Abstract
Background
Interdisciplinary teams (IDTs) have been implemented to improve collaboration in hospital care, but their impact on patient outcomes, including readmissions, has been mixed. These mixed results might be rooted in differences in organization of IDT meetings between hospitals, as well as variation in IDT characteristics and function. We hypothesize that relationships between IDT members are an important team characteristic, influencing IDT function in terms of how members make sense of what is happening with patients, a process called sensemaking
Objective
(1) To describe how IDT meetings are organized in practice, (2) assess differences in IDT member relationships and sensemaking during patient discussions, and (3) explore their potential association with risk-stratified readmission rates (RSRRs).
Design
Observational, explanatory convergent mixed-methods case-comparison study of IDT meetings in 10 Veterans Affairs hospitals.
Participants
Clinicians participating in IDTs and facility leadership.
Approach
Three-person teams observed and recorded IDT meetings during week-long visits. We used observational data to characterize relationships and sensemaking during IDT patient discussions. To assess sensemaking, we used 2 frameworks that reflected sensemaking around each patient’s situation generally, and around care transitions specifically. We examined the association between IDT relationships and sensemaking, and RSRRs.
Key Results
We observed variability in IDT organization, characteristics, and function across 10 hospitals. This variability was greater between hospitals than between teams at the same hospital. Relationship characteristics and both types of sensemaking were all significantly, positively correlated. General sensemaking regarding each patient was significantly negatively associated with RSRR (− 0.65, p = 0.044).
Conclusions
IDTs vary not only in how they are organized, but also in team relationships and sensemaking. Though our design does not allow for inferences of causation, these differences may be associated with hospital readmission rates.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07744-6.
KEY Words: care transitions, readmissions, interdisciplinary teams, sensemaking
BACKGROUND
Since the Hospital Readmissions Reduction Program was instituted, improving patients’ transitions from hospitals to home has received attention (https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/HRRP/Hospital-Readmission-Reduction-Program). Effective transitions require multiple complementary interventions, including medication reconciliation, patient/family education, home services, and timely follow-up care.1 Accomplishing these tasks requires collaboration between patients, caregivers, and clinicians.2
To promote interdisciplinary collaboration, the Joint Commission requires creating interdisciplinary care plans for all hospitalized patients.3 However, usual inpatient care poses challenges for clinicians to communicate directly and coordinate each patient’s care and post-discharge plans. Interdisciplinary team (IDT) meetings, also known as interprofessional rounds, have been widely implemented as opportunities to coordinate care,4–6 enabling clinicians to discuss patients’ unique situations, develop shared understandings, and integrate care plans.3 Meetings may be held in nursing stations, in conference rooms, or at the bedside.5,6
Despite their ubiquity, IDT implementation is not consistently associated with decreased readmission rates or length of stay.5 Three systematic reviews of IDT meetings note variability in organization, including timing, location, and participants.5–7 One potential reason for inconsistent outcomes is variability in how IDT meetings actually improve team function.8,9
We sought to examine IDT meetings in practice, to see if IDTs could be distinguished based on team characteristics and function, and explore whether differences were associated with readmission rates. Based on our prior work, we considered relationships a key team characteristic. Healthcare team relationships have been studied across settings, demonstrating the association between relationships and a range of patient outcomes.10–15 Relationships are essential to supporting effective team function, shaping how team members develop shared understandings of what is happening.10,13
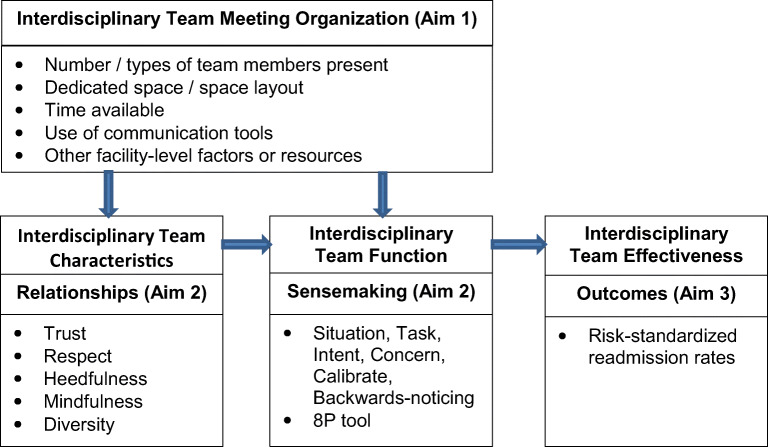
These shared understandings are the foundation for action, a process called sensemaking. Sensemaking in healthcare is a social activity through which patients, caregivers, and clinicians use their shared understanding to act.10,11 For example, recognizing a complication quickly, and acting to intervene, is an example of sensemaking.16 Similarly, recognizing a caregiver’s limitations in managing a new condition after hospitalization, and deploying home services, is also sensemaking. The ways IDT meetings are organized may impact team relationships, influencing how teams function in making sense of what is happening, and in turn impacting team effectiveness and patient outcomes such as readmission rates (Fig. 1).
Figure 1.
Conceptual model linking relationships and sensemaking during IDT meetings, and readmission rates.
The aims of this paper are to (aim 1) describe IDT meeting organization in practice; (aim 2) assess whether IDTs can be distinguished based on team relationships and sensemaking through examining patient care discussions; and (aim 3) explore the association between IDT relationships, sensemaking, and risk-stratified readmission rates (RSRR).
METHODS
Design/Setting
We analyzed data from a convergent, mixed-methods, observational study17 of care transitions and readmissions conducted in 10 Veterans Affairs hospitals purposively selected18 based on prior participation in at least one national readmissions improvement initiative, and having 5-year trends of either improving or worsening RSRRs.19 We conducted week-long observational visits at each hospital from 2015 to 2018, collecting qualitative and quantitative data to assess associations between relationships, sensemaking, and RSRRs. In convergent designs, qualitative and quantitative data are triangulated for analysis, which may include quantification of qualitative data, or vice versa.17 We converted qualitative data to quantitative data for statistical analysis to test our conceptual model, utilizing this explanatory observational approach to study associations between observed IDT organization, characteristics, function, and outcomes. This study was approved by the University of Texas Health San Antonio Institutional Review Board and the South Texas Veterans Health Care System Research and Development Committee.
Recruitment
Inpatient medicine physicians were contacted for permission to observe IDT meetings. At the first meeting observed for each team, we distributed IRB-approved information sheets to participants and asked permission to record discussions.
Descriptions of IDT Meeting Organization
Three-person teams conducted observations, including a general internist, clinical health psychologist, and medical anthropologist or organizational researcher. All had qualitative and mixed-methods research experience. To observe the greatest variation in IDTs, and include patients from all medical units, we sought to observe at least one IDT meeting per team during each site visit.
We used a structured template to document IDT organization: location and timing of meetings, number and roles of participants, use of structured communication tools to guide discussions, and who spoke. We described the topics discussed and noted anything that seemed relevant to team function, such as whether people were paying attention or when people entered or left the room.
Assessing Relationships
To assess relationships in a standardized way across teams, we audio-recorded and transcribed IDT meetings, identifying discussions of patients definitely or potentially being discharged home. Discussions of patients being transferred to another healthcare setting, or who were expected to die, were excluded. We selected the two longest discussions for in-depth content analysis. For the few observations we could not record, we only included patient discussions if detailed field notes from two observers were available, selecting the longest discussions based on word count. Using qualitative content analysis,20 two research team members with mixed-methods and qualitative experience (JP and HL) coded transcripts and field notes of sampled discussions. Both coders had significant previous experience coding the variables included in this analysis.
We assessed relationships using a framework previously developed in healthcare settings, focusing on characteristics relevant to IDTs: trust, respect, heedfulness, mindfulness, and diversity.12 We developed a codebook from this framework to assess these characteristics, and reviewed transcripts using these codes to identify instances of each of these characteristics. If we observed positive instances of a characteristic, a rating of “1” was given. If we did not observe evidence of a characteristic, or observed a negative example, a “0” was given. Table 1 summarizes definitions and examples. The number of present characteristics was summed for each discussion to yield scores from 0 to 4. The two coders worked together on the first four transcripts to ensure a consistent analytical approach. The remaining transcripts were divided equally among the coders to code independently. The coding for each transcript was then jointly reviewed, discussed, and modified if needed to reach final consensus.
Table 1.
Definitions and Examples of Relationship Characteristics in IDTs
| Trust | |
|
• Expressing vulnerability; demonstrating confidence in other team members; accepting peers’ clinical judgments, particularly those lower in hierarchy or of other professions; deferring to/asking for another’s judgment; asking to discuss an issue as a team • Berating/belittling others is considered mistrust | |
|
• Team member saying “I don’t know.” “I defer to your judgment,” “I would like your input,” “I think we need to discuss as a team,” etc. • Team member asking for others’ input on what’s happening | |
| Respect | |
|
• Extent to which team members listen to each other, allow each other to talk without interruption, and consider each other’s suggestions • Interruptions/over-talking are not always a sign of disrespect (they might be cooperative interruptions). Observed interruptions should be interpreted in context of interactions | |
|
• Case manager interrupting an attending to add to what attending is saying • Attending listening without interruption to a nurse | |
| Heedfulness | |
|
• Acknowledging potential/actual impact of one’s behaviors on others’ tasks, on patient care, or on disposition planning • Can include offering help, sympathy, or empathy | |
|
• Attending says, “Sorry I held you up,” because he has not signed a note, preventing social worker from making discharge arrangements • Inconsiderate: physician saying “I don’t think I need to do that.” | |
| Mindfulness | |
|
• Responding to each other’s ideas for the evolving plan. Suggesting new ideas or discussing how team might do things differently • Being open to new possibilities | |
|
• Medical student expresses concern about sending patient home alone; the attending agrees it is difficult and reports on his conversation with nurse related to those concerns • Utilization management (UM) nurse reports patient not meeting admission criteria, but recognizes that team was not comfortable discharging the patient |
Because IDTs are intended to enhance collaboration and communication across professions, we thought diversity was particularly important21–23 and considered diversity separately. While physicians always speak, other participants’ contributions vary. Therefore, we assessed diversity by calculating the ratio of non-physician speakers to total speakers. Higher ratios reflected greater diversity.
Assessing Sensemaking
Clinical teams make sense of many different aspects of hospitalized patients’ circumstances and care trajectory.10 Similar to our prior work examining inpatient sensemaking, we applied two complementary frameworks for assessing different aspects of sensemaking in the sampled IDT disussions.10 The same two researchers coded the data for sensemaking using the approach described above.
Sensemaking framework 1—STICC+: We previously used the Situation, Task, Intent, Concern, and Calibrate (STICC)24–28 framework to assess inpatient physician team sensemaking.10 STICC encompasses general assessments of patients’ illnesses and social situations, making it appropriate to examine IDT discussions. An additional sensemaking concept, “backward noticing,”29 or discussion of prior events, also seemed relevant, as it could encompass discussions of patients’ prior situations, or prior patients with similar circumstances. Therefore, we included backward noticing as an additional component, calling this expanded framework STICC+. Table 2 summarizes STICC+ definitions and examples. For each patient discussion, we noted the presence or absence of each STICC+ element, assigning “1” if present or “0” if absent, yielding scores ranging from 0 to 6.
Table 2.
Definitions and Examples of STICC + Sensemaking in IDTs Situation
| • Discussion of patient’s situation, including working diagnosis, clinical status, home environment | |
|
• Attending explains that when at home, the patient got confused about his medications and that was why he was admitted • The resident reports nothing new overnight; the patient is constipated | |
| Task | |
| • Discussion about specific care tasks and activities that need to be done | |
|
• Attending tells resident to coordinate with urology to get “boxes lined up” for discharge • Case manager says she will send orders to resident for signature | |
| Intent | |
| • Explanation of rationale for actions in the care plan | |
|
• Attending quotes article as the rationale for new medication • Resident says plan is to keep patient hospitalized because she will pass soon | |
| Concern | |
|
• Discussion of concerns; things that could go wrong; aspects of plan that fall short • Discussions of back-up plans should something go wrong with current plan | |
|
• Nurse raises concern that patient will be discharged without having a bowel movement. Physicians will give patient medication to induce one • Nurse is concerned about a patient being “wobbly.” Attending says PT will see patient to “clear” him going home | |
| Calibrate | |
| • Feedback from team sought regarding plan, or concerns or adjustments to consider | |
| • Attending and resident had planned to discharge patient. Social worker states nurses’ concern that patient is too weak to walk, and would like a physical therapy evaluation. Attending agrees | |
| Backward noticing | |
| • Encompasses processing past events and applying them to current situation. Specifically, includes discussing (1) prior patients with similar issues or (2) current patient’s prior events | |
| • Attending says patient’s situation has “snowballed” since his wife died—he is depressed, does not go out, and has lost strength. The resident notes the patient was hospitalized 3 times for this issue |
Sensemaking framework 2—8Ps: IDT discussions often focus on care transitions. We wanted to assess sensemaking regarding care transitions using an alternative framework specific to this task. We used the Project Boost “8P” Screening Tool elements30, 31 to assess discussion of factors known to be associated with risk of readmissions and adverse events post-discharge: (1) potential medication issues; (2) psychological/mental status; (3) principal diagnosis; (4) physical limitations; (5) poor health literacy or adherence; (6) family/caregiver support; (7) hospitalizations in prior 6 months; and (8) palliative care or goals of care. We coded patient discussions for comments reflecting each factor, scoring “0” if the factor was not mentioned; “1” if the factor was mentioned; and “2” if the factor was discussed in detail. Global comments such as “this patient has no needs,” with no other discussion, were assigned 0s for all 8P elements. Summing the eight elements yielded total 8P scores ranging from 0 to 16.
Assessing RSRRs
RSRRs are calculated quarterly to assess readmissions in VA hospitals, and are adjusted for 40 patient demographic and medical conditions, using guidelines from the Agency for Healthcare Research and Quality.32 RSRRs for the 21 months surrounding each site visit were obtained from the VA Hospital-Wide 30-day Readmission Cube.33 Because values from one quarter to the next could vary by up to two percentage points, we calculated a 21-month best-fit RSRR for each hospital using the RSRR from four quarters prior to the visit, the quarter that included the visit, and two quarters after the visit, building a linear regression model from the 7 RSRRs and using the predicted value from the quarter of the visit, as described previously.34
Data Analysis
We calculated descriptive statistics for discussion time, speaker diversity, relationship characteristics, sensemaking STICC+, and sensemaking 8P scores for each sampled patient discussion, averaging across patient discussions for each team, and across teams for each hospital. For each variable, we compared variability in scores between teams within each hospital to variability between hospitals using single-factor ANOVAs.
We tested associations between relationships, sensemaking (STICC+), sensemaking (8P), and RSRR, using the Spearman correlation coefficient (designed for ordinal variables). Analyses were done using R, version 3.6.3.35
RESULTS
Descriptions of IDTs
During 45 unique IDT meetings across the 10 hospitals, we observed 1205 patient discussions among 62 of 67 (92.5%) unique teams (some meetings included multiple teams in succession). Each IDT included physicians and one or more other healthcare professionals. Table 3 summarizes numbers of IDTs and discussions observed. Thirty-seven of 45 meetings were audio-recorded; one recording was unusable due to poor quality. Eight were not recorded due to participant request (n = 3) or recording challenges (n = 5). Physician participants included both teaching teams and attending physicians working alone. The average number of patients discussed per IDT ranged from 7.3 to 14.7 across hospitals. Four teams had only one discussion of a patient being discharged home. The longest sampled timed patient discussions ranged from 7 to 514 s with a mean (sd) of 121 (94); hospital averages ranged from 42 to 203 s.
Table 3.
Summary of IDT Observations at Each Hospital
| Hospital | # of attending physician teams observed/% total | Number of IDT observations | # of patient discussions observed | Patients discussed per physician mean (range) | Average and range patient discussion time (s) |
|---|---|---|---|---|---|
| 1 | 6 (100%) | 6 | 66 | 10.3 (7–12) | 64 (30–126) |
| 2 | 4 (80%) | 4 | 56 | 14 (11–18) | 190 (104–295) |
| 3 | 14 (100%) | 3 | 285 | 7.3 (4–12) | 42 (7–147) |
| 4 | 5 (100%) | 3 | 62 | 8.9 (6–12) | 203 (95–464) |
| 5 | 5 (100%) | 3 | 185 | 13.2 (10–16) | 82 (62–115) |
| 6 | 5 (83.3%) | 5 | 72 | 7.9 (3–11) | 143 (71–280) |
| 7 | 5 (100%) | 4 | 200 | 10 (4–20) | 130 (78–213) |
| 8 | 5 (71.4%) | 5 | 34 | 8.5 (7–12) | 177 (50–368) |
| 9 | 6 (100%) | 4 | 147 | 14.7 (12–18) | 161 (62–410) |
| 10 | 7 (87.5%) | 8 | 98 | 12.3 (5–16) | 150 (8–514) |
| Total | 62 (92.5%) | 45 | 1205 | N/A | 121 (7–514) |
We saw variability between hospitals in the organization of IDTs. Meetings were held either separately in dedicated team-specific work rooms or in centralized conference rooms or shared unit break/work rooms through which multiple team participants rotated. Meetings held in team-specific work rooms, and in which social workers and/or case managers were assigned by team rather than unit, appeared to have more focused and efficient patient discussions. In scenarios in which multiple teams rotated through shared conference or break rooms, more people were physically present, but not every individual had a role in every discussion. These meetings tended to be noisier and have people who were not paying attention, and were more likely to have “false starts” with confusion about which patient was being discussed. They were also more likely to include participation or observation by leadership or non-team personnel (e.g., chief hospitalist). The space layout also influenced discussions through facilitating or hindering participants’ abilities to face and visually attend to each other during discussions.
Use of structured checklists or “scripts” to guide discussion was limited; one hospital used a projected spreadsheet to prompt discussion about patient status or risk factors, tracking factors throughout the hospitalization and focusing participants on salient issues.
IDT composition varied greatly between hospitals (Appendix Table 6). Besides physicians, social workers consistently participated at all 10 hospitals. Other professions’ participation was less consistent, even within sites. Bridging/transition roles (i.e., someone who interacted with patients across inpatient and outpatient settings) were only present at two hospitals on a limited basis for disease-specific groups (e.g., CHF) or high-risk patients. Bedside nurses attended IDT meetings at only one hospital, although unit nurse managers participated at four hospitals. One hospital had two unique roles: (1) a clerk who functioned as post-discharge appointment coordinator and (2) a post-discharge coordinator who made follow-up phone calls to all patients. Five hospitals included utilization management.
Relationships
Relationship characteristic scores ranged across hospitals from 0.9 to 3.1. Trust was most frequently observed (58% of patient discussions), while respect (42%), mindfulness (41%), and heedfulness (34%) were observed less often. Speaker diversity as assessed by ratio of team members who spoke ranged from 0.33 to 0.63. Across the sampled discussions, the total number of speakers ranged from 1 to 6. In 16 discussions (14%), only a physician spoke; all of these were at one hospital. Single-factor ANOVAs indicated that the relationship variance between hospitals was significantly greater than the variance among teams within hospitals (all p < 0.0001) (Table 4).
Table 4.
Assessment of Relationships, Sensemaking, and RSRR at Each Site
| Site | Relationship score* | Speaker diversity | STICC+ score | 8P score | RSRR |
|---|---|---|---|---|---|
| 1 | 0.9 | 0.62 | 3.0 | 2.3 | 16.1 |
| 2 | 2.4 | 0.54 | 3.0 | 2.5 | 15.2 |
| 3 | 0.5 | 0.33 | 2.4 | 1.5 | 14.7 |
| 4 | 2.7 | 0.75 | 4.0 | 4.9 | 12.8 |
| 5 | 2.1 | 0.63 | 3.8 | 4.0 | 13.0 |
| 6 | 3.1 | 0.43 | 4.3 | 4.2 | 14.1 |
| 7 | 1.3 | 0.55 | 3.8 | 3.5 | 11.9 |
| 8 | 2.0 | 0.56 | 3.3 | 2.6 | 13.1 |
| 9 | 2.5 | 0.44 | 4.0 | 3.5 | 11.8 |
| 10 | 2.0 | 0.53 | 3.7 | 3.1 | 12.9 |
*Relationship score includes trust, respect, mindfulness, and heedfulness
Sensemaking
IDT discussions varied from brief pronouncements about patients’ status or discharge disposition (“no change” or “going home today, no needs”), or succinct physician updates, to prolonged interactive discussions.
Discharge barriers dominated most discussions. Readmission risk factors were infrequently discussed. Participants sometimes noted that patients were “bounce-backs,” but rarely discussed future readmission risk. Some hospitals were unique in terms of focusing on specific areas. For example, IDT participants at one hospital discussed each patient’s transportation needs, while participants at another hospital noted scheduling of primary care follow-up appointments (time frame and whether in-person or by phone).
Sensemaking (general STICC+ and transition-specific 8P) scores are detailed in Table 4. STICC+ scores ranged from 2.4 to 4.3 between hospitals. Appendix Table 7 details the frequency of STICC+ and 8P discussion items. Situation and Task were observed in over 90% of discussions; Intent and Concern were observed in half to two-thirds of discussions, while Calibrate was observed in only 12%. Backwards-looking historical information was included in 28% of discussions. 8P scores ranged from 1.5 to 4.9. Among 8P items, Principal Diagnosis (65%) and Family/Caregiver (53%) were most frequently discussed, while Health Literacy/Adherence was discussed in only 7% of discussions.
RSRRs
Detailed in Table 4.
Associations Between Relationships, Sensemaking, and RSRR
At the patient-discussion level, discussion time, relationship scores, and sensemaking scores were positively associated (range 0.44 to 0.59, p < 0.0001) (Appendix Table 8). Table 5 shows hospital-level correlations between relationship scores, speaker diversity, STICC+, 8P, and RSRR. Relationship characteristics, STICC+, and 8P scores were significantly, positively correlated. STICC+ scores were significantly negatively associated with RSRR (− 0.65, p = 0.044). 8P scores were also negatively correlated with RSRR, but with a p value = 0.087.
Table 5.
Correlation Matrix Between Relationships, Sensemaking, and RSRR
| Correlation | Relationship scores | Speaker diversity | STICC+ | 8P | RSRR |
|---|---|---|---|---|---|
| Relationship scores | 1 | 0.23 (p = 0.52) | 0.77* (p = 0.01) | 0.75* (p = 0.012) | − 0.35 (p = 0.32) |
| Speaker diversity | 0.23 (p = 0.52) | 1 | 0.30 (p = 0.40) | 0.53 (p = 0.11) | − 0.11 (p = 0.77) |
| STICC+ | 0.77* (p = 0.01) | 0.30 (p = 0.40) | 1 | 0.91* (p ≤ 0.001) | − 0.65* (p = 0.044) |
| 8P | 0.75* (p = 0.012) | 0.53 (p = 0.11) | 0.91* (p < 0.001) | 1 | − 0.57 (p = 0.087) |
| RSRR | − 0.35 (p = 0.32) | − 0.11 (p = 0.77) | − 0.65* (p = 0.044 ) | − 0.57 (p = 0.087) | 1 |
*Signifies p < 0.05
DISCUSSION
We describe IDTs in practice, linking front-line organization with a conceptual model that considers relationships and sensemaking as key team characteristics and functions that in turn influence patient outcomes. Our observations at 10 hospitals revealed variability, including where and how meetings were held, who was present, and how participants related to each other and made sense of what was happening. Discussions about patients ranged from brief updates to rich, interactive discussions. Typically, discussions were brief. The finding that the average discussion per patient per hospital ranged from 42 s to 3 min, 23 s is striking, though perhaps not surprising when overall IDT meeting brevity is considered.
Consistent with our other studies of healthcare teams, relationship characteristics varied between IDTs.12, 13 Teams that had displayed more positive relationship characteristics of trust, respect, heedfulness, and mindfulness were significantly more likely to also discuss each patient’s general situation and care transition plans more completely, supporting our conceptual model that relationships are crucial for teams to effectively make sense of what is happening. Interestingly, speaker diversity was not significantly associated with either other relationship characteristics or sensemaking. This may reflect a relative lack of variation in speaker diversity, as speaker ratios largely ranged from 0.4 to 0.6. It may also reflect that diversity as a stand-alone marker of relationships is not sufficiently sensitive, or is inadequate in the absence of other relationship characteristics.
We used two frameworks to assess sensemaking: the general STICC+ and the care-transition-specific 8P. STICC+ scores ranged from 2.4 to 4.3, with almost all teams having a score of 4 or less; no discussion included all 5 elements. Teams most typically talked about each patient’s diagnosis and plan, but only talked about the rationale for care plans about half the time. Similarly, teams only raised potential concerns in half of IDT discussions, and sought feedback from each other in only 12%. Based on our prior work, talking about intent and concerns and seeking feedback are vital for developing shared understandings that allow care plans to be effectively followed, and potential issues to be rapidly identified. Similarly, teams discussed a minority of 8P elements, despite their being recognized as important to care transitions. Teams frequently discussed each patient’s diagnosis and mentioned family or caregiver support about half the time, but the remaining topics were typically unaddressed. These unaddressed STICC+ and 8P topics represent potential communication failures and lost opportunities to develop more robust understandings and care plans.
The STICC+ and 8P frameworks for sensemaking reflect common dual purposes of IDTs: communicating regarding what is happening during the hospitalization and preparing for discharge. Both were negatively associated with RSRR, though only STICC+ was significant. This may reflect the relative importance of having more general discussions, or given borderline p value for 8P and RSRR, an insufficient sample size in an exploratory analysis. Regardless, our findings reinforce the importance of sensemaking as an important team function that supports positive patient outcomes.
Our observations suggest potential ways to support relationships, sensemaking, and IDT effectiveness. The greater variance in team characteristics between hospitals versus within hospitals underscores the importance of hospital-level factors in shaping IDT function and effectiveness. We observed commonalities in hospitals whose teams had higher relationship and sensemaking scores. First, they had dedicated time and space for IDT meetings. Participants in these meetings were involved in every patient’s care, and were more likely to be focused on the discussions and less likely to be distracted by side-bar conversations. Discussions were more organized, with fewer “stops and starts” related to inattention. Similarly, having a social worker/case manager assigned to a specific team seemed important for promoting positive team relationships. On the IDT team level, actions that appear to promote positive relationships include expressing vulnerability, asking for and considering others’ input, and being aware of how one’s actions impact others.
Our observations also suggest strategies for promoting effective sensemaking. The use of structured tools to support IDT discussions was generally lacking. Incorporating STICC+ or 8P as part of a script or template could be helpful in prompting teams to discuss intentions, concerns, contingency plans, and risk factors. One hospital used a projected spreadsheet to efficiently review and discuss each patient, potentially helping team members develop a shared understanding of each patient.
These findings do not indicate a single “right way” to organize IDT meetings. For example, if teams do not have dedicated space, clearly separating different teams’ discussions may be helpful to minimize people coming and going and other distractions. Similarly, using STICC+ versus 8P in templates or structured tools may not matter as much as consistently, systematically discussing patients, identifying potential issues and their mitigation. Policymakers may consider updating care plan standards to include more specific, structured guidance.
Our observational study has several limitations. Although our visits were conducted at ten hospitals in eight geographically diverse areas, they were part of an integrated system and not nationally representative. Additionally, we could not control for patient diagnoses or illness severity. Variability in discussion time and content could have reflected differences in patient acuity. Finally, we did not have access to readmission data for specific patients discussed, instead using a hospital-level RSRR. However, because variance in IDT relationships was greater between than within hospitals, looking at a hospital-level outcome in this exploratory manner is reasonable. Other endpoints more specifically tied to proximal outcomes, such as patient/family understanding, or follow-up with post-hospital care, could provide valuable information regarding the impact of IDT relationships and sensemaking.
The complex task of transitioning patients from hospital to home depends on teams’ ability to work together to make sense of patients’ needs. Our study adds important knowledge of front-line IDTs’ organization in practice, supports our conceptual model of the importance of IDT relationships in shaping how team members make sense of what is happening, and suggests potential strategies for improving IDT effectiveness.
Supplementary Information
Below is the link to the electronic supplementary material.
(DOCX 41.8 kb)
Acknowledgements
Contributors: We acknowledge the contributions of the Department of Veterans Affairs employees who participated in this study, and the directors and chiefs of staff who supported this work. We also thank Musarrat Nahid for her work on this study.
Funding
This work was funded by the Department of Affairs Health Services Research & Development Services Grant #HSR1-031-12W. The views expressed do not reflect the position of the Department of Veterans Affairs.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Prior presentation: None
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kripilani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission: current strategies and future directions. Annu Rev Med. 2014;65:471–85. doi: 10.1146/annurev-med-022613-090415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goncalves-Bradley DC, Lannin NA, Clemson LM, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database Syst Rev 2016(1). 10.1002/14651858.CD000313.pub5 [DOI] [PMC free article] [PubMed]
- 3.The Joint Commission. Transitions of care. The need for a more effective approach to continuing patient care. Hot Topics in Health Care. 2012. Joint Commission Center for Transforming Healthcare.
- 4.Gonzalo JD, Kuperman E, Lehman E, Haidet P. Bedside interprofessional rounds: perceptions of benefits and barriers by internal medicine nursing staff, attending physicians, and house staff physicians. J Hosp Med. 2014;9(10):646–51. doi: 10.1002/jhm.2245. [DOI] [PubMed] [Google Scholar]
- 5.Pannick S, Beveridge I, Wachter RM, Sevdalis N. Improving the quality and safety of care on the medical ward: a review and synthesis of the evidence base. Eur J Intern Med. 2014;25(10):874–887. doi: 10.1016/j.ejim.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 6.Bhamidipati VS, Elliott DJ, Justice EM, Belleh E, Sonnad SS, Robinson EJ. Structure and outcomes of inter-disciplinary rounds in hospitalized medicine patients: a systematic review and suggested taxonomny. J Hosp Med. 2016;11:513–523. doi: 10.1002/jhm.2575. [DOI] [PubMed] [Google Scholar]
- 7.Ratelle JT, Sawatsky AP, Kashiwagi DT, Schouten WM, Erwin PJ, Gonzalo JD, Beckman TJ, West CP. Implementing bedside rounds to improve patient-centered outcomes: a systematic review. BMJ Qual Saf. 2019;28:317–326. doi: 10.1136/bmjqs-2017-007778. [DOI] [PubMed] [Google Scholar]
- 8.O’Leary KJ, Johnson JK, Auerbach AD. Do interdisciplinary rounds improve patient outcomes? Only if they improve teamwork. J Hosp Med. 2016;11(7):524–525. doi: 10.1002/jhm.2587. [DOI] [PubMed] [Google Scholar]
- 9.Leykum LK, O'Leary K. Annals for hospitalists inpatient notes - sensemaking—fostering a shared understanding in clinical teams. Ann Intern Med. 2017;167:HO2–HO3. doi: 10.7326/M17-1829. [DOI] [PubMed] [Google Scholar]
- 10.Leykum LK, Chesser H, Lanham HJ, Carla P, Palmer R, Ratcliffe T, Reisinger H, Agar M, Pugh J. The association between sensemaking during team rounds and hospitalized patient outcomes. J Gen Intern Med. 2015;30(12):1821–7. doi: 10.1007/s11606-015-3377-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blatt R, Christianson MK, Sutcliffe KM, Rosenthal MM. A sensemaking lens on reliability. J Organ Behav. 2006;27(7):897–917. doi: 10.1002/job.392. [DOI] [Google Scholar]
- 12.Lanham HJ, McDaniel RR, Jr, Crabtree BF, Miller WL, Stange KC, Tallia AF, Nutting PA. How improving practice relationships among clinicians and nonclinicians can improve quality in primary care. Jt Comm J Qual Patient Saf. 2009;35(9):457–AP2. doi: 10.1016/s1553-7250(09)35064-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McAllister C, Leykum LK, Lanham H, Reisinger HS, Kohn JL, Palmer R, Pezzia C, Agar M, Parchman M, Pugh J, McDaniel RR. Relationship with inpatient physician housestaff teams and their association with hospitalized patient outcomes. J Hosp Med. 2014;9:764–771. doi: 10.1002/jhm.2274. [DOI] [PubMed] [Google Scholar]
- 14.Lanham HJ, Palmer RF, Leykum LK, McDaniel RR, Jr, Nutting PA, Stange KC, Crabtree BF, Miller WL, Jaén CR. Trust and reflection in primary care practice redesign. Health Serv Res. 2016;51(4):1489–514. doi: 10.1111/1475-6773.12415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leykum LK, Lanham HJ, Pugh JA, Parchman M, Anderson RA, Crabtree BF, Nutting PA, Miller WL, Stange KC, McDaniel RR. Manifestations and implications of uncertainty for improving healthcare systems: an analysis of observational and interventional studies grounded in complexity science. Implement Sci. 2014;9:165. doi: 10.1186/s13012-014-0165-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009;350(6):1029–34. doi: 10.1097/SLA.0b013e3181bef697. [DOI] [PubMed] [Google Scholar]
- 17.Palinkas LA, Aarons GA, Horwitz S, Chamberlain P, Hurlburt M, Landsverk J. Mixed methods designs in implementation research. Adm Policy Ment Health. 2011;38:44–53. doi: 10.1007/s10488-010-0314-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eisenhardt KM. Building theories from case study research. Acad Manag Rev. 1989;14(4):532–50. doi: 10.2307/258557. [DOI] [Google Scholar]
- 19.Penney LS, Leykum LK, Noel P, Finley EP, Lanham HJ, Pugh J. Protocol for a mixed methods study of hospital readmissions: sensemaking in Veterans Health Administration healthcare system in the USA. BMJ Open. 2018;8(4):e020169. doi: 10.1136/bmjopen-2017-020169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Forman J, Damschroder L. Qualitative Content Analysis. In: Empirical Methods for Bioethics: a Primer 2007 Dec 5. Emerald Group Publishing Limited.
- 21.Pelled LH, Eisenhardt KM, Xin KR. Exploring the black box: an analysis of work group diversity, conflict and performance. Adm Sci Q. 1999;44(1):1–28. doi: 10.2307/2667029. [DOI] [Google Scholar]
- 22.Kilduff M, Angelmar R, Mehra A. Top management-team diversity and firm performance: examining the role of cognitions. Organ Sci. 2000;11(1):21–34. doi: 10.1287/orsc.11.1.21.12569. [DOI] [Google Scholar]
- 23.Martins LL, Schilpzand MC, Kirkman BL, Ivanaj S, Ivanaj V. A contingency view of the effects of cognitive diversity on team performance: the moderating roles of team psychological safety and relationship conflict. Small Group Res. 2013;44(2):96–126. doi: 10.1177/1046496412466921. [DOI] [Google Scholar]
- 24.Weick KE, Roberts KH. Collective mind in organizations: heedful interrelating on flight decks. Adm Sci Q. 1993;1:357–81. doi: 10.2307/2393372. [DOI] [Google Scholar]
- 25.Weick KE. The collapse of sensemaking in organizations: the Mann Gulch disaster. Adm Sci Q. 1993;1:628–52. doi: 10.2307/2393339. [DOI] [Google Scholar]
- 26.Sutcliffe KM, Lewton E, Rosenthan MM. Communication failures: an insidious contributor to medical mistakes. Acad Med. 2005;79:186–95. doi: 10.1097/00001888-200402000-00019. [DOI] [PubMed] [Google Scholar]
- 27.Vogus TJ, Sutcliffe KM. The Safety Organizing Scale: development and validation of a behavioral measure of safety culture in hospital nursing units. Med Care. 2007;1:46–54. doi: 10.1097/01.mlr.0000244635.61178.7a. [DOI] [PubMed] [Google Scholar]
- 28.Maitlis S, Christianson M. Sensemaking in organizations: taking stock and moving forward. Acad Manag Ann. 2014;8(1). 10.5465/19416520.2014.873177.
- 29.Weick KE. Sensemaking in organizations. Sage; 1995. [Google Scholar]
- 30.The 8P Screening Tool: identifying your patient’s risk for adverse events after discharge. Society of Hospital Medicine Project Boost. https://www.hospitalmedicine.org/globalassets/clinical-topics/clinical-pdf/8ps_riskassess-1.pdf. Accessed 31 Jul 2022.
- 31.Hansen LO, Greenwald JL, Budnitz T, Howell E, Halasyamani L, Maynard G, Vidyarthi A, Coleman EA, Williams MV. Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8:421–427. doi: 10.1002/jhm.2054. [DOI] [PubMed] [Google Scholar]
- 32.Barrett M, Raetzman S, Andrews R. Overview of key readmission measures and methods. 2012. HCUP Methods Series Report #2012-04. ONLINE December 20, 2012. U.S. Agency for Healthcare Research and Quality. Available: http://www.hcup- us.ahrq.gov/reports/methods/methods.jsp. Accessed 31 Jul 2022.
- 33.VA Hospital-Wide 30-day Readmission (HWR) Cube, a product of the Veterans Health Administration Support Service Center (VSSC) VSSC URL: (URL: https://bioffice.pa.cdw.va.gov/default.aspx?bookid=99284cd4-f909-4eee-aa8e-49065f12afeb|ispasFalse|report04a80ff9-b3fd-4223-a583-47d3859101d1|ws1|wsb0|isDisabledAnalyticsFalse|isDashboardPanelOnTrue). (Note: the Cube can also be accessed by going to the Quality of Care page on the VSSC website (URL: https://vssc.med.va.gov/VSSCMainApp/products.aspx?PgmArea=82) and then clicking on Product Name: Hospital-Wide 30-day Readmission Cube.)
- 34.Pugh J, Penney LS, Noël PH, et al. Evidence based processes to prevent readmissions: more is better, a ten-site observational study. BMC Health Serv Res. 2021;21:189. doi: 10.1186/s12913-021-06193-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.R Core Team . R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 41.8 kb)