Abstract
Background
Low-value care cascades, defined as the receipt of downstream health services potentially related to a low-value service, can result in harm to patients and wasteful healthcare spending, yet have not been characterized within the Veterans Health Administration (VHA).
Objective
To examine if the receipt of low-value preoperative testing is associated with greater utilization and costs of potentially related downstream health services in Veterans undergoing low or intermediate-risk surgery.
Design
Retrospective cohort study using VHA administrative data from fiscal years 2017–2018 comparing Veterans who underwent low-value preoperative electrocardiogram (EKG) or chest radiograph (CXR) with those who did not.
Participants
National cohort of Veterans at low risk of cardiopulmonary disease undergoing low- or intermediate-risk surgery.
Main Measures
Difference in rate of receipt and attributed cost of potential cascade services in Veterans who underwent low-value preoperative testing compared to those who did not
Key Results
Among 635,824 Veterans undergoing low-risk procedures, 7.8% underwent preoperative EKG. Veterans who underwent a preoperative EKG experienced an additional 52.4 (95% CI 47.7–57.2) cascade services per 100 Veterans, resulting in $138.28 (95% CI 126.19–150.37) per Veteran in excess costs. Among 739,005 Veterans undergoing low- or intermediate-risk surgery, 3.9% underwent preoperative CXR. These Veterans experienced an additional 61.9 (95% CI 57.8–66.1) cascade services per 100 Veterans, resulting in $152.08 (95% CI $146.66–157.51) per Veteran in excess costs. For both cohorts, care cascades consisted largely of repeat tests, follow-up imaging, and follow-up visits, with low rates invasive services.
Conclusions
Among a national cohort of Veterans undergoing low- or intermediate-risk surgeries, low-value care cascades following two routine low-value preoperative tests are common, resulting in greater unnecessary care and costs beyond the initial low-value service. These findings may guide de-implementation policies within VHA and other integrated healthcare systems that target those services whose downstream effects are most prevalent and costly.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07561-x.
KEY WORDS: low-value care, care cascades, preoperative testing, Veterans Health Administration
INTRODUCTION
Low-value care, defined as the use of a health service whose costs or harms exceed its benefits, is common and accounts for over $100 billion in annual US healthcare expenditures.1–5 Low-value care may result in care cascades, which include unnecessary testing, treatments, procedures, or visits that occur as a result of a low-value service.6–12 For example, among Medicare beneficiaries undergoing cataract surgery, 11% received a low-value preoperative electrocardiogram, which was associated with 5–11 cascade services per 100 beneficiaries, such as repeat electrocardiograms and stress tests.7
In addition to Medicare and private health insurers, low-value care is prevalent within the Veterans Health Administration (VHA), an integrated and federally operated healthcare system.13,14 In a national cohort of Veterans who received VHA care in 2015, the frequency of low-value diagnostic testing for low back pain, headache, syncope, and sinusitis ranged from 5 to 20% among Veterans with each respective underlying condition.14 While prior studies within VHA have focused on single low-value services, care cascades have not been well characterized.
Preoperative electrocardiograms (EKGs) and chest radiographs (CXRs) in low-risk patients undergoing low- or intermediate-risk surgeries provide an opportunity to understand low-value care cascades within VHA. Preoperative EKGs and CXRs in low-risk patients are widely recognized low-value services yet remain prevalent and are associated with care cascades.3,7,15–19 Understanding the use and cost of low-value care as part of a cascade beyond the initial preoperative test would provide information regarding the full impact of low-value preoperative care within VHA. This would enable VHA to target de-implementation policies and interventions at those services that result in the greatest degree of overall low-value health service utilization and cost.
Our objective was to examine if the receipt of low-value preoperative testing is associated with greater utilization and costs of potentially related downstream health services in Veterans undergoing low or intermediate risk surgery.
METHODS
Study Design and Data Sources
We conducted a retrospective cohort study of Veterans continuously enrolled in VHA in October 1, 2016–September 30, 2018 (FY17-FY18). We used the VA Corporate Data Warehouse to identify patient sociodemographic characteristics, medical comorbidities, International Classification of Disease 10th Edition (ICD-10) codes, and Common Procedural (CPT) codes. We used the Area Health Resource File and the VHA Support Service Center files to determine facility-level covariates and the VA Planning Systems Support Group database to obtain patient driving distance to their nearest VA facility. This study was approved by the VA Pittsburgh Healthcare System Institutional Review Board.
Study Cohort
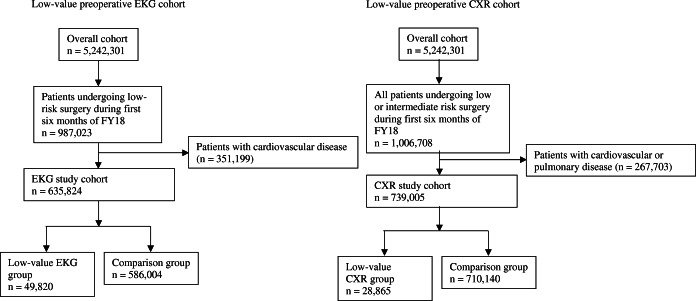
From a national cohort of VHA beneficiaries (N=5,242,301) established for a larger study examining the use and cost of low-value care within VHA,20 we created two study cohorts, representing Veterans at risk of receiving a low-value preoperative EKG or CXR (Fig. 1). We generated the cohorts based on accepted preoperative guidelines, findings in peer-reviewed literature, and the clinical expertise of the research team.21–26 Details on the algorithms and administrative billing codes used to generate the cohorts are found in Appendix Table 1.
Fig. 1.
Study cohort flow diagram for service-specific cohorts. Veterans with history of arrhythmia, coronary artery disease, valvular disease, heart failure, or a cardiology visit within 1 year prior to their surgery date or who had an EKG as part of an inpatient stay or ED visit within 30 days prior to their surgery date were excluded from the low-value preoperative EKG cohort. Veterans with history of valvular disease, heart failure, chronic obstructive pulmonary disease, asthma, other interstitial lung disease, or a pulmonary visit within one year prior to their surgery date or history of acute respiratory illness within 60 days prior to their surgery date or who had a CXR as part of an inpatient stay or ED visit within 30 days prior to their surgery date were excluded from the low-value CXR cohort. EKG = electrocardiogram; CXR – chest radiograph
To create the EKG study cohort, we identified Veterans who underwent a low-risk non-cardiothoracic surgery during the first 6 months of FY18. We excluded Veterans with a history of cardiac disease or who had seen a cardiologist in a year prior to their surgery date. Due to undercoding of diagnoses within VHA27,28, we applied broad exclusion criteria, such as recent cardiology visit, when creating the cohort of low-risk Veterans. The remaining Veterans represented those at low risk of cardiac disease undergoing low-risk surgery and thus at risk of receiving a low-value preoperative EKG.
For the CXR study cohort, we identified Veterans who underwent a low or intermediate-risk non-cardiothoracic surgery and then excluded those with history of cardiopulmonary disease to create a cohort of Veterans in which preoperative CXR would not be indicated.
Low-Value Preoperative Test Groups and Comparison Groups
To create low-value EKG and low-value CXR groups (e.g., exposure groups), we identified those within each service-specific cohort who had undergone a preoperative EKG or CXR (Appendix Table 1). For Veterans undergoing more than one low-value preoperative test, we defined the first test as the index service and the corresponding surgery as the index surgery. Our comparison group consisted of the remaining Veterans within each cohort who had undergone a qualifying surgery but did not undergo preoperative testing. In instances where those within the comparison group underwent more than one surgery, we chose the first qualifying surgery as the index surgery.
Utilization and Cost of Potential Cascade Services
The primary outcomes were additional services that patients experienced within 6 months subsequent to and plausibly as a result of the low-value preoperative test, which we labeled as potential cascade services. The services were defined by practicing clinicians on the research team considering their clinical knowledge and based upon the findings of relevant literature.7,8,10 For the EKG cohort, potential cascade services included subsequent EKGs, related outpatient visits, lab tests, cardiac imaging, stress testing, evaluations for arrhythmias, and invasive procedures such as cardiac catheterizations. For the CXR cohort, potential cascade services included subsequent CXR, related outpatient visits, follow-up imaging, pulmonary function testing, and bronchoscopy (Appendix Table 1).
For the exposure groups, the outcome assessment period was 6 months from the date of the preoperative test. For the comparison group, the start of the 6-month outcome period corresponded to the mean time prior to undergoing the index surgery that patients in the corresponding low-value service groups underwent a preoperative EKG or CXR.7 We chose this follow-up period based on literature examining wait times within VHA to capture services that may take several months to schedule.29 We also conducted sensitivity analysis using a 90-day outcome period to allow for direct comparison with existing literature.7
We computed the costs by applying VA Health Economics Resource Center (HERC) value estimates to CPT codes associated with the initial preoperative test or cascade services. These validated estimates represent hypothetical reimbursement based on average national Medicare and private-sector reimbursement rates.30
Patient and Facility-Level Covariates
Using data from FY17, we established the following patient-level covariates: age, sex, race/ethnicity, VA priority group (assigned at VHA enrollment based on service-connected illness, era of service, and socioeconomic status), driving distance to nearest VHA facility, and number and presence of specific Elixhauser conditions.31 We also assigned Veterans to the VA Medical Center (VAMC) where they received most of their outpatient care in FY17 and determined the corresponding academic affiliation, census region, rurality, facility complexity level (based on patient volume, number and breadth of physician specialists, patient case mix, intensive care unit capabilities, and degree of teaching and research), and size (based on outpatient visit volume).32
We categorized Veterans’ index surgeries based on Berenson-Eggers Type of Service (BETOS) categories and level of cardiopulmonary risk (Appendix Table 2).23
Statistical Analysis
Within the low-value service and comparison groups of both cohorts, we determined the proportions of Veterans undergoing each potential cascade service as well as counts of the individual services during the 6-month outcome period, presented as the event rate per 100 Veterans. We imputed missing values (≤5% on any individual variable) using single imputation by chained equations.
We used inverse probability of treatment weighting based on propensity scores to create balance among the low-value service and comparison groups with regard to baseline covariates and index surgery type. To generate the inverse probability of treatment weights (IPTWs), we first estimated propensity scores using multivariable logistic regression models with receipt of the low-value preoperative test as the binary outcome variable and baseline covariates as the predictor variables. We then estimated the probability of receiving the low-value preoperative test for each Veteran and created an IPTW by taking the inverse of the propensity score.33,34 We checked balance between groups after applying the IPTWs by calculating weighted standardized mean differences (SMDs) for all covariates. We defined balance between groups as a weighted SMD in the mean or proportion of each individual covariate of < 0.10.33,35
We created negative binomial regression models that included the IPTWs to determine adjusted rates of undergoing each potential cascade service for Veterans in the low-value service groups (cascade event rates) and in the comparison groups (baseline event rates). We calculated the cascade-attributable event rates (CAERs) by subtracting the baseline event rate from the cascade event rate. This represents the rate of receipt of a potential cascade service that can be plausibly attributed to the index low-value service.7 We also applied robust variance estimates to adjust for clustering effects at the VAMC level.
We also created weighted linear regression models, adjusting for facility-level clustering effect, to determine the adjusted cost per Veteran of each individual potential cascade service as well as an overall adjusted cost per Veteran for those in the low-value service and comparison groups. We represented the difference in cost between both groups as the cascade-attributable cost. Analyses were conducted using SAS (version 7.1, SAS Institute) and Stata (version 15.1, StataCorp).
RESULTS
Prevalence and Cost of Care Cascades Following Low-Value Preoperative EKG Testing
We identified 635,824 Veterans at risk of undergoing a low-value EKG, of whom 7.8% underwent a low-value EKG (Fig. 1). Veterans who received a low-value EKG had a greater comorbidity burden and received care at VHA facilities with higher complexity ratings than those Veterans who did not (Table 1). After applying IPTWs, the SMDs were <0.10 for all covariates and index surgery types, including those individual comorbidities with baseline differences, indicating appropriate balance for all covariates through use of our propensity score model (Appendix Table 3 and Appendix Table 4).
Table 1.
Baseline patient and VA Medical Center (VAMC)-level characteristics within each service-specific cohort by receipt of low-value preoperative testing before propensity score weighting
| EKG study cohort† | CXR study cohort† | |||
|---|---|---|---|---|
| Low-value EKG group (n=49,820) |
Comparison group (n=586,004) |
Low-value CXR group (n=28,865) |
Comparison group (n=710,140) |
|
| Patient-level characteristics | ||||
| Age, year, mean (SD) | 63.2 (12.4) | 63.5 (13.7) | 64.4 (13.0) | 64.5 (13.7) |
| Male sex, n (%) | 45,269 (90.9) | 532,878 (90.9) | 26,655 (92.3) | 653,626 (92.0) |
| Race/ethnicity, n (%) | ||||
| Non-Hispanic White | 36,060 (72.4) | 415,344 (70.9) | 19,602 (67.9) | 510,843 (71.9) |
| Non-Hispanic Black | 9,843 (19.8) | 118,794 (20.3) | 6,342 (22.0) | 136,961 (19.3) |
| Hispanic | 2,625 (5.3) | 35,460 (6.1) | 2,183 (7.6) | 43,022 (6.1) |
| Non-Hispanic/multiracial | 1,292 (2.6) | 16,406 (2.8) | 738 (2.6) | 19,314 (2.7) |
| VA priority group‡, n (%) | ||||
| 1 | 18,409 (37.0) | 228,698 (39.0) | 10,884 (37.7) | 276,583 (39.0) |
| 2–6 | 24,911 (50.0) | 276,651 (47.2) | 14,278 (49.5) | 332,328 (46.8) |
| 7–8 | 6,500 (13.1) | 80,655 (13.8) | 3,703 (12.8) | 101,229 (14.3) |
| Number of Elixhauser conditions§, mean (SD) | 1.7 (1.8) | 1.5 (1.6) | 1.9 (1.9) | 1.5 (1.6) |
| Driving distance to nearest VA facility, miles, mean (SD) | 14.8 (14.7) | 14.9 (14.6) | 14.3 (14.1) | 15.0 (14.5) |
| VAMC-level characteristics | ||||
| Academic affiliation, yes, n (%) | 48,881 (98.1) | 574,075 (98.0) | 28,577 (99.0) | 696,434 (98.1) |
| Facility size, total # outpatient visits FY18, mean (SD) | 768,038 (366,899) | 802,318 (395,800) | 852,268 (389,269) | 809,367 (400,211) |
| Census region, n (%) | ||||
| Northeast | 5,932 (11.9) | 7,4691 (12.8) | 3,092 (10.7) | 92,170 (13.0) |
| Midwest | 12,677 (25.5) | 133,995 (22.9) | 5,825 (20.2) | 162,437 (22.9) |
| South | 19,154 (38.5) | 256,116 (43.7) | 14,164 (49.1) | 310,237 (43.7) |
| West | 12,057 (24.2) | 121,202 (20.7) | 5,784 (20.0) | 145,296 (20.5) |
| Rurality, n (%) | ||||
| Large metropolitan | 22,682 (45.5) | 623,481 (45.0) | 14,849 (51.4) | 319,720 (45.0) |
| Small metropolitan | 17,488 (35.1) | 210,327 (35.9) | 9,267 (32.1) | 254,668 (35.9) |
| Micropolitan | 5,557 (11.2) | 64,652 (11.0) | 2,644 (9.2) | 77,975 (11.0) |
| Noncore rural | 4,093 (8.2) | 47,544 (8.1) | 2,105 (7.3) | 57,777 (8.1) |
| Facility complexity level‖, n (%) | ||||
| High complexity | 41,687 (83.7) | 478,725 (81.7) | 25,548 (88.5) | 548,240 (82.3) |
| Medium complexity | 4,857 (9.8) | 54,428 (9.3) | 2,064 (7.2) | 65,279 (9.2) |
| Low complexity | 3,276 (6.6) | 52,851 (9.0) | 1,253 (4.3) | 60,621 (8.5) |
EKG electrocardiogram, CXR chest radiograph
†With the exception of driving distance for the EKG study cohort and age and sex for the CXR cohort, the low-value service groups and comparison groups had statistically significant differences in characteristics (p<0.05). Absolute standardized mean differences were <0.10 for all variables after applying propensity score weights (Appendix Table 3 and Appendix Table 5)
‡Veterans are assigned to 1 of 8 priority groups at VA enrollment based on service-connected illnesses, era of Service, and socioeconomic status determined by means testing. Priority group determines level of co-payment. Priority groups are condensed for presentation in the table based on similarity of copays between groups but were included separately in our models
§Individual Elixhauser conditions shown in Appendix Table 3 and Appendix Table 5
‖The complexity rating is based on a VAMC’s patient volume, number and breadth of physician specialists, patient case mix, intensive care unit capabilities, and degree of teaching and research
Missing values for race/ethnicity (4% missing), VA priority group (<0.1%), driving distance to nearest VA facility (0.1%), census region (0.8%), rurality (0.1%) generated using single imputation
Among those Veterans who underwent a low-value preoperative EKG, 29.0% received at least one potential cascade service within 6 months. Comparing Veterans who did and did not undergo a low-value preoperative EKG, we found an overall adjusted CAER of 52.4 per 100 Veterans (95% CI 47.7–57.2). Repeat EKG occurred at an adjusted CAER of 21.6 per 100 Veterans (95% CI 18.3–25.0) followed by a troponin test (6.7/100 Veterans, 95% CI 5.6–7.8) and echocardiogram (7.4/100 Veterans, 95% CI 6.8–8.0). Cardiac catheterization, coronary artery bypass/coronary repair, and valve replacement/repair occurred infrequently (Table 2). In our sensitivity analysis at 90 days, we found an overall adjusted CAER of 30.7 (27.1–34.3). Similar to the 6-month outcome period, noninvasive services and follow-up visits occurred at the highest rates.
Table 2.
Utilization of potential cascade services after low-value preoperative electrocardiogram (EKG)
| Unadjusted event rate per 100 Veterans | Unadjusted cascade-attributable event rate* | Adjusted cascade-attributable event rate (95% CI)† | ||
|---|---|---|---|---|
| Cascade service | Low value-EKG group (n=49,820) |
Comparison group (n=586,004) |
||
| Any cascade service | 76.4 | 29.3 | 47.1 | 52.4 (47.7–57.2) |
| Outpatient EKG | 33.2 | 11.4 | 21.8 | 21.6 (18.3–25.0) |
| Outpatient visit for abnormal EKG‡ | 1.0 | 0.5 | 0.5 | 0.7 (0.4–1.1) |
| Outpatient visit to cardiologist | 7.0 | 3.5 | 3.5 | 5.1 (4.8–5.4) |
| Troponin | 11.9 | 4.9 | 7.0 | 6.7 (5.6–7.8) |
| Brain natriuretic peptide | 5.4 | 2.6 | 2.8 | 3.1 (2.4–3.7) |
| Echocardiogram | 9.5 | 3.5 | 6.0 | 7.4 (6.8–8.0) |
| Stress test | 5.1 | 1.8 | 3.3 | 5.0 (4.4–5.5) |
| Other cardiac imaging§ | 0.4 | 0.1 | 0.3 | 0.4 (0.2–0.5) |
| Evaluation for arrhythmia‖ | 2.6 | 1.0 | 1.6 | 2.3 (1.9–2.7) |
| Cardiac catheterization | 0.1 | 0.1 | 0.1 | 0.14 (0.08–0.20) |
| CABG/coronary artery repair | 0.08 | 0.02 | 0.06 | 0.07(0.04–0.10) |
| Valve replacement/repair | <0.1 | <0.1 | <0.1 | <0.1 |
CABG coronary artery bypass graft, EKG electrocardiogram
*Defined as the difference in the rate of care cascade service per 100 Veterans in those who received a low-value preoperative EKG compared who those who did not receive a low-value preoperative EKG
†Adjusted for patient and facility-level covariates (age, sex, race/ethnicity, VA priority group, driving distance to nearest VA, number of Elixhauser conditions, individual Elixhauser conditions, academic affiliation, facility size, census region, rurality, complexity level) and surgery type using propensity score weighting
‡Outpatient visit with primary diagnosis of abnormal electrocardiogram, abnormal result of cardiovascular function study, abnormal findings on diagnostic imaging of heart and coronary circulation, not including cardiology visits
§Includes cardiac magnetic resonance imaging (cMRI), cardiac positron emission tomography (PET), nuclear imaging, coronary ultrasound, coronary computed tomography angiography (CTA)
‖Includes Holter monitor, event monitor, implantable loop recorder, electrophysiology (EP) testing, EP procedure, pacemaker evaluation, pacemaker procedure
The total cost associated with a low-value preoperative EKG was $7,942,486, which includes $1,802,182 for the initial EKG and $6,140,304 for potential cascade services. Relative to the comparison group, those Veterans who underwent low-value preoperative EKG incurred, on average, an additional $138.28 (95% CI 126.19–150.37) per Veteran in adjusted costs. This includes an average additional cost per Veteran of $36.57 (95% CI 34.32–38.81) for the initial EKG and $101.72 (95% CI 89.58–113.85) per Veteran for potential cascade services. Cardiac imaging and repeat EKG accounted for the greatest proportion of additional costs while invasive procedures accounted for very little of the additional costs due to their low frequency (Table 3).
Table 3.
Cost of potential cascade services after low-value preoperative electrocardiogram (EKG)
| Average unadjusted cost per Veteran | Unadjusted cascade-attributable cost per Veteran† ($) | Adjusted cascade-attributable cost per Veteran (95% CI)‡ ($) | ||
|---|---|---|---|---|
| Cascade service* | Low value-EKG group ($) (n=49,820) |
Comparison group ($) (n=586,004) |
||
| Any cascade service | 123.3 | 45.9 | 77.3 | 101.7 (89.6–113.9) |
| Outpatient EKG | 14.0 | 5.0 | 9.0 | 9.0 (7.6–10.3) |
| Outpatient visit for abnormal EKG§ | 0.6 | 0.3 | 0.3 | 0.4 (0.2–0.6) |
| Outpatient visit to cardiologist | 4.4 | 2.1 | 2.3 | 3.3 (3.1–3.6) |
| Troponin | 1.5 | 0.6 | 0.9 | 0.8 (0.7–1.0) |
| Brain natriuretic peptide | 4.4 | 2.1 | 2.3 | 2.5 (2.0–3.0) |
| Echocardiogram | 48.4 | 18.0 | 30.5 | 37.7 (34.5–40.8) |
| Stress test | 14.9 | 5.5 | 9.4 | 13.9 (11.6–16.3) |
| Other cardiac imaging‖ | 2.7 | 0.8 | 1.9 | 2.2 (0.8–3.6) |
| Evaluation for arrhythmia‖ | 17.8 | 5.5 | 12.3 | 16.5 (9.9–23.1) |
| Cardiac catheterization | 14.6 | 6.1 | 8.6 | 15.4 (9.1–21.7) |
CABG coronary artery bypass graft, EKG electrocardiogram
*Cost data unavailable for CPT codes associated with CABG/coronary repair and valve replacement/repair
†Determined by subtracting cost of care cascade services per Veteran in those who did not receive a low-value preoperative EKG from those who did receive a low-value preoperative EKG
‡Adjusted for patient and facility-level covariates (age, sex, race/ethnicity, VA priority group, driving distance to nearest VA, number of Elixhauser conditions, individual Elixhauser conditions, academic affiliation, facility size, census region, rurality, complexity level) and surgery type using propensity score weighting
§Outpatient visit with primary diagnosis of abnormal electrocardiogram, abnormal result of cardiovascular function study, abnormal findings on diagnostic imaging of heart and coronary circulation, not including cardiology visits
‖Includes cardiac magnetic resonance imaging (cMRI), cardiac positron emission tomography (PET), nuclear imaging, coronary ultrasound, coronary computed tomography angiography (CTA)
‖Includes Holter monitor, event monitor, implantable loop recorder, electrophysiology (EP) testing, EP procedure, pacemaker evaluation, pacemaker procedure
Prevalence and Cost of Care Cascades Following Low-Value Preoperative CXR Testing
Among 739,005 Veterans at risk, 3.9% underwent a low-value preoperative CXR (Fig. 1). Veterans who received a preoperative CXR had higher comorbidity burden and received care at VHA facilities with higher complexity levels compared to those who did not (Table 1). The SMDs between all covariates and index surgery types in those who did and did not undergo a low-value CXR were <0.10 after applying the IPTWs, indicating appropriate balance for all covariates (Appendix Table 5 and Appendix Table 6).
Among those who underwent a low-value preoperative CXR, 37.9% received at least one potential cascade service. Comparing Veterans who did and did not undergo low-value preoperative CXR, we found an overall adjusted CAER of 61.9 cascade services per 100 Veterans (95% CI 57.8–66.1). Repeat CXR occurred at an adjusted CAER of 42.2 per 100 Veterans (95% CI 38.8–45.6). Computed tomography chest and pulmonary function tests occurred at adjusted CEAR of 9.1 per 100 Veterans (95% CI 8.6–9.7) and 5.3 per 100 Veterans (95% CI 4.5–6.0%), respectively. Other chest imaging and bronchoscopy occurred less frequently (Table 4). In our sensitivity analysis at 90 days, we found an overall adjusted CAER of 52.8 (48.3–57.3).
Table 4.
Utilization of potential cascade services after low-value preoperative chest radiograph (CXR)
| Unadjusted event rate per 100 Veterans | Unadjusted cascade-attributable event rate* | Adjusted cascade-attributable event rate (95% CI)† | ||
|---|---|---|---|---|
| Cascade service | Low-value CXR group(n=28,865) | Comparison group(n=710,140) | ||
| Any cascade service | 99.6 | 24.4 | 75.2 | 61.9 (57.8–66.1) |
| Outpatient CXR | 67.5 | 13.0 | 54.5 | 42.2 (38.8–45.6) |
| Outpatient visit for abnormal CXR‡ | 2.6 | 1.4 | 1.2 | 1.1 (1.0–1.3) |
| Outpatient visit to pulmonologist | 3.7 | 1.2 | 2.4 | 2.3 (1.9–2.8) |
| Outpatient visit to thoracic surgeon | 1.4 | 0.3 | 1.1 | 0.9 (0.7–1.1) |
| Computed tomography chest | 16.2 | 5.9 | 10.4 | 9.1 (8.6–9.7) |
| Other chest imaging§ | 1.1 | 0.4 | 0.7 | 0.59 (0.48–0.70) |
| Pulmonary function test | 6.6 | 2.1 | 4.5 | 5.3 (4.5–6.0) |
| Bronchoscopy | 0.5 | 0.1 | 0.4 | 0.36 (0.27–0.45) |
CXR, chest radiograph
*Defined as the difference in the rate of care cascade service per 100 Veterans in those who received a low-value preoperative CXR compared who those who did not receive a low-value preoperative CXR
†Adjusted for patient and facility-level covariates (age, sex, race/ethnicity, VA priority group, driving distance to nearest VA, number of Elixhauser conditions, individual Elixhauser conditions, academic affiliation, facility size, census region, rurality, complexity level) and surgery type using propensity score weighting
‡Defined as outpatient visit with primary diagnosis of solid pulmonary nodule or other nonspecific abnormal findings of the lung field, not including pulmonary visits
§Includes magnetic resonance imaging (MRI) of chest and thorax, magnetic resonance angiography (MRA) of chest
The Veterans who underwent low-value preoperative CXR were subject to $5,739,35 in total costs associated with the low-value preoperative test, $2,149,829 for the initial CXR and $3,589,525 for potential cascade services. Relative to the comparison group, Veterans in the low-value CXR group incurred, on average, an additional $152.08 (95% CI $146.66–157.51) per Veteran in adjusted costs. This includes an average additional cost per Veteran of $74.33 (95% CI 72.31–76.34) for the initial CXR and $77.75 (95% CI 72.25–83.25) for potential cascade services. Related imaging and repeat CXR contributed most to the overall costs whereas pulmonary function testing and bronchoscopy accounted for very little (Table 5).
Table 5.
Cost of potential cascade services after low-value preoperative chest radiograph (CXR)
| Average unadjusted cost per Veteran | Unadjusted cascade-attributable cost per Veteran* ($) | Adjusted cascade-attributable cost per Veteran (95% CI)† ($) | ||
|---|---|---|---|---|
| Cascade service | Low-value CXR group ($) (n=28,865) |
Comparison-group ($) (n=710,140) |
||
| Any cascade service | 124.4 | 34.4 | 89.9 | 77.8 (72.3–83.3) |
| Outpatient CXR | 49.0 | 9.5 | 39.4 | 30.6 (28.2–33.0) |
| Outpatient visit for abnormal CXR‡ | 1.6 | 0.9 | 0.6 | 0.6 (0.5–0.7) |
| Outpatient visit to pulmonologist | 2.6 | 0.9 | 1.7 | 1.7 (1.3–2.0) |
| Outpatient visit to thoracic surgeon | 0.7 | 0.2 | 0.6 | 0.5 (0.3–0.6) |
| Computed tomography chest | 41.7 | 14.4 | 27.3 | 23.6 (22.2–25.0) |
| Other chest imaging§ | 4.8 | 1.8 | 3.1 | 2.6 (2.1–3.2) |
| Pulmonary function test | 13.9 | 4.6 | 9.4 | 11.2 (9.5–12.8) |
| Bronchoscopy | 10.0 | 2.2 | 7.8 | 7.1 (5.1–9.1) |
CXR chest radiograph
*Determined by subtracting cost of care cascade services per Veteran in those who did not receive a low-value preoperative CXR from those who did receive a low-value preoperative EKG
†Adjusted for patient and facility-level covariates (age, sex, race/ethnicity, VA priority group, driving distance to nearest VA, number of Elixhauser conditions, individual Elixhauser conditions, academic affiliation, facility size, census region, rurality, complexity level) and surgery type using propensity score weighting
‡Defined as outpatient visit with primary diagnosis of solid pulmonary nodule or other nonspecific abnormal findings of the lung field, not including pulmonary visits
§Includes magnetic resonance imaging (MRI) of chest and thorax, magnetic resonance angiography (MRA) of chest
DISCUSSION
Among a national cohort of VHA beneficiaries undergoing low- or intermediate-risk surgery, care cascades following low-value preoperative testing were common, resulting in 52 potential cascade services per 100 Veterans after low-value EKG and 62 potential cascade services per 100 Veterans after undergoing a low-value CXR. Veterans who received preoperative testing incurred greater than $100 in additional costs associated with the low-value test compared to those who did not undergo preoperative testing.
Prior studies have demonstrated that low-value care is prevalent within VHA; however, these studies have largely focused on single low-value services.13,14,36,37 We build upon this work by examining the use and costs of a series of downstream services that could plausibly result from each of these low-value service. Our findings are also consistent with and add to prior studies examining care cascades in other patient populations. Among a sample of low-risk Medicare beneficiaries undergoing cataract surgery, Ganguli et al. showed that those who received a preoperative EKG experienced an overall CAER of approximately 11 cascade services per 100 beneficiaries during a 90-day outcome period.7 The higher rate of total cascade services in our study, even after conducting sensitivity analysis using a 90-day outcome period, was largely driven by higher rates of subsequent EKGs. This may be partially explained by the fact that Veterans, in general, have higher medical complexity and thus clinicians may be more likely to order additional tests in anticipation of complications even if they are not necessary. Nonetheless, the authors similarly found that follow-up cardiac imaging and related outpatient visits occurred at a higher rate than invasive services such as cardiac catheterization.7 By using a cohort of low-risk Veterans undergoing any low or intermediate-risk surgery as opposed to cataract surgery alone and in applying a longer outcome period, our work builds upon these studies by providing a more comprehensive examination of care cascades following low-value preoperative testing.
The cascade services in our study consisted of mostly repeat testing, follow-up imaging, and follow-up visits but few invasive procedures, which aligns with studies examining care cascades in other patient populations.7,8 The fact that few Veterans experienced invasive procedures such as bronchoscopy suggests that the preoperative test did not reveal a meaningful finding that needed intervention and that the majority of the downstream care was unnecessary. For a subset of Veterans, these invasive downstream services may also be unnecessary. While the total frequency and cost of these invasive services are low in our study, on an individual-level, they are associated with high costs and risk of additional downstream consequences.
While low-value services, such as preoperative testing, may seem low-risk, downstream care may result in unanticipated harms to patients such as anxiety surrounding false-positive results, inconvenience associated with downstream testing and visits, and risks of invasive procedures. The total cost of nearly $14 million associated with low-value preoperative testing in our study was low in comparison to the $72.3 billion in total VA expenditures in FY18. However, patients may experience additional costs that we did not directly calculate such as those associated with transportation or missed work. These negative experiences may erode a patient’s trust and cause them to ignore recommendations regarding future follow-up testing that is in fact necessary. Additional qualitative research examining patients’ experiences with care cascades is warranted to further explore this.
Our study provides a template for characterizing often unmeasured, unnecessary downstream care and can inform future studies that seek to characterize care cascades following other low-value services. This has the potential to impact de-implementation policies and interventions both within and outside VHA. Health systems should target those services associated with more prevalent or costly downstream care. For example, health systems could focus their de-implementation efforts on preoperative tests that result in greater cascades of care through interventions such as preoperative bundles within the electronic medical record or standardized preoperative clinics.
Our study has several important limitations. Using a claims-based approach lacks clinical granularity such as provider decision-making or the ability to determine if the downstream care revealed a meaningful finding. We may have identified an initial preoperative test to be low value when it was actually for diagnostic purposes. By using broad exclusion criteria, we hoped to better capture truly low-value tests. Similarly, we were unable to definitively identify downstream care that occurred as a result of the initial test; however, by using a comparison group, we attempted to account for the baseline level of care occurring in our study sample. Lastly, cost data was unavailable for several invasive services such as valve repair, valve replacement, and coronary bypass surgery. However, these occurred at very low rates within our cohort and likely contributed very little to the overall cost.
In summary, low-value care cascades following two common low-value preoperative tests are common and result in potentially unnecessary care and cost beyond the initial low-value service within the Veterans Health Administration. Characterizing care cascades that result from low-value services can aid health systems and payers to prioritize which low-value services to target for de-implementation, thus reducing the potential for patient harms and mistrust, while yielding the greatest degree of downstream cost savings.
Supplementary Information
(DOCX 68 kb)
Acknowledgements
The authors would like to acknowledge Scott Rothenberger, PhD, Division of General Internal Medicine, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA, who acted as a statistical consultant on this study.
Funding
This work was funded by VA HSR&D Merit Award IIR 19-089 (PI: C. Thorpe). Dr. Oakes’ effort on this study was supported by a postdoctoral fellowship from the Department of Veterans Affairs Office of Academic Affiliations. Dr. Pickering is supported by the National Center For Advancing Translational Sciences of the National Institute of Health under Award Number TL1TR001858.
Declarations
Conflict of Interest
Aaron Schwartz reports receiving personal fees from the Lown Institute, CVS Health, and the Medicare Payment Advisory Commission for prior research consulting outside the scope of the submitted work.
Disclaimer
The Department of Veterans Affairs and the National Institutes of Health had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Carolyn T. Thorpe and Thomas R. Radomski are co-senior authors.
Prior Presentations: This work has not been previously presented.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shrank WH, Rogstad TL, Parekh N. Waste in the US Health Care System: Estimated Costs and Potential for Savings. JAMA. 2019;322(15):1501–1509. doi: 10.1001/jama.2019.13978. [DOI] [PubMed] [Google Scholar]
- 2.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med. 2014;174(7):1067–1076. doi: 10.1001/jamainternmed.2014.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chalmers K, Smith P, Garber J, et al. Assessment of Overuse of Medical Tests and Treatments at US Hospitals Using Medicare Claims. JAMA Netw Open. 2021;4(4):e218075. doi: 10.1001/jamanetworkopen.2021.8075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oakes AH, Radomski TR. Reducing Low-Value Care and Improving Health Care Value. JAMA. 2021;325(17):1715–1716. doi: 10.1001/jama.2021.3308. [DOI] [PubMed] [Google Scholar]
- 6.Korenstein D, Chimonas S, Barrow B, Keyhani S, Troy A, Lipitz-Snyderman A. Development of a Conceptual Map of Negative Consequences for Patients of Overuse of Medical Tests and Treatments. JAMA Intern Med. 2018;178(10):1401–1407. doi: 10.1001/jamainternmed.2018.3573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ganguli I, Lupo C, Mainor AJ, et al. Prevalence and Cost of Care Cascades After Low-Value Preoperative Electrocardiogram for Cataract Surgery in Fee-for-Service Medicare Beneficiaries. JAMA Intern Med. 2019;179(9):1211–1219. doi: 10.1001/jamainternmed.2019.1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bouck Z, Calzavara AJ, Ivers NM, et al. Association of Low-Value Testing With Subsequent Health Care Use and Clinical Outcomes Among Low-risk Primary Care Outpatients Undergoing an Annual Health Examination. JAMA Intern Med. 2020;180(7):973–983. doi: 10.1001/jamainternmed.2020.1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacobs JC, Jarvik JG, Chou R, et al. Observational Study of the Downstream Consequences of Inappropriate MRI of the Lumbar Spine. J Gen Intern Med. 2020;35(12):3605–3612. doi: 10.1007/s11606-020-06181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhatia RS, Bouck Z, Ivers NM, et al. Electrocardiograms in Low-Risk Patients Undergoing an Annual Health Examination. JAMA Intern Med. 2017;177(9):1326–1333. doi: 10.1001/jamainternmed.2017.2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Acker E. How cascade events harm patients. https://lownhospitalsindex.org/publication/how-cascade-events-harm-patients/. Published 2021. Accessed June 30, 2021.
- 12.Ganguli I, Simpkin AL, Lupo C, et al. Cascades of Care After Incidental Findings in a US National Survey of Physicians. JAMA Netw Open. 2019;2(10):e1913325. doi: 10.1001/jamanetworkopen.2019.13325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Radomski TR, Huang Y, Park SY, et al. Low-Value Prostate Cancer Screening Among Older Men Within the Veterans Health Administration. J Am Geriatr Soc. 2019;67(9):1922–1927. doi: 10.1111/jgs.16057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Radomski TR, Feldman R, Huang Y, et al. Evaluation of Low-Value Diagnostic Testing for 4 Common Conditions in the Veterans Health Administration. JAMA Netw Open. 2020;3(9):e2016445. doi: 10.1001/jamanetworkopen.2020.16445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenberg A, Agiro A, Gottlieb M, et al. Early Trends Among Seven Recommendations From the Choosing Wisely Campaign. JAMA Intern Med. 2015;175(12):1913–1920. doi: 10.1001/jamainternmed.2015.5441. [DOI] [PubMed] [Google Scholar]
- 16.Sigmund AE, Stevens ER, Blitz JD, Ladapo JA. Use of Preoperative Testing and Physicians’ Response to Professional Society Guidance. JAMA Internal Medicine. 2015;175(8):1352–1359. doi: 10.1001/jamainternmed.2015.2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirkham KR, Wijeysundera DN, Pendrith C, et al. Preoperative testing before low-risk surgical procedures. Cmaj. 2015;187(11):E349–e358. doi: 10.1503/cmaj.150174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Colla CH, Sequist TD, Rosenthal MB, Schpero WL, Gottlieb DJ, Morden NE. Use of non-indicated cardiac testing in low-risk patients: Choosing Wisely. BMJ Qual Saf. 2015;24(2):149–153. doi: 10.1136/bmjqs-2014-003087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Colla CH, Morden NE, Sequist TD, Schpero WL, Rosenthal MB. Choosing wisely: prevalence and correlates of low-value health care services in the United States. J Gen Intern Med. 2015;30(2):221–228. doi: 10.1007/s11606-014-3070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Radomski TR, Zhao X, Sileanu FE, et al. The Use and Cost of Low-Value Services Delivered to Veterans Through Veterans Affairs Medical Centers and VA Community Care Programs. In: Abstracts from the 2021 Annual Meeting of the Society of General Internal Medicine. J Gen Intern Med. 2021;36(Suppl 1):1–469. [Google Scholar]
- 21.Choosing Wisely: An Intiative of the ABIM Foundation. http://www.choosingwisely.org. Accessed November 11, 2020.
- 22.Feely MA, Collins CS, Daniels PR, Kebede EB, Jatoi A, Mauck KF. Preoperative testing before noncardiac surgery: guidelines and recommendations. Am Fam Physician. 2013;87(6):414–418. [PubMed] [Google Scholar]
- 23.Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64(22):e77–137. doi: 10.1016/j.jacc.2014.07.944. [DOI] [PubMed] [Google Scholar]
- 24.Kristensen SD, Knuuti J, Saraste A, et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA) Eur Heart J. 2014;35(35):2383–2431. doi: 10.1093/eurheartj/ehu282. [DOI] [PubMed] [Google Scholar]
- 25.Noordzij PG, Boersma E, Bax JJ, et al. Prognostic value of routine preoperative electrocardiography in patients undergoing noncardiac surgery. Am J Cardiol. 2006;97(7):1103–1106. doi: 10.1016/j.amjcard.2005.10.058. [DOI] [PubMed] [Google Scholar]
- 26.Joo HS, Wong J, Naik VN, Savoldelli GL. The value of screening preoperative chest x-rays: a systematic review. Can J Anaesth. 2005;52(6):568–574. doi: 10.1007/BF03015764. [DOI] [PubMed] [Google Scholar]
- 27.Byrne MM, Kuebeler M, Pietz K, Petersen LA. Effect of using information from only one system for dually eligible health care users. Med Care. 2006;44(8):768–773. doi: 10.1097/01.mlr.0000218786.44722.14. [DOI] [PubMed] [Google Scholar]
- 28.Rosen AK, Gardner J, Montez M, Loveland S, Hendricks A. Dual-system use: are there implications for risk adjustment and quality assessment? Am J Med Qual. 2005;20(4):182–194. doi: 10.1177/1062860605275791. [DOI] [PubMed] [Google Scholar]
- 29.Griffith KN, Ndugga NJ, Pizer SD. Appointment Wait Times for Specialty Care in Veterans Health Administration Facilities vs Community Medical Centers. JAMA Network Open. 2020;3(8):e2014313–e2014313. doi: 10.1001/jamanetworkopen.2020.14313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Phibbs C, Scott J, Flores N, Barnett P. HERC’s Outpatient Average Cast Dataset for VA Care: Fiscal Year 2013 Update. Guidebook. In: Department of Veterans Affairs, ed. Menlo Park, CA: VA Palo Alto, Health Economics Resource Center (HERC); 2014.
- 31.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 32.US Dept of Veterans Affairs. Summary of VHA Facility Complexity Model. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=2793591&FileName=VA118-16-R-1059-A00002002.docx. Accessed December 10, 2020.
- 33.Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thomas L, Li F, Pencina M. Using Propensity Score Methods to Create Target Populations in Observational Clinical Research. JAMA. 2020;323(5):466–467. doi: 10.1001/jama.2019.21558. [DOI] [PubMed] [Google Scholar]
- 35.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–3679. doi: 10.1002/sim.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saini SD, Powell AA, Dominitz JA, et al. Developing and Testing an Electronic Measure of Screening Colonoscopy Overuse in a Large Integrated Healthcare System. J Gen Intern Med. 2016;31(Suppl 1):53–60. doi: 10.1007/s11606-015-3569-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubenstein JH, Pohl H, Adams MA, et al. Overuse of Repeat Upper Endoscopy in the Veterans Health Administration: A Retrospective Analysis. Am J Gastroenterol. 2017;112(11):1678–1685. doi: 10.1038/ajg.2017.192. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 68 kb)