Abstract
Background
Little is known about knowledge, attitudes and behaviors concerning Chagas disease (CD) among Latin American migrants in Germany to inform public health decision making.
Methods
A cross-sectional, questionnaire-based study was conducted between March 2014 and October 2019 among Latin American migrants in six cities in Germany to obtain information on migration history, socioeconomic and insurance status, knowledge about CD, potential risk factors for Trypanosoma cruzi infection, and willingness to donate blood or organs.
Results
168 participants completed the questionnaire. The four countries with the highest proportion of participants contributing to the study population were Colombia, Mexico, Peru and Ecuador. Before migrating to Europe, the majority of the study population resided in an urban setting in houses made of stone or concrete, had higher academic education and was integrated into the German healthcare and healthcare insurance system. The majority of all study participants were also willing to donate blood and organs and a quarter of them had donated blood previously. However, many participants lacked basic knowledge about symptoms and modes of transmission of Chagas disease. One out of 56 serologic tests (1.8%) performed was positive. The seropositive female participant born in Argentina had a negative PCR test and no signs of cardiac or other organ involvement.
Conclusions
The study population does not reflect the population structure at risk for T. cruzi infection in endemic countries. Most participants had a low risk profile for infection with T. cruzi. Although the sample size was small and sampling was not representative of all persons at risk in Germany, the seroprevalence found was similar to studies previously conducted in Europe. As no systematic screening for T. cruzi in Latin American blood and organ donors as well as in women of child-bearing age of Latin American origin is implemented in Germany, a risk of occasional transmission of T. cruzi remains.
Keywords: Chagas, non-endemic country, Latino, migrant, immigration, primary prevention, health initiative, knowledge
Introduction
Infection with the parasite Trypanosoma cruzi (T. cruzi) can cause Chagas disease (CD), which constitutes a major health problem in the Latin American (LA) region. According to the World Health Organization (WHO), CD belongs to the group of neglected tropical diseases which are typically associated with poverty (WHO, 2022b). CD is a chronic disease associated with disability, stigma, and a high socioeconomic burden for patients as well as for the societies in which the disease is endemic (Conteh et al., 2010; WHO, 2022b).
T. cruzi persists for a lifetime within host cells and the infection can cause irreversible organ damage. Organs such as the heart and gastrointestinal tract are particularly affected (Bern, 2015). Infection with T. cruzi remains undiagnosed in most cases. As a consequence, only 1% of patients receive treatment in the acute phase, and even less patients receive adequate medical care in the chronic phase. It is estimated that at least 6-7 million people are infected with T. cruzi globally, with about 38,000 new cases every year in Latin America (PAHO, 2019; WHO, 2022a).
For many decades, CD was considered an infection transmitted by contact with the faeces of an infected triatomine bug in rural areas. Migration to larger cities in the LA region led to a change in the epidemiological profile towards an emerging infection in semi-urban and urban areas (Delgado et al., 2013; Gaspe et al., 2020; WHO, 2021)
Today, due to international migration, a significant number of people infected with T. cruzi live in regions where the infection is not endemic. By 2009, only 4,290 T. cruzi cases were diagnosed in Europe; the estimated number of cases however ranges from 70,000 to 120,000 (Basile et al., 2011; Strasen et al., 2014). For this reason, the WHO strongly recommends the implementation of preventive measures to avoid transmission of T. cruzi infection in the European region. In some countries, such as in Spain, seroprevalence studies were conducted successfully and measures of infection control, such as screening of blood and organ donors and women of child-bearing age, were implemented and are still ongoing in people of LA origin (Monge-Maillo and L Opez-V Elez, 2017; Iglesias-Rus et al., 2019).
Estimations based on prevalence in endemic countries combined with the corresponding migrant population in Germany suggest that approximately 2,000 (range 759-3,256) migrants infected with T. cruzi are currently living in Germany (Strasen et al., 2014). To date, only two studies with small sample sizes have been conducted in Germany giving information on seroprevalence; a prevalence of 2% in a Latin American and a prevalence of 9% in a Bolivian migrant population were reported (Frank et al., 1997; Navarro et al., 2017 ).
Similar to the low level of awareness in their countries of origin, it can be assumed that people of LA origin residing in non-endemic countries are not aware of their risk for infection and their infection status (Hurtado et al., 2014; Di Girolamo et al., 2016). Moreover, they may not be aware of the fact that they could transmit the infection to others (Romay-Barja et al., 2021). Therefore, the implementation of CD screening, counseling and testing programs targeted to the population at risk could be an important public health measure to prevent T. cruzi transmission in Germany. This study therefore aims to examine knowledge, attitudes and behaviors towards CD in LA migrants in Germany and to explore their attitude and potential history of blood and/or organs donation to identify potential starting points for public health interventions in Germany.
Methods
ELCiD is a German network dedicated to the identification and management of CD patients in Germany (German: “Erkennung und Lenkung von Chagas Patienten in Deutschland”, http://chagas.info). A cross-sectional study was conducted in six cities across Germany between March 2014 and October 2019. Study centers were located at Charité University Hospital in Berlin, Bernhard Nocht Institute for Tropical Medicine (BNITM) in Hamburg, Department of Infectious Diseases and Tropical Medicine at Ludwig-Maximilians University (LMU) in Munich, Department of Tropical Medicine at Missioklinik Würzburg and University Hospital in Würzburg, University Hospital in Marburg, and Kliniken Maria Hilf in Mönchengladbach. Participants meeting at least one of the following criteria were eligible: a place of birth in a country endemic to CD, residence in an endemic country for at least 10 years while under the age of 25 or a mother born in an endemic country. Endemic countries were defined according to the WHO country list (WHO, 2022a). All participants had to have their place of residence in Germany at the time of study participation. The recruitment of participants employed convenience sampling through different strategies: Individuals with LA migration background were recruited in healthcare institutions at tropical medicine outpatient departments (predominantly when attending the hospital for other pathologies or prenatal care) or at Latin American socio-cultural events. Leaflets, informative talks, and social media were used to spread information. Participants were also encouraged to invite friends and relatives to participate in the study.
After obtaining written informed consent, each participant was given a self-administered questionnaire consisting of 52 questions in their preferred language (German, Spanish or Portuguese). The questions aimed to collect data on demographics, socioeconomic background, migration history, knowledge awareness and behavior towards CD as well as willingness to donate blood and/or organs. The paper-based questionnaires were pseudonymized and imported into an electronic database located at the Comprehensive Heart Failure Center (CHFC) Würzburg. Positive response rates were used for descriptive analysis (e.g., willingness to donate blood, knowledge of CD, willingness to donate organs). Data analysis was carried out with Stata (version 15.1), Microsoft Office Excel 2019 for Mac v.16.52, and Graphpad Prism V.9.4.1. A frequency of a positive response in the range of 10% up to 50% was anticipated (Salim et al., 2010). We calculated a minimum sample size of 139 participants to achieve a precision of ±5% at a confidence level of 95% for a positive response rate of 10%.
Participants were offered testing and counselling for CD. For participants below 18 years of age, an additional version in simpler language was handed out, and consent was also obtained by parents or the legal guardian.
Blood samples were analyzed at LMU in Munich and BNITM in Hamburg. In-house ELISA and in-house IFAT assays were used for serological diagnosis of infection with T. cruzi (for more information on testing for T.cruzi in institutions in Germany, see Guggenbühl Noller et al., 2020). A blood sample was considered positive only if both, ELISA and IFAT were positive. In case of a positive serologic test result, further medical care including screening for clinical manifestations of CD and - if indicated - treatment with Benznidazole was offered. The study received ethical approval at Charité – Universitätsmedizin Berlin (EA2/209/18) and at each of the participating study sites. The study was performed according to the Helsinki declaration.
Results
Survey sample description
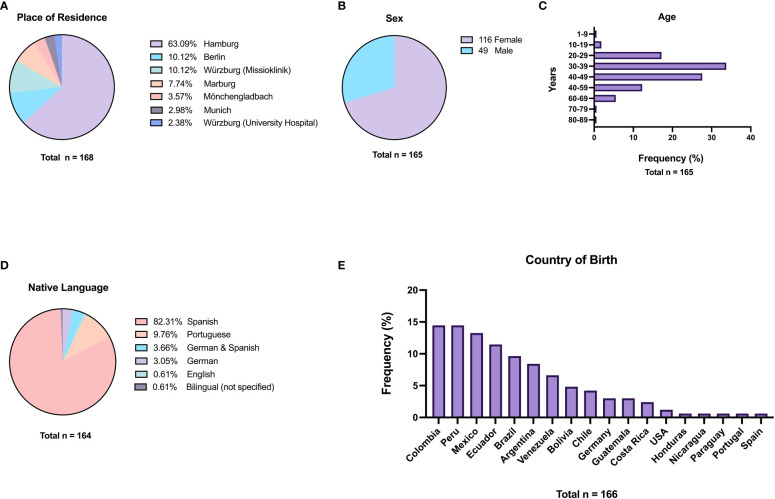
In total, 168 participants were included and answered the questionnaire. Most participants were recruited in Hamburg (63.1%), Würzburg (12.5%) Berlin (10.1%), and in Marburg (7.7%) ( Figure 1A ). Demographic characteristics of the study population are summarized in Figures 1A–E . Most participants were women (70.3%). The largest group of participants was aged 30 to 39 years (33.7%), followed by participants aged 40 to 49 years (27.6%). 76.7% of participating women were of reproductive age (15-49 years). Participants originated from 14 LA countries; a minimum of 10% of participants came from each of the following countries: Colombia, Peru, Mexico, and Ecuador. For most participants, the country of birth and the country where the participants were raised was identical (86.3%); this applied also to the declared country of last residence before moving to Europe (also 86.3%). 8 (4.8%) participants born in Germany, Spain, and the U.S. were included based on their mothers being born in an endemic country. Most participants (82.3%) declared to speak Spanish as their native language, and 9.7% of the participants declared to speak Portuguese as native language. Only 3.7% answered having been raised bilingually in German and Spanish. The largest group of participants migrated to Germany between 2010 and 2019 (39.1%), followed by the groups migrating between 2000 and 2009 (31.4%) and between 1990 and 1999 (19.9%) to Germany. The remaining 9.6% immigrated before 1990. Reasons for migration to Europe were marriage (32.5%) closely followed by education (30.6%), family reunification (13.8%), work (11.9%), and other reasons (11.2%).
Figure 1.
Characteristics of the study participants. (A) Place of residence in Germany; (B) Sex; (C) Age at time of study; (D) Native language; (E) Country of birth.
Socioeconomic risk factors for Chagas disease
Participants were asked for known risk factors of T. cruzi infection related to the setting and type of housing as well as the construction material of their last residence in LA during childhood ( Table 1 ). The vast majority of participants (≥90%) lived in urban (for convenience, defined as a city of ≥10,000 inhabitants) areas in LA prior to migration to Germany as well as during childhood. Of all participants, 87.5% lived in houses constructed with stone or concrete, and only a minority lived in houses built with adobe or wood. Nevertheless, 36.9% of participants declared to have seen a kissing bug in their own house during childhood.
Table 1.
Risk factors for Chagas disease related to location and type of housing.
| Question | Choices | No. of answers | Rate of answers (%) | Total no. of answers | Total answer rate (%) |
|---|---|---|---|---|---|
| Where in Latin America did you spend most part of your childhood? | Urban | 137 | 90.7 | 151 | 89.9 |
| Rural | 14 | 9.3 | |||
| Your last residence in Latin America before coming to Europe was | Urban | 141 | 92.2 | 153 | 91.1 |
| Rural | 12 | 7.8 | |||
| What kind of material was the house made of in which you spent your childhood? | Stone/Concrete | 140 | 87.5 | 160 | 95.2 |
| Adobe | 9 | 5.6 | |||
| Wood | 8 | 5 | |||
| Others | 3 | 1.9 | |||
| Have you ever seen an insect called a kissing bug* in your own house? | Yes | 58 | 36.9 | 157 | 93.4 |
*Or vinchucha, barbeiro, chirimacha, pito, chichâ.
We asked participants about their own and their parents´ educational backgrounds ( Table 2 ). The participants´ highest educational degree was a university degree in 55.1% (47.5% among parents of participants) and completed professional training in 23.4% (20.6% among parents of participants). 19.6% (19.4% among parents of participants) finished secondary school and very few (1.9%, 10% among parents of participants) had finished primary school only. None of the participants answered to have no educational degree whereas 2.5% of participant´s parents had no educational degree.
Table 2.
Socioeconomic risk factors for infection with T. cruzi.
| Question | Choices | No. of answers | Rate of answers (%) | Total no. of answers | Total answer rate (%) |
|---|---|---|---|---|---|
| What is your highest level of education? | No degree | 0 | 0 | 158 | 94.0 |
| Primary school | 3 | 1.9 | |||
| Secondary school | 31 | 19.6 | |||
| Professional Training | 37 | 23.4 | |||
| University degree | 87 | 55.1 | |||
| What is the highest level of education of your parents? | No degree | 4 | 2.5 | 160 | 95.2 |
| Primary school | 16 | 10 | |||
| Secondary school | 31 | 19.4 | |||
| Professional Training | 33 | 20.6 | |||
| University degree | 76 | 47.5 | |||
| Have you ever heard of Chagas disease in your country of origin? | Yes | 80 | 50 | 160 | 95.2 |
| No | 80 | 50 | |||
| Does anyone in your close family suffer from/did suffer from Chagas disease?* | Yes | 4 | 2.6 | 155 | 92.3 |
| No | 101 | 65.2 | |||
| I don´t know | 50 | 32.2 | |||
| Do you know people in your place of residence in Latin America with Chagas disease? | Yes | 21 | 13.1 | 160 | 95.2 |
*of the 4 participants, 2 indicated mother and 2 grandmothers as family members with Chagas.
Knowledge about Chagas disease
Half of the participants had heard about CD in their country of origin before coming to Europe and 13.1% of participants knew someone with CD in their former place of residence in LA. Four participants even had close family members with CD, two of them reported having a mother suffering from CD and two reported having a grandmother with CD.
We asked participants using an open question to name the most frequent symptoms of Chagas disease ( Table 3 ). Less than 5% of all study participants named at least three correct symptoms, 13.1% named two symptoms and 10.7% named only one correct symptom of CD. More than 70% gave incorrect answers or did not answer the question at all.
Table 3.
Knowledge about Chagas disease.
| Question | Choices | No. of answers | Rate of answers (%) | Total no. of answers | Total answer rate (%) |
|---|---|---|---|---|---|
| Which health problems are caused by Chagas disease? Please name the three most frequent symptoms. (Open question) |
3 correct symptoms | 8 | 4.8 | n/a | n/a |
| 2 correct symptoms | 22 | 13.1 | |||
| 1 correct symptom | 18 | 10.7 | |||
| None correct or not answered | 120 | 71.4 | |||
| How is Chagas disease transmitted? (Multiple answers possible) | Vinchuca | 92 | 55.8 | 165 | 98.2 |
| Mother/child | 29 | 17.5 | |||
| Sexual | 2 | 1.2 | |||
| Sugar cane juice | 5 | 3.0 | |||
| Blood transfusion | 38 | 23.0 | |||
| Organ transplant | 19 | 11.5 | |||
| Mosquito bite | 15 | 9.1 | |||
| Physical contact with infected person | 1 | 0.6 | |||
| Modes of transmission unknown | 45 | 27.3 | |||
| Is it possible to have Chagas disease without having symptoms? | Yes | 65 | 42.2 | 154 | 91.7 |
| No | 8 | 5.2 | |||
| I don´t know | 81 | 52.6 |
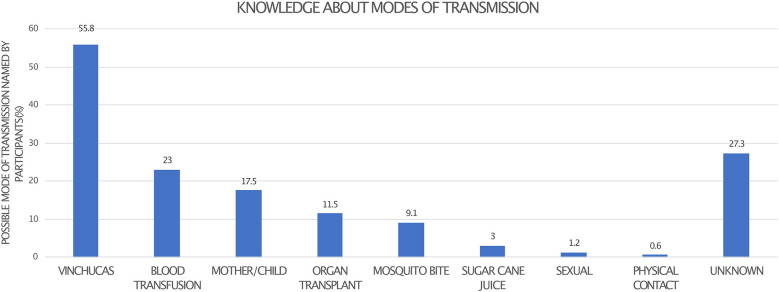
We then offered several pre-specified correct and incorrect answers for CD transmission (see Supplementary Material ) and participants were asked to mark the correct modes of transmission. 55.8% correctly identified transmission via a vector, 23% transmission via blood transfusion, and 17.5% congenital transmission from mother to child. Only 3% of participants considered oral infection by consuming contaminated sugar cane juice as a correct option; for details see Figure 2 . 42.2% of respondents confirmed correctly that affected persons can be without symptoms despite being infected with T. cruzi.
Figure 2.
Participants were asked to name all correct modes of CD transmission.
Attitude towards blood and organ donation
66% of participants are willing to donate blood in the future and 55.1% are willing to donate organs. 43 participants (26.9%) had donated blood previously, 14 (32.6%) of them in Germany. 11 participants (6.9%) had received a blood transfusion previously, and six of those received the transfusion in a country endemic to CD ( Table 4 ).
Table 4.
Risk of transmission in non-endemic areas.
| Question | Choices | No. of answers | Rate of answers (%) | Total no. of answers | Total answer rate (%) |
|---|---|---|---|---|---|
| Have you ever received a blood transfusion? | Yes | 11 | 6.9 | 160 | 95.2 |
| No | 149 | 93.1 | |||
| Have you ever donated blood? | Yes | 43 | 26.9 | 160 | 95.2 |
| No | 117 | 73.1 | |||
| Country of previous blood donation | Argentina | 4 | 10 | 40 | 93.0* |
| Brazil | 2 | 5 | |||
| Chile | 2 | 5 | |||
| Colombia | 3 | 7.5 | |||
| Ecuador | 1 | 2.5 | |||
| Germany | 11 | 27.5 | |||
| Guatemala | 1 | 2.5 | |||
| Mexico | 7 | 17.5 | |||
| Peru | 2 | 5 | |||
| Spain | 2 | 5 | |||
| USA | 1 | 2.5 | |||
| Venezuela | 1 | 2.5 | |||
| Germany and LA | 3 | 7.5 | |||
| Year of blood donation | 1970-1979 | 1 | 3.2 | 31 | 72.1* |
| 1980-1989 | 0 | 0 | |||
| 1990-1999 | 6 | 19.4 | |||
| 2000-2009 | 8 | 25.8 | |||
| 2010-2019 | 16 | 51.6 | |||
| Are you willing to donate blood in the future? | Yes | 107 | 66.0 | 162 | 96.4 |
| No | 33 | 20.4 | |||
| I don´t know | 22 | 13.6 | |||
| Are you willing to donate organs after death? | Yes | 93 | 57.1 | 163 | 97.0 |
| No | 36 | 22.1 | |||
| I don´t know | 34 | 20.9 |
*Answer rate of all participants that replied “Yes” to blood donation.
Serological status and prior Chagas treatment
Only 13 participants (8%) stated to have been tested for CD before, with two of them reporting a positive result (details see Table 5 ). One participant indicated to have received Chagas therapy before. Of all 168 participants, 56 (33.9%) consented to serological testing for CD after completing the questionnaire. One participant was found to have a positive test result. The seroprevalence of infection with T. cruzi was 1.8% in our study population. The participant with a positive test was a female born in 1988 in Argentina to a mother known to be seropositive. She never had lived in a rural area and reported to have never seen a triatomine bug or having received a blood transfusion; congenital transmission is the most probable way of infection in this case. The participant who tested positive was asymptomatic, had a negative PCR result, and no evidence of CD in ECG and echocardiography. She had never donated blood before. She was aware of her serostatus before the test was done and stated that she had been looking unsuccessfully for specialized medical care as she felt that her German family practitioner did not take her condition seriously.
Table 5.
Medical history.
| Question | Choices | No. of answers | Rate of answers (%) | Total no. of answers | Total answer rate (%) |
|---|---|---|---|---|---|
| Have you ever been tested for Chagas disease? | Yes | 13 | 8.0 | 163 | 97.0 |
| No | 150 | 92.0 | |||
| Year of previous test | 1990-1999 | 3 | 25 | 12 | 7.1 |
| 2000-2009 | 3 | 25 | |||
| 2010-2019 | 6 | 50 | |||
| Result of previous test | Positive | 2 | 18.2 | 11 | 6.5 |
| Negative | 9 | 81.8 | |||
| Have you ever received treatment against Chagas disease? | Yes | 1 | 5.6 | 18 | 10.7 |
| No | 17 | 94.4 | |||
| Do you suffer from heart disease? | Yes | 6 | 3.7 | 161 | 95.8 |
| No | 155 | 96.3 | |||
| If you suffer from heart disease, what is the diagnosis? | Hypertension | 1 | 16.7* | 3 | 1.8 |
| Myocardial infarction | 2 | 33.3* | |||
| Do you suffer from gastrointestinal disease? | Yes | 20 | 13.1 | 153 | 91.1 |
| No | 133 | 86.9 | |||
| If yes, what are your symptoms or which diagnosis was given to you? (open question, multiple answers possible) |
Chronic constipation | 1 | 5** | 20 | 11.9 |
| Diarrhea | 1 | 5** | |||
| Esophageal hernia | 1 | 5** | |||
| Fatty liver | 1 | 5** | |||
| Flatulence | 1 | 5** | |||
| Food intolerance | 1 | 5** | |||
| Fructose intolerance | 1 | 5** | |||
| Gall stones | 1 | 5** | |||
| Gastritis | 6 | 30** | |||
| Gastroenteritis | 1 | 5** | |||
| Irritable bowel syndrome | 3 | 15** | |||
| Lactose intolerance | 2 | 10** | |||
| Pain in the mouth/stomach | 1 | 5** | |||
| Reflux | 5 | 25** | |||
| Stomach problems | 2 | 10** |
* Of all participants that suffer from heart disease.
** of all participants that suffer from gastrointestinal disease.
Access to healthcare in Germany
More than 90% of participants were members of the German health insurance system (statutory or private health insurance), and 4.2% had student insurance. Only 2.5% were insured with foreign insurance and 2.5% had no health insurance ( Table 6 ).
Table 6.
Access to medical care in Germany.
| Question | Choices | No. of answers | Rate of answers (%) | Total no. of answers | Total answer rate (%) |
|---|---|---|---|---|---|
| Do you get sufficient medical care in Germany? | Yes, there are no problems to get sufficient health care | 134 | 84.3 | 159 | 94.6 |
| Yes, but there are some problems to get health care | 16 | 10.1 | |||
| No, there are severe problems to get health care | 9 | 5.7 | |||
| What kind of health insurance do you have in Germany? | German health insurance (statutory/private) | 148 | 90.8 | 163 | 97.0 |
| Health insurance for students | 7 | 4.3 | |||
| Foreign insurance | 4 | 2.5 | |||
| None | 4 | 2.5 |
The vast majority of respondents (84.3%) did not report difficulties obtaining adequate healthcare in Germany, 10.1% reported that they encountered minor problems and 5.7% said they experienced high barriers to access medical care.
Discussion
This cross-sectional study among people living in Germany with a history of migration from countries where CD is endemic presents information on knowledge, behavior, social determinants, and serological results relevant for understanding the epidemiology and potential risk factors for T. cruzi infection in Germany.
In general, the results indicate that the population in Germany at risk for infection with T. cruzi may differ in many aspects from the typical population at risk in endemic countries. The majority of participants come from urban areas and are either well educated or come for academic or professional purposes to Germany. Most participants grew up in houses with a low risk for vector infestation. Our results confirm earlier observations from a cohort of Bolivian migrants in Munich where a very similar population structure in terms of education and socioeconomic status was found (Navarro et al., 2017). Even though the representativeness of these two available studies in Germany is still limited, the data nevertheless indicate that assumptions made e.g., on the prevalence of T. cruzi infection in the home countries of migrants may not apply to the corresponding migrant population in Germany. This may have implications, particularly for the frequently used method of estimating prevalence in non-endemic countries by extrapolating prevalence in endemic countries to the migrant population in non-endemic countries (Gascon et al., 2010; Strasen et al., 2014; Requena-Méndez et al., 2015). As the risk profile for this poverty-related infection among LA migrants in Germany was lower than the average in the respective LA countries, there is a risk for over-estimating prevalence in non-endemic settings. Regarding screening activities for T. cruzi infection in Germany, these results show that - besides CD prevalence in the country of origin - an evaluation of individual risk factors (e.g., exposure to vectors in childhood, housing status and setting, individual socioeconomic status) might be more important than using migration history from LA alone as the dominant criterion assessing the individual risk for infection with T. cruzi.
Population-representative studies accurately determining seropositivity for T. cruzi infection in non-endemic countries do not exist, but accurate data would be of outstanding importance for making public health decisions, e.g., for ante- and perinatal medical care or screening in blood and organ donors. The best available data comes from cohorts of LA blood donors in Spain where seroprevalence rates between 0.05% and 1.38% among LA migrants were observed, which is slightly less than the average of the calculated country-specific prevalence in Spain obtained by extrapolation from endemic country prevalence (average 2.1%, range 0 - 10.9%) (Gascon et al., 2010). A recent study analyzing laboratory data from German test centers found a positivity rate of 1.4% among all tested individuals (not all persons tested were of LA origin) (Guggenbühl Noller et al., 2020). Together with the only other study in Germany (Frank et al., 1997) giving a prevalence estimate of 2%, data from this study adds further information to support the hypothesis that an overall prevalence among LA migrants in Germany between 1 – 2% can be assumed.
The majority of respondents in our study were willing to donate blood. 14 (8.3%) of them had already donated blood in Germany. Unfortunately, the German blood transfusion system is not yet prepared to prevent Chagas transmission. Currently, the following policy, which is in line with the European Commission guidelines on the quality and safety of blood and tissue banks, is in place: If a donor is aware of being infected with T. cruzi, he/she will be automatically excluded from donation (Bundesärztekammer et al., 2021). However, if the donor is not aware of an infection and no routine screening for CD is performed at the blood bank, a transmission is not prevented via blood donation in Germany. Supported by the data from this and other European studies, this practice should be reconsidered and blood donors of LA origin should actively be offered screening for infection with T. cruzi.
Local access to healthcare is a key determinant of health for migrants. Although access to healthcare varies among the specific countries and immigrant populations, it is a common pattern that especially undocumented migrants experience very limited access to healthcare. In our group of participants, more than 80% declare to have sufficient access to the German medical system, while only 5.7% reported having problems.
Regarding the congenital transmission of CD in non-endemic regions, the most well-documented data comes from the U.S. and Spain. It is estimated that there are approximately 40,000 women of childbearing age infected with CD in the U.S. while the risk of transmission ranges from 1 - 5%. Thus, there may be as many as 300 congenital cases in the United States per year (Bennett et al., 2018; Edwards et al., 2019). In Europe, similar transmission rates in Spain and Italy (Rodari et al., 2018; Basile et al., 2019) are reported. There are no preventive measures in place to avoid congenital transmission in Germany until now. In our study, we show that only 21.3% (17 out of 80) of women of childbearing age were aware of the possibility of vertical transmission. This finding, in combination with lacking routine screening measures in pregnancy, indicates a potential risk for Chagas vertical transmission in Germany.
Overall, our results show that most Latin Americans who participated in the study lacked knowledge about CD, particularly about how it can be transmitted despite the participants’ high socio-economic and education status. Taking further into account that information about CD could have been conveyed prior to study participation, we must assume that knowledge about CD in the general LA migrant population is even lower than described here. The lack of information in the study population can be explained by the fact that CD is a neglected and stigmatized disease in endemic countries. Most participants were curious after completing the questionnaire and wanted to learn more. They received comprehensive information about CD after study participation.
This cross-sectional study had limitations. The sample size is limited and the study team did not have resources to conduct a study representative of Germany’s entire LA migrant population. Convenient sampling was used, which likely caused a sampling bias. In particular, participants with a lower socioeconomic status could have experienced higher barriers and had less opportunity to take part in this study. Participants recruited at healthcare institutions probably had already less problems accessing the healthcare system than the average LA migrant population. Moreover, a network bias (i.e., persons of the same socioeconomic status may have promoted participation mostly to other people with similar status) can be assumed.
In conclusion, migrants from LA living in Germany who participated in this study had a high socioeconomic status, a high level of education, and were well integrated into the German society. Despite a potential bias in recruitment, the results indicate that the LA migrant population in Germany may differ from the population structure in their respective home countries. Risk factors for infection with T. cruzi may not be evaluated by migration status alone; an individual assessment of known risk factors of exposure in their respective home countries and the risk of vertical transmission should be equally considered. Despite a high level of education, knowledge about CD was still poor. Serological prevalence of infection with T. cruzi in this non-representative study was comparable to previous and other European data but highlights again the need for improved guidelines and practices particularly regarding ante- and postnatal care as well as blood transfusion and organ transplantation services.
Data availability statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MW, AS, MP and TZ conceived the study. All authors contributed to data collection. MW, RG analyzed the data; MW, RG and wrote the manuscript and TZ guided the writing process. All authors contributed to reviewing the final manuscript.
Acknowledgments
We thank all of the participants who voluntarily participated in this survey and for sharing their time and experiences.
Funding Statement
This cross-sectional study did not receive specific funding. RG was supported and gratefully acknowledges a Merit-based Ph.D. scholarship from the Konrad Adenauer Foundation (KAS). Serologic testing for participants was made possible by a fee reduction for testing from Division of Infectious Diseases and Tropical Medicine, University Hospital, Ludwig-Maximilians-Universität München, and by private donations collected by Missionsärztliches Institut Würzburg.
Conflict of interest
Author MB was employed by Medical Department of the worldwide air ambulance Unicair GmbH, Idstein, Germany and Department of Occupational Medicine, B.A.D, Health Center, Koblenz, Germany.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcimb.2022.1047281/full#supplementary-material
References
- Basile L., Jansa J. M., Carlier Y., Salamanca D. D., Angheben A., Bartoloni A., et al. (2011). Chagas disease in european countries: The challenge of a surveillance system. Eurosurveillance 16 (37), 3. doi: 10.2807/ESE.16.37.19968-EN/CITE/PLAINTEXT [DOI] [PubMed] [Google Scholar]
- Basile L., Ciruela P., Requena-Méndez A., Vidal M. J., Dopico E., Martín-Nalda A., et al. (2019). Epidemiology of congenital chagas disease 6 years after implementation of a public health surveillance system, Catalonia 2010 to 2015. Euro surveillance: Bull. Europeen sur les maladies transmissibles = Eur. communicable Dis. Bull. 24 (26), 15–30. doi: 10.2807/1560-7917.ES.2019.24.26.19-00011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett C., Straily A., Haselow D., Weinstein S., Taffner R., Yaglom H., et al. (2018). Chagas disease surveillance activities — seven states 2017. Morbidity Mortality Weekly Rep. 67 (26), 738. doi: 10.15585/MMWR.MM6726A2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bern C. (2015). Chagas’ disease. New Engl. J. Med. 373 (5), 456–466. doi: 10.1056/NEJMRA1410150 [DOI] [PubMed] [Google Scholar]
- Bundesärztekammer et al. (2021) Richtlinie zur gewinnung von blut und blutbestandteilen und zur anwendung von blutprodukten (Richtlinie hämotherapie). Available at: https://www.bundesaerztekammer.de/themen/medizin-und-ethik/wissenschaftlicher-beirat/stellungnahmen-richtlinien-jahresberichte/haemotherapie-transfusionsmedizin/richtlinie-zur-gewinnung-von-blut-und-blutbestandteilen-und-zur-anwendung-von-blutprodukten-richtlinie-haemotherapie (Accessed 4 September 2022). Gesamtnovelle 2017, umschriebene Fortschreibung 2021.
- Conteh L., Engels T., Molyneux D. H. (2010). Socioeconomic aspects of neglected tropical diseases. Lancet 375 (9710), 239–247. doi: 10.1016/S0140-6736(09)61422-7 [DOI] [PubMed] [Google Scholar]
- Delgado S., Ernst K. C., Pumahuanca M. L., Yool S. R., Comrie A. C., Sterling C. R., et al. (2013). A country bug in the city: urban infestation by the chagas disease vector triatoma infestans in arequipa, Peru. Int. J. Health Geogr. 12, 48. doi: 10.1186/1476-072X-12-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Girolamo C., Martelli G., Ciannameo A., Vocale C., Fini M., Stefanini A., et al. (2016). Chagas disease in a non-endemic country: A multidisciplinary research, Bologna, Italy. J. immigrant minority Health 18 (3), 616–623. doi: 10.1007/s10903-015-0214-0 [DOI] [PubMed] [Google Scholar]
- Edwards M. S., Stimpert K. K., Bialek S. R., Montgomery S. P. (2019). Evaluation and management of congenital chagas disease in the united states. J. Pediatr. Infect. Dis. Soc. 8 (5), 461–469. doi: 10.1093/JPIDS/PIZ018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank M., Hegenscheid B., Janitschke K., Weinke T. (1997). Prevalence and epidemiological significance of trypanosoma cruzi infection among Latin American immigrants in Berlin, Germany. Infection 25 (6), 355–358. doi: 10.1007/BF01740817 [DOI] [PubMed] [Google Scholar]
- Gascon J., Bern C., Pinazo M. J. (2010). Chagas disease in Spain, the united states and other non-endemic countries. Acta Tropica 115 (1–2), 22–27. doi: 10.1016/J.ACTATROPICA.2009.07.019 [DOI] [PubMed] [Google Scholar]
- Gaspe M. S., Fernández M. D. P., Cardinal M. V., Enriquez G. F., Rodríguez-Planes L. I., Macchiaverna N. P., et al. (2020). Urbanisation, risk stratification and house infestation with a major vector of chagas disease in an endemic municipality of the Argentine chaco. Parasites Vectors 13 (1), 316. doi: 10.1186/S13071-020-04182-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guggenbühl Noller J. M., Froeschl G., Eisermann P., Jochum J., Theuring S., Reiter-Owona I., et al. (2020). Describing nearly two decades of chagas disease in Germany and the lessons learned: A retrospective study on screening, detection, diagnosis, and treatment of trypanosoma cruzi infection from 2000 – 2018. BMC Infect. Dis. 20 (1), 919. doi: 10.1186/S12879-020-05600-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurtado L. A., Calzada J. E., Pineda V., González K., Santamaría A. M., Cáceres L., et al. (2014). Conocimientos y factores de riesgo relacionados con la enfermedad de chagas en dos comunidades panameñas donde rhodnius pallescens es el vector principal. Biomed. Rev. del Instituto Nacional Salud 34 (2), 260–270. doi: 10.1590/S0120-41572014000200012 [DOI] [PubMed] [Google Scholar]
- Iglesias-Rus L., Romay-Barja M., Boquete T., Benito A., Blasco-Hernández T. (2019). The role of the first level of health care in the approach to chagas disease in a non-endemic country. PloS Negl. Trop. Dis. 13 (12), e0007937. doi: 10.1371/JOURNAL.PNTD.0007937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monge-Maillo B., L Opez-V Elez R. (2017). Challenges in the management of chagas disease in Latin-American migrants in Europe. Clin. Microbiol. Infect. 23, 290–295. doi: 10.1016/j.cmi.2017.04.013 [DOI] [PubMed] [Google Scholar]
- Navarro M., Berens-Riha N., Hohnerlein S., Seiringer P., von Saldern C., Garcia S., et al. (2017). Cross-sectional, descriptive study of chagas disease among citizens of Bolivian origin living in Munich, Germany. BMJ Open 7 (1), e013960. doi: 10.1136/BMJOPEN-2016-013960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- PAHO (2019) Guidelines for the diagnosis and treatment of chagas disease. Available at: https://iris.paho.org/bitstream/handle/10665.2/49653/9789275120439_eng.pdf (Accessed 4 September 2022).
- Requena-Méndez A., Aldasoro E., de Lazzari E., Sicuri E., Brown M., Moore D., et al. (2015). Prevalence of chagas disease in Latin-American migrants living in Europe: A systematic review and meta-analysis. PLoS Negl. Trop. Dis. 9 (2), e0003540. d.oi: 10.1371/journal.pntd.0003540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodari P., Angheben A., Gennati G., Trezzi L., Bargiggia G., Maino M., et al. (2018). Congenital chagas disease in a non-endemic area: Results from a control programme in bergamo province, northern Italy. Travel Med. Infect. Dis. 25, 31–34. doi: 10.1016/J.TMAID.2018.04.011 [DOI] [PubMed] [Google Scholar]
- Romay-Barja M., Iglesias-Rus L., Boquete T., Benito A., Blasco-Hernández T. (2021). Key chagas disease missing knowledge among at-risk population in Spain affecting diagnosis and treatment. Infect. Dis. Poverty 10 (1), 55. doi: 10.1186/s40249-021-00841-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salim A., Schulman D., Ley E. J., Berry C., Navarro S., Chan L. S. (2010). Contributing factors for the willingness to donate organs in the Hispanic American population. Arch. Surg. (Chicago Ill.: 1960) 145 (7), 684. doi: 10.1001/ARCHSURG.2010.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strasen J., Williams T., Ertl G., Zoller T., Stich A., Ritter O. (2014). Epidemiology of chagas disease in Europe: Many calculations, little knowledge. Clin. Res. Cardiol. 103 (1), 1–10. doi: 10.1007/S00392-013-0613-Y [DOI] [PubMed] [Google Scholar]
- WHO . (2021). WHO calls for comprehensive equitable access to health care for every chagas disease patient. Available at: https://www.who.int/news/item/14-04-2021-who-calls-for-comprehensive-equitable-access-to-healthcare-for-every-chagas-disease-patient (Accessed 4 September 2022).
- WHO . (2022. a). WHO fact sheet chagas disease. Available at: https://www.who.int/news-room/fact-sheets/detail/chagas-disease-(american-trypanosomiasis) (Accessed 4 September 2022).
- WHO . (2022. b). WHO neglected tropical diseases. Available at: https://www.who.int/health-topics/neglected-tropical-diseases#tab=tab_2 (Accessed 4 September 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.