Abstract
Diagnostic schemas are frameworks that depict organized clinical knowledge and serve as a bridge between problem representation and differential diagnosis generation. Schema-based problem solving is increasingly used among clinician educators and is widely featured in digital media. We examine the origins of schemas and their theoretical background, review existing literature on their applications in medicine, and explore their utility for learners and teachers.
A first-year medicine resident has just evaluated a 75-year-old man with shortness of breath. She arrives at the correct diagnosis — a heart failure exacerbation — but her preceptor is not sure she has an organized approach to reasoning through the clinical problem of dyspnea. The preceptor asks if she has a “schema” for shortness of breath and the resident gives her preceptor a puzzled look.
Diagnostic schemas are frameworks that depict organized clinical knowledge and serve as the bridge between problem representation and differential diagnosis in the clinical reasoning process. In recent years, the term “schema” has been increasingly used in clinical and educational settings. This adoption reflects the integration of cognitive psychology into clinical instruction,1 as well as the influence of textbooks,2 medical educators,3,4 case reports,5 and digital media6–8 that have introduced schemas into the clinical reasoning vernacular. In this paper, we explore how diagnostic schemas (hereafter referred to as “schemas”) can serve as powerful tools for both teacher and learners.
THE HISTORY OF SCHEMAS
The word “schema” originates from the Greek word for “shape” or “plan” and has long been in the lexicon of philosophy and psychology.9 The eighteenth century German philosopher Immanuel Kant introduced the term “schema” to describe structures that organize thinking and give form to abstract concepts.10 In the second half of the twentieth century, psychologist Jean Piaget defined schemas as “mental representations” that organize a unit of knowledge.11 He proposed that with age and experience, a child will acquire and retrieve increasingly complex schemas, such as what constitutes a chair (object schema) or how to order food in a restaurant (action schema). Schema theory emerged in the 1970s and posited that an individual’s knowledge is represented in memory as the sum of their schemas, and that the mind has schemas for all things, including people, objects, and abstract concepts.9
HOW SCHEMAS WORK
When the human mind encounters a problem, it activates knowledge to arrive at a solution.12 Enumerating a list of all solutions for a complex problem is cognitively taxing and inconsistent between episodes. Activating a schema is a more feasible and reproducible first step when solving a problem. A schema “chunks” isolated pieces of knowledge into units that are easier to manage in long-term memory.13 In clinical problem solving, a schema transforms a long list of potential diagnoses into more manageable groups of diagnoses.3
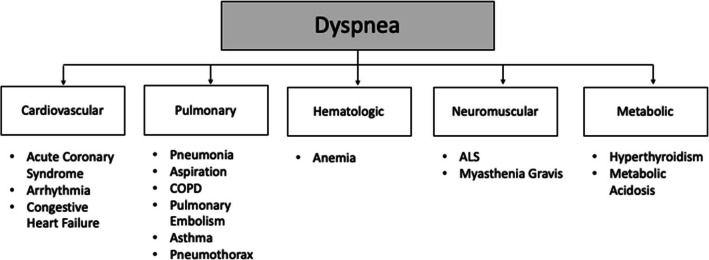
For the resident in the introductory case, recalling all relevant causes of dyspnea would be mentally taxing and haphazard. But sequentially considering several categories of dyspnea — pulmonary, cardiac, hematologic, neuromuscular, and metabolic — is a reproducible approach to solving dyspnea that can structure her differential diagnosis generation (Fig. 1). Schema-based problem solving differs from hypo-theticodeductive reasoning, which is characterized by sequential hypothesis generation fueled by incoming data.14
Figure 1.
Simplified dyspnea schema.
Diagnostic schemas are distinct from diagnostic checklists which ensure consideration of a lengthy differential diagnosis or enforce a diagnostic “time out” with metacognition.15,16 Schemas also differ from mnemonics17, which are memory aids that facilitate recall without connecting to an underlying knowledge structure or meaning (e.g., MUDPILES for anion gap metabolic acidosis).
In cognitive psychology, both illness scripts (encapsulated knowledge about a single disease)18 and frameworks to approach a problem are considered types of schemas (i.e., structured representations of knowledge in memory). However, in the clinical reasoning literature, schemas have come to refer to the latter, even though the two forms are closely linked in learning and problem solving.3
SCHEMAS IN MEDICINE
Schemas were introduced into undergraduate medical education at the University of Calgary in the 1990s.14 The goal was to promote organized problem solving by providing students with schemas for common clinical problems. This differed from the more widespread approach of teaching about diseases and leaving learners to construct their own idiosyncratic approaches to diagnosis through observation and trial and error. Three decades later, schemas continue to form an integral part of the University of Calgary medical program.3
Several studies have demonstrated that schemas organize learning and guide problem solving, reduce cognitive load (the amount of working memory resources used in a learning or workplace task19), and mitigate premature closure among medical students.20 In a randomized trial of second year medical students learning with a cardiopulmonary simulator, schema-based instruction was associated with improved discrimination between diagnoses and greater diagnostic accuracy compared to standard instruction.21 Another study showed that medical students who used a diagnostic schema to conceptualize metabolic alkalosis maintained expert-type (deep rather than superficial) knowledge structures longer than students who did not use schemas.22 Other studies of medical students demonstrated that schemas were associated with greater diagnostic accuracy with EKGs,23 electrolyte and acid-base problems,24 congenital heart disease cases,25 and gastroenterology conditions.26
In a study of clerkship students, Coderre et al. demonstrated that learners with problem-specific schemas had better diagnostic performance on cases of dyspnea, chest pain, anemia, and abnormal liver function than students with generic knowledge structures. The higher performing students organized differential diagnoses according to clinically relevant categories for a specific problem, such as approaching dyspnea by chest X-ray results, as opposed to more generic categories that can be applied to all problems (e.g., VINDICATE mnemonic).27
Although a schema-based approach to knowledge construction and problem solving has not been widely adopted in medical schools, schemas are being embraced by learners and teachers in digital education resources like podcasts and social media.6,28
SCHEMA FORM
A diagnostic schema is a hierarchal conceptual framework with a branching connection between upper and lower levels. Schemas can be formed for any data point, such as a symptom (e.g., dyspnea), sign (e.g., jaundice), imaging result (e.g., ground-glass opacities), or lab value (e.g., hypercalcemia).5 Practical schemas have higher-level categories with parallel construction (e.g., organ-based or mechanisms) that narrow to subsidiary categories and eventually terminate at individual diagnoses.13 The initial branch points and overall layout often reflect the practical considerations and resources available when solving a specific problem in the typical clinical setting (Table 1).
Table 1.
Examples of Schema Branch Points
| Branch point type | Problem | Primary branch point |
|---|---|---|
| Test result | Ascites | Serum ascites albumin gradient > 1.1 |
| Hypercalcemia | Parathyroid hormone level | |
| Urgency of diagnosis | Headache | Primary vs. secondary |
| Myelopathy | Intrinsic vs. extrinsic (compressive) | |
| Categories of disease | Altered mental status | Metabolic, infectious, structural, toxic |
| Mechanism | Hemolysis | Intravascular vs. extravascular |
| Anatomic | Chest pain | Cardiac, pulmonary, esophageal, musculoskeletal, dermatologic |
IS THERE ONE RIGHT SCHEMA?
There is no gold standard schema for any problem because there are multiple successful pathways to addressing the same issue.29 Some schemas are widespread (e.g., pre-, intra-, and post-renal approach to acute kidney injury [AKI]), while others have multiple widely used iterations and variations (e.g., anemia analysis based on erythrocyte size, kinetics, or sites of production and destruction).
Schemas should be practical and may vary by clinical environment. For example, an emergency medicine clinician approaching chest pain may prefer an initial branch point that identifies or excludes coronary artery disease–related chest pain, rather than an approach considering five anatomic compartments in parallel.
Schemas will mature and grow in complexity based on clinical experience. For instance, a student will gradually develop a more nuanced understanding of AKI and elaborate the tripartite approach by expanding the intrarenal category to include glomerular, tubular, interstitial, and vascular etiologies. Each category will expand further during residency.
Schemas will evolve as knowledge of disease mechanisms improves. For instance, inflammatory disease currently categorized by patterns of presentation (e.g., symmetric vs asymmetric arthritis) may eventually be organized by the underlying cytokines driving inflammation (e.g., IL-6 mediated).30 A traditional cancer of unknown origin schema may shift from pursuing the tissue of origin (e.g., sarcoma or GI adenocarcinoma) to classifying the underlying malignancy according to genetic profiles and driver mutations.31
SCHEMAS AS A LEARNING TOOL
Using schemas as the scaffold for knowledge in memory promotes a systematic approach to problem solving.3 Learners can practice retrieving schemas by routinely using them as a bridge between problem representation and differential diagnosis generation.
Most learners begin by adopting available schemas for common problems. This is an effective starting point, but downloading and saving schemas alone does not equate with knowledge and comprehension.32 Repeatedly writing and recalling schemas for common problems draws on learning sciences principles like retrieval practice, elaboration, and dual coding, which improve memory and understanding.33,34 Regardless of whether a schema is borrowed or built, it should be rehearsed and revised so that it evolves with clinical experience and captures a successful approach to the clinical problem. These efforts can be aided by a paper or electronic schema repository35 which features easy modification36 and rapid accessibility (e.g., as a reference before seeing new patients to focus history of present illness questions).
When presenting their assessment of a patient, learners should demonstrate their organized approach to a problem by articulating their schema. After accurately labeling the patient’s primary problem, such as thrombocytopenia, the learner should briefly elaborate the relevant schema in a succinct sentence (e.g., “thrombocytopenia is caused by decreased production, increased consumption, or sequestration”). The schema, which is agnostic to any patient, can then guide the construction of a prioritized differential diagnosis, which is specific to each patient. Inevitably, certain categories or classifications will be forgotten with initial recall efforts, but with increased practice, the major categories will become familiar, and attention can be turned to deeper branch points in the algorithm.
Learners can also access their schemas when a patient’s trajectory is not evolving as anticipated. When the pursuit of an infection in a febrile ICU patient is unrevealing, a learner can use their schema to shift their attention to alternative categories of disease. Like a map guiding a lost traveler, schemas can provide direction when the diagnosis remains uncertain.
SCHEMAS AS A TEACHING TOOL
One of the challenges of teaching clinical reasoning is making implicit knowledge explicit for learners. By regularly elaborating schemas, instead of lengthy differential diagnoses, teachers can simplify their representation of how doctors approach a problem. When teachers can draw schemas or narrate their structure in a memorable way, the resulting visual simplification gives learners a foothold into a complex topic from which they can build.37
Teachers can promote the development of schemas by encouraging their integration into learners’ presentations. Teachers may set expectations that learners name the problem and then succinctly articulate a schema for the problem before their elaboration of the prioritized differential diagnosis. In the opening case, the learner arrived at the diagnosis of acute heart failure without a brief description of the schema for the presenting symptom. Even if the diagnosis was correct, the teacher had no reassurances that the learner could reason through the clinical problem of dyspnea for the next patient. Hearing her schema for dyspnea (“dyspnea is primarily caused by pulmonary, cardiac, hematologic, ...”) would have helped the preceptor confirm that the learner arrived at the right diagnosis with a comprehensive understanding of the problem. Conversely, analysis of her schema may reveal a gap in the learner’s understanding of how to approach dyspnea (e.g., conflation of hypoxemia with dyspnea), which would serve as a launching point for teaching and discussion.
Educators must determine where to intervene along the reasoning process.38 Schemas have more educational utility when learners would benefit from an overview of the approach to a problem rather than the details of specific diagnoses. This may occur when reframing a case, after an accurate problem representation, or in the process of generating a differential diagnosis. When patients are incorrectly framed or have multiple interacting problems, the discussion may be better centered around points other than the diagnostic schema. For example, in some contexts, analyzing the illness script or management script39 for atrial fibrillation will be more relevant than reviewing the diagnostic schema for tachycardia.
CONCLUSION
Diagnostic schemas are powerful tools to organize knowledge and facilitate clinical problem solving. What began in the minds of psychologists and philosophers has been carried into the realm of diagnostic reasoning by clinician educators. Schema-based instruction provides learners with a structured approach to knowing and learning that starts during training and can continue throughout a career in medicine.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schmidt HG, Mamede S. How cognitive psychology changed the face of medical education research. Adv Health Sci Educ Theory Pract. 2020;25(5):1025–1043. doi: 10.1007/s10459-020-10011-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Monsoor AM. Frameworks for Internal Medicine. Philadelphia: Wolters Kluwer; 2019. [Google Scholar]
- 3.Blackbook. About. Available at blackbook.ucalgary.ca/about. Accessed 3 June 2022.
- 4.Mandin H, Harasym P, Eagle C, Watanabe M. Developing a “clinical presentation” curriculum at the University of Calgary. Acad Med. 1995;70(3):186–93. doi: 10.1097/00001888-199503000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Martin M, Sedighi Manesh R, Henderson MC, Critchfield JM. Diagnostic scheming. J Gen Intern Med. 2015;30(12):1874–8. doi: 10.1007/s11606-015-3478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ow GM, Shipley LC, Nematollahi S, Stetson GV. Morning report for all: a qualitative study of disseminating case conferences via podcasting. BMC Med Educ. 2021;21(1):392. doi: 10.1186/s12909-021-02799-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sachs S, Sherman S, Fang C, Hwang J. 34M with Fever, Headache, and Myalgias. Core IM Podcast. January 16, 2019. Available at https://www.coreimpodcast.com/2019/01/16/hoofbeats-34m-with-fever-headache-and-myalgias/
- 8.Clinical Reasoning Exercises. Diagnostic Schema. Journal of General Internal Medicine. sgim.org/web-only/clinical-reasoning-exercises/diagnostic-schema. Accessed 6 June 2022.
- 9.Seel NM. Schema(s). In: Seel, N.M. (eds) Encyclopedia of the Sciences of Learning. Boston, MA; Springer; 2012.
- 10.Kant I. Critique of pure reason. Trans. N. K. Smith. New York: St. Martin’s Press. 1781/1929
- 11.Simply Psychology. Piaget’s Stages of Cognitive Development. Available at simplypsychology.org/Piaget.html. Accessed 3 June 2022.
- 12.Mandin H, Jones A, Woloschuk W, Harasym P. Helping students learn to think like experts when solving clinical problems. Acad Med. 1997;72(3):173-9 [DOI] [PubMed]
- 13.Thalmann M, Souza AS, Oberauer K. How does chunking help working memory? J Exp Psychol Learn Mem Cogn. 2019;45(1):37-55. [DOI] [PubMed]
- 14.Woloschuk W, Harasym P, Mandin H, Jones A. Use of scheme-based problem solving: an evaluation of the implementation and utilization of schemes in a clinical presentation curriculum. Med Educ. 2000;34(6):437-42. [DOI] [PubMed]
- 15.Ely JW, Graber MA. Checklists to prevent diagnostic errors: a pilot randomized controlled trial. Diagnosis (Berl). 2015;2(3):163–169. doi: 10.1515/dx-2015-0008. [DOI] [PubMed] [Google Scholar]
- 16.Ely JW, Graber ML, Croskerry P. Checklists to reduce diagnostic errors. Acad Med. 2011;86(3):307-13 [DOI] [PubMed]
- 17.Odigwe C, Davidson S. Mnemonics. BMJ. 2005; 331:0509325.
- 18.Minter DJ, Manesh R, Cornett P, Geha RM. Putting schemas to the test: an exercise in clinical reasoning. J Gen Intern Med. 2018;33(11):2010-2014. [DOI] [PMC free article] [PubMed]
- 19.Young JQ, Van Merrienboer J, Durning S, Ten Cate O. Cognitive Load Theory: implications for medical education: AMEE Guide No. 86. Med Teach. 2014;36(5):371-84. [DOI] [PubMed]
- 20.Blissett S, Morrison D, McCarty D, Sibbald M. Should learners reason one step at a time? A randomised trial of two diagnostic scheme designs. Med Educ. 2017;51(4):432-441. [DOI] [PubMed]
- 21.Blissett S, Cavalcanti RB, Sibbald M. Should we teach using schemas? Evidence from a randomised trial. Med Educ. 2012;46(8):815-22. [DOI] [PubMed]
- 22.Novak K, Mandin H, Wilcox E, McLaughlin K. Using a conceptual framework during learning attenuates the loss of expert-type knowledge structure. BMC Med Educ. 2006;6:37. [DOI] [PMC free article] [PubMed]
- 23.Blissett S, Cavalcanti R, Sibbald M. ECG rhythm analysis with expert and learner-generated schemas in novice learners. Adv Health Sci Educ Theory Pract. 2015;20(4):915-33. [DOI] [PubMed]
- 24.McLaughlin K, Coderre S, Mortis G, Mandin H. Expert-type knowledge structure in medical students is associated with increased odds of diagnostic success. Teach Learn Med. 2007 Winter;19(1):35-41. [DOI] [PubMed]
- 25.Beck AL, Bergman DA. Using structured medical information to improve students’ problem-solving performance. J Med Educ. 1986;61(9 Pt 1):749-56. [DOI] [PubMed]
- 26.Coderre S, Mandin H, Harasym PH, Fick GH. Diagnostic reasoning strategies and diagnostic success. Med Educ. 2003;37(8):695-703. [DOI] [PubMed]
- 27.Coderre S, Jenkins D, McLaughlin K. Qualitative differences in knowledge structure are associated with diagnostic performance in medical students. Adv Health Sci Educ Theory Pract. 2009;14(5):677-84. [DOI] [PubMed]
- 28.Infographic - The Curbsiders - #126 Kashlak Morning Report with Human Dx- Diagnostic Schema - Final. https://thecurbsiders.com/podcast/126-kashlak-morning-report-human-dx/attachment/infographic-the-curbsiders-126-kashlak-morning-report-with-human-dx-diagnostic-schema-final. Accessed 18 Sept 2022.
- 29.Geha RM, Manesh R. Episode 185: VMR with R&R. Dissecting the Learning Process with Rabih & Reza. Clinical Problem Solvers. June 30, 2021.
- 30.Schett G, McInnes IB, Neurath MF. Reframing immune-mediated inflammatory diseases through signature cytokine hubs. N Engl J Med. 2021;385(7):628-639. [DOI] [PubMed]
- 31.Varadhachary GR, Raber MN. Cancer of unknown primary site. N Engl J Med. 2014;371(8):757-65. [DOI] [PubMed]
- 32.Goldberg C. In Praise of Paper(s). Am J Med. 2012;125(11):1047-8. [DOI] [PubMed]
- 33.McDaniel MA, Donnelly CM. Learning with analogy and elaborative interrogation. J Educ Psychol. 1996;88, 508-519.
- 34.Mayer RE, Anderson RB. The instructive animation: Helping students build connections between words and pictures in multimedia learning. J Educ Psychol. 1992; 4, 444-452.
- 35.Glass Health. Glass Notebook. Available at: glass.health. Accessed 3 June 2022.
- 36.McArthur E. Shematify: a web app for creation and visualization of medical diagnostic schemas. Available at: https://www.youtube.com/watch?v=u-gjhf2LF4I. Accessed 10 Oct 2022.
- 37.Marshall SP. Schema-Based Instruction. In: Seel, N.M. (eds) Encyclopedia of the Sciences of Learning. Boston: Springer; 2012.
- 38.Bowen JL. Educational strategies to promote clinical diagnostic reasoning. N Engl J Med. 2006;355(21):2217-25. [DOI] [PubMed]
- 39.Parsons AS, Wijesekera TP, Rencic JJ. The management script: a practical tool for teaching management reasoning. Acad Med. 2020;95(8):1179-1185. [DOI] [PubMed]