater stability in infant negative affect. These results suggest that environmental uncertainty, linked to fluctuating maternal anxiety, may shape early socioemotional development.
Keywords: maternal anxiety, affect-biased attention, infancy, longitudinal
Affect-biased attention, commonly measured using emotional facial configurations, is an automatic process that prioritizes stimuli that are emotionally or motivationally salient to an individual (Todd et al., 2012). Although researchers often study affect-biased attention as static, there is reason to believe that affect-biased attention reflects a dynamic developmental process that may underlie how individuals come to experience and understand their environment (Field & Lester, 2010; Morales et al., 2016). Prior work links patterns of affect-biased attention to socioemotional profiles. In particular, affect-biased attention patterns focused on threat may become entrenched or inflexible over time, contributing to anxiety risk (Bar-Haim et al., 2007). Here, we leverage a large-scale longitudinal study to examine potential bidirectional relations between affect-biased attention, infant negative affect, and maternal anxiety symptoms across the first two years of life.
Across the lifespan, there is normative variation in which socioemotional stimuli draw attention (Todd et al., 2012). Infants may go through a period of time, beginning around 7-months, when threatening stimuli are particularly salient (Peltola et al., 2008), potentially marking an evolutionary drive to detect threat in the environment (LoBue & DeLoache, 2010). Recent work suggests this peak in affect-biased attention to indirect signals of threat, like fearful facial configurations, may dissipate by the time infants turn two (Peltola et al., 2018). In contrast, biased attention to direct signals of threat, such as angry facial configurations, may only just emerge between 18 and 24 months (Leppänen et al., 2018; Reider et al., in press; Xie et al., 2021). Affect-biased attention to direct threats, as measured by attention to angry facial configurations, is related to anxiety in children and adults (Bar-Haim et al., 2007). Examining the affect-biased attention during infancy can provide valuable insight into a developmental process that may precede particular socioemotional outcomes, including social withdrawal and anxiety risk.
Field and Lester (2010) proposed three potential models for the development of affect-biased attention to threat: the integral bias, the moderation and the acquisition models. In the integral bias model, some individuals are born with an attention bias to threat that is stable across the lifespan. In the moderation model, all individuals are born with an attention bias to threat, but individual differences, such as temperament, influence which individuals continue to show this bias across the lifespan. Finally, in the acquisition model, stable patterns of attention bias to threat are not evident in early life. Rather, individual differences and experience shape the extent to which an attention bias to threat develops over time. In each case, the continued presence of an attention bias to threat, whether inherent, maintained, or acquired, is thought to be associated with anxiety risk.
Cross-sectional research provides conflicting results regarding relations between affect-biased attention to threat and individual differences during the first years of life (Fu et al., 2020; Morales, Brown, et al., 2017; Pérez-Edgar et al., 2017). Research with children and infants suggests that rigid patterns of attention, rather than a specific bias towards threat, may be more informative for understanding attention-anxiety relations (Morales, Taber-Thomas, et al., 2017; Vallorani et al., 2021). Rigid patterns of attention, regardless of the target of attention, may reduce an infant or child’s ability to flexibly respond to their environment and, over time, may set the foundation for developmental trajectories towards anxiety. Thus, to understand the development of affect-biased attention during infancy, it is important to take an approach that is longitudinal, investigates attention to both threatening and non-threatening stimuli, and allows for the assessment of how individual difference factors, including infant temperamental negative affect and maternal anxiety, may influence the stability of attention patterns.
One particularly strong predictor of later anxiety is fearful temperament, which is characterized by hypervigilance and withdrawal from social and novel environments (Pérez-Edgar & Fox, 2005). Theoretical perspectives on attention suggest that more rigid attention patterns are related to elevated anxiety in the context of fearful temperament, (Henderson & Wilson, 2017), potentially due to difficulty flexibly responding to social environments. Although this perspective examines higher-order attentional control, functional precursors may be developing early in life. Indeed, the orienting network, evident in the first months of life (Petersen & Posner, 2012), is associated with rapid attentional processes that can regulate emotion (Todd et al., 2012). Early attentional patterns developed through the orienting network to regulate emotion may feed into the emergence of more stable executive network functioning and emotion regulation at 3- and 4-years of age (Rothbart et al., 2011). Thus, attentional patterns acquired during infancy may influence downstream processes that crystallize stability in attention and environmental responding, which at the extremes could constitute rigidity in approach and response.
Infant temperamental negative affect, characterized by elevated levels of distress, anger and sadness, can be measured as early as 4-months and is related to later-emerging fearful temperament (Fox et al., 2015). Variation in negative affect is also associated with early developing patterns of biased attention. For example, younger infants low in negative affect who spend more time dwelling to angry facial configurations are faster to disengage from angry facial configurations to then fixate on novel cues (Pérez-Edgar et al., 2017). Additionally, older infants high in both negative affect and attentional control are faster to orient to neutral versus emotional facial configurations in a vigilance task (Fu et al., 2020). In previous work, negative affect was not associated with affect-biased attention when examining engagement with facial configurations (Morales, Taber-Thomas, et al., 2017; Vallorani et al., 2021), but did interact with maternal anxiety (Vallorani et al., 2021), such that infants higher in negative affect who also had mothers higher in anxiety were more likely to exhibit elevated affect-biased attention. Thus, negative affect may function as a relatively stable individual difference factor that underlies rigidity in how infants filter, process and react to socioemotional stimuli in their environment.
Maternal anxiety, conversely, may shape an infant’s environmental experience, especially for infants with extreme temperaments who may be especially sensitive to environmental input from parents (Slagt et al., 2016). Parental expressions of anxiety are related to infant avoidance of novel stimuli (Aktar et al., 2013). Anxious parents may signal to infants that an environment is unsafe even in contexts that are relatively safe (Kalomiris & Kiel, 2016), potentially increasing wariness in infants when wariness is unwarranted. Elevated wariness could elicit hypervigilance, triggering a cycle leading to stable patterns of affect-biased attention. Indeed, new evidence suggests infants and parents exhibit similar patterns of affect-biased attention (Aktar et al., 2022).
The available data on the relation between maternal anxiety and infant affect-biased attention is mixed. Postnatal maternal anxiety is associated with less disengagement from fearful facial configurations in 8-month-old boys, and less disengagement from emotional facial configurations more generally in 8-month-old girls (Kataja et al., 2019). Additionally, previous cross-sectional research found that infants (4- to 24-months) of mothers with higher anxiety symptoms exhibited less disengagement from angry facial configurations (Morales, Brown, et al., 2017). However, maternal anxiety symptoms were related to more disengagement from emotional facial configurations when considering both threatening and non-threatening facial configurations simultaneously (Vallorani et al., 2021). Longitudinal assessments of both parents and children in relation to anxiety and affect-biased attention are limited. Parental anxiety prospectively, but not concurrently, relates to children’s attention to threat (Aktar et al., 2019). Research assessing child affect-biased attention and parental anxiety simultaneously at multiple assessments is needed to parse between-person and within-person variability that might explain the role of parental anxiety in child affect-biased attention development (Field & Lester, 2010; Morales et al., 2016).
The classic overlap task (Peltola et al., 2008) is commonly employed to assess infant affect-biased attention. The task presents (Figure 1), a single face in the center of the screen alone for 1000 ms, at which point a checkerboard appears in the left or right visual field. The face and checkerboard are presented simultaneously for 3000 ms. Researchers have used both latency to orient to the checkerboard (Kataja et al., 2019; Peltola et al., 2008) and dwell to the face in the presence of the checkerboard as their main dependent measures (Morales, Brown, et al., 2017; Vallorani et al., 2021). Dwell to the face, measured by both fixations and saccades within the area of a given facial stimulus, in the presence of the checkerboard captures engagement with the face (Vallorani et al., 2021) and may be particularly developmentally sensitive in young infants, as infants 4-months and younger have difficulty rapidly shifting gaze between stimuli (Hunnius & Geuze, 2004). By creating bias or residual scores between neutral and emotional facial configurations in the presence of the checkerboard, it is then possible to assess affect-biased attention in a developmentally sensitive way.
Figure 1.
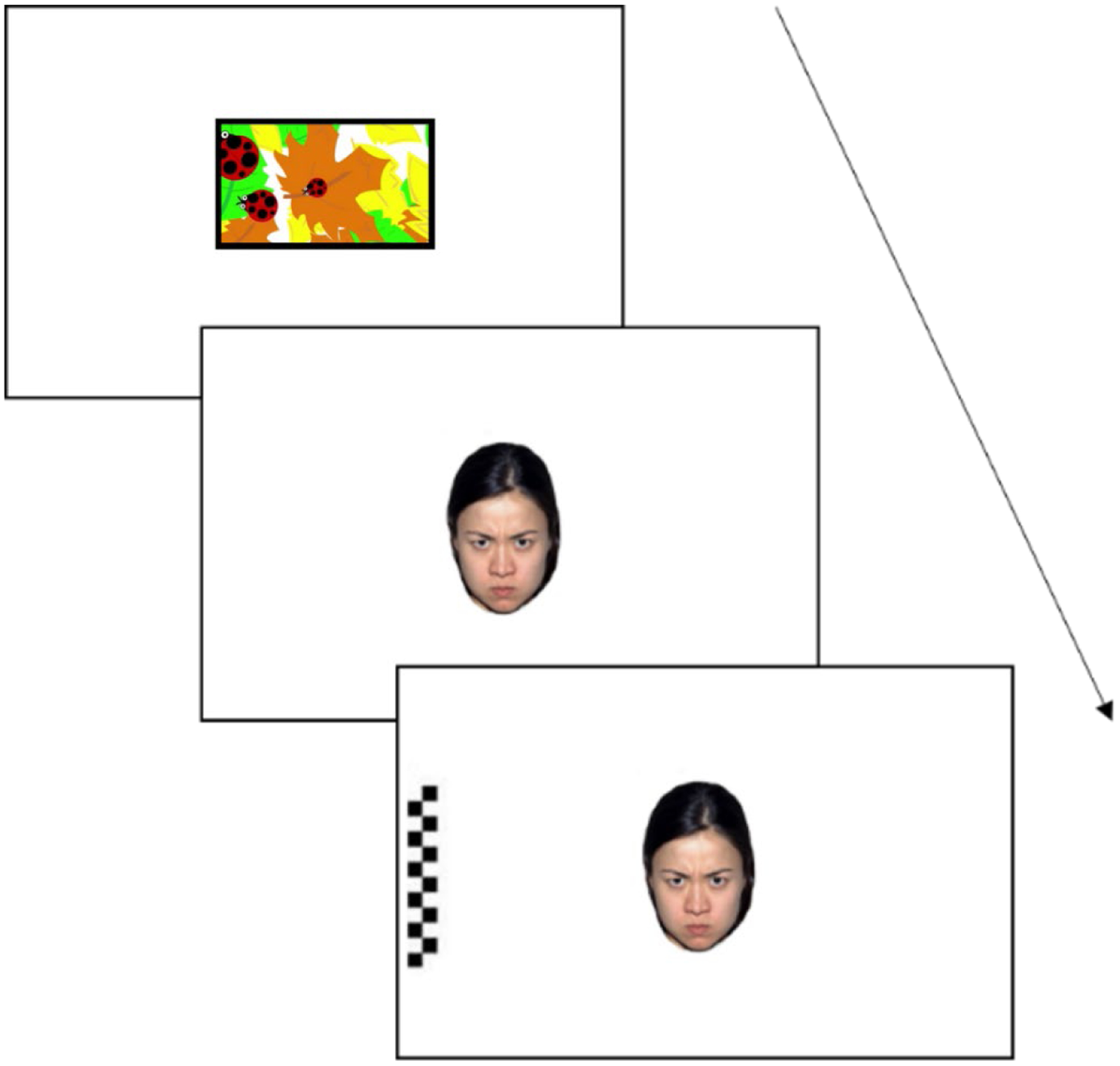
Overlap task. Images drawn from NimStim face set (Tottenham et al., 2009), approved for publication and not of the authors. Initial fixation presented for 1000ms. Central face present alone for 1000ms. Central face presented with peripheral checkerboard for 3000ms.
Developmental theory (Lerner et al., 2015) highlights the importance of studying developmental processes as complex systems of drives that bidirectionally influence the course of development and affect-biased attention too may develop through the bidirectional coordination of multiple cognitive and socioemotional processes (Morales et al., 2016). Evidence of bidirectional influences between parents and children in attention biases, temperament and anxiety is still emerging. However, research does suggest that maternal anxiety and infant negative affect are mutually reinforcing (Brooker et al., 2015). Given known relations between maternal anxiety and infant attention biases (Morales, Brown, et al., 2017) and infant negative affect and infant affect-biased attention (Fu et al., 2020; Pérez-Edgar et al., 2017), a mutually reinforcing process between infant negative affect and maternal anxiety could potentiate infant affect-biased attention. Indeed, infants higher in negative affect with anxious mothers may show elevated levels of affect-biased attention across emotional facial configurations (Vallorani et al., 2021). The effects of infant affect-biased attention on parent anxiety, however, remains an open question.
Here we examined potential bidirectional relations between infant affect-biased attention, infant negative affect and maternal anxiety symptoms in a diverse sample of infants and mothers drawn from a multi-site, longitudinal study (Pérez-Edgar et al., 2021). We employed a random intercepts cross-lagged panel model (RI-CLPM) which is useful for separating between-person variation (random intercepts) from within-person variation (relations between individual constructs) when assessing bidirectional relations (Hamaker et al., 2015). After accounting for an individual’s latent average on a construct (random intercepts), we can examine if within-person deviations from the latent average are related across constructs. Within-person deviations can either exhibit stability (smaller within-person deviations from the latent average) or fluctuation (larger within-person deviations from the latent average). Positive relations amongst individual constructs represent lower within-person deviations on one construct (stability) relating to lower within-person deviations on a second construct (stability). Negative relations amongst individual constructs represent higher within-person deviations on one construct (fluctuation) relating to lower within-person deviations on a second construct (stability). As with correlations amongst between-subjects variables, the reverse is also true. That is, positive relations also represent higher within-person deviations on one construct relating to higher within-person deviations on a second construct and negative relations also represent lower within-person deviations on one construct relating to higher within-person deviations on a second construct. By including cross-lagged regressions we are able to describe how 1) constructs prospectively relate to each other and 2) mothers and infants may bidirectionally relate to each other.
We specifically anticipated the data would not support the integral bias model based on a wealth of previous research linking affect-biased attention with individual differences (Bar-Haim et al., 2007; Fu et al., 2020; Morales, Brown, et al., 2017; Pérez-Edgar et al., 2017; Vallorani et al., 2021). Although theoretically we are inclined to believe the acquisition model is the most likely candidate to explain affect-biased attention development, the current study cannot definitively differentiate between the acquisition and moderation models given the theoretical models anticipate divergences beginning at birth. Thus, we hypothesized, consistent with the acquisition and moderation models, that within-person deviations in maternal anxiety symptoms would relate to within-person deviations in infant affect-biased attention to threat. In particular, our model allowed us to assess how maternal anxiety symptoms related to stability in infant affect-biased attention to angry facial configurations. Positive relations would suggest mothers exhibiting stable levels of anxiety symptoms have infants who exhibit stable affect-biased attention, whereas negative relations would suggest mothers exhibiting fluctuating levels of anxiety symptoms have infants who exhibit stable affect-biased attention. We did not make a-prior hypotheses about directionality as these data are the first to examine longitudinal cross-lagged relations between maternal anxiety symptoms and infant affect-biased attention. Previous results in cross-sectional data, or studies where only the infant or maternal metrics were longitudinal, do not provide clear expectations for how maternal anxiety and infant affect-biased attention may interact over time. Thus, these analyses provide an important step in answering this question.
In keeping with previous research showing bidirectional relations between maternal anxiety and infant negative affect (Brooker et al., 2015), we anticipated that infant negative affect and maternal anxiety symptoms may bidirectionally relate to each other. Additionally, we anticipated that these bidirectional relations would relate to stability in infant affect-biased attention to angry facial configurations, in keeping with previous work (Vallorani et al., 2021). As a probe for affective specificity, we also examined patterns of affect-biased attention to happy facial configurations.
The current analyses expand on the results observed in Vallorani et al. (2021), which examined relations between infant affect-biased attention, maternal anxiety symptoms and infant negative affect in infants between 4 and 24 months of age. Importantly, data analyzed in Vallorani et al. (2021) were cross-sectional and the focus of the research was to understand differences in variable-centered and person-centered approaches to measure affect-biased attention development. The current paper takes a variable-centered approach in a longitudinal sample of infants from the ages of 4- to 24-months to examine relations between infant affect-biased attention, maternal anxiety symptoms and infant negative affect over time. In contrast to Vallorani et al. (2021), which employed eye-tracking metrics from three affect-biased attention tasks (dot-probe, overlap and vigilance), here we focus on the overlap task. By focusing on a single affect-biased attention task and taking a variable-centered approach, we center our analytical power on observing how both between- and within-person relations in both infants and mothers may bidirectionally influence affect-biased attention development over time.
Further, the current analyses expand on the affect-biased attention literature more generally focusing on the stability versus fluctuation of attention biases over time rather than on the magnitude of a given attention bias, or biases, as is more typical (Kataja et al., 2019; Morales, Brown, et al., 2017; Peltola et al., 2008; Vallorani et al., 2021). Thus, our analyses can expand our understanding of how individual differences (Field & Lester, 2010) and bidirectional influences (Morales et al., 2016) may impact patterns of affect-biased attention (Morales, Taber-Thomas, et al., 2017; Vallorani et al., 2021) over the first two years of life.
Method
Overview
The current study was part of a larger study (N = 357) examining the development of attention and temperament across the first two years of life (Pérez-Edgar et al., 2021). A community sample was selected to ensure that a spectrum of observed behaviors, and variation in behaviors across time, was assessed to best characterize possible early risk for anxiety. Participants were recruited via mailings sent to parents identified using a university-based database of families interested in research and community advertisements. For the current project, infants provided stationary eye-tracking data during laboratory visits at 4-, 8-, 12-, 18- and 24-months. Mothers reported their own anxiety symptoms as well as their infant’s negative affect at each assessment. Parents provided informed consent for both their own and their infant’s participation. Families were compensated for their participation. Procedures were approved by the Pennsylvania State University and Rutger’s University Institutional Review Boards. Data are accessible through Databrary (LoBue et al., 2021) for those participants who consented to data sharing.
Participants
The final sample for the current analyses consisted of 342 infants (50% reported as assigned female at birth) and their mothers (see S1 for information on exclusions). Mother-infant pairs each provided some usable data on the measures of interest and a-priori power analyses indicated our sample size was sufficient for our planned analyses (S2). Table 1 displays ages and demographics for the sample.
Table 1.
Demographic information
| Infant Ages | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 4-Month Assessment |
8-Month Assessment |
12-Month Assessment |
18-Month Assessment |
24-Month Assessment |
||||||
| M | SD | M | SD | M | SD | M | SD | M SD | SD | |
| Age Eye-Tracking Visit Completed | 4.49 | 0.47 | 8.20 | 0.54 | 12.16 | 0.46 | 18.18 | 0.52 | 24.14 | 0.46 |
| Age Questionnaires Completed | 4.43 | 0.66 | 8.10 | 0.72 | 12.19 | 0.67 | 18.08 | 0.73 | 23.99 | 0.65 |
| Infant Race/Ethnicity | |||||
|---|---|---|---|---|---|
| White | Hispanic | Black | Multiracial | Asian | Not Reported |
| 177 (52%) | 73 (21%) | 52 (15%) | 27 (8%) | 9 (3%) | 4 (1%) |
| Parent Education | ||||||||
|---|---|---|---|---|---|---|---|---|
| Grade School | High School | High School Degree | College/Technical School | College Degree | Graduate School | Graduate Degree | Not Reported | |
| Mother’s Education | 10 (3%) | 17 (5%) | 36 (11%) | 56 (16%) | 73 (21%) | 57 (17%) | 65 (19%) | 28 (8%) |
| Father’s Education | 10 (3%) | 15 (4%) | 50 (15%) | 59 (17%) | 69 (20%) | 42 (12%) | 55 (16%) | 42 (12%) |
| Family Income | ||
|---|---|---|
| Below Recruitment Area Median Income | Above Recruitment Area Median Income | Not Reported |
| 91 (27%) | 203 (59%) | 48 (14%) |
Data collection began at 4-months as this is a classic time point for first assessing temperament, reflecting the first emergence of stable daily patterns of activity and affect (Fox et al., 2015). From there, we chose 4 month increments in the first year of life due to the very rapid development of multiple socioemotional and attentional processes across those first 12 months. We extended to 6 month increments in the second year of life as the speed of developmental change decreases some in the second year meaning we could lessen the data collection burden on our families by requiring fewer assessments while still adequately capturing developmental change in our processes of interest.
Although recent evidence suggests attention to direct threats are later emerging (Reider et al., in press; Xie et al., 2021) and may not be specific to maternal symptoms of depression or anxiety (Leppänen et al., 2018), those data have been assessed cross-sectionally or without consideration for individual differences. To thoroughly test theories of affect-biased attention development (Field & Lester, 2010; Morales et al., 2016), it was important to employ a longitudinal design from the earliest ages that repeatedly assessed both mothers and infants.
Measures
Overlap Task.
Infants completed a version of the classic overlap task (Morales, Brown, et al., 2017; Peltola et al., 2008) to assess attention to emotional facial configurations. Infants are first presented with a facial configuration in the center of the screen for 1000ms. A checkerboard then appears in either the left or right periphery of the screen while the facial configuration remains present for 3000ms. Eye tracking data were collected across sites using SMI eye tracking systems, either the SMI RED or REDm system, both offering comparable specifications/capabilities (SensoMotoric Instruments, Teltow, Germany). Participants were seated ~60cm from a 22” Dell monitor for stimulus presentation, in a high-chair. If needed, infants could also sit on their parent’s lap or on the lap of an experimenter. Gaze was calibrated using a 5-point calibration followed by a 4-point validation, using an animated flower on a black screen and infant-friendly music. Gaze data were sampled at 60 Hz and collected by Experiment Center (SensoMotoric Instruments, Teltow, Germany). Infants/toddlers were calibrated below of 4° of visual angle from all calibration points.
Infants were presented with up to 30 experimental trials (fewer when the infant could no longer attend to the task). Each trial was initiated when the infant’s attention was on a video clip presented centrally on the screen, which was triggered either when the infant fixated for at least 100ms or when the experimenter determined that the infant was looking at the video clip. If the participant did not attend to the center of the screen, the slide advanced after 10000ms. A facial configuration sampled from the NimStim facial configuration set (10 actors/5 male; providing neutral, happy and angry closed mouth images; Tottenham et al., 2009) was presented in the center of the screen for 1000ms. Facial configuration stimuli were approximately 12 cm × 8cm and the visual angle of each facial configuration was 11.42° × 7.63°. Following the presentation of the facial configuration, a checkerboard stimulus then appeared in either the left or right periphery of the screen adjacent to the facial configuration (20.78° visual angle) for 3000ms. The checkerboard was 12 cm × 2.5cm, 11.42° × 2.39° visual angle. This progression of stimuli was concluded with a 1000ms ITI (blank screen). No consecutive trials were identical in terms of facial configuration and checkerboard placement.
Areas of interest (AOIs) were drawn as ellipses enclosing the facial configuration and rectangles enclosing the checkerboards. A 2cm “error margin” was added to each AOI, to account for the deviation permitted in the calibration procedure (max 4°). Analyses were based on gaze to these designated AOIs. Fixations, defined as gaze maintained for at least 80ms within a 100-pixel maximum dispersion, were extracted with BeGaze (SensoMotoric Instruments, Teltow, Germany). Distribution of valid trials by assessment is reported in Table S1. We computed dwell to the central facial configuration while the checkerboard stimulus (probe) was present (Morales, Brown, et al., 2017) for all facial configurations (angry, happy and neutral) using in-house R scripts. For base processing, dwell was defined as the duration of fixations as well as saccades within the designated AOI. Dwells were scaled from milliseconds to seconds. Figure 2 displays correlations between raw dwells at each assessment.
Figure 2.
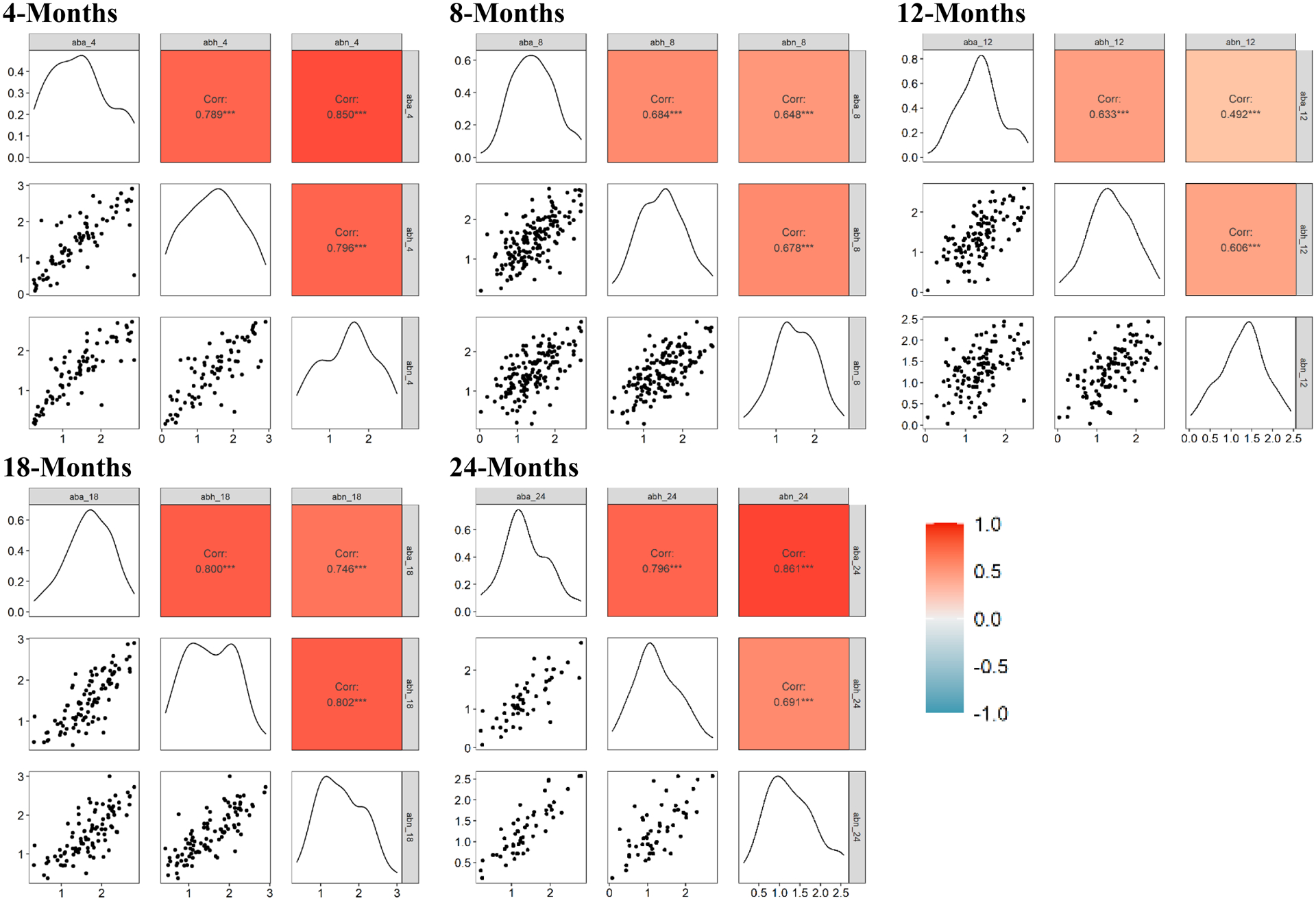
Relations between dwell to angry (aba), happy (abh) and neutral (abn) facial configurations in the presence of the probe. At all assessments, attention to all facial configurations was highly correlated.
We then computed residual scores by regressing angry and happy facial configurations, respectively, on neutral facial configurations to obtain separate scores of affect-biased attention. Although difference scores are commonly used in the literature, residual scores have greater reliability (Meyer et al., 2017). Fearful facial configurations are common stimuli in the overlap task, particularly in infants (Peltola et al., 2008). We focused here on angry facial configurations due to the much larger literature surrounding relations between attention to angry facial configurations and anxiety (Bar-Haim et al., 2007) as well as the literature highlighting angry facial configurations as a marker of direct threat (Leppänen & Nelson, 2012).
Infant Negative Affect.
The Infant Behavior Questionnaire—Revised (IBQ-R) is a 191-item survey designed to assess general patterns of behavior associated with temperament in infancy from 3–12 months (Parade & Leerkes, 2008). Parents rated how often they observed a behavior in the past week at the 4-, 8-, and 12-month assessments. Each item describes an infant behavior (e.g., During feeding, how often did the baby lie or sit quietly?) using a 7-point scale (never to always). Parents are also given a “not applicable” response option for use when the infant has not been observed in the situation described. Each item loads onto one of 14 subscales. Items from each subscale are averaged to obtain scale scores. Each scale, in turn, loads onto one of three broader factors (Surgency, Negativity, Orienting/Regulation).
The Toddler Behavior Assessment Questionnaire (TBAQ) is a 120-item survey designed to assess general patterns of behavior associated with temperament in young children from 2–3 years (Goldsmith, 1996). It was collected at the 18- and 24-month assessments. Parents rated how often their toddler displayed a specific behavior in the past month using a 7-point Likert scale (never to always). Each item loads onto one of 11 subscales. Items from each subscale are averaged to obtain scale scores. Goldsmith (1996) reported high levels of convergence with various subscales of the IBQ.
For the current analyses, we used the Negativity factor from the IBQ, composed of the Sadness, Distress to Limitations, Fear, and Falling Reactivity subscales, at 4-, 8- and 12-months (αs ≥ .82). We also created a Negativity composite from the TBAQ, composed of the Anger, Sadness, Social Fear, and Object Fear subscales, at 18- and 24-months (αs ≥ .85). To examine infant negative affect as a continuous construct over time, we standardized our Negativity factors from both the IBQ and TBAQ prior to inclusion in our models.
Maternal Anxiety.
The Beck Anxiety Inventory (BAI), collected at all assessments, is a 21-item self-report questionnaire for evaluating the severity of anxiety in healthy and psychiatric populations (Beck et al., 1988). The BAI was specifically designed to distinguish cognitive and somatic symptoms of anxiety from symptoms of depression. Parents rated individual symptoms of anxiety (e.g., fear of losing control) in the past month using a four-point Likert scale (not at all to severely). The BAI is scored by adding the highest ratings for all 21 items, for a score range from 0 to 63. Higher scores indicate greater symptom severity. Internal reliability was good (αs ≥ .89). Prior to inclusion in the model, maternal anxiety was divided by 10 and scaled.
Data Analysis
The primary aim of the current analysis was to assess potential bidirectional relations between infant affect-biased attention to threat, infant negative affect and maternal anxiety symptoms in the context of proposed models of affect-biased attention development (Field & Lester, 2010; Morales et al., 2016). To do so, we fit our data to a random intercepts cross-lagged panel model (RI-CLPM; see Databrary for analysis code).
Data were modeled in lavaan (Rosseel, 2012) using R 4.0.3 (R Core Team, 2020) with parameters estimated and missing data handled using maximum likelihood estimation (see S3, S4 and S5 for additional information). As described in S5, data were systematically missing as a function of data collection site, indicating the data were likely missing at random (Lodder, 2013). Thus, we included site as a covariate on the random intercepts in our model. Random intercept loadings were fixed at 1.00 and regressions and covariations were freely estimated. Model fit was assessed using CFI, RMSEA and SRMR (Kenny, 2020). We included affect-biased attention to angry and happy facial configurations (residual scores) to assess the specificity of threat (angry facial configurations). Due to the high correlations amongst the residual scores for both facial configurations, a single random intercept was created to capture attention biases. However, we modeled the individual deviations for angry and happy facial configurations separately. The primary model was compared to a model with suggested modification indices and a model including mother-reported infant sex as a covariate on the random intercepts (S6). The model with suggested modification indices, but without sex as a covariate, was retained for interpretation as it produced the best fit. Inclusion of sex did not significantly alter the main results (see Databrary for results of all tested models).
When interpreting an RI-CLPM, the random intercepts represent the latent average of a construct. After accounting for the random intercepts, it is possible to assess within-person deviations from the latent average of the same constructs. These within-person relations can be concurrent (ex: the relation between maternal anxiety symptoms and infant affect-biased attention to angry facial configurations at 4-months), longitudinal (ex: the relation between maternal anxiety symptoms at 4-months and 8-months) or cross-lagged (ex: the relation between maternal anxiety at 4-months and infant affect-biased attention at 8-months). Positive relations amongst constructs represent lower within-person deviations on one construct (stability) relating to lower within-person deviations on a second construct (stability). Negative relations amongst constructs represent higher within-person deviations on one construct (fluctuation) relating to lower within-person deviations on a second construct (stability).
Results
Descriptive statistics and zero-order correlations for the sample are reported in Table 2 and Table 3. Overall, we note relatively strong rank-order stability in infant negative affect and maternal anxiety. Infant affect-biased attention did not show significant rank-order stability. However, at any given assessment, affect-biased attention to angry and happy facial configurations were highly correlated.
Table 2.
Descriptive statistics
| N | M | SD | Range | |
|---|---|---|---|---|
| site | 342 | |||
| sex | 342 | |||
| aba4 | 78 | 0 | 0.28 | −1.01 – 1.36 |
| aba8 | 164 | 0 | 0.43 | −1.34 – 1.08 |
| aba12 | 119 | 0 | 0.47 | −1.19 – 1.45 |
| aba18 | 99 | 0 | 0.37 | −1.13 – 0.81 |
| aba24 | 54 | 0 | 0.32 | −0.65 – 0.58 |
| abh4 | 79 | 0 | 0.33 | −1.15 – 1.42 |
| abh8 | 164 | 0 | 0.41 | −0.98 – 1.04 |
| abh12 | 119 | 0 | 0.36 | −1.01 – 1.10 |
| abh18 | 98 | 0 | 0.36 | −1.20 – 0.99 |
| abh24 | 54 | 0 | 0.38 | −0.98 – 0.76 |
| na4 | 239 | 0 | 1.00 | −2.57 – 3.36 |
| na8 | 218 | 0 | 1.00 | −2.16 – 2.98 |
| na12 | 188 | 0 | 1.00 | −3.53 – 2.66 |
| na18 | 177 | 0 | 1.00 | −2.41 – 3.07 |
| na24 | 139 | 0 | 1.00 | −1.99 – 2.61 |
| ma4 | 213 | 6.77 | 7.99 | 0 – 53.00 |
| ma8 | 198 | 5.65 | 6.70 | 0 – 35.00 |
| ma12 | 160 | 7.24 | 8.82 | 0 – 42.00 |
| ma18 | 161 | 7.02 | 8.83 | 0 – 46.00 |
| ma24 | 123 | 5.34 | 6.34 | 0 – 37.00 |
Note: aba = affect-biased attention to angry face configurations, abh = affect-biased attention to happy face configurations, na = infant negative affect, ma = maternal anxiety symptoms
Table 3.
Zero-order correlations
| 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | 18. | 19. | 20. | 21. | 22. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. sex | .04 | .21 | −.06 | .08 | −.05 | −.02 | −.08 | −.09 | −.01 | −.19 | .08 | −.02 | .02 | .09 | .19 | .21 | .04 | .01 | .09 | .02 | .01 |
| 2. site | .09 | −.05 | .02 | −.18 | .12 | −.01 | −.01 | .07 | −.11 | .10 | .17 | .21 | .15 | .11 | .13 | −.14 | .00 | .09 | .04 | −.07 | |
| 3. aba4 | .19 | −.01 | −.05 | .34 | .35 | .28 | −.13 | .01 | .33 | −.17 | −.05 | −.05 | .02 | −.23 | .33 | .09 | .03 | .40 | .32 | ||
| 4. aba8 | .30 | .13 | −.22 | .23 | .44 | .17 | .06 | −.42 | .00 | −.10 | .12 | .12 | .02 | .13 | .14 | .31 | .07 | .26 | |||
| 5. aba12 | −.12 | −.13 | .07 | .20 | .48 | −.09 | −.03 | .23 | .12 | .13 | .22 | .20 | −.01 | .10 | −.03 | .09 | .21 | ||||
| 6. aba18 | −.06 | −.15 | .21 | −.11 | .51 | .09 | .12 | .20 | .18 | .15 | .29 | .06 | −.01 | −.12 | .13 | −.14 | |||||
| 7. aba24 | .17 | −.25 | .01 | −.01 | .55 | −.11 | .06 | −.10 | .06 | .11 | .00 | −.12 | −.15 | −.14 | −.20 | ||||||
| 8. abh4 | .26 | .13 | −.06 | .28 | .00 | −.03 | −.14 | −.13 | .05 | .19 | .03 | .07 | .37 | .37 | |||||||
| 9. abh8 | −.03 | .02 | −.32 | .13 | .06 | .18 | .14 | .07 | .12 | .10 | .19 | .09 | .18 | ||||||||
| 10. abh12 | −.12 | −.06 | .03 | .05 | .10 | .27 | .07 | .02 | .08 | .06 | .07 | .36 | |||||||||
| 11. abh18 | .15 | −.10 | −.03 | −.08 | −.01 | .11 | .20 | −.05 | −.28 | −.05 | −.33 | ||||||||||
| 12. abh24 | −.08 | .12 | .19 | .14 | .29 | .15 | −.07 | −.10 | −.21 | −.13 | |||||||||||
| 13. na4 | .68 | .53 | .51 | .36 | .09 | .11 | .05 | .11 | .23 | ||||||||||||
| 14. na8 | .67 | .41 | .53 | .11 | .12 | .21 | .13 | .10 | |||||||||||||
| 15. na12 | .45 | .59 | .09 | .24 | .22 | .17 | .29 | ||||||||||||||
| 16. na18 | .63 | .20 | .12 | .04 | .05 | .11 | |||||||||||||||
| 17. na24 | .20 | .23 | .26 | .17 | .10 | ||||||||||||||||
| 18. ma4 | .69 | .41 | .59 | .72 | |||||||||||||||||
| 19. ma8 | .61 | .59 | .62 | ||||||||||||||||||
| 20. ma12 | .37 | .56 | |||||||||||||||||||
| 21. ma18 | .74 | ||||||||||||||||||||
| 22. ma24 |
Note: aba = affect-biased attention to angry face configurations, abh = affect-biased attention to happy face configurations, na = infant negative affect, ma = maternal anxiety symptoms; p < .05.
Figure 3 displays the random intercepts and significant paths of the RI-CLPM. The final model exhibited a good fit (CFI = .902, RMSEA = .049), although SRMR was slightly high (.102). At the between-subjects level (random intercepts), infant negative affect and maternal anxiety were positively related. Additionally, infant affect-biased attention and maternal anxiety symptoms were positively related. Data collection site was positively associated with infant negative affect and negatively associated with maternal anxiety symptoms.
Figure 3.
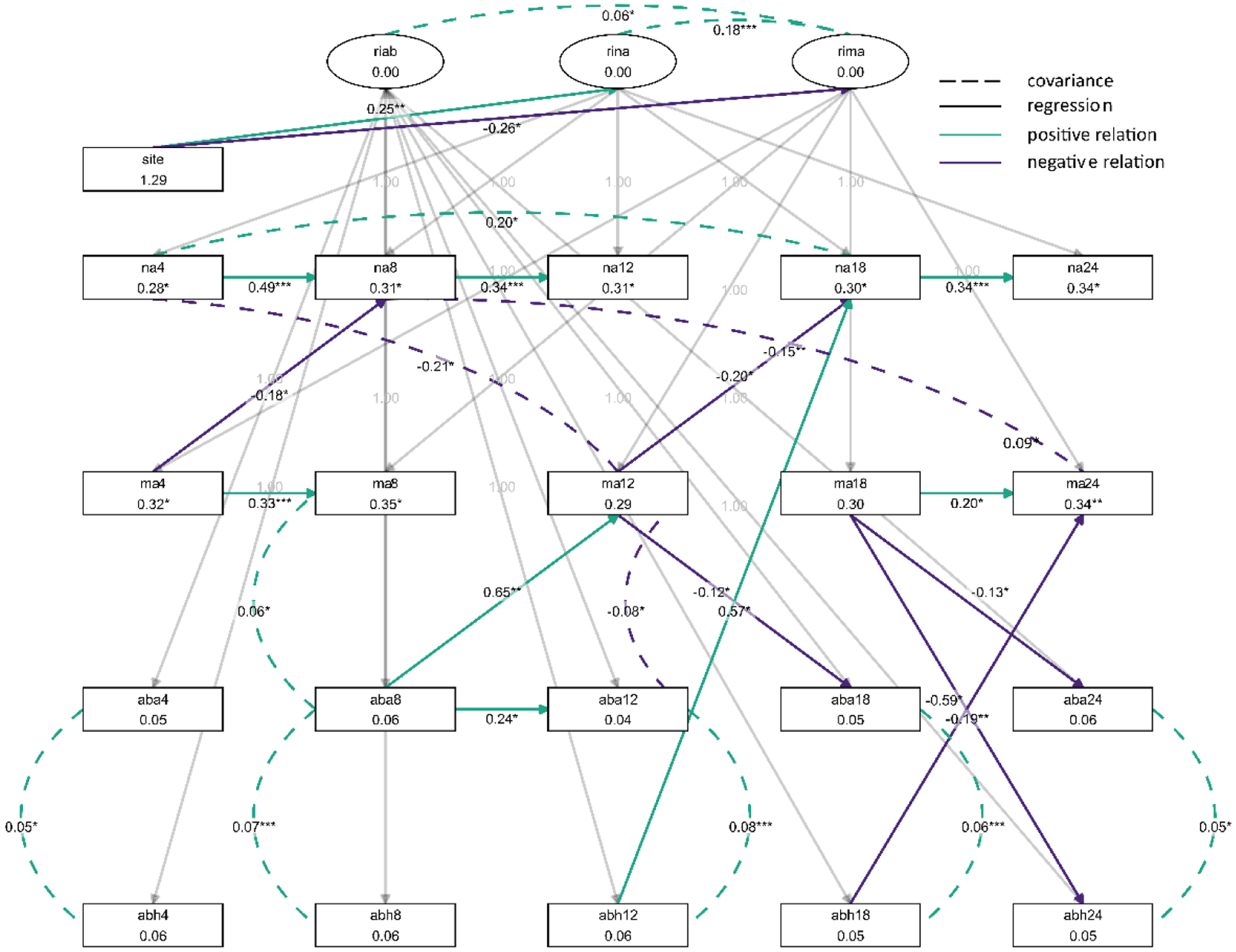
RI-CLPM assessing bidirectional relations between infant negative affect (na), maternal anxiety symptoms (ma), infant affect-biased attention to angry facial configurations (aba) and infant affect-biased attention to happy facial configurations (abh). RI-CLPM models measure within-person deviation in relation to the latent average of a construct (random intercepts). For observed constructs, positive relations represent lower within-person deviations (stability) in one construct relating to lower within-person deviations (stability) in another construct and negative relations represent greater within-person deviations (fluctuation) in one construct relating to lower within-person deviations (stability) in another construct. Visualization created using tidySEM (Van Lissa, 2019).
Concurrent relations.
At every assessment, relations between affect-baised attention to angry facial configurations and affect-biased attention to happy facial configurations were positive, meaning that infants who deviated less in affect-biased attention to angry facial configurations (stability) also deviated less in affect-biased attention to happy facial configurations (stability). At the 8-month assessment, the relation between maternal anxiety and affect-biased attention to angry facial configurations was positive, meaning that mothers who deviated less in maternal anxiety (stability) had infants who deviated less in affect-biased attention to angry facial configurations (stability). At the 12-month assessment, the relation between maternal anxiety symptoms and affect-biased attention to angry facial configurations was negative, meaning mothers who deviated more in maternal anxiety symptoms (fluctuating) had infants who deviated less in affect-biased attention to angry facial configurations (stability).
Longitudinal relations.
Relations between negative affect over time were positive, with a break between the 12- and 18-month assessments, meaning that infants who deviated less in the negative affect at one assessment (stability) generally deviated less at the following assessment (stability). Likewise, relations between maternal anxiety symptoms were positive at the 4- to 8-month and 18- to 24-month assessments, meaning that mothers who deviated less in maternal anxiety symptoms at one assessment (stability) deviated less in maternal anxiety symptoms at the following assessment (stability). Finally, the relation between affect-biased attention to angry facial configurations at the 8- to 12-month assessments was positive, meaning that infants who deviated less in affect-biased attention to angry facial configurations at 8-months (stability) also deviated less at 12-months (stability). No relations were found across time for happy facial configurations.
Cross-lag relations.
Relations between maternal anxiety symptoms and infant negative affect were negative at the 4- to 8-month and 12- to 18-month assessments, meaning that mothers who deviated more in maternal anxiety (fluctuating) had infants who deviated less in negative affect (stability). Additionally, the relations between maternal anxiety symptoms and infant affect-biased attention to angry facial configurations were negative at the 12- to 18-month assessments and 18- to 24-month assessments, meaning that mothers who deviated more in maternal anxiety symptoms (fluctuating) had infants who deviated less in affect-biased attention to angry facial configurations (stability). Further, the relation between maternal anxiety symptoms and infant affect-biased attention to happy faces was negative at the 18- to 24-month assessments, meaning mothers who deviated more in maternal anxiety (fluctuating) had infants who deviated less in affect-biased attention to happy facial configurations (stability).
The relation between affect-biased attention to angry facial configurations and maternal anxiety symptoms was positive at the 8- to 12-month assessment, meaning that infants who deviated less in affect-biased attention to angry facial configurations (stability) had mothers who deviated less in maternal anxiety symptoms (stability). The relation between infant affect-biased attention to happy facial configurations and infant negative affect was positive at the 12- to 18-month assessments, meaning that infants who deviated less in affect-biased attention to happy facial configurations (stability) deviated less in negative affect (stability). The relation between infant affect-biased attention to happy facial configurations and maternal anxiety symptoms at the 18- to 24-month assessments was negative, meaning that infants who deviated less in affect-biased attention to happy facial configurations (stability) had mothers who deviated more in maternal anxiety (fluctuating).
Discussion
The current study capitalized on data from a multi-site, longitudinal cohort to assess potential bidirectional relations between infant affect-biased attention, infant temperamental negative affect and maternal anxiety symptoms (Morales et al., 2016) to better understand patterns of affect-biased attention over time (Field & Lester, 2010). Our model allowed us to build on prior work aimed at understanding the role of individual differences in affect-biased attention development by examining both between- and within-person variation. As such, we accounted for change across multiple measures and prospective relations between these measures. At the between-subjects level (random intercepts), we found that greater infant affect-biased attention to emotional facial configurations was related to higher levels of maternal anxiety symptoms, replicating previous findings (Kataja et al., 2019; Morales, Brown, et al., 2017).
Because our study design collected all measures longitudinal, we were also able to examine how within-person variation further contributed to affect-biased attention above and beyond the between-subjects level. At the within-person level (deviations), we found that mothers who fluctuated more in maternal anxiety symptoms (deviated more from their base symptom level) at the 12- and 18-month assessments had infants who exhibited more stable affect-biased attention to angry facial configurations at the following assessments and happy facial configurations (deviated less from their base affect-biased attention level) at the 24-month assessment. Thus, our results suggest that while overall higher maternal anxiety is related to greater infant affect-biased attention (random intercepts), at the individual level (cross-lags) fluctuating anxiety levels during an infant’s second year of life may elicit more stable attention patterns to both angry and happy facial configurations in infants. It may be that an inconsistent emotional environment, in this case inconsistent maternal signals about the environment due to fluctuating symptoms (Aktar et al., 2013), may elicit more stability in socioemotional processing as infants try to make sense of an uncertain environment. Naturalistic work assessing maternal behaviors and child gaze patterns using mobile eye-tracking may better elucidate this possibility (Adolph et al., 2018).
These findings are consistent with previous work suggesting that patterns of attention, rather than specific emotion biases, are important for understanding attention-anxiety relations (Morales, Taber-Thomas, et al., 2017; Vallorani et al., 2021). Indeed, attentional rigidity, or consistency and stability in attentional patterns is indicative of both temperamental risk for anxiety (Henderson & Wilson, 2017) and anxiety symptoms (Morales, Taber-Thomas, et al., 2017). Here, we noted that greater fluctuations in maternal anxiety symptoms are similarly associated with greater stability in infant attention, first with angry, and then happy, facial configurations. Stable patterns of attention, whether towards or away from emotional stimuli, may limit the scope of environmental stimuli infants experience and process. Consistent filtering of the environment beginning as early as infancy could lead to biases in processing and interpreting social information (Pérez-Edgar, 2018), which may lead to future socioemotional difficulties.
Contrary to our expectations, we did not find that relations with maternal anxiety symptoms were specific to angry facial configurations. Instead, a relation with happy facial configurations also emerged after 18 months. Previous work suggests that maternal anxiety is related to infant attention to emotion more generally (Kataja et al., 2019; Vallorani et al., 2021). Furthermore, evidence suggests that elevated attention to indirect threats, such as fearful facial configurations, during the first year of life may taper off within the second year of life (Peltola et al., 2018), but that attention to direct threats, such as angry facial configurations may emerge (Leppänen et al., 2018; Reider et al., in press; Xie et al., 2021). During the second year of life, infants may broaden their processing of socioemotional stimuli and incorporate environmental input across more diverse aspects of the social world, including biases to positive stimuli.
Our findings provide evidence supporting the acquisition or moderation models, which both suggest changes in affect-biased attention over time due to individual difference factors. Contrary to the integral bias model, we neither observed that all infants exhibited attention biases (Figure 2, Figure S1), nor that affect-biased attention to angry or happy facial configurations was stable (Table 2). Rather, our results suggest that both between-subjects and within-person differences in infant affect-biased attention may be at least partially driven by individual differences in maternal anxiety symptom. Thus, it is possible that interventions targeting parental symptomatology could alter emerging patterns of infant affect-biased attention. Indeed, a recent systematic review indicated that maternal anxiety is associated with overprotective parenting (Jones et al., 2021), which is known to relate to childhood anxiety (Buss et al., 2021). Interventions that target parenting behaviors, such as over protectiveness, are associated with notable reductions in child anxiety (Rapee et al., 2010). Early interventions geared towards alleviating maternal anxiety or targeting parenting could alter early processes that may cause children to experience difficulties with socioemotional processing, social withdrawal or anxiety.
We anticipated that relations between maternal anxiety and infant affect-biased attention would be enhanced through bidirectional relations between infant negative affect and maternal anxiety symptoms. However, we did not observe consistent bidirectional relations. Instead, we found that maternal anxiety symptoms prospectively related to infant negative affect such that mothers who exhibited more fluctuation in maternal anxiety symptoms at the 4- and 12-month assessments had infants with more stable negative affect at the following assessments. However, it does not appear that bidirectional relations between infant negative affect and maternal anxiety symptoms propelled affect-biased attention development. Previous work in infants suggests negative affect and maternal anxiety may be mutually reinforcing, particularly when disambiguating shared genetic variance (Brooker et al., 2015). Future work assessing attention in the context of shared genetic variance may better assess the potential influence of bidirectional relations between infant negative affect and maternal anxiety on affect-biased attention.
We also found that infants who had more stable attention to angry facial configurations at 8-months had mothers with more stable patterns of maternal anxiety at 12-months. Additionally, infants with more stable attention to happy facial configurations at 18-months had mothers who fluctuated more in maternal anxiety at 24-months. These infant-to-mother relations were unexpected. Differences in patterns between these two relations could be due both to infant age and differences in angry versus happy facial configurations. Future work using more naturalistic techniques, such as mobile eye-tracking during home visits (Adolph et al., 2018), may better capture how infant attention to socioemotional stimuli may influence patterns of behavior and anxiety in mothers.
Our findings should be considered with several limitations in mind. First, our assessments began at 4-months, rather than at birth, limiting our ability to capture the earliest biases, if they exist, or rule out early experiential effects on attention bias. Alternative methods may be needed to adequately assess infant affect-biased attention from birth to make distinctions between the moderation and acquisition models. Second, mothers provided both our measures of maternal anxiety symptoms and infant negative affect. Reporter bias could shape these results. However, maternal anxiety symptoms and infant negative affect were not highly correlated (rs < .29) when compared to the internal stability of reported infant negative affect (rs > .36) and maternal anxiety symptoms (rs > .37). These relations suggest that mothers were able to differentially report their own anxiety versus their infant’s negative affect as suggested by previous research (Olino et al., 2021).
Third, our data cannot speak to the role of genetic influences on these processes. There is clear evidence for the role of genetics in bidirectional relations between infant negative affect and maternal anxiety (Brooker et al., 2015). However, the ways in which social attention may be biologically based are less clear. Recent work showing similarity in attention to emotional facial configurations between mothers and infants may suggest a genetic component to attention biases (Aktar et al., 2022). However, it could also be the case that infants learn to attend to certain emotional cues based on parental behavior to specific socioemotional cues (Aktar et al., 2013). Further, although genetic transmission undoubtedly plays a role in anxiety risk (Hettema et al., 2001), evidence also indicates that environmental experience may be more influential (Eley et al., 2015). As with most developmental processes, it is likely a complex interplay between genetics and the environment (Sameroff, 2010) that best explains affect-biased attention development and future research should better assess genetic contributions.
Fourth, our results are limited to mothers and their infants. Fathers also play an important role in shaping child trajectories of affect-biased attention and anxiety (Aktar et al., 2019; Field et al., 2020). Additionally, contextual elements, such as home or community environments, could influence how attention biases develop and influence anxiety risk. Future work should assess these relations in more generalizable contexts, integrating different family and cultural systems to better understand individual differences in affect-biased attention development. Finally, we focused on angry facial configurations as a measure of direct threat (Leppänen & Nelson, 2012) as angry facial configurations are commonly used in research related to anxiety (Bar-Haim et al., 2007). However, fearful facial configurations are commonly used as a measure of indirect threat in infancy research. Future work could compare longitudinal relations in attention to direct (angry) versus indirect (fearful) threat and how this relates to anxiety risk.
In conclusion, we found that mothers who fluctuated more in maternal anxiety at the 12- and 18-month assessments had infants who exhibited more stable affect-biased attention, first to angry facial configurations and then also the happy facial configurations. Additionally, mothers who fluctuated more in maternal anxiety at the 4- and 12-month assessments had infants who exhibited more stable patterns of negative affect. Consistent bidirectional relations were not found. In line with the acquisition and moderation models (Field & Lester, 2010), patterns of individual difference factors were prospectively related to infant affect-biased attention. Our results provide an important first step in understanding affect-biased attention development. Acknowledging that attention biases are not constant suggests targeted interventions could alter trajectories towards social withdrawal and anxiety. Early interventions geared towards alleviating maternal anxiety or providing early parenting interventions (Rapee et al., 2010) could alter the course of affect-biased attention and socioemotional development.
Supplementary Material
Public Significance Statement.
The current study capitalizes on a multi-site, longitudinal data set to assess individual differences associated with affect-biased attention development and early anxiety risk. We found that although overall mothers with higher levels of anxiety symptoms have infants that exhibit greater affect-biased attention, over time, infants with mothers who fluctuate more in maternal anxiety symptoms have infants who exhibit more stable affect-biased attention. Environmental uncertainty, linked to fluctuating maternal anxiety, may shape early socioemotional development.
Acknowledgments
This study was supported by grants from the National Institute of Mental Health (NIMH) to Drs. Koraly Pérez-Edgar, Kristin A. Buss & Vanessa LoBue (R01 MH109692) and Alicia Vallorani (F31 MH121035), the National Institute of Neurological Disorders and Stroke (NINDS) to Berenice Anaya (F99/K00 NS120411), the Eunice Kennedy Shriver Institute of Child Health and Human Development (NICHD) to Jessica L. Burris (K99 HD099328-01), and a National Science Foundation (NSF) Graduate Research Fellowship to Kelley E. Gunther (DGE1255832).
Footnotes
There are no additional conflicts of interest to report.
Data and analytic code are available on Databrary (LoBue et al., 2021). The study was not preregistered.
References
- Adolph K, Tamis-LeMonda C, Gilmore R, & Soska K (2018). Play & learning across a year (PLAY) project summit. Databrary. https://nyu.databrary.org/volume/724 [Google Scholar]
- Aktar E, Majdandžić M, de Vente W, & Bögels SM (2013). The interplay between expressed parental anxiety and infant behavioural inhibition predicts infant avoidance in a social referencing paradigm: Expressed parental anxiety and infant behavioural inhibition. Journal of Child Psychology and Psychiatry, 54(2), 144–156. 10.1111/j.1469-7610.2012.02601.x [DOI] [PubMed] [Google Scholar]
- Aktar E, Nimphy CA, Kret ME, Pérez-Edgar K, Raijmakers MEJ, & Bögels SM (2022). Attention biases to threat in infants and parents: Links to parental and infant anxiety dispositions. Research on Child and Adolescent Psychopathology. 10.1007/s10802-021-00848-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aktar E, Van Bockstaele B, Pérez‐Edgar K, Wiers RW, & Bögels SM (2019). Intergenerational transmission of attentional bias and anxiety. Developmental Science, 22(3), e12772. 10.1111/desc.12772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, & van IJzendoorn MH (2007). Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin, 133(1), 1–24. 10.1037/0033-2909.133.1.1 [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, & Steer RA (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897. 10.1037/0022-006X.56.6.893 [DOI] [PubMed] [Google Scholar]
- Brooker RJ, Neiderhiser JM, Leve LD, Shaw DS, Scaramella LV, & Reiss D (2015). Associations between infant negative affect and parent anxiety symptoms are bidirectional: Evidence from mothers and fathers. Frontiers in Psychology, 6. 10.3389/fpsyg.2015.01875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buss KA, Zhou AM, & Trainer A (2021). Bidirectional effects of toddler temperament and maternal overprotection on maternal and child anxiety symptoms across preschool. Depression and Anxiety, 38(12), 1201–1210. 10.1002/da.23199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eley TC, McAdams TA, Rijsdijk FV, Lichtenstein P, Narusyte J, Reiss D, Spotts EL, Ganiban JM, & Neiderhiser JM (2015). The Intergenerational Transmission of Anxiety: A Children-of-Twins Study. American Journal of Psychiatry, 172(7), 630–637. 10.1176/appi.ajp.2015.14070818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders C, & Bandalos D (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling: A Multidisciplinary Journal, 8(3), 430–457. 10.1207/S15328007SEM0803_5 [DOI] [Google Scholar]
- Field AP, & Lester KJ (2010). Is there room for ‘development’ in developmental models of information processing biases to threat in children and adolescents? Clinical Child and Family Psychology Review, 13(4), 315–332. 10.1007/s10567-010-0078-8 [DOI] [PubMed] [Google Scholar]
- Field AP, Lester KJ, Cartwright-Hatton S, Harold GT, Shaw DS, Natsuaki MN, Ganiban JM, Reiss D, Neiderhiser JM, & Leve LD (2020). Maternal and paternal influences on childhood anxiety symptoms: A genetically sensitive comparison. Journal of Applied Developmental Psychology, 68, 101123. 10.1016/j.appdev.2020.101123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox NA, Snidman N, Haas SA, Degnan KA, & Kagan J (2015). The relations between reactivity at 4 months and behavioral inhibition in the second year: Replication across three independent samples. Infancy, 20(1), 98–114. 10.1111/infa.12063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu X, Morales S, LoBue V, Buss KA, & Pérez-Edgar K (2020). Temperament moderates developmental changes in vigilance to emotional faces in infants: Evidence from an eye-tracking study. Developmental Psychobiology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith HH (1996). Studying temperament via construction of the toddler behavior assessment questionnaire. Child Development, 67(1), 218–235. 10.1111/j.1467-8624.1996.tb01730.x [DOI] [PubMed] [Google Scholar]
- Hamaker EL, Kuiper RM, & Grasman RPPP (2015). A critique of the cross-lagged panel model. Psychological Methods, 20(1), 102–116. 10.1037/a0038889 [DOI] [PubMed] [Google Scholar]
- Henderson HA, & Wilson MJG (2017). Attention processes underlying risk and resilience in behaviorally inhibited children. Current Behavioral Neuroscience Reports, 4(2), 99–106. 10.1007/s40473-017-0111-z [DOI] [Google Scholar]
- Hettema JM, Neale MC, & Kendler KS (2001). A review and meta-analysis of the genetic epidemiology of anxiety disorders. American Journal of Psychiatry, 158(10), 1568–1578. 10.1176/appi.ajp.158.10.1568 [DOI] [PubMed] [Google Scholar]
- Hunnius S, & Geuze RH (2004). Gaze shifting in infancy: A longitudinal study using dynamic faces and abstract stimuli. Infant Behavior and Development, 27(3), 397–416. 10.1016/j.infbeh.2004.02.003 [DOI] [PubMed] [Google Scholar]
- Jones LB, Hall BA, & Kiel EJ (2021). Systematic review of the link between maternal anxiety and overprotection. Journal of Affective Disorders, 295, 541–551. 10.1016/j.jad.2021.08.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalomiris AE, & Kiel EJ (2016). Maternal anxiety and physiological reactivity as mechanisms to explain overprotective primiparous parenting behaviors. Journal of Family Psychology, 30(7), 791–801. 10.1037/fam0000237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kataja E-L, Karlsson L, Parsons CE, Pelto J, Pesonen H, Häikiö T, Hyönä J, Nolvi S, Korja R, & Karlsson H (2019). Maternal pre- and postnatal anxiety symptoms and infant attention disengagement from emotional faces. Journal of Affective Disorders, 243, 280–289. 10.1016/j.jad.2018.09.064 [DOI] [PubMed] [Google Scholar]
- Kenny DA (2020). Measuring Model Fit. http://www.davidakenny.net/cm/fit.htm
- Leppänen JM, Cataldo JK, Bosquet Enlow M, & Nelson CA (2018). Early development of attention to threat-related facial expressions. PLOS ONE, 13(5), e0197424. 10.1371/journal.pone.0197424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppänen JM, & Nelson CA (2012). Early Development of Fear Processing. Current Directions in Psychological Science, 21(3), 200–204. 10.1177/0963721411435841 [DOI] [Google Scholar]
- Lerner RM, Hershberg RM, Hilliard LJ, & Johnson SK (2015). Concepts and theories of human development. In Bornstein MH (Ed.), Developmental Science: An Advanced Textbook (6th ed., pp. 3–41). Psychology Press. [Google Scholar]
- LoBue V, & DeLoache JS (2010). Superior detection of threat-relevant stimuli in infancy: Threat detection in infancy. Developmental Science, 13(1), 221–228. 10.1111/j.1467-7687.2009.00872.x [DOI] [PubMed] [Google Scholar]
- LoBue V, Pérez-Edgar K, & Buss KA (2021). Publications from the Longitudinal Attention and Temperament Study (LANTS). Databrary. https://nyu.databrary.org/volume/1288 [Google Scholar]
- Lodder P (2013). To impute or not impute: That’s the question. In Mellenbergh GJ & Adèr HJ (Eds.), Advising on research methods. Johannes van Kessel Publishing. [Google Scholar]
- Meyer A, Lerner MD, De Los Reyes A, Laird RD, & Hajcak G (2017). Considering ERP difference scores as individual difference measures: Issues with subtraction and alternative approaches. Psychophysiology, 54(1), 114–122. 10.1111/psyp.12664 [DOI] [PubMed] [Google Scholar]
- Morales S, Brown KM, Taber-Thomas BC, LoBue V, Buss KA, & Pérez-Edgar KE (2017). Maternal anxiety predicts attentional bias towards threat in infancy. Emotion, 17(5), 874–883. 10.1037/emo0000275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales S, Fu X, & Pérez-Edgar KE (2016). A developmental neuroscience perspective on affect-biased attention. Developmental Cognitive Neuroscience, 21, 26–41. 10.1016/j.dcn.2016.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales S, Taber-Thomas BC, & Pérez-Edgar KE (2017). Patterns of attention to threat across tasks in behaviorally inhibited children at risk for anxiety. Developmental Science, 20(2), e12391. 10.1111/desc.12391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Michelini G, Mennies RJ, Kotov R, & Klein DN (2021). Does maternal psychopathology bias reports of offspring symptoms? A study using moderated non-linear factor analysis. Journal of Child Psychology and Psychiatry, jcpp.13394. 10.1111/jcpp.13394 [DOI] [PubMed] [Google Scholar]
- Parade SH, & Leerkes EM (2008). The reliability and validity of the infant behavior questionnaire-revised. Infant Behavior and Development, 31(4), 637–646. 10.1016/j.infbeh.2008.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltola MJ, Leppänen JM, Palokangas T, & Hietanen JK (2008). Fearful faces modulate looking duration and attention disengagement in 7-month-old infants. Developmental Science, 11(1), 60–68. 10.1111/j.1467-7687.2007.00659.x [DOI] [PubMed] [Google Scholar]
- Peltola MJ, Yrttiaho S, & Leppänen JM (2018). Infants’ attention bias to faces as an early marker of social development. Developmental Science, 21(6), e12687. 10.1111/desc.12687 [DOI] [PubMed] [Google Scholar]
- Pérez-Edgar K (2018). Attention mechanisms in behavioral inhibition: Exploring and exploiting the environment. In Pérez-Edgar K & Fox NA (Eds.), Behavioral Inhibition (pp. 237–261). Springer International Publishing. 10.1007/978-3-319-98077-5_11 [DOI] [Google Scholar]
- Pérez-Edgar K, & Fox NA (2005). Temperament and anxiety disorders. Child and Adolescent Psychiatric Clinics of North America, 14(4), 681–706. 10.1016/j.chc.2005.05.008 [DOI] [PubMed] [Google Scholar]
- Pérez-Edgar K, LoBue V, Buss KA, Field AP, & LAnTs Team. (2021). Study protocol: Longitudinal attention and temperament study. Frontiers in Psychiatry, 12, 656958. 10.3389/fpsyt.2021.656958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Edgar K, Morales S, LoBue V, Taber-Thomas BC, Allen EK, Brown KM, & Buss KA (2017). The impact of negative affect on attention patterns to threat across the first 2 years of life. Developmental Psychology. 10.1037/dev0000408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen SE, & Posner MI (2012). The attention system of the human brain: 20 years after. Annual Review of Neuroscience, 35(1), 73–89. 10.1146/annurev-neuro-062111-150525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Coffman DL (2006). Computing power and minimum sample size for RMSEA. http://quantpsy.org/
- Rapee RM, Kennedy SJ, Ingram M, Edwards SL, & Sweeney L (2010). Altering the trajectory of anxiety in at-risk young children. American Journal of Psychiatry, 167(12), 1518–1525. 10.1176/appi.ajp.2010.09111619 [DOI] [PubMed] [Google Scholar]
- Reider LB, Bierstedt L, Burris JL, Vallorani A, Gunther KE, Buss KA, Pérez-Edgar K, Field AP, & LoBue V (in press). Developmental patterns of affective attention across the first two years of life. Child Development. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y (2012). lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software, 48(2). 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- Rothbart MK, Sheese BE, Rueda MR, & Posner MI (2011). Developing mechanisms of self-regulation in early life. Emotion Review, 3(2), 207–213. 10.1177/1754073910387943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sameroff AJ (2010). A unified theory of development: A dialectic integration of nature and nurture. Child Development, 81(1), 6–22. 10.1111/j.1467-8624.2009.01378.x [DOI] [PubMed] [Google Scholar]
- Slagt M, Dubas JS, Deković M, & van Aken MAG (2016). Differences in sensitivity to parenting depending on child temperament: A meta-analysis. Psychological Bulletin, 142(10), 1068–1110. 10.1037/bul0000061 [DOI] [PubMed] [Google Scholar]
- Todd RM, Cunningham WA, Anderson AK, & Thompson E (2012). Affect-biased attention as emotion regulation. Trends in Cognitive Sciences, 16(7), 365–372. 10.1016/j.tics.2012.06.003 [DOI] [PubMed] [Google Scholar]
- Tottenham N, Tanaka JW, Leon AC, McCarry T, Nurse M, Hare TA, Marcus DJ, Westerlund A, Casey B, & Nelson C (2009). The NimStim set of facial expressions: Judgments from untrained research participants. Psychiatry Research, 168(3), 242–249. 10.1016/j.psychres.2008.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallorani A, Fu X, Morales S, LoBue V, Buss KA, & Pérez-Edgar K (2021). Variable- and person-centered approaches to affect-biased attention in infancy reveal unique relations with infant negative affect and maternal anxiety. Scientific Reports, 11(1), 1719. 10.1038/s41598-021-81119-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Lissa CJ (2019). TidySEM: A tidy workflow for running, reporting, and plotting structural equation models in lavaan or Mplus (0.1.6). https://github.com/cjvanlissa/tidySEM/
- Xie W, Leppänen JM, Kane-Grade FE, & Nelson CA (2021). Converging neural and behavioral evidence for a rapid, generalized response to threat-related facial expressions in 3-year-old children. NeuroImage, 229, 117732. 10.1016/j.neuroimage.2021.117732 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data and analytic code are available on Databrary (LoBue et al., 2021). The study was not preregistered.


