Abstract
Injuries are predicted to become a greater cause of mortality than communicable diseases in sub-Saharan Africa by 2030, signaling a public health dilemma for governments and citizens in each country. This article uses epidemiological estimates of injuries in Zambia, considers the socio-economic impact of injuries, examines current policies for prevention, and provides a rapid situation analysis to help develop an action and research agenda for injury prevention in the country. It calls for better epidemiological data, capacity building for human resources, and adoption of evidence-based targets and interventions. For Zambia to reduce its burden of injuries, funding for research and training should be integral to the future of its national health agenda.
Keywords: Injuries, trauma, Zambia, low- and middle-income countries
Introduction
In 2019, approximately 4.3 million deaths occurred globally due to injuries, constituting an estimated 7.61% of global mortality.1 Road traffic injuries (RTIs) alone caused 1.2 million deaths in 2019.2 Low- and middle-income countries (LMICs) faced a majority of the burden from injuries worldwide (62.98 per 100,000).3 Roughly half of the world’s LMICs are located in sub-Saharan Africa where RTI rates are highest in the world.1, 4 Compounded by the fact that approximately 40% of the population in sub-Saharan Africa lives under 1.90 US dollars (USD) per day,5, 6 the social and economic impacts of injuries are significant.7–9 Within the region, however, there are vast discrepancies in how injuries are measured and recorded.2, 10
Zambia is one of the countries with a high rate of deaths from injuries out of the 54 countries in sub-Saharan Africa.1 In this paper, we argue that injuries are negatively affecting the health of Zambians and call for increased research, policy response and community attention. We briefly review selected epidemiological estimates of injuries in Zambia, consider the socio-economic impact of injuries, examine current policies for prevention, and provide a rapid situation analysis to make the case for expanded action and research for injury prevention and training in the country. We hope that this paper will stimulate global and national dialogue on the need for injury-related investments in Zambia and southern Africa.
Snapshot of Injuries in Zambia
In Zambia, injuries contribute to 1 in 5 premature deaths and 7% of all deaths annually.1, 11 In 2019, injuries caused 46.58 deaths per 100,000 population signaling an important public health burden for the Zambian government and its citizens (Table 1).1 Males are disproportionately impacted by deaths from injuries (69.56 per 100,000) across nearly all causes (Table 1).1 Transport injuries, the 14th leading cause of death in Zambia, caused the highest rates of injury deaths for both men and women, and comprised over a quarter of Zambia’s injury-related deaths in 2019 (Figure 1).1 An epidemiological study found that deaths from RTIs in Zambia were higher among public transport occupants than private vehicle occupants due to safety concerns, such as driver fatigue and long distances.12 The Zambia Road Transport & Safety Agency reported that speeding was one of the top contributing factors (14.4%) for RTIs in the country.13
Table 1:
Summary of injury burden in Zambia, 2019
| Epidemiological Measure | Value |
|---|---|
| Population | 17,861,030 |
| % of all deaths due to injuries | 6.88 |
| Estimated number of deaths due to injuries per year | 8,495 |
| Males | 6,272 |
| Females | 2,223 |
| Injury-related death per 100,000 population | 46.58 |
| Males | 69.56 |
| Females | 24.11 |
| Injury-related deaths per 100,000, by age groups | |
| 0–1 | 41.47 |
| 1–4 | 24.09 |
| 5–14 | 12.41 |
| 15–49 | 48.94 |
| 50–69 | 139.77 |
| >70 | 365.81 |
| Estimated incidence of injuries per year | 1,218,389 |
| Males | 678,886 |
| Females | 539,502 |
| Injury-related morbidity per 100,000, by sex | 6,681 |
| Males | 7,529 |
| Females | 5,851 |
| Injury-related morbidity per 100,000, by age groups | |
| 0–1 | 9,441 |
| 1–4 | 7,791 |
| 5–14 | 7,057 |
| 15–49 | 6,188 |
| 50–69 | 5,367 |
| >70 | 6,962 |
Source: Global Burden of Disease, 20191
Figure 1:
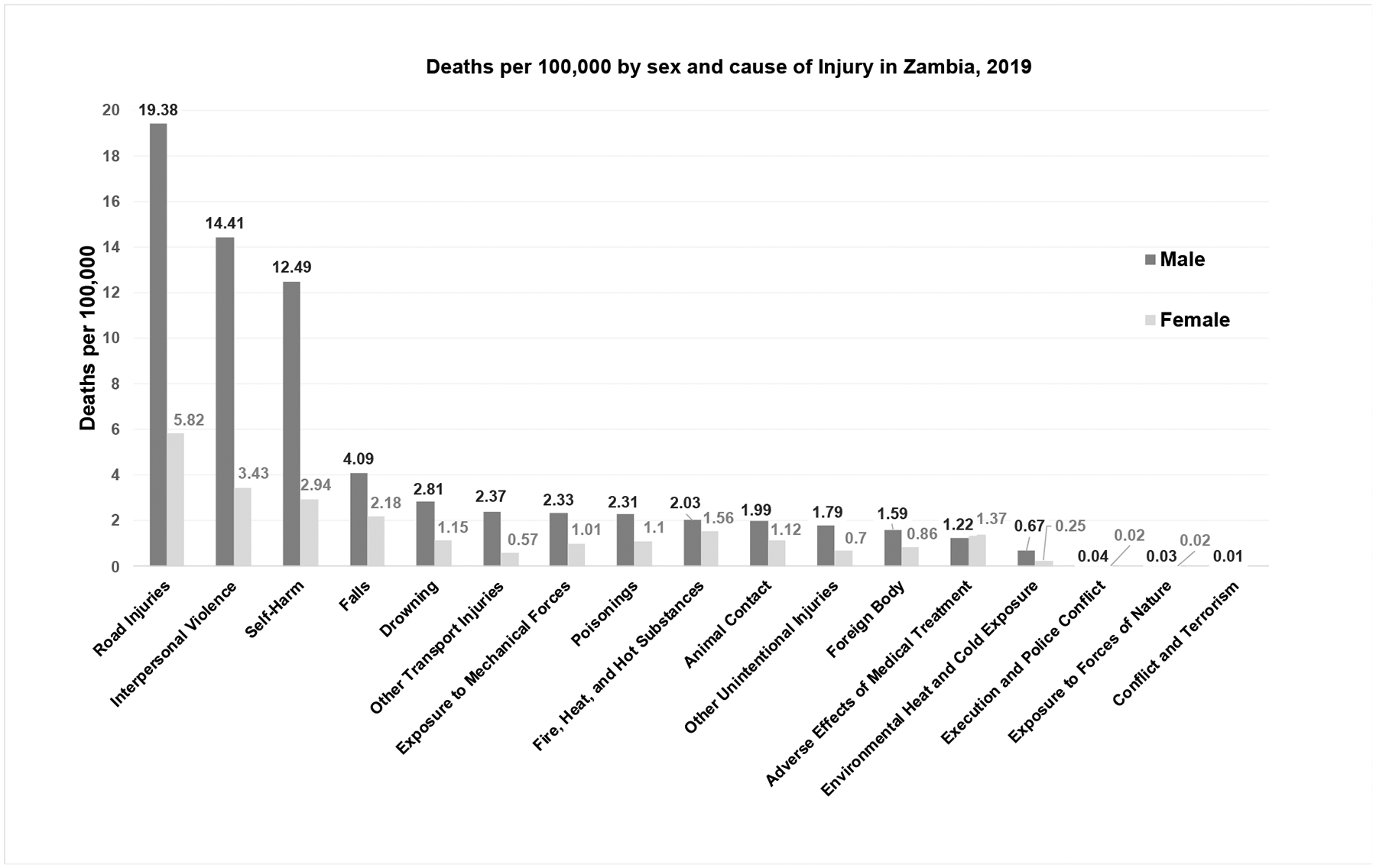
Injury deaths per 100,000 by sex and cause in Zambia, 2019
*Source: Global Burden of Disease, 20191
Between 2010 and 2019, the incidence of injuries in Zambia increased by approximately 6%.1 Morbidity from injuries was more common among males (7,529.14 injuries per 100,000) than females (5,850.87 injuries per 100,000); however the rate increased more rapidly for females (+7.37% and +4.96% between 2010 and 2019, respectively), indicating a growing concern for the future.1 The injury rate was highest among children under 1 year of age (9,440.57 injuries per 100,000) and these children were most impacted by exposure to mechanical forces, foreign bodies, and animal contact.1 For all ages combined, the top three causes of morbidity due to injuries were falls, exposure to mechanical forces, and animal contact.1 Causes for the high injury morbidity due to exposure to mechanical forces were inadequate training on proper use of equipment and lack of funding for inspection oversight.14 RTIs, falls, and interpersonal violence were also the top three causes of years lived with disability (YLD) among all persons (Figure 2).1
Figure 2:

Injury disability-adjusted life years (DALYs), years lived with disability (YLDs), and years of life lost (YLLs) by sex, Zambia, 2019
*Source: Global Burden of Disease, 20191
Over 2,415 disability-adjusted life years (DALYs) per 100,000 were lost from all injuries in Zambia, representing 61% of the total disease burden in 2019.1, 2 The rate of DALYs was higher for males (4,046.88 per 100,000) than for females (1,584.28 per 100,000).1 RTIs caused the highest rate of DALYs, followed by interpersonal violence, and self-harm.1 DALYs decreased from 2010 to 2019 by 16.10%, however, YLD increased by 11.5% during the same timeframe, suggesting that while there have been fewer years of life lost due to injury, there are more years lived with disability in Zambia (Figure 2).
Socioeconomic Impact of Injuries in Zambia
Zambia acknowledged injuries as a major cause of disability and premature death in the 2013–2016 Strategic Plan on Non-Communicable Diseases (NCDs), though very little (<1%) of its national Gross Domestic Product (GDP) was allocated to total health expenditures (9% or US$ 3 per capita) in 2018.4, 15 Moreover, out-of-pocket expenditures make up a significant proportion of injury costs in the country.16 In 2018, the total number of DALYs due to injury totaled 504,000,1 which resulted in $738 million dollars (USD 2018) in economic productivity loss; about 58% of economic productivity losses were to individuals aged 15–49 years.15 Compared to 2010, the economic productivity loss increased by 13% in 2018, a direct result of increasing injuries and a growing Zambian economy.15
As Zambia’s population is younger in age and growing in size, injuries become an even greater concern for individual and national socio-economic wellbeing. The population of Zambia is projected to more than double by 2050, and increase five times by 2100, making it one of the fastest growing countries in the world.17, 18 In 2015, Zambia had one of the lowest median ages in the world (16.7 years), and is expected to result in a growing number of people in peak working productivity years, increased life expectancy, and higher proportion of elderly (65+).17, 19 All of these factors affect the growing burden of injuries among Zambians in the future.
Zambia is also experiencing rapid urbanization with 44% of people living in urban areas in 2020 and projected to increase to 50% by 2035, increasing exposure to high-risk environments for injuries.18, 20, 21 Contributing to this environment is the negative impact of early stages of economic improvements characterized by unhealthy lifestyles, increasing prevalence of unsafe transportation, excessive intake of alcohol, and unsafe work environments.5, 22, 23 In addition, the geo-political situation in Zambia, and in southern Africa, makes the country extremely vulnerable to political and societal changes.20, 24 These risk factors drive a high burden of injuries affecting young Zambians.25
Summary of Policy Movements
Zambia has expressed a desire to reduce the burden of injuries, but commitment to developing and enforcing national policy interventions has been variable (Table 2). The earliest policy statement on injuries came in 2011 when Zambia participated in a regional consultation convened by the WHO African Region to expand the conversation about NCDs and injury.3 This led to the Brazzaville Declaration, which asserted awareness of the significant impact injuries have on development and health.26
Table 2:
Policy events involving injuries and trauma, Zambia
| Year | Policy Action/Documents | Major Agenda |
|---|---|---|
| 1994 | Firearms Act35 | First time ratifying gun control legislation |
| 2002 | Road Traffic Act No. 1136 | First time stablishing a nationwide Road Transport and Safety Agency |
| 2006 | Vision 203037 | Shaped Zambia’s healthcare vision and asserted the importance of equality in access to care |
| 2010 | Occupational and Safety Act38 | First International Labor Organization workplace safety act ratified |
| 2011 | Brazzaville Declaration on Non-Communicable Diseases Prevention and Control in the WHO African Region26 | First time acknowledging injuries as a severe development challenge on a regional stage |
| 2015 | Zambian Ministry of Health Non-Communicable Disease and Injury Strategic Plan (2013–2016)25 | First national plan that included injuries |
| 2015 | Lancet Commission on Global Surgery39 | One of first countries to sign on join this commission to design and implement a National Surgical and Anesthesia Plan |
| 2016 | Lancet Commission on Reframing NCDs and Injuries for the Poorest Billion3 | First time engagement with global commission on injuries |
| 2017 | Health-in-All-Policies27 | First time announcing a public health strategy across all government sectors |
| 2017 | Zambia National Health Strategic Plan 2017 – 202111 | First country to adopt the Lancet’s regional research approach to strengthen Zambia’s surgical field in order to respond to injuries and other conditions |
In the Non-Communicable Disease and Injury (NCDI) Strategic Plan for 2013–2016 the Zambian ministry of health highlighted RTIs, assaults, and burns as leading causes of injuries.25 It also described drugs and substance abuse, excess alcohol use, and occupational risks as common risk factors for injuries.27 The Ministry of Health (MoH) acknowledged that the prevention of injuries is multi-sectoral, not only requiring equipment and medicines at district health facilities, but also scaling up road infrastructure, information and public awareness of injuries, and enforcement of relevant policies and legislation.25 In 2016, Zambia joined the Lancet Commission on Reframing NCDs and Injuries for the Poorest Billion (Lancet NCDI Poverty Commission), which aims to prevent deaths from NCDs and injuries for people living in extreme poverty across the globe by “elevating an emerging NCDI Poverty movement and accountability mechanism(s) that will contribute to health and shared prosperity for all.”3, 28
The Zambian MoH in 2016 also partnered with the Lancet Commission on Global Surgery to develop the National Surgery Obstetric and Anesthesia Strategic Plan 2017–21.11 This plan was aimed at strengthening surgical and obstetric care to the most neglected areas of health delivery, including trauma-related injuries which were noted to be among the top five causes of morbidity and mortality in Zambia.11 The government of Zambia in 2017 approved a five-year Health-in-All-Policies strategy that brings diverse sectors together to address complex health problems and offers a pathway for coordinated action on social determinants of health related to injuries.27 This approach reaffirms the United Nations’ Sustainable Development Goals and recognizes the importance of social determinants of health, which drive morbidity and mortality injury outcomes at different upstream and downstream levels.27
Also, in 2017, the Zambia government developed the National Health Strategic Plan 2017–21, which supports the National Vision 2030.27 This plan is a transformative agenda aimed at delivering quality health services to all Zambians. The plan highlights trauma and injuries as the third greatest cause of mortality in health institutions from 2011–2015; and called for a 50% reduction in road traffic crashes.11
Key Challenges For the Future
The situation of injuries in Zambia is framed by two fundamental issues: there is a high burden of injury-related death and disability; and a paucity of detailed information and actions addressing that high burden. Although injuries are rising in Zambia, the lack of national and disaggregated data does not allow the magnitude of the burden to be fully recognized and poses a barrier to defining risks, vulnerable groups, and the impact of potential interventions. And while there have been policies and declarations supporting the control of injuries, their implementation and success is unclear.
Zambia lacks an organized injury surveillance system or trauma registry, which makes accurate appraisal of the burden of injuries difficult.29 The current health information system is not focused on injuries, lacks centralized storage for data, has poor coverage and inadequate disaggregation of injury data by gender, socio-economic status, and geographical conditions.30 Injury data collected from external organizations is also insufficient to capture the detailed burden of injuries in Zambia. For example, the most recent World Health Organization (WHO) Global Status Report on Road Safety in which data from Zambia was presented dates back to 2015; while data from the country is missing from latest 2018 version of the report.29, 31
According to the Zambian MoH, one the major challenges deterring the effective prevention and control of injuries is the lack of human resources.30 The absence of any programs in the science of injury prevention, disability assessment, quality of life estimation, and the lifelong social and economic impact within the larger public health sector in Zambia is a serious impediment to analytic and operational work in this field. There is an immediate need to address these barriers through development of research programs in Zambia that will define the burden of injury, develop sustainable data systems, and train Zambians in injury research. Zambia must also develop models for integrated delivery of interventions for injury, establish training sites and national operational plans, and build financial and technical partnerships to support scale up activities.
We propose a number of action and research recommendations categorized into three domains: evidence, policy, and interventions (Table 3). These recommendations build on previous work and our understanding of injury in Zambia.3 It is critical that Zambia allocate resources towards systematically collecting data on injuries that can be used to inform national policy; such data should include cause-specific analysis of injuries, definition of local risk factors, and impact of different ages and genders. Developing a multi-sectoral action plan for injury prevention is important and will require assessing the current injury policy landscape and enforcing policies; like WHO’s “best buy” policies for injury prevention including Save Lives: a road safety technical package of evidence-based interventtions.29, 32
Table 3:
Recommendations for research and action on injuries in Zambia
| Selected examples | ||
|---|---|---|
| Action agenda | Research agenda | |
| Evidence |
|
|
| Policy |
|
|
| Interventions |
|
|
Zambia must use evidence-based targets to enforce and monitor the success of injury-prevention policies. For example, the UN Global Road Safety Targets are a good model and include increasing the proportion of motorcyclists who correctly use standard helmets, reducing the proportion of vehicles that travel above the speed limit, and reducing the number of injuries related to alcohol use while driving.33 These targets can be adopted and operationalized by Zambia consistent with the specific risks present in the country. WHO also recommends that a holistic approach to injury prevention be prioritized at levels of hospital care for trauma management.34
Finally, Zambia will need to expand training programs at all levels to establish a robust program that can prevent and manage injuries. Zambian professionals trained in the science of injury prevention, trauma care, and program management will need to address and respond to this burden of death and disability. For Zambia to reduce its burden of injuries, funding for research and training will be integral to the future of its national health agenda. It is for this reason that we call for a more concerted, whole of government approach to address and reduce the rising burden of death and disability from injuries in Zambia.
Highlights.
In Zambia, injuries are a major public health issue contributing to 1 in 5 premature deaths and 7% of all deaths annually.
A high burden of injury-related death and disability and a paucity of detailed information and actions addressing that high burden are two fundamental issues that frame the injury situation in Zambia.
A suggested action and research recommendations for evidence, policy, and interventions in include allocating resources towards systematically collecting data on injuries that can be used to inform national policy; using evidence-based targets to enforce and monitor the success of injury-prevention policies; expanding training programs at all levels to establish a robust program that can prevent and manage injuries.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Global Bruden of Disease 2019, Data Visualizations [Internet]. Institute for Health Metrics and Evaluation. 2021. [cited June 21, 2022]. Available from: https://vizhub.healthdata.org/gbd-compare/. [Google Scholar]
- 2.Chisumpa VH, Odimegwu CO, Saikia N. Adult mortality in sub-Saharan Africa: cross-sectional study of cuases of death in Zambia. A European Journal of Tropical Medicine and International Health. 2019;24(10):1208–20. doi: 10.1111/tmi.13302. [DOI] [PubMed] [Google Scholar]
- 3.Bukhman G, Mokumbi AO, Atun R, Becker AE, Bhutta Z, Binagwaho A, et al. The Lancet NCDI Poverty Commissin: bridging a gap in universal health coverage for the poorest billion. The Lancet. 2020;396(991–1044). doi: 10.1016/S0140-6736(20)31907-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The World Bank. End poverty in all its forms everywhere. No Poverty [Internet]. 2017 June 21, 2022. Available from: https://datatopics.worldbank.org/sdgatlas/archive/2017/SDG-01-no-poverty.html.
- 5.Ely M, West P, Sweeting H, Richards M. Teenage family life, life chances, lifestyles and health: a comparison of two contemporary cohorts. International Journal of Law, Policy and Family. 2000;14(1):1–30. doi: 10.1093/lawfam/14.1.1. [DOI] [Google Scholar]
- 6.The World Bank. The number of poor people continues to rise in Sub-Saharan Africa, despite a slow decline in the poverty rate. Published on Data Blog [Internet]. 2020 June 21, 2022. Available from: https://blogs.worldbank.org/opendata/number-poor-people-continues-rise-sub-saharan-africa-despite-slow-decline-poverty-rate.
- 7.Abdychev A, Alonso C, Alper E, Desruelle D, Kothari S, Liu Y, et al. The future of work in sub-Saharan Africa. Departmental Papers [Internet]. 2018 June 21, 2022. Available from: https://www.imf.org/en/Publications/Departmental-Papers-Policy-Papers/Issues/2018/12/14/The-Future-of-Work-in-Sub-Saharan-Africa-46333.
- 8.Bollyky TJ, Templin T, Andridge C, Dieleman JL. Between noncommunicable diseases, unhealthy lifestyles, and country wealth 2015 June 21, 2022. Available from: https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2015.0343. [DOI] [PubMed]
- 9.Sow M Figures of the week: sub-Saharan Africa’s labor market in 2017. Africa in Focus [Internet]. 2017 June 21, 2022. Available from: https://www.brookings.edu/blog/africa-in-focus/2017/01/11/figures-of-the-week-sub-saharan-africas-labor-market-in-2017/.
- 10.Bigna JJ, Noubiap JJ. The rising burden of non-communicable diseases in sub-Saharan Africa. The Lancet. 2019;7(10):E1295–E6. doi: 10.1016/S2214-109X(19)30370-5. [DOI] [PubMed] [Google Scholar]
- 11.Ministry of Health. Zambia National Health Strategic Plan 2017–2021. Ministry of Health, 2017. [Google Scholar]
- 12.Fisa R, Nakazwe C, Michelo C, Musonda P. Modelling deaths associated with road traffic accidents and other factors on Great North Road in Zambia between the years 2010 and 2016 using Poisson models. The Open Public Health Journal. 2019;12:68–77. doi: 10.2174/1874944501912010068. [DOI] [Google Scholar]
- 13.Road Transport and Safety Agency. 2019 Annual road traffic crash report. Lusaka, Zambia: Road Transport and Safety Agency, 2020. [Google Scholar]
- 14.International Labor Office. Decent work country profile: Zambiia. Geneva, Switzerland: International Labor Office, 2012. [Google Scholar]
- 15.NHA indicators [Internet]. World Health Organization. [cited June 21, 2022]. Available from: https://apps.who.int/nha/database/ViewData/Indicators/en.
- 16.Kaonga O, Banda C, Masiye F. Hardship financing of out-of-pocket payments in the context of free healthcare in Zambia. Plos One. 2019;14(4):e0214759. doi: 10.1371/journal.pone.0214750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Population Reference Bureau. 2020 World Population Data Sheet. Online: Population Reference Bureau, 2020. [Google Scholar]
- 18.Population and demographic projections 2011–2035 [Internet]. Central Statistical Office,. 2013. [cited June 21, 2022].
- 19.UNICEF. Children in Zambia June 21, 2022. Available from: https://www.unicef.org/zambia/children-zambia.
- 20.Seidenberg P, Cerwensky K, Brown RO, Hammond E, Mofu Y, Lungu J, et al. Epidemiology of injuries, outcomes, and hospital resource utilisation at a tertiary teaching hospital in Lusaka, Zambia. African Journal of Emergency Medicine. 2014;4(3):115–22. doi: 10.1016/j.afjem.2014.01.006. [DOI] [Google Scholar]
- 21.Stewart B, Gyedu A, Otupiri E, Nakua E, Boakye G, Mehta K, et al. Comparison of childhood household injuries and risk factors between urban and rural communities in Ghana: A cluster-randomized, population-based, survey to inform injury prevention research and programming. Injury. 2021;52(7):1757–11765. doi: 10.1016/j.injury.2021.04.050. [DOI] [PubMed] [Google Scholar]
- 22.Farhud DD. Impact of lifestyle on health. Iran J Public Health. 2015;44(11):1442–4. [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. Global status report on noncommunicable diseases 2014. Switzerland: World Health Organization, 2014. [DOI] [PubMed] [Google Scholar]
- 24.JEANNENEY SG, GUILLAUMONT P State fragility and economic vulnerability: what is measured and why? Workind Papers [Internet]. 2009 June 21, 2022; Ideas. Available from: https://ideas.repec.org/p/cdi/wpaper/1096.html.
- 25.Ministry of Health. Zambian Strategc Plan 2013–2016: non-communicable diseases and their risk factors. Online: World Health Organization, 2013. [Google Scholar]
- 26.World Health Organization. The Brazzaville Declaration on Non-Communicable Diseases Prevention and Control in the WHO African Region. Online: World Health Organization, 2011. [Google Scholar]
- 27.Ministry of Health. National health in all policies strategic framework. Lusaka, Zambia: Ministry of Health of Zambia, 2018. [Google Scholar]
- 28.Commission TLNP. Bridging a gap in universal health coverage for the poorest billion Online2022 [cited 2022 June 21]. Available from: http://www.ncdipoverty.org/about.
- 29.World Health Organization. Global status report on road safety 2015. Geneva, Switzerland: World Health Organization, 2016. [Google Scholar]
- 30.Ministry of Health. Assessment of the health information system in Zambia. Online: Ministry of Health, Republic of Zambia, 2007. [Google Scholar]
- 31.World Health Organization. Global Status Report on Road Safety. Geneva, Switzerland: World Health Organization, 2018. [Google Scholar]
- 32.World Health Organization. Save lives: a road safety technical package. Geneva, Switzerland: World Health Organization, 2017. [Google Scholar]
- 33.World Health Organization. Global Road Safety Performance Targets. Online: World Health Organization, 2017. [Google Scholar]
- 34.World Health Organization. Guidelines for essential trauma care. Online: World Health Organization, 2012. [Google Scholar]
- 35.National Assembly of Zambia. The Firearms Act. Online: National Assembly of Zambia, 1994. [Google Scholar]
- 36.Road Transport and Safety Agency. About Online 2022. [cited 2022 June 21]. Available from: https://www.rtsa.org.zm/about-us/about-rtsa/.
- 37.Republic of Zambia. Vision 2030: “A prosperous middle-income nation by 2030”. Online: 2006.
- 38.International Labour Organization. Zambia occupational safety act, 2010. Online: 2010.
- 39.The Lancet Commission on Global Surgery. The Commission Process Online: The Lancet; 2015. [cited 2022 June 2021]. Available from: https://www.lancetglobalsurgery.org/background.


