Abstract
Introduction
HIV incidence remains high in the U.S. as do disparities in new HIV diagnosis between White and Black populations and access to preventive therapies like pre-exposure prophylaxis (PrEP). The federal Ending the HIV Epidemic (EHE) initiative was developed to prioritize resources to 50 jurisdictions with high HIV incidence.
Methods
We conducted secondary analyses of data (2013–2019) from the CDC, Census Bureau, and AIDSVu to evaluate the correlation between PrEP use, HIV incidence, and HIV incidence disparities. We compared the PrEP-to-need ratio (PnR) with the ratio of Black and White HIV incidence rates in 46 EHE counties. Subsequent analyses were performed for the seven states that contained multiple EHE counties.
Results
These 46 counties represented 25.9% of the U.S. population in 2019. HIV incidence ranged from 10.5 in Sacramento County, CA, to 59.6 in Fulton County, GA (per 100,000). HIV incidence disparity ranged from 1.5 in Orleans Parish, LA, to 12.1 in Montgomery County, MD. PnR ranged from 26.8 in New York County, NY, to 1.46 in Shelby County, TN. Change in HIV incidence disparities and percent change in PnR were not significantly correlated (ρ = 0.06, p = 0.69). Change in overall HIV incidence was significantly correlated with increase in PnR (ρ = −0.42, p = 0.004).
Conclusions
PrEP has the potential to significantly decrease HIV incidence; however, this benefit has not been conferred equally. Within EHE priority counties, we found significant HIV incidence disparities between White and Black populations. PrEP has decreased overall HIV incidence, but does not appear to have decreased HIV incidence disparity.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07687-y.
KEY WORDS: HIV, PrEP, disparity, county-level, incidence, PrEP-to-Need
INTRODUCTION
In 2019, over 36,000 individuals were newly diagnosed with HIV in the USA.1 While this represents a 9% decrease from 2015, neither the burden of disease nor improvements therein are experienced equally by all racial and ethnic groups. For example, Black people experienced a disproportionate burden of new HIV diagnoses in 2019 (42%), compared to their White counterparts (25%). This equates to an HIV incidence rate of 37.3 per 100,000 population for Black people compared to 4.6 per 100,000 among White people.1 These rates represent little change from 2015, with incidence rates of 41.2 and 5.1 for Black and White populations, respectively.1
The FDA approval of emtricitabine/tenofovir disoproxil fumarate (TDF/FTC) for use as daily HIV pre-exposure prophylaxis (PrEP) in 2012 was a major milestone in HIV prevention.2 When taken daily, PrEP is up to 99% effective at preventing HIV and is safely tolerated with minimal side effects.3 Since its approval, there have been concerns about racial inequities in PrEP prescription further propagating disparities in HIV incidence between White and Black communities.4,5 In 2019, only 23% of all people eligible for PrEP were actually prescribed this intervention; however, PrEP coverage remains significantly unequal between eligible White (63%) and Black (8%) people, a gap that has only widened since 2012.6
One metric used to monitor PrEP implementation is the PrEP-to-Need Ratio (PnR)—the ratio of PrEP prescriptions (numerator) to new HIV diagnoses (denominator) in a particular geography or population over a set period.7 For example, a PnR of 5 indicates 5 people prescribed PrEP per 1 HIV diagnosis. Over years of implementation, the PnR should theoretically continue to increase as the use of PrEP contributes to lower HIV incidence thus decreasing the denominator criteria among a specific population. Similar to disparities observed in PrEP prescription, studies examining PnR have observed lower ratios in counties with greater percentages of Black compared to White residents.8 This is likely contributing to observed, persistent disparities in HIV incidence between these groups.1 Indeed, counties with the greater percentages of Black residents have demonstrated the slowest increases in PnR from 2012 to 2018.8
In an effort to leverage critical scientific advances in HIV prevention and treatment, the national Ending the HIV Epidemic in the U.S. (EHE) initiative was established in 2019 by the U.S. Department of Health and Human Services and Centers for Disease Control and Prevention (CDC).9 Phase 1 of EHE aims to reduce the number of new HIV infections by 75% by 2025, focusing on 50 priority jurisdictions that account for over 50% of new HIV diagnoses.10 The priority jurisdictions represent 48 U.S. counties/cities, San Juan, Puerto Rico, and Washington, D.C.9 Regionally, 41.3% of the EHE priority jurisdictions are located in the Southern U.S. which is due to the well documented pattern of high HIV incidence and low PrEP use in this region.7,11,12
County-level data are essential given the role of local health departments in monitoring HIV and sexually transmitted infection (STI) rates and in developing interventions and programs specific to the needs of their communities, especially in their role as safety-net service providers.13–16 Analysis performed at the county-level may provide particularly important, actionable insight into persistent HIV incidence disparities as all counties within a single state are operating under the same, state-level policies, such as Medicaid expansion. Thus, county-level analysis may yield examples or prototypes for jurisdictions that appear to have been able to expand PrEP use while decreasing HIV incidence disparities.
The current paper aims to provide county-level data for the EHE priority counties describing the following: HIV incidence for Black and White populations and racial disparities in incidence, the PnR, and the relationship between Black:White disparities in HIV incidence and the PnR. Understanding the relationship between PrEP use and Black:White HIV incidence disparities at the county-level provides a framework for healthcare providers, county leaders, and policy makers to design targeted interventions to reduce HIV incidence through equal access and prescription to PrEP for prevention. Given their designation as EHE priority areas, understanding the relationship between incidence disparities and PnR at this level may help highlight areas for improvement as we move to the next phases of EHE.
METHODS
We conducted secondary analyses of publicly available de-identified data to (1) describe HIV incidence by race; (2) calculate Black:White incidence rate ratios (IRR); (3) present PnR (PrEP use); and (4) investigate the relationship between PrEP use and the incidence disparity at the county-level for 46 EHE priority jurisdictions. We excluded San Juan, Puerto Rico; San Francisco County, CA; Orange County, CA; and Suffolk County, MA, due to HIV incidence data suppression. Of note, Baltimore City, MD, is the only non-county jurisdiction included in the EHE priority list. For simplicity, we refer to priority counties and county-level data throughout the paper.
Measures
HIV Incidence
We obtained the overall HIV incidence rate, as well as the HIV incidence rate for White and Black people at the county-level from the CDC National Center for HIV/AIDS, Viral Hepatitis, STI, and TB Prevention (NCHHSTP).17 These values were obtained for the years 2012–2019. We also obtained the state-level Black and White HIV incidence rates for the years 2012–2019 for states containing greater than 3 EHE priority counties. All rates were per 100,000 people.
Black:White Incidence Rate Ratio (Incidence Disparity)
We calculated the Black:White IRR, a measure of incidence disparity, by dividing the county Black HIV incidence rate (numerator) by the county White HIV incidence rate (denominator). An incidence disparity > 1 indicates higher HIV incidence among Black people compared to White people, while an incidence disparity < 1 indicates the opposite. We also calculated state-level incidence disparity using state HIV incidence for White and Black populations.
PrEP Prescription Data
County- and state-level data about PrEP use was obtained from a public dataset aggregated by AIDSVu, a collaboration between Gilead Sciences®, Symphony Health®, and Emory University.18 This dataset reports the number of PrEP users in each county or state, defined as “a prescription for TDF/FTC active for more than 30 days prescribed without other antiretrovirals,” removing TDF/FTC prescriptions used for diagnoses other than HIV PrEP (e.g., hepatitis B, post-exposure prophylaxis) via a validated algorithm cross-checking with health insurance claims data.18,19 Using this data, county- and state-level PnR were reported for the years 2012–2019.
Demographic Variables
Total county population was taken from the U.S. Census Bureau American Community Survey (ACS) 5-year estimates (Table B02001) for the years 2012–2019.20 Total U.S. population was also taken from the Census Bureau.21
Statistical Analyses and Data Organization
We used county Federal Information Processing Standard (FIPS) codes to link variables between NCHHSTP, AIDSVu, and ACS datasets. For all counties included in the analysis, we plotted the incidence disparity and PnR in a quadrant graph to demonstrate performance on both metrics simultaneously. We also calculated the percent change in each county’s overall HIV incidence, incidence disparity, and PnR between 2013 and 2019. We opted to use the years 2013–2019 to account for the potential effect of initial prescriptions of PrEP (2012) on HIV incidence and thus incidence disparities. We calculated Spearman’s rho (ρ) correlation coefficients between the percent change in PnR, percent change in HIV incidence disparity (IRR), and percent change in overall HIV incidence. We also calculated the correlation between PrEP use and incidence disparity for the year 2019. For the 7 states that contained more than 3 EHE priority counties, we performed a separate set of descriptive analyses of the relationship between county PnR and HIV disparity and changes over the years of 2013–2019 and produced similar performance plots.
All data was managed and organized utilizing Microsoft Excel (Redmond, WA). Analysis was performed with Stata V17 (Stata Corp., College Station, TX).
RESULTS
Collectively, the 46 counties in this analysis represented 84,891,138 people, or 25.9% of the total U.S. population in 2019. Data for all years is presented in Supplemental Table 1. Results are presented based on performance for each metric throughout the “Results” section, with better performance corresponding to lower IRR and higher PnR. During 2019, overall HIV incidence across EHE counties ranged from a low of 10.5 in Sacramento County, CA, to a high of 59.6 in Fulton County, GA (Table 1). HIV incidence among Black people ranged from a low of 27.8 in Sacramento County, CA, to a high of 106.1 in Fulton County, GA. Among White persons, HIV incidence ranged from a low of 3.2 in Queens County, NY, to a high of 35.2 in Orleans Parish, LA.
Table 1.
Overall HIV incidence across EHE counties
| Overall Incidence | White Incidence | Black Incidence | Black:White IRR | PnR | %∆ Overall Incidence | %∆ IRR | %∆ PnR | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jurisdiction name | 2013 | 2019 | 2013 | 2019 | 2013 | 2019 | 2013 | 2019 | 2013 | 2019 | |||
| Maricopa County, AZ | 14.2 | 13.7 | 9.3 | 8.3 | 48.4 | 52.1 | 5.20 | 6.28 | 0.39 | 5.37 | −3.5% | 20.6% | 1,277% |
| Alameda County, CA | 16.0 | 15.4 | 9.6 | 10.5 | 51.3 | 51.5 | 5.34 | 4.90 | 0.65 | 7.52 | −3.8% | −8.2% | 1,057% |
| Los Angeles County, CA | 21.0 | 17.4 | 16.7 | 13.4 | 49.2 | 44.6 | 2.95 | 3.33 | 0.39 | 6.04 | −17.1% | 13.0% | 1,449% |
| Riverside County, CA | 12.6 | 13.2 | 14.2 | 10.2 | 22.7 | 29.2 | 1.60 | 2.86 | 0.35 | 5.28 | 4.8% | 79.1% | 1,409% |
| Sacramento County, CA | 13.8 | 10.5 | 8.3 | 7.2 | 32.5 | 27.8 | 3.92 | 3.86 | 0.37 | 4.82 | −23.9% | −1.4% | 1,203% |
| San Bernardino County, CA | 11.5 | 16.2 | 7.4 | 9.8 | 26.2 | 40.6 | 3.54 | 4.14 | 0.27 | 2.83 | 40.9% | 17.0% | 948% |
| San Diego County, CA | 18.1 | 13.0 | 12.3 | 7.7 | 40.6 | 32.8 | 3.30 | 4.26 | 0.40 | 7.30 | −28.2% | 29.1% | 1,725% |
| District of Columbia, DC | 86.9 | 42.2 | 37.5 | 8.0 | 129.9 | 74.4 | 3.46 | 9.30 | − | 13.4 | −51.4% | 168.5% | − |
| Broward County, FL | 41.5 | 35.8 | 27.0 | 17.7 | 78.6 | 59.5 | 2.91 | 3.36 | 0.25 | 5.69 | −13.7% | 15.5% | 2,176% |
| Duval County, FL | 39.0 | 34.2 | 14.3 | 18.7 | 92.5 | 70.3 | 6.47 | 3.76 | 0.16 | 2.18 | −12.3% | −41.9% | 1,263% |
| Hillsborough County, FL | 27.5 | 21.5 | 16.2 | 10.6 | 69.1 | 63.3 | 4.27 | 5.97 | 0.22 | 5.11 | −21.8% | 40.0% | 2,223% |
| Miami-Dade County, FL | 50.8 | 49.6 | 27.3 | 30.6 | 114.2 | 88.2 | 4.18 | 2.88 | 0.17 | 4.15 | −2.4% | −31.1% | 2,341% |
| Orange County, FL | 33.5 | 39.7 | 20.0 | 18.5 | 72.9 | 84.9 | 3.65 | 4.59 | 0.22 | 4.28 | 18.5% | 25.9% | 1,845% |
| Palm Beach County, FL | 26.8 | 18.3 | 10.4 | 6.7 | 92.6 | 52.8 | 8.90 | 7.88 | 0.26 | 4.10 | −31.7% | −11.5% | 1,477% |
| Pinellas County, FL | 18.7 | 21.3 | 9.6 | 12.8 | 85.5 | 79.0 | 8.91 | 6.17 | 0.29 | 4.89 | 13.9% | −30.7% | 1,586% |
| Cobb County, GA | 20.9 | 28.2 | 10.1 | 8.9 | 50.1 | 69.5 | 4.96 | 7.81 | 0.20 | 2.91 | 34.9% | 57.4% | 1,355% |
| Dekalb County, GA | 63.6 | 55.7 | 26.5 | 15.4 | 82.4 | 82.9 | 3.11 | 5.38 | 0.13 | 2.70 | −12.4% | 73.1% | 1,977% |
| Fulton County, GA | 70.5 | 59.6 | 21.6 | 16.9 | 118.9 | 106.1 | 5.50 | 6.28 | 0.16 | 3.01 | −15.5% | 14.1% | 1,781% |
| Gwinnett County, GA | 14.7 | 27.3 | 4.3 | 7.4 | 38.6 | 58.0 | 8.98 | 7.84 | 0.33 | 3.54 | 85.7% | −12.7% | 973% |
| Cook County, IL | 27.2 | 20.3 | 11.1 | 6.1 | 58.7 | 50.6 | 5.29 | 8.30 | 0.34 | 8.33 | −25.4% | 56.9% | 2,350% |
| Marion County, IN | 28.9 | 26.1 | 9.4 | 9.5 | 67.9 | 57.5 | 7.22 | 6.05 | 0.27 | 4.04 | −9.7% | −16.2% | 1,396% |
| East Baton Rouge Parish, LA | 53.2 | 41.7 | 7.8 | 10.6 | 108.1 | 77.8 | 13.9 | 7.34 | 0.12 | 2.34 | −21.6% | −47.0% | 1,850% |
| Orleans Parish, LA | 82.6 | 47.4 | 48.6 | 35.2 | 97.5 | 53.2 | 2.01 | 1.51 | 0.12 | 3.76 | −42.6% | −24.7% | 3,033% |
| Montgomery County, MD | 20.4 | 15.0 | 4.1 | 4.1 | 72.3 | 49.7 | 17.6 | 12.1 | 0.31 | 6.42 | −26.5% | −31.3% | 1,971% |
| Prince George's County, MD | 52.8 | 36.7 | 9.6 | 9.0 | 63.5 | 47.6 | 6.61 | 5.29 | 0.13 | 2.28 | −30.5% | −20.0% | 1,654% |
| Baltimore City, MD | 71.0 | 39.5 | 21.8 | 12.8 | 92.8 | 52.4 | 4.26 | 4.09 | 0.09 | 2.37 | −44.4% | −3.8% | 2,533% |
| Wayne County, MI | 22.4 | 19.6 | 5.9 | 6.7 | 46.5 | 39.3 | 7.88 | 5.87 | 0.24 | 3.79 | −12.5% | −25.6% | 1,479% |
| Clark County, NV | 22.8 | 23.7 | 16.1 | 15.6 | 53.5 | 75.1 | 3.32 | 4.81 | 0.18 | 2.64 | 3.9% | 44.9% | 1,367% |
| Essex County, NJ | 45.3 | 35.4 | 7.2 | 8.1 | 74.1 | 60.9 | 10.3 | 7.52 | 0.17 | 2.48 | −21.9% | −26.9% | 1,359% |
| Hudson County, NJ | 33.4 | 25.9 | 22.5 | 8.2 | 78.4 | 61.6 | 3.48 | 7.51 | 0.33 | 4.89 | −22.5% | 115.6% | 1,382% |
| Bronx County, NY | 46.5 | 42.9 | 9.4 | 6.2 | 66.1 | 69.4 | 7.03 | 11.2 | 0.50 | 4.89 | −7.7% | 59.2% | 878% |
| Kings County, NY | 33.0 | 21.9 | 9.3 | 8.2 | 58.7 | 39.7 | 6.31 | 4.84 | 0.42 | 10.7 | −33.6% | −23.3% | 2,440% |
| New York County, NY | 46.4 | 23.3 | 28.8 | 8.5 | 75.8 | 72.5 | 2.63 | 8.53 | 0.87 | 26.8 | −49.8% | 224.1% | 2,977% |
| Queens County, NY | 23.7 | 18.4 | 8.7 | 3.2 | 30.7 | 33.9 | 3.53 | 10.6 | 0.56 | 8.14 | −22.4% | 200.2% | 1,354% |
| Mecklenburg County, NC | 28.3 | 28.9 | 10.6 | 9.6 | 57.1 | 60.5 | 5.39 | 6.30 | 0.26 | 3.94 | 2.1% | 17.0% | 1,415% |
| Cuyahoga County, OH | 21.4 | 15.4 | 8.0 | 5.0 | 43.0 | 36.6 | 5.38 | 7.32 | 0.37 | 7.42 | −28.0% | 36.2% | 1,905% |
| Franklin County, OH | 23.2 | 19.6 | 13.8 | 9.6 | 51.5 | 48.5 | 3.73 | 5.05 | 0.23 | 8.63 | −15.5% | 35.4% | 3,652% |
| Hamilton County, OH | 24.7 | 25.4 | 12.1 | 16.2 | 57.8 | 49.2 | 4.78 | 3.04 | 0.20 | 3.27 | 2.8% | −36.4% | 1,535% |
| Philadelphia County, PA | 46.9 | 33.6 | 12.0 | 15.4 | 83.3 | 52.9 | 6.94 | 3.44 | 0.41 | 5.40 | −28.4% | −50.5% | 1,217% |
| Shelby County, TN | 37.4 | 34.3 | 6.9 | 9.0 | 57.8 | 51.5 | 8.38 | 5.72 | 0.06 | 1.46 | −8.3% | −31.7% | 2,333% |
| Bexar County, TX | 25.5 | 20.5 | 9.9 | 8.3 | 35.5 | 39.7 | 3.59 | 4.78 | 0.14 | 3.17 | −19.6% | 33.4% | 2,164% |
| Dallas County, TX | 40.3 | 34.2 | 20.8 | 16.2 | 62.2 | 56.8 | 2.99 | 3.51 | 0.15 | 3.37 | −15.1% | 17.2% | 2,147% |
| Harris County, TX | 35.3 | 31.4 | 10.9 | 10.3 | 73.8 | 58.7 | 6.77 | 5.70 | 0.17 | 2.72 | −11.0% | −15.8% | 1,500% |
| Tarrant County, TX | 16.4 | 17.9 | 7.2 | 6.7 | 39.3 | 45.2 | 5.46 | 6.75 | 0.17 | 4.05 | 9.1% | 23.6% | 2,282% |
| Travis County, TX | 23.5 | 16.2 | 14.0 | 7.8 | 45.4 | 36.9 | 3.24 | 4.73 | 0.32 | 10.4 | −31.1% | 45.9% | 3,134% |
| King County, WA | 14.0 | 12.7 | 10.6 | 7.6 | 43.4 | 55.6 | 4.09 | 7.32 | 0.66 | 12.9 | −9.3% | 78.7% | 1,847% |
Values for overall HIV incidence, HIV incidence in White people, HIV incidence in Black people, the Black:White HIV incidence rate ratio (IRR) and PrEP to Need Ratio (PnR) for the EHE jurisdictions included in this analysis for years 2013 and 2019. The percent change in overall HIV incidence (∆% Overall), Black:White IRR (∆% IRR), and PnR (∆%PnR) between years 2013 and 2019 are also presented.
Across all counties, the HIV incidence disparity between Black and White populations ranged from a low of 1.5 in Orleans Parish, LA, to a high of 12.1 in Montgomery County, MD, in 2019. In 43 of 46 counties, HIV incidence among Black people was over 3 times that seen among White people in 2019. In 2019, PrEP use ranged from a high of 26.8 in New York County, NY, to a low of 1.46 in Shelby County, TN (Table 1).
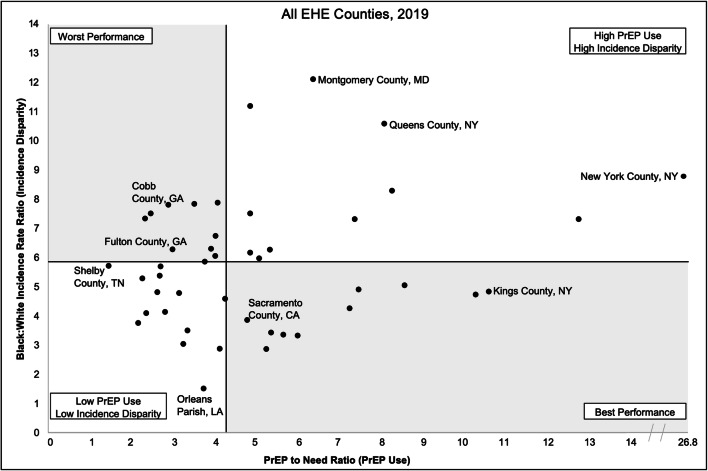
Plotting Performance
Figure 1 provides an integrated comparison of incidence disparity and PrEP use across the 46 EHE counties in 2019. The better-performing counties were those with a PnR above the all-county median of 4.1 and an incidence disparity below the all-county median of 5.7. This signifies relatively high PrEP use, meaning many individuals with a PrEP prescription per HIV diagnosed person (PnR), and a relatively low HIV incidence disparity between Black and White populations. For example, Kings County, NY, performed relatively well, with a PnR of 10.67, and an incidence disparity of 4.84 between Black and White residents.
Fig. 1.
County Performance Plot, 2019. The relationship between county PrEP use (PnR) and the HIV incidence disparity between White and Black populations (IRR) for the year. Quadrants represent counties that performed relatively well or poor on both or one metric. The horizontal and vertical reference lines represent the calculated median value for each metric among the group of 46 EHE counties included in the analysis.
The lower-performing counties were those with a PnR below the all-county median and an incidence disparity above the median, indicating low PrEP use and high incidence disparity. For example, Cobb County, GA, performed relatively poorly, with a PnR of 2.91 and an incidence disparity of 7.81.
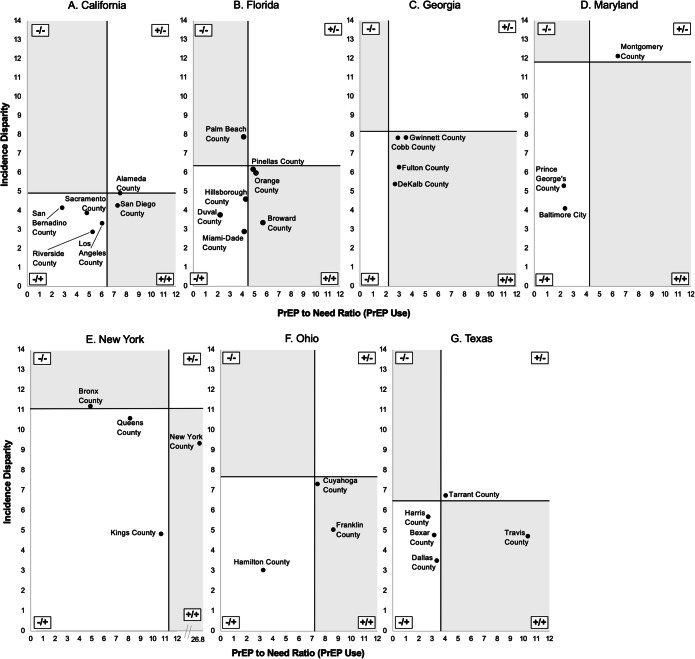
State Analyses
There were 7 states that contained more than 3 EHE priority counties, including California (6), Florida (7), Georgia (4), Maryland (3), New York (4), Ohio (3), and Texas (5). We identified variation in both HIV incidence disparity and PrEP use for the EHE counties within these states (Fig. 2(A–G)). For example, across the 6 EHE counties in California, the incidence disparity ranged from a low of 2.86 in Riverside County to a high of 4.90 in Alameda County, while PnR ranged from a high of 7.52 in Alameda County to a low of 2.83 in San Bernadino County (Fig. 2(A)).
Fig. 2.
State-level Performance Plots, 2019. (A–G) The relationship between PrEP use (PnR) and the HIV incidence disparity between White and Black populations (IRR) for the year 2019 among the seven states with more than three EHE counties. The vertical crossline indicates the State PnR and the horizontal crossline indicates the State IRR. Each quadrant includes the following notation to describe the relationship between PnR and IRR: (−/+): low PnR, low HIV IRR, (+/−): high PnR, high HIV IRR, (−/−): low PnR, high HIV IRR, (+/+): high PnR, low HIV IRR.
Changes in Overall Incidence and Incidence Disparity
Across the 46 EHE counties, the largest percent change in overall HIV incidence (85.7%) between 2013 (14.7) and 2019 (27.3) was observed in Gwinnett County, GA, while the smallest percent change in overall HIV incidence (−51.4%) was observed for Washington, D.C., which had an overall incidence of 86.9 in 2013 which decreased to 42.2 in 2019 (Table 1). The largest percent change in incidence disparity (+224.1%) between 2013 (2.63) and 2019 (8.53) was observed for New York County, NY. The smallest percent change was observed in Philadelphia County, PA, as the incidence disparity decreased by 50.5% between 2013 and 2019 (6.94 vs. 3.44).
All 46 EHE counties reported positive percent increases in PnR between 2013 and 2019 (Table 1). The largest percent increase in PnR (3,652.2%) was observed for Franklin County, OH, which had a PnR of 0.23 in 2013 that increased to 8.63 in 2019. The smallest percent increase in PnR (878.0%) was observed for Bronx County, NY, which had a PnR of 0.50 in 2013 which increased to 4.89 in 2019 (Table 1).
We observed a moderately strong, statistically significant correlation between percent change in PrEP use (PnR) and the percent change in overall HIV incidence (ρ = −0.42, p = .004), indicating that the larger the percent increase in PnR, the greater the percent decrease in overall HIV incidence between 2013 and 2019 (Table 1). However, we observed no relationship between the percent change in PrEP use and the percent change in HIV incidence disparity (IRR) (ρ = 0.06, p = .69). Similarly, the correlation between the 2019 single-year incidence disparity and PrEP use was not statistically significant (ρ = 0.19, p = .21).
DISCUSSION
Our analysis of 46 EHE counties identified, (1) considerable cross-county variation in PrEP use (PnR), HIV incidence disparities (IRR), and percent changes in incidence disparities, and (2) a significant, negative correlation between changes over time in PrEP use and overall HIV incidence, but no relationship between change in PrEP use and change in HIV incidence disparity.
Across the country, PnR varied, with counties in the South demonstrating lower PnRs relative to counties in the Northeast or West. Of the 20 counties with the lowest PnRs, more than half were in the South. Studies exploring regional differences in PrEP uptake in the USA suggest that PrEP uptake may be lower in Southern counties because of their dispersed population across rural areas, comparatively lower numbers of PrEP providers, low rates of health insurance, lack of Medicaid expansion, and significant social stigma surrounding PrEP and HIV.12,22,23
While impacted by the same state-level policies and regulations, EHE counties within a single state did not perform uniformly regarding PrEP use, HIV incidence disparities, or changes in these metrics. Across the 7 states with 3 or more EHE counties, it was not uncommon to observe a two- to threefold difference in PrEP use or HIV incidence disparities between counties with higher and lower performance. Furthermore, there was considerable variability between the EHE counties in a state with respect to changes in incidence, incidence disparities, and PrEP use over the years of U.S. PrEP availability (2013–2019).
Some counties were successful in both increasing PrEP use and simultaneously reducing HIV incidence disparities, while others recorded worsening disparities alongside increased PrEP use. For example, New York County, NY, recorded the highest PrEP use in 2019 (PnR = 26.8) but also the greatest increase in incidence disparity between Black and White people (224.1%) of all EHE counties in this analysis. This increase in disparity was accompanied by a 49.8% decrease in the overall county HIV incidence rate. Combined, these results show that New York County made progress in expanding PrEP use overall, but suggests PrEP prescriptions were disproportionately given to White people as the incidence disparity increased during the same period. In the same state, Kings County, NY, recorded a 2,440.0% increase in PnR between 2013 and 2019 while simultaneously reporting a 23.3% decrease in incidence disparity, suggesting that PrEP prescriptions were distributed more equitably.
While individual counties reported encouraging changes in incidence disparities and PrEP use, when considering all the EHE counties, there was a significant negative correlation between changes in PrEP use and overall HIV incidence and the lack of relationship between changes in PrEP use and HIV incidence disparities. Taken together, these findings suggest that while PrEP has shown success in reducing HIV incidence, it has not moved the needle on the marked disparities in new HIV diagnoses. These disparities may be due to racial biases in prescribing practices, lack of PrEP providers in communities of color, lower PrEP awareness, and stigma surrounding PrEP among Black populations.24–26 Ultimately, the observed disparities in HIV incidence in the EHE counties are the product of a combination of gaps at the level of individual clinicians, patients, local health departments, and health systems which in sum create systemic and structural barriers to reducing HIV incidence among Black populations.25,26 Interventions addressing these barriers to improve PrEP implementation and decrease the Black:White HIV incidence disparity must also adopt this multilevel structure.27
Local health departments and community partners in EHE counties are tasked with implementing comprehensive strategies to reduce HIV incidence through increasing prevention (PrEP uptake) and treatment (identification, linkage, and retention).9,28 Assessing the relationship between local PnR and HIV disparities can guide allocation of resources and development of indicators to monitor impact of implementation strategies. Local-level measures of PnR using open access and surveillance data could be used to develop and influence HIV prevention strategies while simultaneously ensuring these strategies do not exacerbate existing racial disparities or create new ones. The cross-county (both national and within-state) variation observed in our analysis reinforces the value of focusing on smaller units of geography when evaluating epidemiologic trends in HIV incidence and PrEP use to develop and evaluate interventions. Smaller units of geography (e.g., county), particularly those in the same state, may also invite the opportunity to identify models of best practice for reducing HIV incidence, incidence disparities, and scale up of PrEP for other counties operating under the same state policy environment.
Limitations
The findings of the current study should be interpreted in the context of several limitations. First, our analysis is ecological at the county-level, which limits the ability to establish a causal relationship between PrEP use and changes in disparities. Correlation analyses can present evidence of a trend however do not allow us to make a direct conclusion about the use of PrEP and incidence rates, disparities in incidence, or changes in these metrics. Furthermore, we are unable to make assessments or analyses of which, if any, state-level policies or programs may have led to changes in HIV incidence disparity or PrEP use for a one group of counties compared to another; however, this is an important area of future study.
A related set of limitations are those related to HIV incidence disparities overall. First, our focus on White or Black race only did not allow us to evaluate correlations based on other racial/ethnic identities, which is an important avenue for future work given the documented disparities in PrEP use and HIV incidence among Latinx people in the USA.1 Second, the NCHHSTP datasets do not account for the known disparities in HIV testing frequency between White and Black people which may exacerbate the frequency of HIV diagnosis with more frequent testing among Black people.29,30
Our estimates of county PnR likely reflect lower bounds, as a conservative approach was used to identify PrEP users and the publicly available dataset does not contain prescription information from closed healthcare systems (e.g., Kaiser Permanente in California).18,31 AIDSVu data also do not provide a breakdown of PrEP prescriptions filled by patient race.18,31 Thus, it was not possible for us to draw a direct connection between the racial disparities in HIV incidence and known racial disparities in PrEP prescription.6,8 Collection and dissemination of this type of more granular data would be an interesting area of future research and may allow for a more nuanced relationship between PrEP prescription and HIV incidence disparities to be investigated.
Finally, it is important to note that PnR does not account for duration of PrEP use, adherence to PrEP, or whether the medication was actually used by the prescribed patient, and thus we cannot assess longitudinal impact of prescriptions on HIV incidence which may be important given some reports of an approximate 40% PrEP discontinuation rate.32 Future PnR calculations should consider prescription renewals or refill data to derive robust measures of use and assess impact of duration on incidence. Additionally, our analysis was limited by its cross-sectional design and future work investigating the changes in PnR and HIV incidence disparity over time may provide more detailed and actionable information for embarking on the next phases of the EHE.
CONCLUSIONS
Establishing the EHE priority counties was an important first step towards truly ending the HIV epidemic in the USA. However, the results of the present analysis show that significant work remains in reducing HIV incidence among communities of color. As modalities of PrEP are diversifying, with approval of a long-acting injectable PrEP formulation (cabotegravir), it is crucial that equitable access and implementation be planned to ensure the gap between Black and White HIV incidence does not widen further. Allocation of resources to smaller units of geography, especially those areas that disproportionately report new HIV diagnoses, will make important inroads towards interrupting the continually high annual HIV incidence in the USA. However, focus must shift from reducing incidence overall to reducing disparities in HIV incidence.
Supplementary Information
(DOCX 44 kb)
Declarations
Conflict of Interest
SRB and AH report receiving unrestricted research funding from Gilead Sciences for research unrelated to the present study. The authors declare that they have no other conflicts of interest to disclose.
Footnotes
Previous Presentations
No portions of the work described in this manuscript have been presented previously.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control & Prevention. HIV Surveillance Report, 2019. 2021.
- 2.U.S. Preventive Services Task Force. Owens DK, Davidson KW, et al. Preexposure Prophylaxis for the Prevention of HIV Infection: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;321(22):2203–2213. doi: 10.1001/jama.2019.6390. [DOI] [PubMed] [Google Scholar]
- 3.Riddell J, Amico KR, Mayer KH. HIV Preexposure Prophylaxis: A Review. JAMA. 2018;319(12):1261–1268. doi: 10.1001/jama.2018.1917. [DOI] [PubMed] [Google Scholar]
- 4.Philpott S. Social justice, public health ethics, and the use of HIV pre-exposure prophylaxis. Am J Prev Med. 2013;44(1 Suppl 2):S137–140. doi: 10.1016/j.amepre.2012.09.029. [DOI] [PubMed] [Google Scholar]
- 5.Caceres CF, Koechlin F, Goicochea P, et al. The promises and challenges of pre-exposure prophylaxis as part of the emerging paradigm of combination HIV prevention. J Int AIDS Soc. 2015;18(4 Suppl 3):19949. doi: 10.7448/IAS.18.4.19949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control & Prevention. 2019 National HIV Surveillance System Reports: PrEP Coverage in the U.S. by Race/Ethnicity, 2019. https://www.cdc.gov/nchhstp/newsroom/2021/2019-national-hiv-surveillance-system-reports.html#Graphics. Published 2021. Accessed September 2021.
- 7.Siegler AJ, Mouhanna F, Giler RM, et al. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol. 2018;28(12):841–849. doi: 10.1016/j.annepidem.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siegler AJ, Mehta CC, Mouhanna F, et al. Policy- and county-level associations with HIV pre-exposure prophylaxis use, the United States, 2018. Ann Epidemiol. 2020. [DOI] [PMC free article] [PubMed]
- 9.U.S. Department of Health and Human Services. About Ending the HIV Epidemic in the U.S. https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview. Published 2021. Accessed October 2021.
- 10.Centers for Disease Control & Prevention. Ending the HIV Epidemic in the U.S. (EHE): Jurisdictions. https://www.cdc.gov/endhiv/jurisdictions.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fendhiv%2Fpriorities.html. Published 2021. Accessed October 2021.
- 11.Sullivan PS, Giler RM, Mouhanna F, et al. Trends in the use of oral emtricitabine/tenofovir disoproxil fumarate for pre-exposure prophylaxis against HIV infection, United States, 2012-2017. Ann Epidemiol. 2018;28(12):833–840. doi: 10.1016/j.annepidem.2018.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reif S, Cooper H, Warren M, Wilson E. HIV in the U.S. Deep South: Trends from 2008-2019. Durham NC: Center for Health Policy and Inequalities Research, Duke University; 2021.
- 13.Cramer R, Leichliter JS, Gift TL. Are safety net sexually transmitted disease clinical and preventive services still needed in a changing health care system? Sex Transm Dis. 2014;41(10):628–630. doi: 10.1097/OLQ.0000000000000187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cuffe KM, Esie P, Leichliter JS, Gift TL. HIV Services Provided by STD Programs in State and Local Health Departments - United States, 2013-2014. MMWR Morb Mortal Wkly Rep. 2017;66(13):355–358. doi: 10.15585/mmwr.mm6613a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leichliter JS, Seiler N, Wohlfeiler D. Sexually Transmitted Disease Prevention Policies in the United States: Evidence and Opportunities. Sex Transm Dis. 2016;43(2 Suppl 1):S113–121. doi: 10.1097/OLQ.0000000000000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pearson WS, Kumar S, Habel MA, et al. Sexually transmitted disease clinics in the United States: Understanding the needs of patients and the capabilities of providers. Prev Med. 2021;145:106411. doi: 10.1016/j.ypmed.2020.106411. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control & Prevention. NCHHSTP AtlasPlus. https://www.cdc.gov/nchhstp/atlas/index.htm. Accessed September 2021.
- 18.Sullivan PS, Woodyatt C, Koski C, et al. A Data Visualization and Dissemination Resource to Support HIV Prevention and Care at the Local Level: Analysis and Uses of the AIDSVu Public Data Resource. J Med Internet Res. 2020;22(10):e23173. doi: 10.2196/23173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacCannell T, Verma S, Shvachko V, Rawlings K, Mera R. Validation of a Truvada for PrEP Algorithm using an Electronic Medical Record. 8th IAS Conference on HIV Pathogenesis, Treatment & Prevention; July, 2015; Vancouver, Canada.
- 20.U.S. Census Bureau. American Community Survey Data Tables: Table B02001. 2021.
- 21.U.S. Census Bureau. QuickFacts United States Population Estimates. https://www.census.gov/quickfacts/fact/table/US/PST045219. Published 2021. Accessed October 2021.
- 22.Karletsos D, Stoecker C. Impact of Medicaid Expansion on PrEP Utilization in the US: 2012-2018. AIDS Behav. 2021;25(4):1103–1111. doi: 10.1007/s10461-020-03070-2. [DOI] [PubMed] [Google Scholar]
- 23.Colasanti JA, Armstrong WS. Challenges of reaching 90-90-90 in the Southern United States. Curr Opin HIV AIDS. 2019;14(6):471–480. doi: 10.1097/COH.0000000000000577. [DOI] [PubMed] [Google Scholar]
- 24.Ojikutu BO, Bogart LM, Higgins-Biddle M, et al. Facilitators and Barriers to Pre-Exposure Prophylaxis (PrEP) Use Among Black Individuals in the United States: Results from the National Survey on HIV in the Black Community (NSHBC) AIDS Behav. 2018;22(11):3576–3587. doi: 10.1007/s10461-018-2067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mayer KH, Agwu A, Malebranche D. Barriers to the Wider Use of Pre-exposure Prophylaxis in the United States: A Narrative Review. Adv Ther. 2020;37(5):1778–1811. doi: 10.1007/s12325-020-01295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pleuhs B, Quinn KG, Walsh JL, Petroll AE, John SA. Health Care Provider Barriers to HIV Pre-Exposure Prophylaxis in the United States: A Systematic Review. AIDS Patient Care STDs. 2020;34(3):111–123. doi: 10.1089/apc.2019.0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pinto RM, Berringer KR, Melendez R, Mmeje O. Improving PrEP Implementation Through Multilevel Interventions: A Synthesis of the Literature. AIDS Behav. 2018. [DOI] [PMC free article] [PubMed]
- 28.Horn T, Sherwood J, Remien RH, et al. Towards an integrated primary and secondary HIV prevention continuum for the United States: a cyclical process model. J Int AIDS Soc. 2016;19(1):21263. doi: 10.7448/IAS.19.1.21263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lo CC, Runnels RC, Cheng TC. Racial/ethnic differences in HIV testing: An application of the health services utilization model. SAGE Open Med. 2018;6:2050312118783414. doi: 10.1177/2050312118783414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henny KD, Zhu W, Huang YA, Townes A, Delaney KP, Hoover KW. HIV Testing Trends Among Persons with Commercial Insurance or Medicaid - United States, 2014-2019. MMWR Morb Mortal Wkly Rep. 2021;70(25):905–909. doi: 10.15585/mmwr.mm7025a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.AIDSVu. Data Methods – National-, Regional-, State-, County-Level. https://aidsvu.org/data-methods/data-methods-statecounty/. Accessed September 2021.
- 32.van Epps P, Maier M, Lund B, et al. Medication Adherence in a Nationwide Cohort of Veterans Initiating Pre-exposure Prophylaxis (PrEP) to Prevent HIV Infection. J Acquir Immune Defic Syndr. 2018;77(3):272–278. doi: 10.1097/QAI.0000000000001598. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 44 kb)