Abstract
Background
The advent of fractionated picosecond (ps) lasers has provided an opportunity to explore new ways of creating microinjuries in the skin to induce skin rejuvenation.
Objective
To compare the efficacy and safety of diffractive optical element (DOE)-assisted ps neodymium: yttrium-aluminum-garnet (Nd:YAG) lasers with 532-nm and 1,064-nm wavelengths (532-nm and 1,064-nm Nd:YAG P-DOE) using a novel fractional handpiece for the treatment of photoaged skin.
Methods
An ex vivo guinea pig skin experiment was performed by evaluating the histology of the skin after 532-nm Nd:YAG P-DOE irradiation. A randomized, prospective, split-face study was performed on eight subjects with 532-nm and 1,064-nm Nd:YAG P-DOE.
Results
Based on the histological evaluation using ex vivo guinea pig skin, a reasonable safety profile and the potential to generate effective skin rejuvenation was observed using the 532-nm Nd:YAG P-DOE. Results demonstrated that both 532- and 1,064-nm Nd:YAG P-DOE were similarly effective in improving skin texture and skin pores; however, 532-nm Nd:YAG P-DOE was more effective in treating dyspigmentation.
Conclusion
At a preliminary level, this study revealed that 532-nm and 1,064-nm ps Nd:YAG lasers using DOE fractional technology may improve photoaged skin. In conclusion, 532-nm Nd:YAG P-DOE may be especially beneficial for skin with epidermal pigmentary lesions.
Keywords: Asian, Lasers, Rejuvenation, Skin aging
INTRODUCTION
Skin photoaging manifests as changes in skin texture, dyspigmentation, enlarged skin pores, and wrinkles. Until now, various laser treatments, such as long-pulsed 1064-nm neodymium:yttrium-aluminum-garnet (Nd:YAG) lasers, have been widely used for skin rejuvenation. Recently, the advent of fractionated picosecond (ps) lasers has provided an opportunity to explore new ways of creating microinjuries in the epidermis and dermis, known as “laser-induced optical breakdown (LIOB),” with minimal adjacent tissue damage. LIOB is a unique histologic finding that is induced by a fractionated ps laser, which is the result of multiphoton ionization due to high temperature and pressure created by high-energy irradiances with extremely short pulse durations1. This may confer superior healing characteristics, which are beneficial for skin rejuvenation, especially when treating pigmented skin types2,3,4. Improvements in skin appearance following treatment with fractionated ps lasers have been previously reported, most of which used ps Nd:YAG lasers with a 1,064-nm wavelength3,5,6,7,8,9,10.
Commercially available Nd:YAG ps lasers can emit both 532-nm and 1,064-nm wavelengths and create fractionated arrays; however, 532-nm ps Nd:YAG lasers alone have seldom been used for dermal remodeling. This is because the 532-nm wavelength has a limited depth of penetration relative to the 1,064-nm wavelength, although it selectively targets melanin. To create fractionated arrays, microlens arrays (MLAs) or diffractive optical elements (DOEs) are used11. Although, currently, MLA is more commonly used, DOE has the advantage of creating a more uniform distribution of the microbeams. Recently, a novel DOE fractional handpiece for ps Nd:YAG lasers was devised using a new technology patented in the Republic of Korea (Patent No. 101042687000 [KR]). This technology allows for the stable implementation of high-power irradiation of a specific target at the desired depth using both 1,064-nm and 532-nm wavelengths.
Herein, we performed a split-face study to compare the efficacy and safety of a DOE-assisted ps Nd:YAG laser (P-DOE) with a 532-nm wavelength (532-nm Nd:YAG P-DOE) and DOE-assisted ps Nd:YAG laser (P-DOE) with a 1064-nm wavelength (1,064-nm Nd:YAG P-DOE) for the treatment of photoaged skin. Furthermore, we evaluated the histological patterns induced by 532-nm Nd:YAG P-DOE treatment in ex vivo guinea pig skin tissue to achieve a comprehensive understanding of the specific skin response.
MATERIALS AND METHODS
Ex vivo guinea pig skin experiment
1) Laser irradiation
To explore the effect of 532-nm Nd:YAG P-DOE treatment on dermal remodeling and the risk of damages to the epidermal and dermo-epidermal junction (DEJ), the 532-nm Nd:YAG P-DOE treatment using a ps-laser system (PicoLO™; Laseroptek, Seongnam, Korea) was employed on ex vivo guinea pig skin (Hartley) prior to in vivo application on human skin. A single pulse of 532-nm Nd:YAG P-DOE treatment with a total energy of 73 mJ or 122 mJ was performed. We used two different fluences to evaluate the effects of different energy settings. A 532-nm handpiece equipped with DOE fractional technology (focal length=200 mm, 81 microbeams, spot size=7×7 mm) was used to generate multiple microbeams. Thus, the microbeam energy was between 0.9 mJ/microbeam and 1.5 mJ/microbeam.
2) Histopathology and immunohistochemistry
To evaluate the formation of LIOB, all treated tissue samples were collected 10 minutes after laser irradiation (LIOB is known to occur most frequently within 10 minutes of laser irradiation), fixed in 3.7% formalin (Sigma Aldrich, St Louis, MO, USA), sectioned into 5 µm, and stained with hematoxylin-eosin (H&E).
To evaluate the wound healing process and collagen deposition, all treated tissue samples were collected after 10 minutes and 1, 7, 14, and 28 days of laser irradiation. Inflammatory cell (macrophage and neutrophil) infiltration, morphological changes, and tissue damage were observed using H&E, Masson trichrome, Victoria blue staining, and collagen type I immunostaining were performed to evaluate dermal remodeling.
In vivo clinical pilot experiment
1) Study design and patient enrollment
Based on the results of ex vivo experiment, a randomized, prospective, split-face, evaluator-blinded study was performed to compare the clinical outcomes of 1,064-nm vs. 532-nm Nd:YAG P-DOE treatment in accordance with the Declaration of Helsinki. The Institutional Review Board at Chung-Ang University Hospital approved all study protocols, informed consent forms, and relevant supporting data (IRB No. 2092-002-433). After obtaining informed consent, each subject received a single treatment session on each side of their faces and were followed up after 2 weeks.
Eight subjects from the Republic of Korea (all women, aged 24~50 years, four with Fitzpatrick skin type III, and four with type IV) were enrolled. Subjects were excluded from the study if they had received any other laser treatment 6 months before study enrollment. None of the subjects underwent other treatments (chemical, mechanical, or laser resurfacing) during the study period. The exclusion criteria included a history of hypertrophic scar or keloid formation, concomitant systemic diseases, immunosuppressed condition, or presence of skin tumors.
2) Laser irradiation
After random subject allocation, half of their face was treated with 1,064-nm Nd:YAG P-DOE and the other half with 532-nm Nd:YAG P-DOE. Before laser irradiation, a lidocaine-based topical anesthetic cream (EMLA; AstraZeneca, London, UK) was applied to the entire face for 30 minutes. The parameters used for the 532-nm Nd:YAG P-DOE treatment were fluence, 0.2 J/cm2 (1.2 mJ/microbeam); spot size, 7×7 mm; frequency, 10 Hz; and two passes; while those for the 1,064-nm Nd:YAG P-DOE treatment were fluence, 0.25 J/cm2 (3.1 mJ/microbeam); spot size, 10×10 mm; frequency, 10 Hz; and 3~4 passes (until the clinical endpoints of mild erythema and edema were reached).
3) Clinical outcome assessment
Photographs of each subject were taken at baseline, immediately after completing laser therapy, and after 2 weeks of treatment using an imaging tool (MarkVu®; PSI PLUS, Suwon, Korea). Images were graded by two blinded dermatologists who rated the global improvement and improvement in skin texture, dyspigmentation, pore size, fine lines/wrinkles, and skin laxity from baseline, using a five-point scale (failure, grade 0=no improvement; mild, grade 1=1%~25% improvement; moderate, grade 2=26%~50% improvement; good, grade 3=51%~75% improvement; and excellent, grade 4=76%~100% improvement). In addition, changes in melanin components were recorded in photographs captured using the ultraviolet (UV)-ray mode of the MarkVU® system.
Subjects were also asked to rate their satisfaction for each side of their face using a five-point Likert scale. The subjects were asked about any irritation during the laser treatment. At the end of each session, clinicians observed the treated sites, and any early skin reactions to the laser treatment were recorded. Other postprocedural complaints after treatment, such as pinpoint bleeding, hyperpigmentation, and secondary scarring, were also documented. We received the patient’s consent form about publishing all photographic materials.
Statistical analyses
All statistical analyses were performed using the SPSS package (SPSS for Windows, version 24.0; IBM Corp., Armonk, NY, USA). The Wilcoxon signed-rank test was used to compare the efficacy of 532-nm and 1,064-nm Nd:YAG P-DOE treatments. Statistical significance was set at p<0.05.
RESULTS
Ex vivo guinea pig skin experiment
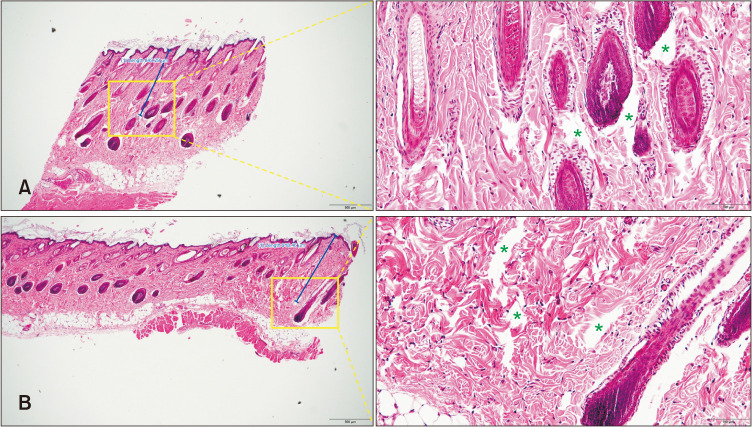
Fig. 1 shows H&E staining images of the skin after 532-nm Nd:YAG P-DOE irradiation at 73 mJ and 122 mJ. The LIOB was generated under all conditions. A single pulse of 532-nm Nd:YAG P-DOE treatment with a total energy of 73 mJ elicited intradermal LIOBs, ranging from 861.15 µm to 1,229 µm in depth (average 979.81±215.88 µm) and 1,752.49±128.34 µm2 in size. With a total energy of 122 mJ, intradermal LIOBs, ranging from 600.66 µm to 918.46 µm in depth (average 708.19±148.98 µm) and 1,434.20±136.17 µm2 in size were formed.
Fig. 1. Histological analysis of guinea pig skin tissue after irradiation with 532-nm Nd:YAG P-DOE at a fluence of 73 mJ and 122 mJ. LIOB is marked with a light green asterisk. (A) with a fluence of 73 mJ. LIOBs were formed at a depth of 861.15~1,229 µm with a size of 1,752.49±128.34 µm2 (H&E stain, left: ×40, right: ×200), (B) with a fluence of 122 mJ. LIOBs were formed at a depth of 600.66~918.46 µm with a size of 1,434.20±136.17 µm2. Lower energy irradiation induced LIOB formation at a deeper layer of the dermis (H&E stain, left: ×40, right: ×200). Nd:YAG: neodymium:yttrium-aluminum-garnet, Nd:YAG P-DOE: diffractive optical element-assisted picosecond Nd:YAG laser, LIOB: laser-induced optical breakdown.
In both specimens, no intraepidermal LIOBs were found, and there was no damage to the stratum corneum, epidermis, or DEJ. LIOBs were observed immediately after laser irradiation for 14 days after treatment. Furthermore, 7 days after laser irradiation, macrophage infiltration was observed, and neocollagenesis and neoelastinogenesis were observed until 28 days after laser irradiation (Fig. 2). Masson trichrome and victoria blue staining revealed deposition of de novo collagen and elastic fibers 7 days after laser irradiation. Compared with the baseline biopsies, an increase in dermal collagen (greater in volume and denser spaces) and elastic fibers were noted. Immunohistochemical staining for type I collagen further supported this finding (Supplementary Fig. 1).
Fig. 2. Histological analysis of guinea pig skin tissue after 10 minutes, and 7, 14, and 28 days of laser irradiation with 532-nm Nd:YAG P-DOE at a fluence of 73 and 122 mJ (H&E, ×200). Seven days after laser irradiation, macrophage infiltration was observed, and neocollagenesis and neoelastinogenesis were observed until 28 days after laser irradiation (LIOB marked as green asterisk; neocollagenesis and neoelastinogenesis marked as yellow asterisks). Nd:YAG: neodymium:yt trium-aluminum-garnet, Nd:YAG P-DOE: diffractive optical element-assisted picosecond Nd:YAG laser, LIOB: laser-induced optical breakdown.
In vivo clinical pilot experiment
1) Clinical outcome
In total, eight subjects completed the study. All subjects (100%) were female, and the mean age of the subjects was 38±8.8 years (range, 24~50 years). Four subjects (50.0%) had Fitzpatrick skin type III, and four (50.0%) had type IV skin. After 2 weeks of laser treatment, global improvement from baseline was moderate (average score of 2) for the 532-nm Nd:YAG P-DOE-treated side and mild-to-moderate (average score of 1.875) for the 1,064-nm Nd:YAG P-DOE-treated side (Fig. 3). The improvement in skin texture was moderate (average score of 2) for the 532-nm Nd:YAG P-DOE-treated side and mild-to-moderate (average score of 1.875) for the 1,064-nm Nd:YAG P-DOE-treated side. Improvement of dyspigmentation was moderate (average score of 2) for the 532-nm Nd:YAG P-DOE-treated side and mild (average score of 1.125) for the 1,064-nm Nd:YAG P-DOE-treated side. The improvement in pore size was moderate (average score of 2) for the 532-nm Nd:YAG P-DOE-treated side and mild-to-moderate (average score of 1.75) for the 1,064-nm Nd:YAG P-DOE-treated side. Improvement of fine wrinkles and skin laxity were all less than mild (average score of 0.75) for both the 532-nm and 1,064-nm Nd:YAG P-DOE-treated side. Statistical analysis revealed significant differences between the 532-nm and 1,064-nm Nd:YAG P-DOE-treated sides in improving dyspigmentation, favoring 532-nm Nd:YAG P-DOE. However, in all other evaluated aspects, there was no significant difference between the 532-nm and 1,064-nm Nd:YAG P-DOE-treated sides.
Fig. 3. Results of blinded photographic evaluation of global improvement, skin texture, dyspigmentation, pore size, fine lines/wrinkles, and skin laxity. Images of patients were graded by two blinded dermatologists using a five-point scale (failure, grade 0=no improvement; mild, grade 1=1%~25% improvement; moderate, grade 2=26%~50% improvement; good, grade 3=51%~75% improvement; and excellent, grade 4=76%~100% improvement). Moderate improvement in the global improvement, skin texture, dyspigmentation, and pore size were observed for the 532-nm Nd:YAG P-DOE-treated side and mild-to-moderate improvement were observed for the 1,064-nm Nd:YAG P-DOE-treated side. Significant difference was observed in dyspigmentation (*). Mild improvement were observed in the fine lines/wrinkles and skin laxity. Nd:YAG: neodymium:yttrium-aluminum-garnet, Nd:YAG P-DOE: diffractive optical element-assisted picosecond Nd:YAG laser.
Representative clinical photographs and images captured using the UV-ray mode are shown in Fig. 4. In subject 1, both sides of the face treated with 532-nm and 1,064-nm Nd:YAG P-DOE showed good improvement with respect to visible pores, skin texture, and pigmentation (Fig. 4A). In subject 2, both sides of the face showed good improvement with respect to visible pores, skin texture, and skin laxity, but a more significant improvement of melasma was observed on the 532-nm Nd:YAG P-DOE-treated side of the face (Fig. 4B). Most subjects reported a degree of satisfaction with both treatments (average satisfaction score of 0.75, both 532-nm and 1,064-nm Nd:YAG P-DOE treated sides of the face). There were no significant differences in subject satisfaction between the two groups.
Fig. 4. Representative clinical photographs (upper) and images captured using the ultraviolet-ray mode (lower) after treatment with 534-nm and 1,064-nm Nd:YAG P-DOE. (A) In subject 1, mild improvement in skin texture and pigmentation and marked improvement in pore size were noted on both sides of the face. (B) In subject 2, mild improvement in skin texture and pore size was noted on both sides, but more improvement in pigmentation was noted on the 532-nm P-DOE-treated side of the face. Nd:YAG: neodymium:yttrium-aluminum-garnet, Nd:YAG P-DOE: diffractive optical element-assisted picosecond Nd:YAG laser.
2) Adverse events
All subjects developed transient erythema and burning sensations that lasted 2~3 days on both sides of the face. One subject (with Fitzpatrick skin type IV) developed hyperpigmentation similar to a tiger mask that commonly occurs after intense pulsed light treatment on the facial half that was treated with a 532-nm Nd:YAG P-DOE (Fig. 5A), and it was improved after 2 months only with a sun-protection (Fig. 5B). No other adverse reactions were reported in any of the subjects.
Fig. 5. (A) One subject developed hyperpigmentation on the mandibular area similar to tiger mask-like hyperpigmentation, which commonly occurs after intense pulsed light treatment, on the facial half that was treated with a 532-nm Nd:YAG P-DOE. (B) Improved after 2 months with sun-protection. Nd:YAG: neodymium:yttrium-aluminum-garnet, Nd:YAG P-DOE: diffractive optical element-assisted picosecond Nd:YAG laser.
DISCUSSION
The fractionated ps laser creates numerous microbeams in which each beam emits a very high fluence with a low fluence background. Therefore, it preserves the surrounding skin with minimal thermal injury compared with the bare beam. To create a fractionated array using ps-domain Nd:YAG lasers, an MLA is commonly used11. However, MLA concentrates the maximum energy at the center and the intensity decreases at both tails because of the intrinsic optical features of non-uniform beam spreading12. In contrast, incident laser light is homogenized by DOE as a holographic beam, creating uniform distributions of the microbeams. The light homogenization from the DOE results in a more uniform delivery of the microbeams compared with that with MLA. In a previous study, irradiation of ex vivo porcine skin confirmed that irradiation using DOE generated more homogenous microbeams (deviation of ≤3%) compared with irradiation using MLA (deviation of ~26%). These results suggest that DOE-assisted ps laser irradiation may allow for more effective fractional skin treatment because it can achieve more uniform vacuolization1. However, a major drawback of the DOE system is energy loss. Due to beam homogenization, DOE accompanied a 15% energy loss when compared to MLA1. Previous ex vivo studies have reported that ps laser irradiation with DOE resulted in small vacuoles (~50 µm), which were restricted to the epidermis of human skin2,4. Kim et al.1 also showed that with the same energy, DOE generated smaller, shallower vecuoles relative MLA in the dermis on ex vivo porcine skin.
Therefore, the major limitation of the use of DOE in fractional ps laser for skin rejuvenation (which requires intradermal LIOB formation) is the insufficient pulse energy.
The principal mechanism of the fractionated ps laser in skin rejuvenation is the development of LIOB. This localized damage is known to be associated with dermal remodeling by increasing dermal collagen and elastin13,14,15. Yeh et al.16 showed that the 532-nm Nd:YAG P-DOE treatment can create LIOB in the dermal layer in ex vivo studies conducted on Asian human skin. Consistent with previous studies, our ex vivo guinea pig skin experiment showed LIOB formation in the dermis. Notably, 532-nm Nd:YAG P-DOE treatment elicited intradermal LIOB under the basal membrane while leaving the epidermis intact. Additionally, previous studies using fractionated Nd:YAG P-DOE lasers have reported hemorrhages associated with damage to superficial blood vessels or an LIOB involving the DEJ4. In contrast, hemorrhage was not observed in our histological evaluation. Finally, neocollagenesis and neoelastinogenesis were observed 7 days after laser irradiation, which was further confirmed by special staining of the specimen. Therefore, based on the histological evaluation, a reasonable safety profile and the potential to generate effective skin rejuvenation using a 532-nm Nd:YAG P-DOE lasers was confirmed. Interestingly, in our study, lower energy irradiation induced LIOB formation at deeper layers of the dermis, which is consistent with the results of previous studies16. The underlying mechanism has been suggested as follows: When a low-energy laser beam which cannot reach the threshold for intraepidermal LIOB formation bypasses the epidermis and reaches the dermis, it induces intradermal LIOB formation. In contrast, when a high-energy laser beam passes the threshold for intraepidermal LIOB formation, a large portion of energy is absorbed by the plasma surrounding the LIOBs, and only the little remaining energy can reach the dermis.
Next, we performed a pilot clinical study to compare the clinical efficacy of 532-nm and 1,064-nm Nd:YAG P-DOE for skin rejuvenation. The results demonstrated that both treatments were similarly effective in improving skin texture and skin pores; however, 532-nm Nd:YAG P-DOE was more effective in treating dyspigmentation. We assume that this may be because the 532-nm wavelength has a higher absorption coefficient for melanin and lower absorption coefficient for hemosiderin than those for the 1,064-nm wavelength17. Despite this advantage, the use of 532-nm lasers has been limited because the short wavelength cannot penetrate as deep as other longer wavelengths, thus leading to a higher incidence of side effects, such as dyspigmentation and scarring18,19. However, the use of a DOE fractional handpiece allowed us to overcome this major drawback of 532-nm lasers. MLA is prone to bleeding due to the concentration of energy, and the depth of the laser beam is not adjusted according to the position of the lens. DOE allows the laser beam to reach a predetermined depth according to the pre-designed cross-sectional view. In this study, although only a single treatment session was performed, a greater improvement in dyspigmentation was noted in the 532-nm Nd:YAG P-DOE-treated side compared with the 1,064-nm Nd:YAG P-DOE-treated side. Therefore, we suggest that 532-nm Nd:YAG P-DOE may be more suitable for patients with significant baseline pigmentation, which merits further study using multiple treatment sessions with longer follow-up periods.
Despite the advantages and potential of 532-nm Nd:YAG P-DOE treatment, it must also be noted that one subject (with Fitzpatrick skin type IV) in our study developed hyperpigmentation similar to tiger mask-like hyperpigmentation on the mandibular area after treatment with 532-nm Nd:YAG P-DOE. The physician who performed the laser treatment later reported that it appeared that the tip of the handpiece failed to completely adhere to the skin surface during laser treatment, especially when treating around the edge of the face. This incomplete adhesion of the laser handpiece may have decreased the targeted focal depth of laser irradiation, and thus may have targeted the epidermis and DEJ rather than the dermis, leading to unwanted side effects. Therefore, it must be emphasized that to maximize treatment efficacy and avoid side effects, the tip of the handpiece must be completely in contact with the skin surface to create LIOB at the targeted depth. Since it is difficult to control the laser handpiece on the edge of the face, such as under the chin or in the mandibular area, physicians must pay more attention when treating these areas. Furthermore, increased melanin indices and high fluence are associated with larger, more numerous, and superficially located LIOBs. Therefore, when treating patients with darker skin, physicians should be particularly careful and may adjust to a lower energy fluence to prevent the risk of postinflammatory hyperpigmentation.
The major limitation of this study is that we only performed a single treatment with a very short follow-up period. Since it is known that tissue remodeling can continue until 1-year during the wound healing process, a one-month period for histological evaluation and clinical evaluation 2 weeks after treatment may not be enough to capture the full range of changes in tissue remodeling. However, previous histological studies evaluating the wound healing process have shown that fibroblasts start to migrate and produce new collagen from days 5~7, and that significant neocollagenesis and neoelastinogenesis were histopathologically proven from 2 weeks after ps laser irradiation in various studies, supporting the clinical results of our study20,21,22,23. Nonetheless, based on the results of this pilot study, additional larger studies with at least 6 months of follow-up are warranted in the future. Furthermore, although we observed histological changes after 532-nm Nd:YAG P-DOE irradiation in an ex vivo guinea pig skin model, ex vivo tissue may not accurately reflect various factors in in vivo human tissue. Therefore, future histological studies involving in vivo human skin are necessary to evaluate the dependence of DOE-induced LIOB on human skin with various melanin contents and distributions. The small number of participants (8 patients) was another limitation of our study. Despite these limitations, our pilot clinical and histopathological study supports the use of ps-domain Nd:YAG laser irradiation with both 532-nm and 1,064-nm wavelengths using DOE fractional technology as a viable treatment option for skin rejuvenation.
The results of our histological and clinical study demonstrated that 532-nm and 1,064-nm ps-domain Nd:YAG lasers using DOE fractional technology may improve photoaged skin and that 532-nm Nd:YAG P-DOE may be especially beneficial for skin with greater baseline pigmentation. Treatments were well tolerated, and patient satisfaction was moderate, which is consistent with the positive outcomes of fractionated ps laser treatments reported in the literature.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
FUNDING SOURCE: This work was funded by Laseroptek Inc.
DATA SHARING STATEMENT
Research data are not shared.
SUPPLEMENTARY MATERIALS
Supplementary data can be found via http://anndermatol.org/src/sm/ad-22-070-s001.pdf.
Histological images of Masson trichrome (×40), and Victoria blue staining (×40) and immunohistochemical (IHC) staining for type I collagen (×40) of guinea pig skin tissue after 10 minutes, and 7 days of laser irradiation with 532-nm Nd:YAG P-DOE at a fluence of 73 and 122 mJ. Compared with the baseline, increases in dermal collagen and elastic fibers were noted.
References
- 1.Kim H, Hwang JK, Jung M, Choi J, Kang HW. Laser-induced optical breakdown effects of micro-lens arrays and diffractive optical elements on ex vivo porcine skin after 1064 nm picosecond laser irradiation. Biomed Opt Express. 2020;11:7286–7298. doi: 10.1364/BOE.410991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tanghetti EA. The histology of skin treated with a picosecond alexandrite laser and a fractional lens array. Lasers Surg Med. 2016;48:646–652. doi: 10.1002/lsm.22540. [DOI] [PubMed] [Google Scholar]
- 3.Wat H, Yee-Nam Shek S, Yeung CK, Chan HH. Efficacy and safety of picosecond 755-nm alexandrite laser with diffractive lens array for non-ablative rejuvenation in Chinese skin. Lasers Surg Med. 2019;51:8–13. doi: 10.1002/lsm.23014. [DOI] [PubMed] [Google Scholar]
- 4.Tanghetti Md E, Jennings J. A comparative study with a 755 nm picosecond Alexandrite laser with a diffractive lens array and a 532 nm/1064 nm Nd:YAG with a holographic optic. Lasers Surg Med. 2018;50:37–44. doi: 10.1002/lsm.22752. [DOI] [PubMed] [Google Scholar]
- 5.Zhang M, Huang Y, Wu Q, Lin T, Gong X, Chen H, et al. Comparison of 1064-nm and Dual-Wavelength (532/1064-nm) Picosecond-domain Nd:YAG lasers in the treatment of facial photoaging: a randomized controlled split-face study. Lasers Surg Med. 2021;53:1158–1165. doi: 10.1002/lsm.23404. [DOI] [PubMed] [Google Scholar]
- 6.Yu W, Zhu J, Yu W, Shang Y, Lyu D, Lin X, et al. Three-year results of facial photoaging in asian patients after alexandrite 755 nm picosecond laser with diffractive lens array: a split-face, single-blinded, randomized controlled comparison. Lasers Surg Med. 2021;53:1065–1072. doi: 10.1002/lsm.23393. [DOI] [PubMed] [Google Scholar]
- 7.Wong CSM, Chan MWM, Shek SYN, Yeung CK, Chan HHL. Fractional 1064 nm picosecond laser in treatment of melasma and skin rejuvenation in Asians, a prospective study. Lasers Surg Med. 2021;53:1032–1042. doi: 10.1002/lsm.23382. [DOI] [PubMed] [Google Scholar]
- 8.Manuskiatti W, Yan C, Tantrapornpong P, Cembrano KAG, Techapichetvanich T, Wanitphakdeedecha R. A prospective, splitface, randomized study comparing a 755-nm picosecond laser with and without diffractive lens array in the treatment of melasma in Asians. Lasers Surg Med. 2021;53:95–103. doi: 10.1002/lsm.23312. [DOI] [PubMed] [Google Scholar]
- 9.Kim YJ, Suh HY, Choi ME, Jung CJ, Chang SE. Clinical improvement of photoaging-associated facial hyperpigmentation in Korean skin with a picosecond 1064-nm neodymium-doped yttrium aluminum garnet laser. Lasers Med Sci. 2020;35:1599–1606. doi: 10.1007/s10103-020-03008-z. [DOI] [PubMed] [Google Scholar]
- 10.Lee CH, Jin EM, Seo HS, Ryu TU, Hong SP. Efficacy and safety of treatment with fractional 1,064-nm picosecond laser with diffractive optic element for wrinkles and acne scars: a clinical study. Ann Dermatol. 2021;33:254–262. doi: 10.5021/ad.2021.33.3.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang CY, Chen CC. Serial change in laser-induced optical breakdown by 1064-nm Nd:YAG picosecond laser. Photodermatol Photoimmunol Photomed. 2020;36:63–64. doi: 10.1111/phpp.12505. [DOI] [PubMed] [Google Scholar]
- 12.Lee HC, Childs J, Chung HJ, Park J, Hong J, Cho SB. Pattern analysis of 532- and 1,064-nm picosecond-domain laser-induced immediate tissue reactions in ex vivo pigmented micropig skin. Sci Rep. 2019;9:4186. doi: 10.1038/s41598-019-41021-7. Erratum in: Sci Rep 2019;9:18372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanghetti EA, Tartar DM. Comparison of the cutaneous thermal signatures over twenty-four hours with a picosecond alexandrite laser using a flat or fractional optic. J Drugs Dermatol. 2016;15:1347–1352. [PubMed] [Google Scholar]
- 14.Habbema L, Verhagen R, Van Hal R, Liu Y, Varghese B. Minimally invasive non-thermal laser technology using laser-induced optical breakdown for skin rejuvenation. J Biophotonics. 2012;5:194–199. doi: 10.1002/jbio.201100083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brauer JA, Kazlouskaya V, Alabdulrazzaq H, Bae YS, Bernstein LJ, Anolik R, et al. Use of a picosecond pulse duration laser with specialized optic for treatment of facial acne scarring. JAMA Dermatol. 2015;151:278–284. doi: 10.1001/jamadermatol.2014.3045. [DOI] [PubMed] [Google Scholar]
- 16.Yeh YT, Peng JH, Peng P. Histology of ex vivo skin after treatment with fractionated picosecond Nd:YAG laser in high and low-energy settings. J Cosmet Laser Ther. 2020;22:43–47. doi: 10.1080/14764172.2019.1710536. [DOI] [PubMed] [Google Scholar]
- 17.Guss L, Goldman MP, Wu DC. Picosecond 532 nm neodymium-doped yttrium aluminium garnet laser for the treatment of solar lentigines in darker skin types: safety and efficacy. Dermatol Surg. 2017;43:456–459. doi: 10.1097/DSS.0000000000000922. [DOI] [PubMed] [Google Scholar]
- 18.Al-Dhalimi MA, Al-Janabi MH. Split lesion randomized comparative study between long pulsed Nd:YAG laser 532 and 1,064 nm in treatment of facial port-wine stain. Lasers Surg Med. 2016;48:852–858. doi: 10.1002/lsm.22584. [DOI] [PubMed] [Google Scholar]
- 19.Lee YJ, Shin HJ, Noh TK, Choi KH, Chang SE. Treatment of melasma and post-inf lammatory hyperpigmentation by a picosecond 755-nm alexandrite laser in Asian patients. Ann Dermatol. 2017;29:779–781. doi: 10.5021/ad.2017.29.6.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santos TS, Santos IDDD, Pereira-Filho RN, Gomes SVF, Lima-Verde IB, Marques MN, et al. Histological evidence of wound healing improvement in rats treated with oral administration of hydroalcoholic extract of Vitis labrusca. Curr Issues Mol Biol. 2021;43:335–352. doi: 10.3390/cimb43010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O Connor K, Cho SB, Chung HJ. Wound healing profile after 1064- and 532-nm picosecond lasers with microlens array of in vivo human skin. Lasers Surg Med. 2021;53:1059–1064. doi: 10.1002/lsm.23390. [DOI] [PubMed] [Google Scholar]
- 22.Kim HK, Kim HJ, Hong JY, Park J, Lee HC, Lyu H, et al. Interactive tissue reactions of 1064-nm focused picosecond-domain laser and dermal cohesive polydensified matrix hyaluronic acid treatment in in vivo rat skin. Skin Res Technol. 2020;26:683–689. doi: 10.1111/srt.12853. [DOI] [PubMed] [Google Scholar]
- 23.Nakano S. Histological investigation of picosecond laser-toning and fractional laser therapy. Laser Ther. 2020;29:53–60. doi: 10.5978/islsm.20-OR-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Histological images of Masson trichrome (×40), and Victoria blue staining (×40) and immunohistochemical (IHC) staining for type I collagen (×40) of guinea pig skin tissue after 10 minutes, and 7 days of laser irradiation with 532-nm Nd:YAG P-DOE at a fluence of 73 and 122 mJ. Compared with the baseline, increases in dermal collagen and elastic fibers were noted.
Data Availability Statement
Research data are not shared.