Abstract
Background
There is growing interest in incorporating social determinants of health (SDoH) data collection in inpatient hospital settings to inform patient care. However, there is limited information on this data collection and its use in inpatient general internal medicine (GIM). This scoping review sought to describe the current state of the literature on SDoH data collection and its application to patient care in inpatient GIM settings.
Methods
English-language searches on MedLine, Embase, Web of Science, CINAHL, Cochrane, and PsycINFO were conducted from 2000 to April 2021. Studies reporting systematic data collection or use of at least three SDoH, sociodemographic, or social needs variables in inpatient hospital GIM settings were included. Four independent reviewers screened abstracts, and two reviewers screened full-text articles.
Results
A total of 8190 articles underwent abstract screening and eight were included. A range of SDoH tools were used, such as THRIVE, PRAPARE, WHO-Quality of Life, Measuring Health Equity, and a biopsychosocial framework. The most common SDoH were food security or malnutrition (n=7), followed by housing, transportation, employment, education, income, functional status and disability, and social support (n=5 each). Four of the eight studies applied the data to inform patient care, and three provided community resource referrals.
Discussion
There is limited evidence to guide the collection and use of SDoH data in inpatient GIM settings. This review highlights the need for integrated care, the role of the electronic health record, and social history taking, all of which may benefit from more robust SDoH data collection. Future research should examine the feasibility and acceptability of SDoH integration in inpatient GIM settings.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07937-z.
KEY WORDS: social determinants of health, social needs, sociodemographic, social medicine, social history, general internal medicine, screening tools, scoping review
INTRODUCTION
There is growing interest in integrating data collection on the social determinants of health (SDoH) — our daily living and working conditions, including income, race, and disability — into medical practice.1–4 SDoH and behaviors contribute to approximately 80% of health outcomes5 and influence quality of life.6, 7 Socioeconomic determinants have been associated with hospital length of stay,8 healthcare utilization,9 and hospital readmission.10–12 SDoH data collection in healthcare settings facilitates patient-centered care and identifies health inequities, which can inform health system changes and patient outcomes.1, 2, 4, 13
Compared to primary care,14 inpatient hospital settings have not routinely integrated SDoH data collection or interventions.15, 16 Instead, data collection in hospitals has typically been for research purposes, to understand associations or predictions between determinants and conditions or healthcare utilization.17, 18 There is less knowledge on SDoH data collection efforts and interventions in general internal medicine (GIM), a high-volume, high-complexity service — especially in safety net hospitals.19 Although physicians are encouraged to conduct a comprehensive social history of their patients using a patient-centered care approach, this is often inadequate20–22 due to inconsistent training, and taking an in-depth history is time consuming.23–25 While social medicine curriculum in internal medicine is focused on understanding the social context of patient care, it has not been widely developed or adopted.26
The National Academy of Medicine recommended the systematic collection of SDoH information across healthcare settings.27 In 2020, the Society of General Internal Medicine called for internists to identify health inequities and understand patients’ SDoH.28 To our knowledge, there has yet to be a review of SDoH data collection and its application during GIM hospitalization. Given this knowledge gap and the potential for SDoH data collection to improve health systems, clinical decision-making, and patient outcomes, this study sought to describe the state of the literature on SDoH data collection and its application to patient care in hospitalized GIM settings.
METHODS
This scoping review was conducted using the five main stages of Arksey and O’Malley’s methodological framework: research question formulation, identifying studies, selecting studies, data charting, and organizing, summarizing, and presenting the results.29 The Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guided the reporting.30 The definition of SDoH encompassed seventeen determinants identified in Social Determinants of Health: The Canadian Facts.31 SDoH use was defined as the application of patient-level SDoH data to inform care, either indirectly or directly through individual- or hospital-level initiatives, as opposed to the application of population-level data. This definition captured studies describing patient-level initiatives (e.g., community resource referrals, social worker, navigator, social programs), including studies where data was used for discharge planning, tailored treatment, or organizational- and changes (e.g., funding allocation, staff hiring and training) aligned with more equitable care provision. Importantly, this included the provision of resources or in-hospital services for unmet social needs assessed on an individual basis.
Data Sources and Searches
The Population-Concept-Context mnemonic was used to design the inclusion criteria by considering the population of interest, the concept of investigation, and the context (Appendix 1).32 The search strategy was developed and conducted by a research librarian (Appendix 2). Databases queried for English-language publications between 2000 and April 2021 included the following: MedLine, Embase, Web of Science, CINAHL, Cochrane, and PsycINFO. Searches were conducted from April 4 to 14, 2021.
Study Selection
Articles were managed using Covidence software.33 Title screening and abstract screening were performed by four independent screeners who completed a calibration exercise to ensure consistency. Articles underwent full-text review by two authors (VHD, LR) and disagreements were resolved by a third reviewer or meeting.
Articles were included if they reported the collection and/or use of SDoH, sociodemographic, or social needs data in hospital GIM settings. These terms were selected as they overlap in the literature. Studies described the systematic collection of SDoH information as opposed to collecting information through the social history, given that the social history is inconsistently conducted. SDoH data collection was considered to be a precursor to SDoH data use — thus, data collection was the focus of the search strategy. Search terms related to data use were not included as it would have needlessly restricted the search. Articles specifically related to data use were excluded if they solely applied the information to make predictions or examine associations with medical outcomes.
Peer-reviewed journal articles, conference proceedings, or abstracts reporting primary source data were included. Abstracts and proceedings were included given the expectation that few articles would meet inclusion criteria. Exclusion criteria included the following: not patient-level data collection; sole focus on data to predict or describe an association with a medical outcome; unspecified data collection method; or less than three SDoH, social needs, or sociodemographic variables collected. This requirement ensured that studies reported a more comprehensive social background. When the hospital setting was unclear or the data was not stratified by GIM in the article, the corresponding authors were contacted for clarification.
A standardized data extraction form was created in Excel, and two authors (VHD, LR) independently extracted each article to ensure consistency and accuracy. Extracted data included objectives; methods; intervention details (if applicable); results; method of data collection; SDoH, social needs, and sociodemographic variables collected; the use of collected data; and barriers to data collection.
Data Synthesis and Analysis
Data was combined by narrative synthesis due to the heterogeneity of included articles. The focus was on SDoH collected, the tools used, the purpose of the data collection, and data use.
RESULTS
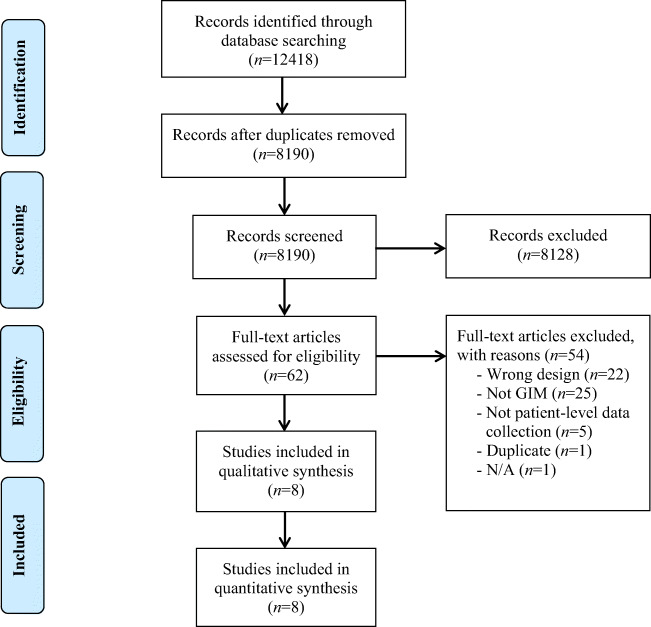
The search yielded 12,418 results (including duplicates), and 8190 articles underwent abstract and title screening (Fig. 1). Of these, 8128 articles were excluded, leaving 62 articles for full-text screening. Fifty-four studies were excluded, resulting in eight studies meeting inclusion criteria. Reasons for full-text exclusion included the following: setting outside of GIM or results were not stratified by GIM (n=25, 40%); sole focus on SDoH information for predictions or associations with medical outcomes (n=22, 35%); not patient-level data collection (n=5, 8%); and an additional duplicate and a not applicable study (n=1, 2% each).
Figure 1.
PRISMA diagram. Adapted from Tricco et al.30
Context, Aims, and Results
There were two case series, three quasi-experimental, and one of each: a mixed methods, cohort, and cross-sectional study (Table 1). The studies had diverse objectives: curriculum development, quality improvement, description, program evaluation, and understanding the prevalence or impacts of SDoH data. Most studies were in North America (n=5), and Italy, Tunisia, and Turkey (all n=1). Data was verbally collected by medical students (n=2); trained research staff (n=1); or unspecified (n=5).
Table 1.
Characteristics of Included Studies (N=8)
| Study, year (reference) | Country | Population | Participants, N | Design | Objectives | Findings | Relevant tools or frameworks |
|---|---|---|---|---|---|---|---|
| Parunyan et al. 202034 | USA | Third year medical students | 158; 41 finished surveys | Quasi-experimental mixed methods; quality improvement | Assess intervention on students’ knowledge and skills with screening and referral tools |
- Improved confidence in giving resources (p<.001) - 63% used resource directory - Meaningful to have access to screening and resources; should not only be required from students - Inpatient setting is too difficult/busy for screening - Challenges using EHR technology for resources - Unequipped to recommend resources |
THRIVE |
| Salma et al. 201648 | Tunisia | Sixty-five years and older; Average age 73.5 ± 6.6 years | 60 | Case series | Report on the nutrition and activity in daily living among elderly inpatients |
- Most were middle class - 18% lived alone; 18% had social and family issues - 73% were vulnerable or exposed to malnutrition - 13% were functionally dependent |
MNA-SF, ADL of KATZ, SDoH tool not listed |
| Bui et al. 202037 | USA | Patients at high risk for readmissions, living in low-income postal codes; 76% were black, 55% female | 187 | Quasi-experimental; quality improvement | Implement SDoH screening program to reduce readmissions and enhance primary care transitions. To learn about barriers to community referrals. |
- Food security was often addressed - More challenges with addressing utility bill payments, home and caregiving support - Food insecurity was reported to have a decreased readmission rate from 38% to 27% after intervention - Increase in primary care provider follow-up visits from 22% to 35% |
PRAPARE |
| Yaman et al. 200346 | Turkey | Hospitalized adult patients; mean (±SD) age: 41±17 years, 62% women | 99 | Case series | Describe health-related QOL among inpatients |
- Low QOL, particularly among women - Association between QOL and social relationships and environment (p<.05), and physical health, independence, psychological well-being (p<.001) |
WHOQOL |
| Nardi et al. 200751 | Italy | DHD patients in a medium size country hospital, mean age: 82 | 99 | Cross-sectional | Understand the prevalence of DHD, report clinical and social background of patients, provide targeted post-discharge assistance |
- DHD represented 5.4% of annual patient admissions - 95% lacked family support - 24% experienced malnutrition - 58% lacked autonomy in daily living - 80% had functional and/or cognitive challenges |
BINA index, SDoH tool not listed |
| Williams et al. 201945 | USA | Fourth year medical students | 38 intervention notes and 24 control notes | Quasi-experimental | Assess if framework assisted students with non-biomedical history taking, and whether it is viewed as applicable or allow social factors to be intervened on |
- Intervention group had more biopsychosocial information domains excluding behavioral health (p≤.001) - Reported enhanced team-based care and recognition of SDoH information that could be assisted with the provision of interdisciplinary team and resources |
Six-domain biopsychosocial framework |
| Smith et al. 201743 | Canada | Patients discharged from large teaching hospital, median age: 67 (IQR 50–81), female (54%), and white (69%) | 1427 | Prospective cohort | Understand sociodemographic relationship with 30-day readmissions |
- 46% did not want to disclose or did not know their income - Most frequently reported income was below CAD$20,000 (14%) - 80% were comfortable speaking with healthcare team in English - 57% had post-secondary schooling - 14% had 30-day readmissions; sociodemographics were not associated with readmissions |
Measuring Health Equity |
| Kearney et al. 202035 | USA | COPD patients in urban safety-net hospital | 51 | Mixed methods | To examine SDoH challenges among COPD patients and barriers to self-management |
- 86% had at least one social need; of those, 71% desired help, particularly with transportation to medical appointments, housing, food, and mental health - SDoH were barriers to managing COPD symptoms |
THRIVE |
MNA-SF, Mini Nutritional Assessment short-form; ADL, Activities of Daily Living; PRAPARE, Protocol for Responding to and Assessing Patients’ Risks, Assets, and Experiences; WHOQOL, World Health Organization Quality of Life; DHD, difficult hospital discharges; BINA, Breve Indice della Non Autosufficienza.
SDoH Collected and Screening Tools
The most common SDoH was food security or malnutrition (n=7), and five different studies collected housing, transportation, employment, functional status or disabilities, social support, education and income (Table 2). The authors did not comment on operational challenges or other experiences using their screening tools.
Table 2.
SDoH Variables Collected Across Included Studies (N=8)
| Parunyan et al., 202034 and Kearney et al., 202035 | Salma et al., 201648 | Bui et al., 202037 | Yaman et al., 200346 | Nardi et al., 200751 | Williams et al., 201945 | Smith et al., 201743 | |||
|---|---|---|---|---|---|---|---|---|---|
| Key areas | Variables | THRIVE | MNA-SF, ADL of KATZ; SDoH tool not listed | PRAPARE | WHOQOL | BINA; SDoH tool not listed | Six-Domain Biopsychosocial Framework | Measuring Health Equity | Total Count |
| Sociodemographic Variables | Household living status | X | X | X | X | 4 | |||
| Marriage status | X | X | X | 3 | |||||
| Gender | X | X | X | 3 | |||||
| Race and ethnicity | X | X | 2 | ||||||
| Spirituality or religion | X | X | 2 | ||||||
| Refugee status | X | 1 | |||||||
| Birth location | X | 1 | |||||||
| Farmworker status | X | 1 | |||||||
| Veteran status | X | 1 | |||||||
| Sexual orientation | X | 1 | |||||||
| Economic stability | Food insecurity or malnutrition | 2X | X | X | X | X | X | 7 | |
| Employment or employment capacity | 2X | X | X | X | 5 | ||||
| SES or income | X | X | X | X | X | 5 | |||
| Housing instability | 2X | X | X | X | 5 | ||||
| Transportation (medical and/or other) | 2X | X | X | X | 5 | ||||
| Ability to afford utility bills | 2X | X | 3 | ||||||
| Education | Education or educational needs | 2X | X | X | X | 5 | |||
| Language | X | X | 2 | ||||||
| Social and community context | Social support and relationships | X | X | X | X | X | 5 | ||
| Fear of partner, physical and/or emotional safety | X | X | X | 3 | |||||
| Care for a child, elder, or person living with disabilities | 2X | 2 | |||||||
| History of incarceration | X | 1 | |||||||
| Health and healthcare | Ability to afford medications | 2X | X | X | 4 | ||||
| Insurance status | X | X | 2 | ||||||
| Health and social care accessibility and quality | X | X | 2 | ||||||
| Health literacy | X | 1 | |||||||
| Neighborhood and built environment | Access to recreation or safe exercise community | X | 1 | ||||||
| Disability and physical status | Functional status, disabilities, or activities of daily living | X | X | X | X | X | 5 |
Underlined X indicates optional category.
MNA-SF, Mini Nutritional Assessment short-form; ADL, Activities of Daily Living; PRAPARE, Protocol for Responding to and Assessing Patients’ Risks, Assets, and Experiences; WHOQOL, World Health Organization Quality of Life; DHD, difficult hospital discharges; BINA, Breve Indice della Non Autosufficienza; SES, socioeconomic status.
THRIVE
Two studies used the THRIVE screening and resource referral tool.34, 35 One study also included alcohol/drug use and stress/depression.35 THRIVE was created by the Boston Medical Center (BMC) as an electronic health record (EHR) method of screening and addressing needs and has been implemented in all of BMC’s ambulatory primary care clinics.39, 46–48
Eight common SDoH areas are covered by 11 questions in the THRIVE tool.36 The tool asks patients which areas they want assistance with.36 The questions were adapted from validated tools in ambulatory settings (e.g., WE CARE).36
Protocol for Responding to and Assessing Patients’ Risks, Assets, and Experiences (PRAPARE)
A study used PRAPARE,37 which was developed by the National Association of Community Health Centers, Association of Asian Pacific Community Health Organizations, and the Oregon Primary Care Association for screening in community health centers.38 PRAPARE has been implemented in 36% of US Medicaid-managed health centers.39 Similar to THRIVE, PRAPARE is integrated into the EHR.40 PRAPARE is a more comprehensive screening tool that covers 17 sociodemographic and social needs questions and four optional questions.40 PRAPARE has undergone some psychometric testing.41, 42
Measuring Health Equity Survey
One study examined 13 sociodemographic variables from the Measuring Health Equity survey.43 Patients were surveyed by trained researchers and staff.43 Surveys were translated in 11 languages and interpreters helped collect data for non-English-speaking populations.43 The survey was developed by the Toronto Central Local Health Integration Network and other healthcare organizations based on expert consultations and has not undergone psychometric testing.44
Six-Domain Biopsychosocial Framework
One study did not have a set of mandatory SDoH questions; rather, medical students asked a question from each of six key domains.45 The domains were identified from the authors’ experience using and reviewing assessments and clinical models, and categories in the Diagnostic and Statistical Manual of Mental Disorders.45
World Health Organization Quality of Life (WHOQOL)
One study used the WHOQOL-100 assessment, which has undergone psychometric testing across multiple countries.46, 47 The study used the Turkish version with 103 items over seven SDoH areas.46 Sociodemographic variables were also included.46
Other Tools and Variables
Other studies did not specify the survey used for some or all SDoH variables. A study collected socioeconomic status, marriage status, living status, age, gender, social and family challenges, functional status, and malnutrition.48 Malnutrition was measured by the Mini-Nutritional Assessment - Short Form (MNI-SF), which has been assessed for validity,49 similar to the Katz Activities of Daily Living (ADL) which measures disability and functional status.48, 50
Another study used multiple tools to assess difficult hospital discharge: an assessment for dependency and functional capacity using the Breve Indice della Non Autosufficienza (BINA) tool, including patients’ social support, medical needs, and communication abilities; Short Portable Mental Status Questionnaire; nursing complexity; and SDoH, the questions and tools not explicitly mentioned other than by “exploring patient’s and his/her family characteristics”.51 Due to language barriers, the psychometric properties of BINA were not assessed.
Application of SDoH Data to Patient Care
Four studies applied the data to inform care. Three studies provided patients with information or interprofessional assistance for their needs.34, 37, 45 One used the THRIVE web-based directory equipped with a search engine to help providers find resources for patients.34 Most medical students found it was simple to navigate the directory (51%), search for resources (61%), and input patients THRIVE information into the EHR (63%).34
An American study trained volunteer college students as part of the Social Needs Action Program (SNAP) to provide referrals to patients for their social needs upon discharge.37 The SNAP physician and volunteers met weekly to follow-up on patients until their needs were met.37 For patients that qualified as high risk for readmission, volunteers would go to their home and assist with booking appointments.37
Another study involved an intervention on biopsychosocial history taking.45 Medical students contacted social workers, care managers, pharmacists, and/or nurses to discuss barriers to care, resources to assist with care planning and to address behavioral and social needs.45 Some students reported that the intervention helped to identify high-risk patients and increased their understanding of their patient and patient needs.45
Lastly, one study focused on difficult hospital discharges and used comprehensive medical and social assessments to provide tailored sheltered discharge and linkages to essential community services and supports.51 However, the authors do not describe whether these supports aimed to improve their social and economic conditions or to fill a gap in facilitating sheltered discharge.51
DISCUSSION
SDoH Categories
Included studies focused on a limited number of SDoH. Food security was most frequently reported, followed by housing, transportation, employment, social support, education, socioeconomic level or income, and functional status or disability. These results are supported by a technical report of 106 studies across healthcare settings, which found food security was most often screened, then finances, housing, and transportation.42 This indicates a focus on material determinants, compared to other sociodemographic characteristics such as race. While race-based data collection can inform anti-racist reforms and interventions to address inequities,52 this data collection is less applicable in shorter-term outcome periods and more relevant to larger-scale data collection efforts to inform systemic change.
SDoH Screening Tools
There were a variety of screening tools, which is consistent with a review which recommended that clinicians choose a tool and adapt it to their local context, population, and needs.53 This approach may be better suited for individual, secondary prevention efforts, but is insufficient for larger-scale, systematic initiatives which benefit from standardized, reliable, and validated tools and methods to compare outcomes across health systems to inform policy efforts and resource allocation. At an individual-level, social history taking would accomplish similar data collection to a standardized tool;24 however, conducting the social history can vary depending on the setting and skill of the provider.20, 25
Primary literature demonstrates a paucity of psychometric evidence of tools across the healthcare settings where the tools were developed.54–57 Psychometric evaluation is important to inform decisions on implementing tools for a particular population and setting, and resource allocation for providing social needs assistance.54 However, exclusive focus on using such tools may be unnecessarily labor-intensive. The basics of a clinical assessment and art of a patient interview may accomplish similar data collection as part of the clinical assessment, where interactions between patients and providers can facilitate a therapeutic relationship aligned with a patient-centered care approach.21
Method of SDoH Data Collection
This review identified limited information describing data collection methods. Three of eight studies specified which personnel administered tools, and two reported the method of administration. Data collection methods have important implications for patients’ willingness to disclose information. Patients across a variety of settings have reported concerns about the implications of this data collection, including fear of discrimination, stigma, and changes to their care.1, 3, 58, 59 Concerns may vary depending on the relationship between provider and patient (i.e., primary care versus hospital internist), which emphasizes the importance of a patient-centered approach to screening and addressing needs. Transparency, data ownership, privacy, and culturally sensitive data collection are needed to promote screening in a safe manner.58 Patients may also question the hospital setting for this data collection. For example, in a survey of public opinion of sociodemographic data collection in Ontario, Canada, only 49% of participants agreed that it was important for hospitals to collect this information.60
An alternative approach involves dedicated staff to screen and address unmet social needs. A study found that 65% of physicians believe that population health teams should assist providers with addressing social needs.63 There are notable examples of this approach. Kaiser Permanente Southern California used Health Leads — a screening tool and hub that partners with communities and health systems to meet social needs — in a large-scale intervention.9 Dedicated program associates conducted social needs screening by telephone and provided navigation by explaining social resources information.9 Similarly, SNAP screening involved community helpers from a program modeled after Health Leads instead of solely relying on physicians.37
Data collection initiatives in primary care have similar themes to this review. In an evaluation of screening implementation in primary care, some recommended best practices included the following: ensure the screening tool is appropriate in terms of literacy, culture, and language; integrate screening into clinic workflows; make screening universal; implement a data-tracking system; and staff the program appropriately.61 Similar implementation barriers have been identified; however, the integration of social medicine and emphasis on holistic and social care in primary care settings means awareness and screening are likely more acceptable than inpatient settings.61, 62 This may be reflected by differences in the experiences and training between various specialist physicians (e.g., surgical, medicine, neurology) and primary care physicians. For example, 78% of primary care physicians believe that SDoH screening is worth the risks, compared to 54% of specialists (p < 0.01).63
Overall, experience in ambulatory settings could be leveraged to develop models for inpatient GIM, as there are often many health providers, in addition to social workers, already involved in patient care. Further, with the evolution of EMRs, providers may have an opportunity to integrate screening into a social history that is directly entered in the EHR. For example, one study in this review reported that most medical residents felt it was easy to input the THRIVE tool into EPIC.34 This way, data collection is integrated as part of the social history as opposed to a separate activity. Tools could complement this process by providing a framework to speak with patients about their social history in a patient-centered manner, as it has been suggested that health systems should identify and prioritize systematic implementation of collection of social variables in the EHR.64
As in most settings, there is a need for interdisciplinary collaboration, education, and training. In addition to ensuring staff with expertise in social services are involved in patient care so that needs are actionable, there are health system issues to consider. For example, if data is collected in primary care, documented in an EHR, and available to acute care providers, there would not be a need for data collection in hospital settings. However, some patients rely on acute care in the absence of having a primary care provider, and there are important demographic differences in populations with and without access to primary care.65, 66 Individuals without a primary care provider may be more likely to have significant social needs, meaning data collection in GIM remains important.65, 67
Applying SDoH Data Collection to Patient Care
Four of the eight studies applied the data to inform patient care. Five did not report efforts to assist patients with their needs through resource referrals. There remain gaps in identifying needs and providing patient-centered, holistic care for high needs populations. Effective screening for SDoH in practice should involve interventions or resources to assist patients with identified needs, and tools should be chosen based on organizational capacity to address patients’ needs in those specific domains.68
However, as above, there are many barriers to screening and addressing needs. Additional challenges include limited financial resources and infrastructure, feeling overworked, lack of training and knowledge of resources, and lack of confidence to approach patients.24, 53, 69–71 For example, medical students expressed feeling unprepared to counsel patients on resources, and felt that GIM was not the most appropriate setting to conduct SDoH screening.34 Similarly, one study reported that a greater number of specialists believe that primary care physicians should be solely in charge of addressing social needs, compared to primary care physicians themselves (p < 0.01).63
More research is needed to understand how to best use and collect SDoH data in inpatient GIM. Despite the importance and impact on healthcare utilization,69–71 SDoH may not be appreciated at the provider or population level, or explicitly linked to internal medicine among physicians and trainees. This may reflect a lack of training in medical school and residency,72–74 and medical education may have a role in developing data collection practices, whether in screening programs or social history taking.24 Based on a social medicine framework, there is a need for clinician reflection and training to improve comprehensive social history taking, as well as revision of medical education curricula and trainee experiences.24 This illustrates the importance of systemic changes in attitudes and training for providers to be successful in SDoH data collection in the context of an inclusive social history.
This study has a few strengths. It adopted a highly robust search strategy to capture a range of studies, due to the complexity and specificity of the target GIM setting and patient-level data on at least three SDoH, social needs and sociodemographic data variables. Additionally, the search extended beyond North America to include international perspectives. To our knowledge, this is the first review that examines SDoH data collection and use in inpatient GIM settings. This review identifies gaps in the literature, despite increasing interest in this area and in social medicine overall.
There are also limitations. Only English language articles were included, which may have limited the generalizability of the findings. This review describe studies and abstracts with relatively few participants. Therefore, the findings of this review should be considered exploratory and intended for hypothesis generation.
CONCLUSIONS
This scoping review found that a limited number of studies reported the collection and use of SDoH data in inpatient GIM settings. Further, there were variable tools and methods to collect these determinants. If there is a movement toward systematic data collection, psychometric testing of SDoH tools in inpatient GIM settings is important, especially for integration into an EHR. However, psychometric testing may not be necessary for providing individual-level support, particularly information that is elicited in a patient-centered social history. This review highlights the need for integrated care, the role of the EHR, and the practice of social history taking, all of which may benefit from more robust SDoH data collection. Future research should examine the feasibility and acceptability of SDoH integration in inpatient GIM settings, including the use of screening tools versus a patient-centered, comprehensive social history alongside social medicine.
Supplementary Information
(DOCX 38.3 kb)
Acknowledgements
We would like to sincerely thank Carolyn Ziegler, MA, MISt, Information Specialist, Library Services, Unity Health Toronto, for devising the search strategy with our team and executing the search. We thank David Lightfoot for providing a peer review of the Medline search according to the CADTH PRESS checklist. We also thank Tarnbir Aulakh and Thiyaana Jeyabalan for their help in screening abstracts and titles for this study. We are grateful to Drs. Irfan Dhalla, Katie Dainty and Kathleen Sheehan for their feedback on the manuscript.
Funding
There was no external funding for this scoping review. The corresponding author’s (Victoria Davis) graduate funding was contributed by the Canadian Institutes of Health Research (CIHR) and Ontario Graduate Scholarship.
Declarations
Conflict of Interest
The authors do not have any conflicts of interest to report.
Footnotes
Prior Presentations
An abstract was accepted for an oral presentation at the 2022 Annual Meeting of the Society of General Medicine but was not published in the conference proceedings due to an inability to attend the conference. The initial submission of this article is included in part of Victoria Davis’ thesis, which will be publicly released in 2024.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lofters AK, Shankardass K, Kirst M, Quiñonez C. Sociodemographic data collection in healthcare settings: an examination of public opinions. Med Care. 2011;49(2):193–9. doi: 10.1097/MLR.0b013e3181f81edb. [DOI] [PubMed] [Google Scholar]
- 2.Moscrop A, Ziebland S, Roberts N, Papanikitas A. A systematic review of reasons for and against asking patients about their socioeconomic contexts. Int J Equity Health. 2019;18(1):112. doi: 10.1186/s12939-019-1014-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pinto AD, Glattstein-Young G, Mohamed A, Bloch G, Leung FH, Glazier RH. Building a foundation to reduce health inequities: routine collection of sociodemographic data in primary care. J Am Board Fam Med. 2016;29(3):348–55. doi: 10.3122/jabfm.2016.03.150280. [DOI] [PubMed] [Google Scholar]
- 4.Williams-Roberts H, Neudorf C, Abonyi S, Cushon J, Muhajarine N. Facilitators and barriers of sociodemographic data collection in Canadian health care settings: a multisite case study evaluation. Int J Equity Health. 2018;17(1):186. doi: 10.1186/s12939-018-0903-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hood CM, Gennuso KP, Swain GR, Catlin BB. County health rankings: relationships between determinant factors and health outcomes. Am J Preventive Med. 2016;50(2):129–35. doi: 10.1016/j.amepre.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 6.Kivits J, Erpelding ML, Guillemin F. Social determinants of health-related quality of life. Revue d’Épidémiologie et de Santé Publique. 2013;61:S189–94. doi: 10.1016/j.respe.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Gu Y, Zhang H, Ali SH, Huang M, Wei J, Gu S, et al. Social determinants of health-related quality of life among residents in Zhejiang and Qinghai, China. Int J Environ Res Public Health. 2019;16(8):1314. doi: 10.3390/ijerph16081314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coindre JP, Crochette R, Breuer C, Piccoli GB. Why are hospitalisations too long? A simple checklist for identifying the main social barriers to hospital discharge from a nephrology ward. BMC Nephrol. 2018;19(1):227. doi: 10.1186/s12882-018-1023-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schickedanz A, Sharp A, Hu YR, Shah NR, Adams JL, Francis D, et al. Impact of social needs navigation on utilization among high utilizers in a large integrated health system: a quasi-experimental study. J Gen Intern Med. 2019;34(11):2382–9. doi: 10.1007/s11606-019-05123-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meddings J, Reichert H, Smith SN, Iwashyna TJ, Langa KM, Hofer TP, et al. The impact of disability and social determinants of health on condition-specific readmissions beyond Medicare risk adjustments: a cohort study. J Gen Intern Med. 2017;32(1):71–80. doi: 10.1007/s11606-016-3869-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nagasako Em, M R, B W, Dunagan WC. Adding socioeconomic data to hospital readmissions calculations may produce more useful results. Health Aff (Millwood). 2014;33(5):786–91. [DOI] [PMC free article] [PubMed]
- 12.Nnadozie Emechebe MPH, Pamme Lyons Taylor MBA, Oluyemisi Amoda MHA, Zachary Pruitt P. Passive social health surveillance and inpatient readmissions. Am J Manag Care. 2019;25(8):388–95. [PubMed]
- 13.Andermann A. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ. 2016;188(17–18):E474–83. doi: 10.1503/cmaj.160177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGregor J, Mercer SW, Harris FM. Health benefits of primary care social work for adults with complex health and social needs: a systematic review. Health Social Care Comm. 2018;26(1):1–13. doi: 10.1111/hsc.12337. [DOI] [PubMed] [Google Scholar]
- 15.Freij M, Dullabh P, Lewis S, Smith SR, Hovey L, Dhopeshwarkar R. Incorporating Social Determinants of Health in Electronic Health Records: Qualitative Study of Current Practices Among Top Vendors. JMIR Med Inform. 2019;7(2):e13849. [DOI] [PMC free article] [PubMed]
- 16.Truong HP, Luke AA, Hammond G, Wadhera RK, Reidhead M, Joynt Maddox KE. Utilization of social determinants of health ICD-10 Z-Codes among hospitalized patients in the United States, 2016-2017. Med Care. 2020;58(12):1037–43. doi: 10.1097/MLR.0000000000001418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Int Med. 2016;176(10):1501–9. doi: 10.1001/jamainternmed.2016.4419. [DOI] [PubMed] [Google Scholar]
- 18.Wang A, Pridham KF, Nisenbaum R, Pedersen C, Brown R, Hwang SW. Factors associated with readmission among general internal medicine patients experiencing homelessness. J Gen Intern Med. 2021;36(7):1944–50. doi: 10.1007/s11606-020-06483-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verma AA, Guo Y, Kwan JL, Lapointe-Shaw L, Rawal S, Tang T, et al. Patient characteristics, resource use and outcomes associated with general internal medicine hospital care: the General Medicine Inpatient Initiative (GEMINI) retrospective cohort study. CMAJO. 2017;5(4):E842–9. doi: 10.9778/cmajo.20170097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walsh C, Elhadad N. Modeling clinical context: rediscovering the social history and evaluating language from the clinic to the wards. AMIA Jt Summits Transl Sci Proc. 2014;2014:224–31. [PMC free article] [PubMed] [Google Scholar]
- 21.Wu BJ. History Taking in reverse: beginning with the social history. Consultant360. 2013;53(1).
- 22.Anderson R, Schiedermayer D. The social history matters! Acad Med. 2010;85(7):1103. doi: 10.1097/ACM.0b013e3181e19330. [DOI] [PubMed] [Google Scholar]
- 23.Srivastava R. Complicated lives — taking the social history. New England J Med. 2011;365(7):587–9. doi: 10.1056/NEJMp1106985. [DOI] [PubMed] [Google Scholar]
- 24.Behforouz HL, Drain PK, Rhatigan JJ. Rethinking the social history. New Engl J Med. 2014;371(14):1277–9. [DOI] [PubMed]
- 25.Alrasheedi AA. Deficits in history taking skills among final year medical students in a family medicine course: a study from KSA. J Taibah Univ Med Sci. 2018;13(5):415–21. doi: 10.1016/j.jtumed.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bradley J, Styren D, LaPlante A, Howe J, Craig SR, Cohen E. Healing through history: a qualitative evaluation of a social medicine consultation curriculum for internal medicine residents. BMC Med Educ. 2021;21(1):95. [DOI] [PMC free article] [PubMed]
- 27.NASEM. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington (DC): National Academies Press (US); 2015. [PubMed]
- 28.Byhoff E, Kangovi S, Berkowitz SA, DeCamp M, Dzeng E, Earnest M, et al. A society of general internal medicine position statement on the internists’ role in social determinants of health. J Gen Intern Med. 2020;35(9):2721–7. doi: 10.1007/s11606-020-05934-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32.
- 30.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. [DOI] [PubMed]
- 31.Raphael D, Bryant T, Mikkonen J, Raphael A. Social Determinants of Health: The Canadian Facts. 2nd ed. Ontario Tech University Faculty of Health Sciences and York University School of Health Policy and Management; 2020.
- 32.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–26. doi: 10.11124/JBIES-20-00167. [DOI] [PubMed] [Google Scholar]
- 33.Covidence Systematic Review Software. Veritas Health Innovation, Melbourne, Australia. Available at: https://www.covidence.org. Accessed June 9, 2019.
- 34.Parunyan M, Hollander L, Hong H, Sylvester D, Desphande J, Eyllon M, et al. Improving medical students’ skills to address social determinants of health during the internal medicine clerkship. J Health Care Poor Underserved. 2020;31(5):286–305. doi: 10.1353/hpu.2020.0154. [DOI] [PubMed] [Google Scholar]
- 35.Kearney L, Wiener RS, Dahodwala M, Fix G, Drainoni ML, Hicks J, et al. Assessing social determinants of health that are barriers to self-management in COPD patients hospitalized at a large safety-net hospital. Am Thoracic Soc. 2020;201:A4286.
- 36.Buitron de la Vega P, Losi S, Sprague Martinez L, Bovell-Ammon A, Garg A, James T, et al. Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Medical Care. 2019;57:S133. [DOI] [PubMed]
- 37.Bui T, George L, Bowersox M, Hawk M. Hospital-based initiatives to address unmet social needs of high-risk patients. J Gen Int Med. 2020;35(Supplement 1).
- 38.National Association of Community Health Centers, Association of Asian Pacific Community Health Organizations. Who We Are. PRAPARE. Available at: https://prapare.org/who-we-are/. Accessed January 2, 2022.
- 39.Moore J, Adams C, Tuck, K. Medicaid Access & Coverage to Care in 2018. Institute for Medicaid Innovation. 2019. Available at: https://www.medicaidinnovation.org/_images/content/2019_Annual_Medicaid_MCO_Survey_Results_FINAL.pdf. Accessed June 2, 2020.
- 40.National Association of Community Health Centers, Association of Asian Pacific Community Health Organizations, Oregon Primary Care Association. PRAPARE Implementation and Action Toolkit. 2019. Available at: https://www.nachc.org/research-and-data/prapare/toolkit/. Accessed June 16, 2019.
- 41.National Association of Community Health Centers, Association of Asian Pacific Community Health Organizations, Oregon Primary Care Association. PRAPARE Validation Using 8 “Gold Standard” Stages of Measure Development. 2019. Available at: https://aapcho.org/wp-content/uploads/2021/02/prapare_validation-fact-sheet-2019-9-26.pdf. Accessed June 16, 2020.
- 42.Eder M, Henninger M, Durbin S, Iacocca M, Martin A, Gottlieb LM, et al. Screening and Interventions for Social Risk Factors: A Technical Brief to Support the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality. 2021;299. Report No.: AHRQ Publication No. 20-05267-EF-1.
- 43.Smith RW, Kuluski K, Costa AP, Sinha SK, Glazier RH, Forster A, et al. Investigating the effect of sociodemographic factors on 30-day hospital readmission among medical patients in Toronto, Canada: a prospective cohort study. BMJ Open. 2017;7(12). [DOI] [PMC free article] [PubMed]
- 44.Toronto Public Health, St. Michael’s Hospital Research, CAMH, Mount Sinai Hospital. We Ask Because We Care: The Tri-Hospital + TPH Health Equity Data Collection Research Project Report. 2013. Available at: https://www.stmichaelshospital.com/quality/equity-data-collection-report.pdf. Accessed June 4, 2019.
- 45.Williams BC, Ward DA, Chick DA, Johnson EL, Ross PT. Using a Six-Domain Framework to Include Biopsychosocial Information in the Standard Medical History. Teaching and Learning in Medicine. 2019;31(1):87–98. doi: 10.1080/10401334.2018.1480958. [DOI] [PubMed] [Google Scholar]
- 46.Yaman GL, Karan A, Karan MA, Erten NN, Aksoy C. Quality of life perceptions of hospitalized patients. Ann Saudi Med. 2003;23(6):399–401. doi: 10.5144/0256-4947.2003.399. [DOI] [PubMed] [Google Scholar]
- 47.The World Health Organization Quality of Life Group. The World Health Organization quality of life assessment (WHOQOL): Development and general psychometric properties. Social Science & Medicine. 1998;46(12):1569–85. [DOI] [PubMed]
- 48.Salma S, Fadwa C, Sameh M, Lobna A, Radhwan G, Zouhair B, et al. Nutritional and functional status among hospitalized elderly people. European Geriatric Medicine. 2016;7(Supplement 1).
- 49.Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, et al. Validation of the Mini Nutritional Assessment short-form (MNA®-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782. doi: 10.1007/s12603-009-0214-7. [DOI] [PubMed] [Google Scholar]
- 50.Arik G, Varan HD, Yavuz BB, Karabulut E, Kara O, Kilic MK, et al. Validation of Katz index of independence in activities of daily living in Turkish older adults. Arch Gerontol Geriatr. 2015;61(3):344–50. [DOI] [PubMed]
- 51.Nardi R, Scanelli G, Tragnone A, Lolli A, Kalfus P, Baldini A, et al. Difficult hospital discharges in internal medicine wards. Intern Emerg Med. 2007;2(2):95–9. doi: 10.1007/s11739-007-0029-7. [DOI] [PubMed] [Google Scholar]
- 52.Goodman MS, Gilbert KL, Hudson D, Milam L, Colditz GA. Descriptive analysis of the 2014 race-based healthcare disparities measurement literature. J Racial and Ethnic Health Disparities. 2017;4(5):796–802. doi: 10.1007/s40615-016-0281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Andermann A. Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Rev. 2018;39(1):19. doi: 10.1186/s40985-018-0094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lewis CC, Wellman R, Jones SMW, Walsh-Bailey C, Thompson E, Derus A, et al. Comparing the performance of two social risk screening tools in a vulnerable subpopulation. J Family Med Primary Care. 2020;9(9):5026–34. doi: 10.4103/jfmpc.jfmpc_650_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morone J. An integrative review of social determinants of health assessment and screening tools used in pediatrics. J Pediatr Nurs. 2017;37:22–8. doi: 10.1016/j.pedn.2017.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Olson DP, Oldfield BJ, Morales Navarro S. Standardizing Social Determinants Of Health Assessments. Health Affairs Forefront. 2019.
- 57.Garg A, Sheldrick RC, Dworkin PH. The inherent fallibility of validated screening tools for social determinants of health. Acad Pediatrics. 2018;18(2):123–4. doi: 10.1016/j.acap.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 58.Petkovic J, Duench SL, Welch V, Rader T, Jennings A, Forster AJ, et al. Potential harms associated with routine collection of patient sociodemographic information: a rapid review. Health Expect. 2019;22(1):114–29. doi: 10.1111/hex.12837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Varcoe C, Browne AJ, Wong S, Smye VL. Harms and benefits: collecting ethnicity data in a clinical context. Soc Sci Med. 2009;68(9):1659–66. doi: 10.1016/j.socscimed.2009.02.034. [DOI] [PubMed] [Google Scholar]
- 60.Kirst M, Shankardass K, Bomze S, Lofters A, Quiñonez C. Sociodemographic data collection for health equity measurement: a mixed methods study examining public opinions. Int J Equity Health. 2013;12(1):75. doi: 10.1186/1475-9276-12-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bloch G, Rozmovits L. Implementing social interventions in primary care. CMAJ. 2021;193(44):E1696–701. doi: 10.1503/cmaj.210229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.O’Gurek DT, Henke C. A practical approach to screening for social determinants of health. FPM. 2018;25(3):7–12. [PubMed] [Google Scholar]
- 63.Palacio A, Seo D, Medina H, Singh V, Suarez M, Tamariz L. Provider perspectives on the collection of social determinants of health. Popul Health Manag. 2018;21(6):501–8. doi: 10.1089/pop.2017.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lasser EC, Kim JM, Hatef E, Kharrazi H, Marsteller JA, DeCamp LR. Social and behavioral variables in the electronic health record: a path forward to increase data quality and utility. Acad Med. 2021;96(7):1050–6. doi: 10.1097/ACM.0000000000004071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Levine DM, Linder JA, Landon BE. Characteristics of Americans with primary care and changes over time, 2002-2015. JAMA Int Med. 2020;180(3):463–6. doi: 10.1001/jamainternmed.2019.6282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hay C, Pacey M, Bains N, Ardal S. Understanding the unattached population in Ontario: evidence from the Primary Care Access Survey (PCAS). Healthcare Policy. 2010;6(2):33–47. [PMC free article] [PubMed]
- 67.Khandor E, Mason K, Chambers C, Rossiter K, Cowan L, Hwang SW. Access to primary health care among homeless adults in Toronto, Canada: results from the Street Health survey. Open Med. 2011;5(2):e94–103. [PMC free article] [PubMed] [Google Scholar]
- 68.Herrera CN, Brochier A, Pellicer M, Garg A, Drainoni ML. Implementing social determinants of health screening at community health centers: clinician and staff perspectives. J Prim Care Comm Health. 2019;10:1–10. doi: 10.1177/2150132719887260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by US physician practices and hospitals. JAMA Network Open. 2019;2(9):e1911514. doi: 10.1001/jamanetworkopen.2019.11514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Quiñones-Rivera A, Wing HE, Barr-Walker J, Yee M, Harrison JM, Gottlieb LM. Provider impacts of socioeconomic risk screening and referral programs: a scoping review. J Am Board Fam Med. 2021;34(4):820–31. doi: 10.3122/jabfm.2021.04.210039. [DOI] [PubMed] [Google Scholar]
- 71.Gruß I, Bunce A, Davis J, Dambrun K, Cottrell E, Gold R. Initiating and implementing social determinants of health data collection in community health centers. Popul Health Manag. 2021;24(1):52–8. doi: 10.1089/pop.2019.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gard LA, Peterson J, Miller C, Ghosh N, Youmans Q, Didwania A, et al. Social determinants of health training in U.S. primary care residency programs: a scoping review. Acad Med. 2019;94(1):135–43. [DOI] [PubMed]
- 73.Gard LA, Cooper AJ, Youmans Q, Didwania A, Persell SD, Jean-Jacques M, et al. Identifying and addressing social determinants of health in outpatient practice: results of a program-wide survey of internal and family medicine residents. BMC Med Educ. 2020;20(1):18. doi: 10.1186/s12909-020-1931-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Doobay-Persaud A, Adler MD, Bartell TR, Sheneman NE, Martinez MD, Mangold KA, et al. Teaching the social determinants of health in undergraduate medical education: a scoping review. J Gen Intern Med. 2019;34(5):720–30. doi: 10.1007/s11606-019-04876-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 38.3 kb)